Abstract
Background:
Osteochondral allograft transplant (OCA) and osteochondral autograft transfer (OAT) replace damaged cartilage with a plug of bone and overlying articular cartilage; however, limited research is available regarding the survival of these osteoarticular grafting procedures.
Hypothesis:
We hypothesized that patients who underwent OCA would have a higher rate of subsequent surgery over the course of 5 years compared with patients who underwent OAT.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
The PearlDiver Mariner administrative database was used to identify patients 10 to 59 years old who had undergone OCA or OAT between 2010 and 2018. All included patients were assessed for subsequent knee surgeries, defined by the occurrence of a subsequent osteochondral procedure (OCA or OAT) or any type of knee arthroplasty for the duration of the time they were included in the data set (maximum of 10 years). Analyses were performed for the total population and those with allograft versus autograft (compared using the Fisher exact test). The 5-year Kaplan-Meier survival curves for operation-free survival were compared using a Mantel-Cox log-rank test.
Results:
In total, 2598 patients were identified: 1631 patients who underwent OCA (34.5 ± 12.1 years old; 51.6% female) and 967 patients who underwent OAT (32.1 ± 12.9 years old; 51.0% female). Both groups had similarly high rates of subsequent knee surgeries (23.9% vs 21.9%, respectively; P = .249), with no statistical differences in rates of subsequent surgery between groups. Kaplan-Meier survival curves comparing operation-free survival at 5 years indicated no significant difference between the groups (OCA, 88.0% vs OAT, 89.5%; P = .235).
Conclusion:
Both osteochondral grafting procedures carried a relatively high rate of secondary surgery, which increased with time. The 5-year survival analysis revealed similarly high rates of subsequent surgery.
Keywords: osteochondral, allograft, autograft, transplantation, revision
Damage to the hyaline articular cartilage can compromise its natural function and result in pain and decreased activity tolerance. 14 Cartilage damage within the knee, such as chondral lesions and localized cartilage defects, has been reported in between 20% and 65% of knees during routine arthroscopic procedures. 5,17 Furthermore, these lesions and defects have been shown to worsen over time, which may increase the chance of developing severe osteoarthritis. 17 A recent study reported that patients who experience these cartilaginous defects report a similar impact on quality of life as those scheduled for knee replacement surgery. 10
A spectrum of possible procedures can be considered for symptomatic chondral lesions of the knee that are unresponsive to nonoperative measures. Abrasion arthroplasty or microfracture attempts to induce the formation of fibrocartilage in order to repair lesions, rather than replacing hyaline cartilage. 11 Osteochondral allograft transplant (OCA) or osteochondral autograft transfer (OAT) can also be considered in order to replace damaged cartilage with a plug of bone and overlying articular (hyaline) cartilage, which prevents fibrocartilage formation seen in other restoration procedures. 17 In addition to restoring the articular cartilage, osteochondral grafts can repair the subchondral bone and restore the contour of the articular surface.
OAT procedures are typically considered for localized lesions <2 cm2. 4,7,15,18,19 OAT procedures offer the theoretical advantages of replacing damaged hyaline cartilage with the patient’s own hyaline cartilage. 15,19,20 In a prospective study of outcomes among patients with articular cartilage lesions, 27 of 28 patients (96%) treated by OAT had good or excellent surgical outcomes, compared with 15 of 29 patients (52%) treated by microfracture (P < .0001). 9 OAT has been shown to produce favorable results for lesions that are between 2 and 4 cm2. 2,18 Traditionally, OCA has been indicated for patients who experience failure of surgical treatments from microfracture, autologous chondrocyte implantation, and OAT or those with lesions considered too large to accommodate the donor-site morbidity of multiple grafts for an autograft transfer. 2 However, cartilaginous lesions that have failed in the past with the aforementioned procedures (typically those >2 cm2) are now increasingly being treated primarily with OCA. 2 Finally, with larger lesions (>4 cm2) or multifocal lesions, OCA has shown the best results. 2
Osteochondral autograft and allograft procedures are performed for challenging situations and are noted to carry a relatively high rate of secondary surgery, which increases with time. 1 In the case of a failure of osteochondral autograft, a patient may undergo OCA or, based on age and activity level, knee arthroplasty. 3 Reported rates of failure after OAT or OCA range from 0% to 24%. 4,6 –8,11 –13
Limited comparative research is available regarding osteochondral allograft and autograft, and most studies are small case series that lack mid- to long-term follow-up. Thus, the purpose of the current study was to analyze the frequency of subsequent surgeries in patients who underwent OCA versus OAT. We hypothesized that patients who underwent OCA would have a higher rate of subsequent surgeries over 5 years compared with patients who underwent OAT.
