Abstract
Background and Objective
Mediastinal thymic cysts are a relatively rare pathology. With the expansion of eligible individuals screened with cross-sectional imaging for lung cancer, it is likely that there will be an increase in the number of individuals presenting with these cysts. Understanding this rare pathology will become more important when this incidental pathology is encountered.
Methods
Search of PubMed was undertaken using keywords “mediastinal”, “mediastinum”, “thymic”, “thymus”, “cyst”. Relevant literature was reviewed and selected for this comprehensive narrative review, including case reports, case series, and retrospective reviews.
Key Content and Findings
Thymic cysts in the mediastinum can be classified into two broad categories, congenital and inflammatory. Accurate diagnosis by imaging is challenging and the majority of patients are asymptomatic. Literature suggests that the majority of cysts are benign, however an unknown percentage may harbor neoplastic processes and over time can cause significant compressive symptoms. Definitive treatment and diagnosis is surgical, with overall excellent outcomes. The decision to pursue surgical treatment versus surveillance requires a shared decision making approach with patients.
Conclusions
Given the scarcity of available high quality evidence regarding the management of mediastinal thymic cysts, this review provides practitioners a broad knowledge base to guide patients to make informed decisions.
Keywords: Mediastinum, thymic, cyst
Introduction
Mediastinal thymic cysts are exceedingly rare and the true incidence is difficult to estimate. In patients undergoing imaging for lung cancer screening, the prevalence of any mediastinal mass was 0.77% and mediastinal thymic cysts were 0.01% (1,2). Other studies have reported that mediastinal thymic cysts represent only 1% to 4% of all mediastinal masses diagnosed (3,4). Because of their relatively scarcity, available evidence regarding thymic cysts within the chest are limited to a few small retrospective observational studies, a number of case series, and a myriad of case reports. Much of the understanding regarding this disease process, including physiology, symptomatology, diagnosis, and treatment has evolved over the decades, and in the context of limited evidence, has been primarily driven by clinical judgment. Despite the low prevalence of this pathology, an increasing number of mediastinal cysts are likely to be incidentally discovered with expansion of lung cancer screening (5). Accordingly, the diagnosis and management of mediastinal thymic cysts will become increasingly important. This chapter will comprehensively discuss mediastinal thymic cysts, including available literature, to give clinicians essential information to best manage this rare pathology. We present the following article in accordance with the Narrative Review reporting checklist (available at https://med.amegroups.com/article/view/10.21037/med-22-25/rc).
Methods
With the low incidence of mediastinal thymic cysts in the population, English language, case reports, case series and retrospective studies of patients were selected from PubMed without date restriction up to June 2022. Search keywords including “mediastinal/mediastinum”, “thymic/thymus”, and “cyst”, were used to select representative literature to highlight the pathophysiology, histology, diagnosis, symptomatology, and treatment of this pathology. Published works focusing solely on cervically located cysts were excluded from inclusion in this narrative review. Referenced sources of selected studies, reports, and series were also reviewed and evaluated for inclusion. These referenced sources were included if they contributed comprehensively to outline the sub-topics above, or if they provided historical value. Table 1 reviews the overall search strategy. Table 2 includes case reports, case series and Table 3 outlines retrospective reviews as an example of the broad date ranges and topics used for selection.
Table 1. Search strategy summary.
| Items | Specification |
|---|---|
| Date of search | June 1st 2022 |
| Databases and other sources searched | PubMed |
| Search terms used | “Mediastinal”, “mediastinum”, “thymic”, “thymus”, “cyst” |
| Example: (mediastinal) OR (mediastinum)) AND ((thymic) OR (thymus)) AND (cyst) | |
| Timeframe | Date unrestricted to July 2022 |
| Inclusion and exclusion criterion | Inclusion: (I) English language; (II) Case reports, case series, retrospective cohort series; (IIII) Focusing on subtopics of: pathophysiology, histology, diagnosis, symptomatology, and treatment; (IV) Studies of historical relevance |
| Exclusion: Studies on cervical located cysts | |
| Selection process | Keaton Cooley-Rieders selected literature, both authors chose those for inclusion |
| Any additional considerations | References of selected studies were reviewed for inclusion |
Table 2. Summary of cited case series (less than 4 patients) and reports.
