Abstract
This randomized controlled trial tested the Vermont Family Based Approach (VFBA) in primary care pediatrics. The VFBA is a model of healthcare delivery that shifts the focus from the individual to the family, emphasizes emotional and behavioral health, and uses evidence-based health promotion/prevention along with the treatment of emotional and behavioral problems. Participants were 81 families of 3–15-year-olds. For children, the VFBA was associated with greater reductions than the Control condition on the Child Behavior Checklist Emotionally Reactive, Withdrawn, Sleep Problems, Aggressive Behavior and Total Problems scales. For parents, the VFBA was associated with greater reductions than the Control condition on the Adult Self-Report Anxious/Depressed, Rule-Breaking Behavior, Internalizing Problems and Total Problems scales. The VFBA was also associated with greater improvement than the Control condition in the parents’ health-related quality of life, as indicated by all scales of the Medical Outcomes Study Health Survey.
Keywords: Vermont Family Based Approach, Family-based healthcare, Health promotion and prevention, RCT
Introduction
The American healthcare system faces complex challenges, such as the compartmentalization and inefficiency of care, overemphasis on treatment at the expense of health promotion, and the ever-increasing healthcare costs [1, 2]. The Vermont Family Based Approach (VFBA) is a model of healthcare delivery that was developed to address some of these challenges [3, 4]. The VFBA prioritizes emotional and behavioral health, shifts the focus from the individual to the family, and offers health promotion and illness prevention along with intervention.
Main Features of the VFBA
The VFBA brings emotional and behavioral health to the center of healthcare. Emotional and behavioral health is treated as a foundational aspect of health that affects all other aspects. It is continuously monitored at the population level, and is supported and treated, as needed. The VFBA focuses on emotional and behavioral health because emotional and behavioral problems predict or influence the course of a broad range of other health conditions [5, 6], while positive psychological functioning predicts longevity and protects against health problems [7–9]. As they often have a childhood onset and affect most everyone by adulthood [10, 11], emotional and behavioral health conditions are also the most ubiquitous health conditions. They are also the most costly health conditions in the US [12], and are among the key drivers of the global burden of disease in children, adolescents, and adults [13–16].
The VFBA organizes emotional and behavioral healthcare around the entire family, rather than the individual. Organizing healthcare around the family includes continuously monitoring and treating both children’s and parents’ emotional and behavioral health, and, where needed, delivering evidence-based interventions from the family perspective. The VFBA also focuses on the family by directly targeting the family’s health culture, or the health-related knowledge, attitudes, and practices shared by family members. The VFBA shifts the focus of healthcare from the individual to the family because health is familial: Good general health [17–19], general health problems [20–22], and health-related behaviors [23–25] cluster in families. Parents’ and children’s emotional and behavioral health also transact over time [26–29], and the treatment of parents’ emotional and behavioral health problems reduces children’s problems [30, 31]. Parents also create the family’s health culture, and pass it on to their children. Because parents’ and children’s emotional and behavioral health are so closely related and poor parental emotional and behavioral health compromises the parents’ ability to create a robust family health culture [32–34], the VFBA addresses both parents’ and children’s emotional and behavioral health.
The VFBA also emphasizes health promotion. Families are helped to develop a strong health culture by promoting healthy family routines and practices. The VFBA emphasizes family activities that have been empirically supported for enhancing emotional and behavioral health, such as mindfulness and music practice, exercise, sleep, healthy nutrition, and positive community connection (social support) [35–46]. These areas of health promotion serve as the VFBA pillars of wellness. The VFBA emphasizes health promotion based on the evidence that lifestyle interventions are associated with better emotional and behavioral, cardiovascular, endocrine, neurological, renal, and respiratory health [47–52].
Finally, the VFBA is also a population-based approach. It is designed for community settings, as will be demonstrated in this paper. However, it can also be implemented in specialty mental health clinics [53, 54]. The population-based design of the VFBA is based on the abundant evidence that combining the treatment of existent health conditions with ongoing community-wide health monitoring, prevention, and early intervention is associated with better population health than providing treatment alone [55–57].
Implementation of the VFBA
The Family Wellness Coach (FWC)
The FWC is a new healthcare professional introduced in the VFBA. FWCs receive training in foundations of behavior change, motivational interviewing (MI) [58], and evidence-based health promotion. They work with families on a comprehensive program of health and wellness, which is organized around the VFBA pillars of wellness. FWCs also help families to navigate the healthcare system and overcome healthcare barriers (e.g., low health literacy, transportation problems, stigma), and advocate on behalf of the family to the healthcare team. Because the VFBA emphasizes emotional and behavioral health, FWCs also continuously monitor the emotional and behavioral health of family members using empirically based assessment instruments.
The Focused Family Coach (FFC) and Family Based Psychiatrist (FBP)
The VFBA is a team-based model of healthcare delivery. If at any point the results of ongoing assessment indicate that family members are experiencing significant emotional and behavioral problems, FWCs connect them to other members of the VFBA treatment team, FFCs and FBPs. FFCs are credentialed psychotherapists who offer evidence-based treatment from the family perspective. Treatment may comprise individual psychotherapy for child or parent, or family psychotherapy for several or all family members. FBPs provide evidence-based psychiatric care from the family perspective by treating child and adult family members separately or together.
Health Promotion Resources
The VFBA provides families with health promotion opportunities for free or at a discounted rate. These include group or individual exercise, nutrition, music, mindfulness, and parenting classes. Some of these are offered by FWCs who generally hold formal credentials in at least one domain of health promotion, and others are offered by community partners.
The Present Study
We previously tested the feasibility of the VFBA in Head Start programs in South Dakota and Vermont [59, 60]. The intervention was feasible in both states, and results in Vermont indicated a significant decrease in children’s emotional and behavioral problems, as measured by the CaregiverTeacher Report Form [61].
The present study was the first randomized controlled trial (RCT) of the VFBA. It was a small, institutionally-funded pilot RCT conducted in the University of Vermont Children’s Hospital Pediatric Primary Care Clinic (UVM Pediatrics). Its primary aim was to test the feasibility of the VFBA in community primary care pediatrics.
Primary care pediatrics offers an especially fitting environment for the VFBA. Primary care removes many structural and attitudinal barriers for accessing mental health services, such as unfamiliarity, inaccessibility, and stigma [62]. Not surprisingly, integrating primary and behavioral healthcare for children leads to significantly improved behavioral health outcomes than providing primary care alone [63].
Ivanova et al. presented results of this trial on feasibility and healthcare engagement [3]. They reported that the project was successfully implemented at UVM Pediatrics, and that families in the VFBA group demonstrated high engagement with family wellness coaching, having had on average 36.35 (SD = 25.51) contacts with FWCs over the course of the study. Over the course of the intervention, the VFBA group demonstrated a significantly steeper increase than the Control group in both looking into and receiving psychotherapy, as well as exercise/fitness, mindfulness and music training [3].
In this paper, we present results of analyses that tested the efficacy of the VFBA for improving emotional and behavioral health for parents and children. Because of our previous finding that the VFBA was effective at engaging parents in mental health services [64], we also tested whether the VFBA was associated with improved parental health-related quality of life.
Method
Design
The study was an RCT with open (un-blinded) randomization and consecutive recruitment. From December, 2015 to December, 2017 we recruited 81 families. Data collection concluded in June, 2018 to allow families that were recruited in December 2017 at least 6 months to experience the study conditions. Families thus experienced 6–30 months of their assigned intervention.
