Abstract
This study aimed to evaluate the effects of bystander cardiopulmonary resuscitation (CPR) and dispatcher-assisted CPR (DA-CPR) on outcomes after out-of-hospital cardiac arrest (OHCA). We conducted a prospective observational study using the Korean Cardiac Arrest Research Consortium registry database and enrolled adults aged > 20 years who sustained OHCA. The study population comprised 13,864 patients from October 1, 2015, to June 30, 2021. All enrolled patients were transported to the emergency room and resuscitated by the emergency medical personnel. Patients with terminal illnesses, pregnancy, “do not resuscitate” cards, and insufficient recorded information were excluded. Good neurologic outcomes were noted in 6.5%, 9.9%, and 9.6% of patients in the “no bystander”, “standard bystander”, and “compression-only bystander” CPR groups, respectively, and differed significantly (p < 0.001). Survival to discharge differed significantly (p < 0.001) between groups at 10.8%, 13.1%, and 13.2%, respectively. In a multivariable model, the interaction between “compression-only” and DA-CPR showed a positive effect on good neurological outcomes and survival to discharge with an odds ratio of 1.93 (Confidence interval, CI 1.28–2.91, p = 0.002) and 1.74 (CI 1.24–2.44, p = 0.001), respectively. In conclusion, the interaction between compression-only CPR and DA-CPR is significantly associated with good neurological and survival outcomes after OHCA. Education for bystanders and dispatchers should adhere to the current guidelines to improve outcomes among OHCA victims.
Subject terms: Health care, Medical research
Introduction
Out-of-hospital cardiac arrest (OHCA) is a global public health problem with a low survival rate. Survival rates vary between communities but generally range between 5 and 10%1–4. From the perspective of the prehospital system to manage OHCAs, the role of the bystander and emergency medical services (EMS) is crucial. Therefore, international guidelines highly recommend cardiopulmonary resuscitation (CPR) initiated by bystanders and continued by EMS5–7. However, it remains debated how bystanders can be encouraged to provide immediate CPR. Although there is no doubt that early CPR performed by bystanders is important, there are factors hindering bystanders from attempting resuscitation, such as fear, cultural aspects, and a lack of confidence regarding CPR8–10. Dispatcher-assisted CPR (DA-CPR) was introduced in 2010 to overcome these problems11. In this study, we aimed to evaluate the effects of bystander CPR methods and DA-CPR, on neurological and survival outcomes after OHCA.
Methods
Korean EMS system
The EMS system in Korea is a public fire department-based system operated by the government. Partially dual-dispatch ambulances (BLS-fire engine, ACLS-ambulances) are dispatched for each OHCA case from regional EMS agencies. Emergency Medical Technicians in Korea provide basic to intermediate levels of service, equivalent to the EMT-basic and EMT-intermediate levels of the North American EMS. EMS dispatch and on-scene management are provided under the national EMS protocol. The National Emergency Management Agency has developed and implemented a DA-CPR protocol since August 2012. The protocol includes two key questions regarding mental status and respiration for recognising cardiac arrest. If the answers to both questions are “no response” and “abnormal respiration”, respectively, the dispatcher instructs callers to perform chest compression-only CPR if standard CPR cannot be performed independently. A declaration of death at the scene is prohibited unless the patient has obvious signs of death. This declaration is only to be carried out under direct medical control by an EMS physician on duty at a dispatch centre. Therefore, most patients with OHCA are transported to an eligible hospital for continuing CPR12,13.
Study population
We conducted a prospective observational study using the Korean Cardiac Arrest Research Consortium (KoCARC) registry database, a multicentre OHCA patient registry from 65 hospitals in the Republic of Korea (ClinicalTrials.gov, NCT03222999). This database was developed in 2014 by a collaborative research network of clinicians to coordinate research on OHCA14. Researchers collected OHCA cases in a web-based electronic database registry using a standardised registry form based on the Utstein-style guidelines for the uniform reporting of cardiac arrest, including Utstein core elements and specific variables15. We enrolled adults aged > 20 years who had sustained an OHCA presumed to be of cardiac origin between October 1, 2015, and June 30, 2021. All enrolled patients were transported to the emergency room and resuscitated by the EMS. The exclusion criteria included patients with terminal illnesses; pregnant women; patients with “do not resuscitate” cards; cases of noncardiac OHCA caused by trauma, drowning, poisoning, burns, electrocution, or asphyxia; and those with insufficient information in their records.
Human ethical approval and informed consent
The requirement for informed consent was by the institutional review boards (IRBs) of the participating institutions (Seoul National University Hospital, Konkuk University Medical Center, Kyung Hee University Hospital, Korea University Guro Hospital, Korea University Anam Hospital, SMG-SNU Boramae Medical Center, Yonsei University Severance Hospital, Yonsei University Gangnam Severance Hospital, Hallym University Kangdong Sacred Heart Hospital, Hallym University Kangnam Sacred Heart Hospital, Hanyang University Seoul Hospital, Kyungpook National University Hospital, Chosun University Hospital, Seoul National University Bundang Hospital, Myongji Hospital, Korea University Ansan Hospital, Dongguk University Ilsan Hospital, Bundang Jesaeng Hospital, Wonkwang University Sanbon Hospital, Hallym University Dongtan Sacred Heart Hospital, Chungbuk National University Hospital, Soonchunhyang University Cheonan Hospital, Jeju National University Hospital, Hanyang University Guri Hospital, Gyeongsang National University Hospital, Ajou University Hospital, Pusan National University Yangsan Hospital, Ewha Womans University Mokdong Medical Center, Inha University Hospital, and Hallym University Sacred Heart Hospital). However, Samsung Medical Center, Asan Medical Center, Wonju Severance Christian Hospital and Incheon St. Mary’s Hospital received informed consent from individual participants for the follow-up survey of neurological outcomes and death. (The requirement for informed consent was waived for participants who did not need a telephone interview for the follow-up survey.) This study was approved by the Ethics Committee of Kangdong Sacred Heart Hospital (No. 2015–09-002). All methods were carried out in accordance with KoCARC research guidelines and regulations. In addition, the researchers used anonymised data and did not have access to any personal identifiers of the individuals in the registry.
