Abstract
Aims
To evaluate the burden of cardiovascular risk factors and disease (CVD) among five Asian groups living in Catalonia (Spain): Indian, Pakistani, Bangladeshi, Filipino, and Chinese.
Methods and results
Retrospective cohort study using the Catalan Health Surveillance System database including 42 488 Pakistanis, 40 745 Chinese, 21 705 Indians, 9544 Filipinos, and 6907 Bangladeshis; and 5.3 million native individuals (‘locals’). We estimated the age-adjusted prevalence (as of 31 December 2019) and incidence (during 2019) of diabetes, hypertension, hyperlipidaemia, obesity, tobacco use, coronary heart disease (CHD), cerebrovascular disease, atrial fibrillation, and heart failure (HF). Bangladeshis had the highest prevalence of diabetes (17.4% men, 22.6% women) followed by Pakistanis. Bangladeshis also had the highest prevalence of hyperlipidaemia (23.6% men, 18.3% women), hypertension among women (24%), and incident tobacco use among men. Pakistani women had the highest prevalence of obesity (28%). For CHD, Bangladeshi men had the highest prevalence (7.3%), followed by Pakistanis (6.3%); and Pakistanis had the highest prevalence among women (3.2%). For HF, the prevalence in Pakistani and Bangladeshi women was more than twice that of locals. Indians had the lowest prevalence of diabetes across South Asians, and of CHD across South Asian men, while the prevalence of CHD among Indian women was twice that of local women (2.6% vs. 1.3%). Filipinos had the highest prevalence of hypertension among men (21.8%). Chinese men and women had the lowest prevalence of risk factors and CVD.
Conclusions
In Catalonia, preventive interventions adapted to the risk profile of different Asian immigrant groups are needed, particularly for Bangladeshis and Pakistanis.
Keywords: Cardiovascular disease, Coronary heart disease, Diabetes mellitus, Hypertension, Risk factors, South Asian
Introduction
With a population of 4.7 billion, Asia is home to more than 60% of humankind.1 Besides the Asian continent, many countries around the world including various European nations have large, rapidly growing communities of people of Asian ancestry.2-5 The size and rate of expansion of these populations has triggered interest in gaining a detailed understanding of their cardiovascular risk profile, as this knowledge can inform tailored preventive interventions and the allocation of healthcare resources.
Importantly, Asian subgroups are diverse, and there is substantial variation in their cardiovascular risk profile. Studies in Europe have demonstrated that immigrants of South Asian ancestry are at increased risk of diabetes and coronary heart disease (CHD) compared to East Asian immigrants and local Whites.6-10 However, differences in cardiovascular risk between large South Asian subgroups (Indian, Pakistani, and Bangladeshi) remain unexplored in many countries. In the United Kingdom (UK), Pakistanis and Bangladeshi men carry a higher cardiovascular risk than other South Asian subgroups.6 Nevertheless, whether these trends in the UK (where South Asian migration has been happening for more than three generations) are generalizable to other European nations, where this phenomenon is more recent and the socioeconomic profiles of South Asian immigrants may be distinct, is unknown. Granular information of South Asian subgroups can help develop targeted public health and individual-level preventive interventions in areas in which these communities are large.
Data on the burden of cardiovascular disease (CVD) in Filipino and Chinese immigrants are also scarce in Europe. The American Heart Association recommends using disaggregated data of Asian subgroups to better define their unique health characteristics.11 Catalonia (in Northeastern Spain) has large populations of first-generation immigrants from several Asian nations.12 All residents have access to high-quality universal public healthcare, and the local healthcare databases capture exhaustive health information for all. The aim of this study was thus to use data from the healthcare databases of Catalonia to compare the prevalence and incidence of risk factors and CVD among first-generation immigrants from five Asian groups: Indian, Pakistani, Bangladeshi, Filipino, and Chinese.
Methods
Data source
The present study was conducted using 2019 data from the Catalan Health Surveillance System (CHSS), the automated administrative healthcare database of the Health Department of Catalonia. This exhaustive, quality-controlled database includes all legal residents in Catalonia, regardless of whether they actively use the public healthcare system or not, and captures any healthcare-related information generated by the interactions between each of them and the local public healthcare system. This includes detailed information on medical diagnoses, which are coded using the International Classification of Diseases, 9th Edition, Clinical Modification (ICD 9-CM), 10th Edition (ICD-10), and 10th Edition Clinical Modification (ICD 10-CM); and medication use, which is coded using the Anatomical Therapeutic. Chemical (ATC) Classification System; among other characteristics. Although the primary use of the CHSS is for administrative and evaluation purposes, since 2011 the database has also been used extensively for population-based epidemiological research.10,13,14
Study population
For the present analysis, we included all residents from Catalonia who were 18 years of age or older as of 31 December 2019 and were either born in any of the Asian countries listed below, or anywhere in Catalonia/Spain [from now on, the latter group (those born in Catalonia/Spain) will be referred to as ‘locals’]. Information on country of origin was available from the local Census, which was linked to the CHSS. Five groups of first-generation Asian immigrants were defined: Indian, Pakistani, Bangladeshi, Filipino, and Chinese. Individuals from other Asian countries were very few (<6000 in total, and <2000 for each individual country) and were not included in the analysis.
