Purpose of review
This article recounts the history of the diet-heart hypothesis from the late 1950s up to the current day, with revelations that have never before been published in the scientific literature. Insights include the role of authorities in launching the diet-hypothesis, including a potential conflict of interest for the American Heart Association; a number of crucial details regarding studies considered influential to the hypothesis; irregularities in the scientific reviews on saturated fats, for both the 2015 and 2020 Dietary Guidelines for Americans; and possible conflicts of interest on the relevant subcommittee reviewing saturated fats for the 2020 Dietary Guidelines Advisory Committee. Information obtained via the Freedom of Information Act (FOIA) on emails from the 2015 process is published here for the first time. These findings are highly relevant to the 2025–2030 Dietary Guidelines process, now underway, which has plans for a new review on saturated fats.
Recent findings
Recent findings include shortcomings in the scientific review processes on saturated fats, for both the current 2020–2025 Dietary Guidelines for Americans and the previous edition (2015–2020). Revelations include the fact the 2015 Advisory Committee acknowledged, in an e-mail, the lack of scientific justification for any specific numeric cap on these fats. Other, previously unpublished findings include significant potential financial conflicts on the relevant 2020 guidelines subcommittee, including the participation of plant-based advocates, an expert who promotes a plant-based diet for religious reasons, experts who had received extensive funding from industries, such as tree nuts and soy, whose products benefit from continued policy recommendations favoring polyunsaturated fats, and one expert who had spent more than 50 years of her career dedicated to ‘proving’ the diet-heart hypothesis.
Summary
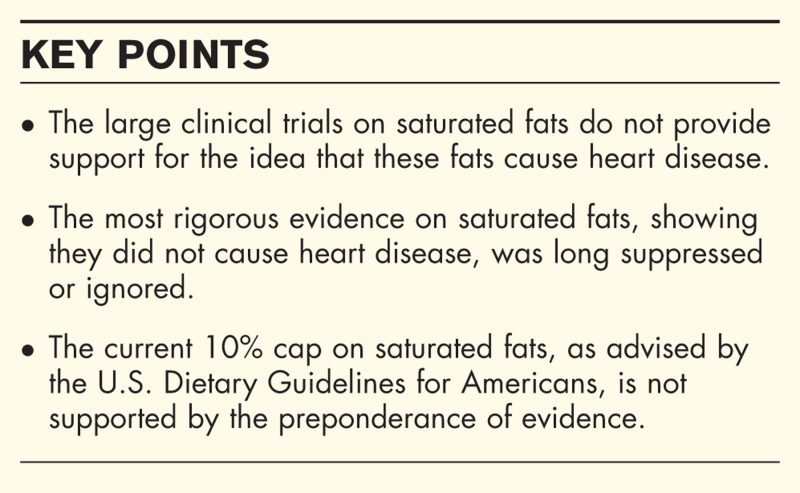
The idea that saturated fats cause heart disease, called the diet-heart hypothesis, was introduced in the 1950s, based on weak, associational evidence. Subsequent clinical trials attempting to substantiate this hypothesis could never establish a causal link. However, these clinical-trial data were largely ignored for decades, until journalists brought them to light about a decade ago. Subsequent reexaminations of this evidence by nutrition experts have now been published in >20 review papers, which have largely concluded that saturated fats have no effect on cardiovascular disease, cardiovascular mortality or total mortality. The current challenge is for this new consensus on saturated fats to be recognized by policy makers, who, in the United States, have shown marked resistance to the introduction of the new evidence. In the case of the 2020 Dietary Guidelines, experts have been found even to deny their own evidence. The global re-evaluation of saturated fats that has occurred over the past decade implies that caps on these fats are not warranted and should no longer be part of national dietary guidelines. Conflicts of interest and longstanding biases stand in the way of updating dietary policy to reflect the current evidence.
Keywords: dietary guidelines, food policy, polyunsaturated fats, saturated fats
INTRODUCTION
The concept that saturated fat causes cardiovascular disease by raising serum cholesterol is called the ‘diet-heart hypothesis’, a highly influential idea that has been a lynchpin of nutrition policy for some 60 years. This hypothesis remains today a foundation of public health policy, with nearly all dietary guidelines worldwide recommending a cap on saturated fat consumption as a primary measure of protection against heart disease. Over the past 12 years, however, there has been a major shift in scholarly understanding of these fats, with now >20 review papers, by independent teams of scientists, on the whole concluding that saturated fats have no effect on major cardiovascular outcomes, including heart attacks, strokes or cardiovascular mortality, or total mortality. National dietary guidelines have not recognized this new thinking on saturated fats, however, and continue to promote policies based on outdated or insufficient evidence.