Outcome variables
The primary outcome was the comparison among groups depending on the method of bystander CPR received: no bystander CPR, standard bystander CPR, or compression-only bystander CPR. The no bystander CPR group consisted of individuals who did not receive immediate chest compressions by bystanders at the scene. The standard bystander CPR group consisted of those who received chest compressions and ventilation from bystanders. The compression-only bystander CPR group consisted of those who received chest compressions without ventilation from bystanders.
The secondary outcomes were neurologic outcomes at discharge and survival to discharge. Neurologic outcomes were divided into good neurologic outcomes and poor neurologic outcomes, defined by CPC score. Good neurologic outcomes refer to a CPC score of 1 (good recovery) or 2 (moderate disability) on the five-category scale. Poor neurologic outcomes refer to a CPC score of 3 (severe disability), 4 (a vegetative state), or 5 (death)16,17.
Statistical analysis
The participants were divided into three groups according to the bystander CPR method received: “no attempt”, “standard” CPR, and “compression-only” CPR. Groups were compared using the chi-squared test for categorical variables and analysis of variance tests for continuous variables. Continuous variables were tested for normality using the Shapiro–Wilk test. A multivariable logistic regression analysis was conducted to estimate the effect of each bystander CPR method on neurological and survival outcomes, and the results were expressed as adjusted odds ratios (ORs) with 95% confidence intervals. The regression model was adjusted for the potential confounders of age, sex, history of diabetes and hypertension, the bystander CPR method, the attachment of an AED pad, place, type of initial ECG, and the provision of dispatch CPR. Interaction analyses were performed to investigate the relationship between bystander CPR method and the provision of DA-CPR. We used the Akaike information criterion (AIC) model selection to compare the multivariable analyses with and without the interaction. R (version 4.0, R Foundation for Statistical Computing) was used for all computational analyses. Statistical significance was defined as a two-tailed P-value of < 0.05.
Results
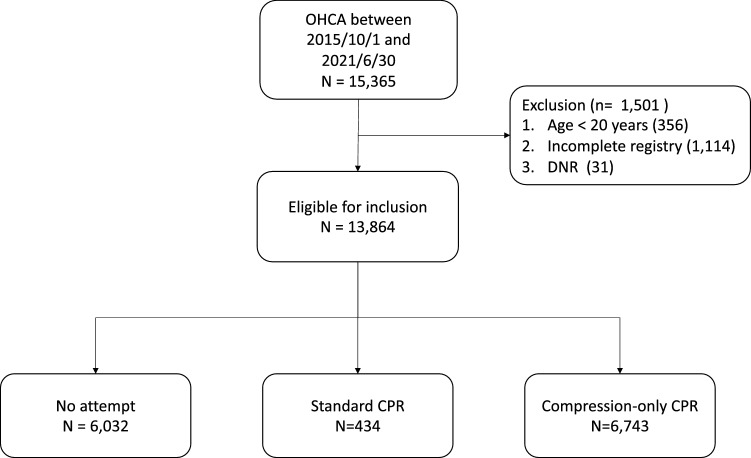
During the study period, 15,365 cardiac arrests occurred. Of these, 1501 cases were excluded because of blow age criteria, incomplete registry, and advanced directives. Finally, 13,864 patients met the inclusion criteria (Fig. 1). The study population was predominantly elderly, with more males than females (65.4%). The population had a low prevalence of diabetes and hypertension. “Standard” CPR, defined as performing chest compressions and delivering ventilation, was rarely started. On the contrary, half of the population received “compression-only” CPR. Most individuals resided in residence facilities. The automated external defibrillator (AED) was rarely applied at the scene. A shockable rhythm on the initial electrocardiogram (ECG) was observed in 18.5% of the study population, which consisted of 2367 cases of ventricular fibrillation and 81 cases of pulseless ventricular tachycardia compared to those of a non-shockable rhythm (3045 cases of pulseless electrical activity, 7758 cases of asystole). DA-CPR was provided for 73.6% of the study population. A good cerebral performance category (CPC) score of 1 or 2 and survival upon hospital discharge accounted for 8.1% and 12.1% of the population, respectively. This study adhered to the registered protocol. Nevertheless, some variables had missing values, ranging from 0.4 to 4.7% of the variable’s data (Table 1).
Figure 1.
Diagram of the study OHCA, Out-of-hospital cardiac arrest; DNR, do-not-resuscitate; CPR, Cardiopulmonary resuscitation.
Table 1.
General characteristics of study population.
| Variables | Missing | stats | |
|---|---|---|---|
| Age | Mean ± SD | 0 (0.0%) | 68.5 ± 15.4 |
| Sex | Female | 0 (0.0%) | 4798 (34.6%) |
| Male | 9066 (65.4%) | ||
| Diabetes | No | 0 (0.0%) | 10,731 (77.4%) |
| Yes | 3133 (22.6%) | ||
| Hypertension | No | 0 (0.0%) | 9455 (68.2%) |
| Yes | 4409 (31.8%) | ||
| Bystander witness | No | 0 (0.0%) | 6057 (43.7%) |
| Yes | 7807 (56.3%) | ||
| Bystander CPR | No CPR | 655 (4.7%) | 6032 (45.7%) |
| Standard CPR | 434 (3.3%) | ||
| Compression-only CPR | 6743 (51.0%) | ||
| AED | No | 49 (0.4%) | 12,662 (91.7%) |
| Yes | 1153 (8.3%) | ||
| Place | Non-residence | 238 (1.7%) | 4929 (36.2%) |
| Residence | 8697 (63.8%) | ||
| Initial ECG | Non-shockable | 613 (4.4%) | 10,803 (81.5%) |
| Shockable | 2448 (18.5%) | ||
| DA-CPR | No | 288 (2.1%) | 3579 (26.4%) |
| Yes | 9997 (73.6%) | ||
| CPC* | Poor | 0 (0.0%) | 12,740 (91.9%) |
| Good | 1124 (8.1%) | ||
| Survival to discharge | No | 0 (0.0%) | 12,184 (87.9%) |
| Yes | 1680 (12.1%) |
CPR Cardiopulmonary resuscitation; AED Automated electrical defibrillator; ECG Electrocardiography; DA-CPR Dispatcher-assisted CPR; CPC Cerebral Performance Category.
