Abstract
Background:
Since the 1980s, primary care (PC) in the US has been recognized as the backbone of healthcare providing comprehensive care to complex patients, coordinating care among specialists, and rendering preventive services to contain costs and improve clinical outcomes. However, the effect of PC visits on total patient care cost has been difficult to quantify.
Objective:
To assess the effect of PC visits on total patient care cost.
Methods:
This is a retrospective study of over 5 million patients assigned to a PC provider in the Veterans Health Administration (VHA) in each of the 4 fiscal years (FY 2016-2019). The main outcome of interest is total annual patient care cost. We assessed the effect of primary care visits on total patient care cost first by descriptive statistics, and then by multivariate regressions adjusting for severity of illness and other confounders. We conducted in-depth sensitivity analyses to validate the findings.
Results:
On average, each additional in-person PC visit was associated with a total cost reduction of $721 (per patient per year). The first PC visit was associated with the largest savings, $3976 on average, and a steady diminishing return was observed. Further, the higher the patient risk (severity of illness), the larger the cost reduction: Among the top 10% of high-risk patients, the first PC in-person visit was associated with a reduction of $16 406 (19%).
Conclusions:
These findings, substantiated by our exhaustive sensitivity analyses, suggest that expanding PC capacity can significantly reduce overall health care costs and improve patient care outcomes given the former is a strong proxy of the latter.
Keywords: primary care, medical cost, impact evaluation, cost-effectiveness, health outcomes
Introduction
Ever-rising healthcare costs balloon government deficits and create financial burdens for employers and patients alike.1-5 More importantly, high costs mirror poor health and more human suffering. In the US, to curb escalating healthcare expenditures and improve quality of care, policymakers have turned to primary care (PC) for solutions, as evidenced by the rise and fall of managed care (HMOs) in the 1980s, the shift toward value-based care models such as accountable care organizations (ACOs) and patient-centered medical homes (PCMHs), and the primary care incentive provision in the Affordable Care Act.6,7
Indeed, in addition to treating complex patients with multiple comorbidities, PC plays a vital role in providing both preventive care and coordination of care that can lower the overall healthcare resource use.8,9 Published literature has shown effective PC (continuity, comprehensiveness, and regularity) is associated with reduced emergency department (ED) visits, hospitalizations, and health expenditures.10-16 In addition, studies examining regional PC variations indicated that more PC services may be associated with lower total healthcare expenditures.17-19 Moreover, a recent study found the average annual total cost of the patients having a PC provider (PCP) was 27.4% lower than those without a PCP.20 Finally, in recent years, PCMHs and ACOs have demonstrated a modest total cost reduction,21,22 but it is not clear what portion of the savings is due to primary care. And critics suspect that the cost reduction might come from rationing care rather than improving the long-term health of the patients.23
Despite the rich literature, the effect of primary care visits on total patient care costs remains unclear. To bridge this gap, the US Veterans Health Administration (VHA) system can serve as a living laboratory with several advantages: (1) large scale—a total annual operating budget of more than $80 billion with over 8 million enrollees across the nation,24 (2) clinicians have no incentives to ration or overuse services since they are largely salaried, (3) actual costs rather than billed charges or payments are recorded, and (4) centralized databases retain comprehensive patient demographic and clinical information.
Leveraging VHA’s unique healthcare delivery structure, in this study we ascertained the effect of increasing PC visits on total patient care cost by analyzing VHA system-wide patient-level data from fiscal years (FY) 2016 through 2019. And we conducted exhaustive sensitivity analyses to validate the findings.
Methods
Study Population and Data Sources
All veteran patients (employees were excluded) who were assigned to a primary care provider (PCP) and with any recorded costs in the VHA system during FY 2016 -2019 were included in the analysis. The VHA’s Corporate Data Warehouse (CDW) containing comprehensive patient demographic, socioeconomic, clinical, and cost information is our primary data source. For sensitivity analyses, we also linked the VHA data to Medicare cost data obtained from the Centers for Medicare and Medicaid Services (CMS).
Outcome, Treatment, and Confounding Variables
The main outcome was total annual cost at the patient level, which was also analyzed by its components (inpatient, outpatient, community care, and prescription drug costs). All costs were inflation-adjusted to 2019 dollars using the medical care component of the Consumer Price Index (CPI).25 The exposure or treatment variable we focused on in this study is the number of PC in-person visits at the patient level. We examined PC in-person visits as a continuous as well as a discrete variable for potential nonlinear effects. In addition, we also examined other types of PC encounters, that is, clinical video telehealth (hereinafter “telehealth visit”), and telephone clinic (hereinafter “phone visit”).