Methods
Study Population
The large insurance claims PearlDiver Mariner database was used. The Mariner database includes Health Insurance Portability and Accountability Act–compliant medical record data on 122 million patients within the United States, which can be organized and analyzed by International Classification of Diseases (ICD)–9 and ICD-10 diagnosis and procedural codes, by Current Procedural Terminology (CPT) codes, and by demographic factors such as age, sex, and geographic region. This study was exempt from institutional review board approval, as the PearlDiver database contains only deidentified patient data.
We queried the database for patients aged 10 to 59 years who had undergone OCA or OAT between 2010 and 2018. CPT codes were used to identify those who underwent open or arthroscopic OCA (CPT codes 27415 and 29867, respectively) or OAT (CPT codes 27416 and 29866, respectively). Patient follow-up was assessed by any additional medical encounter, diagnosis, or procedural code included in the patient’s medical record. Within the current edition of the PearlDiver Mariner data set, patient data are available for a maximum of 10 years.
A Kaplan-Meier analysis of the PearlDiver software was used to assess 5-year operation-free survival after the index procedure, and patients who were lost to follow-up for various reasons (eg, change in insurance coverage, no further physician follow-up, or death) at each time point were censored.
Secondary Surgery
From the time of the index OCA or OAT procedure, patient records were analyzed, and all subsequent medical encounters and procedures were recorded. More granular data on the specific subsequent knee surgeries patients underwent are provided in Table 1 and Appendix Table A1.
Table 1.
Procedural Codes Representing Secondary Surgeries After Index OCA or OAT
| CPT Code | Description |
|---|---|
| 27412 | Autologous chondrocyte implantation knee |
| 27415 | Osteochondral allograft knee open |
| 27416 | Osteochondral autograft knee open mosaicplasty |
| 29866 | Arthroscopy knee surgical; osteochondral autograft(s) (eg, mosaicplasty) (includes harvesting of the autograft) |
| 29867 | Arthroscopy knee surgical; osteochondral allograft (eg, mosaicplasty) |
| 29879 | Arthroscopy knee surgical; abrasion arthroplasty (includes chondroplasty where necessary) or multiple drilling or microfracture |
| 27442 | Arthroplasty femoral condyles or tibial plateau(s) knee |
| 27443 | Arthroplasty femoral condyles or tibial plateau(s) knee; with debridement and partial synovectomy |
| 27446 | Arthroplasty knee condyle and plateau; medial or lateral compartment |
| 27447 | Arthroplasty knee condyle and plateau; medial and lateral compartments with or without patellar resurfacing (total knee arthroplasty) |
CPT, Current Procedural Terminology; OAT, osteochondral autograft transfer; OCA, osteochondral allograft transplant.
Statistical Analysis
Individual patient records are not accessible within PearlDiver in order to protect patient privacy. However, PearlDiver does provide descriptive statistics for the study population under analysis, including the number of patients, mean, median, range, and interquartile range. Statistical determination of mean ± SD was performed using PearlDiver analytical tools. The Fisher exact test was used to determine the significance of changes in the proportion of patients undergoing secondary surgery when comparing the osteochondral allograft and autograft cohorts. Kaplan-Meier survival curves for secondary surgery were compared using a Mantel-Cox log-rank test. Statistical significance was set at P < .05 (PearlDiver Technologies, Colorado Springs, CO, USA).
