Abstract
Background:
Arthroscopic and open surgical procedures are commonly used to repair distal radioulnar joint (DRUJ) instability. Both may result in patient dissatisfaction and recurrence of DRUJ instability. An alternative treatment that yields improved outcomes is a limited open approach using a bone anchor to support the DRUJ.
Methods:
A retrospective chart review of 58 patients (59 extremities) aged 18 to 60 years with type 1B Palmer rupture (3 months or more after injury) of the triangular fibrocartilage complex (TFCC) without distal radius fracture was conducted. Inclusion criteria are: 3 to 12 months after injury, clinical DRUJ instability, and minimum of 6 months of postoperative follow-up. Operative fixation with Stryker Sonic or Depuy Mitek anchor was done by the same surgeon using a limited open procedure. Preoperative and postoperative assessments included Disability of the Arm, Shoulder, and Hand; Brief Pain Inventory; Wong-Baker FACES Pain Rating Scale; Numeric Pain Scale; range of motion; and recurrence of instability. A multivariate analysis of variance model was fit to imputed data to assess the effect of both anchors.
Results:
Clinical and statistical differences were found in preoperative and postoperative assessments for either the Stryker Sonic or the Depuy Mitek anchor but not between anchor types. There was no recurrence after 3 years with either anchor.
Conclusion:
Patients requiring TFCC repair using the Stryker Sonic or Depuy Mitek anchor experienced: (1) significant clinical and statistical improvement in postoperative assessments; (2) patient satisfaction; and (3) corrected DRUJ instability. Consequently, major determinants in deciding which bone anchor to use may be based on cost or surgeon’s preference.
Keywords: wrist, anatomy, fracture/dislocation, diagnosis, outcomes, surgery, specialty, treatment, research and health outcomes
Introduction
The stability of the distal radioulnar joint (DRUJ) is maintained by the integrity of both bone and the surrounding soft tissue structures. Although isolated injuries are common, DRUJ instability typically occurs because of fractures in the distal radius with an incidence from 10% to 19%.1-4 In contrast, the incidence of triangular fibrocartilage complex (TFCC) injury in distal radius fractures is from 30% to 70%. 5 Injury to the TFCC is the most common wrist ligament injury and a common source of ulnar wrist pain. 6 Depending on the severity of trauma, TFCC injury can lead to DRUJ instability due to its role in load transmission and stabilization of the ulnar side of the radiocarpal joint and the DRUJ. A mild injury is typically referred to as a wrist sprain, whereas a more significant injury can lead to disabling conditions in the wrist. Traumatic injuries commonly occur due to a fall onto an outstretched hand while in pronation, resulting in forced axial loading or compression of the wrist. A TFCC tear occurs when sufficient force is transmitted through the ulnar side of the outstretched wrist. People at an increased risk of traumatic tears of the TFCC include tennis players, gymnasts, and people who use power drills. Degenerative injuries more commonly occur in older populations, due to the natural thinning of soft tissues, and can occur with minimum force or trauma. Repetitive pronation with the palm in a downward position may also be a higher risk factor for degenerative changes.
Surgical treatment of DRUJ instability remains a challenge for hand surgeons because of the incidence of recurrent instability after the treatment, specifically after chronic injuries. Different surgical techniques have been described to treat TFCC injuries. These include arthroscopic-assisted repair, open repair, and limited open repair.