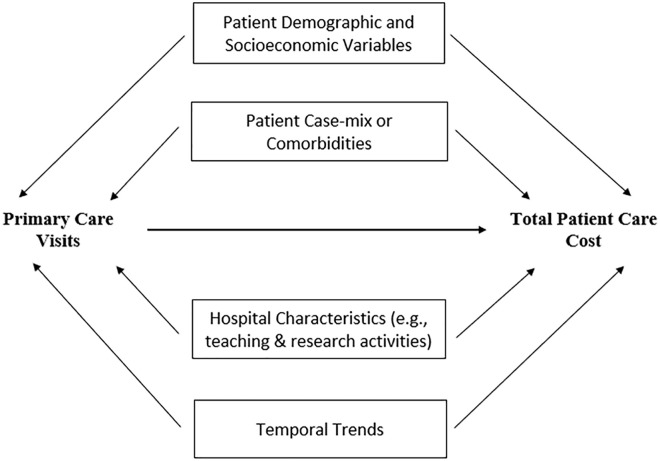
To reliably ascertain the effect of PC visits on total cost, we used a causal directed acyclic graph (DAG) to identify and visualize potential confounders and causal paths.26 As shown in Figure 1, there were 4 groups of confounding variables: (1) Patient demographic and socioeconomic variables, including age, age groups (for non-linear effect), gender, marital status (yes or no), race/ethnicity (White, Black, and “other” including Native American, Latino, Asian, or unknown), service-connected disability ratings (the VA rates service-connected disability from 0% to 100%), driving time to the nearest VHA facility providing PC services, and the status of Medicare, Medicaid, and private insurance enrollment. (2) Patient disease severity measured by the VHA’s Case-mix for Performance Management (CPM) risk score, which has been used in patient care operations since 2014.27-29 (3) Hospital characteristics such as trauma center levels, teaching versus non-teaching, rural versus urban, and local practice patterns, which were taken into account by fixed effects in the regression analyses. (4) Temporal trend, which was adjusted for by time (fiscal year) dummy variables.
Figure 1.
Causal directed acyclic graph (DAG).
Statistical Analysis
We first tabulated the study population characteristics, the number of PC visits, and total costs of care. We then stratified patients by the CPM risk score decile and the number of PC in-person visits to show how total costs vary with the latter. To further control for the 4 groups of confounders, we employed multivariate linear regressions (see Supplemental Material for details of model specifications).
We conducted exhaustive sensitivity analyses. For example, we validated the results by using 4 alternative patient risk or case-mix scores, adding Medicare costs, excluding telehealth and phone visits from the model, stratifying patients by the CPM risk score and age to rule out endogeneity induced bias, comparing fixed with random effects, and testing multicollinearity and heteroscedasticity. Details and results of the sensitivity analyses are presented in the Supplemental Material. All analyses were carried out by using SAS Enterprise Guide 8.2.
Results
The patient characteristics (FY 2016-2019) are reported in Table 1. As shown, the number of patients who had a PC provider in the VHA system slightly increased each year from 5 186 112 in FY 2016 to 5 410 034 in FY 2019. Most of the patient characteristics were relatively stable over the 4-year period. The average age was about 61.9, and 32% were between age 65 and 75. The majority of the patients were male (92%), married (56%), and White (75%). A 46% of the patients were enrolled in Medicare, only 1% were enrolled in Medicaid, and 12% were covered by private insurance. The average disability rating increased from 27.3% in FY 2016 to 32.9% in FY 2019, and the percentage of patients with disability rating above 70% also increased from 21% to 27% during the same period.
Table 1.
Study Population Characteristics (FY 2016-2019).
| Variable | FY 2016 (N = 5 186 112) | FY 2017 (N = 5 261 550) | FY 2018 (N = 5 373 568) | FY 2019 (N = 5 410 034) | ||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | |
| Age | 61.9 | 16.5 | 62.0 | 16.4 | 61.9 | 16.6 | 61.8 | 16.8 |
| Age < 35 | 9% | 0.28 | 9% | 0.28 | 9% | 0.28 | 8% | 0.28 |
| Age ≥ 35 and <45 | 7% | 0.26 | 8% | 0.27 | 8% | 0.28 | 9% | 0.29 |
| Age ≥ 45 and <55 | 12% | 0.32 | 12% | 0.33 | 12% | 0.32 | 12% | 0.32 |
