Abstract
Background:
This study sought to characterize charges associated with operative treatment of distal radius fractures and identify sources of variation contributing to overall cost.
Methods:
A retrospective study was performed using the New York Statewide Planning and Research Cooperative System database from 2009-2017. Outpatient claims were identified using the International Classification of Diseases-9/10-Clinical Modification diagnosis codes for distal radius fixation surgery. A multivariable mixed model regression was performed to identify variables contributing to total charges of the claim, including patient demographics, anesthesia method, surgery location (ambulatory surgery center [ASC] versus a hospital outpatient department [HOPD], operation time, insurance type, Charlson Comorbidity Index, and billed procedure codes.
Results:
A total of 9029 claims were included, finding older age, private primary insurance, surgery performed in a HOPD, and use of local anesthesia (vs general or regional) associated with increased total charges. There was no difference between gender, race, or ethnicity. Additionally, open reduction and internal fixation (ORIF), increased operative time/fracture complexity, and use of perioperative medications contributed significantly to overall costs.
Conclusions:
Charges for distal radius fracture surgery performed in a HOPD were 28.3% higher than compared to an ASC, and cases with local anesthesia had higher billed claims compared to regional or general anesthesia. Furthermore, charges for percutaneous fixation were 54.6% lower than ORIF of extraarticular fracture, and claims had substantial geographic variation. These findings may be used by providers and payers to help improve value of distal radius fracture care.
Level of Evidence:
Level III
Keywords: cost, factors, fixation, fracture, radius
Introduction
Cost is an important and growing concern in orthopedics and healthcare, as expenditures can dramatically outpace inflation and strain the healthcare system in an unsustainable way.1-3 Therefore, it is imperative to evaluate orthopedic management strategies by not only their clinical benefits, but also their financial costs. A number of studies have identified substantial variation in the costs of implants and procedures—even between similar types of injuries—which identifies a modifiable cost factor for improving value in orthopedic surgery.4-10
Depending on the needs of individual patients and severity of their injuries, distal radius fractures can be treated with several different methods, including both nonoperative (with or without reduction, depending on the severity of the fracture) and operative. Surgery may consist of closed reduction and percutaneous pinning (CRPP), open reduction and internal fixation (ORIF), and/or external fixation, each of which has its own advantages and disadvantages.11-14
A recent randomized-controlled trial comparing CRPP and ORIF of distal radius fractures in adults found no difference in functional outcomes between the 2 treatment methods, and also that CRPP was less expensive (£727) and faster (31 vs. 66 minutes) than ORIF. 15 However, the ideal treatment method for distal radius fractures remains controversial, and the costs vary substantially.9,16 Furthermore, cost can be challenging to compare across populations and systems with different insurance carriers and reimbursements, contracts, patient demographics, and costing methods, and often carry a risk of systematic bias. 17
Financial terminology in healthcare can be opaque and confusing, but it is important to distinguish between different terms. “Cost” can have different meanings: to providers, cost is the expense incurred to deliver health care services; to payers, it is the amount they pay to providers; to patients, it is the out-of-pocket expense. 18 “Reimbursement” is a payment made by a payer (usually a third-party insurer) to a provider, which can be for a particular service (fee-for-service), a period of time (per diem), episode of care (ie, diagnosis-related group, or DRG), or patient under care (capitation). “Charge,” which is the unit considered here, is the amount billed by a provider of service.
We sought to characterize the charges associated with operative treatment of distal radius fractures in an outpatient setting in a large, statewide, captured population. We additionally aimed to identify sources of variation, including patient demographics, comorbidities, treatment location, anesthetic variables, and procedure type.
Methods
Adult patients (18 years and older) were identified in the New York Statewide Planning and Research Cooperative System (SPARCS) database from 2009 to 2017. SPARCS is a comprehensive all-payer database collecting all inpatient and outpatient preadjudicated claims in New York. This includes all International Classification of Diseases (ICD) diagnosis codes and ICD/Current Procedural Terminology (CPT) procedure codes associated with all visits.
Claims in the outpatient setting were identified using the ICD-9-Clinical Modification (CM) and ICD-10-CM diagnosis codes for distal radius fractures (see Table 1 for codes used). The patients included in the analysis had a primary diagnosis of distal radius fracture to avoid more complex cases which would have increased charges but did allow for secondary procedures such as ulnar styloid fixation. Claims were then further filtered for distal radius fixation surgery (CPT codes 25606, 25607, 25608, 25609; with or without 20690), and only included outpatient surgery. Charges for each claim were adjusted for inflation to January 2017 prices. 19 Only a patient’s first surgery was included in the analysis.
