Abstract
Background
The inclusion of patient-reported outcome measures (PROMs) serves to better quantify aspects of patient outcomes missed with objective measures, including radiographic indices and physical examination findings. We hypothesize that PROMs are inconsistently and heterogeneously captured in the treatment of distal radius fractures.
Methods
We performed a systematic review following Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines of all level I and II randomized controlled trials (RCTs) of distal radius fracture treatment of any modality for those older than 50 years of age from January 2008 to January 2018. A total of 23 studies were included in the final analysis. The metrics used by each study to assess outcomes were collected, compared, and described.
Results
Physical examination findings and radiographic measures were reported in 70% and 74% of studies, respectively. Patient-reported outcomes measures were used to assess outcomes in 74% of studies. Only the Disabilities of the Arm, Shoulder, and Hand was used in greater than half of the studies (57%). Pain scores were assessed in 39% of studies and complications in only 26%.
Conclusions
There is substantial heterogeneity and lack of standardization in the collection of both objective outcome measures and PROMs in level I and II RCTs for the treatment of distal radius fractures. The ability to compare between studies or aggregate data among studies is therefore limited. Radiographic and physical examination findings remain frequently reported despite known limitations of these metrics. The routine collection of PROMs after the treatment of distal radius fractures can ensure care is directed toward improving what is most important to patients.
Keywords: distal radius, systematic review, patient-reported outcome measures, randomized controlled trial
Introduction
Distal radius fractures are one of the most common musculoskeletal injuries in the United States, with more than 600 000 cases reported annually.1,2 This poses a significant burden on the health care system. Numerous randomized controlled trials (RCTs) have investigated treatment modalities for distal radius fractures, particularly in patients aged 50 years or older. The outcomes used to determine treatment efficacy in these studies vary widely and include radiographic findings, wrist and forearm range of motion, complications, pain, and patient-reported outcome measures (PROMs).3-5 Given the heterogeneity and lack of standardized outcome reporting among studies, meaningfully comparing studies remains challenging.6,7
Historically, radiographic findings have been frequently used as primary outcome measures, despite multiple studies showing that radiographic outcomes often poorly correlate with function.8,9 Arora et al 3 reported on 73 patients randomized to volar locking plate fixation versus nonoperative management, and although radiographic parameters were significantly superior in the surgical group, there were no differences in pain scores, Patient-Rated Wrist Evaluation (PRWE), or Disabilities of the Arm, Shoulder, and Hand (DASH) scores. Anzarut et al 8 reported on 74 patients aged 55 years and older who underwent closed treatment for distal radius fractures and found that an acceptable radiographic reduction was not associated with subsequent upper extremity disability or decreased satisfaction compared with those with a suboptimal reduction. Furthermore, radiographic metrics do not capture pain or the magnitude of associated limitations, such as subsequent disability. A patient with excellent radiographic parameters may still not be able to return to his or her desired activities for a number of reasons, and as a result may ultimately deem the result poor. By omitting these measures when reporting outcomes, it is difficult for RCTs to be fully comprehensive in their assessment of patient outcomes.
Objective clinical examination findings are also commonly reported outcomes, and there is wide agreement in the literature regarding the importance of specific metrics.10,11 Although wrist range of motion and grip strength have been shown to be strongly associated with satisfaction, they have also been shown to account for only a portion of variation seen in PROM scores, meaning that a significant component of patient satisfaction and reported function is not associated with these measurable examination findings.12,13 Patient-reported outcome measures for upper extremity injury, including the Michigan Hand Questionnaire, the DASH questionnaire, and the PRWE, aim to capture these other variables and have been shown to be validated measures in evaluating outcomes for distal radius fracture.14-16 If radiographic and clinical metrics only convey a part of the patient story, other subjective measures like PROMs should be included if the goal is to be comprehensive in the assessment of patient outcomes, with the understanding that PROMs have their own limitations and may struggle to fully elucidate subtle differences.
