Abstract
A 28-year-old male with bilateral testicular seminoma underwent bilateral orchiectomy and radiation therapy of the retroperitoneum. After 17 years, he had a retroperitoneal tumor detected, which was removed 7 years later at age 52 because of its progressive enlargement. Due to its partially cystic and partially solid structure, the radiologic findings could not exclude the possibility of regressively altered seminoma metastasis. After radical surgical removal of the tumor, the histopathological and immunohistochemical examination of the tumor revealed ancient schwannoma. These tumors, although unusual, might pose a clinical diagnostic challenge with the risk of undesired overtreatment.
Keywords: Seminoma metastasis, Retroperitoneal, Ancient schwannoma, Germ cell tumor
1. Introduction
Seminoma, along with other germ cell tumors, usually affects males in the age group between 20 and 40 years, in which they are the most common malignant tumors.1 If confined only to the testicle, the treatment consists of orchiectomy. In adverse course of the disease, patients develop metastases, initially in retroperitoneal sentinel lymph nodes, thereafter in distant lymph nodes and organs. To prevent the metastasis formation or to eradicate ones already formed, the patients may undergo radiation therapy and/or chemotherapy.1
We present a case of a patient initially diagnosed with bilateral testicular seminoma, who underwent orchiectomy and radiation therapy of the retroperitoneum. 17 years following the surgery, the patient has had a progressively enlarging retroperitoneal tumor detected.
2. Case report
2.1. Clinical report
A 28-year-old man was diagnosed with seminoma affecting both his testicles (right - pT2, left - pT1), without signs of metastases in organs, but with a CT finding of an aggregate of lymphatic nodes situated ventrally to vena cava inferior, with diameters of 28 × 17 × 45 mm (clinical stage IIB). Following the bilateral radical orchiectomy, he received radiation therapy with dose of 40 Gy targeting the retroperitoneal lymph nodes, without administration of chemotherapy.
The follow-up CT and USG checkups revealed no apparent recurrence of seminoma. 17 years after the surgery, an abdominal CT scan revealed a hypodense, cyst-like lesion (density 10 HU) without opacification, in the level of vertebra L3, ventrally to the left psoas major muscle, with dimensions of 21 × 20 mm. The lesion was separated from visualized lymphatic nodes (which had no apparent tumor changes) and adjacent organs, however the possibility of a colliquated lymphatic node could not be ruled out. On PET/CT scan, the lesion had an increased uptake of glucose. 7 years later, the abdominal USG check-up revealed significant enlargement of the cystic lesion, which now measured up to 10 cm. On CT measurement, the lesion had dimensions of 102 × 85 × 110 mm, part of the mass had a cystic character, the caudal part was solid and compact (Fig. 1). Of the serum testicular germ cell tumor markers, only alfa-fetoprotein was evaluated, which had value of 3,4 μg/l.
Fig. 1.
PET, CT and PET/CT examination findings (upper row – 17 years after orchiectomy; bottom row – 24 years after orchiectomy). Arrows point towards the enlarging cystic mass in the left retroperitoneum, near the left psoas major muscle.
2.2. Pathological examination
After surgical resection of the retroperitoneal tumor, the specimen grossly consisted of a cystic mass with greatest diameter of 12 cm, the thickness of the cyst wall was 2 mm, and a solid mass attached to the cyst from the outer wall, which was 13 cm long and 1,5 cm thick (Fig. 2). Histopathological evaluation of the mass revealed a tumor composed of spindle-shaped cells with slender nuclei, without cytologic or nuclear atypia (Fig. 3), without increased mitotic activity (Ki-67 < 5%), the cells were growing in bundles, nests, and bands. Some areas were hypercellular, composed predominantly of tumor cells (Antoni A), some areas were hypocellular with abundance of stroma (Antoni B) with edematous and myxoid appearance (Fig. 3). The cystic part of the tumor showed degenerative changes - abundance of fibrous connective tissue, hyalinization, giant cell inflammatory reaction, signs of hemorrhages. Vessels had a thickened, hyalinized walls, no apparent vascular invasion by the tumor cells was identified (Fig. 3). The immunohistochemical profile (positivity of vimentin, S100, SOX10, CD56; negativity of AE1/3, SMA, desmin, CD34, CD117, EMA, inhibin, PLAP, CD30, AFP) and histomorphological picture of the tumor are typical for the diagnosis of schwannoma, due to the extensive degenerative changes termed ancient schwannoma.
Fig. 2.
Resected specimen with cystic part (black arrows) and solid part (blue arrows) after grossing. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
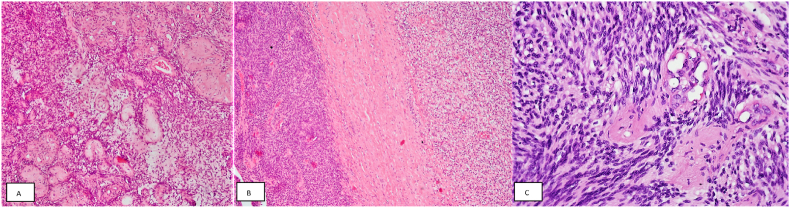
Fig. 3.
