Abstract
Objective:
Our objective was to review the use of videoconferencing as a practical tool for remote surgical education and to propose a model to overcome the impact of a pandemic on resident training.
Summary Background Data:
In response to the coronavirus disease 2019 pandemic, most institutions and residency programs have been restructured to minimize the number of residents in the hospital as well as their interactions with patients and to promote physical distancing measures. This has resulted in decreased resident operative exposure, responsibility, and autonomy, hindering their educational goals and ability to achieve surgical expertise necessary for independent practice.
Methods:
We conducted a narrative review to explore the use of videoconferencing for remote broadcasting of surgical procedures, telecoaching using surgical videos, telesimulation for surgical skills training, and establishing a didactic lecture series.
Results and Conclusions:
We present a multimodal approach for using practical videoconferencing tools that provide the means for audiovisual communication to help augment residents’ operative experience and limit the impact of self-isolation, redeployment, and limited operative exposure on surgical training.
Keywords: surgical education, training, videoconference, telesimulation, telecoaching
Mini abstract: In response to the COVID-19 pandemic, most institutions have been restructured in ways that have affected surgical training. This review explores the use of videoconferencing as a practical tool for remote surgical education and to propose a model to overcome the impact of a pandemic on resident training.
The coronavirus disease 2019 (COVID-19) pandemic has caused dramatic changes to all facets of healthcare access and delivery, and as a result, healthcare workers and institutions are relentlessly adapting to overcome the many unprecedented challenges.1 As part of the overhaul and restructuring process, healthcare systems and institutions have adopted a “damage-control” response to limit the impact of this devastating illness, by focusing on ensuring the adequate supply of personal protective equipment, human resources, and capacity to handle the constant flow of patients, as well as preventative measures such as physical distancing.2–4 As a result, most surgical departments have temporarily suspended nonurgent surgeries, in accordance with recommendations from local governmental agencies, the American College of Surgeons and other regulatory bodies, and have implemented redeployment protocols to redistribute human resources where they are most needed.5–8 Surgical trainees have been an integral part of the response to COVID-19 with many institutions adopting unique models to restructure residency programs to minimize the daily number of residents in the hospital as well as the frequency of interactions with patients.9
Although these measures have maximized physical distancing and promoted flattening of the COVID-19 incidence curve, it has also affected training and the development of surgical expertise amongst residents. The cancelation and postponement of scheduled surgeries means that many residents who had planned to rotate on specific subspecialty rotations may not have opportunities to do so. Often these rotations are the only exposure residents would obtain throughout their residency, confounding a problem already present by lower case volumes for more specialized procedures. The lack of patient care and operative experience can leave trainees with a gap in their surgical training and limited exposure to unique and rare surgical pathologies that are vital for their training. Furthermore, the atmosphere within the operative theater has become increasingly more stressful where the central objective is to perform the procedure in a safe and expeditious manner and limit the operating team’s exposure to patients. This results in residents having decreased intraoperative responsibility and autonomy, often requiring 2 attending surgeons to double-scrub on more complex cases to minimize operating time. Most hospitals have also implemented restrictions to limit the number of nonessential healthcare workers into and out of the operating room to minimize the risk of transmission and to preserve personal protective equipment. Consequently, many residents do not have opportunities to observe, let alone scrub, on cases.
Theories of professional expertise suggest that learning is fostered through a continuous process of “experiencing, reflecting, thinking, and acting,” whereby new experiences provide learners with new data that are assimilated into their mental model.10 This cycle continues until, over time, a level of understanding is reached that allows a surgeon to retrieve this knowledge quickly, adaptively, flexibility, and creatively for unique and related operative scenarios. For instance, an endocrine surgery rotation provides a limited but unique experience for understanding the complex intricacies of neck anatomy. A lack of participation in such cases will severely limit graduating residents’ ability to acquire the necessary expertise to independently manage surgical pathologies in the neck (eg, penetrating neck trauma). There is therefore a need to augment surgical training, not only for redeployment of human resources to handle the clinical challenges of the pandemic but also to ensure that residents’ educational objectives continue to be met by actively engaging them throughout all aspects of the operative experience. This review summarizes the use of videoconferencing as a practical tool for surgical education to limit the impact of self-isolation, redeployment, and limited operative exposure on surgical training during a pandemic.