| Age ≥ 55 and <65 | 19% | 0.40 | 19% | 0.39 | 18% | 0.39 | 18% | 0.38 |
| Age ≥ 65 and <75 | 32% | 0.47 | 32% | 0.47 | 32% | 0.47 | 32% | 0.47 |
| Age ≥ 75 | 21% | 0.41 | 20% | 0.40 | 20% | 0.40 | 21% | 0.40 |
| Gender (female) | 8% | 0.27 | 8% | 0.27 | 8% | 0.28 | 9% | 0.28 |
| Marital status (married) | 56% | 0.50 | 56% | 0.50 | 56% | 0.50 | 56% | 0.50 |
| Racial status (White) | 75% | 0.43 | 74% | 0.43 | 76% | 0.44 | 75% | 0.43 |
| Racial status (Black) | 18% | 0.38 | 18% | 0.38 | 17% | 0.38 | 18% | 0.38 |
| Racial status (other) | 7% | 0.26 | 8% | 0.27 | 7% | 0.26 | 7% | 0.26 |
| Enrolled in Medicare | 46% | 0.50 | 46% | 0.50 | 46% | 0.50 | 46% | 0.50 |
| Enrolled in Medicaid | 1% | 0.11 | 1% | 0.11 | 1% | 0.11 | 1% | 0.11 |
| Covered by private insurance | 12% | 0.33 | 12% | 0.33 | 12% | 0.33 | 12% | 0.33 |
| Disability rating (%) | 27.3 | 35.3 | 29.2 | 36.1 | 30.9 | 36.9 | 32.9 | 37.6 |
| Disability rating 70%+ (% of patients) | 21% | 0.41 | 23% | 0.42 | 25% | 0.43 | 27% | 0.44 |
| Drive time to closest VHA PCP (Min) | 21.0 | 16.9 | 21.3 | 16.2 | 21.7 | 16.6 | 21.6 | 16.6 |
| CPM risk score | 104.3 | 54.3 | 103.9 | 53.6 | 104.0 | 53.5 | 104.1 | 52.9 |
| Number of visits (in person) | 2.3 | 2.2 | 2.3 | 2.2 | 2.3 | 2.2 | 2.4 | 2.2 |
| Number of visits (tele-health) | 0.03 | 0.4 | 0.1 | 0.5 | 0.1 | 0.5 | 0.1 | 0.5 |
| Number of visits (phone) | 1.2 | 2.4 | 1.1 | 2.3 | 1.1 | 2.3 | 1.1 | 2.3 |
| Average outpatient cost | $7739 | 13 130 | $7889 | 13 350 | $8122 | 13 688 | $8387 | 14 170 |
| Average inpatient cost | $2700 | 17 080 | $2632 | 16 952 | $2732 | 17 418 | $2664 | 17 292 |
| Average community care cost | $1285 | 8137 | $1173 | 8012 | $1534 | 8830 | $1362 | 7995 |
| Average prescription cost | $1133 | 8753 | $1107 | 9642 | $1135 | 6657 | $1215 | 7388 |
| Average total cost per patient | $11 724 | 26 783 | $11 693 | 26 812 | $12 388 | 27 859 | $12 413 | 27 570 |
Total cost = outpatient cost + inpatient cost + community care cost. Prescription drug cost (part of the inpatient, outpatient, and community care costs) is separated for additional information.
The drive time to the closest PC provider was about 21 minutes, and the number of PC in person visits, telehealth visits, phone visits per patient were approximately 2.3, 0.1, and 1.1 in each of the 4 years. All costs except for inpatient cost increased slightly during the 4-year period; as a result, the average total cost per patient increased from $11 724 in FY 2016 to $12 413 in FY 2019.
Table 2 reports the costs stratified by the CPM risk score decile and the number of PC in-person visits (see the full Table in Supplemental Table 1). As shown, the CPM risk score has an excellent predicting or discriminating power: The average total cost of the patients with the lowest risk score (first decile) was $1119 while it was $60 310 among the highest risk patients (tenth decile), a discriminating ratio of 53.9 (60 310/1119). Among the patients with the lowest risk, the effect of PC visits on costs was minimum, limited to only the first visit. Moving higher along risk score deciles, the PC visit effect became more pronounced. Among the patients with the highest risk score (10th decile), PC visits had the greatest effect on costs: compared to the patients who had no PC visit, the average total cost of those with 1 visit was $16 406 lower, which amounted to a $2.5 billion cost reduction, given 153 207 patients in the highest risk group.
Table 2.
Annual Average Patient Care Costs by CPM Risk Decile and Number of PC Visits (Pooled FY 2016-2019).