A Markedly thickened hyalinized vessels surrounded by tumor cells (HE, 100x). B Hypercellular area (Antoni A – left) and hypocellular area with edematous stroma (Antoni B – right) separated by broad, dense connective tissue band (HE, 100x). C Spindle-shaped tumor cells with bland nuclei, without cytologic or nuclear atypia, growing in bundles in Antoni A area (HE, 400x).
3. Discussion
Schwannoma is a benign tumor derived from the Schwann cells, which surround majority of peripheral nerves. It can originate from any nerve covered by the Schwann cells, approximately in one third of cases in the head and neck region.2 Its occurrence in the retroperitoneum is rare (0,7–2,7% of all schwannomas), nevertheless it is the most frequent benign nerve tumor of the retroperitoneum.2 Its benign behavior is emphasized by an encapsulated, long-term growth, where the potential problems arise due to compression of adjacent structures. Histologically, schwannomas are composed of spindle-shaped cells, characteristically with alternation of highly cellular (Antoni A) and less cellular areas with predominance of stroma (Antoni B).3 Numerous variants and growth patterns have been described in schwannomas, the ancient variant is one of the more infrequent types. First described in 1951, it is believed to be a result of extensive degenerative changes occurring during the tumor growth as an indirect result of vascular insufficiency affecting the tumor mass. The described degenerative changes include edema, fibrosis, hyalinization, calcification, inflammation, xanthomatous changes and necrosis, the latter ones can result in a cystic space formation.2
Despite the impressive size it can reach, schwannoma is a benign tumor (with very rare rate of malignant transformation) and usually the surgical removal is curative.2 In schwannomas with extensive degenerative changes, the radiologic features might not be always sufficient for distinguishing between a malignant and a benign lesion.4 Auxiliary methods such as fine-needle aspiration cytology might prove false results, therefore the diagnosis should be confirmed on a resected specimen.
Metastases of malignant tumors, such as seminoma, pose a grave threat and need to be discerned as such. Unlike majority of malignant tumors, schwannomas do not respond well to chemotherapy nor radiotherapy.4 In patients with testicular cancer, the features distinguishing retroperitoneal metastases and other retroperitoneal tumors could be elevation of germ cell tumor serum markers (alfa-fetoprotein, human chorionic gonadotropin, lactate dehydrogenase) and direct involvement of retroperitoneal sentinel lymph nodes in the tumor mass. If lymph nodes are affected by a tumor mass in a patient with testicular cancer, the location of the lymph node might be helpful in discerning between a metastasis of a testicular tumor and a tumor of another site.5
4. Conclusion
Retroperitoneal mass in a patient with testicular germ cell tumor occurring simultaneously or subsequently is very suspicious of metastasis, which might lead to unjustified radiotherapy or chemotherapy. Ancient retroperitoneal schwannoma is a very rare tumor which can mimic germ cell tumor metastasis, therefore awareness of this rare phenomenon needs to be raised, especially in patients with a medical history of this malignancy.
Authors contributions
SH - Writing - Original Draft, Visualization; ZC - Writing - Original Draft, Investigation, Conceptualization; IK - Writing - Review & Editing, Investigation; VD and MH - Investigation, Resources; MC - Investigation, Resources, Supervision.
Funding
This work was supported by the Slovak Research and Development Agency [grant number APVV-20-0158].
Declaration of competing interest
The authors declare no conflict of interests.
References
- 1.Beyer J., Collette L., Sauvé N., et al. International germ cell cancer classification update consortium. Survival and new prognosticators in metastatic seminoma: results from the IGCCCG-update consortium. J Clin Oncol. 2021 May 10;39(14):1553–1562. doi: 10.1200/JCO.20.03292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choudry H.A., Nikfarjam M., Liang J.J., et al. Diagnosis and management of retroperitoneal ancient schwannomas. World J Surg Oncol. 2009 Feb 2;7:12. doi: 10.1186/1477-7819-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rodriguez F.J., Folpe A.L., Giannini C., Perry A. Pathology of peripheral nerve sheath tumors: diagnostic overview and update on selected diagnostic problems. Acta Neuropathol. 2012 Mar;123(3):295–319. doi: 10.1007/s00401-012-0954-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hamada K., Ueda T., Higuchi I., et al. Peripheral nerve schwannoma: two cases exhibiting increased FDG uptake in early and delayed PET imaging. Skeletal Radiol. 2005 Jan;34(1):52–57. doi: 10.1007/s00256-004-0845-z. [DOI] [PubMed] [Google Scholar]
- 5.Blok J.M., Kerst J.M., Vegt E., et al. Sentinel node biopsy in clinical stage I testicular cancer enables early detection of occult metastatic disease. BJU Int. 2019 Sep;124(3):424–430. doi: 10.1111/bju.14618. [DOI] [PMC free article] [PubMed] [Google Scholar]