Abstract
Background
Human mobility changed in unprecedented ways during the SARS-CoV-2 pandemic. In March and April 2020, when lockdowns and large travel restrictions began in most countries, global air-travel almost entirely halted (92% decrease in commercial global air travel in the months between February and April 2020). Initial recovery in global air travel started around July 2020 and subsequently nearly tripled between May and July 2021. Here, we aim to establish a preliminary link between global mobility patterns and the synchrony of SARS-CoV-2 epidemic waves across the world.
Methods
We compare epidemic peaks and human global mobility in two time periods: November 2020 to February 2021 (when just over 70 million passengers travelled) and November 2021 to February 2022 (when more than 200 million passengers travelled). We calculate the time interval during which continental epidemic peaks occurred for both of these time periods, and we calculate the pairwise correlations of epidemic waves between all pairs of countries for the same time periods.
Results
We find that as air travel increases at the end of 2021, epidemic peaks around the world are more synchronous with one another, both globally and regionally. Continental epidemic peaks occur globally within a 20 day interval at the end of 2021 compared with 73 days at the end of 2020, and epidemic waves globally are more correlated with one another at the end of 2021.
Conclusions
This suggests that the rebound in human mobility dictates the synchrony of global and regional epidemic waves. In line with theoretical work, we show that in a more connected world, epidemic dynamics are more synchronized.
Keywords: Mobility, epidemic synchrony, travel, SARS-CoV-2
Background
Globally, human mobility shifted in unprecedented ways during the SARS-CoV-2 pandemic.1 Initially, when rapid spread of a novel respiratory pathogen in China began to be recognized, travel bans and restrictions within China and against select countries were implemented in a bid to limit the virus’ movement out of the fast-evolving epicentres. Ultimately, as the virus was introduced and spread within countries worldwide, uncertainty over its severity in the absence of effective and licensed treatment or vaccines prompted nations to close their borders and restrict the movement of their citizens locally through lockdowns.2 Periods of local lockdowns and international travel restrictions persisted in cycles over the first 2 years of the pandemic as governments worldwide responded to successive waves of infections.
Undoubtedly, these important shifts in human mobility influenced the way in which epidemic waves unfolded globally. Various studies reporting on the relationship between human mobility and SARS-CoV-2 epidemiology have focused on the size of epidemic waves and rates of transmission, often related to lockdowns. For instance, early in the pandemic, a clear effect of human mobility and related control measures were observed within China.3,4 As the virus propagated around the world, similar effects of decreased prevalence linked to reduced mobility, or case resurgences associated with increased mobility were reported in several countries and cities at several periods during the pandemic.5–9 Mobility patterns have also been used to reconstruct the invasion dynamics of emerging variants of SARS-CoV-2, for example where the dispersal of the B.1.1.7 lineages in the UK was shown to be highly dictated by connectivity with the town of its first detection.10 However, only a few studies have described the synchrony of epidemic waves related to human mobility patterns, and available reports have been mostly with a regional focus. For example, early restrictions in Wuhan were associated with a lag in epidemic propagation to other Chinese provinces,3,4 and, conversely, highly connected areas in Europe experienced correlated epidemics during the first and second wave of 2020.11,12 In this study, we aim to establish a preliminary link between shifting mobility patterns and the synchrony of SARS-CoV-2 epidemic waves on a global scale.
Methods
Data sources
SARS-CoV-2 reported cases
We analysed trends in daily reported numbers of cases of SARS-CoV-2 globally for the periods of November 2020 to February 2021, and November 2021 to February 2022 from publicly released data provided by the Our World in Data repository (https://github.com/owid/covid-19-data/tree/master/public/data) for continents and for individual countries (OWID).
Effective reproductive (Re) number estimates
The estimations for effective daily Re of SARS-CoV-2 in all countries worldwide were obtained from the COVID-19-Re data repository (https://github.com/covid-19-Re/dailyRe-Data)13 for the described time periods. The effective Re describes the average number of secondary infections caused by an infected individual. As described previously,13 the relevant method of calculation of Re builds upon another method developed by Cori et al.,14 accessible through the EpiEstim R package. Instead of using a time series of infection incidence, the relevant method infers the infection incidence time series based on secondary sources of information, such as COVID-19 confirmed case data, hospital admissions and deaths. This was considered in combination with two other sets of time variables: (i) the duration of SARS-CoV-2 incubation period and (ii) the time delays between onset of symptoms and a positive test, a hospital admission or the death of a patient. The relevant method infers infection time series from the stated observed incidence data by deconvolution.15,16
Air travel passenger volumes
We evaluated travel data generated from the International Air Transport Association (IATA) to quantify passenger volumes originating from international airports during the study period. IATA data accounts for ~90% of passenger travel itineraries on commercial flights, excluding transportation via unscheduled charter flights (the remainder is modelled using market intelligence).