Patient-reported outcome measures are often not routinely assessed outside of academic medicine, as there are concerns that collection may disrupt clinic workflow, be labor-intensive, and cause financial burdens. 17 In a systematic review of 109 studies on distal humerus fracture outcomes, Zarezadeh et al 18 reported that 39% of studies reported 1 PROM or none at all, with a range of 20 different PROMs being reported across the studies. We hypothesized that there is heterogeneity of PROM reporting in distal radius literature, whereas reporting of radiographic and physical examination measures is more standardized.
Methods
Identification of Relevant Literature
Using methodology established from the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA), we searched PubMed/Medline, Embase, CINAHL, and Web of Science for English-language, level I or II RCTs from January 2007 to April 2018 for distal radius fractures and treatments in adults (search criteria in Supplemental Appendix I). The search criteria were reviewed and revised by a board-certified hand surgeon to ensure completeness of search terms.
Abstract and Full Text Selection
A board-certified orthopedic hand surgeon and 2 research assistants initially screened all RCT article titles for relevance. If an abstract confirmed that the article focused on distal radius fracture treatment, the full text of the article was reviewed. We did not discriminate between studies investigating operative or nonoperative measures or exclude studies based on the type of distal radius fracture treated. We attempted to capture all RCT studies addressing any component of the treatment of all forms of distal radius fractures. Discrepancies between reviewers were resolved by discussion until consensus was achieved. Based on an initial screening of the literature, the low-end age cutoff for inclusion in some studies assessing distal radius fracturs in the “elderly” was 50 years. In an effort to have our systematic review reflect the literature, we decided to use the same age threshold for this study,
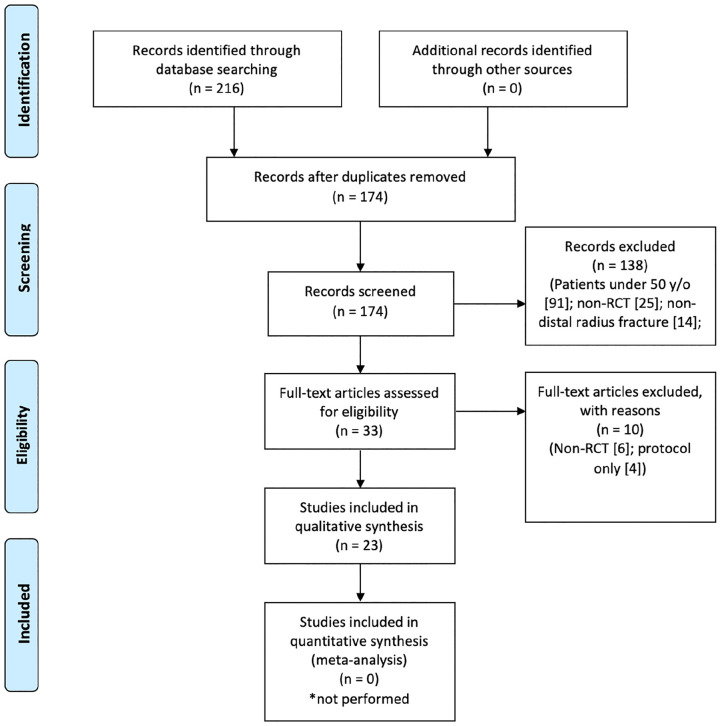
The PRISMA flowchart outlines our screening process (Figure 1). We assessed the full texts of 33 studies using a data abstraction tool. 19 Ten studies were excluded for the following reasons: 6 were found to not fit criteria for a qualifying RCT and 4 studies were protocol only. The remaining 23 studies were thoroughly reviewed, and outcome metrics within each study were categorized and analyzed (Table 1). Of these 23 studies, 14 used 50 years of age as the low-end cutoff for inclusion, with the remaining studies using 55, 60, or 65 years.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analysis flow diagram demonstrating study selection.
Note. RCT = randomized controlled trials.
Table 1.