Box 1.
no caption available
HISTORICAL PERSPECTIVE ON DIETARY SATURATED FAT
The diet-heart hypothesis was first proposed in the 1950s by Ancel Keys, a physiologist at the University of Minnesota with an interest in nutrition [1]. Keys based his idea on a handful of small feeding experiments conducted on humans together with some animal data suggesting that high blood cholesterol caused fatty deposits of the type thought to clog arteries and cause heart attacks [2]. Keys had further observed, on travels through post-War Europe, that less wealthy populations in Sardinia, Naples, and Spain, appeared to suffer lower rates of heat attacks while consuming diets low in saturated fat-rich foods, such as meat and dairy [3–5]. Keys postulated that saturated fat and cholesterol caused heart disease – his diet-heart hypothesis – whose claims he asserted in no fewer than 20 papers in 1957 and 1958 [2]. Keys has been widely described by his colleagues as having a highly persuasive, even aggressive, personality, and these attributes may have in part allowed him to ensure that his idea edged out competing hypotheses to become the dominant paradigm explaining cardiovascular disease for the next 70 years.
One authority whom Keys successfully won over was Paul Dudley White, an influential cardiologist and the personal doctor for President Dwight D. Eisenhower. When Eisenhower suffered the first of several heart attacks, in September 1955, Keys’ ideas were elevated by White into the national spotlight [1]. With the President hospitalized, the nation became laser-focused on the question of what caused heart disease, a relatively new and terrifying condition that had been rare in the early 1900s yet had risen by the 1950s to become the country's leading cause of death. White made it clear that diet was to blame. Under his guidance, Eisenhower undertook a new regimen, low in cholesterol and saturated fats. As charted in news headlines across the nation, Eisenhower shunned butter for polyunsaturated margarine and ate melba toast for breakfast [2].
The second authority that came to adopt the diet-heart hypothesis was ultimately more enduring in its influence. This was the American Heart Association (AHA), the nation's largest nonprofit organization and long a respected leader in the field of heart disease. White had been an AHA founder, and Eisenhower hosted fundraisers for the group in the White House [2]. Throughout the 1950s, the AHA had resisted giving advice on heart disease prevention, citing a lack of evidence, yet in 1960, Keys was appointed to the group's nutrition committee, and one year later, although no greater evidence could be cited, he had convinced his colleagues to recommend his idea as official AHA policy. Thus, from 1961 on, the AHA recommended that all men (and subsequently women) decrease their consumption of saturated fat, replacing these fats whenever possible with polyunsaturated vegetable oils, as the most promising measure of protection against heart disease [6].
The 1961 AHA advice to limit saturated fat is arguably the single-most influential nutrition policy ever published, as it came to be adopted first by the U.S. government, as official policy for all Americans, in 1980, and then by governments around the world as well as the World Health Organization. It is worth noting that the AHA had a significant conflict of interest, since in 1948, it had received $1.7 million, or about $20 million in today's dollars, from Procter & Gamble (P&G), the makers of Crisco oil [2]. This donation was transformative for the AHA, propelling what was a small group into a national organization; the P&G funds were the ‘bang of big bucks’ that ‘launched’ the group, according to the organization's own official history [7]. Vegetable oils such as Crisco have reaped the benefits of this recommendation ever since, as Americans increased their consumption of these oils by nearly 90% from 1970 to 2014 [8].
THE SEVEN COUNTRIES STUDY
The Seven Countries Study (SCS), led by Keys, was for many decades considered the bedrock data for the diet-heart hypothesis [9]. Launched in 1957, the study was larger and more ambitious than any U.S. nutrition study to date. By 2004, according to one estimate, SCS had already been cited more than one million times [2]. The SCS followed some 12 770 men in 16 locations within seven countries, including Italy, Greece, Yugoslavia, Finland, the Netherlands, the United States and Japan. Keys, due to his worldwide travels, knew that choosing these countries was likely to confirm his hypothesis. He did not include, for instance, places like Germany, Switzerland, and France, where people ate a great deal of saturated fat yet experienced rates of heart disease similarly low to those included in the SCS. Keys’ selection of nations has given rise to the critique that he ‘cherry picked’ countries to ‘prove’ his hypothesis. While defenders of the SCS have attempted to dismiss this allegation [10], it remains true that Keys used a nonrandom approach for the selection of countries in SCS, allowing for the introduction of bias [11].
