Abstract
Objectives:
Acceptance and Commitment Therapy (ACT) is a third-wave behavioral and cognitive therapy that increases psychological flexibility through mindfulness, acceptance, and value-driven behavior change. ACT has been successfully used to inform a variety of health interventions. Using non-therapists to deliver ACT-based behavioral health interventions offers an opportunity to provide cost efficient and integrated care, particularly among underserved populations experiencing barriers to mental health care, such as inadequate insurance, mental health stigma, and provider shortages. This systematic review aims to: 1) identify ACT-informed behavioral health interventions delivered by laypeople and 2) review the specific characteristics of each intervention including number and duration of sessions, delivery modality, interventionist training, and intervention outcomes.
Methods:
Two databases (PubMed and PsycINFO) were systematically searched for relevant literature. To further identify relevant studies, references of included manuscripts were checked, the Association for Contextual Behavioral Science’s webpage was examined, and an email was sent to the ACBS Health Special Interest Group listserv. Study abstracts and full texts (in English) were screened, resulting in 23 eligible articles describing 19 different interventions.
Results:
A total of 1,781 abstracts were screened, 76 were eligible for full-text review, and 23 were included in a narrative synthesis. There were 19 unique interventions identified and delivered by the following: general healthcare workers (n= 7), trained researchers (n = 5), women/mothers (n= 2), municipal workers (n= 2), and teachers (n = 3). Eleven studies were RCTs and eight utilized alternative study designs. Study quality varied, with two rated as high risk for bias and eight rated to have some concerns. Target populations included clinical and non-clinical samples. There was some consistency in the effects reported in the studies: increases in pain tolerance, acceptance, and identifying and engaging in value driven behavior, improvements in cognitive flexibility, and reductions in psychological distress.
Conclusions:
Findings suggest that ACT interventions can be successfully delivered by a variety of laypeople and effectively address psychological distress and increase health behaviors.
Keywords: Acceptance and Commitment Therapy (ACT), intervention, review, laypeople, behavioral health, task-shifting
Introduction
Acceptance and Commitment Therapy (ACT) is a third-wave behavioral and cognitive therapy that emphasizes mindfulness, acceptance, and value-driven behavior change (Hayes, Luoma, Bond, Masuda, & Lillis, 2006; Hayes, Strosahl, & Wilson, 2011; Wilson, Bordieri, Flynn, Lucas, & Slater, 2011). ACT is informed by Relational Frame Theory and experimental work regarding the influence of language on behavior (De Houwer, Barnes-Holmes, & Barnes-Holmes, 2016; Zettle, 2005). ACT has been described as targeting internal experiences related to: Thoughts, Emotions, Associations, Memories, Sensations (TEAMS) (Robinson, Gould, & Strosahl, 2010) and works to enhance psychological flexibility (Hayes et al., 2006). ACT employs six core therapeutic processes: acceptance, cognitive defusion, mindfulness, self-as-context, committed action, and valued living (Hayes et al., 2006). The combination of these processes facilitate behavior change through helping individuals define and plan realistic and effective behaviors congruent with their own values. There are four properties of psychological flexibility fundamental to mental and physical health, as well as overall well-being: (1) recognizing/adapting to situational demands, (2) shifting perspective when functioning is compromised, (3) balancing competing life domains, and (4) being aware, open, and committed to behaviors that are congruent with personal values (Kashdan & Rottenberg, 2010). These properties of psychological flexibility fuel behavioral maintenance to healthy living (Kwasnicka, Dombrowski, White, & Sniehotta, 2016). When long term values are ignored, health outcomes and quality of life can suffer (Spleen, Lengerich, Camacho, & Vanderpool, 2014). Delaying preventive healthcare, medication nonadherence, and denial about behavioral risk are associated with poor health (Byrne, 2008). ACT increases willingness to experience unpleasant TEAMS to allow individuals to engage in meaningful and healthy behaviors (Hayes et al., 2006).
ACT has been successfully used to inform a variety of mental health conditions including anxiety (Swain, Hancock, Hainsworth, & Bowman, 2013), depression (Bai, Luo, Zhang, Wu, & Chi, 2020) and psychosis (Yıldız, 2020). Although initially developed for the treatment of psychopathology (Hayes et al., 2006), ACT has been found to also be beneficial in addressing health behaviors, adjustment to chronic illness, and other life conditions. ACT has been used to address physical health conditions and health behavior change including: smoking cessation (Zeng, Heffner, Copeland, Mull, & Bricker, 2016), chronic pain (Lin et al., 2017; Trompetter, Schreurs, Heuts, & Vollenbroek-Hutten, 2014), diet and physical activity (Goodwin, Forman, Herbert, Butryn, & Ledley, 2012), weight control (Lillis, Hayes, & Levin, 2011), health anxiety (Hoffmann, Rask, Hedman-Lagerlof, Ljotsson, & Frostholm, 2018), and diabetes (Nes, Van Dulmen, Eide, Finset, Kristjansdottir, Steen, & Eide, 2012).
A global priority to help eliminate mental health treatment gaps is to improve access to high-quality and evidence-based mental health services through sustainable public health systems (Wainberg et al., 2017). The World Health Organization (WHO) has recommended talking therapies as a first-line treatment for many mental health concerns, which can easily be delegated to laypersons. Task-shifting in mental health is when aspects of therapy are delegated to non-specialists, such as laypersons. Existing evidence supports the use of task-shifting in mental health (Winiarski, Rufa, & Karnik, 2019). For example, the Common Elements Treatment Approach (CETA) was created to provide treatment via laypersons for adults with depression, anxiety, substance use and trauma and stress related disorders in low- and middle-income countries (Murray et al., 2014). Similar interventions have been successful in the United States (US). One study found that, when provided training, laypeople with a bachelor-level education could successfully deliver effective cognitive behavior therapy (CBT) for older adults with generalized anxiety disorder (Stanley et al., 2014). Another intervention successfully employed empathetic listening, delivered through laypersons, to address loneliness, depression, and anxiety (Kahlon et al., 2021). In 2020, a video-conferenced behavioral activation intervention, delivered by laypersons, decreased loneliness, depression, and disability among an older population (Choi, Pepin, Marti, Stevens, & Bruce, 2020). Task-shifting interventions show global promise even when administered via diverse modalities (in-person, phone, video calls).
Using non-clinicians or laypeople to deliver ACT-based health interventions offers an opportunity to provide cost-efficient and integrated care, particularly among underserved populations experiencing barriers to mental health care such as inadequate insurance coverage (Mongelli, Georgakopoulos, & Pato, 2020). Additionally, ACT interventions incorporating laypeople as interventionists may address other barriers to mental health care including stigma (Mongelli et al., 2020). Utilizing laypersons within a community creates an opportunity to eliminate language barriers, enhance rapport and willingness to seek mental health services, and decrease biases held by individuals from different cultures. For example, recruiting members of the LBGTQ+ community alleviates antigay prejudices among providers. Further, many individuals prefer to seek mental health treatment from non-clinicians (Iheanacho et al., 2021). Offering mental health services from laypersons, such as clergy, enhances willingness to seek services and addresses racial disparities in mental health. Furthermore, community-level barriers, including mental health workforce shortages, geographical clustering of providers, and few community-based interventions reinforces gaps in treatment that could be attenuated by training laypeople to deliver ACT-based interventions (Mongelli et al., 2020).