| Number of PC visits (annual) | Number of patients | VA outpatient cost | VA inpatient cost | Community care cost | Prescription drug cost | Total cost | |
|---|---|---|---|---|---|---|---|
| Lowest health risk (1st decile) | 0 | 564 336 | $1052 | $205 | $120 | $112 | $1377 |
| 1 | 1 271 184 | $886 | $2 | $29 | $95 | $917 | |
| 2 | 238 206 | $1372 | $0 | $35 | $133 | $1407 | |
| 3 | 38 712 | $1777 | $0 | $44 | $143 | $1821 | |
| 4 | 7441 | $2237 | $0 | $59 | $154 | $2296 | |
| 5 | 1939 | $2589 | $0 | $71 | $159 | $2660 | |
| 6 | 619 | $3024 | $0 | $81 | $174 | $3105 | |
| 7 | 227 | $3090 | $0 | $103 | $140 | $3193 | |
| 8 | 127 | $3746 | $0 | $21 | $170 | $3767 | |
| 9 | 75 | $3936 | $0 | $35 | $208 | $3971 | |
| 10 | 67 | $3583 | $0 | $15 | $138 | $3598 | |
| 11 | 70 | $3768 | $0 | $3 | $189 | $3771 | |
| 12 | 95 | $3858 | $0 | $12 | $189 | $3870 | |
| >12 | 200 | $4637 | $0 | $29 | $214 | $4667 | |
| Highest health risk (10th decile) | 0 | 153 207 | $31 576 | $41 220 | $12 898 | $6281 | $85 694 |
| 1 | 203 374 | $26 594 | $32 946 | $9748 | $5529 | $69 288 | |
| 2 | 315 723 | $27 253 | $24 156 | $7603 | $5136 | $59 012 | |
| 3 | 350 971 | $28 136 | $20 582 | $6888 | $4879 | $55 606 | |
| 4 | 309 975 | $28 938 | $18 994 | $6620 | $4587 | $54 552 | |
| 5 | 238 998 | $29 970 | $18 341 | $6696 | $4487 | $55 007 | |
| 6 | 170 330 | $30 996 | $18 148 | $6877 | $4400 | $56 021 | |
| 7 | 116 035 | $32 129 | $18 254 | $7019 | $4404 | $57 402 | |
| 8 | 78 356 | $33 278 | $18 404 | $7202 | $4462 | $58 883 | |
| 9 | 52 399 | $34 300 | $18 239 | $7468 | $4411 | $60 007 | |
| 10 | 35 646 | $35 356 | $18 447 | $7613 | $4504 | $61 416 | |
| 11 | 24 297 | $36 524 | $19 096 | $7817 | $4550 | $63 438 | |
| 12 | 17 467 | $37 383 | $19 385 | $7854 | $4603 | $64 623 | |
| >12 | 55 900 | $41 252 | $18 658 | $7619 | $5147 | $67 529 |
Only deciles 1 and 10 are shown here; full Table is reported in Supplemental Table 1.
The additional cost reduction associated with the second PC visit was still substantial among patients with the highest risk, $10 276 per patient, an additional total cost reduction of $2.1 billion. Nevertheless, PC visits appeared to have a diminishing return. Based on this basic risk stratification, PC visits of more than 4 or 5 were not associated with further cost reduction.
Table 3 presents the estimate of cost reduction associated with PC in-person visits after controlling for the patient risk score and other confounders by multivariate linear regression (pooled FY 2016 to 2019 data; see Supplemental Material for the coefficient interpretations). On average, each additional PC in-person visit was associated with a cost reduction of $721.2. We repeated this analysis by fitting the model separately for each year and observed consistent results: $664.2, $658.9, $748.4, and $797.4, respectively for FY 2016 to 2019 (see Supplemental Table 2).
Table 3.
Multivariate Linear Model Estimate of PC Visit Effect on Total Patient Care Cost.
| Variables | Parameter estimate | 95% confidence interval | P > |t| | |
|---|---|---|---|---|
| Lower bound | Upper bound | |||
| Intercept | −22 208.0 | −22 308.1 | −22 107.9 | <.0001 |
| Number of PC visits (in person) | −721.2 | −724.9 | −717.5 | <.0001 |
| Number of PC visits (telehealth) | −299.6 | −314.7 | −284.5 | <.0001 |
| Number of PC visits (phone) | −78.9 | −82.3 | −75.6 | <.0001 |
| Age | −64.9 | −66.8 | −63.1 | <.0001 |
| Age ≥ 35 and <45 | 486.7 | 447.3 | 526.0 | <.0001 |
| Age ≥ 45 and <55 | 1251.3 | 1201.4 | 1301.1 | <.0001 |
| Age ≥ 55 and <65 | 1788.2 | 1724.0 | 1852.4 | <.0001 |
| Age ≥ 65 and <75 | 2326.1 | 2246.4 | 2405.7 | <.0001 |
| Age ≥ 75 | 3529.8 | 3426.6 | 3633.0 | <.0001 |
| Gender (female) | −588.9 | −615.4 | −562.5 | <.0001 |
| Marital status (married) | −721.4 | −736.3 | −706.6 | <.0001 |
| Racial status (White) | −765.6 | −786.1 | −745.2 | <.0001 |
| Racial status (Black) | −1022.5 | −1049.2 | −995.9 | <.0001 |
| Enrolled in Medicare | 190.7 | 169.3 | 212.1 | <.0001 |
| Enrolled in Medicaid | 264.6 | 199.4 | 329.9 | <.0001 |
| Covered by private insurance | −1519.7 | −1542.7 | −1496.6 | <.0001 |
| Disability rating (%) | −9.3 | −9.7 | −8.9 | <.0001 |
| Disability rating 70%+ (% of patients) | 119.4 | 85.5 | 153.3 | <.0001 |
| Drive time to closest VHA PCP (min) | −3.6 | −4.0 | −3.1 | <.0001 |
| CPM risk score | 393.0 | 392.8 | 393.1 | <.0001 |
| FY 2017 | 81.4 | 61.5 | 101.4 | <.0001 |
| FY 2018 | 710.4 | 690.5 | 730.3 | <.0001 |
| FY 2019 | 1221.5 | 1201.5 | 1241.6 | <.0001 |
The fixed effects of the 140 hospitals are not shown here. Age < 35, racial status (other), and FY 2016 were used as reference groups. Pooled data: FY 2016 to 2019; N = 21 231 264.