Advocates for an arthroscopic-assisted repair point out the advantages of direct visualization of the injury, smaller incision with less destruction of surrounding structures, faster functional recovery, and fewer complications. 6
Although arthroscopic debridement to scope and debride damaged tissue may be sufficient for simple tears, for more severe TFCC injuries, such as those with subluxation greater than 50% at the DRUJ or if a fracture occurs, open repair techniques may be required. Open repair gives the surgeon a better view of and access to the damaged area and may be more effective for severe tears that require reattachment with repair sutures and hardware to hold the repaired tissue in place while it heals. However, open repair might lead to higher rates of extensor carpi ulnaris (ECU) tendinitis and neuroma of the dorsal cutaneous branch, possibly due to the larger incision adjacent to the tendon sheets and capsule. 6
In a clinical comparison of arthroscopic and open techniques, the common complications were recurrent DRUJ instability (13% with arthroscopic repair and 21% with open surgery repair), superficial nerve neuritis, and ECU tendinitis. 2
An alternative treatment for TFCC injuries that yields improved outcomes is a limited open approach using a bone anchor to provide adequate pull-out strength to support the DRUJ. The limited open approach allows more accurate placement of an anchor such as Stryker Sonic and Depuy Mitek.7,8 The Stryker Sonic anchor is a bioresorbable implant designed to aid the reattachment of soft tissue to bone and is a relatively new method for treatment of TFCC injuries with limited reports on its use in the literature. The Depuy Mitek anchor has been commercially available longer than the Stryker Sonic anchor and has been widely used in open procedures of the foot, ankle, knee, hand, wrist, shoulder, and elbow.
There are no reports in the literature that compare the clinical outcomes of different types of anchors used with the limited open surgical repair in patients with chronic DRUJ instability. This report compares assessments that measure: (1) disability and pain with the Disability of the Arm, Shoulder, and Hand (DASH) questionnaire; 9 (2) the psychosocial impact of pain using the Brief Pain Inventory (BPI); 10 and (3) the level of pain with the Wong-Baker FACES Pain Rating Scale (WBFPS) 11 and Numeric Pain Scale, 12 as well as range of motion (ROM) and recurrence of instability in patients who have undergone the limited open surgical repair of a type 1B Palmer tear of the TFCC, without distal radius fractures, using either the Stryker Sonic or the Depuy Mitek anchor.
Anatomy and Classification
The DRUJ places the hand in a specific position that allows for rotation of the forearm and wrist to perform different tasks. The stability of the DRUJ is provided by the interactions between ligaments, muscles, bones, and soft tissues surrounding the joint. The structures that help stabilize the DRUJ are the TFCC, ulnocarpal ligament (UCL) complex, ECU tendon/sheath, pronator quadratus (PQ) muscle, interosseous membrane (IOM) including the interosseous ligament (IOL), the bone itself, and the joint capsule. 13 Passive and active stabilizers contribute to the stability of the DRUJ, allowing it complete 150° of pronation and supination. Failure of one or more of these stabilizers may lead to DRUJ instability or dislocation. 14 The joint capsule, UCLs, TFCC, and distal portion of the IOM have been characterized as passive stabilizers, whereas the PQ and ECU are considered dynamic stabilizers during pronation and supination. Although the capsule and UCLs, specifically the ulnotriquetral and ulnolunate ligaments, do not have a significant biomechanical role, cadaveric studies have shown that repairing the joint capsule restores motion when in pronation and supination. 14 The TFCC is a cartilaginous structure located on the ulnar side of the wrist and is composed of the triangular fibrocartilage discus, the radioulnar ligaments (RULs), and the UCLs. 15 The dorsal and palmar RULs provide most of the stability to the DRUJ, whereas bony structures provide 20% of the stability. 16 The RULs attach to the distal radius and insert on the ulna at the styloid and the fovea. 17 The foveal insertion of the TFCC is important because of its key role in stabilizing the DRUJ and the ulnocarpal joint.
A classification system proposed by Andrew Palmer divides TFCC lesions into categories based on type of injury. Traumatic tears were classified as type 1 injuries and degenerative tears as type 2.3,18 Traumatic tears were further categorized based on the location of the injury, whereas degenerative tears were subclassified based on the extent of degeneration. As an example, type 1B injuries consist of traumatic tears involving the periphery of the TFCC and may be associated with an ulnar styloid fracture. 18 These criteria help create a consistent approach to each patient when deciding on the most appropriate treatment. The criteria were also used as the guidelines followed in this study. Maintaining a constant approach to each patient helps standardize the injuries and allows for a better comparison between outcomes.