VIDEOCONFERENCING
To overcome these unprecedented educational challenges during the COVID-19 pandemic, advances in distance communication technology can be leveraged to help alleviate the impact on surgical education by providing the means for remote and meaningful interactions between mentors and mentees to promote educational objectives while adhering to restrictions in physical distancing. This includes simple audiovisual communication (eg, videoconferencing), as well as interfaces that can accommodate more advanced functions, such as telestration. Our institution has begun implementing a multimodal approach using videoconferencing tools to augment residents’ operative experience (Fig. 1). In this model, videoconferencing is used for: (1) remote broadcasting of surgical procedures; (2) telecoaching using surgical videos; (3) telesimulation for surgical skills training; and (4) didactic lecture series.
FIGURE 1.
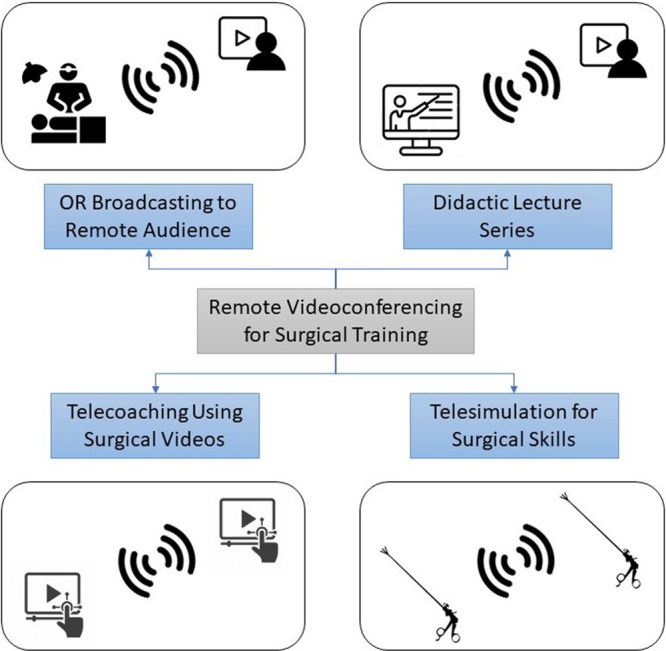
A multimodal approach using videoconferencing tools to augment residents’ operative experience through remote broadcasting of surgical procedures, telecoaching using surgical videos, telesimulation for surgical skills training, and didactic lecture series.
Remote OR Broadcasting
Although it may not be possible to bring some residents into the operating room to watch or be actively engaged, it is certainly possible to broadcast procedures to members of the surgical team remotely. The availability of advanced digital intraoperative cameras and endoscopy can provide high-definition video feeds that provide pristine views of the surgical anatomy. As a result, live streaming of surgical videos has proven to be a highly valuable asset in surgical education and an increasingly common method for continuing professional development activities in the surgical community.11,12 By having an infrastructure that permits residents to have a virtual presence in the OR, staff surgeons can engage with them and provide real-time teaching. For image-guided surgeries, many new operating suites come equipped with an integrated digital platform whose video feed can be broadcasted. Although not all institutions have this capability, several commercially available platforms can also be linked to provide views of both the surgical field and the operating room for a virtual presence (Fig. 2). These systems are often equipped with a microphone and speakers such that members of the audience can freely interact with the operating team. Open procedures tend to be more challenging due to the innate difficulty of obtaining the optimal camera angle, image resolution, and focus. In such instances, telemedicine platforms that contain cameras often have powerful zoom functions and resolution and can be positioned accordingly to view the area of interest. Some platforms even provide the capability of remote control of the camera angle and zoom to minimize any interference with the surgical workflow. Other options include the use of head-mounted cameras worn by the surgical team for recording or live streaming of open procedures. To optimize the educational value of a broadcasted operation, it may also be more valuable to have a moderator surgeon who can provide ongoing commentary and answer questions to the group during the case. Regardless of the approach or platform, it is critical for educators to be familiar with institutional protocols for ethics approval and patient consent, and to adhere to patient privacy standards when sharing this data (eg, Health Insurance Portability and Accountability Act [USA] and Personal Health Information Protection Act [Ontario, Canada]).
FIGURE 2.