Table 4 shows the results produced by the multivariate model where the number of PC in-person visits was reconstructed into discrete variables for nonlinear effects (1-12 visits, and more than 12 visits). As shown, there was a clear diminishing return on PC in-person visits. The first visit was associated with $3976 of cost reduction compared to no visit (baseline), the second visit was associated with an additional reduction of $1149, and the third was associated with another $896. The trend continued until the 10th visit where costs started to rise with additional visits. The results were consistent when the model is fitted year by year separately (see Supplemental Table 3)
Table 4.
Multivariate Linear Model Estimate of PC Visit Effect on Total Patient Care Cost (PC visits as a discrete variable).
| Variables | Parameter estimate | 95% confidence interval | P > |t| | |
|---|---|---|---|---|
| Lower bound | Upper bound | |||
| Intercept | −20 112.0 | −20 213.0 | −20 011.0 | <.0001 |
| In-person visit 1 (# patients: 7 146 586) | −3976.1 | −4002.7 | −3949.5 | <.0001 |
| In-person visit 2 (# patients: 5 258 878) | −5124.8 | −5152.5 | −5097.0 | <.0001 |
| In-person visit 3 (# patients: 3 029 363) | −6020.8 | −6051.3 | −5990.3 | <.0001 |
| In-person visit 4 (# patients: 1 667 632) | −6777.6 | −6812.7 | −6742.5 | <.0001 |
| In-person visit 5 (# patients: 911 810) | −7431.7 | −7473.8 | −7389.6 | <.0001 |
| In-person visit 6 (# patients: 509 521) | −8064.4 | −8116.4 | −8012.5 | <.0001 |
| In-person visit 7 (# patients: 290 515) | −8622.6 | −8687.9 | −8557.4 | <.0001 |
| In-person visit 8 (# patients: 171 693) | −9130.5 | −9212.6 | −9048.4 | <.0001 |
| In-person visit 9 (# patients: 105 242) | −9614.1 | −9716.8 | −9511.3 | <.0001 |
| In-person visit 10 (# patients: 67 480) | −9882.8 | −10 009.5 | −9756.1 | <.0001 |
| In-person visit 11 (# patients: 45 235) | −9837.6 | −9991.0 | −9684.1 | <.0001 |
| In-person visit 12 (# patients: 34 151) | −9113.5 | −9289.3 | −8937.7 | <.0001 |
| In-person visits >12 (# patients: 112 902) | −7671.2 | −7770.8 | −7571.6 | <.0001 |
| Number of visits (tele-health) | −314.8 | −329.9 | −299.7 | <.0001 |
| Number of visits (phone) | −50.5 | −53.8 | −47.1 | <.0001 |
| Age | −59.5 | −61.3 | −57.6 | <.0001 |
| Age ≥ 35 and <45 | 577.0 | 537.8 | 616.3 | <.0001 |
| Age ≥ 45 and <55 | 1392.6 | 1342.8 | 1442.3 | <.0001 |
| Age ≥ 55 and < 65 | 1954.4 | 1890.3 | 2018.4 | <.0001 |
| Age ≥ 65 and <75 | 2485.5 | 2406.1 | 2565.0 | <.0001 |
| Age ≥ 75 | 3483.0 | 3380.0 | 3585.9 | <.0001 |
| Gender (female) | −503.1 | −529.5 | −476.7 | <.0001 |
| Marital status (married) | −663.2 | −678.1 | −648.4 | <.0001 |
| Racial status (White) | −408.2 | −428.8 | −387.7 | <.0001 |
| Racial status (Black) | −688.0 | −714.7 | −661.3 | <.0001 |
| Enrolled in Medicare | 190.3 | 168.9 | 211.6 | <.0001 |
| Enrolled in Medicaid | 239.0 | 173.9 | 304.1 | <.0001 |
| Covered by private insurance | −1474.4 | −1497.4 | −1451.4 | <.0001 |
| Disability rating (%) | −8.5 | −9.0 | −8.1 | <.0001 |
| Disability rating 70%+ (% of patients) | 88.7 | 54.9 | 122.5 | <.0001 |
| Drive time to closest VHA PCP (min) | −3.8 | −4.2 | −3.3 | <.0001 |
| CPM risk score | 392.9 | 392.7 | 393.1 | <.0001 |
| FY 2017 | 77.9 | 58.0 | 97.8 | <.0001 |
| FY 2018 | 688.4 | 668.5 | 708.2 | <.0001 |
| FY 2019 | 1212.5 | 1192.5 | 1232.6 | <.0001 |
The fixed effects of the 140 hospitals are not shown here. Visit 0 (1 880 256 patients hd no PC visit), age <35, racial status (other), and FY 2016 were used as reference groups. Pooled data: FY 2016 to 2019; N = 21 231 264.