Table 1.
Current Procedural Terminology Codes for Distal Radius Fracture Fixation.
| Code | Description |
|---|---|
| 25606 | Percutaneous fixation distal radius fracture or epiphyseal separation |
| 25607 | Open treatment of extraarticular distal radial fracture or epiphyseal separation, with or without fracture of ulnar styloid, with or without internal or external fixation |
| 25608 | Open treatment of intraarticular distal radial fracture or epiphyseal separation with internal fixation of 2 fragments |
| 25609 | Open treatment of intraarticular distal radial fracture or epiphyseal separation with internal fixation of 3 or more fragments |
| 20690 | Application of a uniplane (pins or wires in 1 plane), unilateral, external fixation system |
A multivariable mixed model regression with random effects for the facility was performed to assess the variables that contribute significantly to the total charge of the claim. The total charge was modeled as the natural log of the total charge to account for the nonnormal distribution. The variables included in the regression were patient age, sex, anesthesia method (local without or without monitored anesthesia care [MAC], regional, or general), whether the surgery took place in an ambulatory surgery center (ASC) versus a hospital outpatient department (HOPD), operation time in minutes, primary insurance type, race, ethnicity, and Charlson Comorbidity Index (CCI). 20 Charlson Comorbidity Index was dichotomized to a score of 0 versus a score of ≥ 1.
Outliers for operation time in minutes were removed. A lower limit was set at 5 minutes and an upper limit was set at Q3 + 1.5 * interquartile range (IQR). Once these outliers were removed, to avoid modeling outlier charges, we used 80% of the average charge reported by Medicare in each year in New York across each CPT code used for surgical fixation of distal radius which was $572- to $671 for CPT 25606, $615 to $743 for CPT 25607, $702 to $834 for CPT 25608, and $896 to -$1,060 for CPT 25609. 21 These lower bounds were applied to the charges before they were adjusted for inflation. 19 After charges were adjusted for inflation, an upper bound was set at Q3 + 1.5 * IQR for the billed charges.
P-values were adjusted using the false discovery rate method to adjust for type I error given the number of independent variables in the regression model. An adjusted P-value < .05 was considered significant across all statistical analyses. All analyses were performed using SAS 9.4 (SAS Inc, Cary, North Carolina).
Results
From 2009 to 2017, 9029 claims were included, with significantly more women (73.2%) than men (26.8%) (Table 2). The number of cases stayed relatively constant over the time period reaching a maximum of 1259 (range: 713 to 1259) cases in 2014. The median charge per claim was $12,729 with a mean of $13,541. The majority of patients had a Charlson Comorbidity Index of 0 at the time of surgery. The median time in the operating room in minutes was 81 minutes (Table 2).
Table 2.
Patient Demographics and Characteristics.
| Demographic | n = 9029 | P-value |
|---|---|---|
| Total charge, median (mean, SD) | $12,729 ($13,541, 6044) | |
| Age, median (mean, SD) | 58 (56.3, 15.8) | |
| Operation time in minutes, median, (mean, SD) | 81 (86.1, 37.2) | |
| Gender, n (%) | ||
| Female | 6606 (73.2) | <.0001 |
| Male | 2423 (26.8) | — |
| Ethnicity, n (%) | ||
| Hispanic | 700 (7.8) | |
| Non-Hispanic | 8329 (92.3) | |
| Race, n (%) | ||
| White | 7347 (81.4) | |
| Asian | 364 (4.0) | |
| African American | 361 (4.0) | |
| Other | 957 (10.6) | |
| Primary insurance, n (%) | ||
| Private | 4983 (55.2) | |
| Federal | 3007 (33.3) | |
| Worker’s compensation | 539 (6) | |
| Self-pay | 500 (5.5) | |
| Charlson Comorbidity Index, n (%) | ||
| 0 | 7765 (86.0) | <.0001 |
| ≥ 1 | 1264 (14.0) | — |
| Primary procedure | ||
| CPT 25606 | 528 (5.9) | |
| CPT 25607 | 2635 (29.2) | |
| CPT 25608 | 3202 (35.5) | |
| CPT 26509 | 2664 (29.5) | |
Note. CPT = Current Procedural Terminology.