Epidemic peak timing
The timing of epidemic peaks for each continent in the two time periods being studied was computed from the time-varying daily reported cases (7-day moving average) per continent using a custom script that scans for local maxima using a rolling window of 100 days. The time interval during which continental epidemic peaks occurred was calculated as the number of days between the peak date of the earliest continental peak to the latest.
Epidemic correlations
We calculated pairwise correlations of time-varying daily reported cases for all pairs of countries globally where data were available (Source: Our World in Data), for the two time periods being studied. Both Pearson and Spearman methods were used to compute the correlations. For each time period, an average and standard deviation of all pairwise correlations were calculated and displayed. This analysis was repeated with time-varying Re data for each country.
Results
In March and April 2020, when lockdowns and large travel restrictions began in most countries, global air-travel initially halved, falling from 100 million in February 2020 to around 50 million in March 2020 and almost entirely halted in the months after (92% decrease in global travel in the months between February and April 2020). Initial recovery in global travel started around July 2020 to around 20 million passengers and remained stable for the next 10 months. Beginning May 2021, and over the next 3 months, global air travel nearly tripled, reaching a new equilibrium of roughly 60 million monthly air travel passengers (Figure 1a). This happened as countries worldwide relaxed most mobility-related mitigation measures after mass vaccination campaigns helped reduce the public health threat caused by COVID-19.
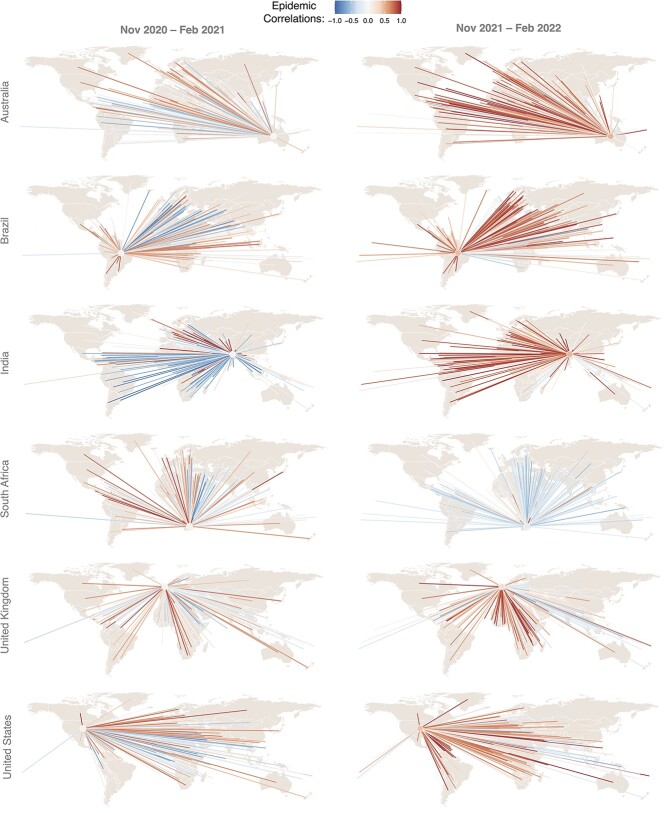
Figure 1.
(A) Total monthly air passenger volumes from February 2020 to March 2022. (B) Daily reported cases (7-day rolling average; source: Our World in Data) through time per continent with periods analysed in this work marked in grey. Continental peaks in daily reported cases are marked with dashed lines, along with the number of days from the first and the last continental peaks in each time period. (C) Global epidemic wave correlation indices for the two time periods of interest (mean and standard deviations shown). Wave correlations are calculated by computing pairwise correlations (Pearson and Spearman) of the daily case counts between pairs of all countries with available data in each time period, and all pairwise correlations are averaged out for each time period.