Paper Details of the 23 Studies Included.
| Author | Year | Treatment comparison | Pathology | Outcome measures (primary in bold, if specified) | Minimum age | Modified Coleman rating |
|---|---|---|---|---|---|---|
| Arora et al | 2011 | ORIF with volar locking plate vs closed reduction and cast immobilization | Displaced and unstable fractures | PRWE, DASH, pain (VAS), grip strength, wrist ROM, complications, radiographic findings | 65 | Fair |
| Bartl et al | 2014 | ORIF vs closed reduction and cast immobilization | Unstable intraarticular fractures | SF-36, DASH. radiographic findings, wrist ROM, EQ-5D | 65 | Fair |
| Chappuis et al | 2011 | Dorsal IM nailing vs volar plating | Extra-articular fractures | Wrist ROM, tightening strength, DASH, Mayo Clinic scale, radiographic findings, complications | 50 | Poor |
| Christersson et al | 2016 | Early mobilization vs standard casting | Stable dorsally angulated fractures | Radiographic findings (dorsal angulation) | 50 | Fair |
| Christersson et al | 2015 | Growth factor injection with ex-fix vs ex-fix alone | Unstable fractures | Radiographic findings, wrist ROM, grip strength, pain (VAS), DASH | 50 | Poor |
| Goehre et al | 2016 | Plate vs K-wire fixation | Unstable extra-articular or simple articular fractures | Radiographic findings, wrist ROM, DASH, PRWE, Castaing score | 65 | Poor |
| Gong et al | 2012 | Early initiation of bisphosphonate vs standard | Low-energy mechanism fractures | Radiographic findings (time to radiographic union), DASH, wrist ROM, grip strength | 50 | Fair |
| Gutierrez et al | 2017 | Supervised physical therapy vs home exercise therapy | Extra-articular multifragment fractures | PRWE, VAS, wrist ROM, grip strength, radiographic findings | 60 | Good |
| Hollevoet et al | 2014 | K-wire fixation vs palmar plating | Dorsally displaced fractures | Radiographic findings, DASH, grip and pinch strength | 50 | Fair |
| Jakubietz et al | 2011 | ORIF with bone graft vs ORIF alone | Intra-articular fractures | Wrist ROM, grip strength, DASH, Gartland score | 50 | Poor |
| Jakubietz et al | 2012 | Palmar plate vs dorsal plate | Complete articular fractures | Wrist ROM, radiographic findings | 50 | Fair |
| Karponis et al | 2015 | Salmon calcitonin vs placebo | Extra-articular fractures | Pain (VAS) | 50 | Poor |
| Kim et al | 2011 | Calcium phosphate bone cement vs control | Unstable fractures | Grip strength, wrist ROM, pain (VAS), Mayo scores, DASH, radiographic findings | 65 | Fair |
| Kuo et al | 2013 | Early digit mobilization vs control | Intra-articular and extra-articular fractures | Grip strength, dexterity (Purdue pegboard), MAM-36 | 50 | Poor |
| Lazovic et al | 2012 | Pulsed electromagnetic field vs control | Low-energy displaced fractures | Pain (VAS), wrist and forearm ROM, complications | 55 | Poor |
| Lei et al | 2016 | Probiotic vs placebo | Nondisplaced fractures | DASH, pain (VAS), CRPS, wrist ROM, grip strength | 60 | Fair |
| Magnus et al | 2013 | Unilateral strength training vs standard | Intraarticular and extraarticular fractures | Grip strength, wrist ROM, PRWE | 50 | Fair |
| Marchiex et al | 2010 | Palmar fixed-angle pinning vs mixed pinning | Dorsally displaced fractures | Radiographic findings, DASH, Herzberg score | 50 | Fair |
| Mellstrand-Navarro et al | 2010 | Volar locking plate vs external fixation | Dorsally displaced fractures | DASH, EQ-5D, radiographic findings, complications, PRWE, wrist ROM, grip strength | 50 | Good |
| Park et al | 2017 | Short-arm vs long-arm cast | Stable fractures | Radiographic findings (change in radial length), DASH, pain (VAS) | 55 | Good |
| Uchiyama et al | 2013 | Early administration of alendronate vs placebo | Fragility fractures | Radiographic findings (related to healing), wrist ROM, grip strength, tenderness to palpation, qDASH | 50 | Good |
| Wik et al | 2009 | Complete cast vs dorsal splint | Dorsally displaced fractures | Radiographic findings, pain (VAS) | 50 | Fair |
| Wong et al | 2010 | Casting vs percutaneous pinning | Unstable dorsally displaced extra-articular fractures | Radiographic findings, Mayo Wrist Score, satisfaction, WHOQOL, healing time, complications | 65 | Good |
Note. ORIF = open reduction internal fixation; PRWE = Patient-Rated Wrist Evaluation; SF-36 = Short Form 36; DASH = Disabilities of the Arm, Shoulder, and Hand; qDASH = quick DASH; VAS = Visual Analog Scale; ROM = range of motion; MAM-36 = Manual Ability Measure–36; WHOQOL = World Health Organization Quality of Life; EQ-5D = EuroQol 5-dimensional; CRPS = complex regional pain syndrome; K-wire = Kirschner wire; IM = intramedullary.