An example of a laparoscopic low anterior resection remotely broadcasted live to an audience of surgical residents with video feeds from a camera in the operating theater and from the endoscopy platform.
Aside for the technological and logistical challenges, live broadcasting of surgical cases can have several drawbacks, including interference with the operating team, workflow, surgical performance, and potentially patient outcomes. Synchronized Deferred Live Surgery has emerged as an alternative solution to recreate the live surgical environment by recording a procedure using multiple cameras.13 The procedure can therefore be watched and paused for discussion at the audience’s pace with a moderator. This model also overcomes most trainees and audience members’ hesitation with asking questions.
Telecoaching Using Surgical Videos
There is an abundance of e-learning platforms available to surgical trainees on both computers and mobile devices, many of which provide large libraries of procedures for residents to watch and learn from.14 Although this can be a great source of information for residents’ self-directed learning, without active experiential learning, these surgical videos and e-learning platforms have limited educational value. Evidence suggests that professional expertise in complex tasks is attained and retained when learners engage in deliberate practice of specific and measurable competencies—that is by focusing on difficult aspects and areas of weakness, receiving immediate, and focused feedback on performance and ample opportunities for repetitions.15 By providing a trainee the means to be more intentional about how they think and behave, this form of training can lead to more long-term and robust learning.
Remote telestration using surgical videos has shown to be a more deliberate method of improving advanced cognitive skills.16,17 In this simulation exercise, a moderator shares surgical videos with trainees. Instead of simply watching the video as a group, the video is paused at specific time-points and trainees are prompted to make critical decisions throughout the case, specifically by making annotations (free-hand drawing) on the surgical field (Fig. 3), with subsequent assessment and feedback on their decisions by the moderator. For instance, trainees are asked to describe the best plane of dissection, the location of critical anatomical structures, or the optimal location and vector of retraction. In this manner, participants are deliberately practicing and committing themselves to making intraoperative decisions while getting immediate feedback on the results of their decisions, with multiple opportunities for repetition—a phenomenon that is often neglected, but all-too critical to the acquisition of expertise. This form of training by using visual concordance of annotations on a surgical canvas has shown to be a very promising method of improving intraoperative judgment.18,19
FIGURE 3.
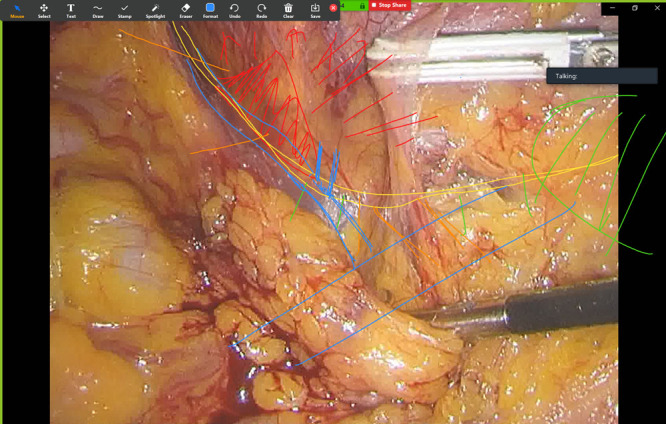
Example of telecoaching using surgical videos for laparoscopic transabdominal adrenalectomy. The coach prompts multiple audience members to actively engage by making annotations on the surgical field, with real-time feedback on their situational awareness and decision-making.
Telesimulation for Technical Skills
Deliberate practice, refinement and retention of technical skills are an added challenge for surgical trainees during a pandemic. Telesimulation is a method of linking instructors to learners at a distant location, to provide real-time training and feedback with a focus on the psychomotor domain of surgical performance. Telesimulation also offers a trainee-centered approach to surgical education by tailoring instruction to prioritize the individual objectives of each learner. This simulated experience is an opportunity for residents to evaluate, refine, and enhance the mental models that can improve operative performance in real life. Telesimulation has been shown to be a cost-effective way of teaching the Fundamentals of Laparoscopic Surgery skills in resource-restricted countries and can be applied to any setting with internet access.20 It is particularly well-suited for scenarios requiring self-isolation and physical distancing, where remote linking of simulators can facilitate demonstration and hands-on practice of skills between 2 parties.