As a proxy for global wave synchrony, we analysed the time interval between continental epidemic peaks and estimated the degree of correlations of epidemic waves of individual countries, using both time-varying numbers of reported cases and estimates of the effective reproduction (Re) number, during two time periods: November 2020 to February 2021 (when just over 70 million passengers travelled), and November 2021 to February 2022 (when more than 200 million passengers travelled). We observe that there were more than 70 days between epidemic peaks during the first time period from November 2020 to February 2021 (Figure 1b). One year later, in November 2021–February 2022, continental peaks in daily reported cases occurred within only 20 days of one another (Figure 1b). We then calculated pairwise correlations of time-varying daily reported cases for all pairs of countries globally where data were available (Source: Our World in Data), for each of these time periods. A high correlation value between two countries could be interpreted as a higher synchrony between their epidemic waves. After averaging out all the pairwise correlations for the two time periods, we find that while between November 2020 and February 2021, global epidemic waves show no correlation (mean of all Pearson correlations = 0.01, sd = 0.47; mean of all Spearman correlations = 0.03, sd = 0.48), they appear to be positively correlated between November 2021 and February 2022 (mean of all Pearson correlations = 0.29, sd = 0.43; mean of all Spearman correlations = 0.33, sd = 0.42) (Figure 1c). While not all countries relaxed their entry requirements in the second time period analysed here, our data suggest that the tripling in global travel volume led to overall more synchronized epidemic patterns worldwide. Stratifying the pairwise country correlations by region, we see that on average, each continent also showed higher pairwise correlations both between countries of the same continent and with countries in the rest of the world during the second time frame, demonstrating that the patterns of more synchronous epidemic were not concentrated to any particular part of the world (Appendix Figure 1). Some specific subregions still show more disconnected epidemic patterns in the second time frame (for example, some parts of Africa, southeast Asia and Oceania), which could point towards places with remaining entry restrictions that can delay seedings events of a new wave, or local epidemic-control measures different to the rest of the world that can influence the rate of epidemic expansion. Yet, the overall trend suggests that the rebound in human mobility dictates the synchrony of global and regional epidemic waves (a pattern observed for other infectious diseases). Due to potential inconsistencies in reporting, we repeated the analysis with estimates of the time varying reproduction number (Re) and found similar trends (Appendix Figures 2 and 3). As air travel increases at the end of 2021, increasing incidence in one part of the world meant that other parts of the world experienced epidemic waves soon thereafter (within less than 1 month). Stated more simply, in a more connected world, epidemic dynamics are more coordinated.
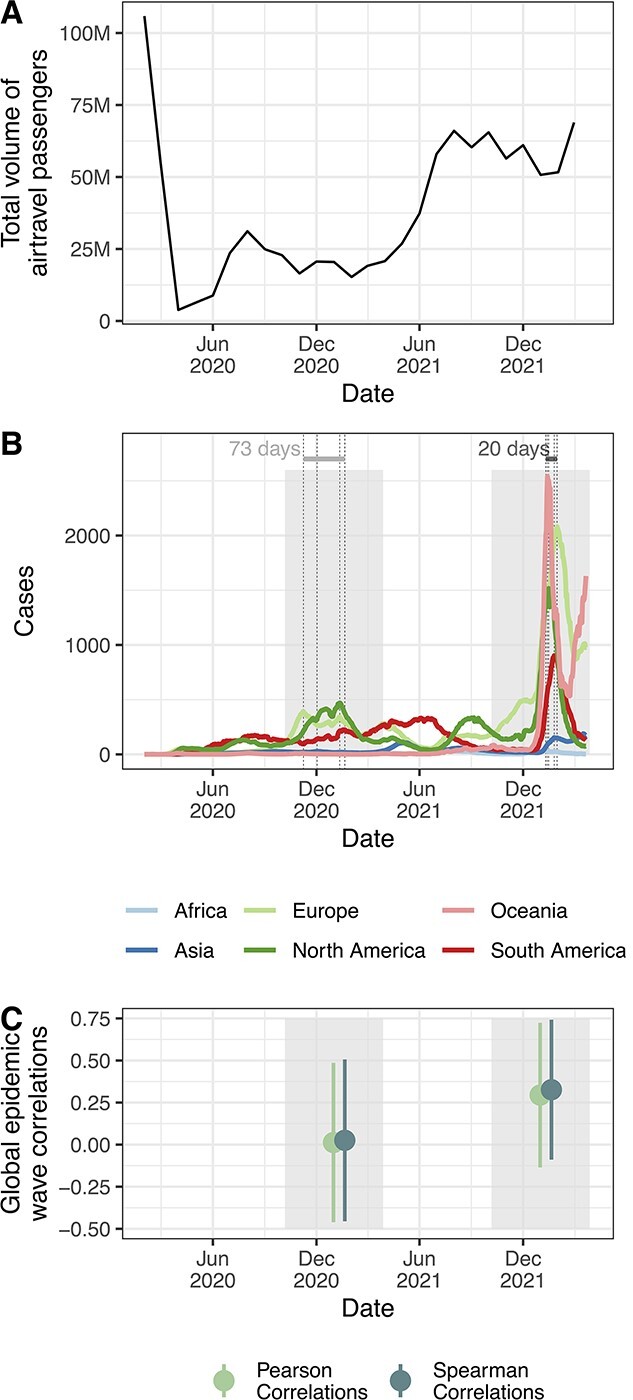
This trend is also observed when considering individual countries. Figure 2 depicts the levels of epidemic correlations between South Africa, the United Kingdom (UK), India, Brazil, the United States (US) and Australia, and the rest of the world. Bright red lines connecting the specified countries to another denote very synchronous epidemics between the two (positive correlations), while bright blue lines denote very asynchronous epidemics (negative correlations). While the UK appears to have had relatively highly correlating epidemic waves with other countries already in November 2020–February 2021, Brazil, the US, India and Australia quite clearly experienced more highly coordinated epidemics with the rest of the world between November 2021 and February 2022 (Figure 2). However, a striking pattern emerges in the case of South Africa. While wave synchrony generally increases globally in the second time frame, South Africa experiences a marked decrease in the synchrony of its epidemic