Primary outcome measures, if specified, are in bold.
Data Abstraction
Our data abstraction process was guided by prior work from Mead et al. 19 We included study features such as design, level of evidence, collection period, collection site, participant population, inclusion and exclusion criteria, data sources, and dependent/independent variables, as well as the study’s methods, results, and conclusions and methodological rigor. Two authors independently abstracted these data points from the 23 final studies. Any disagreements between the 2 reviewers on the data were discussed until consensus was reached.
Study Quality Assessment
We graded the methodology of each study with the Coleman Methodology Score. 20 This instrument was originally developed to assess the methods of clinical studies on patellar and Achilles tendinopathy and has previously been modified for assessment of the literature on lateral epicondylitis. 21 Our Modified Coleman Methodology is available in Supplemental Appendix I. Briefly, the Coleman Methodology instrument provides a rating from 0 to 100. A study is considered to have excellent methodology for a rating between 85 and 100, good if between 70 and 84, fair if between 55 to 69, and poor if 54 or less.
Results
The reviewed studies had a mean of 4.1 outcome metrics per study (SD = 1.7, range = 1-7). Sixteen studies (70%) used at least 1 physical examination test to compare treatments. The most commonly used test was wrist range of motion (65%), followed by grip strength (57%). Seventeen studies (74%) used radiographic studies to evaluate various parameters of fracture healing. Seventeen studies (74%) used a PROM. The most common PROM was the DASH questionnaire (57%), followed by the PRWE and Mayo Wrist Score (22% and 13%, respectively). Ten studies (44%) assessed patient pain with the Visual Analog Scale (VAS). Five studies (22%) assessed complications of treatment. Table 2 summarizes metric frequencies and individual metrics used in each study. Eleven studies (48%) defined a primary outcome measure. Of these, 4 designated a radiographic measure, 4 designated a PROM, 2 designated a physical examination finding, and 1 study reported pain score as the primary end point.
Table 2.
Summary of the Reported Metrics in Included Studies.
| Total studies | 23 |
| Mean total metrics per study | 4.1 |
| Maximum metrics in 1 study | 7 |
| Metrics | Frequency (% of studies with attribute) |
|---|---|
| Physical examination | 16 (69.6) |
| Wrist ROM | 15 (65.2) |
| Grip strength | 13 (56.5) |
| Forearm ROM | 1 (4.3) |
| Purdue pegboard | 1 (4.3) |
| Pinch strength | 1 (4.3) |
| Fracture evaluation | 17 (73.9) |
| Radiographic findings | 16 (69.6) |
| Castaing score | 1 (4.3) |
| Herzberg score | 1 (4.3) |
| Time to heal | 1 (4.3) |
| PROMs | 17 (73.9) |
| DASH | 15 (56.5) |
| PRWE | 5 (21.7) |
| Mayo Wrist Score | 3 (13.0) |
| EQ-5D | 2 (8.7) |
| SF-36 | 1 (4.3) |
| Satisfaction | 1 (4.3) |
| WHOQOL | 1 (4.3) |
| QuickDASH | 1 (4.3) |
| Pain (with VAS) | 10 (43.5) |
| Complications (general) | 5 (21.7) |
Note. ROM = range of motion; PROMs = patient-reported outcome measures; DASH = Disabilities of the Arm, Shoulder, and Hand; PRWE = Patient-Rated Wrist Evaluation; SF-36 = Short Form 36; WHOQOL = World Health Organization Quality of Life; VAS = Visual Analog Scale; EQ-5D = EuroQol 5-dimensional.