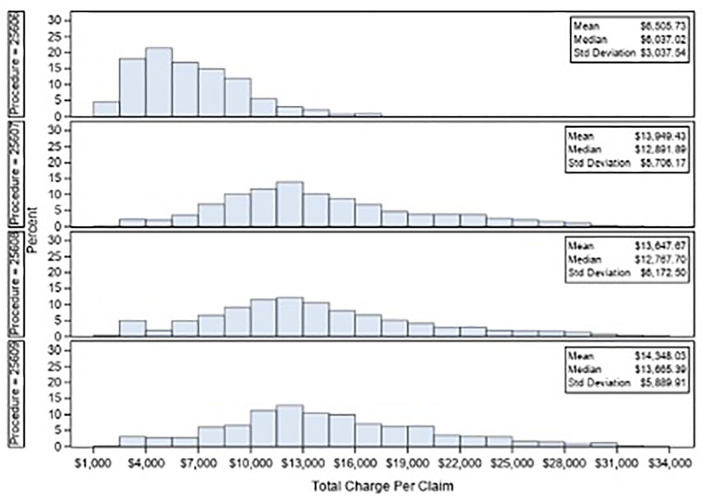
There were significant differences in average billed claims between Health Service Areas (HSA, Figure 1, Supplemental Table 1). The most expensive region was Nassau and Suffolk counties (which encompass Long Island, New York), which had an average claim 2-fold higher than the least expensive HSA, the Finger Lakes region ($16,867 vs. $8,399).
Figure 1.
Relative value of average billed claims by Health Service Area. Darker shaded regions indicate a higher bill than lighter-shaded regions (range: $8399-$16,867).
The CPT code 25608 (open reduction internal fixation, 2-part intraarticular fracture) was the dominant procedure with approximately 35.5% cases whereas CPT code 25606 (closed reduction and percutaneous pinning) was the least common accounting for approximately 5.9% of cases (Table 2). The majority of cases were performed in a HOPD (84.5%) as opposed to an ASC. General anesthesia was the most common method of anesthesia accounting for 73% of cases (Table 3).
Table 3.
Predictors for Total Billed Amount for Distal Radius Fracture Surgery.
| n = 9029 (%) | Fractional estimate of change from baseline (95% CI) | SE | P-value | |
|---|---|---|---|---|
| Age | — | 0.1% (0.05% to 0.12%) | 0.002% | <.0001 |
| Females a | 6606 (73.2) | 0.5% (−0.6% to 1.7%) | 0.6% | .4782 |
| Anesthesia method b | ||||
| General | 6590 (73) | −12.6% (−15.0% to −10.3%) | 1.2% | <.0001 |
| Regional | 1512 (16.8) | −9.1% (−11.6% to −6.5%) | 1.3% | <.0001 |
| HOPD c | 7627 (84.5) | 28.3% (12.5% to 44.0%) | 8.04% | .0012 |
| Operation time (per minute) | — | 0.3% (0.2% to 0.3%) | 0.01% | <.0001 |
| Primary payer d | ||||
| Federal | 3007 (33.3) | −0.7% (−1.9% to 0.5%) | 0.6% | .3072 |
| Self-Pay | 500 (5.5) | −2.2% (−4.52% to 0.16%) | 1.19% | .1274 |
| Worker’s compensation | 539 (6) | −3.0% (−5.1% to −1.0%) | 1.05% | .0102 |
| Charlson Comorbidity Index ≥ 1 e | 1264 (14) | 1.6% (0.2% to 3.1%) | 0.73% | .055 |
| Race f | ||||
| Asian | 364 (4) | 0.2% (−2.4% to 2.8%) | 1.34% | .9133 |
| African-American | 361 (4) | 1.8% (−0.8% to 4.4%) | 1.31% | .2479 |
| Other | 957 (10.6) | 1.3% (−0.7% to 3.2%) | 1.02% | .3066 |
| Hispanic ethnicity g | 700 (7.8) | 0.8% (−1.5% to 3.1%) | 1.18% | .6043 |
| Procedure code categories | ||||
| Anticholinergic agent | 24 (0.3) | 7.8% (−1.5% to 17.0%) | 4.71% | .166 |
| Anticoagulant agent | 41 (0.5) | 7.2% (−1.0% to 15.4%) | 4.19% | .1555 |
| Anti-emetic agent | 3,356 (37.2) | −0.6% (−2.0% to 0.9%) | 0.75% | .5486 |