| Year | Author | Age/sex | Symptoms | Size/type | Location | Surgical approach | Complications | Associated condition |
|---|---|---|---|---|---|---|---|---|
| 1961 | Schillhammer | 14 y/M | Cough | 15 cm, unknown | Right, anterior | Thoracotomy | None | None |
| 29 y/M | Asymptomatic | 13×5 cm, unknown | Anterior | Thoracotomy | None | None | ||
| 44 y/F | Cough | Unknown, unilocular | Right, anterior | Thoracotomy | Ileus | None | ||
| 1976 | Cuasay | 44 y/M | Dyspnea, heart failure | 9×6×5 cm, multilocular | Right, anterior | Thoracotomy | None | Mitral valve replacement |
| 1979 | Moskowitz | 12 y/M | Chest pain | 2 cm, multilocular | Anterior | Mediastinoscopy | Death | Aplastic anemia, E. coli bacteremia |
| 6 y/F | Anemia | 8×8×8 cm, multilocular | Left, anterior | Mediastinoscopy | Stridor, death | Aplastic anemia | ||
| 1983 | Dunne | 27 y/F | Anemia | 3×5 cm, unknown | Right, anterior | Thoracotomy | None | Aplastic anemia |
| 1984 | Woolley | 55 y/M | Hoarseness, dysphagia | Unknown, unilocular | Anterior | Unknown | None | Vocal cord palsy |
| 1985 | Lindfors | 20 y/F | Adenopathy | 10×7 cm, multilocular | Left | Thoracotomy | None | Hodgkins |
| 19 y/M | Tracheal compression | 9 cm, multilocular | Right, anterior | Thoracotomy | None | Hodgkins | ||
| 39 y/M | Chest pain, hoarseness | 12 cm, multilocular | Left, anterior | Thoracotomy | None | Hodgkins | ||
| 1988 | Davis | 14 y/F | Dyspnea | 4×6 cm, multilocular | Anterior | Sternotomy | None | None |
| 1992 | Fraile | 64 y/M | Asymptomatic | 12 cm, unknown | Anterior | Cervical | None | Horner syndrome |
| 1994 | Borgna-Pignatti | 9 y/unknown | Weight loss, anorexia, shoulder pain | 7.5×5×2.5 cm, multilocular | Anterior, left | Thoracotomy | Recurrence | Non-Hodgkin’s lymphoma |
| 1995 | Leonidas | 11 y/M | Pneumonia | 14×10×5 cm, multilocular | Left, anterior | Thoracotomy | None | HIV |
| 5 y/M | Pneumonia | 5×5×4 cm multilocular | Anterior | Not resected | None | HIV | ||
| 44 y/M | Pneumonia/sepsis | Unknown, multilocular | Anterior | Thoracotomy | None | HIV | ||
| 1995 | Sirivella | 54 y/F | Cough, dyspnea, weight loss | 6×5 cm, multilocular | Anterior | Sternotomy | None | None |
| 34 y/F | Cough, dyspnea, weight loss | 6×7 cm, multilocular | Anterior | Mediastinoscopy biopsy, unknown | Infection after biopsy | Compression of pulmonary artery | ||
| 31 y/M | Cough, dyspnea, weight loss | 7×7 cm, multilocular | Anterior | Sternotomy | Pneumonia | Tracheal shift | ||
| 1996 | Yamashita | 60 y/F | Cough, chest pain | 14×7 cm, multilocular | Right, anterior | Unknown | Recurrence of SCC | Thymic carcinoma |
| 1999 | Silverman | 16 y/M | Fever, weight loss, chest pain | 8×5×3 cm, multilocular | Right, anterior | VATS | None | Seminoma |
| 2000 | Wakely | 58 y/M | Chest pain, right arm numbness | 10×7 cm, multilocular | Anterior | Sternotomy | Renal failure, death | Confused as aortic aneurysm, Langerhans histiocytosis |
| 2001 | Tollefsen | 8 y/F | Neck swelling | 5×10.5 cm, unknown | Right, anterior | Cervical incision | None | None |
| 2004 | Becit | 56 y/M | Chest pain | 34×25×16 cm, unknown | Anterior | Sternotomy | Post-op respiratory failure | Cardiac, lung compression |
| 2004 | Rakheja | 12 y/F | Chest pain, dyspnea | 7.5×5.5×3.5 cm, multilocular | Anterior | Unknown | None | Teratoma |
| 11 y/M | Chest pain, fatigue, flushing | 9×6×3 cm, multilocular | Left, anterior | Unknown | None | Teratoma | ||
| 2005 | Lachanas | 61 y/F | Chest pain, dyspnea | 25 cm, multilocular | Right, anterior | VATS and thoracotomy | None | Lung compression |
| 2006 | Stas | 68 y/M | Dyspnea, cough | 18.5 cm, multilocular | Right, anterior | VATS and thoracotomy | None | SVC, right atrial compression |
| 2007 | Constantacos | 16 y/F | Chest pain | 22×11×2.5 cm, multilocular | Left, anterior | Left VATS | Small Pneumothorax | None |
| 2007 | Eifinger | 5 w/M | Dyspnea | 5×3.5×3.2 cm, multilocular | Anterior | Sternotomy | Hemorrhage into right chest | Thymic hyperplasia |
| 2007 | Iyer | 40 y/M | Chest pain, facial swelling | 3.5×4.9 cm, unknown | Right, paratracheal | Mediastinoscopy | None | SVC compression |
| 2008 | Amanatidou | 5 y/M | Neck swelling | 17×8×6 cm | Left, anterior, cervical | Sternotomy and cervical incision | None | None |
| 2008 | Fujiwara | 52 y/M | Chest pain | 12×8×6 cm, multilocular | Anterior | Unknown | Hemorrhage into cyst | Thymoma |
| 2008 | Tiveron | 79 y/F | Chest pain, dyspnea | 11.5×6.8× 9 cm, unilocular | Anterior | Sternotomy | None | Pericardial effusion |
| 2009 | Efthymiou | 72 y/M | Dizziness | 11×9×3 cm, unilocular | Left, anterior | VATS | None | Tachy-brady syndrome |
| 2009 | Morikawa | 68 y/F | Asymptomatic | 4 cm, multilocular | Right, anterior | VATS | None | Papillary adenocarcinoma, thymoma |
| 2010 | Bruno | 37 y/M | Chest pain, dyspnea, lower extremity edema | 12 cm, unilocular | Right | Thoracotomy | None | Lung compression |
| 2010 | Saito | 55 y/M | Chest pain | 5×4.5 cm, multilocular | Right, Anterior | Sternotomy | Hemorrhage into right chest | None |
| 2011 | Tamango | 15 y/F | Dyspnea, chest pain, facial swelling | 13×10×17 cm, multilocular | Anterior | Clamshell | None | HIV |
| 2011 | Schweigert | 41 y/M | Chest pain, cough, dyspnea | 20 cm, unilocular | Anterior | Sternotomy | None | Thymoma |
| 2012 | Luk | 64 y/F | Syncope | 5.3 cm, unknown | Posterior | VATS and thoracotomy | None | None |
| 2012 | Shi | 47 y/F | Cough, chest pain, facial swelling | 7.1×2.7×8.8 cm, multilocular | Anterior | Unknown | None | HIV |
| 2012 | Stienmuller | 19 y/M | Chest pain, dyspnea | 17.6 x 7.1 x 6.8cm, multilocular | Right, anterior | Sternotomy | None | Hodgkins |
| 2015 | Jennings | 76 y/F | Asymptomatic | 20.5×16.2×10 cm, unilocular | Anterior | Sternotomy | Atrial fibrillation | None |
| 2016 | Kanakis | 15 y/F | Asymptomatic | 16×8 cm, multilocular | Right, Anterior | Sternotomy | None | Pulmonary valve stenosis |
| 2016 | Lee | 55 y/M | Asymptomatic | 10.8×4 cm, multilocular | Anterior | VATS | Hemorrhage into cyst | None |
| 2018 | Gorospe | 43 y/F | Asymptomatic | Unknown, multilocular | Anterior | VATS | None | Sjogrens |
| 2019 | Oda | 44 y/M | Asymptomatic | Unknown, multilocular | Anterior | Subxiphoid, VATS | None | IgG4 disease |
| 2019 | Yano | 42 y/F | Myasthenia | 11 cm, multilocular | Anterior | Subxiphoid, VATS | None | Thymoma |
| 2021 | Alzahran | 22 m/F | Dyspnea | Unknown, unilocular | Right, anterior | Thoracotomy | Post-op respiratory failure | Spontaneous infection |
| 2021 | Feng | 67 y/M | Chest pain | 11×9.7 cm, unilocular | Right | Thoracotomy | Hemorrhage into cyst | None |
| 2021 | Liu | 28 y/M | Asymptomatic | 7.1×8.1 cm | Anterior, right | EBUS aspiration | Sepsis, mediastinitis, pleural effusion | None |
M, male; F, female; w, weeks; m, months; y, years; VATS, video-assisted thoracoscopic surgery; SVC, superior vena cava; HIV, human immunodeficiency virus; SCC, squamous cell carcinoma; EBUS, endobronchial ultrasound.