Trainees are provided with a laparoscopic box trainer, all essential equipment (ie, penrose drains, sutures, and needle drivers), and are connected with a surgeon-mentor using basic videoconferencing technology (Fig. 4). A duplicate box trainer is used by the surgeon to demonstrate the correct manner in which fundamental skills, such as intracorporeal suturing and knot tying, are to be performed. This is followed by repetitive practice and learner-specific feedback. Residents are encouraged to continue to practice at home and are invited to several follow-up sessions to maximize retention and optimize performance. The availability of a laparoscopic skills simulator at home also facilitates independent learning as on-site training facilities, such as simulation centers, may be closed during a pandemic and not readily accessible to residents. Telesimulation is a portable, accessible, convenient, and relatively inexpensive solution to support surgical skills training, especially during periods of resource limitation such as a pandemic. This approach can also be modified using different simulators and webcams to teach many different technical skills.21,22
FIGURE 4.
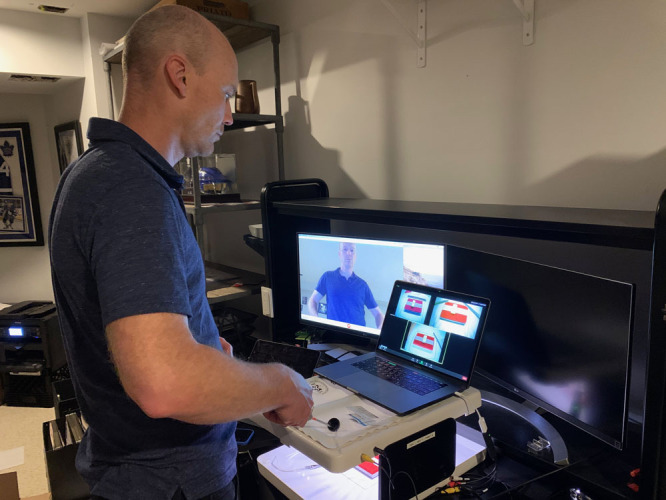
Telesimulation provides real-time training and feedback with a focus on the psychomotor domain of surgical performance. In this example, residents and proctors are provided box trainers with inanimate objects and predefined tasks for replicating an intracorporeal anastomosis. The proctor provides live feedback through demonstration and according to the needs of the learner.
Didactic Lectures
Implementing a didactic lecture series is important to supplement the experiential learning offered by remote OR broadcasting, telecoaching, and telesimulation. This can be accomplished by engaging a diverse cohort of surgeons, with unique clinical and research interests, tasked to deliver theory and knowledge about specific surgical conditions or topics related to their area of expertise. The virtual format can facilitate delivery across multiple sites, thereby targeting a larger body of trainees, from medical students to senior residents. Besides faculty-led didactics, there are a multitude of other e-learning platforms that can provide free, online education for surgical residents during the pandemic. Some examples include the Behind the Knife podcast, Incision Academy, and the Project Quarantine: Surgical Education series sponsored by the American College of Surgeons. The utility of these resources, however, hinges on trainee motivation to allocate self-study time. These platforms also provide a limited opportunity to ask questions and clarify concepts in real-time. At times, their effectiveness is also limited by the large number of attendees (150–200) from across North America, which can preclude any meaningful interaction with the presenter. Our weekly series consists of three to four 60-minute sessions, with a maximum of 15 learners across 2 hospitals. The didactic component of each session is complemented by case-based learning, which has been shown to improve understanding, retention, and application of theoretical concepts into the clinical setting.
ASSESSMENT
In addition to finding creative and practical solutions to training residents, surgical educators are also finding it increasingly challenging to assess residents’ operative performance. The lack of resident participation and engagement in the operating room means there are less opportunities for them to be evaluated on specific competencies and domains of intraoperative performance: psychomotor skills, declarative knowledge, advanced cognitive skills, interpersonal skills, and personal resourcefulness.23 Although videoconferencing cannot fully replace the full operative experience (especially for the nontechnical aspects of an operation), it can help bridge this gap. For instance, psychomotor skills for basic and advanced laparoscopic tasks can be evaluated via telesimulation in a simulated environment.24,25 Also, surgical videos can be used to immerse trainees into operative scenarios, where they can be prompted at various time points to assess their declarative knowledge (eg, recitable facts about relevant anatomy, pathology, and surgical techniques) and more complex tacit knowledge representing higher-order mental processes that determine intraoperative judgment. As a supplement, the Visual Concordance Test provides an objective and measurable metric to remotely evaluate intraoperative decision-making using telestration.18,19 Users are asked to answer specific questions by making annotations on the surgical field (eg, location of critical anatomy, safe planes of dissection) and those annotations are compared to experts’ annotations to yield accuracy scores.