*A CPC score of 1 or 2 was considered a good neurological outcome, and a score of 3, 4, or 5 was considered a poor neurological outcome.
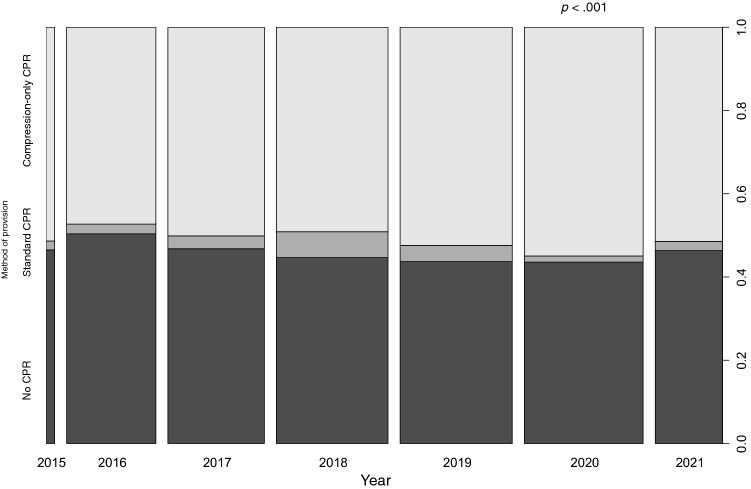
We investigated the association between bystander CPR performance and time (Fig. 2). The proportion of patients in the “compression-only” bystander CPR group significantly increased over the years (p < 0.001) compared to that in the no bystander CPR group and the standard bystander CPR group.
Figure 2.
The spine plot of the association test for the bystander CPR methods performed over the years. The horizontal axis chronologically describes the study period, with the width of the bar indicating the proportion of participants each year compared to the total number of participants. The vertical axis shows the bystander CPR method. There was a statistically significant difference in the proportion of compression-only CPR over the years compared to no bystander CPR and standard bystander CPR (p < .001).
Table 2 shows statistically significant differences among the three groups for all variables except for sex and medical history of diabetes. The “standard” bystander CPR group and “compression-only” CPR group were more likely to receive DA-CPR and have favourable clinical outcomes compared to that of the no bystander CPR group.
Table 2.
Comparison among groups depending on the method of CPR.
| Variables | No bystander CPR (N = 6032) | Standard bystander CPR (N = 434) | Compression-only CPR (N = 6743) | p | |
|---|---|---|---|---|---|
| Age | Mean ± SD | 69.1 ± 15.1 | 68.1 ± 15.8 | 68.2 ± 15.6 | .006 |
| Sex | Female | 2078 (34.4%) | 155 (35.7%) | 2332 (34.6%) | .865 |
| Male | 3954 (65.6%) | 279 (64.3%) | 4411 (65.4%) | ||
| Diabetes | No | 4672 (77.5%) | 340 (78.3%) | 5206 (77.2%) | .835 |
| Yes | 1360 (22.5%) | 94 (21.7%) | 1537 (22.8%) | ||
| Hypertension | No | 4186 (69.4%) | 297 (68.4%) | 4510 (66.9%) | .010 |
| Yes | 1846 (30.6%) | 137 (31.6%) | 2233 (33.1%) | ||
| Bystander witness | No | 2693 (44.6%) | 144 (33.2%) | 2927 (43.4%) | < .001 |
| Yes | 3339 (55.4%) | 290 (66.8%) | 3816 (56.6%) | ||
| AED | No | 5266 (87.4%) | 391 (90.1%) | 6450 (95.7%) | < .001 |
| Yes | 758 (12.6%) | 43 (9.9%) | 289 (4.3%) | ||
| Place | Non-residence | 2332 (39.2%) | 190 (44.7%) | 2188 (32.8%) | < .001 |
| Residence | 3624 (60.8%) | 235 (55.3%) | 4482 (67.2%) | ||
| Initial ECG | Non-shockable | 4954 (86.1%) | 288 (75.4%) | 5141 (78.2%) | < .001 |
| Shockable | 801 (13.9%) | 94 (24.6%) | 1436 (21.8%) | ||
| DA-CPR | No | 2733 (46.7%) | 61 (14.4%) | 594 (8.9%) | < .001 |
| Yes | 3113 (53.3%) | 362 (85.6%) | 6084 (91.1%) | ||
| CPC* | Poor | 5641 (93.5%) | 391 (90.1%) | 6098 (90.4%) | < .001 |
| Good | 391 (6.5%) | 43 (9.9%) | 645 (9.6%) | ||
| Survival to discharge | No | 5380 (89.2%) | 377 (86.9%) | 5852 (86.8%) | < .001 |
| Yes | 652 (10.8%) | 57 (13.1%) | 891 (13.2%) |
CPR Cardiopulmonary resuscitation; AED Automated electrical defibrillator; ECG Electrocardiography; DA-CPR Dispatcher-assisted CPR; CPC Cerebral performance category.
*A CPC score of 1 or 2 was considered a good neurological outcome, and a score of 3, 4, or 5 was considered a poor neurological outcome.
We performed a logistic regression analysis to adjust for potential confounding factors from the prehospital Utstein elements on good neurologic outcomes and survival upon discharge (Tables 3 and 4). The multivariable model revealed that the “compression-only” CPR group had less favourable outcomes than those of the no bystander CPR group and the provision of DA-CPR had less favourable outcomes as well. However, in an interaction model, there was a significantly positive interaction when “compression-only” CPR by bystanders and DA-CPR were performed simultaneously. The interaction models with good neurological and survival outcomes showed lower AIC scores than the models without an interaction. Therefore, we selected an interaction model to explain this phenomenon.