Training laypeople as interventionists for ACT-based counseling could allow medically underserved populations to access care in the community and at venues within easy geographic reach. ACT has been applied in a variety of intervention modalities, including one day workshops, in-person sessions, and telephone or video conferencing (Dindo, Van Liew, & Arch, 2017) and has been effectively delivered by laypeople who are not mental health professionals (e.g. physical therapists (Godfrey et al., 2019), parents (Y. Y. Chong, Y. W. Mak, S. P. Leung, S. Y. Lam, & A. Y. Loke, 2019), correctional officers (Zarling & Berta, 2017), and counselor/nurse/occupational therapists (Gaudiano & Herbert, 2006; Moitra, LaPlante, Armstrong, Chan, & Stein, 2017). This positions ACT as a potentially useful and cost-effective treatment to deploy within communities as it applies to a wide range of mental health and physical health conditions and can be effectively delivered by those without professional mental health training.
Many prior non-ACT interventions delivered by laypersons have a protocol for the intervention, including training and supervision needed for interventionists. For example, to become a CETA counselor, laypersons must complete a protocoled brief training and receive ongoing supervision (Murray et al., 2014). Little is known about what ACT-based interventions delivered by laypersons currently exist or the training necessary for successful implementation. Understanding the delivery of ACT interventions by laypeople in different community settings will inform future successful protocol development for ACT-based interventions both in the US and internationally. To date, we are not aware of systematic reviews specifically evaluating ACT-based behavioral health interventions delivered by laypeople. Therefore, the current investigation aims to address this gap in the literature by systematically reviewing published literature to date for ACT-informed behavioral health interventions delivered by non-mental health professionals. We define behavioral health interventions as interventions that target human actions that impact health. Our aims were to: 1) identify ACT-informed behavioral health interventions delivered by laypeople and 2) review the specific characteristics of each intervention including number and duration of sessions, delivery modality, interventionist training, and intervention outcomes. Knowing the characteristics of impactful interventions will inform future research and implementation efforts.
Methods
An extensive systematic literature review was conducted, according to the guidelines proposed by the PRISMA-S (Preferred Reporting Items for Systematic reviews and Meta-Analyses literature search extension) checklist (Rethlefsen et al., 2021). The PRISMA-S provides guidelines for authors to verify that each component of a literature search is reported and reproducible.
Inclusion/Exclusion Criteria
The Population, Intervention, Comparison, Outcomes and Study (PICOS) formulation is an accepted mechanism used in systematic reviews to frame a review question about interventions, in this case layperson delivered ACT informed interventions (Brown et al., 2006; Fineout-Overholt & Johnston, 2005; Higgins et al., 2019). Our inclusion and exclusion criteria were developed using PICOS guidelines, which helped operationalize a systematic and consistent approach for selecting appropriate studies. Table 1 outlines the PICOS criteria. The title, abstract, and methods sections of citations attained from initial searches and via secondary examination of reference lists were subjected to the below inclusion and exclusion criteria. Full papers of retained citations were retrieved and re-subjected to the below full inclusion and exclusion criteria. To enable maximum breadth of the review, no inclusion restrictions were placed on study design, age of participants, health concern of interest, setting, control/comparison condition, or duration of follow-up.
Table 1.
PICOS Criteria for Study Inclusion
| Population | All participants currently engaged in a behavioral health ACT based intervention. The review included all age ranges, races, ethnicities, and genders. |
| Intervention | ACT informed behavioral health interventions (e.g., chronic pain, stress management, medication uptake/adherence) delivered by non-mental health professionals. Intervention studies that specified they used ACT to inform the intervention or ACT as part of the building process. Studies with laypeople delivering the intervention or someone not typically delivering mental health services. Those who practice general medicine (doctors, nurses, etc.) not previously trained in ACT were included. |
| Comparison | Anyone not currently engaged in the ACT intervention undergoing testing including waitlist controls, active control, superiority, enhanced usual control, treatment as usual (TAU) and no intervention. The review was not limited by comparison studies. |
| Outcome | There were no specific outcomes of interest. Interventions examining a variety of health conditions and behaviors were included |
| Study Design | Both single and multiple arm study designs including non-randomized, quasi-experimental, waitlist control, quasi-experimental designs and randomized control trials. This review was not limited by study design. |
Exclusion criteria included the following: 1) study types including literature reviews, meta-analyses, measure validation studies, qualitative studies, theoretical articles, and book chapters; 2) studies with experienced or novice mental health professionals (psychiatrist, psychologist, counselor, therapist, social worker, psychiatry nurse, behavior analyst, clinical or counseling fellows, clinical psychology or counseling grad students, etc.) delivering the intervention; 3) studies with technological delivery of the intervention (online, app, gaming, etc.) with no supplementary interventionist meetings; or with self-administered intervention (i.e., self-help guidebooks, workbooks, diaries) without a supplementary interventionist meeting; and 4) articles not prepared in English.
Search and screening procedures
Database Search.
Electronic searches of the PsycInfo and PubMed databases were undertaken; see Table 2 for search terms. The search was conducted in March 2021 and included any published literature meeting search criteria up to that date.
Table 2.
Databases and Key Terms Searched
| Search | Search Date | Dataset | Key Terms | # of Articles |
|---|---|---|---|---|
| 1 | 3/11/21 | PsycInfo & Pubmed | “Acceptance and commitment therap*” AND “Intervention” | 1509 |
| 2 | 3/11/21 | PsycInfo & Pubmed | “Acceptance and commitment therap*” AND “Trial” | 781 |
| 3 | 3/11/21 | PsycInfo & Pubmed | “Acceptance and commitment therap*” AND “Randomized controlled trial” | 407 |
| 4 | 3/11/21 | PsycInfo & Pubmed | “Acceptance and commitment therap*” AND “Non-therapist interventionist” | 167 |
| 5 | 3/11/21 | PsycInfo & Pubmed | “Acceptance and commitment therap*” AND “teachers” | 19 |
| 6 | 3/11/21 | PsycInfo & Pubmed | “Acceptance and commitment therap*” AND “parent*” | 193 |
| 7 | 3/11/21 | PsycInfo & Pubmed | “Acceptance and commitment therap*” AND “physical therapist*” | 3 |
| 8 | 3/11/21 | PsycInfo & Pubmed | “Acceptance and commitment therap*” AND “caregiver*” | 81 |
| 9 | 3/11/21 | PsycInfo & Pubmed | “Acceptance and commitment therap*” AND “partner*” | 76 |
| 10 | 3/11/21 | PsycInfo & Pubmed | “Acceptance and commitment therap*” AND “employee* | 45 |
| 11 | 3/11/21 | PsycInfo & Pubmed | “Acceptance and commitment therap*” AND “doctor*” | 42 |
Literature Review Reference Search.
The Association for Contextual Behavioral Science webpage (ACBS) (http://contextualscience.org/) is an international online learning and research community for professionals with an interest in ACT. We searched the published articles on this site for recently published relevant literature reviews. We identified four comprehensive literature reviews and reviewed their reference lists for additional articles (Brown, Glendenning, Hoon, & John, 2016; Coronado et al., 2020; Dochat, Wooldridge, Herbert, Lee, & Afari, 2021; Graham, Gouick, Krahé, & Gillanders, 2016).
ACBS Listserv Search.
An email requesting ACT based interventions delivered by non-mental health professionals was sent to the ACBS Health Special Interest Group (SIG) ACT for Health SIG.
Data extraction, synthesis and quality assessment
All potential articles were uploaded into the web-based software, Covidence (Babineau, 2014), for review. Three reviewers independently reviewed the title, abstract, and methods section against inclusion and exclusion criteria. A separate reviewer double checked at random 30% (~500) of the articles. Studies included for full text review were then independently reviewed by two reviewers to determine which articles to include. Reference lists of identified studies were examined for additional articles. The final list of studies was discussed as a team to ensure consensus was reached. The following data elements were extracted from selected manuscripts: (1) information specific to publication (e.g., year of publication, authors, title, journal), (2) sample characteristics (e.g., demographics, clinical condition), (3) study design features (e.g., randomization schema, exposures, comparators, and analyzed sample sizes), (4) specific characteristics of ACT based interventions delivered by laypeople including number and duration of sessions, group size, delivery modality, assignment of home practice, interventionist training, and intervention fidelity, and relevant primary outcomes (e.g., treatment satisfaction, mental and physical health outcomes).