LIMITATIONS
Despite the advantages of using videoconferencing and telementoring technology to supplement residents’ surgical experience, there are several limitations. Notably, face-to-face interactions are more personable and have a greater tendency to develop a trusting and longitudinal mentor–mentee relationship, which is critical to the learning process. In contrast, audiovisual communication through computer platforms, while promising and successful in many ways, do not provide the same degree of social interaction that fosters this relationship. The lack of presence and activity in the surgical field also leads to limited kinesthetic and tactile feedback that is necessary to develop trainees’ mental model of surgical anatomy. Furthermore, most videoconferencing platforms require adequate Wi-Fi connectivity and bandwidth to provide high-quality video feeds, which may not always be available in every geographic location. Regardless of whether it is used to augment learning or assessment, videoconferencing will not replace the full operative experience and these strategies are only meant to minimize the impact of a pandemic on resident training. Consistent, deliberate and focused practice in the operating room remains the cornerstone of acquiring surgical expertise.
Another important consideration is patient confidentiality and the use of software that meet privacy standards for recording surgical videos and broadcasting procedures, either live or deferred-live fashion. Although most institutions have protocols and consent forms for using deidentified videos for educational and quality-improvement, these typically do not involve live broadcasting. Institutional ethics review is typically required, along with the use of platforms that adhere to patient privacy standards. Finally, implementing videoconferencing into surgical curricula can be costly both from a material and human resources standpoint, especially when deploying integrated systems and telemedicine platforms with built in cameras, microphones, and speakers. Nevertheless, many videoconferencing platforms are available for free and provide easy solutions for training programs wishing to use preobtained surgical videos for telecoaching and deferred live broadcasting. It is also challenging recruiting faculty to commit their time to engage in educational activities.
CONCLUSION
The COVID-19 pandemic has resulted in many unprecedented challenges, leading to substantive changes to surgical care models and restructuring of residency programs. This has led to decreased resident operative exposure and autonomy, hindering their educational goals and ability to achieve surgical expertise for independent practice. By adhering to best-practices in education, videoconferencing technology can help limit the overwhelming impact felt by surgeons-in-training around the world. Specifically, audiovisual telecommunication can augment residents’ operative learning, assist with evaluating operative performance and limit the impact of self-isolation, redeployment, and limited operative exposure on surgical training.
Footnotes
Disclosure: A.O. has received honoraria for speaking and teaching from Medtronic, Ethicon, and Merck. The other authors declare that they have nothing to disclose.
REFERENCES
- 1.Lancaster EM, Sosa JA, Sammann A, et al. Rapid response of an academic surgical department to the COVID-19 pandemic: implications for patients, surgeons, and the community. J Am Coll Surg. 2020; 230:1064–1073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zarzaur BL, Stahl CC, Greenberg JA, et al. Blueprint for restructuring a department of surgery in concert with the health care system during a pandemic: the University of Wisconsin experience. JAMA Surg. 2020; 155:628–635 [DOI] [PubMed] [Google Scholar]
- 3.Arora KS, Mauch JT, Gibson KS. Labor and delivery visitor policies during the COVID-19 pandemic: balancing risks and benefits. JAMA. 2020; 323:2468–2469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goh KJ, Wong J, Tien JC, et al. Preparing your intensive care unit for the COVID-19 pandemic: practical considerations and strategies. Crit Care. 2020; 24:215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iacobucci G. Covid-19: all non-urgent elective surgery is suspended for at least three months in England. BMJ. 2020; 368:m1106. [DOI] [PubMed] [Google Scholar]