In 1975, when Keys published his results in a special issue of an AHA journal, he found as he had hoped: a strong correlation between the consumption of saturated fat and deaths from heart disease. The SCS was a groundbreaking study in its scope: one of its accomplishments was simply to demonstrate that people living in different nations really did suffer vastly different rates of heart attacks and that therefore the disease could potentially be prevented. Subsequent analyses of the SCS have found numerous shortcomings in the data, however. For instance, Keys sampled dietary data from only 3.9% of the men, which is fewer than 500 total participants, or about 30 per location [2]. Further he used unvalidated and nonstandardized methods of dietary evaluation that differed across groups. On Crete, one of the dietary samples was taken during the period of Lent, which was strictly observed under the Greek Orthodox church and would have banned ‘all animal foods’ [12]. Saturated fats were therefore very likely undercounted in this population, yet Keys downplayed this issue in his report and concluded that the excellent health of the Cretans could be credited to their low consumption of these fats. The failure to adjust for the Lent data was a ‘remarkable and troublesome omission,’ wrote researchers in Public Health Nutrition in 2005 [13], yet this analysis took place long after the diet-heart hypothesis had become solidified as public policy.
In 1989, a re-analysis of the SCS data by some of the original study researchers found that coronary mortality best correlated not with saturated fats, as originally reported, but with ‘sweets,’ defined as sugar products and pastries [14]. Possibly the correlation would have been even stronger if the ‘sweets’ category had included chocolate, ice cream, and soft drinks, but researchers said data on these items were too difficult to combine [2].
Ultimately, the principal limitation of the SCS data was that they could only show an association, not a cause-and-effect relationship. The results of the SCS have never been independently analyzed, and most subsequent studies using similar approaches have failed to confirm its conclusions, as described below.
STUDIES ON SATURATED FATS
Governments around the world, including the United States, Norway, Finland, and Australia, among other countries, recognized the need for more rigorous, clinical trial data that could establish a causal relationship between saturated fat and heart disease. Large, randomized, controlled clinical trials (RCTs) were undertaken in the 1960s and 1970s, in which saturated fats were replaced by polyunsaturated fats from vegetable oils. Altogether, these ‘core’ trials tested the diet-heart hypothesis on about 67 000 people [15] and were especially important, because they assessed long-term clinical outcomes, that is, ‘hard endpoints,’ such as heart attacks and death. These outcomes are considered more reliable for making public health policy compared to studies that use ‘intermediary endpoints,’ such as cholesterol or inflammatory measures, whose value for predicting cardiovascular events is disputed.
These trials provided surprisingly little support for the diet-heart hypothesis. Dramatic reductions in the consumption of saturated fats had successfully lowered the participants’ cholesterol, by an average of 29 mg/dl, ‘indicating a high level of compliance’ among subjects, according to one analysis [16], yet the expected reductions in either cardiovascular or total mortality were not observed in most trials [15]. In other words, although diet could successfully lower blood cholesterol, this reduction did not appear to translate into long-term cardiovascular gains.
By the time these results emerged, however, Keys’ hypothesis had already gained widespread acceptance among his colleagues, including, importantly, leadership at the National Institutes of Health (NIH) [2]. By the late 1960s, a bias in favor of the diet-heart hypothesis was strong enough that researchers with contrary results found themselves unable or unwilling to publish their results. For instance, the largest test of the diet-heart hypothesis, the Minnesota Coronary Survey, involving 9057 men and women over 4.5 years, tested a diet of 18% saturated fat against controls eating 9%, yet did not find any reduction in cardiovascular events, cardiovascular deaths, or total mortality [17]. Although the study had been funded by the NIH, the results were not published for 16 years, after the principal investigator, Ivan Frantz, had retired. Frantz is reported to have said that there was nothing wrong with the study; ‘We were just disappointed in the way it came out’ [1]. Frantz's decision not to publish his results in a timely manner resulted in these contradictory data not being considered for another 40 years [18].
Other results that went unpublished were from one of the most famous heart disease investigations ever undertaken, the Framingham Heart Study, begun in 1948. Vanderbilt University professor George Mann led a dietary investigation, collecting detailed food-consumption data from 1049 subjects [19]. When he calculated the results in 1960, it was very clear that saturated fat was not related to heart disease. Concerning the incidence of coronary heart disease and diet, the authors concluded, simply, ‘No relationship found’ [20]. However, not until 1992 did a Framingham study leader publicly acknowledge the study's findings on fat. ‘In Framingham, Mass, the more saturated fat one ate. … the lower the person's serum cholesterol… and [they] weighed the least,’ wrote William P. Castelli, one of the Framingham directors, in an informal commentary [21]. As a consequence of the nonpublication or disregard of study findings contrary to the diet-heart hypothesis, the idea that saturated fat had possibly been unduly vilified was for decades not seriously considered by most nutrition experts.