Based on the Modified Coleman Methodology Score instrument, no studies received an excellent methodology rating, 4 received a good rating (17%), 11 received a fair rating (48%), and 8 received a poor rating (35%).
Discussion
Objective and subjective measures, together, can ensure appropriate comparisons between populations while also ensuring that aspects of care that are important to patients are collected. When implemented in a similar fashion across studies, outcome metrics can be used to compare and contrast results between investigations. We found that the outcome measures reported in RCTs for the treatment of distal radius fracture are heterogeneous and lack standardization. Radiographic outcomes and physical examination findings were each reported in 74% and 70% of studies, respectively, with either radiographic outcomes or physical examination findings being reported in 95% of studies. Wrist range of motion (61%) and grip strength (52%) were the 2 commonly reported physical examination findings. While most studies reported at least 1 PROM, there was wide variation in the specific measures used outside of the DASH, which was reported in 88% of studies that included PROMs in their analysis. Six other PROMs were reported across the literature, with no other PROM being reported in more than 21% of studies. While various subjective measures were collected with good frequency across studies, objective measures were more homogeneously reported, allowing for easier comparison across cohorts. This is unfortunate, as the literature suggests that traditional objective measures have limitations regarding fully capturing outcomes that are most important to the patients themselves.
Multiple studies have shown that radiographic indices may not correlate with patients’ perceived level of function in the context of distal radius fracture in an older population.3,22-25 Nelson et al reported on 96 patients aged 60 years or older, of which 48 had radiographic evidence of malunion. At a minimum 1-year follow-up, there was no difference in QuickDASH scores, VAS, strength, or range of motion. 23 Furthermore, Shapiro et al found that patients aged 55 years and older with distal radius fractures report radiographic outcome as one of the least important attributes when evaluating the proposed method of treatment for their injury, with only cosmesis and cost to insurance reported to be of lower importance. 26 Radiographic outcomes are important to obtain, easy to measure, and are objective and often standardized, but should not be reported in the absence of other subjective measures. Furthermore, grip strength and wrist range of motion have been shown to correlate with patient satisfaction at 1-year follow-up.12,13,27 Deficits in wrist arc of motion, in particular, may affect overall patient dissatisfaction even when range of motion has been restored to levels adequate for performing activities of daily life (ADLs). Chung et al reported that while existing literature estimated that just 25% to 57% of baseline arc of motion is required for ADLs, patients recovering from distal radius fractures in their cohort needed to obtain 95% of their preinjury arc of motion to be satisfied. 12 Patient-reported outcomes measures aim to capture how patients perceive changes to baseline range of motion and grip strength, although multiple studies have shown that objective clinical examination measures account for a small portion of variability in overall scores for different PROMs.13,28 A combination of relevant objective clinical examination metrics, in particular grip strength and wrist arc of motion, as well as consistently collected PROM scores can be comprehensive outcome assessments in an RCT. Independent assessment of pain scores, which were collected only 44% of the time in our included studies, is also important to incorporate more consistently, as pain does not always correlate with other subjective outcome measures. 27 The degree to which PROMs are influenced by pain scores also varies between metrics, making standardized independent collection of pain scores something to consider for future related RCTs.
Our study has several limitations. Being a systematic review, this work is limited by the number of high-quality randomized controlled studies. We used the Modified Coleman Methodology Score to account for variability in study quality and found that 65% of studies included were of either good or fair quality. Our group performed a similar systematic review of level I and II RCTs for carpal tunnel syndrome and found a similar overall level of study quality (70% of studies rated as good or fair). In an attempt to limit the subjectivity of our screening process, we followed PRISMA guidelines for systematic reviews and had multiple reviewers for each article. We used a previously established method of assessing each study developed by Mead et al 19 to standardize our analysis. Finally, in an effort to be inclusive of all level I and II RCTs, we included studies with a wide variety of treatment modalities, ranging from operative interventions to pharmacologic measures alone. To some degree, heterogeneity in outcome measures may be unavoidable when the treatment arms in each study vary so widely among trials.