Results
After the removal of duplicate articles, 1,736 abstracts were screened at Stage 1, 76 full text articles were reviewed at Stage 2, of which 23 were included in the narrative synthesis. See Figure 1 for a complete breakdown of reviewed articles.
Figure 1:
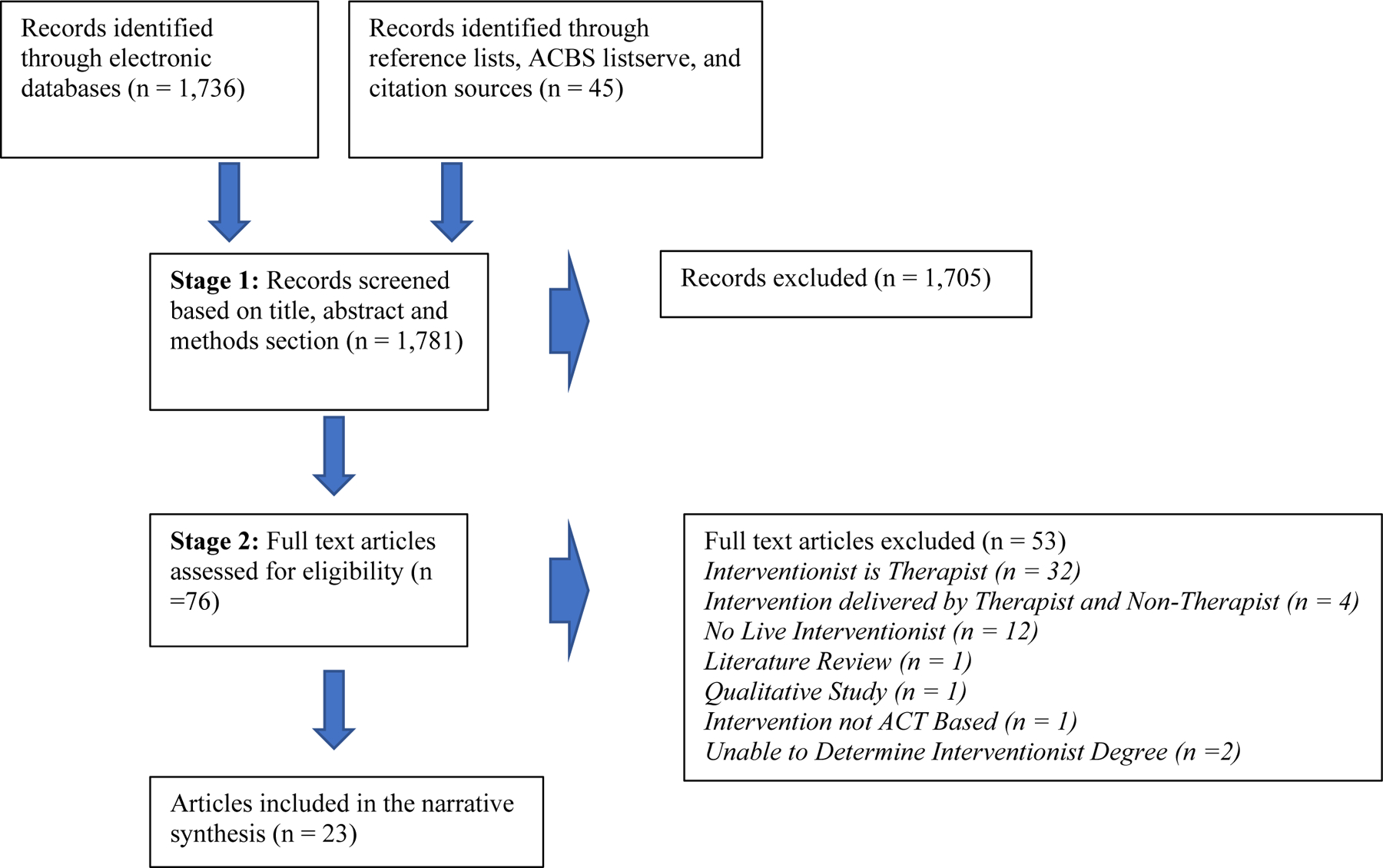
PRISMA-S Flow Diagram
Overview of Included Studies
Table 3 provides an overview of all included published articles. We included 23 articles which covered 19 different interventions. Publications on the same intervention were reported together. There was a broad range of ACT interventionists, which we categorized in the following five subgroups: general healthcare workers (n= 7), trained researchers (n = 5), women/mothers (n= 2), municipal workers (n= 2), and teachers (n = 3). Across studies, session frequency and length ranged from one session to 24 sessions of ACT with the majority of studies offering between 4–6 sessions. Intervention delivery formats were varied and included individual, group, phone, virtual, or some combination of these modalities.
Table 3.
Summary of ACT-Based Interventions and Interventionist ACT Training
| Author/Year | Interventionist Description | Interventionist ACT Training / Supervision | Session Frequency & Length | Session Modality |
|---|---|---|---|---|
| Healthcare Worker Interventionists | ||||
| Godfrey, 2020 | Physical Therapists | Manual, 2-day training program, & monthly group supervision | 3 sessions Sessions 1 & 2 length = 60 minutes Session 3 length = 20 minutes |
2 in person individual sessions 1 telephone call |
| March, 2020 | Physiotherapists | 16-hour online ACT course & 1 day of trial-specific training | 4 sessions Session 1 length = 60 minutes Sessions 2 & 3 length = 30 minutes Session 4 length = 20 minutes |
4 in person individual sessions |
| Chong, 2018Y | Nurses | 5-day ACT training | 4 sessions Session length = 2 Hours |
4 in person group sessions |
|
Hawkes, 2009
Hawkes, 2013
Hawkes, 2014 |
Health coaches (degrees in nursing, psychology, or health promotion) | 6 weeks of study-specific ACT training & weekly supervision | 11 sessions Session length = 31.5 minutes (median) |
11 telephone sessions |
| Makki, 2018 | Treatment team members (psychiatry, nursing, occupational therapy (OT), art therapy and social work) | ACT Videos, ACT training sessions, & a workbook | Sessions offered 7 days per week (Number of sessions dependent on how long patient was admitted) | In person group sessions |
| Jolley, 2020 | Frontline staff and service-user experts |
7-hour ACT workshop & weekly supervision |
6 sessions Session length = 120 minutes |
6 in person group sessions |
| Kasila, 2020 | Lay health workers | 8-month training program | 12 sessions Time not specified |
3 online modules 5 group meetings 4 phone calls |
| Trained Researcher Interventionists | ||||
| Branstetter-Rost, 2009 | Trained experimenters | Not described | 1 Session Session length = 22 minutes |
1 in person individual session |
| Fowler, 2021 | Delivered by a non-licensed, bachelor’s-prepared trained interventionist | Didactics, readings, live demonstrations, role plays, & supervision throughout study | 6 sessions Session length = 60 minutes |
6 telephone sessions |
| Walseth-Hara, 2018 | RTW coordinators had various professional backgrounds (health and non-health related) |
Introductory training in ACT & biweekly supervision | 6 sessions Session length = 73 minutes (average) |
6 telephone or video conference sessions |
| Hulbert-Williams, 2017 | Undergraduate psychology students | Intervention scripts (specific training not described) | 1 session Session length = 8 minutes |
1 in person group session |
| Moradi, 2019 | Researcher | ACT course | 8 sessions Session length = 90 minutes |
8 in person group sessions |
| Women/Mother Interventionists | ||||
| Fung, 2018 | Mothers of children with autism | ACT course, individual training and coaching, & ACT manual | 2 sessions Session 1 = 1.5 days Session 2 = not specified |
2 in person group sessions |
|
Tol, 2018
Tol, 2020 |
Ugandan women | 4-day training & weekly supervision | 5 sessions Session length = 2 hours |
5 audio-recorded sessions Self-help manual |
| Municipal Worker Interventionists | ||||
|
Zarling, 2019
|
Correctional staff | Two 2-day ACT trainings & ongoing supervision | 24 sessions Session length = 1.5 to 2 hours |
24 in person group sessions |
| Stapelfeld, 2015 | Municipal job consultants | 4-day ACT and Individual Placement and Support Model (IPS) course & monthly supervision | Varied number of sessions (tailored to patient needs) | In person individual meetings |
| Teacher Interventionists | ||||
| Shaw, 2020 | Singing teacher | 7-hour ACT training | 6 sessions Session length = 60 minutes |
4 in person individual sessions 2 Skype sessions |
| Van der Gucht, 2017 | Teachers | 2-day ACT training, comprehensive manual, 2 group supervision sessions | 4 sessions Session length = 120 minutes |
4 in person group sessions |
| Hassinen, 2018 | Counselors at the Service Foundation for the Deaf | 2-day workshop & ongoing group supervision | 12 sessions Session length = 60 minutes |
12 in person individual sessions |
Narrative Synthesis
A Narrative Synthesis of the 19 included ACT interventions is presented in Table 4. This includes a summary of the original authors’ reported results. The number of participants included in each study ranged from one (a case study) to over 3,000. Many of the studies focused on adult populations with a few focusing on caregivers and teachers. Most of the studies were randomized controlled trials (RCTs). Target populations included a broad range of individuals experiencing mental health distress, patients with physical illnesses (e.g., cancer, pain, obesity), and caregivers. The amount of ACT training and supervision provided to the interventionists, as well as formal assessment of interventionists’ adherence to the ACT intervention, varied greatly and was not always specified. Interventionist ACT training ranged from two-day workshops to 8-month courses. However, most studies offered a few days of ACT training and ongoing supervision from an ACT expert.