with other countries over the second window in November 2021–February 2022 compared with the year before (Figure 2). Remembering that this was the time of Omicron discovery and expansion in South Africa,17 this provides a stark nod to all the rigorous travel bans imposed on South Africa and other countries in Southern Africa during this time.18 This, in fact, contextualizes this lower synchrony quite pertinently. While the Omicron variant still expanded globally during this general time frame, its spread was primarily driven by exportations from secondary hot spots (e.g. the United Kingdom), a trend also visible for the emergence of Delta.19 This is also what appears to have happened at the beginning of the pandemic, when heavy travel restrictions meant that epidemics were less synchronized, but eventually almost all countries experienced large epidemics.20,21 These trends could be further investigated using phylodynamic approaches.
Figure 2.
Epidemic wave correlations between specified countries, one per continent and all other countries globally for November 2020 to February 2021 and November 2021 to February 2022. Bright red lines connecting the specified countries to another denote very synchronous epidemics between the two (positive correlations), while bright blue lines denote very asynchronous epidemics (negative correlations). Mean correlations for the specified country are also denoted with a circle coloured by the mean of all pairwise correlations for that country.
Discussion
From influenza epidemic dynamics, it is known that synchrony of epidemic waves is influenced by population size, geographical distance, climatic conditions and human movement.22 While population size seems to dictate local synchrony of waves within countries in some instances,23,24 suggesting hierarchical spread between populous regions, geographical distances seem to play a bigger role in others, pointing to greater contributions of land commutes rather than air travel.25 Internationally, however, influenza viral lineage spread between countries has been shown to be heavily influenced by passenger air travel.26 The drastic changes in global air travel during the SARS-CoV-2 pandemic are unprecedented and provide a unique framework to model the contribution of human mobility to global pathogen dissemination and lets us assess its contribution to global case incidence.
The interpretation of human mobility into peak timing prediction is, of course, just one piece of the puzzle. Two intertwining aspects in particular have the potential to complicate the matter. First, there is the consideration of the genomic and antigenic characteristics of the circulating variant(s), particularly whether what variant is circulating is novel (causing a wave of infections for the first time) or existing (having already caused a wave of infections). Then, to add to the mix would be the timing and/or magnitude of the previous wave. As we know, there is a certain level of protective immunity in the population after a wave of infections. The degree of that protection, and its duration depends on the magnitude of the previous wave, and the variant which caused it, in addition to levels of vaccine-induced immunity in the population. This may in fact influence the timing and magnitude of upcoming epidemic waves in ways not related to human mobility. Predictions relying too heavily on human mobility, therefore, could lead to confounding conclusions in some instances. We can consider here the example of the Omicron epidemic in South Africa. The country experienced a very large BA.1 wave, much like the rest of the world, but did not see a significant BA.2 wave, unlike the rest of the world. It turns out that the antigenic patterns of population immunity in South Africa, brought by extensive Delta and BA.1 waves, combined with the timing of growth of BA.2 in the country (not enough time to wane immunity since the last wave) served a protective purpose on the population.27 Here, interpretations of human mobility alone would have not provided an accurate reconstruction of microscale dynamics of SARS-CoV-2. Lastly, seasonality and associated behaviours could be further factors to have influenced global epidemic synchrony independent of human mobility.