Standardization of the collection of patient-centered outcome measures in addition to objective clinical metrics in studies investigating treatment for distal radius fractures has clear benefits for both patients and physicians. Radiographic and physical examination findings remain important to report but have known limitations when reported without supplementary patient-centered outcomes. Our study demonstrates that although PROMs are being used in most studies, measures other than DASH have been used in limited fashion and are inconsistently reported, making accurate comparison between studies difficult. Pain scores and cost remain scarcely reported. These findings can be used to guide future RCTs to include measures in a standardized fashion that will sufficiently supplement traditional radiographic and objective metrics to provide a more comprehensive assessment of the outcomes of most importance to patients enrolled in these studies.
Supplemental Material
Supplemental material, sj-docx-1-han-10.1177_15589447211028919 for Outcome Metrics in the Treatment of Distal Radius Fractures in Patients Aged Above 50 Years: A Systematic Review by Nathaniel Fogel, Kevin Mertz, Lauren M. Shapiro, Allison Roe, Sahitya Denduluri and Robin N. Kamal in HAND
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: Institutional review board approval was not indicated or required.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: This study includes no human subjects, so informed consent was not obtained or required.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: R.K. reports grants from National Institutes of Health; grants from Orthopedic Research and Education Foundation during the conduct of the study; and personal fees from Acumed, Exsomed, Triple Ring, Restor3d, and Foundry Therapeutics 1, outside the submitted work. All other authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by an NIH K23AR073307-01 award to author R.K. The content of this work is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
ORCID iD: Robin N. Kamal  https://orcid.org/0000-0002-3011-6712
https://orcid.org/0000-0002-3011-6712
References
- 1. Nellans KW, Kowalski E, Chung KC. The epidemiology of distal radius fractures. Hand Clin. 2012;28(2):113-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chung K, Spilson S. Frequency and Epidemiology of Forearm Fractures in the United States. J Hand Surg Am. 2001;26A:908-915. [DOI] [PubMed] [Google Scholar]
- 3. Arora R, Gabl M, Gschwentner M, et al. A comparative study of clinical and radiologic outcomes of un- stable Colles type distal radius fractures in patients older than 70 years: nonoperative treatment versus volar locking plating. J Orthop Trauma. 2009;23:237-242. [DOI] [PubMed] [Google Scholar]
- 4. Chappuis J, Bouté P, Putz P. Dorsally displaced extra-articular distal radius fractures fixation: dorsal IM nailing versus volar plating. A randomized controlled trial. Orthop Traumatol Surg Res. 2011;97(5):471-478. [DOI] [PubMed] [Google Scholar]
- 5. Goehre F, Otto W, Schwan S, et al. Comparison of palmar fixed-angle plate fixation with K-wire fixation of distal radius fractures (A0 A2, A3, C1) in elderly patients. J Hand Surg Eur. 2014;39E(3):249-257. [DOI] [PubMed] [Google Scholar]
- 6. Hollevoet N, Vanhoutte T, Vanhove W, et al. Percutaneous K-wire fixation versus palmar plating with locking screws for Colles’ fractures. Acta Orthop Belg. 2011;77:180-187. [PubMed] [Google Scholar]
- 7. MOTION Group. Patient-reported outcomes in orthopaedics. J Bone Joint Surg Am. 2018;100:436-442. [DOI] [PubMed] [Google Scholar]
- 8. Anzarut A, Johnson JA, Rowe BH, et al. Radiologic and patient-reported functional outcomes in an elderly cohort with conservatively treated fractures. J Hand Surg Am. 2004;29:1121-1127. [DOI] [PubMed] [Google Scholar]
- 9. Synn AJ, Makhni EC, Makhni MC, et al. Distal radius fractures in older patients: is anatomic reduction necessary. Clin Orthop Relat Res. 2009;467(6):1612-1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Goldhahn J, Beaton D, Ladd A, et al. ; for International Osteoporosis Foundation (IOF). Recommendation for measuring clinical outcome in distal radius fractures: a core set of domains for standardized reporting in clinical practice and research. Arch Orthop Trauma Surg. 2014;134(2):197-205. [DOI] [PubMed] [Google Scholar]