Setting
The study was conducted at a community primary care pediatric clinic that serves Burlington, Vermont and the surrounding area. With a population of over 42,800 residents, Burlington is the largest city in Vermont. The median household income is $50,324, and 24.7% of residents live below the federal poverty level [65]. Burlington’s population is primarily non-Hispanic White (82.9%), with Asian (6.3%), Black/African American (5.3%), and Hispanic/Latino (2.8%) residents being the largest minority groups [65].
Procedures
We relied on pediatric practitioners to introduce the study during their appointments with families because the UVM Medical Center prohibits direct recruitment of patients by research personnel. Following their clinic appointment, interested families were contacted and consented in person. Families then completed a comprehensive baseline assessment and were randomized to the VFBA or Control groups. All families completed interim assessments every 4–6 months thereafter and a final comprehensive assessment at the conclusion of the study. Study procedures were approved by the UVM Institutional Review Board.
VFBA Condition
Families were partnered with FWCs and received ongoing family wellness coaching. During coaching sessions, FWCs helped families to select health promotion goals, develop step-by-step plans for reaching those goals, and overcome barriers to meeting them. FWCs supported families in executing their plans by teaching them health-related skills, such as preparing nutritious meals, creating healthy sleep routines, and shaping children’s positive behavior.
Families in the VFBA condition also received therapeutic assessment feedback, based on the results of the initial comprehensive family assessment that was conducted before randomization. This assessment included the instruments described under Assessment Instruments below, instruments for assessment of the family environment [66–68], and instruments for assessment of family health engagement that were developed for this study [3]. When the target child or parent(s) obtained a scale score that placed them in the borderline to clinical range on measures of emotional and behavioral problems described under Assessment Instruments below, the FWCs facilitated a “warm” referral to a FFC or FBP, who were immediately available.
Families in the VFBA group were also continuously offered a menu of cost-free health promotion activities and services, most of which were provided or organized by project staff. FWCs offered weekly violin instruction for children and parents (individual or group, depending on the family’s preference) and mindfulness and yoga instruction for children and parents. FWCs also organized regular family wellness events that focused mostly on mindfulness and nutrition, and bi-annual music recitals followed by dinner celebrations for the violin students. FFCs and the FBP held parenting classes based on an evidence-based behavioral parent training protocol [69]. Families in the VFBA group were not remunerated.
The VFBA care team comprising FWCs, FFCs, and the FBP met weekly to coordinate family care. Referrals to FFCs or the FBP were made during these meetings, based on case presentations by FWCs, reviews of family data, and family preferences. FWCs communicated regularly with pediatric practitioners in person or by phone or email. Also, we used an online care coordination platform (ACT.md [70]) to facilitate communication among team members, pediatric practitioners, and parents.
Control Condition
Families received pediatric care as usual. They received $100 for completing comprehensive baseline and final assessments and $50 for completing each smaller interim assessment.
Study Enrollment and Retention
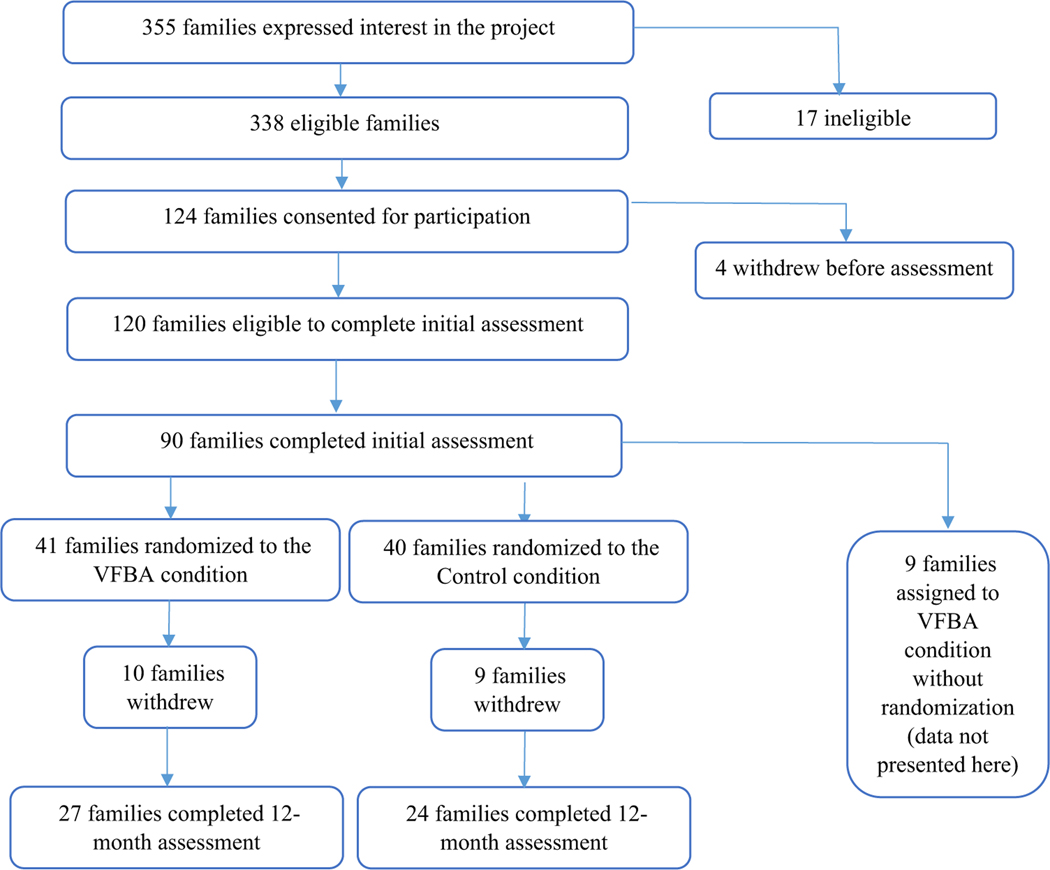
Because we relied on pediatric practitioners to introduce the study to families, we are unable to provide information about the number of families who were approached. However, the 355 families who expressed interest in the study represented about 11% of eligible families who were seen at the clinic during the recruitment period. As Fig. 1 illustrates, of the 355 families that expressed interest in the study, 17 were deemed ineligible (14 due to insufficient English proficiency, 2 for living outside of a reasonably drivable distance from the Medical Center, and 1 for refusing to complete the study paperwork). Of the 338 eligible families, 124 consented for participation, but 4 withdrew before beginning the initial assessment. One-hundredand-twenty families thus began initial assessments, and 90 (75%) completed them. Of the 90, 81 were randomized to the VFBA (N = 41) or Control (N = 40) arms. The remaining 9 were assigned to the VFBA group, and their data are not presented.
Fig. 1.
Consolidated standards of reporting trials (CONSORT) diagram of study enrollment and retention
Rates of attrition were comparable between the groups, with 10 families in the VFBA group (24%) and 9 families in the Control group (23%) withdrawing from the study within the 12-month interval. Reasons for withdrawal were comparable between the groups: In the VFBA group, 2 families moved out of the area, 1 child moved out of the area to live with a different custodial parent, and the remaining 7 families did not provide a reason for their withdrawal. In the Control group, 3 families moved out of the area, and the remaining 6 families did not provide a reason for their withdrawal.
Participants
Eligibility
Parents were required to be seeking non-acute pediatric care for their child and be proficient enough in English to complete assessment materials. Families were not preselected on any risk factor. The study was originally designed as a 12-month trial with families of 3–6-year-olds. Because the UVM Medical Center extended its funding of the project beyond the 12-month period, we expanded the upper age of the children to 15 years during the second year of recruitment to broaden our understanding of the efficacy of the VFBA with older children.