Table 3. Summary of retrospective series.
| Year | Author | Number of patients | Study objectives | Major findings |
|---|---|---|---|---|
| 1968 | Seltzer | 12 patients (all thymic cysts) | Describe mediastinal thymic cysts | 58% symptomatic (cough and chest pain), all anterior, all multiloculated, 58% right sided, 25% left sided, 17% bilateral |
| 2001 | Choi | 8 (all multilocular thymic cysts) | CT vs. histologic findings | 50% of unilocular appearing cysts on imaging actually multilocular, 83% of solid appear lesions non-neoplastic |
| 2003 | Takeda | 105 patients (30 thymic cysts) | Characterize congenital cysts | Second most common cyst type (28.6%), 97% thymic cysts anterior, average age 43.9, predominantly symptoms: none (60%), chest pain (20%), hoarseness (13%), dyspnea (10%) |
| 2006 | Henschke | 9,263 patients (1 thymic cyst) | Describe incidentally found mediastinal masses from lung cancer CT screening | 0.77% incidence of mediastinal masses, 0.43% anterior located, 0.01% thymic cyst, all asymptomatic |
| 2011 | Weissferdt | 7 (all thymic cysts with associated thymic carcinoma) | Characterize thymic cysts associated with thymic carcinoma | All multilocular, all alive at follow-up (43% with disease), emphasis on importance of surgical resection for diagnosis and treatment of anterior cystic mediastinal masses |
| 2018 | Hwang | 18 (3 thymic cysts) | MRI characterization of anterior mediastinal solid lesions versus cysts | T2 bright and relative enhancement ratio <26.1% associated with increased rate of correct diagnosis of cyst |
| 2018 | Shen | 18 patients (all thymic cysts with thymic carcinoma or thymoma) | Characterize thymic cysts associated with thymic carcinoma and thymoma | All multilocular, all with solid component, 56% patients without cysts on CT, all alive at follow-up (11% with disease), major symptoms: none (39%), chest pain (39%), cough (22%) |
| 2020 | Wang | 282 patients (120 thymic cysts) | Outcomes of VATS resection of cysts | Most common cyst (43%), 98% thymic cysts anterior. 50.7% of all cysts correctly diagnosed with CT. Only 1 thymic cyst with associated thymoma. Low rate of complications (5.7%), low rate of conversion to thoracotomy (1%), no recurrence |
| 2018 | Yoon | 56,358 patients (14 thymic cysts) | Describe incidentally found anterior mediastinal masses from asymptomatic CT scans | 0.73% incidence, 0.03% thymic cysts |
CT, computed tomography; MRI, magnetic resonance imaging; VATS, video-assisted thoracoscopic surgery.
Pathophysiology
Mediastinal thymic cysts were first comprehensively described in 1968 by Ronald Seltzer, a radiologist at the University of Cincinnati, and this seminal article has influenced many subsequent writings on the topic (6). Embryologically, the thymus arises from the 3rd pharyngeal pouch during the 6th week of gestation and 2 weeks later descends and fuses at the midline to its proper position in the anterior chest (7,8). This descent has clinical implications, with ectopic thymic tissue possible anywhere from the hyoid to the diaphragm (9). From some of the largest studies, the anterior mediastinum appears to be the most common location for thymic cysts, however middle and posterior locations are also possible (10).
Originally, it was felt that five types of thymic cysts existed: embryological, involutive, neoplastic, degenerative, and mesenchymal (4). However, more recent studies have suggested that broadly these cysts are more simply classified into unilocular, multilocular, congenital, and acquired (3,11). This classification is supported by a prominent theory regarding the formation of inflammatory multilocular thymic cysts secondary to dilation of Hassall’s corpuscles in response to antigens (12). Accordingly, congenital cysts tend to be unilocular while inflammatory cysts appear multilocular, although exceptions have been reported in literature (4,13-15).
Patients of any age can be impacted by this rare pathology from 4 weeks (16) to 79 years old (17) with no preference towards biological sex (10).