| Anti-histamine agent | 432 (4.8) | 1.9% (−0.6% to 4.34%) | 1.27% | .2119 |
| Anti-psychotic agent | 50 (0.6) | −4.4% (−10.9% to 2.1%) | 3.32% | .2688 |
| Benzodiazepine | 3,731 (41.3) | 6.1% (4.5% to 7.6%) | 0.79% | <.0001 |
| Electrocardiogram | 421 (4.7) | 0.2% (−2.2% to 2.6%) | 1.25% | .9133 |
| Functional assessment | 84 (0.9) | 3.9% (−1.5% to 9.3%) | 2.77% | .2479 |
| Imaging | 4948 (54.8) | 3.7% (2.2% to 5.2%) | 0.76% | <.0001 |
| Image guided procedure | 199 (2.2) | 9.8% (5.5% to 14.1%) | 2.21% | <.0001 |
| Immunization | 12 (0.1) | −11.3% (−24.4% to 1.8%) | 6.69% | .1591 |
| Bronchodilator | 48 (0.5) | 2.3% (−4.7% to 9.2%) | 3.52% | .6043 |
| IV fluids | 917 (10.2) | 10.1% (8.0% to 12.3%) | 1.1% | <.0001 |
| Labs | 1495 (16.6) | 1.9% (0.5% to 3.4%) | 0.74% | .0211 |
| Muscle relaxant | 159 (1.8) | −0.1% (−3.9% to 3.7%) | 1.96% | .9556 |
| Muscle strengthener | 170 (1.9) | 3.5% (−0.2% to 7.3%) | 1.91% | .1248 |
| Narcotic | 4615 (51.1) | 4.7% (3.0% to 6.3%) | 0.84% | <.0001 |
| Nonsteroid/narcotic | 1684 (18.7) | 1.8% (0.4% to 3.3%) | 0.74% | .0291 |
| External fixation | 71 (0.8) | 35.9% (30.1% to 41.8%) | 3% | <.0001 |
| Pre-op antibiotics | 3560 (39.4) | 2.4% (1.0% to 3.9%) | 0.73% | .0022 |
| Prophylaxis injection | 179 (2) | 2.0% (−3.7% to 7.8%) | 2.94% | .5986 |
| Pulse oximetry | 244 (2.7) | 3.8% (−2.4% to 10.0%) | 3.15% | .3067 |
| Recovery supplies | 169 (1.9) | 8.4% (1.2% to 15.5%) | 3.63% | .0455 |
| Sedation services | 43 (0.5) | 1.0% (−8.6% to 10.6%) | 4.91% | .9133 |
| Steroid | 1439 (15.9) | 6.6% (4.9% to 8.3%) | 0.87% | <.0001 |
| Surgical supplies | 5269 (58.4) | 16.2% (14.6% to 17.8%) | 0.82% | <.0001 |
| Ventilation | 58 (0.6) | 0.3% (−6.1% to 6.7%) | 3.27% | .9486 |
| Primary procedure code h | ||||
| CPT 25609 | 2664 (29.5) | 2.8% (1.5% to 4.2%) | 0.69% | .0001 |
| CPT 25608 | 3202 (35.5) | 0.2% (−1.1% to 1.4%) | 0.64% | .8759 |
| CPT 25606 | 528 (5.9) | −54.6% (−57.2% to −52.1%) | 1.3% | <.0001 |
Note. CI = confidence interval; HOPD = hospital outpatient department; Charlson Comorbidity Index = Charlson Comorbidity Index; CPT = Current Procedural Terminology; ASC = ambulatory surgery center.
Compared to males.
Compared to local anesthesia (with or without monitored anesthesia care).
Compared to ASC.
Compared to private primary insurance.
Compared to Charlson Comorbidity Index = 0.
Compared to white race.
Compared to non-Hispanic ethnicity.
Compared to CPT 25607.
The bold faced values are those that are statistically significant (i.e. p<0.05).