Table 4.
Narrative Synthesis of Nineteen Included ACT-Based Interventions with Results
| Author/ Year |
Number of participants & Mean Age |
Study Design |
Target Population | Study Conditions |
Summary of Article’s Reported Results |
|---|---|---|---|---|---|
| Healthcare Worker Interventionists | |||||
| Godfrey, 2020 | N = 248 Mean age = 48 years |
Randomized Controlled Trial | Adults with lower back pain | Group 1: Physical therapy Group 2: Physical therapy and ACT |
Physical therapy informed by ACT (PACT) showed significantly greater improvements in secondary measures of pain-related interference compared to physical therapy alone at 3 but not at 12 months. |
| March, 2020 | N = 51 | Randomized Controlled Trial | Adult patients with total knee arthroplasty | Group 1: Usual care Group 2: Usual care plus KOMPACT (Preoperative physiotherapy informed by ACT) |
No results reported. |
| Chong, 2018 | N = 168 Child mean age = 6.8 |
Randomized Controlled Trial | Parents of children (ages 3–12) with asthma | Group 1: ACT group sessions + asthma education Group 2: Asthma education |
The ACT group had significantly fewer visits to clinics and fewer days and nights with asthma symptoms. ACT parents had less psychologically inflexible, fewer negative emotional experiences, and fewer symptoms of stress and better quality of life. |
|
Hawkes, 2009
Hawkes, 2013
Hawkes, 2014 |
N = 410 Mean age = 64.9 |
Randomized Controlled Trial | Adults newly diagnosed colorectal cancer | Group 1: Usual Care Group 2: Usual care & ACT informed health coaching |
The ACT intervention improved psychosocial outcomes and quality of life (physical well-being) at 6 months. |
| Makki, 2018 | N = 184 Mean age = 16.9 |
Naturalistic study design | Adolescents at psychiatric inpatient unit and their parents | Group 1: ACT-based intervention | ACT informed evidence-based intervention can be implemented to adolescents during brief inpatient treatment. Adolescents’ skills in line with ACT processes: accepting thoughts, not suppressing feelings, focusing on present, mindfulness, emotional regulation, and stress reduction techniques. |
| Jolley, 2020 | N = 85 Mean age = 43.3 |
Randomized Controlled Trial | Patients and caregivers in psychosis services | Group 1: ACTp immediately (ACTnow) Group 2: G-ACTp after 12 weeks (ACTlater) |
The ACT intervention was highly acceptable and effect sizes across outcomes ranged from very small to large, mostly favoring ACTnow. |
| Kasila, 2020 | N = 17 Mean age = 45.47 |
Qualitative study | People with obesity | Group 1: Lifestyle intervention | The different types of exercises in the intervention were suitable for learning a variety of self-regulation skills. The ACT-based intervention provided tools for dealing with problematic thoughts and feelings that are often a barrier to life-style changes, assistance in identifying personal values and in setting concrete goals, and encouraged taking value-based actions. |
| Trained Researcher Interventionists | |||||
| Branstetter-Rost, 2009 | N = 99 Mean age = 19.17 |
Randomized Controlled Trial | Individuals with chronic pain | Group 1: control Group 2: ACT model didactics Group 3: ACT model didactics plus 2-minutes imagery exercise |
Acceptance and acceptance plus values intervention had a significant impact on pain tolerance, but not on threshold. The incorporation of values showed significantly greater pain tolerance than acceptance alone. |
| Fowler, 2021 | N = 15 Mean age = 68 |
Single-arm pilot | Caregivers of patients with Alzheimer’s disease or related dementia | Group 1: One-hour telephone sessions | Caregivers showed a large reduction in anxiety symptoms immediately after intervention and were maintained at 3- and 6-month follow-up. Psychological suffering and caregiver burden decreased at 6-month follow-up. |
| Walseth-Hara, 2018 | N = 213 Mean age = 42 |
Randomized Controlled Trial | Adults referred for chronic pain disorders, chronic fatigue, or a common mental disorder and currently unable to work | Group 1: Standard return to work (RTW) follow-up only (control group) Group 2: Boosted RTW follow-up added to standard RTW follow-up |
Intervention group had higher odds of reentering work and more days paid work compared to the control group. |
| Hulbert-Williams, 2017 | N = 63 Mean age = 22.57 |
Randomized Controlled Trial | Adults who experience chocolate cravings | Group 1: Acceptance intervention Group 2: Defusion intervention Group 3: Distraction control |
Each intervention out-performed control in respect of consumption, but not cravings. These techniques may be helpful in managing food cravings. |
| Moradi, 2019 | N = 52 Mean age not reported |
Randomized Controlled Trial | Iranian women with Polycystic ovary syndrome (PCOS) | Group 1: Treatment as usual Group 2: Counseling based on ACT |
The mean scores of body image concern and self-esteem in the ACT intervention group were significantly different from the control group. |
| Women/Mother Interventionists | |||||
| Fung, 2018 | N = 33 Mean age = 44.8 |
1 group design | Mothers of school-age children with autism (<22 years) | Group 1: 1.5 day group session followed by a refresher evening session 1 month later | Improved cognitive flexibility from pre to post with no change from post to follow-up; decreased cognitive fusion pre to post, pre to follow-up and post to follow-up; change of time for values (increases) in the following domains: family, marriage, parenting, friends, fun, community life, self-care. |
|
Tol, 2018
Tol, 2020 |
N = 613 Mean age =30.9 |
Randomized Controlled Trial | Female South Sudanese refugees with psychological distress |
Group 1: Self-Help Plus ACT Group 2: Enhanced usual care |
Overall, the Self-Help Plus intervention can be rapidly deployed to large numbers of participants and reduce psychological distress among South Sudanese female refugees. |
| Municipal Worker Interventionists | |||||
| Zarling, 2019 | N = 3474 Mean age =33.45 |
Non-randomized trial | Male domestic violence offenders in batterer intervention programs | Group 1: Achieving Change Through Values-Based Behavior (ACTV) Group 2: Duluth Model programs also incorporate a cognitive-behavioral therapy (CBT) |
The ACTV group had significantly fewer charges during treatment and at 12-month follow-up. This study offered evidence for the feasibility and effectiveness of an ACT-based group for men who have been arrested for domestic assault. |
| Stapelfeldt, 2015 | Results not published | Controlled study design |
Cancer patients referred to surgery, radiotherapy, or chemotherapy |
Group 1: Usual municipal sickness benefit management Group 2: ACT and Individual Placement and Support Model (IPS) |
Results not published |
| Teacher Interventionists | |||||
| Shaw, 2020 | N=1 Age = 19 |
Case study | College music/theatre students who experience music performance anxiety (MPA) | Group 1: Acceptance and Commitment Coaching (ACC) | The student made clinically significant improvements in acceptance of MPA-related discomfort and defusion from MPA-related thoughts. |