RECONSIDERATION OF THE TRIALS ON SATURATED FATS
Reviews and books critical of the diet-heart hypothesis were not unknown in the 1960s and 1970s, including a publication by a former editor of the Journal of the American Heart Association[22] and articles by other prominent scientists [23–25]. They argued that the hypothesis was not supported by the available data and was contradicted by numerous observations. Over time, however, these critics were effectively marginalized and silenced [2]. Not until the 2000s did this science again come to light, mainly through the work of journalist Gary Taubes [26,27]. The first comprehensive compilation of arguments about why saturated fats are not bad for health was published by this author, also a journalist [2].
The earliest formal analyses of the early data on saturated fats were led by Ronald M. Krauss, a cardiologist and nutrition expert, and published in two papers in the American Journal of Clinical Nutrition in 2010 [28,29]. Krauss experienced formidable hurdles in the peer-review process, evidently due to widespread resistance to re-evaluating a long-standing hypothesis [2]. A colleague of Keys’ attempted to rebut these papers [30], yet soon thereafter, other scientists joined Krauss in reassessing the same data. Results from the core trials have now been analyzed extensively by scientists worldwide, including by the prestigious Cochrane group, most recently in 2020. Altogether, >20 review papers, including umbrella reviews, have been published, with the vast majority concluding that the data from randomized, controlled trials do not provide consistent or adequate evidence for continued recommendations limiting the intake of saturated fat [15].
A few reviews have had findings to the contrary [31,32], yet these have mainly been explained by the inclusion of one trial, called the Finnish Mental Hospital Study, which lacked proper randomization, among other problems, and was therefore excluded in more recent reviews [16]. The finding in Cochrane 2020 of an effect on cardiovascular events disappeared when subjected to a sensitivity analysis inside the report, in which studies that had not successfully reduced saturated fats were excluded [33▪▪]. Reviews that have focused on LDL-cholesterol have ignored the far more definitive, long-term outcomes of cardiovascular events and mortality [31,32]. Overall, therefore, despite extensive testing of the diet-heart hypothesis, the data do not support continued advice to restrict these fats for the prevention of heart disease.
The findings from observational or epidemiological studies constitute less robust data, since these studies are usually limited to demonstrating associations rather than cause-and-effect relationships. However, substantial epidemiological findings that contradict a hypothesis provide reasonable evidence that the hypothesis may be in error. Data from the largest-ever epidemiological cohort study ever conducted, called Prospective Urban Rural Epidemiology (PURE), provides this type of contradictory evidence regarding the diet-heart hypothesis. PURE followed individuals aged 35–70 years, from 2003 to 2013, in 18 countries with a median follow-up of 7 4 years. The PURE investigators found that saturated fat was not associated with risk of myocardial infarction or cardiovascular disease mortality and was significantly associated with lower total mortality as well as lower risk of stroke [34]. This last finding, on stroke, is particularly significant, as it is consistent with other observational studies [35], and saturated fat is the only type of fat found to have a positive effect on this important cardiovascular health outcome. Further, nine reviews of the observational data conducted since 2010 have found no significant associations between the consumption of these fats and coronary heart disease [15].
Epidemiological data of this quality and magnitude meaningfully contribute to the understanding of the relationship between saturated fats and cardiovascular disease. These data reinforce the findings from the more rigorous, clinical trial data, described above.
Despite these extensive findings disproving a relationship between saturated fats and heart disease, speculation about the diet-heart hypothesis continues. For instance, the AHA journal Circulation published findings of an association between linoleic fatty acid, a prominent component of vegetable oils, and a lower incidence of cardiovascular events and mortality [36]. However, this finding is based on nonstandardized, country-level (ecological) data, which is generally regarded to be among the lowest-quality type of evidence.