Study design and relevant variables
This was a retrospective cohort study evaluating the prevalence and incidence of cardiovascular risk factors and clinically overt CVD. The cardiovascular risk factors evaluated included diabetes, hypertension, hyperlipidaemia, obesity, and tobacco use; and the cardiovascular conditions assessed were CHD, cerebrovascular disease, atrial fibrillation, and heart failure (HF). Supplementary material online, Table S1 lists the specific ICD-9-CM codes used to identify each diagnosis; all ICD-10 and ICD-10-CM codes were mapped to ICD-9-CM codes.
Statistical analyses
The demographic characteristics of each group (Indian, Pakistani, Bangladeshi, Filipino, Chinese, and locals) were described using summary statistics, and comparisons across groups were conducted using chi-squared tests and analysis of variance, as appropriate. We also used population pyramids to generate a granular, visual description of the sex and age distribution of the study population by area of origin.
We calculated the age-standardized prevalence of each cardiovascular risk factor and CVD among men and women using the World Health Organization 2000–2025 world standard population.15 The prevalence of each cardiovascular risk factor and condition was also described for each group by sex and 10-year age strata, computed as the number of individuals with recorded evidence of each characteristic (using all historical information recorded in the CHSS until 31 December 2019), divided by the total number of individuals within each group (as of 31 December 2019); and expressed as number per 1000 people. Incidence estimations were also stratified by sex and age and were computed as the number of new cases (between 1 January and 31 December 2019), per 1000 individuals at risk as of 1 January 2019.
Finally, the mean age at the first recording in the CHSS database of each cardiovascular risk factor and condition was computed by area of origin, as a proxy of age at diagnosis. All analyses were conducted using R software.
Research ethics
The study used de-identified data routinely collected for administrative, benchmarking, and other purposes. For these reasons, the requirement for written informed consent was waived.
Results
Study population
The analysis included 5 432 353 adult residents in Catalonia who were born in either any of the five relevant Asian regions, or locally. Table 1 and Supplementary material online, Figure S1 present the demographic characteristics of the six study groups. Specifically, the study included 42 488 Pakistanis, 40 745 Chinese, 21 705 Indians, 9544 Filipinos, 6907 Bangladeshis, and more than 5.3 million locals. Filipinos had the highest proportion of women (60.4%), while South Asians were predominantly men. South Asians were the youngest, particularly Bangladeshis.
Table 1.
Demographic characteristics of the study participants, Catalan Health Surveillance System database 2019
| N | Pakistani 42 488 |
Chinese 40 745 |
Indian 21 705 |
Filipino 9544 |
Bangladeshi 6907 |
Local 5 310 964 |
|---|---|---|---|---|---|---|
| Age, years | 37.0 (11.0) | 41.1 (12.4) | 36.2 (11.0) | 41.8 (12.7) | 34.3 (8.97) | 51.8 (18.6) |
| Sex | ||||||
| Men | 31 679 (74.6%) | 19 391 (47.6%) | 14 236 (65.6%) | 3777 (39.6%) | 5083 (73.6%) | 2 554 304 (48.1%) |
| Women | 10 809 (25.4%) | 21 354 (52.4%) | 7469 (34.4%) | 5767 (60.4%) | 1824 (26.4%) | 2 756 660 (51.9%) |
Results presented as mean (standard deviation) or number (%). Asian groups are sorted by population size.
Cardiovascular risk factors
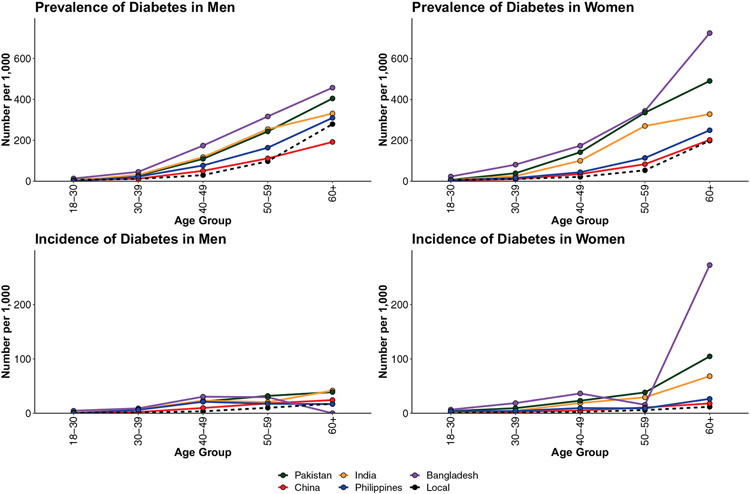
The results for burden of cardiovascular risk factors are presented in Table 2, Figures 1-3 and Supplementary material online, Figures S2-S6. South Asians had the highest age-adjusted prevalence of diabetes in both men and women. In both sex groups, the highest prevalence was observed for Bangladeshis [17.4% among men, prevalence ratio (PR) of 2.5 compared to local men; 22.6% among women, PR of 4.9 compared to local women]; followed by Pakistanis. Absolute and relative differences between national groups were larger among women. Analyses stratified by age and sex are presented in Figure 1.
Table 2.