Table 3.
Logistic regression on the effect of good neurologic outcomes showing odds ratio.
| Variables | Poor CPC* (N = 11,459) | Good CPC (N = 958) | Model 1 (univariable) | Model 2 (multivariable) | Model 3 (multivariable with interaction) | |
|---|---|---|---|---|---|---|
| Age | Mean ± SD | 69.8 ± 15.0 | 56.0 ± 13.5 | 0.95 (0.94–0.95, p < .001) | 0.96 (0.96–0.97, p < .001) | 0.96 (0.96–0.97, p < .001) |
| Sex | Female | 4109 (35.9%) | 183 (19.1%) | |||
| Male | 7350 (64.1%) | 775 (80.9%) | 2.37 (2.01–2.79, p < .001) | 1.07 (0.88–1.30, p = .487) | 1.07 (0.88–1.31, p = .472) | |
| Diabetes | No | 8743 (76.3%) | 841 (87.8%) | |||
| Yes | 2716 (23.7%) | 117 (12.2%) | 0.45 (0.37–0.55, p < .001) | 0.67 (0.53–0.85, p < .001) | 0.67 (0.53–0.85, p = .001) | |
| Hypertension | No | 7738 (67.5%) | 694 (72.4%) | |||
| Yes | 3721 (32.5%) | 264 (27.6%) | 0.79 (0.68–0.92, p = .002) | 1.48 (1.23–1.79, p < .001) | 1.48 (1.22–1.79, p < .001) | |
| Bystander witness | No | 5341 (46.6%) | 171 (17.8%) | |||
| Yes | 6118 (53.4%) | 787 (82.2%) | 4.02 (3.39–4.76, p < .001) | 2.20 (1.81–2.67, p < .001) | 2.22 (1.83–2.70, p < .001) | |
| Bystander CPR | No CPR | 5224 (45.6%) | 345 (36%) | |||
| Standard CPR | 337 (2.9%) | 31 (3.2%) | 0.93 (0.64–1.36, p = .716) | 0.71 (0.45–1.10, p = .125) | 1.07 (0.44–2.61, p = .888) | |
| Compression-only CPR | 5898 (51.5%) | 582 (60.8%) | 0.67 (0.58–0.77, p < .001) | 0.82 (0.68–0.99, p = .036) | 0.77 (0.55–1.09, p = .141) | |
| AED | No | 10,577 (92.3%) | 839 (87.6%) | |||
| Yes | 882 (7.7%) | 119 (12.4%) | 1.70 (1.39–2.09, p < .001) | 1.47 (1.13–1.91, p = .004) | 1.43 (1.10–1.86, p = .007) | |
| Place | Public | 3793 (33.1%) | 576 (60.1%) | |||
| Residence | 7666 (66.9%) | 382 (39.9%) | 0.33 (0.29–0.38, p < .001) | 0.65 (0.55–0.76, p < .001) | 0.64 (0.54–0.76, p < .001) | |
| Initial ECG | Non-shockable | 9976 (87.1%) | 180 (18.8%) | |||
| Shockable | 1483 (12.9%) | 778 (81.2%) | 29.08 (24.50–34.50, p < .001) | 17.73 (14.76–21.29, p < .001) | 17.85 (14.85–21.44, p < .001) | |
| DA-CPR | No | 2912 (25.4%) | 300 (31.3%) | |||
| Yes | 8547 (74.6%) | 658 (68.7%) | 0.75 (0.65–0.86, p < .001) | 0.69 (0.57–0.84, p < .001) | 0.53 (0.41–0.70, p < .001) | |
| Standard CPR x DA-CPR | 0.85 (0.30–2.41, p = .756) | |||||
| Compression-only CPR x DA-CPR | 1.93 (1.28–2.91, p = .002) | |||||
| AIC | 4332 | 4326 |
OR Odds ratio; CPC Cerebral performance category; CPR Cardiopulmonary resuscitation; AED Automated electrical defibrillator; ECG Electrocardiography; DA-CPR Dispatcher-assisted CPR; AIC Akaike Information Criterion.
*A CPC score of 1 or 2 was considered a good neurological outcome, and a score of 3, 4, or 5 was considered a poor neurological outcome.
Table 4.
Logistic regression on the effect of survival to discharge showing odds ratio.