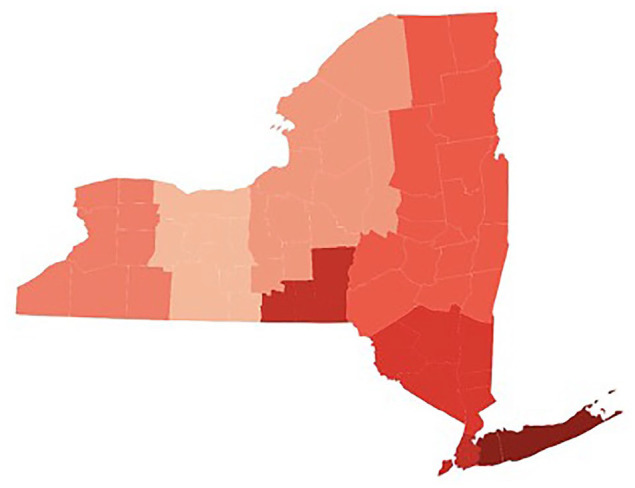
In the multivariable analysis to determine independent risk factors, older age significantly contributed to increased total charge amounts, although this may not be clinically significant (0.1%/year of age). Both general and regional anesthesia were associated with lower total charge with respect to local anesthesia (with or without MAC). Having the procedure in a HOPD was independently associated with approximately a 28.3% (95% CI: 12.5%-44%) increase in total charge amount when compared to ASC. Having worker’s compensation as a primary insurer was associated with lower total charge amounts when compared to private primary insurance. In terms of drugs used, claims with benzodiazepines, narcotics, nonsteroid/narcotic pain agents, preoperative antibiotics, or steroids were associated with higher total charge amounts. Claims that included billing for external fixation (CPT 20690) were associated with 35.9% (95% CI: 30%-41.8%) higher total charge amounts than those without. A 1-minute increase in operation time was associated with a 0.26% (95% CI: 0.24%-0.28%) increase in total charge. Compared to CPT 25607, CPT 25606 had over 50% lower total charges per claim whereas CPT 25609 had increased total charges per claim; CPT 25608 was similar to 25607 (Table 3). The charge distributions for CPT codes 25607, 25608, and 25609 were similar, while CPT code 25606 is distributed toward lower charges (Figure 2).
Figure 2.
Claim charges for operative fixation of distal radius fractures, by current procedural terminology code.
Discussion
In this administrative database study, we found that the charges for surgery performed in a HOPD were 28.3% higher than those performed in an ASC. The charge for CRPP was 54.6% lower than for ORIF of extraarticular fractures, and supplemental external fixation increased claims by 35.9%. Interestingly, cases with local anesthesia (with or without MAC) were associated with a higher billed claim than those performed under regional or general anesthesia. We also found significant regional variation in claim amount.
Fixation with CRPP has consistently been shown to be less costly than ORIF in several recent studies. A multi-center prospective randomized controlled trial found that K-wire fixation was approximately 20% less costly than locking plate fixation; this was consistent when considering both the payer and societal perspectives.15,22 In a database study of 23,453 patients, Huetteman 9 demonstrated that the surgical cost for percutaneous pinning was $3440, compared with $6289 for ORIF (44.3% decrease), and that surgery itself comprised a majority of the overall cost of care. Nandyala et al 23 compared the costs between CRPP and ORIF in the perioperative period out to 1 year postoperatively and found that CRPP was significantly less expensive over all time points, including approximately 63% less perioperatively, although CRPP had worse functional outcomes. Similarly, we found that CRPP was associated with significantly lower billed charges (by 54.6%) than ORIF of extraarticular fractures, while external fixation increased claims by 35.9%. Compared with extraarticular fractures, complex intraarticular fractures may require more operative/anesthesia time and potentially more hardware. 6 The question if ORIF provides an improved outcome commensurate with the increased cost remains controversial.
The location of surgery proved to be a significant and clinically meaningful predictor of overall billed charges. This study demonstrated that compared to ASCs, distal radius fixation performed in HOPDs incurred a 28.3% increase, similar to other recent studies.16,24,25 Mather et al 5 retrospectively compared the cost of volar plate fixation for distal radius fractures at ASCs to inpatient surgery, and found that the mean operative cost of the inpatient facility was significantly greater ($7640) versus the average outpatient facility ($5220). The authors concluded that the only significant predictor of operative cost and time was facility type; set-up and nursing times were 100% longer in the inpatient facility. Treatment location has also been shown to affect cost of care in other surgical procedures. A systemic review of orthopedic procedures found 7 studies with an average savings of 18% to 58% for outpatient procedures compared to inpatient, further reinforcing the cost-containment implications of shifting distal radius fracture surgery to ASCs. 26
Anesthesia method was found to have a significant impact on overall charge, with both general and regional anesthesia incurring approximately 10% lower claim charges when compared to local anesthesia (with or without monitored anesthesia care). Interestingly, claims including the use of benzodiazepines, narcotics, and nonsteroid/narcotic pain agents were associated with higher total charge amounts compared to claims that did not include these agents. A possible explanation may be that local anesthesia requires the use of these adjuvant medications (ie, monitored anesthesia care) to adequately control pain and maintain appropriate sedation levels. While previous studies have noted lower overall costs associated with local anesthesia compared to regional or general anesthesia in minor hand procedures, a review by Lalonde and Martin note that the success of local anesthesia in these procedures is associated with the removal of tourniquet use and relatively quick surgical time.16,25,27-29 Distal radius fracture fixation can involve deep surgical dissection and the use of a tourniquet, which may necessitate the use of adjuvant medication intra-operatively, increasing overall cost. This suggests there is utility to considering regional anesthesia to reduce the use of adjuvant agents that may increase total costs.