Participants
The intent-to-treat sample comprised 81 children and their families. The child sample was 46% female (37 girls/44 boys) and primarily of preschool age at baseline assessment (M = 4.89; SD = 1.88; range: 3–14 years old). The majority of children were Non-Hispanic, White (53 children or 65.4%). Of the remaining 28, 10 (12.3%) were of African, 6 (7.4%) of Asian, 5 (6.2%) of Middle Eastern, 3 (3.7%) of Hispanic, and 4 (4.9%) of mixed descent. Fifteen children (18.5%) were from new American families.
To describe the socioeconomic status (SES) of families, we used the Hollingshead SES index for parental occupations updated by Achenbach [71]. A numeric SES code was assigned to every family, ranging from 10 (low) to 90 (high). SES scores ranged from 10 to 90 (M = 53.95; SD = 25.92). For 21 families (26%) the score was < 30, indicating the very low to low range.
Study participants were thus more diverse in their racial and ethnic background in comparison to Burlington’s population, which is over 82% non-Hispanic White [65]. The proportion of study families whose SES score was in the very low to low range (26%) was comparable to the proportion of Burlington households that live below the federal poverty level (24.7%) [65].
The VFBA and Control groups did not differ with respect to child age, family SES, and proportions of new American families, single-parent families, or families with a history of parental divorce, as tested via independent-sample t-tests (see Supplementary Table 1). For race and ethnicity, we compared proportions of Non-Hispanic, White, African or African-American, Asian, Middle Eastern, and Hispanic children using the “N−1” Chi-squared test [72]. No differences were found, except for the Middle Eastern ethnicity, which was significantly more prevalent in the VFBA than Control sample (X2 = 5.14; p < 0.05).
Assessment Instruments
Children’s Emotional and Behavioral Problems
Children’s emotional and behavioral problems were measured by the Child Behavior Checklist for Ages 1.5–5 and the Child Behavior Checklist for Ages 6–18 (CBCL/1.5–5 and CBCL/6–18) [61, 73] because our sample included children of both age ranges. Normed on a U.S. national household sample, the CBCL obtains parent reports of children’s emotional, behavioral, and social problems. Factor analyses of the CBCL/1.5–5 and CBCL/6–18 yielded 7 and 8 syndromes, respectively [61, 73], which have been supported by confirmatory factor analyses of parent ratings of tens of thousands of children in dozens of societies [74, 75]. CBCL syndrome scales have good psychometric properties [61, 73], and have been used in primary care pediatrics [76, 77].
Parents’ Emotional and Behavioral Problems
Parents’ emotional and behavioral problems were measured with the Adult Self-Report (ASR) [78]. The ASR is a self-report questionnaire that assesses emotional, behavioral, and social problems and adaptive functioning. Factor analyses of the ASR problem items yielded 8 syndrome scales, which have been supported by confirmatory factor analyses of tens of thousands of adults in dozens of societies [79]. All scales were normed on a U.S. national household sample and have good psychometric properties [78].
Parents’ Health-Related Quality of Life
Parents’ health-related quality of life was measured with the MOS 36-item Short-Form Health Survey (MOS SF-36), which was developed to assess general health in the medical outcomes study [80–82]. The MOS SF-36 offers a multidimensional perspective on health-related quality of life, and is widely used in health-related research. Its scales have good internal consistency (αs > 0.78) [81] and validity [82].
Data Analyses
For our primary outcomes, we used Generalized Estimating Equations (GEE) to compare rates of change between the two groups from baseline assessment to the 12-month follow-up [83–85]. GEE is a powerful, iterative, population-averaged, non-parametric estimation approach for modeling non-independent data that offers effective ways of modeling repeated observations via an autoregressive function. We chose GEE because we could not assume that health outcomes for our sample of participants drawn from the same community clinic would be conditionally independent.
We used age and gender of the assessed person as covariates in all models of emotional and behavioral problems because the effects of age and gender on child and adult psychopathology are well established [86–88]. All GEE models were specified with a model-based covariance matrix, first-order autoregressive correlation matrix, 100 maximum iterations, linear scaling, and the Wald chi-square statistics.
Results
Engagement with the VFBA Intervention
Supplementary Table 2 presents program engagement information for the VFBA group. With the exception of the 3 families that withdrew within the first month, all families took advantage of VFBA offerings. The number of VFBA activities or services per family ranged from 2 to 19, with a mean and median of 10 (SD = 3.82). For example, 31 (75.6%) of target children and 5 siblings and 11 (26.8%) of target parents participated in violin lessons; and 16 (39%) of target children and 14 siblings and 31 (75.6%) of target parents participated in yoga or mindfulness training. Many families also took advantage of family-based activities: 5 (12.2%) had family violin lessons, 13 (31.7%) had family yoga or mindfulness sessions, 33 (80.5%) had family nutrition training, and 20 (48.8%) participated in family wellness nights. A large proportion of families also received parenting support. FWCs offered parenting coaching to 26 (63.4%) families, and 8 (19.5%) families attended the 6-session parenting group.
FWCs also connected many families to systems and resources. They provided case coordination or case management to 20 (48.4%) families, and provided coaching addressing housing, food, and transportation insecurity to 6 (14.6%), 4 (9.8%), and 5 (12.2%) families, respectively. Families also took advantage of resources provided by FWCs that allowed them to participate in community-based health promotion, such as YMCA membership (5/12.2%), dance lessons (6/14.6%), and entry passes to state parks (32/78%) and museums (18/43.9%).
More families received care from the project’s FFCs than FBPs. For FFCs, 8 (19.5%) target children, 5 siblings, and 28 (68.3%) of target parents received psychotherapy. For FBPs, 5 (12.2%) target children, 2 siblings and 2 (4.9%) target parents received psychiatric care. In addition, 9 (22%) families received family psychotherapy and 2 (4.9%) received family psychiatric care.
Table 1 presents observed means and standard deviations for the CBCL, ASR, and MOS-SF36 scale scores, along with p values for the time (Pre-Trial vs. 12months follow-up) by group (VFBA vs. Control) interactions from GEE analyses. At baseline, there were no differences between groups on any CBCL, ASR, or MOS-SF36 scale score.
Table 1.