| Variables | No survival discharge (N = 10,987) | Survival to discharge (N = 1430) | Model 1 (univariable) | Model 2 (multivariable) | Model 3 (multivariable with interaction) | |
|---|---|---|---|---|---|---|
| Age | Mean ± SD | 70.0 ± 15.0 | 58.7 ± 14.5 | 0.96 (0.95–0.96, p < .001) | 0.97 (0.96–0.97, p < .001) | 0.97 (0.96–0.97, p < .001) |
| Sex | Female | 3969 (36.1%) | 323 (22.6%) | |||
| Male | 7018 (63.9%) | 1107 (77.4%) | 1.94 (1.70–2.21, p < .001) | 1.05 (0.90–1.22, p = .530) | 1.05 (0.91–1.22, p = .500) | |
| Diabetes | No | 8375 (76.2%) | 1209 (84.5%) | |||
| Yes | 2612 (23.8%) | 221 (15.5%) | 0.59 (0.50–0.68, p < .001) | 0.85 (0.71–1.02, p = .080) | 0.85 (0.71–1.02, p = .082) | |
| Hypertension | No | 7402 (67.4%) | 1030 (72%) | |||
| Yes | 3585 (32.6%) | 400 (28%) | 0.80 (0.71–0.91, p < .001) | 1.27 (1.09–1.48, p = .002) | 1.27 (1.09–1.47, p = .002) | |
| Bystander witness | No | 5221 (47.5%) | 291 (20.3%) | |||
| Yes | 5766 (52.5%) | 1139 (79.7%) | 3.54 (3.10–4.05, p < .001) | 2.27 (1.96–2.64, p < .001) | 2.29 (1.97–2.66, p < .001) | |
| Bystander CPR | No CPR | 4989 (45.4%) | 580 (40.6%) | |||
| Standard CPR | 324 (2.9%) | 44 (3.1%) | 1.17 (0.84–1.62, p = .351) | 0.78 (0.53–1.14, p = .195) | 0.75 (0.33–1.67, p = .476) | |
| Compression-only CPR | 5674 (51.6%) | 806 (56.4%) | 1.22 (1.09–1.37, p < .001) | 1.05 (0.90–1.22, p = .521) | 0.70 (0.52–0.94, p = .018) | |
| AED | No | 10,172 (92.6%) | 1244 (87%) | |||
| Yes | 815 (7.4%) | 186 (13%) | 1.87 (1.57–2.21, p < .001) | 1.45 (1.18–1.79, p < .001) | 1.43 (1.16–1.76, p < .001) | |
| Place | Public | 3560 (32.4%) | 809 (56.6%) | |||
| Residence | 7427 (67.6%) | 621 (43.4%) | 0.37 (0.33–0.41, p < .001) | 0.66 (0.58–0.76, p < .001) | 0.66 (0.57–0.75, p < .001) | |
| Initial ECG | Non-shockable | 9659 (87.9%) | 497 (34.8%) | |||
| Shockable | 1328 (12.1%) | 933 (65.2%) | 13.65 (12.07–15.44, p < .001) | 8.80 (7.69–10.07, p < .001) | 8.85 (7.73–10.12, p < .001) | |
| DA-CPR | No | 2756 (25.1%) | 456 (31.9%) | |||
| Yes | 8231 (74.9%) | 974 (68.1%) | 0.72 (0.63–0.81, p < .001) | 0.75 (0.64–0.88, p < .001) | 0.62 (0.51–0.76, p < .001) | |
| Standard CPR x DA-CPR | 1.15 (0.46–2.87, p = .769) | |||||
| Compression-only CPR x DA-CPR | 1.74 (1.24–2.44, p = .001) | |||||
| AIC | 6559 | 6552 |
OR Odds ratio; CPR Cardiopulmonary resuscitation; AED Automated electrical defibrillator; ECG Electrocardiography; DA-CPR Dispatcher-assisted CPR; AIC Akaike Information Criterion.
Discussion
Among the three groups (no bystander CPR, “standard” bystander CPR, and “compression-only” bystander CPR) in our study, the group without bystander CPR comprised patients who were older, had fewer witnessed OHCA events, fewer shockable rhythms, less DA-CPR provision, poorer CPC, and less survival to discharge compared to those of the other groups. However, more patients received AED use once DA-CPR was initiated despite the low rate of its initiation. One hypothesis for this conflicting finding may be that those who are even reluctant to compress the chest of OHCA victims might apply AED when DA-CPR is successfully initiated.
Chest compression with ventilation has been the main component of resuscitation for OHCA victims since the early 1960s18. However, bystanders’ reluctance to perform CPR has increased because of the resistance associated with the need to perform mouth-to-mouth ventilation8,19,20. Therefore, the European Resuscitation Council and American Heart Association guidelines have introduced two possible methods for bystanders21,22. The first method is “standard” CPR with a 30:2 ratio of compression and ventilation. The second is “compression-only” CPR without pauses for ventilation, intended to encourage bystanders to undertake resuscitation efforts more frequently. Despite this effort, there is wide variation in outcomes across different studies. Some studies have reported that “compression-only” CPR is associated with better outcomes17,23–25. On the contrary, other studies have reported that “standard” CPR had better outcomes for selected patients with OHCA, such as those with a noncardiac OHCA, children, and those in whom there was a delay in CPR initiation26,27. Another study reported no differences in outcomes between “compression-only” CPR and “standard” CPR28–30. Similarly, our study showed heterogeneous outcomes. We suspect that this finding might be associated with the poor quality of CPR because one literature review claimed that the depth of compression in “compression-only” CPR might be shallower than that in “standard” CPR10. According to our results in Table 2, approximately half of the OHCA cases underwent compression-only CPR, and the rate of attempts at standard CPR is extremely low in Korea. The proportion of bystander compression-only CPR has been significantly increasing over time. Unfortunately, we could not obtain detailed information about the bystanders, such as whether they were trained for CPR. We assume that more attempts at compression-only CPR have been encouraged because “compression-only” CPR is simple and easy to learn for bystanders.
There is a need to increase the rate of bystander CPR, one of the critical components in the chain of survival, to provide early CPR before the EMS arrive31. DA-CPR programs are intended to encourage bystanders who are untrained or reluctant to perform CPR5,32,33. However, DA-CPR is less likely to result in favourable real-world outcomes. Our multivariate analysis also showed that DA-CPR had a statistically significant negative effect on good neurological outcomes and survival to discharge. This finding is similar to that of previous studies showing less survival or neurological benefit12,34. These researchers hypothesised that the primary cause of the reduced benefit was the low confidence of dispatchers for DA-CPR. Dispatchers may assist in improving the provision of bystander CPR. However, more time elapsed before CPR initiation under DA-CPR than for self-led bystander CPR because the bystander would instantly initiate CPR soon after they witnessed and identified an OHCA. Moreover, a longer detection time interval (DTI) from the call for an ambulance to the detection of OHCA by the dispatcher showed significantly poorer neurological recovery. This 30-s delay in DTI was associated with a 3% reduction in a good CPC score35.
The interaction between “compression-only” CPR and DA-CPR provision in our study showed a positive effect on good neurological and survival outcomes after adjusting for potential confounders, despite the absence of a positive effect of compression-only CPR or DA-CPR when considered independently. This finding is different from that of previous studies. There were three randomised controlled trials (RCTs) showing no significant difference between compression-only CPR with DA-CPR and standard CPR with DA-CPR28,29,36. One retrospective observational CPR study reported that standard CPR with DA-CPR was associated with good neurological outcomes37. These heterogeneous findings are attributable to multiple factors. First, a 30:2 compression-to-ventilation ratio has been recommended since 200538,39. The above RCTs comprised a 15:2 ratio, as per previous CPR guidelines. Therefore, variability in CPR ratio followed may have a heterogeneous effect on the outcomes. Second, our study population was different from that of the above observational study, which excluded those who received “no attempt” CPR and “unwitnessed” cardiac arrests.