A variety of inflammatory processes have been associated with development of these cysts, including: lupus (13), Sjogrens (18), Human immunodeficiency virus or HIV (19-21), surgery (22), immunoglobulin-G4 disease (23), and bacterial infection (24). Additionally, neoplastic processes associated with development of multilocular cysts are broad, and have included: Thymic carcinoma (12,15,25), Hodgkin’s lymphoma (26,27), Non-Hodgkin’s lymphoma (28), Langerhans histiocytosis (29), thymoma (15,30,31), papillary adenocarcinoma (32), seminoma (33) and, mature teratomas (34).
Although original and newer large studies suggest mediastinal thymic cysts to be a benign pathology (2,10,35) the tremendous number of case reports and case series suggest otherwise, with a clear association between neoplastic processes and inflammatory cysts.
Histology
Histologically, thymic cysts are most readily identified by the inclusion of Hassall’s corpuscles in the cyst wall (22,36-40). These swirl-shaped keratinized structures surrounded by epithelial cells are unique to the thymus (40). Cyst walls are also prominent for fibrous stratified squamous epithelium (8,28). Aspiration of cyst contents usually is non-diagnostic and only lymphocytes are seen (41).
Multilocular cysts microscopically contain numerous cystic spaces lined with squamous epithelium (12,26). Additionally, these spaces are prominent for their inflammatory changes which can include necrosis, cholesterol granulomas, fibrosis, germinal centers, calcifications, and hemorrhage (7,13,16,42-45).
Based on underlying inflammatory process driving cyst formation, additional histologic findings can be observed, such as Reed Sternberg cells in Hodgkin’s lymphoma (26,27), cuboidal or columnar cells in papillary adenocarcinoma (32), dense oval cells with central nuclei in seminoma or thymoma (15,30,33), myofibroblasts in teratoma (34), follicular hyperplasia in HIV (21), and nests of spindle, basaloid, papillary, and squamous cells in thymic carcinoma (12,25).
Diagnosis
CT (computed tomography) imaging, preferably with contrast, is frequently obtained in the evaluation of mediastinal masses. Based on the largest series analyzing the CT characteristics of thymic cysts, these masses appear to be most commonly well defined, round/oval, and laterally positioned in the anterior mediastinum (35). Specific to thymic cysts, contiguous involvement with the thymus is usually present (13). Right, left and bilateral laterality are possible with sizes as large as 34 cm in diameter (46). Case series have suggested that cyst margins tend to be uniformly enhancing. Relative to surrounding structures, margins may be poorly apparent or well delineated on imaging. Gross appearance can also be variable, being smooth or lobular and unilocular or multilocular based on type. Internal components vary and frequently contain solid components (13). Cyst fluid when simple varies from 0 and 62 Hounsfield units (9,13,17,35). Although routinely non-calcified (13) focal (47) and grossly calcified (44,48) mediastinal thymic cysts have been reported.
Serum markers including alpha fetoprotein and human chorionic gonadotropin are routinely obtained in the preoperative assessment and customarily are negative (7,20,41,47)
Definitive diagnosis based on imaging is challenging and ultimately diagnosis is based upon histological evaluation of surgical specimens. Large series demonstrate that the diagnostic sensitivity of CT in making an accurate diagnosis was less than 55% (35). Incorrect diagnosis was especially common with masses less than 3 cm and Hounsfield units greater than 20 on imaging (35). Tissue sampling before surgical excision should not be undertaken, as biopsy of cysts results are often unrevealing (39,49) and risk bacterial seeding, subsequent sepsis and death (41,42,50). Given preoperative diagnostic uncertainty, and overall rarity of this pathology, workup requires a broad differential.
Underscoring the diagnostic uncertainty associated with mediastinal thymic cysts, are case reports where the misdiagnosis of aortic intramural hematomas and Type A dissections have been made (17,29). If a question of diagnosis exists, additional imaging should be obtained with echocardiography which can provide more dynamic information with doppler flow to help exclude vascular or cardiac chamber involvement (7,51,52).
Despite the known limitations of imaging, recent advances in technology such as “radiomics” have proven to be valuable to assist in the accurate diagnosis of cysts by using computer analysis of acquired images (53). Magnetic resonance imaging (MRI), has often been described as an additional adjunctive imaging modality with cysts to aid in diagnosis (19,43). T2 sequences appearing very bright, is a specific, but not sensitive quality that can help aid in identifying thymic cysts from other pathologies (54). T1 MRI sequences also appear to be of value, with signal intensity ratios of 1 to 1.5 being useful in identifying thymic cysts.
Positron emission tomography (PET) is another adjunctive imaging modality to differentiate cysts, with low maximum standardized uptake value, suggesting benign features (55).
Endoscopic ultrasound is a newer technology that can potentially aid in diagnosis of thymic cysts (56-58). As previously discussed, caution should be taken with endoscopic aspiration of cyst contents when diagnosis of thymic or mediastinal cyst is suspected, as analysis of fine needle aspiration is usually non-diagnostic 73% of the time, with risk of infection, sepsis, and death (41,42,50,58).
However, for thymic cysts with significant solid components, which are commonly seen in thymoma or thymic carcinoma, percutaneous needle biopsy is an option for diagnosis with appropriate patient counseling on risks (15).
Prior to cross sectional computed tomography imaging, chest radiographs were the primary diagnostic modality to assess mediastinal masses (8). Because of the varied appearance and locations thymic cysts can occur, heterogeneous radiographs, with obscurement of cardiac borders, sometimes containing calcifications, were described. Historically, lateral chest radiographs were suggested in routine workup, as an anterior location of mass was suggested to be a common feature of thymic cysts (6). Although better imaging technologies exist today, plain chest radiographs could still be useful in resource limited environments.