There was significant regional variation between the Health Service Areas, with a 2-fold difference between the highest and the lowest. Similarly, other investigations demonstrate unexplained geographic differences in cost, intensity of care, and outcomes, despite controlling for patient and population characteristics.30-33 Sun and Baker 34 found that increased market concentration was associated with a 7% increase in physician fees. This may represent a further opportunity to improve value by directing care to providers/facilities that consistently demonstrate low cost and high quality.35,36
The analysis of patient demographics indicated that older age contributes slightly toward increased charges, while patient sex and race did not demonstrate any significant differences, similar to the findings of Kazmers et al. 16 While there is a paucity of literature regarding the effect of comorbidities on the cost of distal radius fracture care, Johnson et al 27 analyzed the relationship of Charlson Comorbidity Index and hip fractures, and found that increasing Charlson Comorbidity Index scores were associated with longer length of stay and increased overall costs. We found a trend toward increased charges for patients with a Charlson Comorbidity Index ≥ 1, although not statistically significant (P = .055). This may be reflective of an overall relatively healthy cohort who underwent surgery.
When accounting for differences between insurance status, Day et al 37 found that hand/wrist patients with Worker’s Compensation insurance had a higher intensity of care than those with commercial insurance, but the difference was often in the diagnostic workup. Considering perioperative related charges alone, we found that Worker’s Compensation insurance was associated with lower billed claim compared to other insurance types. This may be due to differences in insurance contracting and expected claim reimbursement, and represents an area of future study.
The present study has a number of limitations, mostly related to the administrative database design. Several clinically important factors, such as fracture pattern, are not included, nor are clinical or functional outcomes, which may be an important component of value. Although this necessarily and appropriately limits the analysis and conclusions to just the surgical episode, this also allows for more external validity and comparisons with other health systems. The multivariable mixed effects model attempted to adjust for many factors to seek independent associtions, but there may be hidden confounders that were not adequately captured, and therefore not controlled for. Only billed claim amounts are considered, rather than costs or reimbursements In this database, billed claims (charges) were the most robust source of data, and found to be the most reliable. Charges (in addition to costs and reimbursements) will also vary significant between facilities, and while this analysis considers all patients in the state of New York, it may not be directly applicable to any particular institution. Additionally, the patients and treatment patterns may vary by region, and those of New York may be meaningfully different than another region, which may limit the generalizability of the analysis.
In our study of adult patients undergoing outpatient distal radius fracture surgery in New York State, we found that charges for distal radius fracture surgery performed in a HOPD were 28.3% higher than those performed in an ASC, and cases with local anesthesia (with or without MAC) had higher billed claims than those using regional or general anesthesia. Furthermore, charges for CRPP cases were 54.6% lower than ORIF of extraarticular fracture, and the claims had substantial geographic variation. These findings may be used by providers and payers to help improve the value of distal radius fracture care.
Supplemental Material
Supplemental material, sj-docx-1-han-10.1177_15589447221077379 for Charges for Distal Radius Fracture Fixation Are Affected by Fracture Pattern, Location of Service, and Anesthesia Type by Avi D. Goodman, Peter Brodeur, Aristides I. Cruz, Lindsay R. Kosinski, Edward Akelman and Joseph A. Gil in HAND
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: This study was approved by our institutional review board.
State of Human and Animal Rights: There were no experimental human or animal subjects.
Statement of Informed Consent: This article contains only data derived from de-identified patient information. Institutional Review Board approval was waived (Lifespan IRB).