The rate of bystander CPR varies from 26 to 86% internationally40. Our study revealed that the rate of bystander CPR gradually increased to 50%, showing a statistically significant trend over the years. In addition, bystander CPR before the arrival of EMS is associated with an increased chance of survival after OHCA compared with no bystander CPR41. In addition, DA-CPR significantly increased the actual provision of bystander CPR42. For DA-CPR, compression-only CPR is strongly recommended for adults with suspected OHCA, though this recommendation is based on limited evidence43.
Hypertension is a well-known risk factor for cardiac diseases such as myocardial infarction and coronary artery disease. It is associated with a 2–3-fold increase in the risk of cardiac arrest44. Interestingly, our study revealed that hypertension was associated with good neurological and survival outcomes after adjusting for potential confounding factors, even though there was a significant negative effect on outcomes in each univariable analysis. This finding is unexpected. However, previous studies have also claimed that hypertension had a good survival outcome in univariable analysis44–46. In addition, another recent study has shown similar outcomes in univariable and multivariable analyses47. While this study could not fully explain why hypertension had a favourable effect on outcomes after OHCA, the authors explained that the result might come from the pathophysiology of hypertension itself or lifestyle changes and medication after the patient’s diagnosis of hypertension. Once they know of their hypertension, patients have a greater understanding of EMS activation, resulting in early recognition and early activation in the case of an OHCA48. Antihypertensive medications, such as angiotensin-converting enzyme inhibitors, beta-blockers, and calcium-channel blockers, had favourable outcomes in patients with cardiac arrest49,50. However, a recent meta-analysis showed that antihypertensive medications did not reduce the incidence of sudden death, although they did reduce the incidence of fatal and non-fatal myocardial infarction51. Therefore, a more speculative explanation is required.
Limitations
This study has some limitations. First, there may be selection bias. Even though the KoCARC registry was managed by on-site researchers and a quality management committee, it was challenging to complete all sets of variables for each patient. All variables had 0.4–4.7% of their data missing. The top three variables with missing data were the bystander CPR method (4.7%), initial ECG at the scene (4.4%), and application of dispatcher assistance (2.1%). Second, there may be a lack of generalisability. The KoCARC registry is based on one Asian population, and the EMS system is different from that of other countries. Therefore, further evaluation should be conducted internationally. Third, there may be unmeasured bias. This registry was filled with prehospital Utstein elements, which were provided by EMS agencies; therefore, we were not able to collect all potentially relevant variables because EMS agencies were not willing to provide them. Fourth, there were significant shifts in CPR guidelines regarding the compression-to-ventilation ratio from 15:2 to 30:2 in 2005, the introduction of compression-only CPR as an option for bystanders who were unable or unwilling to perform ventilation in 2005, and the recommendation for DA-CPR in 2010. As our study population was enrolled in 2015, this major shift had no effect. However, these changes may influence the ability to compare our results with those of previous studies. Finally, this study was conducted prior to the coronavirus disease 2019 (COVID-19) pandemic but was continued through this period. During the pandemic, standard CPR was prohibited to prevent the spread of COVID-19. Therefore, this may negatively affect the preference for ventilation.
Conclusion
We conclude that the interaction between compression-only CPR and DA-CPR is significantly associated with good neurological and survival outcomes after OHCA. However, each CPR method has an independent negative effect on outcomes. Education for bystanders and dispatchers should adhere to the current guidelines to improve outcomes among OHCA victims.
Author contributions
The authors confirm contribution to the papers as follows. S.Y.: writing original draft and data analysis; C.Y.: writing original draft, data collection, and interpretation of results; C.G.C.: conceptualization, supervision, reviewing, and editing. All authors have read and agreed to the published version of the manuscript. C.G.C. and C.Y. contributed equally to this work as co-corresponding.
Data availability
The data that support the findings of this study are available from KoCARC but restrictions apply to their availability. These data were used under license for the current study and so are not publicly available. The data are however available from the corresponding author upon reasonable request and with the permission of the KoCARC.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Gyu Chong Cho and Youngsuk Cho.