- 6.Angelos P. Surgeons, ethics, and COVID-19: early lessons learned. J Am Coll Surg. 2020; 230:1119–1120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American College of Surgeons. COVID-19: Elective Case Triage Guidelines for Surgical Care. 2020. Available at: https://www.facs.org/covid-19/clinical-guidance/elective-case. Accessed June 12, 2020
- 8.Urbach DR, Martin D. Confronting the COVID-19 surgery crisis: time for transformational change. CMAJ. 2020; 192:E585–E586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coons BE, Tam SF, Okochi S. Rapid development of resident-led procedural response teams to support patient care during the Coronavirus disease 2019 epidemic: a surgical workforce activation team. JAMA Surg. 2020; 155:683–684 [DOI] [PubMed] [Google Scholar]
- 10.Kolb D. Experiential Learning: Experience as the Source of Learning and Development. 1984, Prentice Hall [Google Scholar]
- 11.Lacy AM, Martin-Perez B, Diaz-DelGobbo G, et al. The present and future of surgical education - a video vignette. Colorectal Dis. 2017; 19:303–304 [DOI] [PubMed] [Google Scholar]
- 12.Knol J. Atallah S. Video-based training apps and deferred live surgery. Transanal Minimally Invasive Surgery (TAMIS) and Transanal Total Mesorectal Excision (taTME). 2019, Springer; 475–484 [Google Scholar]
- 13.Knol J, Bonjer J, Houben B, et al. New paradigm of live surgical education: synchronized deferred live surgery. J Am Coll Surg. 2018; 227:467–473 [DOI] [PubMed] [Google Scholar]
- 14.Maertens H, Madani A, Landry T, et al. Systematic review of e-learning for surgical training. Br J Surg. 2016; 103:1428–1437 [DOI] [PubMed] [Google Scholar]
- 15.Ericsson KA. Deliberate practice and acquisition of expert performance: a general overview. Acad Emerg Med. 2008; 15:988–994 [DOI] [PubMed] [Google Scholar]
- 16.Madani A, Grover K, Watanabe Y. Measuring and teaching intraoperative decision-making using the visual concordance test: deliberate practice of advanced cognitive skills. JAMA Surg. 2020; 155:78–79 [DOI] [PubMed] [Google Scholar]
- 17.Madani A, Keller DS. Assessing and improving intraoperative judgement. Br J Surg. 2019; 106:1723–1725 [DOI] [PubMed] [Google Scholar]
- 18.Madani A, Gornitsky J, Watanabe Y, et al. Measuring decision-making during thyroidectomy: validity evidence for a web-based assessment tool. World J Surg. 2018; 42:376–383 [DOI] [PubMed] [Google Scholar]
- 19.Madani A, Watanabe Y, Bilgic E, et al. Measuring intra-operative decision-making during laparoscopic cholecystectomy: validity evidence for a novel interactive web-based assessment tool. Surg Endosc. 2017; 31:1203–1212 [DOI] [PubMed] [Google Scholar]
- 20.Okrainec A, Henao O, Azzie G. Telesimulation: an effective method for teaching the fundamentals of laparoscopic surgery in resource-restricted countries. Surg Endosc. 2010; 24:417–422 [DOI] [PubMed] [Google Scholar]
- 21.Burckett-St.Laurent DA, Burckett-St. Laurent DA, Cunningham MS, et al. Teaching ultrasound-guided regional anesthesia remotely: a feasibility study. Acta Anaesthesiol Scand. 2016; 60:995–1002 [DOI] [PubMed] [Google Scholar]
- 22.Mikrogianakis A, Kam A, Silver S, et al. Telesimulation: an innovative and effective tool for teaching novel intraosseous insertion techniques in developing countries. Acad Emerg Med. 2011; 18:420–427 [DOI] [PubMed] [Google Scholar]
- 23.Madani A, Vassiliou MC, Watanabe Y, et al. What are the principles that guide behaviors in the operating room?: creating a framework to define and measure performance. Ann Surg. 2017; 265:255–267 [DOI] [PubMed] [Google Scholar]
- 24.Choy I, Fecso A, Kwong J, et al. Remote evaluation of laparoscopic performance using the global operative assessment of laparoscopic skills. Surg Endosc. 2013; 27:378–383 [DOI] [PubMed] [Google Scholar]
- 25.Okrainec A, Vassiliou M, Jimenez MC, et al. Remote FLS testing in the real world: ready for “prime time”. Surg Endosc. 2016; 30:2697–2702 [DOI] [PubMed] [Google Scholar]