Results
Study Population
In total, 1631 patients were identified who underwent OCA (34.5 ± 12.1 years old; 51.6% female) and 967 patients were identified who underwent OAT (32.1 ± 12.9 years old; 51.0% female) (Figure 1 and Table 2). We noted a statistically greater percentage of OAT procedures performed arthroscopically compared with OCA (58.8% vs 34.6%, respectively; P < .001).
Figure 1.
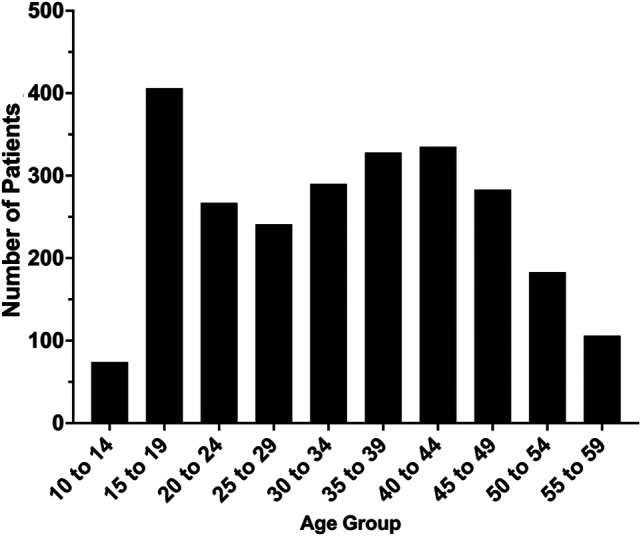
Age breakdown of the study patients (N = 2598).
Table 2.
Characteristics of the OCA and OAT Cohorts a
| Variable | OCA (n = 1631) |
OAT (n = 967) |
|---|---|---|
| Surgery type | ||
| Open | 1067 (65.4) | 398 (41.2) |
| Arthroscopic | 564 (34.6) | 569 (58.8) |
| Sex | ||
| Male | 789 (48.4) | 474 (49.0) |
| Female | 842 (51.6) | 493 (51.0) |
| Age, y | 34.5 ± 12.1 | 32.1 ± 12.9 |
| Age group | ||
| 10-19 y | 257 (15.8) | 240 (24.8) |
| 20-29 y | 324 (19.9) | 204 (21.1) |
| 30-39 y | 434 (26.6) | 205 (21.2) |
| 40-49 y | 420 (25.8) | 215 (22.2) |
| 50-59 y | 196 (12.0) | 103 (10.7) |
a Data are presented as n (%) or mean ± SD. Boldface values indicate statistically significant difference between groups (P < .05). OAT, osteochondral autograft transfer; OCA, osteochondral allograft transplant.
The subset of patients described as having “secondary knee surgeries” underwent surgical procedures defined in Appendix Table A1. Rates of secondary knee surgeries were high in both the OCA and the OAT populations, as shown in Figure 2. The most common secondary surgery was arthroscopic meniscectomy, which occurred in 169 patients (6.5%); this was followed by arthroscopic debridement/chondroplasty (123 patients; 4.7%), removal of deep implant (94 patients; 3.6%), and arthroscopic anterior cruciate ligament reconstruction (92 patients; 3.5%).
Figure 2.