Nevertheless, it is worthwhile for epidemiologists to dwell on understanding the role of human mobility in shaping past and future epidemic waves globally. As air travel rebounds to pre-pandemic levels, potential emerging variants and increasing incidence that they fuel will affect the whole world more simultaneously, posing a potentially major threat to the global economy. This is not restricted to SARS-CoV-2. New pathogens will emerge or known ones will re-emerge and become new concerns. As that happens, and as the world becomes more and more connected, untangling the specificities of the interplay between mobility and the synchrony of global epidemics will become increasingly important to plan for better and more coordinated public health responses.
Funding
KRISP and CERI is supported in part by grants from the Rockefeller Foundation (HTH 017), Abbott Pandemic Defense Coalition (APDC), the African Society for Laboratory Medicine, the National Institute of Health USA (U01 AI151698) for the United World Antivirus Research Network (UWARN) and the INFORM Africa project through IHVN (U54 TW012041), H3BioNet Africa (Grant # 2020 HTH 062), the South African Department of Science and Innovation (SA DSI) and the South African Medical Research Council (SAMRC) under the BRICS JAF #2020/049 and the World Bank (TF0B8412). M.U.G.K. acknowledges support from a Branco Weiss Fellowship, Reuben College Oxford, Google.org, the Foreign, Commonwealth and Development Office and Wellcome (225288/Z/22/Z), The Rockefeller Foundation, and from the European Union Horizon 2020 project MOOD (grant agreement number 874850), and acknowledge support from the Oxford Martin School.
Conflict of interest
K.K. is the founder of BlueDot, a social enterprise that develops digital technologies for public health. C.H. is employed at BlueDot. H.T., T.d.O and M.U.G.K. have no conflicts of interest to declare.
Data availability statement
SARS-CoV-2 reported cases and Effective reproductive (Re) number estimates used in this study are openly available through Our World in Data repository (https://github.com/owid/covid-19-data/tree/master/public/data) and from the COVID-19-Re data repository (https://github.com/covid-19-Re/dailyRe-Data) respectively. Air travel passenger volumes are available under licensing agreement and with permission from the authors.
Supplementary Material
Contributor Information
Houriiyah Tegally, KwaZulu-Natal Research Innovation and Sequencing Platform (KRISP), Nelson R. Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa; Centre for Epidemic Response and Innovation (CERI), School of Data Science and Computational Thinking, Stellenbosch University, Stellenbosch, South Africa.
Kamran Khan, BlueDot, Toronto, Canada; Department of Medicine, Division of Infectious Diseases, University of Toronto, Toronto, Canada.
Carmen Huber, BlueDot, Toronto, Canada.
Tulio de Oliveira, KwaZulu-Natal Research Innovation and Sequencing Platform (KRISP), Nelson R. Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa; Centre for Epidemic Response and Innovation (CERI), School of Data Science and Computational Thinking, Stellenbosch University, Stellenbosch, South Africa; Centre for the AIDS Programme of Research in South Africa (CAPRISA), Durban, South Africa; Department of Global Health, University of Washington, Seattle, WA, USA.
Moritz U G Kraemer, Department of Biology, University of Oxford, Oxford, United Kingdom; Pandemic Sciences Institute, University of Oxford, Oxford, United Kingdom.