Age-standardized prevalence (%) of cardiovascular risk factors and diseases, by sex and area of origin
| Pakistani | Chinese | Indian | Filipino | Bangladeshi | Local | |
|---|---|---|---|---|---|---|
| Men | ||||||
| Risk factors | ||||||
| Diabetes | 13.8 | 6.6 | 12.5 | 9.8 | 17.4 | 7.0 |
| Hypertension | 14.6 | 11.8 | 20.6 | 21.8 | 19.1 | 17.0 |
| Hyperlipidaemia | 14.2 | 9.8 | 14.5 | 15.9 | 23.6 | 15.3 |
| Obesity | 11.0 | 3.1 | 9.5 | 7.5 | 7.7 | 14.3 |
| Tobacco use | 16.5 | 13.3 | 6.1 | 15.9 | 20.3 | 23.4 |
| Cardiovascular disease | ||||||
| Coronary heart disease | 6.3 | 1.8 | 3.6 | 2.5 | 7.3 | 3.3 |
| Cerebrovascular disease | 2.3 | 1.8 | 2.0 | 2.2 | 1.7 | 2.6 |
| Heart failure | 1.5 | 0.5 | 1.0 | 1.1 | 0.8 | 1.3 |
| Atrial fibrillation | 1.2 | 0.7 | 0.4 | 1.6 | 0.2 | 2.1 |
| Women | ||||||
| Risk factors | ||||||
| Diabetes | 16.9 | 6.1 | 12.4 | 7.5 | 22.6 | 4.6 |
| Hypertension | 18.3 | 12.0 | 19.4 | 19.8 | 24.0 | 14.0 |
| Hyperlipidaemia | 10.8 | 8.3 | 10.8 | 11.9 | 18.3 | 13.1 |
| Obesity | 28.8 | 2.9 | 19.9 | 6.9 | 22.6 | 16.2 |
| Tobacco use | 0.6 | 1.4 | 0.6 | 3.9 | 0.8 | 18.6 |
| Cardiovascular disease | ||||||
| Coronary heart disease | 3.2 | 1.0 | 2.6 | 1.1 | 2.1 | 1.3 |
| Cerebrovascular disease | 2.2 | 1.4 | 2.2 | 1.4 | 1.4 | 2.1 |
| Heart failure | 2.2 | 0.5 | 1.4 | 0.5 | 2.1 | 1.0 |
| Atrial fibrillation | 1.2 | 0.6 | 0.6 | 0.6 | 0.4 | 1.3 |
Results presented as age-standardized prevalence in %. Groups sorted by population size. All groups were standardized to the World Health Organization world population for 2000–2025. Cells shaded in grey represent the group with the highest age-standardized prevalence for each risk factor or disease.
Figure 1.
Prevalence and incidence of diabetes, by sex, age, and area of origin.
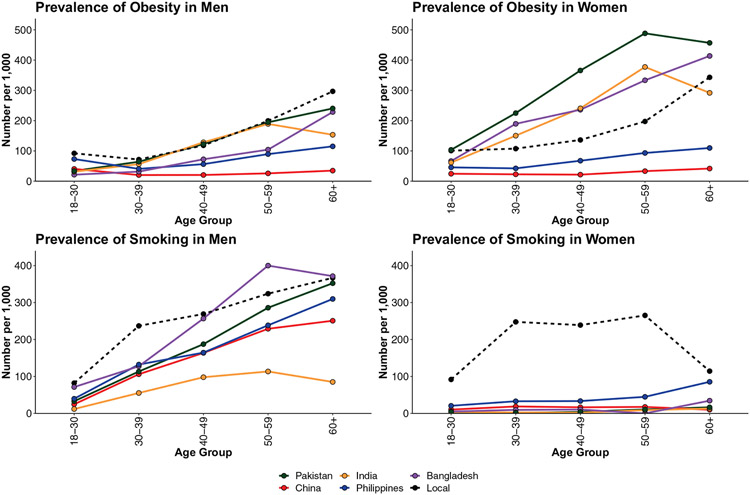
Figure 3.
Prevalence of obesity and smoking, by sex, age, and area of origin.
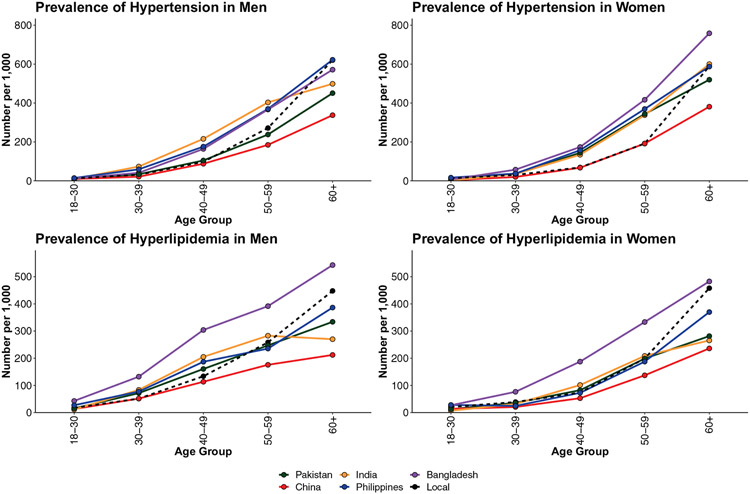
Filipinos had the highest the age-adjusted prevalence of hypertension among men, followed by Indians. Among women, Bangladeshis had the highest prevalence, followed by Filipinas and Indians. Bangladeshis had the highest age-adjusted prevalence of hyperlipidaemia in both sex groups, the difference with locals being large both among men (PR 1.5) and among women (PR 1.4). For all other Asian groups, the age-adjusted prevalence of hyperlipidaemia was similar or lower than among locals.