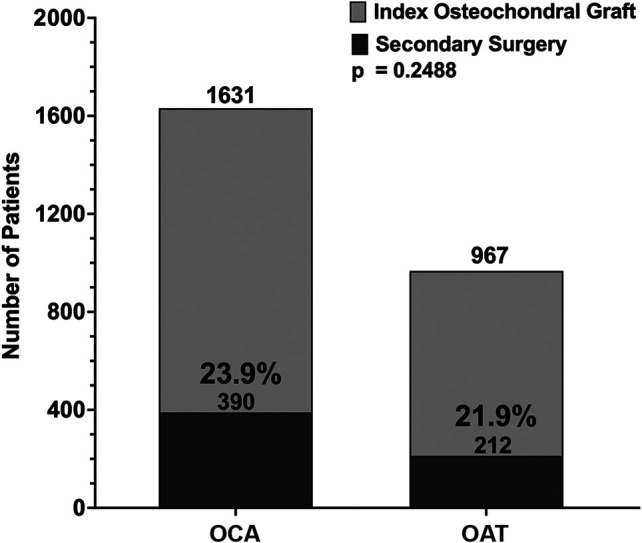
Comparison of secondary surgery rates in patients undergoing osteochondral allograft transplant (OCA) versus osteochondral autograft transfer (OAT). We found no statistical difference in the secondary surgery rate when comparing OCA and OAT cohorts (P = .249).
We found no significant difference in the rate of secondary surgery up to 10 years after OCA versus OAT (23.9% vs 21.9%, respectively; P = .249) (Figure 2). Similarly, the rate of secondary surgery was not significantly different between groups at 5 years postoperatively, according to Kaplan-Meier analysis (88.0% vs 89.5%, respectively; P = .235) (Figure 3).
Figure 3.
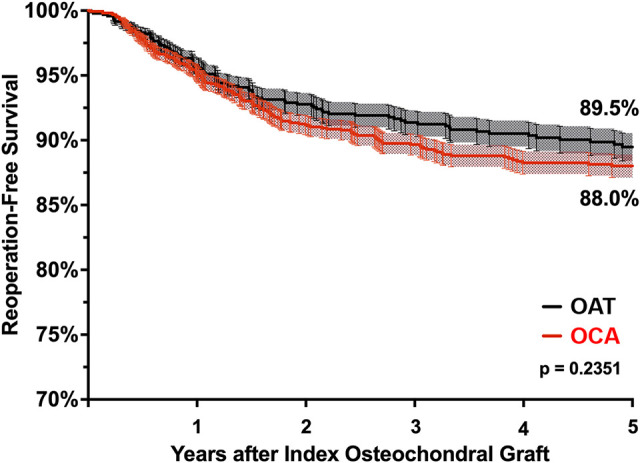
Kaplan-Meier curve comparing 5-year operation-free survival in patients who underwent osteochondral allograft transplant (OCA) versus osteochondral autograft transfer (OAT). We found no statistical difference in reoperation rates when comparing OCA versus OAT using a Mantel-Cox log-rank test (88.0% vs 89.5%, respectively; P = .235).
Discussion
With a total of 2598 patients (1631 patients who underwent OCA and 967 patients who underwent OAT), the current study is the largest single study to date of outcomes after OCA and OAT. Among all patients with OCA and OAT with 5 to 10 years of follow-up, 23.2% (23.9% vs. 21.9%, respectively) of patients underwent a secondary knee surgery indicating revision following index osteochondral surgery. This revision rate is consistent with previous literature, which has suggested that osteochondral failure ranges from 0% to 24%. 2 –4,6 –8 The current study reports a 5-year operation-free survival of 88.0% among 1631 patients with OCA. In a systematic review of failure rates after OCA, which included 19 studies and 1036 patients, Familiari et al 5 reported a 5-year survival rate of 86.7% and a 10-year survival rate of 78.7%. In studies examining outcomes after osteochondral autograft, Gudas et al 8 and Pareek et al 16 reported failure rates of 14% and 11%, respectively.
When comparing the osteochondral allograft and osteochondral autograft cohorts, we found no significant difference in the rates of secondary knee surgeries. In the current study, the operation-free survival of osteochondral allograft versus autograft transplant over 5 years was also not significantly different (88.0% vs 89.5%, respectively; P = .235). As noted previously, the indications for the 2 procedures can differ, with larger lesions more frequently treated with osteochondral allograft. The theoretical benefit of the use of autologous bone and articular cartilage being transferred into a smaller chondral lesion compared with allograft and the expected improved incorporation and durability of native articular cartilage are not demonstrated in the comparative operation-free survival rates of these 2 procedures in the present study.