Limited Open Surgical Technique
The limited open surgical technique allows for access to the fovea and uses the distal styloid of the ulna as a landmark for the incision. The incision is made along the long access of the ulna, dorsally and down the distal styloid, parallel to the ECU, measuring 6 to 7 cm and short of the tip of the styloid process, to prevent injury to the dorsal cutaneous branch of the ulnar nerve. Reinforcement of the dorsal RULs is obtained using local tissue from the subsheath of the ECU. The TFCC is anchored to the fovea, under direct visualization and 6× power loupes magnification (for easier identification of anatomical landmarks), with 1 of the 2 anchors and 2 to 4 fiber wire sutures. Once complete, the incision is then sutured in layers and immobilized in a posterior splint in supination. Figure 1 shows placement of the anchors.
Figure 1.
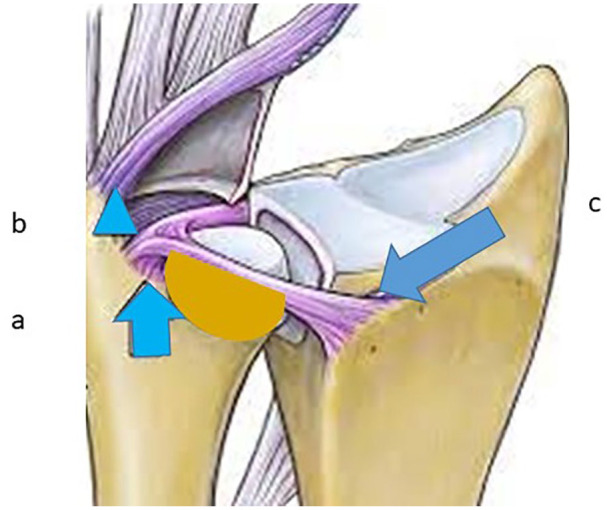
Placement of the Anchors.
Note. (a) Anchor 1 at the fovea centered at the point where previously fibers of the ligament were originating. (b) Rarely a second anchor may be necessary for reinsertion of the ulnar triquetral ligament. (c) Palmar distal radioulnar joint ligament. Figure adapted by permission from Springer Nature Archives of Orthopedic and Trauma Surgery. 19
Materials and Methods
This study was conducted as a retrospective review of previously collected prospective data. Following institutional review board approval, we identified 58 patients (59 extremities) who underwent surgical intervention with a limited open surgical procedure using either the Stryker Sonic or the Depuy Mitek anchor to repair a type 1B Palmer tear of the TFCC (neutral or negative ulnar variance). All patients included in this analysis were operated on specifically for DRUJ instability and by the same surgeon to minimize differences in surgical technique. The key determinant in diagnosing DRUJ instability focused on identifying RUL ruptures at the lateral attachment to the fovea, as the deep portion of the RULs acts as the primary stabilizer of the DRUJ. 20 After the anchor was implanted, the patients were expected to immobilize the treated wrist for 3 weeks, followed by gentle immobilization for 3 weeks and then strengthening therapy for 12 to 16 weeks. The key inclusion criteria for this retrospective analysis were 3 to 12 months after injury, clinical instability of the DRUJ, use of either the Stryker Sonic anchor or the Depuy Mitek anchor to repair the injury, and follow-up with a minimum of 6 months postoperatively. The only exclusion criterion was that the wrist had been previously injured. Preoperative and postoperative measurements included DASH, 9 BPI, 10 WBFPS, 11 Numeric Pain Scale, 12 as well as ROM and DRUJ instability. Postoperative follow-up evaluations were taken from 6 months to 3 years after surgical repair of the injury. Postoperative data from each group were compared to assess the difference in outcomes between the anchors.