Among men, locals had the highest prevalence of obesity, although between ages 30 and 60 years, Indians and Pakistanis had a very similar prevalence to that of locals. Pakistani women had the highest age-adjusted prevalence of obesity, followed by Bangladeshi and Indian women. The high burden of obesity among South Asian women, particularly Pakistanis, compared with the local population was evident since early ages, both in terms of prevalence and incidence. For instance, the incidence of obesity among Pakistani women aged 40–49 years was almost six-fold that of locals. Locals had the highest age-adjusted prevalence of tobacco use in both men and women. Among men, Bangladeshis ranked second highest, while among women, tobacco use was very low in all Asian groups. In analyses stratified by age, Bangladeshi men ranked highest in prevalence of tobacco use between ages 50 and 69 years. Bangladeshi men also had the highest incidence of tobacco use in all age groups.
Coronary heart disease
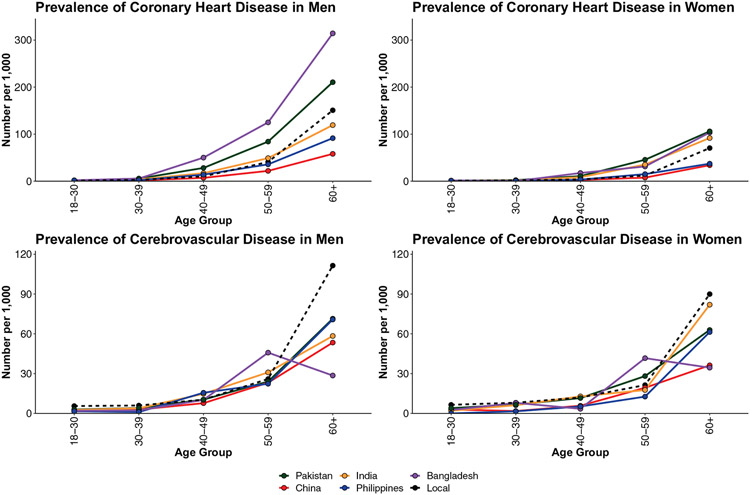
South Asians had the highest age-adjusted prevalence of CHD in both men and women (Table 2 and Supplementary material online, Figure S7). Among men, Bangladeshis ranked highest (PR 2.2 compared with locals), followed by Pakistanis (PR 1.9). On the other hand, the prevalence among Indian men was very close to that of the local population. Among women, Pakistanis ranked highest (PR 2.5) followed by Indian women (PR 2.0). In both sex groups, the prevalence of CHD in Filipinos and Chinese was lower than among locals. Differences between groups in terms of prevalence and incidence of CHD were evident as early as at age 40 years in both men and women Figure 4 and Supplementary material online, Figure S8).
Figure 4.
Prevalence of coronary heart disease and cerebrovascular disease, by sex, age, and area of origin.
Other cardiovascular disease
Absolute differences in the burden of cerebrovascular disease, atrial fibrillation and HF were smaller between groups than for CHD (Table 2 and Figure 4 and Supplementary material online, Figure S7-S11). However, for HF, Pakistani women had a 2.2 age-adjusted PR compared with locals, and this was 2.1 for Bangladeshi women compared with locals. Pakistanis ranked highest in burden of HF among men.
Age at diagnosis
Mean age at first recording in the database was lowest in Bangladeshis for all cardiovascular risk factors and CVDs evaluated (Supplementary material online, Table S2). While Indians ranked second youngest at first recording of most risk factors, Pakistanis ranked second youngest for all CVD.
Discussion
Our study using disaggregated 2019 data for more than 121 000 first-generation immigrants from five Asian groups living in Catalonia allowed to uncover important patterns in terms of burden of risk factors and CVD in each group. Specifically, we observed that (i) all Asian groups evaluated, with the exception of Chinese individuals, had a high burden of cardiovascular risk factors, and (ii) that despite some common patterns, particularly the high prevalence of diabetes across South Asian groups, Asian immigrants in Catalonia comprise a heterogeneous set of populations, each with a unique risk profile. To the best of our knowledge, this is the first disaggregated, population-based analysis of its kind conducted in a European country outside of the UK. Our observations may be used to inform tailored prevention efforts in areas with large South Asian populations, adapted to the characteristics of each country of origin16; as well as in regions with large populations of Filipino immigrants.