Symptoms
The majority of patients with thymic cysts are asymptomatic (3,35). In symptomatic patients, chest pain, hoarseness, dyspnea, cough (3,35), and compressive symptoms appear to be most common. Compressive symptoms are variable and unique based on cyst location. Right atrial (59) or right cardiac chamber compression can mimic symptoms of right heart failure, with elevated jugular venous pressures, hepatic congestion, and peripheral edema (7,46). Facial congestion in the setting of superior vena cava (SVC), extrinsic obstruction by cysts is possible (37). Atrial fibrillation and reversible heart failure has been described in the setting of cysts in proximity of the SVC and right atrium (22). Syncope is possible in the setting of left atrial compression (44). Left sided cysts have also been associated with tachy-brady syndrome (60).
Mass effect on pulmonary structures and resulting atelectasis secondary to cysts has explained dyspnea in otherwise healthy individuals (47). Reversible impairments in formal pulmonary function testing have been demonstrated (38) as well as airway compression related pneumonias (49).
Spontaneous cyst rupture has been reported in literature, mimicking pleural effusions with associated pleuritic chest pain (36).
Neurological symptoms, as prominent as Horner syndrome with anhidrosis, miosis and ptosis have been caused by extrinsic compression of sympathetic structures (61). Temporary unilateral vocal cord paralysis has also been described from probable recurrent laryngeal nerve impingement (62).
Bleeding seems to occur with thymic cysts in patients with thrombocytopenia (11,42) or on platelet inhibitors (39). Cases of spontaneous bleeding in the absence of an identifiable source with associated anemia, rapid cyst enlargement, pleural effusions and mediastinal widening have been described requiring urgent surgical treatment (10,43,45,48).
Treatment
Definitive treatment of mediastinal thymic cysts is surgical. The decision to offer surgical treatment however requires clinical judgment. In the setting of symptomatic cysts, given excellent surgical outcomes and complication rates of 1.1% to 6.5% (10,35) surgical resection should be offered to patients.
The treatment of asymptomatic cysts is less straightforward. The best available literature suggests that the majority of thymic cysts are benign (10) however this contradicts the numerous case reports describing occult neoplastic processes, spontaneous hemorrhages, and substantial insidious subclinical compressive symptoms (38). This conflicting evidence likely stems from the overall rarity of this pathology and an inherent bias of case reports reporting unique patients with mediastinal thymic cysts (1).
Determining a method to stratify asymptomatic cysts based on risk of neoplastic potential poses further challenges. While nearly all neoplastic cysts are multilocular, only approximately half have this appearance on CT imaging (13,15,35). Solid components seem to be common features of neoplasia (12,15), however these do not always appear to be apparent on cross-sectional imaging, and previous research has shown that solid components among multilocular thymic cysts can represent various non-neoplastic tissue such as thymic hyperplasia, normal thymic remnants, hemorrhagic cysts, or numerous small cysts septated by thick inflammatory thymic tissue (13).
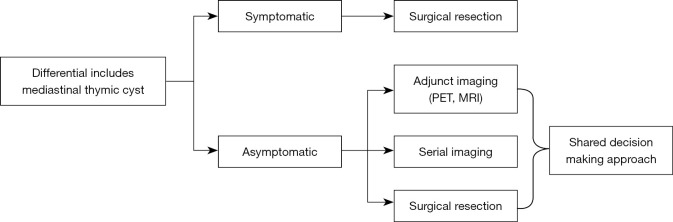
Because no reliable risk stratification can be made based on the presence or absence of imaging features, a shared decision making approach with patients is appropriate regarding management. Risk of malignancy is likely less than 1% (63) and the rate operative of complications is 1% to 5% (10,35). With surgical resection being the only way to establish a concrete diagnosis (13,64), observation with serial imaging, pursuing additional imaging such as MRI, or surgical resection are all reasonable management options and should be driven by patient preference. Figure 1 outlines an approach to treatment of mediastinal thymic cysts.
Figure 1.
Treatment algorithm. PET, positron emission tomography; MRI, magnetic resonance imaging.
Approach to resection should be tailored based on cyst location and urgency of symptoms. A video assisted thoracoscopic (VATS) technique (3,10,32,35,36,39,47) with conversion to anterior thoracotomy (59) as required should be sufficient in the majority of cases, although median sternotomy in instances of very large cysts or clinical instability is appropriate (14,16,17,30,38,43,46). Posterolateral thoracotomy may also be utilized in the setting of a rare posterior mediastinal cyst (44). Robotic resection, although rare, has been utilized (65). Subxiphoid and transcervical approaches seem to be effective in selected patients with anterior midline location cysts with sufficient operator familiarity (9,23,31,66). Clamshell approaches have also been utilized (20) however are morbid and should be cautiously undertaken. Reports of mediastinoscopy for resection have also been described (37,64) however should only be undertaken if complete resection is possible. Incomplete resection from this approach has resulted in deaths from sepsis (42).