In our supplemental analysis, we replicated Tables 2 and 3 by splitting the study population at Medicare eligibility age 65, which revealed that the cost reduction was slightly higher among the senior group ($630.2 vs $798.0; see Supplemental Tables 4 and 5). Further, we reproduced Table 3 by adding Medicare expenditures to the dependent variable, which yielded an estimate of $1157.2 cost reduction for each additional in-person visit (pooled data FY 2016-2019; see Supplemental Table 6). The year-by-year multivariate analysis including Medicare expenditures also showed consistent results: $1023.1, $1034.2, $1163.1, and $1348.9, respectively for FY 2016 to 2019 (Supplemental Table 7).
To further assess the reliability of our findings, we conducted additional sensitivity analyses. We refitted the fixed effect model with random effects which yielded near identical results (Supplemental Table 8). We also validated our findings by using 4 alternative risk scores (2 based on the number of diagnoses for each patient, and 2 based on the Clinical Classifications Software Refined (CCSR) groups) in place of the CPM risk score in the multivariate analyses—the results were consistent (see Supplemental Material for details).
Additionally, we assessed whether inclusion/exclusion of telehealth or phone visits in the regressions affected the estimates of the treatment effect (in-person visits): The resultant estimates were $722.3, $736.0, and $737.3, respectively for excluding telehealth, phone visits, and both from the regressions, which were all close to $721.2 as reported in Table 3. We further conducted other sensitivity analyses such as excluding HBPC (home-based primary care) and/or deceased patients, adding and excluding independent variables; the resultant estimates were consistent with our main findings (see all the sensitivity analyses in Supplemental Material for details).
Discussion
In this large-scale multi-year study, we quantified the effects of PC in-person visits on total patient care cost. Both descriptive statistics and multivariate analyses demonstrated that more PC in-person visits were associated with lower total patient care costs, especially among the high-risk or high-cost patients. Given all other things being equal, the first visit was associated with the largest cost reduction compared to no PC visit. This was consistent with the previous finding that the average total cost of patients having a PCP in the VHA system was $3274 lower compared to those without a PCP.20
It is desired to ascertain the cost effects of PC telehealth and phone visits and attempted to interpret their coefficient estimates (−$299.6 and −$78.9) as the cost reductions associated with telehealth and phone visits. However, our detailed sensitivity analyses indicate such a conclusion may be premature given the limited number of patients using these services and heterogeneity of the services delivered by these 2 modalities.
Our findings are consistent with previous studies demonstrating effective PC is associated with lower emergency department visits, preventable hospitalizations, mortality, healthcare expenditures.14-17,30-36 Our findings are also consistent with an early study of the VHA’s implementation of enhanced primary care showing an increase in PC use was associated with decreases in avoidable hospitalizations and outpatient visits to mental health providers.37 Paradoxically, however, a recent randomized controlled trial found that primary care Intensive management (PIM) in the VHA system did not reduce costs.38 The seemingly contradictory findings may stem from the fact that the average number of PC visits per patient in the trial’s treatment group decreased by 0.21 rather than increased from the baseline.
Taken together, to our best knowledge, the present study is the only large-scale patient-level analysis of the effects of increasing PC visits on overall healthcare costs in a large healthcare system; and our extensive sensitivity analyses indicate the findings are robust.
Unlike HMOs in the 1980s and the current ACOs that are alleged to ration care,22 VHA is mandated by Congress to provide the best care to veterans and resourced to do so with salaried providers. Thus, the most logical explanation behind the cost reduction is that PC provides more comprehensive care, especially to the patients with multiple comorbidities, improves preventative and coordination of care leading to better health, which is corroborated by other studies.39
Nevertheless, our study has limitations. First, VHA patient population is different. With mostly adult and male patients, unlike the private sector, VHA provides fewer prenatal and pediatric services. Second, while our analysis included all the costs incurred in the VHA system and all the costs of services provided by non-VA providers but paid for by the VHA or by Medicare, data on costs incurred through other insurers such as Medicaid and private health plans were not available to us. However, only 1% of the study population was enrolled in Medicaid and 12% enrolled in private health plans, and we also controlled for these 2 confounders in our multivariate analysis. In addition, the cost-saving effect of PC visits remained large among veterans aged over 65, an exogenous marker for Medicare eligibility and use. Furthermore, it is unlikely that patients having more PC visits with the VHA would use more services from non-VA providers. Thus, it is more likely that the estimated cost reduction would be higher if all the costs were included in the analyses. Third, like most observational studies, our analyses were unable to control for all potential confounders. For instance, patients having more PC visits might also have better medication adherence and exercise more. But one can also argue that these health behaviors could be a result of effective primary care. Fourth, we did not ascertain the relationship between the number of PC visits and quality of care, which is beyond the scope of the present study. We postulate patients having more PC visits would experience higher quality of care, but further studies are warranted. And obviously, the effects of clinical video telehealth and telephone clinics on total patient care cost merit further investigation, especially given the increase of their use during the COVID-19 pandemic. Finally, under the current healthcare environment, the generalizability of the findings could be limited given the VA health system is operating on a global budget with salaried clinicians while the private sector in the US is largely operating on a fee-for-service basis.