In our study, Bangladeshis had the highest prevalence of diabetes, hyperlipidaemia and CHD among men, as well as of diabetes, hyperlipidaemia, and hypertension among women. In the British QRISK3 study, which used population-level data for ~8 million people in the derivation cohort, including more than 320 000 South Asians, Hippisley-Cox et al.6 also identified Bangladeshis as the highest-risk South Asian men subgroup. Specifically, their multivariable-adjusted hazard ratio (HR) for CVD events in QRISK3 was 1.70 compared with British White men (95% confidence interval 1.61 to 1.79), followed by Pakistanis (HR 1.62) and Indians (HR 1.30). Small studies in the USA and Asia also found a younger age of onset and lower body mass index at the time of a first diagnosis of myocardial infarction in Bangladeshis compared with Whites, as well as a higher prevalence of triple vessel disease.17,18
In terms of potential upstream factors underlying CVD risk in Bangladeshis, particularly among men, studies in the UK showed that Bangladeshis had the lowest educational attainment and employment, and the highest levels of smoking and alcohol use.19,20 In our study, Bangladeshi men had the highest prevalence of tobacco use between ages 50 and 69 years—a critical age for the development of CVD events. Moreover, the incidence of newly recorded tobacco use in the CHSS database was higher in Bangladeshis than in any other group, at all ages. UK Bangladeshis have also been reported to have a lower health literacy regarding CHD and diabetes when compared with other groups.19,20 This should be assessed in Spain and other areas and if confirmed, acted upon. Another important finding of our study was the high prevalence of hyperlipidaemia in this group, often unnoticed when Bangladeshis are collapsed with other South Asian subgroups in epidemiological studies.10 Prior studies in the UK showed Bangladeshis having a higher prevalence of abnormal total: HDL cholesterol ratio and abnormal triglyceride levels compared with Pakistanis and Indians.19,21-23
Very few studies have looked at the effect of Bangladeshi diets, exercise, and health behaviours on cardiovascular risk factors. Grace24 evaluated this in a representative sample of British Bangladeshis. Many believed that a healthy diet and lifestyle were important and aligned with religious teachings. Rice, lentils (Dhal) were staple, with one to two portions being the norm. However, it was considered rude to not serve large portions of high fat and flavoured food to guests. Traditional Bangladeshi fruit and vegetable intake was expensive, so people often relied on fast food, rather than on cheaper healthy local alternatives. Physical exercise, as defined in the western sense (running/working out in a gymnasium) posed challenges, especially for women for whom cultural expectations complicated physical activity in mixed sex exercise classes.24 Importantly, health professionals caring for these people did not feel comfortable delivering culturally sensitive lifestyle advice to the Bangladeshi population.24
The consistency of our results with other similar observations across countries stresses the need for aggressive preventive interventions in areas with large Bangladeshi populations—in Spain, other European countries, and most likely elsewhere. Importantly, culturally adapted lifestyle interventions tailored for this population have demonstrated success in improving health behaviours and diabetes-related outcomes.25 Achieving a better understanding of the intersection of socioeconomic determinants, cultural factors, and gender norms may help in designing most tailored interventions to reduce CVD in this group.
In our study, Pakistani women had the highest prevalence of obesity and of all CVDs (expect for atrial fibrillation) across all women groups. This included a strikingly high age-adjusted prevalence of obesity and of diabetes, and a 2.5-fold higher prevalence of CHD than locals. Pakistanis also ranked highest in prevalence of obesity and HF among men. In QRISK-3, Pakistani women had the highest multivariable-adjusted risk of CVD events across all groups evaluated.6 Also, in a 2004 analysis of the Health Survey for England, Pakistani women had a higher prevalence of obesity, type 2 diabetes, and increased waist size compared with Indian and Bangladeshi women.26 Our observations highlight the increased cardiovascular risk of Pakistani immigrants compared to a mostly White Mediterranean population, particularly among women. Pakistanis represent the largest South Asian population in Catalonia, Spain, and Greece, and comprise large groups in the UK and Germany.16 These communities should be targeted aggressively as part of primordial and primary CVD prevention efforts—particularly in women’s health initiatives. As with Bangladeshis, gaining an understanding of the intersection between contextual factors (socioeconomic, cultural, gender norms) may help in designing interventions, both at the individual and at the population-level.
The increased risk for cardio-metabolic disease and CVD in Pakistanis likely starts in childhood, with ethnic differences being described in the relationship between insulin resistance and obesity in boys aged 8–11 years.27 However, the contribution of lifestyles later in life to CVD risk is likely to also be critical. Food practices in Pakistanis are often interwoven with a strong sense of hospitality, with certain calorie-rich foods being essential to be a part of the community.28 Furthermore, their health literacy regarding healthy eating practices may be low, as observed in a Norwegian study of Pakistani women in 2010.29 Similarly, while Pakistani women in England considered exercise important, most felt they were engaging in adequate exercise with housework. In the same study, men felt they were too busy working to allocate separate time for exercise.30,31 Pakistani women living in England often did not perceive themselves as overweight even if body mass index calculations showed otherwise; and in fact, being overweight was sometimes viewed as an indicator of good health.30
In our study, Indians had the lowest burden of diabetes and tobacco use among South Asians. This may explain their lowest burden of CHD among all South Asian men groups, which was similar to that of local men. Other studies have also reported a lower prevalence of diabetes among Indian immigrants compared with immigrants from Pakistan, Bangladesh, and Sri Lanka.32-35 However, there is heterogeneity in the risk of diabetes even among Indian immigrants, depending on the area they migrated from.35 In the UK, proposed reasons for a lower risk among Indians compared with other South Asian groups include higher education, higher mean income, and higher levels of physical activity than other groups.19,36 There is also a possibility of religion-based differences in dietary practices and physical activity when Indians are compared with Pakistani and Bangladeshi immigrants.37 Despite this, it must be noted that in our study, Indians had a high prevalence of diabetes and hypertension in both men and women, and of obesity and established CVD among women. Therefore, countries with large populations of mostly Indian South Asians, such as the USA, the UK, Germany, and France,16 should still pursue aggressive public health and preventive interventions targeting these communities.