References
- 1. Schlosser F, Maier BF, Jack O, Hinrichs D, Zachariae A, Brockmann D. COVID-19 lockdown induces disease-mitigating structural changes in mobility networks. Proc Natl Acad Sci U S A 2020; 117:32883–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Flaxman S, Mishra S, Gandy A et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature 2020; 584:257–61. [DOI] [PubMed] [Google Scholar]
- 3. Kucharski AJ, Russell TW, Diamond C et al. Early dynamics of transmission and control of COVID-19: a mathematical modelling study. Lancet Infect Dis 2020; 20:553–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kraemer MUG, Yang CH, Gutierrez B et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science 2020; 368:493–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kissler SM, Kishore N, Prabhu M et al. Reductions in commuting mobility correlate with geographic differences in SARS-CoV-2 prevalence in New York City. Nat Commun 2020; 11:4674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kishore N, Kahn R, Martinez PP et al. Lockdowns result in changes in human mobility which may impact the epidemiologic dynamics of SARS-CoV-2. Sci Rep 2021; 11:6995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mehta SH, Clipman SJ, Wesolowski A, Solomon SS. Holiday gatherings, mobility and SARS-CoV-2 transmission: results from 10 US states following Thanksgiving. Sci Rep 2021; 11:17328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lemey P, Ruktanonchai N, Hong SL et al. Untangling introductions and persistence in COVID-19 resurgence in Europe. Nature 2021;595:713–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lison A, Persson J, Banholzer N, Feuerriegel S. Estimating the effect of mobility on SARS-CoV-2 transmission during the first and second wave of the COVID-19 epidemic, Switzerland, March to December 2020. Euro Surveill 2022; 27:2100374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kraemer MUG, Hill V, Ruis C et al. Spatiotemporal invasion dynamics of SARS-CoV-2 lineage B.1.1.7 emergence. Science 2021; 373:889–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ruktanonchai NW, Floyd JR, Lai S et al. Assessing the impact of coordinated COVID-19 exit strategies across Europe. Science 2020; 369:1465–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lemey P, Ruktanonchai N, Hong SL et al. Untangling introductions and persistence in COVID-19 resurgence in Europe. Nature 2021; 595:713–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Huisman JS, Scire J, Angst DC et al. Estimation and worldwide monitoring of the effective reproductive number of SARS-CoV-2. Elife 2022; 11:e71345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cori A, Ferguson NM, Fraser C, Cauchemez S. A new framework and software to estimate time-varying reproduction numbers during epidemics. Am J Epidemiol 2013; 178:1505–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Goldstein E, Dushoff J, Ma J et al. Reconstructing influenza incidence by deconvolution of daily mortality time series. Proc Natl Acad Sci U S A 2009; 106:21825–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gostic KM, McGough L, Baskerville EB et al. Practical considerations for measuring the effective reproductive number. Rt PLoS Comput Biol 2020; 16:e1008409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Viana R, Moyo S, Amoako DG et al. Rapid epidemic expansion of the SARS-CoV-2 Omicron variant in southern Africa. Nature 2022; 603:679–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mendelson M, Venter F, Moshabela M et al. The political theatre of the UK’s travel ban on South Africa. Lancet 2021; 398:2211–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. McCrone JT, Hill V, Bajaj S et al. Context-specific emergence and growth of the SARS-CoV-2 Delta variant. Nature 2022; 610:154–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chinazzi M, Davis JT, Ajelli M et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science 2020; 368:395–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Russell TW, Wu JT, Clifford S et al. Effect of internationally imported cases on internal spread of COVID-19: a mathematical modelling study. Lancet Public Health 2021; 6:e12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Viboud C, Bjørnstad ON, Smith DL et al. Synchrony, waves, and spatial hierarchies in the spread of influenza. Science 2006; 312:447–51. [DOI] [PubMed] [Google Scholar]
- 23. Geoghegan JL, Saavedra AF, Duchêne S et al. Continental synchronicity of human influenza virus epidemics despite climatic variation. PLoS Pathog 2018; 14:e1006780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Morris SE, Freiesleben de Blasio B, Viboud C et al. Analysis of multi-level spatial data reveals strong synchrony in seasonal influenza epidemics across Norway, Sweden, and Denmark. PLoS ONE 2018; 13:e0197519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Charu V, Zeger S, Gog J et al. Human mobility and the spatial transmission of influenza in the United States. PLoS Comput Biol 2017; 13:e1005382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lemey P, Rambaut A, Bedford T et al. Unifying viral genetics and human transportation data to predict the global transmission dynamics of human influenza H3N2. PLoS Pathog 2014; 10:e1003932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tegally H, Moir M, Everatt J et al. Emergence of SARS-CoV-2 Omicron lineages BA.4 and BA.5 in South Africa. Nat Med 2022;28:1785–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
SARS-CoV-2 reported cases and Effective reproductive (Re) number estimates used in this study are openly available through Our World in Data repository (https://github.com/owid/covid-19-data/tree/master/public/data) and from the COVID-19-Re data repository (https://github.com/covid-19-Re/dailyRe-Data) respectively. Air travel passenger volumes are available under licensing agreement and with permission from the authors.