Conclusions
Over the many decades since the first comprehensive case series of mediastinal thymic cysts were published, much has changed with regards to understanding pathophysiology, presentation, diagnosis, and treatment of this rare pathology. Inflammatory processes appear to be a dominant driver of cyst formation. While the majority of patients appear to be asymptomatic, mass effect and compressive symptoms can occur. Tissue sampling in this pathology should be avoided for its low diagnostic yield. Finally, surgical resection should be pursued with a shared decision making approach when thymic cysts are on the differential because of the strong association with neoplastic etiologies reported in literature, and excellent short and long term surgical results.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Footnotes
Provenance and Peer Review: This article was commissioned by the Guest Editor (Nestor Villamizar) for the series “Mediastinal Cysts” published in Mediastinum. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://med.amegroups.com/article/view/10.21037/med-22-25/rc
Peer Review File: Available at https://med.amegroups.com/article/view/10.21037/med-22-25/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://med.amegroups.com/article/view/10.21037/med-22-25/coif). The series “Mediastinal Cysts” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
References
- 1.Henschke CI, Lee IJ, Wu N, et al. CT screening for lung cancer: prevalence and incidence of mediastinal masses. Radiology 2006;239:586-90. 10.1148/radiol.2392050261 [DOI] [PubMed] [Google Scholar]
- 2.Yoon SH, Choi SH, Kang CH, et al. Incidental Anterior Mediastinal Nodular Lesions on Chest CT in Asymptomatic Subjects. J Thorac Oncol 2018;13:359-66. 10.1016/j.jtho.2017.11.124 [DOI] [PubMed] [Google Scholar]
- 3.Takeda S, Miyoshi S, Minami M, et al. Clinical spectrum of mediastinal cysts. Chest 2003;124:125-32. 10.1378/chest.124.1.125 [DOI] [PubMed] [Google Scholar]
- 4.Dyer NH. Cystic thymomas and thymic cysts. A review. Thorax 1967;22:408-21. 10.1136/thx.22.5.408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Preventive Services Task Force ; Krist AH, Davidson KW, et al. Screening for Lung Cancer: US Preventive Services Task Force Recommendation Statement. JAMA 2021;325:962-70. 10.1001/jama.2021.1117 [DOI] [PubMed] [Google Scholar]
- 6.Sltzer RA, Mills DS, Baddock SS, et al. Mediastinal thymic cyst. Dis Chest 1968;53:186-96. 10.1378/chest.53.2.186 [DOI] [PubMed] [Google Scholar]
- 7.Bruno VD, Mariscalco G, Franzi F, et al. Ectopic congenital thymic cyst in the right pleural cavity. Asian Cardiovasc Thorac Ann 2010;18:486-8. 10.1177/0218492310380280 [DOI] [PubMed] [Google Scholar]
- 8.SCHILLHAMMER WR Jr , TYSON MD. Mediastinal thymic cysts. Report of three cases and review of the literature. Arch Surg 1962;85:410-7. 10.1001/archsurg.1962.01310030058010 [DOI] [PubMed] [Google Scholar]
- 9.Tollefsen I, Yoo M, Bland JD, et al. Thymic cyst: is a correct preoperative diagnosis possible? Report of a case and review of the literature. Eur J Pediatr 2001;160:620-2. 10.1007/s004310100817 [DOI] [PubMed] [Google Scholar]
- 10.Wang X, Li Y, Chen K, et al. Clinical characteristics and management of primary mediastinal cysts: A single-center experience. Thorac Cancer 2020;11:2449-56. 10.1111/1759-7714.13555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davis JW, Florendo FT. Symptomatic mediastinal thymic cysts. Ann Thorac Surg 1988;46:693-4. 10.1016/S0003-4975(10)64738-8 [DOI] [PubMed] [Google Scholar]
- 12.Weissferdt A, Moran CA. Thymic carcinoma associated with multilocular thymic cyst: a clinicopathologic study of 7 cases. Am J Surg Pathol 2011;35:1074-9. 10.1097/PAS.0b013e31821c7402 [DOI] [PubMed] [Google Scholar]
- 13.Choi YW, McAdams HP, Jeon SC, et al. Idiopathic multilocular thymic cyst: CT features with clinical and histopathologic correlation. AJR Am J Roentgenol 2001;177:881-5. 10.2214/ajr.177.4.1770881 [DOI] [PubMed] [Google Scholar]
- 14.Kanakis MA, Danias PG, Chatzis AC. Thymic Cyst Popping Up in a Patient With Congenital Heart Disease. World J Pediatr Congenit Heart Surg 2016;7:372-4. 10.1177/2150135115625185 [DOI] [PubMed] [Google Scholar]
- 15.Shen X, Jin Y, Shen L, et al. Thymoma and thymic carcinoma associated with multilocular thymic cyst: a clinicopathologic analysis of 18 cases. Diagn Pathol 2018;13:41. 10.1186/s13000-018-0719-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eifinger F, Ernestus K, Benz-Bohm G, et al. True thymic hyperplasia associated with severe thymic cyst bleeding in a newborn: case report and review of the literature. Ann Diagn Pathol 2007;11:358-62. 10.1016/j.anndiagpath.2006.04.007 [DOI] [PubMed] [Google Scholar]
- 17.Tiveron MG, Dias RR, Benvenuti LA, et al. Thymic cyst as a differential diagnosis of acute thoracic aortic disease. Rev Bras Cir Cardiovasc 2008;23:575-7. 10.1590/S0102-76382008000400021 [DOI] [PubMed] [Google Scholar]
- 18.Gorospe L, García-Villanueva MJ, García-Cosío-Piqueras M, et al. Multilocular thymic cyst in a patient with Sjögren syndrome. Rheumatology (Oxford) 2019;58:369. 10.1093/rheumatology/key221 [DOI] [PubMed] [Google Scholar]