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Avi D. Goodman  https://orcid.org/0000-0001-8665-8257
https://orcid.org/0000-0001-8665-8257
Peter Brodeur  https://orcid.org/0000-0002-7391-719X
https://orcid.org/0000-0002-7391-719X
Lindsay R. Kosinski  https://orcid.org/0000-0002-8586-7089
https://orcid.org/0000-0002-8586-7089
Joseph A. Gil  https://orcid.org/0000-0002-0117-1026
https://orcid.org/0000-0002-0117-1026
References
- 1. Khullar D, Rajkumar R. Innovations to cut US healthcare prices. BMJ. 2018;361:k1591. doi: 10.1136/bmj.k1591. [DOI] [PubMed] [Google Scholar]
- 2. Dieleman JL, Squires E, Bui AL, et al. Factors associated with increases in US health care spending, 1996-2013. J Am Med Assoc. 2017;318(17):1668-1678. doi: 10.1001/jama.2017.15927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. J Am Med Assoc. 2018;319(10):1024-1039. doi: 10.1001/jama.2018.1150. [DOI] [PubMed] [Google Scholar]
- 4. Wasterlain AS, Melamed E, Bello R, et al. The effect of price on surgeons’ choice of implants: a randomized controlled survey. J Hand Surg Am. 2017;42(8):593-601.e6. doi: 10.1016/j.jhsa.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 5. Mather RC, III, Wysocki RW, Mack Aldridge J, III, et al. Effect of facility on the operative costs of distal radius fractures. J Hand Surg Am. 2011;36(7):1142-1148. doi: 10.1016/j.jhsa.2011.03.042. [DOI] [PubMed] [Google Scholar]
- 6. Goodman AD, Modest JM, Johnson JP, et al. Implant charge differences between distal radius fixation constructs (CPT 25607, 25608, and 25609). HAND. 2020. doi: 10.1177/1558944720963927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Okelana AB, McMillan LJ, Kibble K, et al. Variation in implant selection for ankle fractures. J Orthop Trauma. 2019;33:S26-S31. doi: 10.1097/BOT.0000000000001623. [DOI] [PubMed] [Google Scholar]
- 8. Virkus WW, Wetzel RJ, McKinley TO, et al. Costs and radiographic outcomes of rotational ankle fractures treated by orthopaedic surgeons with or without trauma fellowship training. J Am Acad Orthop Surg. 2018;26(12):e261-e268. doi: 10.5435/JAAOS-D-16-00687. [DOI] [PubMed] [Google Scholar]
- 9. Huetteman H, Zhong L, Chung KC. Cost of surgical treatment for distal. J Hand Surg Am. 2018;43(8):720-730. doi: 10.1016/j.jhsa.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 10. Bhat SB, Liss FE, Beredjiklian PK. Economic analysis of the cost of implants used for treatment of distal radius fractures. Arch Bone Jt Surg. 2018;6(5):371-375. doi: 10.22038/abjs.2017.23467.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Childs S, Mann T, Dahl J, et al. Differences in the treatment of distal radius fractures by hand fellowship trained surgeons: a study of ABOS candidate data. J Hand Surg Am. 2017;42(2):e91-e97. doi: 10.1016/j.jhsa.2016.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Navarro CM, Brolund A, Ekholm C, et al. Treatment of radius or ulna fractures in the elderly: a systematic review covering effectiveness, safety, economic aspects and current practice. PLoS ONE. 2019;14(3):e0214362. doi: 10.1371/journal.pone.0214362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Toon DH, Premchand RAX, Sim J, et al. Outcomes and financial implications of intra-articular distal radius fractures: a comparative study of open reduction internal fixation (ORIF) with volar locking plates versus nonoperative management. J Orthop Traumatol. 2017;18(3):229-234. doi: 10.1007/s10195-016-0441-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pang EQ, Truntzer J, Baker L, et al. Cost minimization analysis of the treatment of distal radial fractures in the elderly. Bone Joint J. 2018;100(2):205-211. doi: 10.1302/0301-620X.100B2.BJJ-2017-0358.R1. [DOI] [PubMed] [Google Scholar]
- 15. Costa ML, Achten J, Plant C, et al. UK DRAFFT: a randomised controlled trial of percutaneous fixation with Kirschner wires versus volar locking-plate fixation in the treatment of adult patients with a dorsally displaced fracture of the distal radius. Health Technol Assess (Rockv). 2015;19(17):1-124. doi: 10.3310/hta19170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kazmers NH, Judson CH, Presson AP, et al. Evaluation of factors driving cost variation for distal. J Hand Surg Am. 2018;43:606-614.e1. doi: 10.1016/j.jhsa.2018.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Basu A, Manning WB. Issues for the next generation of health care cost analyses. Med Care. 2009;47:S109-S114. doi: 10.1097/MLR.0b013e31819c94a1. [DOI] [PubMed] [Google Scholar]
- 18. Arora V, Moriates C, Shah N. The challenge of understanding health care costs and charges. AMA J Ethics. 2015;17(11):1046-1052. doi: 10.1001/journalofethics.2015.17.11.stas1-1511. [DOI] [PubMed] [Google Scholar]
- 19. US Bureau of Labor Statistics. CPI inflation calculator. Date unknown. https://www.bls.gov/data/inflation_calculator.htm. Accessed October 25, 2020.
- 20. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613-619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 21. Physician Fee Schedule Search. Date unknown. https://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx. Accessed October 24, 2020.