References
- 1.Atwood C, Eisenberg MS, Herlitz J, Rea TD. Incidence of EMS-treated out-of-hospital cardiac arrest in Europe. Resuscitation. 2005;67:75–80. doi: 10.1016/j.resuscitation.2005.03.021. [DOI] [PubMed] [Google Scholar]
- 2.Nichol G, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rea TD, et al. Predicting survival after out-of-hospital cardiac arrest: Role of the Utstein data elements. Ann. Emerg. Med. 2010;55:249–257. doi: 10.1016/j.annemergmed.2009.09.018PMID-19944488. [DOI] [PubMed] [Google Scholar]
- 4.Wnent J, et al. To ventilate or not to ventilate during bystander CPR - A EuReCa TWO analysis. Resuscitation. 2021;166:101–109. doi: 10.1016/j.resuscitation.2021.06.006. [DOI] [PubMed] [Google Scholar]
- 5.Soar J, et al. European resuscitation council guidelines 2021: Adult advanced life support. Resuscitation. 2021;161:115–151. doi: 10.1016/j.resuscitation.2021.02.010. [DOI] [PubMed] [Google Scholar]
- 6.Hwang SO, et al. 2020 Korean guidelines for cardiopulmonary resuscitation. Part 2. environment for cardiac arrest survival and the chain of survival. Clin. Exp. Emerg. Med. 2021;8:S8–S14. doi: 10.15441/ceem.21.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Panchal AR, et al. Part 3: Adult basic and advanced life support: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142:S366–S468. doi: 10.1161/cir.0000000000000916PMID-33081529. [DOI] [PubMed] [Google Scholar]
- 8.Shibata K, Taniguchi T, Yoshida M, Yamamoto K. Obstacles to bystander cardiopulmonary resuscitation in Japan. Resuscitation. 2000;44:187–193. doi: 10.1016/s0300-9572(00)00143-x. [DOI] [PubMed] [Google Scholar]
- 9.Riva G, Hollenberg J. Different forms of bystander cardiopulmonary resuscitation in out-of-hospital cardiac arrest. J. Intern. Med. 2021;290:57–72. doi: 10.1111/joim.13260. [DOI] [PubMed] [Google Scholar]
- 10.Min Ko RJ, Wu VX, Lim SH, San Tam WW, Liaw SY. Compression-only cardiopulmonary resuscitation in improving bystanders' cardiopulmonary resuscitation performance: A literature review. Emerg. Med. J. 2016;33:882–888. doi: 10.1136/emermed-2015-204771. [DOI] [PubMed] [Google Scholar]
- 11.Koster RW, et al. European resuscitation council guidelines for resuscitation 2010 section 2: Adult basic life support and use of automated external defibrillator. Resuscitation. 2010;81:1277–1292. doi: 10.1016/j.resuscitation.2010.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim MW, et al. Comparison between dispatcher-assisted bystander CPR and self-led bystander CPR in out-of-hospital cardiac arrest (OHCA) Resuscitation. 2021;158:64–70. doi: 10.1016/j.resuscitation.2020.11.010. [DOI] [PubMed] [Google Scholar]
- 13.Song J, et al. Sex-related disparities in the in-hospital management of patients with out-of-hospital cardiac arrest. Resuscitation. 2022;173:47–55. doi: 10.1016/j.resuscitation.2022.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Kim JY, et al. Korean cardiac arrest research consortium (KoCARC): Rationale, development, and implementation. Clin. Exp. Emerg. Med. 2018;5:165–176. doi: 10.15441/ceem.17.259PMID-30269452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Perkins GD, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest: A statement for healthcare professionals from a task force of the international Liaison committee on resuscitation (American heart association, European resuscitation council, Australian and New Zealand council on resuscitation, heart and stroke foundatioN of Canada, InterAmerican heart foundation, resuscitation council of Southern Africa, resuscitation council of Asia); and the American heart association emergency cardiovascular care committee and the council on cardiopulmonary, critical care perioperative and resuscitation. Circulation. 2015;132:1286–1300. doi: 10.1161/CIR.0000000000000144. [DOI] [PubMed] [Google Scholar]
- 16.Hypothermia after Cardiac Arrest Study Group Group Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. New Engl. J. Med. 2002;346:549–556. doi: 10.1056/nejmoa012689. [DOI] [PubMed] [Google Scholar]
- 17.Bobrow BJ, et al. Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA. 2010;304:1447–1454. doi: 10.1001/jama.2010.1392. [DOI] [PubMed] [Google Scholar]
- 18.Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed-chest cardiac massage. JAMA. 1960;173:1064–1067. doi: 10.1001/jama.1960.03020280004002. [DOI] [PubMed] [Google Scholar]
- 19.Bradley SM, Rea TD. Improving bystander cardiopulmonary resuscitation. Curr. Opin. Crit. Care. 2011;17:219–224. doi: 10.1097/MCC.0b013e32834697d8. [DOI] [PubMed] [Google Scholar]
- 20.Urban J, Thode H, Stapleton E, Singer AJ. Current knowledge of and willingness to perform hands-only CPR in laypersons. Resuscitation. 2013;84:1574–1578. doi: 10.1016/j.resuscitation.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 21.Nolan JP, et al. European resuscitation council guidelines for resuscitation 2010: Section 1 executive summary. Resuscitation. 2010;81:1219–1276. doi: 10.1016/j.resuscitation.2010.08.021. [DOI] [PubMed] [Google Scholar]
- 22.Sayre MR, et al. Hands-only (compression-only) cardiopulmonary resuscitation: A call to action for bystander response to adults who experience out-of-hospital sudden cardiac arrest: A science advisory for the public from the American heart association emergency cardiovascular care committee. Circulation. 2008;117:2162–2167. doi: 10.1161/CIRCULATIONAHA.107.189380. [DOI] [PubMed] [Google Scholar]
- 23.Iwami T, et al. Chest compression-only cardiopulmonary resuscitation for out-of-hospital cardiac arrest with public-access defibrillation: A nationwide cohort study. Circulation. 2012;126:2844–2851. doi: 10.1161/CIRCULATIONAHA.112.109504. [DOI] [PubMed] [Google Scholar]
- 24.Hupfl M, Selig HF, Nagele P. Chest-compression-only versus standard cardiopulmonary resuscitation: A meta-analysis. Lancet. 2010;376:1552–1557. doi: 10.1016/S0140-6736(10)61454-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhan L, Yang LJ, Huang Y, He Q, Liu GJ. Continuous chest compression versus interrupted chest compression for cardiopulmonary resuscitation of non-asphyxial out-of-hospital cardiac arrest. Cochrane Database Syst. Rev. 2017;3:CD010134. doi: 10.1002/14651858.CD010134.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ogawa T, et al. Outcomes of chest compression only CPR versus conventional CPR conducted by lay people in patients with out of hospital cardiopulmonary arrest witnessed by bystanders: Nationwide population based observational study. BMJ. 2011;342:c7106. doi: 10.1136/bmj.c7106. [DOI] [PubMed] [Google Scholar]