Descriptive statistics for the Child Behavior Checklist (CBCL) and Adult Self-Report (ASR) syndrome scores and the MOS-SF36 scores at baseline and 12 months by group
| Syndromes and Scales | VFBA | Control | P time × group interaction | ||
|---|---|---|---|---|---|
|
|
|
||||
| Baseline M (SD) | 12 Months M (SD) | Baseline M (SD) | 12 Months M (SD) | ||
| CBCL | |||||
| Emotionally Reactivea | 2.71 (2.82) | 2.32 (2.16) | 2.55 (2.36) | 2.42 (3.34) | *** |
| Anxious/Depressed | 3.52 (3.99) | 2.51 (3.14) | 2.98 (2.74) | 2.55 (3.18) | |
| Somatic Complaints | 2.00 (2.42) | 1.19 (1.27) | 2.25 (2.53) | 2.03 (2.82) | |
| Withdrawna | 2.39 (2.97) | 2.16 (2.69) | 1.87 (2.17) | 1.5 (1.98) | *** |
| Sleep Problemsa | 2.71 (2.79) | 2.53 (2.46) | 2.61 (3.11) | 3.58 (3.63) | * |
| Attention Problems | 3.44 (3.51) | 2.51 (2.76) | 4.28 (3.7) | 4.1 (4.48) | |
| Aggressive Behavior | 10.29 (8.67) | 6.11 (7.27) | 9.37 (6.59) | 6.52 (7.3) | * |
| Internalizing Problems | 10.35 (9.57) | 6.51 (6.31) | 8.81 (7.47) | 6.65 (8.62) | |
| Externalizing Problems | 12.82 (10.27) | 8.16 (9.48) | 12.25 (8.41) | 8.68 (9.01) | |
| Total Problems | 36.98 (28.45) | 24.54 (23.23) | 34.93 (23.18) | 29.19 (26.48) | * |
| ASR | |||||
| Anxious/Depressed | 7.43 (5.91) | 4.44 (5.56) | 7.81 (6.75) | 5.11 (5.32) | *** |
| Withdrawn | 2.45 (2.44) | 1.11 (2.53) | 2.83 (2.87) | 2.06 (2.55) | |
| Somatic Complaints | 3.05 (2.91) | 2.07 (3.77) | 3.38 (3.66) | 3.67 (5.24) | |
| Thought Problems | 1.72 (1.75) | 1.00 (1.11) | 1.94 (2.13) | 1.83 (3.07) | |
| Attention Problems | 5.97 (4.89) | 3.30 (3.10) | 5.60 (5.17) | 4.33 (4.52) | |
| Aggressive Behavior | 5.28 (4.37) | 2.67 (2.79) | 4.56 (4.70) | 3.00 (3.65) | |
| Rule-Breaking Behavior | 2.03 (2.17) | 0.85 (1.32) | 1.96 (2.55) | 2.00 (2.68) | *** |
| Intrusive | 1.69 (2.04) | 0.96 (1.22) | 1.33 (1.78) | 0.89 (0.76) | |
| Internalizing Problems | 12.93 (9.54) | 7.63 (11.28) | 14.02 (11.37) | 10.83 (11.89) | *** |
| Externalizing Problems | 9.00 (6.93) | 4.48 (3.90) | 7.85 (7.84) | 5.89 (6.11) | |
| Total Problems | 37.41 (23.32) | 21.85 (20.88) | 37.44 (28.86) | 28.89 (27.64) | *** |
| MOS-SF36 | |||||
| Physical Functioning | 84.43 (22.03) | 86.47 (20.58) | 88.11 (18.43) | 85.44 (23.14) | *** |
| Social Functioning | 86.65 (27.94) | 90.91 (24.06) | 91.75 (25.59) | 92.05 (27.03) | *** |
| Role Limitations Due to Physical Health Problemsb | 73.30 (35.93) | 81.62 (28.41) | 71.63 (34.31) | 75.74 (37.68) | *** |
| Role Limitations Due to Personal or Emotional Problemsb | 70.45 (40.80) | 81.37 (31.98) | 69.87 (45.86) | 68.63 (42.59) | *** |
| Emotional Wellbeing | 69.81 (16.08) | 73.75 (17.06) | 71.60 (19.08) | 72.77 (17.17) | *** |
| Energy/Vitality | 46.07 (19.62) | 53.59 (20.49) | 52.00 (21.48) | 59.84 (18.19) | *** |
| Bodily Painb | 72.03 (26.27) | 79.16 (19.59) | 79.01 (21.28) | 75.45 (28.66) | *** |
| General Health | 68.02 (16.48) | 73.39 (14.16) | 66.40 (23.78) | 65.31 (25.17) | *** |
p = p of the interaction of time of assessment (baseline vs. 12 months) and group (VFBA vs. Control);
p < 0.05
p < 0.001
Ages 3–5
Higher scores = less pain and role limitations; all analyses conducted using Generalized Estimating Equations
Emotional and Behavioral Problems
Children’s Emotional and Behavioral Problems
The time-by-group interaction was statistically significant for the CBCL Emotionally Reactive [B = − 0.71 (SD = 0.02); Wald chi-square = 1466.96; p < 0.001], Withdrawn [B = − 0.28 (SD = 0.02); Wald chi-square = 213; p < 0.001], Sleep Problems [B = − 2.50 (SD = 0.98); Wald chisquare = 6.51; p < 0.05], Aggressive Behavior [B = − 2.06 (SD = 1.05); Wald chi-square = 3.89; p < 0.05], and Total Problems [B = − 7.60 (SD = 3.16); Wald chi-square = 5.80; p < 0.05] scale scores. For all significant interactions, except the CBCL Sleep Problems scale, children’s CBCL scale scores decreased over time, but the decrease was significantly larger for the VFBA group. For CBCL Sleep Problems, the score decreased for the VFBA group, but increased for the Control group.
Parents’ Emotional and Behavioral Problems
The interaction was statistically significant for the ASR Anxious/Depressed [B = 1.32 (SD = 0.03); Wald chi-square = 2070.62; p < 0.001], Rule-Breaking Behavior (B = − 0.44 (SD = 0.01); Wald chi-square = 1237.63; p < 0.001), Internalizing Problems [B = 1.25 (SD = 0.05); Wald chi-square = 579.55; p < 0.001], and Total Problems [B = 1.63 (SD = 0.13); Wald chi-square = 154.69; p < 0.001] scale scores. For all significant interactions, except Rule-Breaking Behavior, the ASR scale scores decreased over time, but the decrease was significantly larger for the VFBA group. For ASR Rule-Breaking Behavior, the scale score decreased for the VFBA group, but increased for the Control group.
Parents’ Health-Related Quality of Life
The interaction was statistically significant for the Physical Functioning [B = 4.96 (SD = 0.21); Wald chi-square = 545.36; p < 0.001], Social Functioning [B = 6.68 (SD = 0.16); Wald chi square = 1702.16; p < 0.001], Role Limitations due to Physical Health Problems [B = 6.34 (SD = 0.20); Wald chi-square = 1021.43; p < 0.001], Role Limitations due to Personal or Emotional Problems [B = 17.17 (SD = 0.19); Wald chi-square = 7804.73; p < 0.001], Emotional Wellbeing [B = 2.21 (SD = 0.19); Wald chi-square = 140.66; p < 0.001], Energy/Vitality [B = 0.85 (SD = 0.17); Wald chi-square = 25.66; p < 0.001], Bodily Pain [B = 9.36 (SD = 0.17); Wald chi-square = 3035.48; p < 0.001], and General Health [B = 3.00 (SD = 0.003); Wald chi-square = 1,099,870.05; p < 0.001] scores.
To illustrate the significant time × group interactions, Supplementary Fig. 1a–c plot the estimated marginal means from the GEE analyses for the CBCL and ASR Total Problems scores and the MOS SF-36 Physical Functioning scale.
Effect Sizes (ESs) and Clinical Significance
To calculate the ESs of the VFBA, we weighed the differences of the subtracted pre-post means by the pooled pre-test standard deviations. We calculated the ESs for the CBCL and ASR Total Problems scores as broad indicators of emotional and behavioral health, and for the MOS SF-36 General Health scale as a broad indicator of general health. They ESs were small: d = 0.26, 0.27 and 0.31, respectively.
To determine the clinical significance of pre- to post-intervention changes in children’s and parents’ emotional and behavioral problems, we evaluated the changes in scale scores in relation to their standard errors of measurement (SEMs) based on their normative samples, as proposed by Achenbach et al. [61, 73, 78] We chose this method for our community sample because the CBCL and ASR are normed on representative community samples. For the CBCL and ASR Total Problems scores, the pre- to post-intervention change scores were larger than their SEMs. This indicated that the observed difference exceeded change that was likely to occur by chance 68% of the time.
Discussion
Our results supported the efficacy of the VFBA for improving children’s and parents’ emotional and behavioral health and parents’ health-related quality of life. They indicated that the VFBA is not only feasible and acceptable in primary care pediatrics [3], but is also associated with improved health outcomes for children and parents. The VFBA affected a wide range of emotional and behavioral problems and aspects of health-related quality of life.
The VFBA includes key components of effective models of integration of emotional and behavioral healthcare with primary care that have been identified in the literature, such as population-, measurement-, and team-based care, care management, psychiatric consultation, and evidence-based mental health services [89, 90]. What sets it apart from existing models are its family-based organization of care and strong emphasis on health promotion.
