Objective:
In the frame of the Uric Acid Right for Heart Health (URRAH) study, a nationwide multicenter study involving adult participants recruited on a regional community basis from all the territory of Italy under the patronage of the Working Group on Uric Acid and Cardiovascular Risk of the Italian Society of Hypertension, we searched for the cut-off values of the ratio between serum uric acid (SUA) and serum creatinine (sCr) able to predict cardiovascular (CV) events.
Methods:
Among 20 724 participants followed-up for 126 ± 64 months, after detecting cut-off by the receiver operating characteristic curves, we calculated by Cox models adjusted for confounders having CV events as dependent variable the hazard ratio (HR) of SUA/sCr > cut-off. We also verified if the role of cut-off varied with increasing SUA/sCr.
Results:
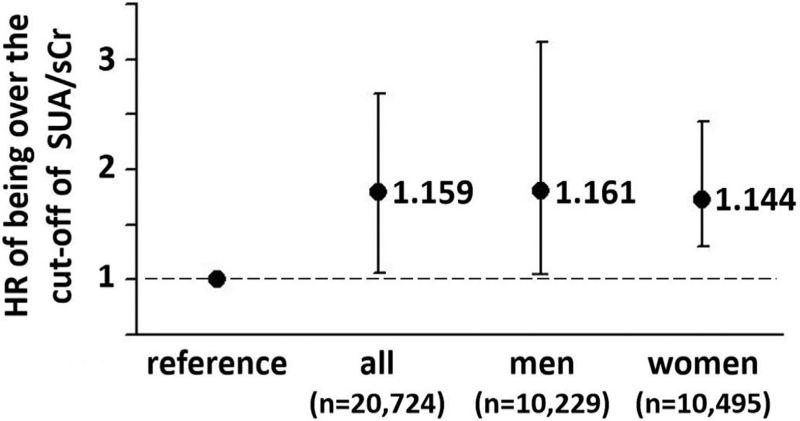
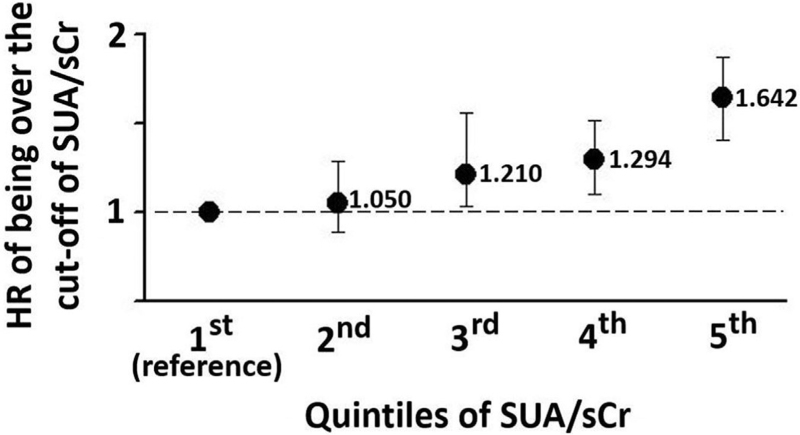
A plausible prognostic cut-off of SUA/sCr was found and was the same in the whole database, in men and in women (>5.35). The HR of SUA/sCr > cut-off was 1.159 (95% confidence interval [CI] 1.092–1.131, P < 0.03) in all, 1.161 (95% CI 1.021–1.335, P < 0.02) in men, and 1.444 (95% CI 1.012–1.113, P < 0.03) in women. In increasing quintiles of SUA/sCr the cut-offs were >3.08, >4.87, >5.35, >6.22 and >7.58, respectively. The HRs significantly increased from the 3rd to the 5th quintile (1.21, 95% CI 1.032–1.467, P = 0.018; 1.294, 95% CI 1.101–1.521, P = 0.002; and 1.642, 95% CI 1.405–1.919, P < 0.0001; respectively), that is, over 5.35, whereas the 2nd quintile was not significantly different from the 1st (reference).
Conclusion:
Having SUA/sCr >5.35 is an independent CV risk indicator both in men and women. The cut-off is dynamic and significantly increases with increasing SUA/sCr.
Keywords: cardiovascular, creatinine, cut-off, epidemiology, uric acid
INTRODUCTION
Uric acid is the final product of purine metabolism in humans. The association between serum uric acid (SUA) and cardiovascular (CV) disease has been investigated for almost 50 years [1] and the role of SUA as a CV risk factor and a metabolic mediator is growing. In the last years, the Uric Acid Right for Heart Health (URRAH) study [2] found univocal prognostic cut-off values of SUA able to predict incidence of CV events [3], myocardial infarction [4], stroke [5] and heart failure [6] also in type-2 diabetic patients [7] and in the aged [8].