Limitations
The limitations associated with this study include those inherent to the PearlDiver database and the retrospective nature of this study. First, when PearlDiver is used, the ability to extract data for analysis is limited to the queries designed by the research team and the original patient data that were entered into the medical record through ICD and CPT coding. By including the entire OCA and OAT population contained within the Mariner database between 2010 and 2018, we were able to assess patients with follow-up ranging from 0 to 10 years. However, as a result, when the entire study cohort is examined, the absolute rates of secondary knee surgery may be affected by patients who were lost to follow-up for various reasons (eg, change in insurance coverage, no physician follow-up, or death). To address this limitation, patients with incomplete follow-up were censored on Kaplan-Meier survival analysis.
Second, due to the nature of administrative databases, relevant data such as the particular technique used by each surgeon, the location of articular damage (femoral condyle, tibial plateau, patella, or trochlea), and the size of the lesion are not specified with current procedural codes and therefore cannot be used to further stratify or analyze our study population. Third, in this study, we did not identify any patients who underwent bilateral OCA or OAT procedures in the same day, nor did the ICD-9 data allow for assessment of laterality and subsequent surgeries that were not necessarily performed on the index knee. Fourth, we did not have access to clinical outcome measures for this population, limiting our analysis of outcomes to secondary surgeries and revision procedures. Fifth, to protect patient privacy, some granular information from individual patient records cannot be accessed, limiting the statistical analyses that can be performed. For instance, the age distributions of the patients with OAT and OCA were somewhat different, and the PearlDiver data structure makes it difficult to analyze whether that factor may be a confounder. Advantages of the PearlDiver Mariner database include its diverse, nationally representative patient population, which covers the nation geographically and also with respect to insurance plan types, including commercial insurance, Medicare, Medicaid, and self-pay.
Conclusion
The current study used a nationally representative database to compare the frequency of secondary surgeries between patients undergoing OCA or OAT. These procedures are performed for challenging situations and are noted to carry a relatively high rate of secondary surgery, which increases with time. 1 Information from this study can inform both patient and surgeon decision making surrounding OCA and OAT procedures, particularly among patients with an articular lesion between 2 and 4 cm2 that may have been treated previously by either method. Continued longer term follow-up analysis is recommended to assess whether these results change with further follow-up duration.
Appendix Table A1.
Secondary Knee Surgeries and Osteochondral Revision Surgeries Analyzed in the Current Study
| CPT Code | Description |
|---|---|
| Secondary Knee Surgeries and “Osteochondral Revision Surgeries” | |
| 27412 | Autologous chondrocyte implantation knee |
| 27415 | Osteochondral allograft knee open |
| 27416 | Osteochondral autograft knee open mosaicplasty |
| 27442 | Arthroplasty femoral condyles or tibial plateau(s) knee |
| 27443 | Arthroplasty femoral condyles or tibial plateau(s) knee; with debridement and partial synovectomy |