Several methodological aspects of our study underscore the robustness of the VFBA’s effects. Our sample size was small, and the variance of our health-related outcomes was likely limited for our healthy community sample. In addition, previous studies have shown that effects of preventive/health promoting interventions with children and families may not emerge until years after the interventions [91–93]. The Control group, which received pediatric care as usual at UVM Pediatrics, provided a formidable comparison condition, as it included emotional-behavioral interventions. UVM Pediatrics has a full-time Social Worker and doctoral-level Clinical Psychologist on staff, who provide case management/care coordination and psychotherapy services, respectively. Overall, the VFBA showed significant therapeutic effects in conditions of limited statistical power and in relation to a rigorous active Control condition.
Our results also indicated that community parents and children are willing to devote considerable time and energy to learning and practicing health promoting skills and activities, provided that common barriers to doing so are minimized. On average, families engaged with 10 VFBA activities and services. This is a conservative figure because it indicates 10 types of activities and services, rather than the number of attended sessions. Rates of engagement with violin lessons and yoga/mindfulness training were especially high (see Supplementary Table 1).
As the first RCT of the VFBA, this was largely a proof of concept study. Our results indicated that a healthcare delivery approach that emphasizes emotional and behavioral health is acceptable to families and practitioners in community primary care settings. Our explicit emphasis on health promotion and prevention rather than psychopathology and our ongoing cost-free wellness offerings likely contributed to the acceptability of the project for families. As indicated by their referrals of patients to the project, the VFBA was also acceptable to pediatric primary care practitioners for whom health promotion and emphasis on emotional and behavioral health are already part of professional culture.
While the VFBA would be especially compatible with a medical home model, our results indicated that it is feasible within a conventional fee-for-service healthcare environment. The project was internally funded by a small institutional grant and leveraged many existing resources. FFCs and the FBP provided their clinical services as part of their regular clinic activity. Because FWCs held credentials in a variety of health promotion disciplines, they provided the health promotion offerings to the VFBA group. Most of the awarded funding was used for Research Project Coordinator and FWC salaries. The Coordinator position is unique to research, and FWC salaries could be offset by selecting FWCs who hold professional mental health credentials and can provide billable psychotherapeutic services as part of their responsibilities.
However, it is important to acknowledge that the generalizability of this approach is limited by the availability of funds to support “pure” FWCs, and by the availability of FWCs who hold both health promotion and professional mental health credentials. Also, although it would be best to build coaching capacity to address every VFBA wellness pillar within a single health practice setting, this may be especially challenging in smaller practices. These limitations can be addressed by establishing partnerships with credentialed health promotion and wellness practitioners in the community.
The results of this study should be interpreted in the context of its limitations. Because our group developed the VFBA, our enthusiasm for the approach could have contributed to group differences by enhancing our therapeutic effectiveness. Open randomization could have further enhanced group differences by setting up condition-consistent expectancies for both families and study personnel. In addition, because FWCs were continuously in touch with families, the VFBA group most likely received more attention from health professionals than the Control group. Furthermore, the health-related outcomes reported in this paper were based solely on parents’ reports, introducing a methodological bias. Finally, although we tried to remove participation barriers by offering all study activities free of charge and in locations accessible by public transportation, we were likely not spared the common limitation of family intervention trials; that families with the least resources are also the least likely to participate. For example, isolated rural families without personal transportation would not have chosen to participate, and neither would have families with limited personal and social resources who could not commit to our extensive protocol.
In the future, we aim to test the VFBA in larger and better powered clinical trials, where we can overcome these limitations. These trials will also answer broader and more complex questions than those pursued in this pilot. For example, we will test individual patient and family differences in clinical responses to the VFBA as a whole and to its therapeutic components. Because the health promotion and prevention aspect of the VFBA targets the broader family health culture and emotional and behavioral health affects other aspects of health, we will also test the effects of the VFBA on general health outcomes. Also, based on the data from this trial, we previously reported that the VFBA was associated with increased engagement in health promotion activities and services and in psychotherapy [3]. However, we lacked statistical power to formally test these changes in engagement as mediators of the effects of the VFBA. Understanding such mechanisms of change would be essential for shaping the development of the VFBA. Finally, we will test our prediction that the VFBA will increase the cost effectiveness of care by preventing serious health problems and reducing the redundancy of provided care by organizing it centrally at the family level.
In conclusion, combined with the results reported by Ivanova et al. [3], results of this study indicated that the VFBA is a promising healthcare delivery model that is acceptable to patients and healthcare providers, feasible in real-life clinical settings, and is associated with positive health outcomes for children and parents.
Summary
This randomized controlled trial conducted in primary care pediatrics tested the effects of the Vermont Family Based Approach (VFBA) on children’s and parents’ emotional and behavioral problems and parents’ health-related quality of life. The VFBA is a model of healthcare delivery that shifts the focus from the individual to the family, emphasizes emotional and behavioral health, and uses evidence-based health promotion and prevention along with the treatment of emotional and behavioral problems. Participants were 81 families of 3- to 15-year-olds who were seeking non-acute care for the children at a community primary care pediatric clinic. Families presented consecutively at the clinic, were not pre-selected on any risk factor, and were openly randomized to the VFBA or Control conditions. The VFBA group received family-based assessment of emotional and behavioral health and family functioning, family wellness coaching, and a menu of cost-free health promotion activities, such as parent and child violin instruction, yoga and mindfulness training, and nutrition counseling. Where indicated by results of the family-based assessment, families in the VFBA group also received family-based evidence-based psychotherapy and psychiatric care. Families in the Control group received pediatric primary care, as usual. For children, the VFBA was associated with greater reductions than the Control condition on the parent-report Child Behavior Checklist (CBCL) Emotionally Reactive, Withdrawn, Sleep Problems, Aggressive Behavior and Total Problems scale scores. For parents, the VFBA was associated with greater reductions than the Control condition on the Adult Self-Report (ASR) Anxious/Depressed, Rule-Breaking Behavior, Internalizing Problems and Total Problems scale scores. The VFBA was also associated with greater improvement in parents’ health-related quality of life than the Control condition, as indicated by all scales of the self-report Medical Outcomes Study 36-item Short-Form Health Survey (MOS SF-36). The VFBA was thus associated with improved emotional and behavioral health outcomes for children and parents and with improved health-related quality of life for parents. A healthcare delivery model that prioritizes mental health and capitalizes on the health promoting power of the family can be effectively implemented in primary care pediatrics.
Supplementary Material
Funding
Funding was provided by the University of Vermont Medical Center.
Footnotes
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s10578-022-01329-4.