Filipino men had the highest prevalence of hypertension among all groups evaluated. This points to the need for targeted preventive interventions especially focused on preventing the onset of hypertension, its screening, and optimizing blood pressure control. Finally, our results for Chinese men and women showed a low prevalence of most risk factors and CVDs evaluated, typically lower than the local population and often the lowest among all six groups. The low prevalence of CHD in this population is consistent with data from the UK and other prior reports.6 Development of risk estimators that account for country of origin, such as QRISK3, in Catalonia and other European regions with large Asian populations may help inform more accurate prevention interventions in these individuals.
Study limitations
Some study limitations should be discussed. The challenges derived from using administrative healthcare databases such as the CHSS to evaluate the cardiovascular health of populations and the incidence and prevalence of risk factors and CVD have been discussed elsewhere.10 Unnoticed risk factors and subclinical forms of disease may not be detected among individuals not interacting with the health system, and even among those, risk factors and subclinical disease will often be missed. This may result in potential underestimation, particularly among immigrants, some of whom tend to use the public healthcare system less often than non-immigrants. In addition, individuals with a shorter length of stay within a territory (e.g. many immigrant residents) may accrue less historical information in databases such as the CHSS than individuals with a longer length of stay. This can result in an underestimation of the prevalence of some diagnoses. In this context, incidence estimations, which inform about newly recorded cases in the database, provide valuable complementary information, although subclinical forms would not be detected either. Prior studies confirm that risk factors such as diabetes are often underdiagnosed in minority groups,38 meaning that the high prevalence observed in some Asian groups in our study could actually be higher. It is also very plausible that the prevalence of obesity may have been underestimated in all Asian groups, as the use of Asian-specific body mass index cut-offs for Asian populations may not be implemented systematically in Catalonia. Information on abdominal obesity, a highly prevalent risk factor in South Asians, was not available.
Undocumented immigrants would not be captured in the database—although this group is expected to be small in Catalonia given the advantages of legal residency and of having access to the local universal healthcare system.10 Also, the analysis classified participants on the basis of country of origin. Therefore, any second-generation people of Asian ancestry would have been included in the local group. However, because Asian immigration to Catalonia is a relatively recent phenomenon, this is likely to have had minimal impact in our analyses. Information on length of stay in Catalonia was not available, which precluded evaluating the effect of Mediterranean acculturation in each group. The Mediterranean diet includes cardiovascular-healthy features such as frequent use of extra virgin olive oil and other healthy sources of fat,39 and whether prolonged exposure to this dietary pattern has health benefits in Asian subgroups at increased cardiovascular risk will require further research.
Though our study did not assess socio-economic status, area of residence, or other socioeconomic determinants of health, Bangladeshi immigrants to Spain are concentrated in low-wage service sector occupations. Future research should therefore examine the role of socioeconomic drivers of CVD in this population. Still, the higher burden of risk factors observed in Bangladeshis is consistent with the findings from INTERHEART,40 as well as with studies in the UK that adjusted for differences in area of residence.6 Also, prior analyses of multiple immigrant groups including people from countries with lower gross domestic product than South Asia suggest, together with the cultural practices described above, that socioeconomic factors may not fully explain the excess burden of CVD in South Asians.
Conclusions
In Catalonia, preventive interventions adapted to the risk profile of different Asian immigrant groups are needed, particularly for Bangladeshis and Pakistanis. Further research is needed to better understand the cultural and socioeconomic drivers of these differences.
Supplementary Material
Figure 2.
Prevalence of hypertension and hyperlipidaemia, by sex, age, and area of origin.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. U.B. received support from the National Institue of Health under grant DP5OD26429.
Footnotes
Supplementary material
Supplementary material is available at European Journal of Preventive Cardiology online.
Conflict of interest: S.S.V.: Research support from the Department of Veterans Affairs, World Heart Federation, and Tahir and Jooma Family, and Honoraria from the American College of Cardiology. The other authors declare that they have no conflicts of interest relevant to the content of this manuscript.
Data availability statement
Study data generated using the CHSS health database from the Government of Catalunya. The raw data is not publicly available, however, summary statistics supporting the findings of this study are available from the corresponding author [M.C.A] on request.
References
- 1.Worldometer. Asia Population 2021. https://www.worldometers.info/world-population/asia-population/ (12 January 2021). [Google Scholar]
- 2.UK Parliament. House of Commons Library. Migration Statistics. https://commonslibrary.parliament.uk/research-briefings/sn06077/#:~:text=In%202019%20there%20were%20approximately,live%20in%20the%20capital%20city (12 January 2021). [Google Scholar]
- 3.Statista. Number of foreigners in Germany from 2017 to 2019, by country of origin. https://www.statista.com/statistics/890277/foreigner-numbers-by-country-of-origin-germany/ (12 January 2021).
- 4.Instituto Nazionale di Statistica. Comunicato Stampa. Cittadini Non Comunitari In Italia. https://www.istat.it/it/archivio/249445 (12 January 2021). [Google Scholar]
- 5.Instituto Nacional de Estadistica. Población extranjera por Nacionalidad, comunidades, Sexo y Año. https://www.ine.es/jaxi/Tabla.htm?path=/t20/e245/p08/l0/&file=02005.px&L=0 (12 January 2021).