| Van der Gucht, 2017 | N = 616 Mean age= 17 |
Randomized Controlled Trial | Schools with a pair of parallel 5th grade classes | Group 1: ACT Group 2: Usual curriculum |
Improvements in both groups with large within-subjects effect sizes for both the control and ACT group. The study failed to show any effects of ACT. |
| Hassinen, 2018 | N = 16 Mean age = 43.8 |
Single case study | Adults from the Finnish deaf population experiencing some psychological concerns | Group 1: Patients treated with ACT Group 2: Waitlist control group |
The ACT-based intervention influenced somatization, interpersonal sensitivity, anxiety composed symptoms of nervousness and tension. The study indicated that counselors with limited knowledge of psychological interventions can deliver an ACT intervention using Finnish Sign Language. The intervention was well accepted by both the clients and the counselors. |
There was little overlap in measurements or constructs used to evaluate the interventions and few effect sizes reported. Thus, we were unable to complete a formal meta-analysis. Two of the included studies were protocol only publications and had no intervention results published (Stapelfeldt, 2015; March, 2020). One study did not yield any differences in the ACT group compared to the control group among a sample of 5th graders (Van der Gucht, 2017). The remaining 16 studies all showed promising results for ACT interventions with no differences observed in interventionists’ previous education, ACT training or supervision, session frequency and length, or session delivery modality. ACT-informed behavioral health interventions were successful in addressing pain tolerance, psychological inflexibility, psychosocial outcomes, anxiety, work attendance, food cravings, and body image concerns.
Risk of bias assessment
Risk of bias was assessed using the revised Cochrane risk-of-bias tool for randomized trials (RoB 2; Sterne et al., 2019;J. A. C. Sterne et al., 2019) (Brantstetter-Rost, 2009; Chong, 2018; Hawkes, 2013; Hawkes, 2014; Jolley, 2020; Moradi, 2019; Walseth-Hara, 2018; Godfrey, 2020; Hulbert-Williams, 2017), the revised Cochrane risk-of-bias tool for cluster-randomized trials (RoB 2 CRT; Sterne et al., 2019) (Tol, 2018; Tol, 2020; Van der Gucht, 2017), or the risk of bias in non-randomized studies of interventions (ROBINS-I; Sterne et al., 2016;J. A. Sterne et al., 2016) (Makki, 2018; Zarling, 2019), based on study type. These analyses are described in Table 5. Eight of the studies were rated as meriting “some concerns” for bias in outcome measurement due to using participant self-report measures. Participants were likely aware of their intervention condition given that the control was treatment as usual or no intervention, which may have influenced their reports (Godfrey, 2020; Hawke, 2013; Hawke, 2014; Jolley, 2020; Moradi, 2019; Tol, 2018; Tol, 2020; Van der Gucht, 2017). The next most identified domain for risk of bias in the included studies was missing data. Five studies were missing outcome data for more than 5% of participants. Missing data may have been associated with the outcome (Godfrey, 2020; Hawkes, 2013; Hawkes, 2014; Jolley, 2020; Moradi, 2019). For one other study, more than 5% of participants were excluded from analyses due to missing data for covariates (Zarling, 2019). We were unable to assess risk of bias in seven of the included studies due to their study design or reported information (i.e., single-arm study, protocol only).
Table 5.
Risk of Bias Evaluation by Included Study
| Study | Randomization Process | Timing / recruitment for cluster randomized trial | Confounding | Selection of Participants | Classification of Interventions | Deviations from Intended Interventions | Missing Outcome Data | Measurement of the Outcome | Selection of Reported Results | Overall Bias |
|---|---|---|---|---|---|---|---|---|---|---|
| Godfrey, 2020 | + | N/A | N/A | N/A | N/A | + | ? | ? | + | ? |
| Chong, 2018 | + | N/A | N/A | N/A | N/A | + | + | + | + | + |
| Hawkes, 2013 | + | N/A | N/A | N/A | N/A | + | ? | ? | + | ? |
| Hawkes, 2014 | + | N/A | N/A | N/A | N/A | + | ? | ? | + | ? |
| Makki, 2018 | N/A | N/A | - | + | + | + | + | + | + | - |
| Jolley, 2020 | + | N/A | N/A | N/A | N/A | + | ? | ? | + | ? |
| Branstetter-Rost, 2009 | + | N/A | N/A | N/A | N/A | + | + | + | + | + |
| Walseth-Hara, 2018 | + | N/A | N/A | N/A | N/A | + | + | + | + | + |
| Hulbert-Williams, 2017 | + | N/A | N/A | N/A | N/A | + | + | + | + | + |
| Moradi, 2019 | + | N/A | N/A | N/A | N/A | ? | ? | ? | ? | - |
| Tol, 2018 | + | + | N/A | N/A | N/A | + | + | ? | ? | ? |
| Tol, 2020 | + | + | N/A | N/A | N/A | + | + | ? | + | ? |
| Zarling, 2019 | N/A | N/A | + | + | + | + | ? | + | + | ? |
| Van der Gucht, 2017 | + | + | N/A | N/A | N/A | + | + | ? | + | ? |
| Kasila, 2020 | N/A Qualitative Study | |||||||||
| Fowler, 2021 | N/A Only One Intervention Group | |||||||||
| Fung, 2018 | N/A Single Arm Study | |||||||||
| Hassinen, 2018 | N/A Single Arm Study | |||||||||
| Shaw, 2020 | N/A Single Arm Study | |||||||||
| March, 2020 | N/A Protocol Only | |||||||||
| Stapelfeldt 2015 | N/A Protocol Only | |||||||||
Note.
Low risk
Some concerns
High risk
Discussion
To our knowledge, this is the first systematic review assessing ACT-informed behavioral health interventions delivered by laypeople. Understanding best practices in the delivery of ACT interventions by laypeople in different settings have numerous benefits. It will help task-shift, eliminate the international mental health treatment gap, and improve access to high-quality and evidence-based mental health services (Wainberg et al., 2017). Overall, findings indicated that effective ACT-informed behavioral health interventions can be successfully delivered by a large variety of non-mental health professionals through a broad range of delivery modalities (e.g., phone, in-person, group sessions). There were no observed differences in effectiveness by modality, including one day workshops, in-person sessions, and telephone or video conferencing. Effects reported in the studies included: increased overall pain tolerance, increased acceptance of TEAMS related to body image and physical pain, increased ability to identify and engage in value driven behavior (e.g., reentering work or serving as caretaker), improved cognitive flexibility, and reduced overall psychological distress (i.e., anxiety and depression). Thus, using laypeople to deliver ACT-based behavioral health interventions through a variety of modalities offers a unique opportunity to provide cost efficient integrated care and address barriers to mental health care (Mongelli et al., 2020). Additionally, the use of laypeople may have the added benefit of avoiding many of the barriers to implementation of evidence-based practices within the context of a mental health care system.