U.S. DIETARY GUIDELINES ON SATURATED FATS
The U.S. government was the first in the world to recommend saturated-fat restriction. The United States Senate Select Committee on Nutrition and Human Needs published the Dietary Goals for the United States in 1977, which recommended that the public ‘reduce saturated fat consumption to account for about 10% of total energy intake …’ [37]. The report was heavily influenced by experts from the AHA and was written by a single Senate staffer with no background in science or nutrition [26]. An early draft of the report further recommended that people ‘decrease consumption of meat,’ based on its saturated fat content. This advice was revised to read: ‘choose meats … which will reduce saturated fat intake’, leading to an emphasis in favor of ‘lean meat.’ Some observers have interpreted this revision to be exclusively due to the interference of the meat industry, yet a 2014 article in the American Journal of Public Health that examined the Senate committee process in detail concludes that ‘a lack of scientific consensus’ was the principal reason for the change in language on meat [38]. This latter interpretation also reflects the absence of rigorous data linking saturated fats to heart disease, as described above.
The Dietary Goals led to the establishment of a policy, co-issued by the U.S. Departments of Agriculture and Health and Human Services (USDA-HHS), called the Dietary Guidelines for Americans (DGA), first published in 1980 and every 5 years since [39]. The inaugural edition of the guidelines included advice to ‘Avoid too much fat, saturated fat, and cholesterol’ but did not include a specific numerical cap on saturated fats. The 1990 guidelines and all subsequent editions have included the target of limiting these fats to 10% of total calories or less.
According to U.S. law, the DGA must reflect ‘the preponderance of the scientific and medical knowledge which is current at the time the report is prepared’ [40]. The subject of saturated fats presents a unique difficulty, however, since the original core trials concluded before the guidelines began. A review of all the DGA expert reports found that none of the expert committees appointed to review the science for each new edition of the guidelines had ever undertaken a direct, systematic review of these core trials on saturated fats [41]. The guidelines had simply inherited the widely held view that saturated fats were linked to cardiovascular disease without its own novel review of the science.
A growing awareness of the core trials from the year 2010 onwards should arguably have spurred one of the subsequent Dietary Guidelines Advisory Committees (DGACs) to initiate a systematic review of these major trials, yet none has occurred. The 2015 DGAC decided at a late stage in the DGA process to undertake a new review of saturated fats, in response to the publication of a review paper on this topic, with authors including professors from Cambridge and Harvard Universities [42], and a prominent article in the Wall Street Journal on the same topic [43]. Both publications suggested a lack of evidence linking saturated fats to heart disease. The DGAC decision to initiate a review of saturated fats was revealed in emails obtained through a request made under the Freedom of Information Act and reflects a discomfort among some DGAC members that these publications ‘contradict[ed] the AHA conclusions’ on saturated fats [44]. DGAC Vice-Chair, Alice Lichtenstein, a Tufts University scientist who had also twice chaired the AHA nutrition committee, suggested in an E-Mail to other DGAC members that they set a numerical cap on saturated fats, even though, she wrote, ‘There is no magic/data for the 10% number or 7% number that has been used previously’ [45].
The 2015 DGAC analysis of saturated fats resulting from this e-mail exchange was a narrative, nonsystematic review of seven external review papers [46]. Two analyses of this 2015 DGAC review found it to have omitted at least one paper with null findings on saturated fat while inappropriately including other papers that supported advice to promote vegetable oils over saturated fats [11,33▪▪]. In one instance, the DGAC included a paper that looked exclusively at linoleic acid, not saturated fats [47]. In another instance, a review paper was included that relied heavily on the Finnish Mental Hospital Study, whose data, for reasons discussed above, had been deemed unreliable [16]. The result was evidently a DGAC review that did not provide a balanced or thorough evaluation of the external review papers current at the time the 2015 report was prepared. The 2015 DGAC concluded that the evidence for a relationship between saturated fats and heart disease was ‘strong.’
For the 2020 guidelines, the DGAC also conducted a review of saturated fats [48]. A recent analysis of the studies included in this review found that 88% did not support a link between these fats and heart disease [33▪▪]. Due to a new rule introduced by the USDA for this guidelines process, the 2020 DGAC was not allowed to examine external review papers and was therefore unable to consider any of the approximately 20 review papers described above. Top experts in the field attempted to introduce this evidence via written comments submitted formally to the USDA [33▪▪], in addition to meeting with the relevant senior staff members at both HHS and USDA, and submitting a letter to members of Congress [49]. Among the external review papers was now a 2021 ‘State of the Art Review,’ in the highly regarded Journal of the American College of Cardiology[15], whose authors included 4 members of previous DGACs and which found that there is ‘no robust evidence that current population-wide arbitrary upper limits on saturated fat consumption in the United States will prevent cardiovascular disease or reduce mortality.’ The paper was named one of the top 100 articles of 2021 by the journal's editor in chief [50], yet this and other reviews were ultimately not considered in the 2020 DGAC review on saturated fats. The DGAC final report makes no mention of any shift in scientific thinking on these fats and concludes that the evidence linking them to heart disease is ‘strong.’