| 27446 | Arthroplasty knee condyle and plateau; medial or lateral compartment |
| 27447 | Arthroplasty knee condyle and plateau; medial and lateral compartments with or without patellar resurfacing (total knee arthroplasty) |
| 29866 | Arthroscopy knee surgical; osteochondral autograft(s) (eg, mosaicplasty) (includes harvesting of the autograft) |
| 29867 | Arthroscopy knee surgical; osteochondral allograft (eg, mosaicplasty) |
| 29879 | Arthroscopy knee surgical; abrasion arthroplasty (includes chondroplasty where necessary) or multiple drilling or microfracture |
| Additional Secondary Knee Surgeries | |
| 20670 | Removal of implant; superficial (eg, buried wire pin or rod) (separate procedure) |
| 20680 | Removal of implant; deep (eg, buried wire pin screw metal band nail rod or plate) |
| 27310 | Arthrotomy knee with exploration drainage or removal of foreign body (eg, infection) |
| 27330 | Arthrotomy knee; with synovial biopsy only |
| 27331 | Arthrotomy knee; including joint exploration biopsy or removal of loose or foreign bodies |
| 27334 | Arthrotomy with synovectomy knee; anterior or posterior |
| 27350 | Patellectomy or hemipatellectomy |
| 27418 | Anterior tibial tubercleplasty (eg, Maquet type procedure) |
| 27420 | Reconstruction of dislocating patella (eg, Hauser-type procedure) |
| 27422 | Reconstruction of dislocating patella; with extensor realignment and/or muscle advancement or release (eg, Campbell-Goldwaite type procedure) |
| 27425 | Lateral retinacular release open |
| 27435 | Capsulotomy posterior capsular release knee |
| 27438 | Arthroplasty patella; with prosthesis |
| 27450 | Osteotomy femur shaft or supracondylar; with fixation |
| 27455 | Osteotomy proximal tibia including fibular excision or osteotomy (includes correction of genu varus [bowleg] or genu valgus [knock-knee]); before epiphyseal closure |
| 27457 | Osteotomy proximal tibia including fibular excision or osteotomy (includes correction of genu varus [bowleg] or genu valgus [knock-knee]); after epiphyseal closure |
| 29870 | Arthroscopy knee diagnostic with or without synovial biopsy (separate procedure) |
| 29871 | Arthroscopy knee surgical; for infection lavage and drainage |
| 29873 | Arthroscopy knee surgical; with lateral release |
| 29874 | Arthroscopy knee surgical; for removal of loose body or foreign body (eg, osteochondritis dissecans fragmentation chondral fragmentation) |
| 29875 | Arthroscopy knee surgical; synovectomy limited (eg, plica or shelf resection) (separate procedure) |
| 29876 | Arthroscopy knee surgical; synovectomy major 2 or more compartments (eg, medial or lateral) |
| 29877 | Arthroscopy knee surgical; debridement/shaving of articular cartilage (chondroplasty) |
| 29880 | Arthroscopy knee surgical; with meniscectomy (medial and lateral including any meniscal shaving) |
| 29881 | Arthroscopy knee surgical; with meniscectomy (medial or lateral including any meniscal shaving) |
| 29882 | Arthroscopy knee surgical; with meniscal repair (medial or lateral) |
| 29884 | Arthroscopy knee surgical; with lysis of adhesions with or without manipulation (separate procedure) |
| 29886 | Arthroscopy knee surgical; drilling for intact osteochondritis dissecans lesion |
| 29888 | Arthroscopically aided anterior cruciate ligament repair/augmentation or reconstruction |
a CPT, Current Procedural Terminology.
Footnotes
Final revision submitted August 2, 2022; accepted September 8, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: M.J.M has received consulting fees and speaking fees from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by Yale University (ref No. 2000026183).