SUA largely depends on renal function, but little is known about the prognostic value of SUA when it is indexed for renal function.
In addition to being generally accepted as another independent CV risk indicator [9], serum creatinine (sCr) is also an index of renal function, and can represent an easily available and inexpensive parameter for indexing SUA to renal function. As a matter of fact, the ratio between SUAmg/dl and sCrmg/dl is strictly associated to metabolic syndrome [10] and has sometimes been proposed as a metabolic mediator [11] and as a new variable able to explore CV risk [12] mainly in some categories of selected people such as patients with diabetes, nephropathy or chronic pulmonary disease [13–16] or in menopausal women [17].
However, curiously, no prognostic cut-off values have ever been determined for this a-dimensional variable.
The URRAH study was conceived and designed by the Working Group on Uric Acid and Cardiovascular Risk under the patronage of the Italian Society of Hypertension in order to ascertain the role of SUA as a risk factor in a nationwide, regional-based protocol involving a great number of Italian people [1,2]. One of the URRAH objectives is to find the cut-off values above which SUA and the variables derived from SUA, for instance the SUA/sCr ratio, entail an increased CV risk, stratifying participants into having or having not an increased probability of developing incident CV events during a long-lasting follow-up.
The present analysis intends to clarify: if the a-dimensional variable represented by the SUAmg/dl/sCrmg/dl ratio is associated with CV risk, if a univariate cut-off level of SUA/sCr exists in men and women and can be confirmed as a risk indicator being accepted in multivariate Cox regression models adjusted for confounders, and if the cut-off values of SUA/sCr, if any, vary across sexes and with varying SUA/sCr value.
METHODS
Database and study protocol
The database called URRAH involves data on individuals aged 18–95 years collected on a regional community basis from all the territory of Italy with a median follow-up period of 133 months (interquartile range from 63 to 153 months) up to 31 July 2017. The study protocol has been previously extensively described [2–4]. In brief, a nationwide Italian database was built by collecting data on individuals from representative cohorts having SUA measurement and complete information about several variables including outcomes. A total of 20 724 participants were taken into account in the present analyses. For all participants, a standardized set of items was recorded, including demographics, anthropometric measures, metabolic parameters, smoking habit, systolic and diastolic arterial blood pressure, renal function, history of cardiovascular, renal and brain disease, concomitant treatments and outcomes. Hypertension was defined by the presence of at least two blood pressure recordings at least 140 or at least 90 mmHg or treatment with antihypertensive medications. Diabetes mellitus was defined if blood glucose was at least 126 mg/dl at fast or at least 200 mg/dl 2 h after 75 g oral glucose load or if glycated hemoglobin was >6%. Renal function was evaluated through sCr, and in sensitivity analysis through estimation of the glomerular filtration rate calculated according to the Chronic Kidney Disease Epidemiology Collaboration equation [18].
Ethics
The study data were collected routinely or ad hoc in previously authorized studies. Participants underwent no extra tests or interventions, and there was no impact on participants’ care or outcome. The URRAH was performed according to the Declaration of Helsinki for Human Research (41st World Medical Assembly, 1990). The processing of the patients’ personal data collected in this study comply with the European Directive on the Privacy of Data. All data to be collected, stored and processed are anonymized, and all study-related documents are retained in a secure location. No personal information is stored on local personal computers. Approval was sought from the Ethical Committee of the Coordinating Center at the Division of Internal Medicine of the University of Bologna (No. 77/2018/Oss/AOUBo). Informed consent was obtained from all subjects at recruitment.
Outcome
According to the URRAH protocol [3], incident events due to acute myocardial infarction, angina pectoris, heart failure, stroke, transient ischemic attack and hypertensive complications were taken into consideration during the follow-up (see Table 1s, Supplemental Digital Content for ICD10 codes). Events were double-checked with hospital and physicians’ files.
Statistics
General description
The SAS package version 9.4 (SAS Institute, Cary, North Carolina, USA) was used for statistical analysis. A preliminary power analysis based on differences from stratified values of uric acid for α = 0.05 and power (1 − β) = 0.80 was performed. To our knowledge, no study exists about possible cut-off values of SUA/sCr discriminating participants into doomed to and not doomed to develop any CV event. Consequently, we considered 1 as a possible difference able to stratify participants according to the above-mentioned outcome. Power analysis showed that the number of participants in the database (n = 20 724) represented a sample largely sufficient to avoid β error. The Kolmogorov-Smirnov normality test was performed. Continuous variables were expressed as mean ± standard deviation and compared among classes or categories by the analysis of covariance adjusted time to time for proper confounders and followed by the Bonferroni's post hoc test. Categorical variables were compared by means of the Pearson χ2 test. In multivariate analyses, the covariables that were not independent from each other were previously log-transformed. The null hypothesis was rejected for values of P < 0.05.