- 22. Tubeuf S, Yu G, Achten J, et al. Cost effectiveness of treatment with percutaneous Kirschner wires versus volar locking plate for adult patients with a dorsally displaced fracture of the distal radius: analysis from the drafft trial. Bone Joint J. 2015;97-B(8):1082-1089. doi: 10.1302/0301-620X.97B8.35234. [DOI] [PubMed] [Google Scholar]
- 23. Nandyala SV, Giladi AM, Parker AM, et al. Comparison of direct perioperative costs in treatment of unstable distal radial fractures. J Bone Jt Surg. 2018;100(9):786-792. doi: 10.2106/JBJS.17.00688. [DOI] [PubMed] [Google Scholar]
- 24. Kakarlapudi TK, Santini A, Shahane SA, et al. The cost of treatment of distal radial fractures. Injury. 2000;31(4):229-232. doi: 10.1016/S0020-1383(99)00248-X. [DOI] [PubMed] [Google Scholar]
- 25. Kazmers NH, Presson AP, Xu Y, et al. Cost implications of varying the surgical technique, surgical setting, and anesthesia type for carpal tunnel release surgery. J Hand Surg Am. 2018;43(11):971-977. doi: 10.1016/j.jhsa.2018.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Crawford DC, Li CS, Sprague S, et al. Clinical and cost implications of inpatient versus outpatient orthopedic surgeries: a systematic review of the published literature. Orthop Rev (Pavia). 2015;7(4):6177. doi: 10.4081/or.2015.6177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Johnson DJ, Greenberg SE, Sathiyakumar V, et al. Relationship between the Charlson Comorbidity Index and cost of treating hip fractures: implications for bundled payment. J Orthop Traumatol. 2015;16:209-213. doi: 10.1007/s10195-015-0337-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lalonde D, Martin A. Tumescent local anesthesia for hand surgery: improved results, cost effectiveness, and wide-awake patient satisfaction. Arch Plast Surg. 2014;41(4):312-316. doi: 10.5999/aps.2014.41.4.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tang JB, Xing SG, Ayhan E, et al. Impact of wide-awake local anesthesia no tourniquet on departmental settings, cost, patient and surgeon satisfaction, and beyond. Hand Clin. 2019;35(1):29-34. doi: 10.1016/j.hcl.2018.08.012. [DOI] [PubMed] [Google Scholar]
- 30. Goz V, Rane A, Abtahi AM, et al. Geographic variations in the cost of spine surgery. Spine (Phila Pa 1976). 2015;40(17):1380-1389. doi: 10.1097/BRS.0000000000001022. [DOI] [PubMed] [Google Scholar]
- 31. Thakore RV, Greenberg SE, Bulka CM, et al. Geographic variations in hospital charges and Medicare payments for major joint arthroplasty. J Arthroplasty. 2015;30(5):728-732. doi: 10.1016/j.arth.2014.12.011. [DOI] [PubMed] [Google Scholar]
- 32. Fisher ES, Wennberg DE, Stukel TA, et al. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138(4):273-287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 33. Veltre DR, Yakavonis M, Curry EJ, et al. Regional variations of Medicare physician payments for hand surgery procedures in the United States. Hand (N Y). 2019;14(2):209-216. doi: 10.1177/1558944717734370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sun E, Baker LC. Concentration in orthopedic markets was associated with a 7 percent increase in physician fees for total knee replacements. Health Aff (Millwood). 2015;34(6):916-921. doi: 10.1377/hlthaff.2014.1325. [DOI] [PubMed] [Google Scholar]
- 35. Zhang H, Cowling DW, Facer M. Comparing the effects of reference pricing and centers-of-excellence approaches to value-based benefit design. Health Aff. 2017;36(12):2094-2101. doi: 10.1377/hlthaff.2017.0563. [DOI] [PubMed] [Google Scholar]
- 36. Morche J, Mathes T, Pieper D. Relationship between surgeon volume and outcomes: a systematic review of systematic reviews. Syst Rev. 2016;5(1):204. doi: 10.1186/s13643-016-0376-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Day CS, Alexander M, Lal S, et al. Effects of workers’ compensation on the diagnosis and surgical treatment of patients with hand and wrist disorders. J Bone Joint Surg Am. 2010;92(13):2294-2299. doi: 10.2106/JBJS.I.00158. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-han-10.1177_15589447221077379 for Charges for Distal Radius Fracture Fixation Are Affected by Fracture Pattern, Location of Service, and Anesthesia Type by Avi D. Goodman, Peter Brodeur, Aristides I. Cruz, Lindsay R. Kosinski, Edward Akelman and Joseph A. Gil in HAND