Training laypeople to deliver ACT-based interventions and provide task-shifting seems like a promising strategy to increase overall access to interventions targeting mental health distress; however more research is needed. For example, there are limited interventions focused on each health condition/behavior. Thus, future studies should aim to replicate these findings for each population, to ascertain that layperson delivered ACT works for each target group.
Additionally, these duplicate studies should utilize different delivery modalities and session lengths and frequencies to determine which is the best method per target population. Most interventions did not specify which ACT core therapeutic processes (acceptance, cognitive defusion, mindfulness, self-as-context, committed action, valued living) they implemented or which TEAMS were targeted (Hayes et al., 2006). Future studies are needed to further assess which processes should be pursued. In addition to further research on the efficacy of layperson-delivered ACT interventions, there is a need for investigations on structural and organizational barriers that facilitate or impede the implementation of these programs in specific settings. For example, in the United States healthcare system, concerns regarding the eligibility of lay-delivered ACT interventions for insurance reimbursement may limit the ability of medical centers to enact such programs, even in the presence of strong support for their efficacy. Cost effectiveness analyses should also be conducted in various environments when combining treatments to determine the overall cost benefit for each intervention. More longitudinal studies are needed to determine cause-effect relationships between the intervention and outcomes. Lastly, future studies should more systematically assess and determine what amount of training and supervision is needed for treatment delivery with fidelity and competency.
Limitations
This review has limitations that should be considered. We were only able to include interventions that were published. This may have prevented us from including less effective ACT based intervention delivered by laypeople and ongoing studies that have yet to publish their protocol or study results. Additionally, many studies did not specify the educational background or training of their interventionist in their titles or abstracts. This barrier prevented us from including studies from conference abstracts or clinicaltrials.gov. Our study procedure included the review of titles, abstracts, and methods sections as part of the initial review; however, we anticipate that some studies meeting inclusion criteria may have been missed during initial screening. Many of the studies did not explicitly report which ACT processes were targeted through the intervention and we are unable to report which processes should be targeted in future interventions. Similar to other reviews, the results from this synthesis may be limited by the selected search procedures and the inability to identify/include all potentially relevant studies, including non-English language publications. Lastly, five of the included studies were missing data from more than 5% of the study participants, thus conclusions drawn from the studies should be considered with caution (Godfrey, 2020; Hawkes, 2013; Hawkes, 2014; Jolley, 2020; Moradi, 2019).
Conclusions
This systematic review identified and appraised the existing ACT based behavioral health interventions delivered by non-mental health professional interventionists and their effectiveness. Overall, findings indicated that ACT interventions can be successfully delivered by a variety of laypeople (e.g., teachers, caregivers) and show promise in being effective at addressing psychological distress and increasing health behaviors. More research is needed to determine the most effective modalities and ACT processes for each intervention.
Funding Sources:
Work by Dr. Trisha Arnold was supported by the National Institute of Mental Health Grant (K23MH124539–01A1). Work by Dr. Lynne B. Klasko-Foster and Dr. Andrew Barnett was supported by the National Institute of Mental Health Grant (T32MH078788).
References
- Babineau J (2014). Product review: Covidence (systematic review software). Journal of the Canadian Health Libraries Association/Journal de l’Association des bibliothèques de la santé du Canada, 35(2), 68–71. [Google Scholar]
- Bai Z, Luo S, Zhang L, Wu S, & Chi I (2020). Acceptance and commitment therapy (ACT) to reduce depression: A systematic review and meta-analysis. Journal of Affective Disorders, 260, 728–737. doi: 10.1016/j.jad.2019.09.040 [DOI] [PubMed] [Google Scholar]
- Branstetter-Rost A, Cushing C, & Douleh T (2009). Personal values and pain tolerance: Does a values intervention add to acceptance? The Journal of Pain, 10(8), 887–892. doi: 10.1016/j.jpain.2009.01.001 [DOI] [PubMed] [Google Scholar]
- Brown M, Glendenning A, Hoon AE, & John A (2016). Effectiveness of web-delivered acceptance and commitment therapy in relation to mental health and well-being: A systematic review and meta-analysis. Journal Medical Internet Research, 18(8), e221. doi: 10.2196/jmir.6200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown P, Brunnhuber K, Chalkidou K, Chalmers I, Clarke M, Fenton M, … Young P (2006). How to formulate research recommendations. BMJ, 333(7572), 804–806. doi: 10.1136/bmj.38987.492014.94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne SK (2008). Healthcare avoidance: a critical review. Holistic nursing practice, 22(5), 280–292. 10.1097/01.HNP.0000334921.31433.c6 [DOI] [PubMed] [Google Scholar]
- Choi NG, Pepin R, Marti CN, Stevens CJ, & Bruce ML (2020). Improving Social Connectedness for Homebound Older Adults: Randomized Controlled Trial of Tele-Delivered Behavioral Activation Versus Tele-Delivered Friendly Visits. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry, 28(7), 698–708. 10.1016/j.jagp.2020.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong Y, Mak Y, Leung S, Lam S, & Loke A (2019). Acceptance and commitment therapy for parental management of childhood asthma: An RCT. Pediatrics, 143(2), e20181723. doi: 10.1542/peds.2018-1723 [DOI] [PubMed] [Google Scholar]
- Chong YY, Mak YW, Leung SP, Lam SY, & Loke AY (2019). Acceptance and Commitment Therapy for Parental Management of Childhood Asthma: An RCT. Pediatrics, 143(2). doi: 10.1542/peds.2018-1723 [DOI] [PubMed] [Google Scholar]
- Coronado RA, Brintz CE, McKernan LC, Master H, Motzny N, Silva FM, … Archer KR (2020). Psychologically informed physical therapy for musculoskeletal pain: current approaches, implications, and future directions from recent randomized trials. Pain Rep, 5(5), e847. doi: 10.1097/pr9.0000000000000847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Houwer J, Barnes-Holmes Y, & Barnes-Holmes D (2016). Riding the waves: A functional-cognitive perspective on the relations among behaviour therapy, cognitive behaviour therapy and acceptance and commitment therapy. Int J Psychol, 51(1), 40–44. doi: 10.1002/ijop.12176 [DOI] [PubMed] [Google Scholar]
- Dindo L, Van Liew JR, & Arch J (2017). Acceptance and commitment therapy: A transdiagnostic behavioral intervention for mental health and medical conditions. Neurotherapeutics, 14(3), 546–553. doi: 10.1007/s13311-017-0521-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dochat C, Wooldridge JS, Herbert MS, Lee MW, & Afari N (2021). Single-session acceptance and commitment therapy (ACT) interventions for patients with chronic health conditions: A systematic review and meta-Analysis. Journal Contextual Behavioral Science, 20, 52–69. doi: 10.1016/j.jcbs.2021.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fineout-Overholt E, & Johnston L (2005). Teaching EBP: asking searchable, answerable clinical questions. Worldviews Evid Based Nurse, 2(3), 157–160. doi: 10.1111/j.1741-6787.2005.00032.x [DOI] [PubMed] [Google Scholar]