- 11. Waljee JF, Ladd A, MacDermid JC, et al. A unified approach to outcomes assessment for distal radius fractures. J Hand Surg Am. 2016;41(4):565-573. [DOI] [PubMed] [Google Scholar]
- 12. Chung KC, Haas A. Relationship between patient satisfaction and objective functional outcome after surgical treatment for distal radius fractures. J Hand Ther. 2009;22(4):302-307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shauver MJ, Chang KW, Chung KC. Contribution of functional parameters to patient-rated outcomes after surgical treatment of distal radius fractures. J Hand Surg Am. 2014;39(3):436-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Karnezis I, Fragkiadakis E. Association between objective clinical variables and patient-rated disability of the wrist. J Bone Joint Surg Br. 2002;84(7):967-970. [DOI] [PubMed] [Google Scholar]
- 15. MacDermid JC. Development of a scale for patient rating of wrist pain and disability. J Hand Ther. 1996;9(2):178-183. [DOI] [PubMed] [Google Scholar]
- 16. MacDermid JC, Richards RS, Donner A, et al. Responsiveness of the short form-36, disability of the arm, shoulder, and hand questionnaire, patient-rated wrist evaluation, and physical impairment measurements in evaluating recovery after a distal radius fracture. J Hand Surg Am. 2000;25(2):330-340. [DOI] [PubMed] [Google Scholar]
- 17. Ayers D, Bozic K. The importance of outcome measurement in orthopaedics. Clin Orthop Relat Res. 2013;471(11):3409-3411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zarezadeh A, Mamelson K, Thomas W, et al. Outcomes of distal humerus fractures: what are we measuring. Orthop Traumatol Surg Res. 2018;104(8):1253-1258. [DOI] [PubMed] [Google Scholar]
- 19. Mead E, Doorenbos A, Javid S, et al. Shared decision-making for cancer care among racial and ethnic minorities: a systematic review. Am J Public Health. 2013;103(12):e15-e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Coleman BD, Khan KM, Maffulli N, et al. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10(1):2-11. [DOI] [PubMed] [Google Scholar]
- 21. Cowan J, Lozano-Calderón S, Ring D. Quality of prospective controlled randomized trials—analysis of trials of treatment for lateral epicondylitis as an example. J Bone Joint Surg Am. 2007;89(8):1693-1699. [DOI] [PubMed] [Google Scholar]
- 22. Mulders M, Detering R, Rikli D, et al. Association between radiological and patient-reported outcomes in adults with a displaced distal radius fracture: a systematic review and meta-analysis. J Hand Surg Am. 2018;43(8):710-719. [DOI] [PubMed] [Google Scholar]
- 23. Diaz-Garcia R, Oda T, Shauver M, et al. A systematic review of outcomes and complications of treating unstable distal radius fractures in the elderly. J Hand Surg Am. 2011;36(5):824-835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nelson GN, Stepan JG, Osei DA, et al. The impact of patient activity level on wrist disability after distal radius malunion in older adults. J Orthop Trauma. 2015;29(4):195-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Barton T, Chambers C, Bannister G. A comparison between subjective outcome score and moderate radial shortening following a fractured distal radius in patients of mean age 69 years. J Hand Surg Eur Vol. 2007;32(2):165-169. [DOI] [PubMed] [Google Scholar]
- 26. Shapiro LM, Eppler SL, Baker LC, et al. The usability and feasibility of conjoint analysis to elicit preferences for distal radius fractures in patients 55 years and older. J Hand Surg Am. 2019;44(10):846-852. [DOI] [PubMed] [Google Scholar]
- 27. Souer J, Lozano-Calderon S, Ring D. Predictors of wrist function and health status after operative treatment of fractures of the distal radius. J Hand Surg Am. 2008;33(2):157-163. [DOI] [PubMed] [Google Scholar]
- 28. Harris JE, MacDermid JC, Roth J. The International Classification of Functioning as an explanatory model of health after distal radius fracture: a cohort study. Health Qual Life Outcomes. 2005;3:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-han-10.1177_15589447211028919 for Outcome Metrics in the Treatment of Distal Radius Fractures in Patients Aged Above 50 Years: A Systematic Review by Nathaniel Fogel, Kevin Mertz, Lauren M. Shapiro, Allison Roe, Sahitya Denduluri and Robin N. Kamal in HAND