Conclusion
The findings of the present study, substantiated by our exhaustive sensitivity analyses, suggest that expanding PC capacity can significantly reduce overall health care costs and improve patient care outcomes given the former is a robust proxy of the latter.
Supplemental Material
Supplemental material, sj-pdf-1-jpc-10.1177_21501319221141792 for The Effect of Primary Care Visits on Total Patient Care Cost: Evidence From the Veterans Health Administration by Jian Gao, Eileen Moran, Rachel Grimm, Andrew Toporek and Christopher Ruser in Journal of Primary Care & Community Health
Acknowledgments
The authors would like to thank Mei-Ling Shen, PhD, for her data assistance.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This material is based upon work supported (or supported in part) by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development.
ORCID iD: Jian Gao  https://orcid.org/0000-0001-8101-740X
https://orcid.org/0000-0001-8101-740X
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Schneider EC, Squires D. From last to first—could the U.S. health care system become the best in the world? N Engl J Med. 2017;377(10):901-904. [DOI] [PubMed] [Google Scholar]
- 2. Mehrotra A, Dudley RA, Luft HS. What’s behind the health expenditure trends? Ann Rev Public Health. 2003;24:385-412. [DOI] [PubMed] [Google Scholar]
- 3. Weinick RM, Byron SC, Bierman AS. Who can’t pay for health care? J Gen Intern Med. 2005;20(6):504-509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Johnson PT, Alvin MD, Ziegelstein RC. Transitioning to a high-value health care model: academic accountability. Acad Med. 2018;93(6):850-855. [DOI] [PubMed] [Google Scholar]
- 5. Monaco RM, Phelps JH. Health care prices, the federal budget, and economic growth. Health Aff. 1995;14(2):248-259. [DOI] [PubMed] [Google Scholar]
- 6. Muhlestein D. Growth and dispersion of accountable care organizations in 2015. Health Affairs. 2015. Accessed August 21, 2020. https://www.healthaffairs.org/do/10.1377/hblog20150331.045829/full/
- 7. Davis K, Abrams M, Stremikis K. How the Affordable Care Act will strengthen the nation’s primary care foundation. J Gen Intern Med. 2011;26(10):1201-1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fine M. Primary care is dead. Long live primary care. Am J Public Health. 2021;111(4):608-609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Allen LN, Barkley S, De Maeseneer J, et al. Unfulfilled potential of primary care in Europe. BMJ. 2018;363:k4469. [DOI] [PubMed] [Google Scholar]
- 10. Phillips RL, Bazemore AW. Primary care and why it matters for US health system reform. Health Aff. 2010;29(5): 806-810. [DOI] [PubMed] [Google Scholar]
- 11. Shi L. Primary care, specialty care, and life chances. Int J Health Serv. 1994;24(3), 431–458. [DOI] [PubMed] [Google Scholar]
- 12. Hussey PS, Schneider EC, Rudin RS, Fox DS, Lai J, Pollack CE. Continuity and the costs of care for chronic disease. JAMA Intern Med. 2014;174(5):742-748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Romaire MA, Haber SG, Wensky SG, McCall N. Primary care and specialty providers: an assessment of continuity of care, utilization, and expenditures. Med Care. 2014;52(12):1042-1049. [DOI] [PubMed] [Google Scholar]
- 14. O’Malley AS, Rich EC, Shang L, et al. New approaches to measuring the comprehensiveness of primary care physicians. Health Serv Res. 2019;54(2):356-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rose AJ, Timbie JW, Setodji C, Friedberg MW, Malsberger R, Kahn KL. Primary care visit regularity and patient outcomes: an observational study. J Gen Intern Med. 2019;34(1):82-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kronman AC, Ash AS, Freund KM, Hanchate A, Emanuel EJ. Can primary care visits reduce hospital utilization among Medicare beneficiaries at the end of life? J Gen Intern Med. 2008;23(9):1330-1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Starfield B, Shi L. Policy relevant determinants of health: an international perspective. Health Policy. 2002;60(3):201-218. [DOI] [PubMed] [Google Scholar]
- 18. Friedberg MW, Hussey PS, Schneider EC. Primary care: a critical review of the evidence on quality and costs of health care. Health Aff. 2010;29(5):766-772. [DOI] [PubMed] [Google Scholar]
- 19. Reschovsky JD, Ghosh A, Stewart K, Chollet D. Paying more for primary care: can it help bend the Medicare cost curve? Issue Brief. 2012;5:1-12. [PubMed] [Google Scholar]