The variable SUA/sCr was also divided into five increasing quintiles of 4145 participants each, to be used in descriptive comparative statistics by analysis of variance, and in multivariate Cox model as described below.
Estimated glomerular filtration rate (eGFR) was calculated [18] and used in sensitivity analysis as a putative further confounder in multivariate Cox models. The null hypothesis was rejected for values of P < 0.05.
Univariate prognostic cut-off values
The receiver operating characteristic (ROC) curves method was used to search for prognostic cut-off of SUA/sCr for CV events in the whole database and by sex. SUA/sCr was used as basic variable and CV events as dichotomic classification variable. The De Long et al. method [19] was used. Ratio of cases in the positive group (prevalence), sensitivity and specificity were calculated. ROC curves were generated in the whole database, and a prognostic cut-off value was identified as the curve point nearest to the 100% of axis of the ordinates [20]. In practical terms, this was made by identifying the SUA value associated to the highest values of the sum sensitivity + specificity. Youden's index [21] defined for all points of ROC curves was used as a criterion for selecting the optimum cut-off. The area under the curve was also shown for each ROC curves analysis [22].
Validation of the prognostic cut-off value and hazard ratio of being over cut-off
The cut-off values of SUA/sCr identified by mean of the ROC curves were used as independent variables in separate multivariate Cox analyses adjusted for the confounders already identified, having combined CV events as dichotomic dependent variable in the whole database. A cut-off value identified via the ROC curves method was considered as valid if accepted in the model being the null hypothesis rejected, otherwise it was considered a false cut-off. The corresponding hazard ratio with 95% confidence interval were obtained.
The validated cut-off values were used in the whole database, in the two sexes and in the five quintiles (see below) to stratify combined CV events in descriptive analysis and for generating outcome curves according to the Kaplan–Meier nonparametric estimator of limit product. Log-rank tests were used to assess differences between curves.
RESULTS
Descriptive statistics
The general characteristics of the 20 724 participants are shown in Table 1, also showing men and women separately. The characteristics of the five quintiles are shown in Table 2s, Supplemental Digital Content.
TABLE 1.
General characteristics of the study participants also showing sex stratification
| Variables | Whole database (n = 20 724) | Men (n = 10 229) | Women (n = 10 495) | P values between sexes |
| Age (years) | 57.2 ± 14.7 | 56.5 ± 14.2 | 58.0 ± 15.4 | <0.0001 |
| Men (%) | 49.4 | – | – | – |
| SUA (mg/dl) | 5.04 ± 1.39 | 5.26 ± 1.38 | 4.83 ± 1.38 | <0.0001 |
| sCr (mg/dl) | 0.93 ± 0.25 | 0.96 ± 0.22 | 0.90 ± 0.28 | <0.0001 |
| SUA/sCr | 5.56 ± 1.74 | 5.60 ± 1.76 | 5.51 ± 1.71 | <0.0001 |
| Smoking habit (yes %) | 24.1 | 27.8 | 20.6 | <0.0001 |
| Ethanol intake (yes %) | 62.6 | 64.8 | 60.4 | <0.0001 |
| Diabetes (yes %) | 10.6 | 10.6 | 10.5 | 0.80 (NS) |
| Hypertension (yes %) | 66.7 | 66.2 | 67.3 | 0.10 (NS) |
| Heart rate (bpm) | 71.8 ± 12.3 | 70.7 ± 12.5 | 72.9 ± 11.9 | <0.0001 |
| Systolic BP (mmHg) | 143.3 ± 2.8 | 143.0 ± 22.6 | 144.3 ± 24.9 | <0.0001 |
| Diastolic BP (mmHg) | 85.4 ± 12.8 | 85.5 ± 12.5 | 85.3 ± 13.1 | 0.20 (NS) |
| BMI (kg/m2) | 25.9 ± 4.2 | 26.6 ± 3.9 | 26.7 ± 4.6 | 0.03 |
| LDLC (mg/dl) | 135.6 ± 35.8 | 134.8 ± 35.9 | 135.1 ± 35.4 | 0.53 (NS) |
BMI, body mass index; BP, arterial blood pressure; LDL-C, low-density-lipoprotein serum cholesterol; NS: no statistical difference; sCr, serum creatinine; SUA, serum uric acid.
During the 240-months follow-up, 2110 participants (10.2%) experienced a CV event, that is, 1030 men (10.1%) and 1080 women (10.3%, P = 0.6 between sex, NS).