An analysis of the 2020 DGAC subcommittee in charge of the saturated fat review found numerous intellectual, financial, and even religious conflicts of interest that may have contributed to a bias against saturated fats [51,52▪▪]. For instance, one member was found to have chaired five vegetarian conferences from 1997 to 2018, which might reflect a bias against saturated fats, since a more liberal policy towards these fats would inevitably allow for greater consumption of animal foods. This member was also found to have been receiving funds from seven soy and tree nut industry groups, which stand to benefit commercially when guidelines favor the type of fats (polyunsaturated) commonly found in these foods. Another member had spent the last 50 years of her career working as a lead investigator on some of the government's largest trials attempting to show that fat and saturated fats are bad for health. A third member is part of a vegetarian activist group which has condemned the evolving science on saturated fats [53]. These and other interests continue to influence the scientific debate on saturated fats.
In conclusion, the DGA process has never systematically reviewed either the ‘core trials’ on saturated fats directly or the subsequent external review papers of those trials. The major change in thinking on saturated fats that has occurred among independent teams of scientists globally over the past 12 years has therefore not been reflected in U.S. nutrition policy. As a result, the Dietary Guidelines must be considered outdated on this topic.
CONCLUSION
For decades following the introduction of the diet-heart hypothesis, many scientists were unaware of the lack of evidence for this theory. However the rediscovery of rigorous clinical trials testing this hypothesis and the subsequent publication of multiple review papers on these data have provided a new awareness of the fundamental inadequacy of the evidence to support the idea that saturated fats cause heart disease. The observed resistance against considering this new science by successive DGACs can potentially be seen as reflecting longstanding biases in the field and the influence of vested interests. Until the recent science on saturated fats is incorporated into the U.S. Dietary Guidelines, the policy on this topic cannot be seen as evidence-based.
Acknowledgements
None.
Financial support and sponsorship
None.
Conflicts of interest
The author receives modest royalties on a book on the history of dietary fat recommendations and otherwise declares no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Taubes G. Good calories, bad calories. New York: Alfred A. Knopf; 2007. [Google Scholar]
- 2.Teicholz N. The big fat surprise. New York, NY: Simon & Schuster; 2014. [Google Scholar]
- 3.Keys A, Anderson JT, Fidanza F, et al. Effects of diet on blood lipids in man. Clin Chem 1955; 1:34–52. [PubMed] [Google Scholar]
- 4.Keys A. Studies on serum cholesterol and other characteristics of clinically healthy men in Naples. Arch Intern Med 1954; 93:328. [DOI] [PubMed] [Google Scholar]
- 5.Keys A, Vivanco F, Minon JLR, et al. Studies on the diet, body fatness and serum cholesterol in Madrid, Spain. Metabolism 1954; 3:195–212. [PubMed] [Google Scholar]
- 6.Page IH, Allen EV, Chamberlain FL, et al. Dietary fat and its relation to heart attacks and strokes. Circulation 1961; 23:133–136. [Google Scholar]
- 7.Marvin HM. 1924–1964: the 40 year war on heart disease. New York: American Heart Association; 1964. [Google Scholar]
- 8. Bentley J. U.S. trends in food availability and a dietary assessment of loss-adjusted food availability, 1970–2014. Usda.gov. 2017. Available at: https://www.ers.usda.gov/webdocs/publications/82220/eib-166.pdf?v=42762 [cited 2022 Jul 21]. [Google Scholar]
- 9.Keys A. Coronary heart disease in seven countries. Circulation 1970; 3:1–211. [PubMed] [Google Scholar]
- 10.Blackburn H, Jacobs D, Jr, Kromhout D, Menotti A. Review of Big Fat Surprise should have questioned author's claims. Lancet 2018; 392:1014. [DOI] [PubMed] [Google Scholar]
- 11.Teicholz N. Response to critique of review of The Big Fat Surprise. Lancet 2019; 393:2124. [DOI] [PubMed] [Google Scholar]