- 6.Hippisley-Cox J, Coupland C, Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ 2017;357:j2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fedeli U, Avossa F, Ferroni E, Schievano E, Bilato C, Modesti PA, Corti MC. Diverging patterns of cardiovascular diseases across immigrant groups in Northern Italy. Int J Cardiol 2018;254:362–367. [DOI] [PubMed] [Google Scholar]
- 8.McKeigue PM, Marmot MG. Mortality from coronary heart disease in Asian communities in London. BMJ 1988;297:903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Regidor E, Astasio P, Calle ME, Martínez D, Ortega P, Domínguez V. The association between birthplace in different regions of the world and cardiovascular mortality among residents of Spain. Eur J Epidemiol 2009;24:503–512. [DOI] [PubMed] [Google Scholar]
- 10.Cainzos-Achirica M, Vela E, Cleries M, Bilal U, Mauri J, Pueyo MJ, Rosas A, Enjuanes C, Blaha MJ, Kanaya AM, Comin-Colet J… Cardiovascular risk factors and disease among non-European immigrants living in Catalonia. Heart 2019;105:1168–1174. [DOI] [PubMed] [Google Scholar]
- 11.Palaniappan LP, Araneta MRG, Assimes TL, Barrett-Connor EL, Carnethon MR, Criqui MH, Fung GL, Narayan KMV, Patel H, Taylor-Piliae RE, Wilson PWF, Wong ND; Council on Cardiovascular Nursing. Call to action: cardiovascular disease in Asian Americans: a science advisory from the American Heart Association. Circulation 2010;122:1242–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gencat. La immigració en xifres. Monogràfic de la Secretaria d’lgualtat, Migracions i Ciutadania. https://treballiaferssocials.gencat.cat/ca/ambits_tematics/immigracio/dades/la-immigracio-en-xifres/(12 January 2021). [Google Scholar]
- 13.Comín-Colet J, Verdú-Rotellar JM, Vela E, Clèries M, Bustins M, Mendoza L, Badosa N, Cladellas M, Ferré S, Bruguera J; working group of the Integrated Program for Heart Failure Management of the Barcelona Litoral Mar Integrated Health Care Area, Spain. Efficacy of an integrated hospital-primary care program for heart failure: a population-based analysis of 56,742 patients. Rev Esp Cardiol (Engl Ed) 2014;67:283–293. [DOI] [PubMed] [Google Scholar]
- 14.Cainzos-Achirica M, Capdevila C, Vela E, Cleries M, Bilal U, Garcia-Altes A, Enjuanes C, Garay A, Yun S, Farre N, Corbella X, Comin-Colet J. Individual income, mortality and healthcare resource use in patients with chronic heart failure living in a universal healthcare system: a population-based study in Catalonia, Spain. Int J Cardiol 2019;277:250–257. [DOI] [PubMed] [Google Scholar]
- 15.NIH. National Cancer Institute. World (WHO 2000-2025) Standard. https://seer.cancer.gov/stdpopulations/world.who.html (12 January 2021).
- 16.Cainzos-Achirica M, Fedeli U, Sattar N, Agyemang C, Jenum AK, McEvoy JW, Murphy JD, Brotons C, Elosua R, Bilal U, Kanaya AM, Kandula NR, Martinez-Amezcua P, Comin-Colet J, Pinto X. Epidemiology, risk factors, and opportunities for prevention of cardiovascular disease in individuals of South Asian ethnicity living in Europe. Atherosclerosis 2019;286:105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silbiger JJ, Ashtiani R, Attari M, Spruill TM, Kamran M, Reynolds D, Stein R, Rubinstein D. Atheroscerlotic heart disease in Bangladeshi immigrants: risk factors and angiographic findings. Int J Cardiol 2011;146:e38–e40. [DOI] [PubMed] [Google Scholar]
- 18.Vasudev R, Shah P, Patel J, Naranjo M, Hosein K, Rampal U, Patel H, Bu J, Roy J, Guragai N, Bhandari P, Virk H, Shamoon F, Bikkina M. Should Bangladeshi race be considered as an independent risk factor for multi vessel coronary artery disease? Vasc Health Risk Manag 2020;16:143–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bhopal R, Unwin N, White M, Yallop J, Walker L, Alberti KG, Harland J, Patel S, Ahmad N, Turner C, Watson B, Kaur D, Kulkarni A, Laker M, Tavridou A. Heterogeneity of coronary heart disease risk factors in Indian, Pakistani, Bangladeshi, and European origin populations: cross sectional study. BMJ 1999;319:215–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rankin J, Bhopal R. Understanding of heart disease and diabetes in a South Asian community: cross-sectional study testing the ‘snowball’ sample method. Public Health 2001;115:253–260. [DOI] [PubMed] [Google Scholar]
- 21.Agyemang C, Bhopal RS. Is the blood pressure of South Asian adults in the UK higher or lower than that in European white adults? A review of cross-sectional data. J Hum Hypertens 2002;16:739–751. [DOI] [PubMed] [Google Scholar]
- 22.Battu HS, Bhopal R, Agyemang C. Heterogeneity in blood pressure in UK Bangladeshi, Indian and Pakistani, compared to White, populations: divergence of adults and children. J Hum Hypertens 2018;32:725–744. [DOI] [PubMed] [Google Scholar]