References
- 1. Assenmacher AT, Pareek A, Reardon PJ, et al. Long-term outcomes after osteochondral allograft: a systematic review at long-term follow-up of 12.3 years. Arthroscopy. 2016;32(10):2160–2168. [DOI] [PubMed] [Google Scholar]
- 2. Christian DR, Oliver-Welsh L, Yanke AB, Cole BJ. Staging and practical issues in complex cases. In: Farr J, Gomoll A, eds. Cartilage Restoration. Springer, Cham; 2018:119–130. [Google Scholar]
- 3. Cotter EJ, Hannon CP, Christian DR, et al. Clinical outcomes of multifocal osteochondral allograft transplantation of the knee: an analysis of overlapping grafts and multifocal lesions. Am J Sports Med. 2018;46(12):2884–2893. [DOI] [PubMed] [Google Scholar]
- 4. Emmerson BC, Gortz S, Jamali AA, et al. Fresh osteochondral allografting in the treatment of osteochondritis dissecans of the femoral condyle. Am J Sports Med. 2007;35(6):907–914. [DOI] [PubMed] [Google Scholar]
- 5. Familiari F, Cinque ME, Chahla J, et al. Clinical outcomes and failure rates of osteochondral allograft transplantation in the knee: a systematic review. Am J Sports Med. 2018;46(14):3541–3549. [DOI] [PubMed] [Google Scholar]
- 6. Gortz S, De Young AJ, Bugbee WD. Fresh osteochondral allografting for steroid-associated osteonecrosis of the femoral condyles. Clin Orthop Relat Res. 2010;468(5):1269–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gross AE, Kim W, Las Heras F, et al. Fresh osteochondral allografts for posttraumatic knee defects: long-term followup. Clin Orthop Relat Res. 2008;466(8):1863–1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gudas R, Gudaite A, Pocius A, et al. Ten-year follow-up of a prospective, randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint of athletes. Am J Sports Med. 2012;40(11):2499–2508. [DOI] [PubMed] [Google Scholar]
- 9. Gudas R, Kalesinskas RJ, Kimtys V, et al. A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy. 2005;21(9):1066–1075. [DOI] [PubMed] [Google Scholar]
- 10. Heir S, Nerhus TK, Rotterud JH, et al. Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis: a comparison of knee injury and osteoarthritis outcome score in 4 patient categories scheduled for knee surgery. Am J Sports Med. 2010;38(2):231–237. [DOI] [PubMed] [Google Scholar]
- 11. Krych AJ, Robertson CM, Williams RJ III; Cartilage Study Group. Return to athletic activity after osteochondral allograft transplantation in the knee. Am J Sports Med. 2012;40(5):1053–1059. [DOI] [PubMed] [Google Scholar]
- 12. LaPrade RF, Botker J, Herzog M, Agel J. Refrigerated osteoarticular allografts to treat articular cartilage defects of the femoral condyles: a prospective outcomes study. J Bone Joint Surg Am. 2009;91(4):805–811. [DOI] [PubMed] [Google Scholar]
- 13. Levy YD, Gortz S, Pulido PA, McCauley JC, Bugbee WD. Do fresh osteochondral allografts successfully treat femoral condyle lesions? Clin Orthop Relat Res. 2013;471(1):231–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Luria A, Chu CR. Articular cartilage changes in maturing athletes: new targets for joint rejuvenation. Sports Health. 2014;6(1):18–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. McCulloch PC, Kang RW, Sobhy MH, Hayden JK, Cole BJ. Prospective evaluation of prolonged fresh osteochondral allograft transplantation of the femoral condyle: minimum 2-year follow-up. Am J Sports Med. 2007;35(3):411–420. [DOI] [PubMed] [Google Scholar]
- 16. Pareek A, Reardon PJ, Macalena JA, et al. Osteochondral autograft transfer versus microfracture in the knee: a meta-analysis of prospective comparative studies at midterm. Arthroscopy. 2016;32(10):2118–2130. [DOI] [PubMed] [Google Scholar]
- 17. Richter DL, Schenck RC, Jr, Wascher DC, Treme G. Knee articular cartilage repair and restoration techniques: a review of the literature. Sports Health. 2016;8(2):153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Richter DL, Tanksley JA, Miller MD. Osteochondral autograft transplantation: a review of the surgical technique and outcomes. Sports Med Arthrosc Rev. 2016;24(2):74–78. [DOI] [PubMed] [Google Scholar]
- 19. Williams RJ III, Ranawat AS, Potter HG, Carter T, Warren RF. Fresh stored allografts for the treatment of osteochondral defects of the knee. J Bone Joint Surg Am. 2007;89(4):718–726. [DOI] [PubMed] [Google Scholar]
- 20. Zouzias IC, Bugbee WD. Osteochondral allograft transplantation in the knee. Sports Med Arthrosc Rev. 2016;24(2):79–84. [DOI] [PubMed] [Google Scholar]