- Fowler NR, Judge KS, Lucas K, Gowan T, Stutz P, Shan M, … Johns SA (2021). Feasibility and acceptability of an acceptance and commitment therapy intervention for caregivers of adults with Alzheimer’s disease and related dementias. BMC Geriatrics, 21(1), 1–10. doi: 10.1186/s12877-021- [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung K, Lake J, Steel L, Bryce K, & Lunsky Y (2018). ACT processes in group intervention for mothers of children with Autism Spectrum Disorder. Journal of Autism and Developmental Disorders, 48(8), 2740–2747. doi: 10.1007/s10803-018-3525-x [DOI] [PubMed] [Google Scholar]
- Gaudiano BA, & Herbert JD (2006). Acute treatment of inpatients with psychotic symptoms using acceptance and commitment therapy: Pilot results. Behaviour Research and Therapy, 44(3), 415–437. doi: 10.1016/j.brat.2005.02.007 [DOI] [PubMed] [Google Scholar]
- Godfrey E, Galea Holmes M, Wileman V, McCracken L, Norton S, Moss-Morris R, … Critchley D (2016). Physiotherapy informed by Acceptance and Commitment Therapy (PACT): Protocol for a randomised controlled trial of PACT versus usual physiotherapy care for adults with chronic low back pain. BMJ Open, 6(6), e011548. doi: 10.1136/bmjopen-2016-011548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godfrey E, Wileman V, Galea Holmes M, McCracken LM, Norton S, Moss-Morris R, … Critchley D (2020). Physical therapy informed by acceptance and commitment t herapy (PACT) versus usual care physical therapy for adults with chronic low back pain: A Randomized Controlled Trial. J Pain doi: 10.1016/j.jpain.2019.05.012 [DOI] [PubMed] [Google Scholar]
- Goodwin CL, Forman EM, Herbert JD, Butryn ML, & Ledley GS (2012). A pilot study examining the initial effectiveness of a brief acceptance-based behavior therapy for modifying diet and physical activity among cardiac patients. Behav Modif, 36(2), 199–217. doi: 10.1177/0145445511427770 [DOI] [PubMed] [Google Scholar]
- Graham CD, Gouick J, Krahé C, & Gillanders D (2016). A systematic review of the use of Acceptance and Commitment Therapy (ACT) in chronic disease and long-term conditions. Clin Psychol Rev, 46, 46–58. doi: 10.1016/j.cpr.2016.04.009 [DOI] [PubMed] [Google Scholar]
- Gucht K, Griffith JW, Hellemans R, Bockstaele M, Pascal-Claes F, & Raes F (2017). Acceptance and Commitment Therapy (ACT) for adolescents: Outcomes of a large-sample, school-based, cluster-randomized controlled trial. Mindfulness, 8(2), 408–416. doi: 10.1007/s12671-016-0612-y [DOI] [Google Scholar]
- Hara KW, Bjørngaard J, Brage S, Borchgrevink P, Halsteinli V, Stiles T, … Woodhouse A (2018). Randomized controlled trial of adding telephone follow-up to an occupational rehabilitation program to increase work participation. Journal of Occupational Rehabilitation, 28(2), 265–278. doi: 10.1007/s10926-017-9711-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassinen L, & Lappalainen R (2018). Acceptance and commitment therapy using Finnish sign language: Training counselors in signed ACT for the deaf – A pilot study. J Contextual Behav Sci, 8, 74–81. doi: 10.1016/j.jcbs.2018.02.005 [DOI] [Google Scholar]
- Hawkes AL., Chambers SK, Pakenham KI, Patrao TA, Baade PD, Lynch BM, … Courneya KS (2013). Effects of a telephone-delivered multiple health behavior change intervention (CanChange) on health and behavioral outcomes in survivors of colorectal cancer: a randomized controlled trial. J Clin Oncol, 31(18), 2313–2321. doi: 10.1200/jco.2012.45.5873 [DOI] [PubMed] [Google Scholar]
- Hawkes AL, Pakenham KI, Chambers SK, Patrao TA, & Courneya KS (2014). Effects of a multiple health behavior change intervention for colorectal cancer survivors on psychosocial outcomes and quality of life: A randomized controlled trial. Ann Behav Med, 48(3), 359–370. doi: 10.1007/s12160-014-9610-2 [DOI] [PubMed] [Google Scholar]
- Hawkes AL, Pakenham KI, Courneya KS, Gollschewski S, Baade P, Gordon LG, … Chambers SK (2009). A randomised controlled trial of a tele-based lifestyle intervention for colorectal cancer survivors (‘CanChange’): Study protocol. BMC Cancer, 9, 286. doi: 10.1186/1471-2407-9-286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, & Lillis J (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour research and therapy, 44(1), 1–25. doi: 10.1016/j.brat.2005.06.006 [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, & Wilson KG (2011). Acceptance and Commitment Therapy, Second Edition: The Process and Practice of Mindful Change: Guilford Publications. [Google Scholar]
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page M, & Welch V (2019). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook. [DOI] [PMC free article] [PubMed]
- Hoffmann D, Rask CU, Hedman-Lagerlof E, Ljotsson B, & Frostholm L (2018). Development and Feasibility Testing of Internet-Delivered Acceptance and Commitment Therapy for severe health anxiety: Pilot Study. JMIR Mental Health, 5(2), e28. doi: 10.2196/mental.9198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulbert-Williams L, Hulbert-Williams NJ, Nicholls W, Williamson S, Poonia J, & Hochard KD (2019). Ultra-brief non-expert-delivered defusion and acceptance exercises for food cravings: A partial replication study. J Health Psychol, 24(12), 1698–1709. doi: 10.1177/1359105317695424 [DOI] [PubMed] [Google Scholar]
- Iheanacho T, Nduanya UC, Slinkard S, Ogidi AG, Patel D, Itanyi IU, Naeem F, Spiegelman D, & Ezeanolue EE (2021). Utilizing a church-based platform for mental health interventions: exploring the role of the clergy and the treatment preference of women with depression. Global mental health (Cambridge, England), 8, e5. 10.1017/gmh.2021.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jolley S, Johns LC, O’Donoghue E, Oliver J, Khondoker M, Byrne M, … Morris E (2020). Group acceptance and commitment therapy for patients and caregivers in psychosis services: Feasibility of training and a preliminary randomized controlled evaluation. British Journal of Clinical Psychology, 59(4), 524–551. doi: 10.1111/bjc.12265 [DOI] [PubMed] [Google Scholar]
- Kahlon MK, Aksan N, Aubrey R, Clark N, Cowley-Morillo M, Jacobs EA, Mundhenk R, Sebastian KR, & Tomlinson S (2021). Effect of Layperson-Delivered, Empathy-Focused Program of Telephone Calls on Loneliness, Depression, and Anxiety Among Adults During the COVID-19 Pandemic: A Randomized Clinical Trial. JAMA psychiatry, 78(6), 616–622. 10.1001/jamapsychiatry.2021.0113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan TB, & Rottenberg J (2010). Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review, 30(7), 865–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasila K, Vainio S, Punna M, Lappalainen P, Lappalainen R, Kaipainen K, & Kettunen T (2020). Individual differences in processes of lifestyle changes among people with obesity: A n acceptance and commitment therapy (ACT) intervention in a primary health care setting. Primary health care research & development, 21, e12. doi: 10.1017/S146342362000016X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwasnicka D, Dombrowski SU, White M, & Sniehotta F (2016). Theoretical explanations for maintenance of behavior change: A systematic review of behavior theories. Health psychology review, 10(3), 277–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lillis J, Hayes SC, & Levin ME (2011). Binge eating and weight control: T he role of experiential avoidance. Behav Modif, 35(3), 252–264. doi: 10.1177/0145445510397178 [DOI] [PubMed] [Google Scholar]