References
- 1.Glied S, Sacarny A (2018) Is the US health care system wasteful and inefficient? Review of the evidence. J Health Polit Policy Law 43(5):739–765. 10.1215/03616878-6951103 [DOI] [Google Scholar]
- 2.Herrmann JA (2018) Complex problems, progressive policy solutions, and one health. Beyond one health: from recognition to results, 1st edn. Wiley, Hoboken, pp 293–306 [Google Scholar]
- 3.Ivanova MY, Dewey L, Swift P, Weinberger S, Hudziak J (2019) Health promotion in primary care pediatrics: initial results of a randomized clinical trial of the Vermont family based approach. Child Adolesc Psychiatr Clin N Am 28(2):237–246. 10.1016/j.chc.2018.11.005 [DOI] [PubMed] [Google Scholar]
- 4.Hudziak J, Ivanova MY (2016) The Vermont Family Based Approach: family based health promotion, illness prevention, and intervention. Child Adolesc Psychiatr Clin N Am 25(2):167–178. 10.1016/j.chc.2015.11.002 [DOI] [PubMed] [Google Scholar]
- 5.Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR et al. (2007) No health without mental health. Lancet 370(9590):859–877. 10.1016/S0140-6736(07)61238-0 [DOI] [PubMed] [Google Scholar]
- 6.Kolappa K, Henderson DC, Kishore SP (2013) No physical health without mental health: lessons unlearned? Bull World Health Organ 91(1):3–3A. 10.2471/BLT.12.115063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DuBois CM, Lopez OV, Beale EE, Healy BC, Boehm JK, Huffman JC (2015) Relationships between positive psychological constructs and health outcomes in patients with cardiovascular disease: a systematic review. Int J Cardiol 195:265–280. 10.1016/j.ijcard.2015.05.121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kubzansky LD, Huffman JC, Boehm JK, Hernandez R, Kim ES, Koga HK et al. (2018) Positive psychological well-being and cardiovascular disease: JACC health promotion series. J Am Coll Cardiol 72(12):1382–1396. 10.1016/j.jacc.2018.07.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Celano CM, Beale EE, Moore SV, Wexler DJ, Huffman JC (2013) Positive psychological characteristics in diabetes: a review. Curr Diab Rep 13(6):917–929 [DOI] [PubMed] [Google Scholar]
- 10.Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R (2003) Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry 60(7):709–717. 10.1001/archpsyc.60.7.709 [DOI] [PubMed] [Google Scholar]
- 11.Copeland W, Shanahan L, Costello EJ, Angold A (2011) Cumulative prevalence of psychiatric disorders by young adulthood: a prospective cohort analysis from the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry 50(3):252–261. 10.1016/j.jaac.2010.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roehrig C (2016) Mental disorders top the list of the most costly conditions in the United States: $201 billion. Health Aff 35(6):1130–1135. 10.1377/hlthaff.2015.1659 [DOI] [PubMed] [Google Scholar]
- 13.Erskine H, Moffitt TE, Copeland W, Costello EJ, Ferrari AJ, Patton G et al. (2015) A heavy burden on young minds: the global burden of mental and substance use disorders in children and youth. Psychol Med 45(7):1551–1563. 10.1017/S0033291714002888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baranne ML, Falissard B (2018) Global burden of mental disorders among children aged 5–14 years. Child Adolesc Psychiatry Ment Health 12(1):19. 10.1186/s13034-018-0225-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE et al. (2013) Global burden of disease attributable to mental and substance use disorders: findings from the global burden of disease study 2010. Lancet 382(9904):1575–1586. 10.1016/S0140-6736(13)61611-6 [DOI] [PubMed] [Google Scholar]
- 16.Vigo D, Thornicroft G, Atun R (2016) Estimating the true global burden of mental illness. Lancet Psychiatry 3(2):171–178. 10.1016/S2215-0366(15)00505-2 [DOI] [PubMed] [Google Scholar]
- 17.You D, Gu D, Yi Z (2010) Familial transmission of human longevity among the oldest-old in China. J Appl Gerontol 29(3):308–332. 10.1177/0733464809340154 [DOI] [Google Scholar]
- 18.An P, Perusse L, Rankinen T, Borecki IB, Gagnon J, Leon AS et al. (2003) Familial aggregation of exercise heart rate and blood pressure in response to 20 weeks of endurance training: the HERITAGE family study. Int J Sports Med 24(01):57–62. 10.1055/s-2003-37200 [DOI] [PubMed] [Google Scholar]
- 19.Schwenk RW, Vogel H, Schürmann A (2013) Genetic and epigenetic control of metabolic health. Mol Metab 2(4):337–347. 10.1016/j.molmet.2013.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cárdenas-Roldán J, Rojas-Villarraga A, Anaya J-M (2013) How do autoimmune diseases cluster in families? A systematic review and meta-analysis. BMC Med 11(1):73. 10.1186/1741-7015-11-73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wassel CL, Loomba R, Ix JH, Allison MA, Denenberg JO, Criqui MH (2011) Family history of peripheral artery disease is associated with prevalence and severity of peripheral artery disease: the San Diego population study. J- Am Coll Cardiol 58(13):1386–1392. 10.1016/j.jacc.2011.06.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Albright F, Teerlink C, Werner TL, Cannon-Albright LA (2012) Significant evidence for a heritable contribution to cancer predisposition: a review of cancer familiality by site. BMC Cancer 12(1):138. 10.1186/1471-2407-12-138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Niermann CY, Spengler S, Gubbels JS (2018) Physical activity, screen time, and dietary intake in families: a cluster-analysis with mother-father-child triads. Front Public Health 6:276. 10.3389/fpubh.2018.00276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Watanabe E, Lee JS, Mori K, Kawakubo K (2016) Clustering patterns of obesity-related multiple lifestyle behaviours and their associations with overweight and family environments: a cross-sectional study in Japanese preschool children. BMJ Open 6(11):e012773. 10.1136/bmjopen-2016-012773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Swaminathan S, Thomas T, Yusuf S, Vaz M (2013) Clustering of diet, physical activity and overweight in parents and offspring in South India. Eur J Clin Nutr 67(2):128–134 [DOI] [PubMed] [Google Scholar]
- 26.McLaughlin KA, Gadermann AM, Hwang I, Sampson NA, Al-Hamzawi A, Andrade LH et al. (2012) Parent psychopathology and offspring mental disorders: results from the WHO world mental health surveys. Br J Psychiatry 200(4):290–299. 10.1192/bjp.bp.111.101253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McAdams TA, Rijsdijk FV, Neiderhiser JM, Narusyte J, Shaw DS, Natsuaki MN et al. (2015) The relationship between parental depressive symptoms and offspring psychopathology: evidence from a children-of-twins study and an adoption study. Psychol Med 45(12):2583–2594. 10.1017/S0033291715000501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shaw DS, Sitnick SL, Reuben J, Dishion TJ, Wilson MN (2016) Transactional effects among maternal depression, neighborhood deprivation, and child conduct problems from early childhood through adolescence: a tale of two low-income samples. Dev Psychopathol 28(3):819–836. 10.1017/S095457941600033X [DOI] [PubMed] [Google Scholar]
- 29.Nicholson JS, Deboeck PR, Farris JR, Boker SM, Borkowski JG (2011) Maternal depressive symptomatology and child behavior: transactional relationship with simultaneous bidirectional coupling. Dev Psychol 47(5):1312. 10.1037/a0023912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pilowsky DJ, Wickramaratne P, Talati A, Tang M, Hughes CW, Garber J et al. (2008) Children of depressed mothers 1 year after the initiation of maternal treatment: findings from the STAR* D-child Study. Am J Psychiatry 165(9):1136–1147. 10.1176/appi.ajp.2008.07081286 [DOI] [PubMed] [Google Scholar]
- 31.Wickramaratne P, Gameroff MJ, Pilowsky DJ, Hughes CW, Garber J, Malloy E et al. (2011) Children of depressed mothers 1 year after remission of maternal depression: findings from the STAR* D-child study. Am J Psychiatry 168(6):593–602. 10.1176/appi.ajp.2010.10010032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seifer R (2011) Parental psychopathology and children’s sleep. In: El-Sheikh M (ed) Sleep and development: familial and socio-cultural considerations. Oxford University Press, Oxford, pp 79–98 [Google Scholar]
- 33.Zajicek-Farber ML, Mayer LM, Daughtery LG (2012) Connections among parental mental health, stress, child routines, and early emotional behavioral regulation of preschool children in low-income families. J Soc Social Work Res 3(1):31–50. 10.5243/jsswr.2012.3 [DOI] [Google Scholar]