- 27.Zhang X, et al. Chest-compression-only versus conventional cardiopulmonary resuscitation by bystanders for children with out-of-hospital cardiac arrest: A systematic review and meta-analysis. Resuscitation. 2019;134:81–90. doi: 10.1016/j.resuscitation.2018.10.032. [DOI] [PubMed] [Google Scholar]
- 28.Rea TD, et al. CPR with chest compression alone or with rescue breathing. N. Engl. J. Med. 2010;363:423–433. doi: 10.1056/NEJMoa0908993. [DOI] [PubMed] [Google Scholar]
- 29.Svensson L, et al. Compression-only CPR or standard CPR in out-of-hospital cardiac arrest. N. Engl. J. Med. 2010;363:434–442. doi: 10.1056/NEJMoa0908991. [DOI] [PubMed] [Google Scholar]
- 30.Bielski K, et al. Meta-analysis of chest compression-only versus conventional cardiopulmonary resuscitation by bystanders for adult with out-of-hospital cardiac arrest. Cardiol. J. 2021 doi: 10.5603/CJ.a2021.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bobrow BJ, Panczyk M, Subido C. Dispatch-assisted cardiopulmonary resuscitation: The anchor link in the chain of survival. Curr. Opin. Crit. Care. 2012;18:228–233. doi: 10.1097/MCC.0b013e328351736b. [DOI] [PubMed] [Google Scholar]
- 32.Ro YS, et al. Effect of dispatcher-assisted cardiopulmonary resuscitation program and location of out-of-hospital cardiac arrest on survival and neurologic outcome. Ann. Emerg. Med. 2017;69(52–61):e51. doi: 10.1016/j.annemergmed.2016.07.028. [DOI] [PubMed] [Google Scholar]
- 33.Travers AH, et al. Part 3: Adult basic life support and automated external defibrillation: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015;132:S51–83. doi: 10.1161/CIR.0000000000000272. [DOI] [PubMed] [Google Scholar]
- 34.Hagihara A, Onozuka D, Shibuta H, Hasegawa M, Nagata T. Dispatcher-assisted bystander cardiopulmonary resuscitation and survival in out-of-hospital cardiac arrest. Int. J. Cardiol. 2018;265:240–245. doi: 10.1016/j.ijcard.2018.04.067PMID-29703565. [DOI] [PubMed] [Google Scholar]
- 35.Ko SY, et al. Effect of detection time interval for out-of-hospital cardiac arrest on outcomes in dispatcher-assisted cardiopulmonary resuscitation: A nationwide observational study. Resuscitation. 2018;129:61–69. doi: 10.1016/j.resuscitation.2018.06.002PMID-29874553. [DOI] [PubMed] [Google Scholar]
- 36.Hallstrom AP. Dispatcher-assisted, "phone" cardiopulmonary resuscitation by chest compression alone or with mouth-to-mouth ventilation. Crit. Care Med. 2000;28:N190–192. doi: 10.1097/00003246-200011001-00004. [DOI] [PubMed] [Google Scholar]
- 37.Goto Y, Funada A, Maeda T, Goto Y. Dispatcher instructions for bystander cardiopulmonary resuscitation and neurologically intact survival after bystander-witnessed out-of-hospital cardiac arrests: A nationwide, population-based observational study. Crit. Care. 2021;25:408. doi: 10.1186/s13054-021-03825-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hazinski MF, et al. Major changes in the 2005 AHA Guidelines for CPR and ECC: Reaching the tipping point for change. Circulation. 2005;112:IV206–211. doi: 10.1161/CIRCULATIONAHA.105.170809. [DOI] [PubMed] [Google Scholar]
- 39.Sandroni C, Cavallaro F. The 2005 European guidelines for cardiopulmonary resuscitation: Major changes and rationale. Minerva Anestesiol. 2008;74:137–143. [PubMed] [Google Scholar]
- 40.Kiguchi T, et al. Out-of-hospital cardiac arrest across the World: First report from the international liaison committee on resuscitation (ILCOR) Resuscitation. 2020;152:39–49. doi: 10.1016/j.resuscitation.2020.02.044. [DOI] [PubMed] [Google Scholar]
- 41.Wissenberg M, et al. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA. 2013;310:1377–1384. doi: 10.1001/jama.2013.278483. [DOI] [PubMed] [Google Scholar]
- 42.Shimamoto T, et al. Dispatcher instruction of chest compression-only CPR increases actual provision of bystander CPR. Resuscitation. 2015;96:9–15. doi: 10.1016/j.resuscitation.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 43.Berg KM, et al. Part 7: Systems of care: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142:S580–S604. doi: 10.1161/CIR.0000000000000899. [DOI] [PubMed] [Google Scholar]
- 44.Yusuf S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. The Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 45.Parry M, Danielson K, Brennenstuhl S, Drennan IR, Morrison LJ. The association between diabetes status and survival following an out-of-hospital cardiac arrest: A retrospective cohort study. Resuscitation. 2017;113:21–26. doi: 10.1016/j.resuscitation.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 46.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: A systematic review and meta-analysis. Circ. Cardiovasc. Qual. Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 47.Jung E, et al. Effect of hypertension across the age group on survival outcomes in out-of-hospital cardiac arrest. Am. J. Emerg. Med. 2019;37:608–614. doi: 10.1016/j.ajem.2018.06.049PMID-30025949. [DOI] [PubMed] [Google Scholar]
- 48.Stecker EC, et al. Ischemic heart disease diagnosed before sudden cardiac arrest is independently associated with improved survival. J. Am. Heart Assoc. 2014;3:e001160. doi: 10.1161/JAHA.114.001160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Domanski MJ, et al. Effect of angiotensin converting enzyme inhibition on sudden cardiac death in patients following acute myocardial infarction. J. Am. Coll. Cardiol. 1999;33:598–604. doi: 10.1016/s0735-1097(98)00609-3. [DOI] [PubMed] [Google Scholar]
- 50.Bertrand ME, et al. Clinical synergy of perindopril and calcium-channel blocker in the prevention of cardiac events and mortality in patients with coronary artery disease. Post hoc analysis of the EUROPA study. Am. Heart J. 2010;159:795–802. doi: 10.1016/j.ahj.2009.12.042. [DOI] [PubMed] [Google Scholar]
- 51.Taverny G, et al. Antihypertensive pharmacotherapy for prevention of sudden cardiac death in hypertensive individuals. Cochrane Database Syst. Rev. 2016;3:CD011745. doi: 10.1002/14651858.CD011745.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from KoCARC but restrictions apply to their availability. These data were used under license for the current study and so are not publicly available. The data are however available from the corresponding author upon reasonable request and with the permission of the KoCARC.