Statistical Analysis
The statistical analysis consisted of a multivariate analysis of variance model that was fit to the imputed data to assess the effect of anchor type (University of Texas El Paso Statistical Consulting Lab). The statistical significance level was .01. Power calculations were done using medium and large effect sizes of 24% and 67%, respectively, for Cohen’s f on a 2-factor analysis of variance.
Results
Of the 58 patients included in this analysis, the Stryker Sonic anchor was used to repair the TFCC tear in 15 patients between 2005 and 2018, and the Depuy Mitek anchor was used to treat 33 patients between 1998 and 2017.
Activity and Function
Analyses of recorded data sets for the 59 extremities showed a significant clinical and statistical difference in preoperative to postoperative measures for each anchor type when evaluating return to activity (Table 1). The average preoperative results for DASH and BPI prior to receiving the Stryker Sonic bone anchor were 60 and 38, respectively, compared with average postoperative scores of 58 (P < .01) for DASH and 27 (P < .01) for BPI. For patients with the Depuy Mitek bone anchor, the average preoperative score for DASH was 83 and 58 for BPI. In reviewing patient postoperative data, an improvement was seen in DASH (n = 42; P < .01) and BPI (n = 17; P < .01). No clinical or statistical differences were observed between the Stryker Sonic and Depuy Mitek anchors when comparing only postoperative activity and function as assessed by DASH (P = .028) and BPI (P = .047) (Table 2).
Table 1.
Preoperative and Postoperative Outcomes With Bone Anchors in the Management of Distal Radioulnar Joint Instability.
| Assessment | Stryker Sonic anchor | Depuy Mitek anchor | ||||
|---|---|---|---|---|---|---|
| Preoperative (n = 34) | Postoperative (n = 34) | P value* | Preoperative (n = 25) | Postoperative (n = 25) | P value* | |
| DASH | 60 | 58 | <.01 | 83 | 42 | <.01 |
| BPI | 38 | 27 | <.01 | 58 | 17 | <.01 |
| WBFPS | 4 | 2 | <.01 | 4 | 2 | <.01 |
| Numeric Pain Scale | 6 | 3 | <.01 | 7 | 2 | <.01 |
Note. DASH = Disability of the Arm, Shoulder, and Hand; BPI = Brief Pain Inventory; WBFPS = Wong-Baker FACES Pain Rating Scale.
Statistical testing was completed using the multivariate analysis of variance. Statistical significance level (α) equals .01.
Table 2.
Comparison of Postoperative Assessments of the Stryker Sonic Bone Anchor and Depuy Mitek Anchor.
| Assessment | Stryker Sonic anchor Postoperative (n = 34) |
Depuy Mitek anchor Postoperative (n = 25) |
P value* |
|---|---|---|---|
| DASH | 58 | 42 | .028 |
| BPI | 27 | 17 | .047 |
| WBFPS | 2 | 2 | .429 |
| Numeric Pain Scale | 3 | 2 | .339 |
Note. DASH = Disability of the Arm, Shoulder, and Hand; BPI = Brief Pain Inventory; WBFPS = Wong-Baker FACES Pain Rating Scale.
Statistical testing was completed using the multivariate analysis of variance. Statistical significance (α) set at P < .01.
Pain
There were significant clinical and statistical differences with respect to pain when preoperative and postoperative measures of both anchor groups were compared. For patients with the Stryker Sonic bone anchor, the average preoperative pain scores, measured by WBFPS and the Numeric Pain Scale, were 4 and 6, respectively (Table 1). In the postoperative evaluations, taken at a minimum of 6 months postoperatively, the pain score improved to 2 with the WBFPS (P < .01) and 3 with the Numeric Pain Scale (P < .01). In patients with the Depuy Mitek bone anchor, the average preoperative WBFPS was 4, and it was 7 for the Numeric Pain Scale. In the postoperative data set, the pain score improved to 2 with both the WBFPS (P < .01) and the Numeric Pain Scale (P < .01). No clinical or statistical differences were observed when comparing only postoperative pain results between patients with either the Stryker Sonic or the Depuy Mitek bone anchor, as measured with the WBFPS (P = .429) and Numeric Pain Scale (P = .339) (Table 2).