- 19.Leonidas JC, Berdon WE, Valderrama E, et al. Human immunodeficiency virus infection and multilocular thymic cysts. Radiology 1996;198:377-9. 10.1148/radiology.198.2.8596835 [DOI] [PubMed] [Google Scholar]
- 20.Tamagno M, Bibas BJ, Bernardi F, et al. Giant multilocular thymic cyst in an HIV-infected adolescent. J Pediatr Surg 2011;46:1842-5. 10.1016/j.jpedsurg.2011.06.009 [DOI] [PubMed] [Google Scholar]
- 21.Shi X, Nasseri F, Berger DM, et al. Large Multilocular Thymic Cyst: A Rare Finding in an HIV Positive Adult Female. J Clin Imaging Sci 2012;2:55. 10.4103/2156-7514.100379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cuasay RS, Fernandez J, Spagna P, et al. Mediastinal thymic cyst after open heart surgery. Chest 1976;70:296-8. 10.1378/chest.70.2.296 [DOI] [PubMed] [Google Scholar]
- 23.Oda R, Okuda K, Murase T, et al. Thymic inflammatory pseudotumor with multilocular thymic cyst caused by immunoglobulin G4-related disease. Thorac Cancer 2019;10:116-9. 10.1111/1759-7714.12914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alzahran A, Shebli B, Dabbas S, et al. Rare mediastinal thymic cyst infection without predisposing disease: a case report. JRSM Open 2021;12:2054270421991801. 10.1177/2054270421991801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yamashita S, Yamazaki H, Kato T, et al. Thymic carcinoma which developed in a thymic cyst. Intern Med 1996;35:215-8. 10.2169/internalmedicine.35.215 [DOI] [PubMed] [Google Scholar]
- 26.Lindfors KK, Meyer JE, Dedrick CG, et al. Thymic cysts in mediastinal Hodgkin disease. Radiology 1985;156:37-41. 10.1148/radiology.156.1.4001419 [DOI] [PubMed] [Google Scholar]
- 27.Steinmüller F, Traeger T, Kühn JP, et al. Rare case of a large mediastinal cyst involved in Hodgkin's lymphoma. Pathol Res Pract 2012;208:306-9. 10.1016/j.prp.2012.02.012 [DOI] [PubMed] [Google Scholar]
- 28.Borgna-Pignatti C, Andreis IB, Rugolotto S, et al. Thymic cyst appearing after treatment of mediastinal non-Hodgkin lymphoma. Med Pediatr Oncol 1994;22:70-2. 10.1002/mpo.2950220115 [DOI] [PubMed] [Google Scholar]
- 29.Wakely P, Jr, Suster S. Langerhans' cell histiocytosis of the thymus associated with multilocular thymic cyst. Hum Pathol 2000;31:1532-5. 10.1053/hupa.2000.20410 [DOI] [PubMed] [Google Scholar]
- 30.Schweigert M, Kaiser J, Fuchs T, et al. Thymoma within a giant congenital thymic cyst. Interact Cardiovasc Thorac Surg 2011;13:442-3. 10.1510/icvts.2011.270645 [DOI] [PubMed] [Google Scholar]
- 31.Yano M, Numanami H, Akiyama T, et al. Thoracoscopic Thymectomy for Large Thymic Cyst: Myasthenia Gravis With Thymoma Concealed by Thymic Cyst. Surg Laparosc Endosc Percutan Tech 2019;29:e34-6. 10.1097/SLE.0000000000000641 [DOI] [PubMed] [Google Scholar]
- 32.Morikawa H, Tanaka T, Hamaji M, et al. Papillary adenocarcinoma developed in a thymic cyst. Gen Thorac Cardiovasc Surg 2010;58:295-7. 10.1007/s11748-009-0518-x [DOI] [PubMed] [Google Scholar]
- 33.Silverman JF, Olson PR, Dabbs DJ, et al. Fine-needle aspiration cytology of a mediastinal seminoma associated with multilocular thymic cyst. Diagn Cytopathol 1999;20:224-8. [DOI] [PubMed] [Google Scholar]
- 34.Rakheja D, Weinberg AG. Multilocular thymic cyst associated with mature mediastinal teratoma: a report of 2 cases. Arch Pathol Lab Med 2004;128:227-8. 10.5858/2004-128-227-MTCAWM [DOI] [PubMed] [Google Scholar]
- 35.Wang X, Chen K, Li X, et al. Clinical features, diagnosis and thoracoscopic surgical treatment of thymic cysts. J Thorac Dis 2017;9:5203-11. 10.21037/jtd.2017.10.148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lachanas E, Konofaos P, Birba G, et al. A rupture of a huge thymic cyst into the pleural cavity: A case report. Respir Med 2006;100:1858-60. 10.1016/j.rmed.2005.12.013 [DOI] [PubMed] [Google Scholar]
- 37.Iyer AP, Sadasivan D, Yadav S, et al. Thymic cyst causing superior venacava syndrome relieved by mediastinoscopy--a rare presentation. Heart Lung Circ 2008;17:510-2. 10.1016/j.hlc.2007.09.003 [DOI] [PubMed] [Google Scholar]
- 38.Jennings S, Stuklis RG, Chan J, et al. Successful Giant Thymic Cyst Removal: Case Report and Review of the Literature. Heart Lung Circ 2015;24:e89-92. 10.1016/j.hlc.2015.02.013 [DOI] [PubMed] [Google Scholar]
- 39.Lee JH, Kim EC, Lim YS, et al. Spontaneous thymic cyst hemorrhage manifesting as a mediastinal mass. Korean J Med 2016;91:62-5. 10.3904/kjm.2016.91.1.62 [DOI] [Google Scholar]
- 40.Suster S, Rosai J. Histology of the normal thymus. Am J Surg Pathol 1990;14:284-303. 10.1097/00000478-199003000-00010 [DOI] [PubMed] [Google Scholar]
- 41.Liu W, Wang Y, Zhang W, et al. Pneumonia, pleurisy, mediastinitis, and mediastinal cyst infection secondary to endobronchial ultrasound-guided transbronchial needle aspiration: A case report. Medicine (Baltimore) 2021;100:e25973. 10.1097/MD.0000000000025973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moskowitz PS, Noon MA, McAlister WH, et al. Thymic cyst hemorrhage: a cause of acute, symptomatic mediastinal widening in children with aplastic anemia. AJR Am J Roentgenol 1980;134:832-6. 10.2214/ajr.134.4.832 [DOI] [PubMed] [Google Scholar]