- 34.Manczak EM, Williams D, Chen E (2017) The role of family routines in the intergenerational transmission of depressive symptoms between parents and their adolescent children. J Abnorm Child Psychol 45(4):643–656. 10.1007/s10802-016-0187-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Demarzo MM, Montero-Marin J, Cuijpers P, Zabaleta-del-Olmo E, Mahtani KR, Vellinga A et al. (2015) The efficacy of mindfulness-based interventions in primary care: a meta-analytic review. Ann Fam Med 13(6):573–582. 10.1370/afm.1863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fjorback LO, Arendt M, Ørnbøl E, Fink P, Walach H (2011) Mindfulness-based stress reduction and mindfulness-based cognitive therapy–a systematic review of randomized controlled trials. Acta Psychiatr Scand 124(2):102–119. 10.1111/j.1600-0447.2011.01704.x [DOI] [PubMed] [Google Scholar]
- 37.Kamioka H, Tsutani K, Yamada M, Park H, Okuizumi H, Tsuruoka K et al. (2014) Effectiveness of music therapy: a summary of systematic reviews based on randomized controlled trials of music interventions. Patient Prefer Adherence 8:727. 10.2147/PPA.S61340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fancourt D, Ockelford A, Belai A (2014) The psychoneuroimmunological effects of music: a systematic review and a new model. Brain Behav Immun 36:15–26. 10.1016/j.bbi.2013.10.014 [DOI] [PubMed] [Google Scholar]
- 39.Biddle SJ, Asare M (2011) Physical activity and mental health in children and adolescents: a review of reviews. Br J Sports Med 45(11):886–895. 10.1136/bjsports-2011-090185 [DOI] [PubMed] [Google Scholar]
- 40.Ross A, Thomas S (2010) The health benefits of yoga and exercise: a review of comparison studies. J Altern Complement Med 16(1):3–12. 10.1089/acm.2009.0044 [DOI] [PubMed] [Google Scholar]
- 41.Itani O, Jike M, Watanabe N, Kaneita Y (2017) Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med 32:246–256. 10.1016/j.sleep.2016.08.006 [DOI] [PubMed] [Google Scholar]
- 42.Shochat T, Cohen-Zion M, Tzischinsky O (2014) Functional consequences of inadequate sleep in adolescents: a systematic review. Sleep Med Rev 18(1):75–87. 10.1016/j.smrv.2013.03.005 [DOI] [PubMed] [Google Scholar]
- 43.Slawson DL, Fitzgerald N, Morgan KT (2013) Position of the academy of nutrition and dietetics: the role of nutrition in health promotion and chronic disease prevention. J Acad Nutr Diet 113(7):972–979. 10.1016/j.jand.2013.05.005 [DOI] [PubMed] [Google Scholar]
- 44.Grosso G, Bella F, Godos J, Sciacca S, Del Rio D, Ray S et al. (2017) Possible role of diet in cancer: systematic review and multiple meta-analyses of dietary patterns, lifestyle factors, and cancer risk. Nutr Rev 75(6):405–419. 10.1093/nutrit/nux012 [DOI] [PubMed] [Google Scholar]
- 45.Gariepy G, Honkaniemi H, Quesnel-Vallee A (2016) Social support and protection from depression: systematic review of current findings in Western countries. Br J Psychiatry 209(4):284–293. 10.1192/bjp.bp.115.169094 [DOI] [PubMed] [Google Scholar]
- 46.Barth J, Schneider S, Von Känel R (2010) Lack of social support in the etiology and the prognosis of coronary heart disease: a systematic review and meta-analysis. Psychosom Med 72(3):229–238. 10.1097/PSY.0b013e3181d01611 [DOI] [PubMed] [Google Scholar]
- 47.Barry MM, Clarke AM, Jenkins R, Patel V (2013) A systematic review of the effectiveness of mental health promotion interventions for young people in low and middle income countries. BMC Public Health 13(1):835. 10.1186/1471-2458-13-835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pennant M, Davenport C, Bayliss S, Greenheld W, Marshall T, Hyde C (2010) Community programs for the prevention of cardiovascular disease: a systematic review. Am J Epidemiol 172(5):501–516. 10.1093/aje/kwq171 [DOI] [PubMed] [Google Scholar]
- 49.Gonzalez-Campoy J, St. Jeor S, Castorino K, Ebrahim A, Hurley D, Jovanovic L et al. (2013) Clinical practice guidelines for healthy eating for the prevention and treatment of metabolic and endocrine diseases in adults. Endocr Pract 19(5):875–887. 10.4158/EP13155.ESGL [DOI] [PubMed] [Google Scholar]
- 50.Solomon A, Mangialasche F, Richard E, Andrieu S, Bennett DA, Breteler M et al. (2014) Advances in the prevention of Alzheimer’s disease and dementia. J Intern Med 275(3):229–250. 10.1111/joim.12178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pak CCY (ed) (2012) Renal stone disease: pathogenesis, prevention, and treatment, vol 5. Springer, Cham [Google Scholar]
- 52.Feldman AS, He Y, Moore ML, Hershenson MB, Hartert TV (2015) Toward primary prevention of asthma. Reviewing the evidence for early-life respiratory viral infections as modifiable risk factors to prevent childhood asthma. Am J Respir Crit Care Med 191(1):34–44. 10.1164/rccm.201405-0901PP [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Swift PJ, Dewey L, Ivanova MY, Foret D, Flanders E, Plasha L et al. (2018) Incorporating family-based care into outpatient child/adolescent psychiatry: initial findings implementing the Vermont Family Based Approach. J Am Acad Child Adolesc Psychiatry 57(10S):S265. 10.1016/j.jaac.2018.09.413 [DOI] [Google Scholar]
- 54.Sung SC, Tng HY, Wong ZJ, Tan YL, Tan YR, Choong SF et al. (2019) Assessing for mood and anxiety disorders in parents of clinically-referred children: laying the foundation for a family-based approach to mental health in Singapore. Ann Acad Med Singap 48:55–62 [PubMed] [Google Scholar]
- 55.McGinnis JM, Williams-Russo P, Knickman JR (2002) The case for more active policy attention to health promotion. Health Aff 21(2):78–93. 10.1377/hlthaff.21.2.78 [DOI] [PubMed] [Google Scholar]
- 56.Frieden TR (2010) A framework for public health action: the health impact pyramid. Am J Public Health 100(4):590–595. 10.2105/AJPH.2009.185652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.van de Vijver S, Oti S, Addo J, de Graft-Atkins A, Agyemang C (2012) Review of community-based interventions for prevention of cardiovascular diseases in low-and middle-income countries. Ethn Health 17(6):651–676. 10.1080/13557858.2012.754409 [DOI] [PubMed] [Google Scholar]
- 58.Miller WR, Rollnick S (2012) Motivational interviewing: helping people change. Guilford, New York [Google Scholar]
- 59.Stanger SB, Ivanova MY, Hall AY, Shaw JS, Slunecka F, Kapaska D et al. (2016) School-based family wellness: a gateway to service utilization. Vermont Center for Children, Youth, and Families; Technical Report [Google Scholar]
- 60.Buckingham S, Paiva-Salisbury M, Ivanova M, McGinnis E, Hall A, Shaw JS, et al. (2017) Feasibility, acceptability, and efficacy of the Vermont Family Based Approach in a school setting: the Addison Central Supervisory Union family wellness program. Vermont Center for Children, Youth, and Families; 2017. Technical Report [Google Scholar]
- 61.Achenbach TM, Rescorla L (2000) Manual for the ASEBA Pre-school Forms & Profiles. Research Center for Children, Youth, and Families, Burlington [Google Scholar]
- 62.Campo JV, Geist R, Kolko DJ (2018) Integration of pediatric behavioral health services in primary care: improving access and outcomes with collaborative care. Can J Psychiatry 63(7):432–438. 10.1177/0706743717751668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Asarnow JR, Rozenman M, Wiblin J, Zeltzer L (2015) Integrated medical-behavioral care compared with usual primary care for child and adolescent behavioral health: a meta-analysis. JAMA Pediatr 169(10):929–937. 10.1001/jamapediatrics.2015.1141 [DOI] [PubMed] [Google Scholar]
- 64.Ivanova MY, Hall A, Weinberger S, Crockett P, Foret D, McGinnis E et al. (2019) RCT of the Vermont Family Based Approach (VFBA) in primary care pediatrics: engagement with health and support services. J Am Acad Child Adolesc Psychiatry 58(10S):S220. 10.1016/j.jaac.2019.08.242 [DOI] [Google Scholar]
- 65.United States Census Bureau (2019) QuickFacts: Burlington city, Vermont. United States Census Bureau, Suitland [Google Scholar]
- 66.Moos BS, Moos RH (2009) Family Environment Scale manual: development, applications, research, 3rd edn. Mind Garden, Palo Alto [Google Scholar]
- 67.Dunst CJ, Leet HE (1987) Measuring the adequacy of resources in households with young children. Child Care Health Dev 13:111–125 [DOI] [PubMed] [Google Scholar]
- 68.Israel AC, Roderick HA, Ivanova MY (2002) A measure of the Stability of Activities in a Family Environment. J Psychopathol Behav Assess 24:85–95 [Google Scholar]
- 69.McMahon RJ, Forehand RL (2005) Helping the noncompliant child: family-based treatment for oppositional behavior, 2nd edn. Guilford, New York [Google Scholar]
- 70.ACT.md. Version 1.0. (2012). Accessed from https://www.activatecare.com.