- 12.Leland GA. Crete: a case study of an underdeveloped area. 1953; Princeton, NJ: Princeton University Press, p. 103. [Google Scholar]
- 13.Sarri K, Kafatos A. The seven countries study in Crete: Olive oil, Mediterranean diet or fasting? Public Health Nutr 2005; 8:666. [DOI] [PubMed] [Google Scholar]
- 14.Menotti A, Kromhout D, Blackburn H, et al. Food intake patterns and 25-year mortality from coronary heart disease: cross-cultural correlations in the Seven Countries Study. Eur J Epidemiol 1999; 15:507–515. [DOI] [PubMed] [Google Scholar]
- 15.Astrup A, Magkos F, Bier DM, et al. Saturated fats and health: a reassessment and proposal for food-based recommendations. J Am Coll Cardiol 2020; 76:844–857. [DOI] [PubMed] [Google Scholar]
- 16.Hamley S. The effect of replacing saturated fat with mostly n-6 polyunsaturated fat on coronary heart disease: a meta-analysis of randomised controlled trials. Nutr J 2017; 16:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frantz ID, Jr, Dawson EA, Ashman PL, et al. Test of effect of lipid lowering by diet on cardiovascular risk. The Minnesota Coronary Survey. Arteriosclerosis 1989; 9:129–135. [DOI] [PubMed] [Google Scholar]
- 18.Ramsden CE, Zamora D, Majchrzak-Hong S, et al. Re-evaluation of the traditional diet-heart hypothesis: analysis of recovered data from Minnesota Coronary Experiment (1968–73). BMJ 2016; 353:i1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mann GV, Pearson G, Gordon T, Dawber TR. Diet and cardiovascular disease in the Framingham study. I. Measurement of dietary intake. Am J Clin Nutr 1962; 11:200–225. [DOI] [PubMed] [Google Scholar]
- 20. Kannel WB, Gordon T. The Framingham Study: an epidemiological investigation of cardiovascular disease. Unpublished paper. Washington, DC: National Heart, Lung, and Blood Institute: 1987; 24. Available at: https://www.scribd.com/document/583903774/Kannel-W-Gordon-T-Framingham-dietary-data-Section-24-unpublished. [Google Scholar]
- 21.Castelli WP. Concerning the possibility of a nut. Arch Intern Med 1992; 152:1371–1372. [PubMed] [Google Scholar]
- 22.Pinckney ER, Pinckney C. The cholesterol controversy. Los Angeles: Sherbourne Press; 1973. [Google Scholar]
- 23.Mann GV. Discarding the diet-heart hypothesis. Nature 1978; 271:500. [Google Scholar]
- 24.Ahrens EH, Jr. Introduction. Am J Clin Nutr 1979; 32:2627–2631. [DOI] [PubMed] [Google Scholar]
- 25.Reiser R. Saturated fat in the diet and serum cholesterol concentration: a critical examination of the literature. Am J Clin Nutr 1973; 26:524–555. [DOI] [PubMed] [Google Scholar]
- 26.Taubes G. Nutrition. The soft science of dietary fat. Science 2001; 291:2536–2545. [DOI] [PubMed] [Google Scholar]
- 27. Taubes G. What if it's all been a big fat lie? The New York Times. 2002 Jul 7; Available at: https://www.nytimes.com/2002/07/07/magazine/what-if-it-s-all-been-a-big-fat-lie.html. [Google Scholar]
- 28.Siri-Tarino PW, Sun Q, Hu FB, Krauss RM. Saturated fat, carbohydrate, and cardiovascular disease. Am J Clin Nutr 2010; 91:502–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Siri-Tarino PW, Sun Q, Hu FB, Krauss RM. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am J Clin Nutr 2010; 91:535–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stamler J. Diet-heart: a problematic revisit. Am J Clin Nutr 2010; 91:497–499. [DOI] [PubMed] [Google Scholar]
- 31.Mozaffarian D, Micha R, Wallace S. Effects on coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med 2010; 7:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sacks FM, Lichtenstein AH, Wu JHY, et al. Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation 2017; 136:e1–e23. [DOI] [PubMed] [Google Scholar]
- 33▪▪.Astrup A, Teicholz N, Magkos F, et al. Dietary saturated fats and health: are the U.S. guidelines evidence-based? Nutrients 2021; 13:3305. [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper contains an original, detailed analysis of the saturated fats review by the 2020 Dietary Guidelines Advisory Committee and concludes that 88% of the studies reviewed did not support the committee's conclusion.