- 43.Saito Y, Murai K, Kawai Y, et al. Spontaneous hemorrhage of a thymic cyst in an adult: report of a case. Surg Today 2010;40:958-62. 10.1007/s00595-009-4136-0 [DOI] [PubMed] [Google Scholar]
- 44.Luk L, Maldjian PD, Kumar A, et al. Thymic cyst arising in the middle mediastinum posterior to the left atrium--a peculiar location. Clin Imaging 2012;36:837-9. 10.1016/j.clinimag.2012.02.019 [DOI] [PubMed] [Google Scholar]
- 45.Fujiwara T, Mizobuchi T, Noro M, et al. Rapid enlargement of a mediastinal mass: thymoma hemorrhage into a thymic cyst. Gen Thorac Cardiovasc Surg 2008;56:472-5. 10.1007/s11748-008-0278-z [DOI] [PubMed] [Google Scholar]
- 46.Becit N, Koçak H, Koçoğullari CU. Giant thymic cyst presenting as cardiac compression. Heart 2005;91:104. 10.1136/hrt.2004.035642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Constantacos C, Lawson NM, Votanopoulos KI, et al. Giant thymic cyst in left lower hemithorax of a healthy teenaged athlete. J Thorac Cardiovasc Surg 2007;134:1373-4. 10.1016/j.jtcvs.2007.07.034 [DOI] [PubMed] [Google Scholar]
- 48.Feng Q, He X. Huge Simple Mediastinal Cyst With Hemorrhage and Calcification. Ann Thorac Surg 2021;112:e475. 10.1016/j.athoracsur.2021.07.049 [DOI] [PubMed] [Google Scholar]
- 49.Sirivella S, Gielchinsky I, Parsonnet V. Mediastinal thymic cysts: a report of three cases. J Thorac Cardiovasc Surg 1995;110:1771-2. 10.1016/S0022-5223(95)70045-5 [DOI] [PubMed] [Google Scholar]
- 50.Mohamed S, Patel AJ, Mehdi R, et al. Infected mediastinal cysts following endobronchial ultrasound guided biopsy-a case series. J Surg Case Rep 2022;2022:rjac158. 10.1093/jscr/rjac158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dunne MG, Weksberg AP. Thymic cyst: computed tomography and ultrasound correlation. J Comput Tomogr 1983;7:351-5. 10.1016/0149-936X(83)90057-7 [DOI] [PubMed] [Google Scholar]
- 52.Liu J, Lv Q, Wang J, et al. Diagnostic value of echocardiography in paracardiac cystic lesions: 43 cases from one single medical center. Int J Cardiovasc Imaging 2021;37:1961-6. 10.1007/s10554-021-02180-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang C, Yang Q, Lin F, et al. CT-Based Radiomics Nomogram for Differentiation of Anterior Mediastinal Thymic Cyst From Thymic Epithelial Tumor. Front Oncol 2021;11:744021. 10.3389/fonc.2021.744021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hwang EJ, Paek M, Yoon SH, et al. Quantitative Thoracic Magnetic Resonance Criteria for the Differentiation of Cysts from Solid Masses in the Anterior Mediastinum. Korean J Radiol 2019;20:854-61. 10.3348/kjr.2018.0699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sugawara H, Ito K, Watanabe H, et al. Clinical usefulness of PET/MRI in differentiating anterior mediastinal masses. Nucl Med Commun 2022;43:92-9. 10.1097/MNM.0000000000001483 [DOI] [PubMed] [Google Scholar]
- 56.Zhao Y, Wang R, Wang Y, et al. Application of endoscopic ultrasound-guided-fine needle aspiration combined with cyst fluid analysis for the diagnosis of mediastinal cystic lesions. Thorac Cancer 2019;10:156-62. 10.1111/1759-7714.12924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yang H, Zhao H, Garfield DH, et al. Endobronchial ultrasound-guided transbronchial needle aspiration in the diagnosis of non-lymph node thoracic lesions. Ann Thorac Med 2013;8:14-21. 10.4103/1817-1737.105714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Aravena C, Patel J, Goyal A, et al. Role of Endobronchial Ultrasound-guided Transbronchial Needle Aspiration in the Diagnosis and Management of Mediastinal Cyst. J Bronchology Interv Pulmonol 2020;27:142-6. 10.1097/LBR.0000000000000640 [DOI] [PubMed] [Google Scholar]
- 59.Stas P, Declercq I, Van Raemdonck D, et al. Cardiac compression by a thymic cyst. Int J Cardiol 2007;114:e91-2. 10.1016/j.ijcard.2006.06.041 [DOI] [PubMed] [Google Scholar]
- 60.Efthymiou CA, Thorpe JA. Thymic cyst presenting as tachy-brady syndrome. Eur J Cardiothorac Surg 2009;35:1108-10. 10.1016/j.ejcts.2009.02.024 [DOI] [PubMed] [Google Scholar]
- 61.Fraile G, Rodriguez-Garcia JL, Monroy C, et al. Thymic cyst presenting as Horner's syndrome. Chest 1992;101:1170-1. 10.1378/chest.101.4.1170 [DOI] [PubMed] [Google Scholar]
- 62.Woolley SL, Espeso A, Smith DR. Complete recovery of an isolated left vocal fold palsy associated with a benign mediastinal thymic cyst. J Laryngol Otol 2008;122:e4. 10.1017/S0022215107001326 [DOI] [PubMed] [Google Scholar]
- 63.Kirmani B, Kirmani B, Sogliani F. Should asymptomatic bronchogenic cysts in adults be treated conservatively or with surgery? Interact Cardiovasc Thorac Surg 2010;11:649-59. 10.1510/icvts.2010.233114 [DOI] [PubMed] [Google Scholar]
- 64.Burjonrappa SC, Taddeucci R, Arcidi J. Mediastinoscopy in the treatment of mediastinal cysts. JSLS 2005;9:142-8. [PMC free article] [PubMed] [Google Scholar]
- 65.Peer M, Azzam S, Gofman V, et al. Robotic Mediastinal Surgery in Patients with Suspected Thymic Neoplasms: First Israeli Experience. Isr Med Assoc J 2018;20:637-41. [PubMed] [Google Scholar]
- 66.Amanatidou V, Mavrokosta M, Kourtesis A, et al. Cervicomediastinal thymic cyst--report of a case. Thorac Cardiovasc Surg 2008;56:177-8. 10.1055/s-2007-965643 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as