- 20. Gao J, Moran E, Woolhandler S, Toporek A, Wilper AP, Himmelstein DU. Primary care’s effects on costs in the US Veterans Health Administration, 2016-2019: an observational cohort study. J Gen Intern Med. 2022;37(13):3289-3294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nichols DE, Haber SG, Romaire MA, Wensky SG. Multi-payer advanced primary care practice evaluation team. Changes in utilization and expenditures for medicare beneficiaries in patient-centered medical homes: findings from the multi-payer advanced primary care practice demonstration. Med Care. 2018;56(9):775-783. [DOI] [PubMed] [Google Scholar]
- 22. Zhang H, Cowling DW, Graham JM, Taylor E. Five-year impact of a commercial accountable care organization on health care spending, utilization, and quality of care. Med Care. 2019;57(11):845-854. [DOI] [PubMed] [Google Scholar]
- 23. Medicare ACOs won’t tell how they pay doctors. pnhp.org. 2017. Accessed November 28, 2021. https://pnhp.org/news/medicare-acos-wont-tell-how-they-pay-doctors/
- 24. Department of Veterans Affairs. Volume II Medical Programs and Information Technology Programs. 2020. Accessed August 21, 2020. https://www.va.gov/budget/docs/summary/fy2021VAbudgetVolumeIImedicalProgramsAndInformationTechnology.pdf
- 25. Health Resources & Services Administration. Consumer Price Index (CPI) for Medical Care. 2020. Accessed September 1, 2020. https://www.hrsa.gov/get-health-care/affordable/hill-burton/cpi.html
- 26. Tennant PWG, Murray EJ, Arnold KF, et al. Use of directed acyclic graphs (DAGs) to identify confounders in applied health research: review and recommendations. Int J Epidemiol. 2021;50(2):620-632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gao J, Moran E, Almenoff PL. Case-mix for performance management. Med Care. 2018;56(6):537-543. [DOI] [PubMed] [Google Scholar]
- 28. Gao J, Moran E, Schwartz A, Ruser C. Case-mix for assessing primary care value (CPCV). Health Serv Manage Res. 2020;33(4):200-206. [DOI] [PubMed] [Google Scholar]
- 29. Gao J, Moran E, Higgins DS, Mecher C. Predicting high-risk and high-cost patients for proactive intervention. Med Care. 2022;60(8):610-615. [DOI] [PubMed] [Google Scholar]
- 30. Macinko J, Starfield B, Shi L. Quantifying the health benefits of primary care physician supply in the United States. Int J Health Serv. 2007;37(1):111-126. [DOI] [PubMed] [Google Scholar]
- 31. Hurley RE, Freund DA, Taylor DE. Emergency room use and primary care case management: evidence from four Medicaid demonstration programs. Am J Public Health. 1989;79(7):843-846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Parchman ML, Culler SD. Preventable hospitalizations in primary care shortage areas. An analysis of vulnerable Medicare beneficiaries. Arch Fam Med. 1999;8(6):487-491. [DOI] [PubMed] [Google Scholar]
- 33. Parchman ML, Culler S. Primary care physicians and avoidable hospitalizations. J Fam Pract. 1994;39(2):123-128. [PubMed] [Google Scholar]
- 34. Bindman AB, Grumbach K, Osmond D. Preventable hospitalizations and access to health care. JAMA. 1995;274(4):305-311. [PubMed] [Google Scholar]
- 35. Edwards ST, Saha S, Prentice JC, et al. Preventing hospitalization with veterans affairs home-based primary care: which individuals benefit most? J Am Geriatr Soc. 2017;65(8):1676-1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Basu S, Berkowitz SA, Phillips RL. Association of primary care physician supply with population mortality in the United States, 2005-2015. JAMA Intern Med. 2019;179(4):506-514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hebert PL, Liu CF, Wong ES, et al. Patient-centered medical home initiative produced modest economic results for Veterans Health Administration, 2010-12. Health Aff. 2014;33(6):980-987. [DOI] [PubMed] [Google Scholar]
- 38. Chang ET, Yoon J, Esmaeili A, et al. Outcomes of a randomized quality improvement trial for high-risk Veterans in year two. Health Serv Res. 2021;56:1045-1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-jpc-10.1177_21501319221141792 for The Effect of Primary Care Visits on Total Patient Care Cost: Evidence From the Veterans Health Administration by Jian Gao, Eileen Moran, Rachel Grimm, Andrew Toporek and Christopher Ruser in Journal of Primary Care & Community Health