- 34.Dehghan M, Mente A, Zhang X, et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet 2017; 390:2050–2062. [DOI] [PubMed] [Google Scholar]
- 35.Kang Z-Q, Yang Y, Xiao B. Dietary saturated fat intake and risk of stroke: systematic review and dose-response meta-analysis of prospective cohort studies. Nutr Metab Cardiovasc Dis 2020; 30:179–189. [DOI] [PubMed] [Google Scholar]
- 36.Marklund M, Wu JHY, Imamura F, et al. Biomarkers of dietary omega-6 fatty acids and incident cardiovascular disease and mortality: An individual-level pooled analysis of 30 cohort studies. Circulation 2019; 139:2422–2436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Select Committee on Nutrition and Human Needs; U.S. Senate. Ninety-Fifth Congress Session 1, Dietary Goals for the United States; U.S. Government Printing Office: Washington, DC, USA, 1977. Available at: https://catalog.hathitrust.org/Record/011389409. [Google Scholar]
- 38.Oppenheimer GM, Benrubi ID. McGovern's Senate Select Committee on Nutrition and Human Needs versus the meat industry on the diet-heart question (1976–1977). Am J Public Health 2014; 104:59–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary guidelines for Americans. U.S. Department of Health and Human Services: Washington, DC, USA, 1980–2020. Available at: https://www.dietaryguidelines.gov/about-dietary-guidelines/previous-editions. [Google Scholar]
- 40. U.S. Congress. National Nutrition Monitoring and Related Research Act of 1990. U.S. Congress. Washington, DC, USA; 1990. [Google Scholar]
- 41.Teicholz N. The scientific report guiding the US dietary guidelines: is it scientific? BMJ 2015; 351:h4962. [DOI] [PubMed] [Google Scholar]
- 42.Chowdhury R, Warnakula S, Kunutsor S, et al. Association of dietary, circulating, and supplement fatty acids with coronary risk: a systematic review and meta-analysis. Ann Intern Med 2014; 160:398. [DOI] [PubMed] [Google Scholar]
- 43. Teicholz N. The questionable link between saturated fat and heart disease. Wall Street Journal. 2014 May 2. Available at: https://www.wsj.com/articles/the-questionable-link-between-saturated-fat-and-heart-disease-1399070926 [cited 2022 Jul 26]. [Google Scholar]
- 44. Records obtained via a Freedom of Information Act request. Available at: https://www.scribd.com/document/311738813/Part-1-of-2-response-to-my-11-18-15-FOIA-request-re-2015-US-DGAC-members-Barbara-Millen-Alice-Lichtenstein-Frank-Hu, 30–38. [Accessed July 25, 2022]. [Google Scholar]
- 45. Records obtained via a Freedom of Information Act request. Available at: https://www.scribd.com/document/312807180/Part-2-of-2-response-to-my-11-18-15-FOIA-request-re-2015-US-DGAC-members-Barbara-Millen-Alice-Lichtenstein-Frank-Hu, 363–364. [Google Scholar]
- 46. Dietary Guidelines Advisory Committee; U.S. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 2015. Washington, DC, USA: Department of Agriculture, Agricultural Research Service; 2015. [Google Scholar]
- 47.Farvid MS, Ding M, Pan A, et al. Dietary linoleic acid and risk of coronary heart disease: a systematic review and meta-analysis of prospective cohort studies. Circulation 2014; 130:1568–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Dietary Guidelines Advisory Committee; U.S. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 2020. Washington, DC, USA: Department of Agriculture, Agricultural Research Service; 2020. [Google Scholar]
- 49.Demasi M. US nutritionists call for dietary guideline limits on saturated fat intake to be lifted. BMJ 2020; 371:m4226. [DOI] [PubMed] [Google Scholar]
- 50.Fuster V. Editor-in-chief's top picks from 2021. J Am Coll Cardiol 2022; 79:695–753. [DOI] [PubMed] [Google Scholar]
- 51. Nutrition Coalition. Unbalanced, One-sided Subcommittee on Saturated Fats. April 7, 2020. Available at: https://www.nutritioncoalition.us/news/unbalanced-subcommittee-on-saturated-fat [Accessed July 14, 2022]. [Google Scholar]
- 52▪▪.Mialon M, Serodio P, Crosbie E, et al. Conflicts of interest for members of the U.S. 2020 Dietary Guidelines Advisory Committee. Public Health Nutr 2022. 1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is the first-ever systematic analysis of financial conflicts of interest on any U.S. Dietary Guidelines Advisory Committee, and it reveals that 95% of the 2020 committee had at least one tie to the food or pharmaceutical industries.
- 53. The truth about saturated fat. True Health Initiative. 2019. Available at: https://www.truehealthinitiative.org/making_the_news/the-truth-about-saturated-fat/ [cited 2022 Jul 28]. [Google Scholar]