- 23.Modesti PA, Fedeli U. Coronary heart disease among non-Western immigrants in Europe. In: Modesti P, Cappuccio F, Parati G (eds), Ethnic Diversities, Hypertension and Global Cardiovascular Risk Springer, Cham.; 2018. pp. 61–73. [Google Scholar]
- 24.Grace C. Nutrition-related health management in a Bangladeshi community. Proc Nutr Soc 2011;70:129–134. [DOI] [PubMed] [Google Scholar]
- 25.Islam NS, Wyatt LC, Taher MD, Riley L, Tandon SD, Tanner M, Mukherji BR, Trinh-Shevrin C. A culturally tailored community health worker intervention leads to improvement in patient-centered outcomes for immigrant patients with type 2 diabetes. Clin Diabetes 2018;36:100–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Becker E, Boreham R, Chaudhury M, Craig R, Deverill C, Doyle M, Erens B, Falaschetti E, Fuller E, Hills A.. Health Survey for England 2004—The Health of Minority Ethnic Groups London: The Information Centre; 2006. pp. 1–444. [Google Scholar]
- 27.Whincup PH, Gilg JA, Papacosta O, Seymour C, Miller GJ, Alberti KGMM, Cook DG. Early evidence of ethnic differences in cardiovascular risk: cross sectional comparison of British South Asian and white children. BMJ 2002;324:635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lawton J, Ahmad N, Hanna L, Douglas M, Bains H, Hallowell N. ‘We should change ourselves, but we can’t’: accounts of food and eating practices amongst British Pakistanis and Indians with type 2 diabetes. Ethn Health 2008;13:305–319. [DOI] [PubMed] [Google Scholar]
- 29.Råberg Kjøllesdal MK, Hjellset VT, Bjørge B, Holmboe-Ottesen G, Wandel M. Perceptions of risk factors for diabetes among Norwegian-Pakistani women participating in a culturally adapted intervention. Ethn Health 2011;16:279–297. [DOI] [PubMed] [Google Scholar]
- 30.Ludwig AF, Cox P, Ellahi B. Social and cultural construction of obesity among Pakistani Muslim women in North West England. Public Health Nutr 2011;14:1842–1850. [DOI] [PubMed] [Google Scholar]
- 31.Lawton J, Ahmad N, Hanna L, Douglas M, Hallowell N. ‘I can’t do any serious exercise’: barriers to physical activity amongst people of Pakistani and Indian origin with Type 2 diabetes. Health Educ Res 2006;21:43–54. [DOI] [PubMed] [Google Scholar]
- 32.Holland AT, Wong EC, Lauderdale DS, Palaniappan LP. Spectrum of cardiovascular diseases in Asian-American racial/ethnic subgroups. Ann Epidemiol 2011;21:608–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harding S, Rosato M, Teyhan A. Trends for coronary heart disease and stroke mortality among migrants in England and Wales, 1979-2003: slow declines notable for some groups. Heart 2008;94:463–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anand SS, Yusuf S, Vuksan V, Devanesen S, Teo KK, Montague PA, Kelemen L, Yi C, Lonn E, Gerstein H, Hegele RA, McQueen M. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic groups (SHARE). Lancet 2000;356:279–284. [DOI] [PubMed] [Google Scholar]
- 35.Banerjee AT, Shah B. One size does not fit all: diabetes prevalence among immigrants of the South Asian Diaspora [published online ahead of print, 2020 Sep 29]. J Immigr Minor Health 2020;doi: 10.1007/s10903-020-01093-4. [DOI] [PubMed] [Google Scholar]
- 36.Bhopal R, Hayes L, White M, Unwin N, Harland J, Ayis S, Alberti G. Ethnic and socioeconomic inequalities in coronary heart disease, diabetes and risk factors in Europeans and South Asians. J Public Health Med 2002;24:95–105. [DOI] [PubMed] [Google Scholar]
- 37.Hirode G, Vittinghoff E, Bharmal NH, Kandula NR, Kanaya AM. The association of religious affiliation with cholesterol levels among South Asians: the Mediators of Atherosclerosis in South Asians Living in America study. BMC Cardiovasc Disord 2019;19:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cheng YJ, Kanaya AM, Araneta MRG, Saydah SH, Kahn HS, Gregg EW, Fujimoto WY, Imperatore G. Prevalence of diabetes by race and ethnicity in the United States, 2011-2016. JAMA 2019;322:2389–2398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Estruch R, Ros E, Salas-Salvadó J, Covas M-I, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutérrez V, Fiol M, Lapetra J, Lamuela-Raventos RM, Serra-Majem L, Pintó X, Basora J, Muñoz MA, Sorlí JV, Martínez JA, Fitó M, Gea A, Hernán MA, Martí-nez-González MA; PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med 2018;378:e34. [DOI] [PubMed] [Google Scholar]
- 40.Joshi P, Islam S, Pais P, Reddy S, Dorairaj P, Kazmi K, Pandey MR, Haque S, Mendis S, Rangarajan S, Yusuf S. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA 2007;297:286–294. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Study data generated using the CHSS health database from the Government of Catalunya. The raw data is not publicly available, however, summary statistics supporting the findings of this study are available from the corresponding author [M.C.A] on request.