- 71.Achenbach TM (2002) General description of 1975 Hollingshead occupational categories updated to 2001. Research Center for Children, Youth, and Families, Burlington [Google Scholar]
- 72.Campbell I (2007) Chi-squared and Fisher-Irwin tests of twoby-two tables with small sample recommendations. Stat Med 26(19):3661–3675. 10.1002/sim.2832 [DOI] [PubMed] [Google Scholar]
- 73.Achenbach TM, Rescorla L (2001) Manual for the ASEBA schoolage forms & profiles. Research Center for Children, Youth, and Families, Burlington [Google Scholar]
- 74.Ivanova MY, Achenbach TM, Rescorla LA, Guo J, Althoff RR, Kan K et al. (2019) Testing syndromes of psychopathology in parent and youth ratings across societies. J Clin Child Adolesc Psychol 48(4):596–609. 10.1080/15374416.2017.1405352 [DOI] [PubMed] [Google Scholar]
- 75.Ivanova MY, Achenbach TM, Rescorla LA, Harder VS, Ang RP, Bilenberg N et al. (2010) Preschool psychopathology reported by parents in 23 societies: testing the seven-syndrome model of the child behavior checklist for ages 1.5–5. J Am Acad Child Adolesc Psychiatry 49(12):1215–1224. 10.1016/j.jaac.2010.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Franz L, Angold A, Copeland W, Costello EJ, Towe-Goodman N, Egger H (2013) Preschool anxiety disorders in pediatric primary care: prevalence and comorbidity. J Am Acad Child Adolesc Psychiatry 52(12):1294–1303. 10.1016/jjaac.2013.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Flynn AB, Fothergill KE, Wilcox HC, Coleclough E, Horwitz R, Ruble A et al. (2015) Primary care interventions to prevent or treat traumatic stress in childhood: a systematic review. Acad Pediatr 15(5):480–492. 10.1016/j.acap.2015.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Achenbach TM, Rescorla L (2003) Manual for the ASEBA adult forms & profiles. Research Center for Children, Youth, and Families, Burlington [Google Scholar]
- 79.Ivanova MY, Achenbach TM, Rescorla LA, Tumer LV, AhmetiPronaj A, Au A et al. (2015) Syndromes of self-reported psychopathology for ages 18–59 in 29 societies. J Psychopathol Behav Assess 37(2):171–183. 10.1007/s10862-014-9448-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ware JE Jr, Sherbourne CD (1992) The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual framework and item selection. Med Care 30(6):473–483. 10.1097/00005650-199206000-00002 [DOI] [PubMed] [Google Scholar]
- 81.McHorney CA, Ware JE Jr, Lu JR, Sherbourne CD (1994) The MOS 36-Item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care 32(1):40–66. 10.1097/00005650-199401000-00004 [DOI] [PubMed] [Google Scholar]
- 82.McHorney CA, Ware JE Jr, Raczek AE (1993) The MOS 36-item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 31(3):247–263. 10.1097/00005650-199303000-00006 [DOI] [PubMed] [Google Scholar]
- 83.Hardin JW (2005) Generalized estimating equations (GEE). In: Everitt BS, Howell DC (eds) Encyclopedia of statistics in behavioral science. Wiley, Hoboken [Google Scholar]
- 84.Hubbard AE, Ahern J, Fleischer NL, Van der Laan M, Lippman SA, Jewell N et al. (2010) To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology 21(4):467–474. 10.1097/EDE.0b013e3181caeb90 [DOI] [PubMed] [Google Scholar]
- 85.Zhang H, Yu Q, Feng C, Gunzler DD, Wu P, Tu XM (2012) A new look at the difference between the GEE and the GLMM when modeling longitudinal count responses. J Appl Stat 39(9):2067–2079. 10.1080/02664763.2012.700452 [DOI] [Google Scholar]
- 86.Nolen-Hoeksema S (2012) Emotion regulation and psychopathology: the role of gender. Annu Rev Clin Psychol 8:161–187. 10.1146/annurev-clinpsy-032511-143109 [DOI] [PubMed] [Google Scholar]
- 87.Kessler RC, Birnbaum HG, Shahly V, Bromet E, Hwang I, McLaughlin KA et al. (2010) Age differences in the prevalence and co-morbidity of DSM-IV major depressive episodes: results from the WHO world mental health survey initiative. Depress Anxiety 27(4):351–364. 10.1002/da.20634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Costello EJ, Copeland W, Angold A (2011) Trends in psychopathology across the adolescent years: what changes when children become adolescents, and when adolescents become adults? J Child Psychol Psychiatry 52(10):1015–1025. 10.1111/j.1469-7610.2011.02446.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kroenke K, Unutzer J (2017) Closing the false divide: sustainable approaches to integrating mental health services into primary care. J Gen Intern Med 32(4):404–410. 10.1007/s11606-016-3967-926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Macchi CR, Kessler R, Auxier A et al. (2016) The practice integration profile: rationale, development, method, and research. Fam Syst Health 34(4):334–341. 10.1037/fsh0000235 [DOI] [PubMed] [Google Scholar]
- 91.Morris S (2008) Estimating effect sizes from pretest-posttest-control group designs. Organ Res Methods 11(2):364–386. 10.1177/1094428106291059 [DOI] [Google Scholar]
- 92.Colon-Rentas O, Gordon L, Montejo LD, Reitsma P, Sánchez FA, Song B (2006) The impact of the sleeper effect and relapse on the dynamics of cigarette smoking among adolescents. Mathematical and Theoretical Biology Institute; Technical Report. MTBI-03–04M [Google Scholar]
- 93.Sklad M, Diekstra R, Ritter MD, Ben J, Gravesteijn C (2012) Effectiveness of school-based universal social, emotional, and behavioral programs: do they enhance students’ development in the area of skill, behavior, and adjustment? Psychol Sch 49(9):892–909. 10.1002/pits.21641 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.