Range of Motion
The measurement of movement of each wrist was done by determining the degree of pronation, supination, flexion, extension, radial deviation, and ulnar deviation. The preoperative and postoperative measurements of each type of movement were statistically significant (P < .01) for wrists with either the Stryker Sonic anchor or the Depuy Mitek anchor.
Discussion
In this retrospective study, we compared the Stryker Sonic and Depuy Mitek bone anchors in patients who underwent the repair of type 1B Palmer tear of the TFCC, with neutral or negative ulnar variance, using the limited open surgical approach. To the best of our knowledge, this report is the first to show the comparison between the Stryker Sonic and Depuy Mitek bone anchors for the repair of TFCC injury using the limited open surgical approach. The patient outcomes reported here were better than those published in the literature in terms of recurrence of instability.
We found significant clinical and statistical differences between the preoperative and postoperative assessments of function and pain (DASH), the psychosocial impact of pain (BPI), pain (WBFPS and Numeric Pain Scale), and ROM for both anchors; however, between anchor types, differences in the postoperative assessments were not significant. In addition, 3 years after repair of the TFCC injury, there was no recurrence of instability, and there was improvement in all measured parameters.
The pull-out strength of an anchor should provide adequate strength to support the DRUJ. The natural pull-out strength of the DRUJ ligaments has a mean from 26 N/mm to 29 N/mm. 21 The mean pull-out strength of the anchors used in this study exceeds that of the natural pull-out strength with 222 N for the Stryker Sonic anchor and 58 N for the Depuy Mitek anchor. 22
After treatment, the patients were advised to immobilize the surgical site to prevent disturbance of the healing process and avoid implant failure.
The limited open repair technique described in this study avoids many of the complications that occur with arthroscopic and open approaches with reports of 97.9% satisfactory results at 3 years from the DASH, BPI, and pain scales.
Conclusion
In the repair of TFCC injury, the limited open approach using either the Stryker Sonic or the Depuy Mitek bone anchor resulted in significant clinical and statistical differences between preoperative and postoperative assessments of function, pain, and ROM and a higher incidence of satisfactory results (97.9%) with no recurrence of DRUJ instability 3 years postoperatively. When deciding which anchor to use, personal preference by the surgeon or availability may influence that decision. Furthermore, costs and insurance coverage may affect the patient’s decision when choosing between the 2 anchors, with the cost of Sonic anchors nearly double that of the Mitek anchor. The limited open surgical approach with the Stryker Sonic or the Depuy Mitek anchor bone may guide the future for the repair of TFCC injuries.
Acknowledgments
The authors thank Dr Amy Wagler, Director, Statistical Consulting Lab, The University of Texas at El Paso, El Paso, Texas
Footnotes
Authors’ Note: Manuscript editing services were provided by Christine Kuepfer, Medical Editor. It was funded by Dr Jose Monsivais.
Ethical Approval: Ethical approval was provided by Burrell College of Medicine Institutional Review Board (IRB # 0020_2017).
Statement of Human and Animal Rights: All human and animal studies have been approved by the Burrell College of Medicine, Las Cruces, New Mexico.