- Lin J, Paganini S, Sander L, Luking M, Ebert DD, Buhrman M, … Baumeister H (2017). An internet-based intervention for chronic pain. Dtsch Arztebl Int, 114(41), 681–688. doi: 10.3238/arztebl.2017.0681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makki M, Hill JF, Bounds DT, McCammon S, Mc Fall-Johnsen M, & Delaney KR (2018). Implementation of an ACT Curriculum on an Adolescent Inpatient Psychiatric Unit: A Quality Improvement Project. Journal of Child & Family Studies, 27(9), 2918–2924. doi: 10.1007/s10826-018-1132-2 [DOI] [Google Scholar]
- March MK, Harmer A, Godfrey E, Venkatesh S, Thomas B, & Dennis S (2020). The KOMPACT-P study: Knee Osteoarthritis Management with Physiotherapy informed by Acceptance and Commitment Therapy-Pilot study protocol. BMJ Open, 10(6), e032675. doi: 10.1136/bmjopen-2019-032675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moitra E, LaPlante A, Armstrong ML, Chan PA, & Stein MD (2017). Pilot Randomized Controlled Trial of Acceptance-Based Behavior Therapy to p romote HIV Acceptance, HIV disclosure, and retention in medical care. AIDS Behav, 21(9), 2641–2649. doi: 10.1007/s10461-017-1780-z02078-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mongelli, Georgakopoulos P, & Pato M (2020). Challenges and opportunities to meet the mental health needs of underserved and disenfranchised populations in the United States. FOCUS, 18(1), 16–24. doi: 10.1176/appi.focus.20190028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, Schaefer JA (1993). Coping resources and processes: Current concepts and measures. Handbook of stress: Theoretical and clinical aspects, 2 Edition, 234–257. [Google Scholar]
- Moradi F, Ghadiri-Anari A, Dehghani A, Reza Vaziri S, & Enjezab B (2020). The effectiveness of counseling based on acceptance and commitment therapy on body image and self-esteem in polycystic ovary syndrome: An RCT. International journal of reproductive biomedicine, 18(4), 243–252. doi: 10.18502/ijrm.v13i4.6887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray LK, Dorsey S, Haroz E, Lee C, Alsiary MM, Haydary A, Weiss WM, & Bolton P (2014). A Common Elements Treatment Approach for Adult Mental Health Problems in Low- and Middle-Income Countries. Cognitive and behavioral practice, 21(2), 111–123. 10.1016/j.cbpra.2013.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nes AA, V an Dulmen S Eide E Finset A Kristjansdottir OB Steen IS& Eide H, (2012). The development and feasibility of a web-based intervention with diaries and situational feedback via smartphone to support self-management in patients with diabetes type 2. Diabetes Res Clin Pract, 97(3), 385–393. doi: 10.1016/j.diabres.2012.04.019 [DOI] [PubMed] [Google Scholar]
- Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, Page MJ, … Group P-S (2021). PRISMA-S: A n extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Systematic Reviews, 10(1), 39. doi: 10.1186/s13643-020-01542-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson PJ, Gould DA, & Strosahl KD (2010). Real behavior change in primary care: Improving patient outcomes and increasing job satisfaction Oakland, CA, US: New Harbinger Publications. [Google Scholar]
- Shaw TA, Juncos DG, & Winter D (2020). Piloting a new model for treating music Performance Anxiety: Training a singing teacher to use acceptance and commitment coaching with a student. Frontiers in psychology, 11, 882. doi: 10.3389/fpsyg.2020.00882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spleen AM, Lengerich EJ, Camacho FT, & Vanderpool RC (2014). Health care avoidance among rural populations: R esults from a nationally representative survey. J Rural Health, 30(1), 79–88. doi: 10.1111/jrh.12032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley MA, Wilson NL, Amspoker AB, Kraus-Schuman C, Wagener PD, Calleo JS, Cully JA, Teng E, Rhoades HM, Williams S, Masozera N, Horsfield M, & Kunik ME (2014). Lay providers can deliver effective cognitive behavior therapy for older adults with generalized anxiety disorder: a randomized trial. Depression and anxiety, 31(5), 391–401. 10.1002/da.22239 [DOI] [PubMed] [Google Scholar]
- Stapelfeldt CM, Labriola M, Jensen AB, Andersen NT, Momsen A-MH, & Nielsen CV (2015). Municipal return to work management in cancer survivors undergoing cancer treatment: A protocol on a controlled intervention study. BMC Public Health, 15(1), 1–11. doi: 10.1186/s12889-015-2062-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, … Higgins JP (2016). ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ, 355, i4919. doi: 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, … Higgins JPT (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ, 366, l4898. doi: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- Swain J, Hancock K, Hainsworth C, & Bowman J (2013). Acceptance and Commitment Therapy in the treatment of anxiety: A systematic review. Clinical Psychology Review, 33(8), 965–978. doi: 10.1016/j.cpr.2013.07.002 [DOI] [PubMed] [Google Scholar]
- Tol WA, Augustinavicius J, Carswell K, Leku MR, Adaku A, Brown FL, … van Ommeren M (2018). Feasibility of a guided self-help intervention to reduce psychological distress in South Sudanese refugee women in Uganda. World psychiatry : official journal of the World Psychiatric Association (WPA), 17(2), 234–235. doi: 10.1002/wps.20537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tol WA, Leku MR, Lakin DP, Carswell K, Augustinavicius J, Adaku A, … van Ommeren M (2020). Guided self-help to reduce psychological distress in South Sudanese female refugees in Uganda: A cluster randomised trial. The Lancet Global Health, 8(2), e254–e263. doi: 10.1016/S2214-109X(19)30504-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trompetter HR, Schreurs KM, Heuts PH, & Vollenbroek-Hutten MM (2014). The systematic implementation of acceptance & commitment therapy (ACT) in Dutch multidisciplinary chronic pain rehabilitation. Patient Educ Couns, 96(2), 249–255. doi: 10.1016/j.pec.2014.05.019 [DOI] [PubMed] [Google Scholar]
- Wainberg ML, Scorza P, Shultz JM, Helpman L, Mootz JJ, Johnson KA, … Arbuckle MR (2017). Challenges and opportunities in global mental health: a Research-to-Practice Perspective. Current psychiatry reports, 19(5), 28–28. doi: 10.1007/s11920-017-0780-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson KG, Bordieri MJ, Flynn MK, Lucas NN, & Slater RM (2011). Understanding Acceptance and Commitment Therapy in context: A history of similarities and differences with other cognitive behavior therapies. In Acceptance and Mindfulness in Cognitive Behavior Therapy (pp. 233–263). [Google Scholar]
- Winiarski DA, Rufa AK, & Karnik NS (2019). Using layperson-delivered cognitive-behavioral therapy to address mental health disparities. Psychiatric Annals, 49(8), 353–357. [Google Scholar]
- Yıldız E (2020). The effects of Acceptance and Commitment Therapy in psychosis treatment: A systematic review of randomized controlled trials. Perspectives in Psychiatric Care, 56(1), 149–167. doi: 10.1111/ppc.12396 [DOI] [PubMed] [Google Scholar]
- Zarling A, Bannon S, & Berta M (2019). Evaluation of Acceptance and Commitment T herapy for domestic violence offenders. Psychology of Violence, 9(3), 257–266. doi: 10.1037/vio0000097 [DOI] [Google Scholar]
- Zarling A, & Berta M (2017). An Acceptance and Commitment Therapy Approach for partner aggression. Partner Abuse(1), 89–109. doi: 10.1891/1946-6560.8.1.89 [DOI] [Google Scholar]
- Zeng EY, Heffner JL, Copeland WK, Mull KE, & Bricker JB (2016). Get with the program: Adherence to a smartphone app for smoking cessation. Addict Behav, 63, 120–124. doi: 10.1016/j.addbeh.2016.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zettle RD (2005). The evolution of a contextual approach to therapy: From comprehensive distancing to ACT. International Journal of Behavioral Consultation and Therapy, 1(2), 77–89. doi: 10.1037/h0100736 [DOI] [Google Scholar]