Statement of Informed Consent: This was a retrospective review of previously collected prospective data. Hence, informed consent was not required.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Jose J. Monsivais  https://orcid.org/0000-0002-4519-5409
https://orcid.org/0000-0002-4519-5409
References
- 1. Mirghasemi AR, Lee DJ, Rahimi N, et al. Distal radioulnar joint instability. Geriatr Orthop Surg Rehabil. 2015;6(3):225-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Anderson ML, Larson AN, Moran SL, et al. Clinical comparison of arthroscopic versus open repair of triangular fibrocartilage complex tears. J Hand Surg Am. 2008;33(5):675-682. [DOI] [PubMed] [Google Scholar]
- 3. Atzei A. New trends in arthroscopic management of type 1-B TFCC injuries with DRUJ instability. J Hand Surg Eur Vol. 2009;34(5):582-591. [DOI] [PubMed] [Google Scholar]
- 4. Kazemian GH, Bakhshi H, Lilley M, et al. DRUJ instability after distal radius fracture: a comparison between cases with and without ulnar styloid fracture. Int J Surg. 2011;9(8):648-651. [DOI] [PubMed] [Google Scholar]
- 5. Bucholz RW, Heckman JD, Court-Brown C. Rockwood and Green’s Fractures in Adults. Philadelphia: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 6. Andersson JK, Åhlén M, Andernord D. Open versus arthroscopic repair of the triangular fibrocartilage complex: a systematic review. J Exp Orthop. 2018;5(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Stryker. SonicAnchor Bioresorbable Anchoring system. https://footankle.stryker.com/en/products/soft-tissue/sonicanchor. Accessed December 30, 2020.
- 8. Depuy Mitek. Small joint anchors with Orthocord. http://prod.mitek.depuy.edgesuite.net/PDFsforWebsite/900979.pdf. Accessed December 30, 2020.
- 9. The DASH outcome measure—disabilitites of the arm, shoulder and hand. https://dash.iwh.on.ca/about-dash. Accessed December 30, 2020.
- 10. Bonafé FSS, de Campos LA, Marôco J, et al. Brief Pain Inventory: a proposal to extend its clinical application. Eur J Pain. 2019;23(3):565-576. [DOI] [PubMed] [Google Scholar]
- 11. Wong-Baker Faces Pain Rating Scale. https://wongbakerfaces.org/. Accessed December 30, 2020.
- 12. Haefeli M, Elfering A. Pain assessment. Eur Spine J. 2006;15(Suppl. 1):S17-S24. doi: 10.1007/s00586-005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Haugstvedt JR, Langer MF, Berger RA. Distal radioulnar joint: functional anatomy, including pathomechanics. J Hand Surg Eur Vol. 2017;42(4):338-345. [DOI] [PubMed] [Google Scholar]
- 14. Marès O. Distal radioulnar joint instability. Hand Surg Rehabil. 2017;36(5):305-313. [DOI] [PubMed] [Google Scholar]
- 15. Kleinman WB. Stability of the distal radioulna joint: biomechanics, pathophysiology, physical diagnosis, and restoration of function what we have learned in 25 years. J Hand Surg Am. 2007;32(7):1086-1106. [DOI] [PubMed] [Google Scholar]
- 16. Carlsen BT, Dennison DG, Moran SL. Acute dislocations of the distal radioulnar joint and distal ulna fractures. Hand Clin. 2010;26(4):503-516. [DOI] [PubMed] [Google Scholar]
- 17. Ahsan ZS, Yao J. Complications of wrist arthroscopy. Arthroscopy. 2012;28(6):855-859. [DOI] [PubMed] [Google Scholar]
- 18. Atzei A, Luchetti R. Foveal TFCC tear classification and treatment. Hand Clin. 2011;27(3):263-272. [DOI] [PubMed] [Google Scholar]
- 19. Spies CK, Langer M, Muller LP, et al. Distal radioulnar joint instability: current concepts of treatment. Arch Orthop Trauma Surg. 2020;140:639-650. [DOI] [PubMed] [Google Scholar]
- 20. Omokawa S, Iida A, Kawamura K, et al. A biomechanical perspective on distal radioulnar joint instability. J Wrist Surg. 2017;6(2):88-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schuind F, An KN, Berglund L, et al. The distal radioulnar ligaments: a biomechanical study. J Hand Surg Am. 1991; 16(6):1106-1114. [DOI] [PubMed] [Google Scholar]
- 22. Wehner T, Jimenez S, Homeier A. Mechanical Performance of the SonicAnchor. Schönkirchen, Germany: Stryker, Trauma & Extremities, Stryker Trauma GmbH; 2016. [Google Scholar]