Search for cut-off value of serum uric acid/serum creatinine
ROC curve furnished plausible univariate cut-off values of SUA/sCr for CV events (5.35), which was the same in the whole database, as well as separately in men and in women. The sex-specific ROC curves are shown in Figure 1s, Supplemental Digital Content, and the ROC parameters by sex in Table 3s, Supplemental Digital Content.
Validation of cut-off values and hazard rations of being over serum uric acid/serum creatinine
After stratifying participants in those until the cut-off and those over the cut-off of SUA/sCr, multivariate Cox analyses adjusted for age (years), sex (1 = men, 0 = women), diabetes mellitus (1 = present, 0 = absent), smoking habit (1 = yes, 0 = no), arterial hypertension (1 = present 0 = absent) and alcohol consumption (1 = yes, 0 = no) demonstrate that being over the cut-off lead to higher risk both in men and in women (Fig. 1). The Cox analysis of the confounders is summarized in Table 4s, Supplemental Digital Content. In men or women, the curves of Kaplan-Mayer generated by being over the CU of SUA/sCr were superimposed (Figure 2s, Supplemental Digital Content).
FIGURE 1.
Hazard ratio (HR) of having SUA/sCr > cut-off in the whole database, in men and in women, after adjustment for age (years), sex when proper (1 = men, 0 = women), diabetes mellitus (1 = present, 0 = absent), smoking habit (1 = yes, 0 = no), arterial hypertension (1 = present 0 = absent) and alcohol consumption (1 = yes, 0 = no). Vertical bars represent the 95% CI. CI, confidence interval; sCr, serum creatinine; SUA, serum uric acid.
Adding eGFR as further confounder did not change significantly the model although accepted as a direct predictive indicator in the whole database (hazard ratio [HR] 1.002, 95% confidence interval [CI] 0.001–0.003, P < 0.0001) and in women (HR 01.004, 95% CI 1.003–1.005, P < 0.0001).
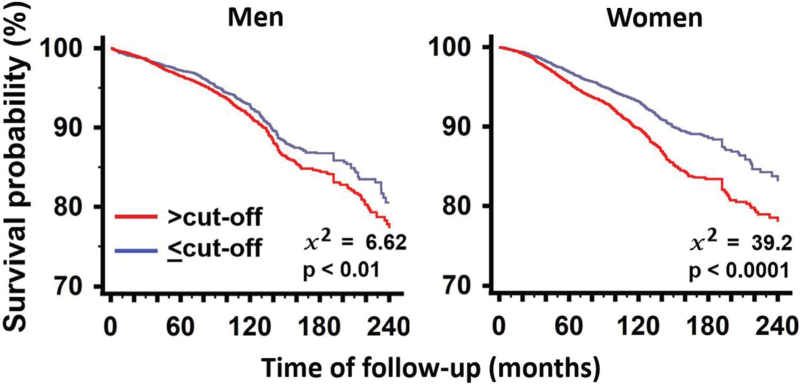
Kaplan–Meier curves after stratification according to cut-off of SUA/sCr are shown in Fig. 2. The curves of participants having SUA ≤ cut-off and SUA > cut-off were clearly separate both in men and women.
FIGURE 2.
Kaplan–Maier curves of survival according to being or being not over the cut-off of SUA/sCr in men and women. NS: nonsignificant difference between sexes. Values of P indicate statistical difference vs. reference. NS: not significant. sCr, serum creatinine; SUA, serum uric acid.
Analysis of the quintiles of serum uric acid/serum creatinine
In the five quintiles of SUA/sCr, the univariate putative prognostic cut-off values of SUA/sCr in relation to CV events were progressively increasing (>3.08 in 1st quintile, >4.87 in the 2nd, >5.35 in the 3rd, >6.22 in the 4th, and >7.58 in the 5th). The results of the ROC curves and analyses are shown in Figure 3s, Supplemental Digital Content and in Table 5s, Supplemental Digital Content, respectively.
When these cut-off values were used in multivariate Cox analyses adjusted for confounders, being over the cut-off positively and increasingly predicted CV events in the 3rd (HR 1.21, 95% CI 1.032–1.467, P = 0.018), 4th (HR 1.294, 95% CI 1.101–1.521, P = 0.002) and 5th quintile (HR 1.642, 95% CI 1.405–1.919, P < 0.0001) using 1st quintile as reference, while the 2nd quintile of SUA/sCr had the same risk than the reference (Fig. 3). The value of SUA/sCr>5.35 corresponding to the 3rd quintile was the threshold over which being over the cut-off had an increasing prognostic role.
FIGURE 3.
HRs of having SUA/sCr>cut-off in the quintiles of SUA/sCr. The 1st quintile is the reference. The 3rd, 4th and 5th quintiles are different from reference. sCr, serum creatinine; SUA, serum uric acid.
When eGFR was added to the analysis as a putative confounder it was rejected from the model.
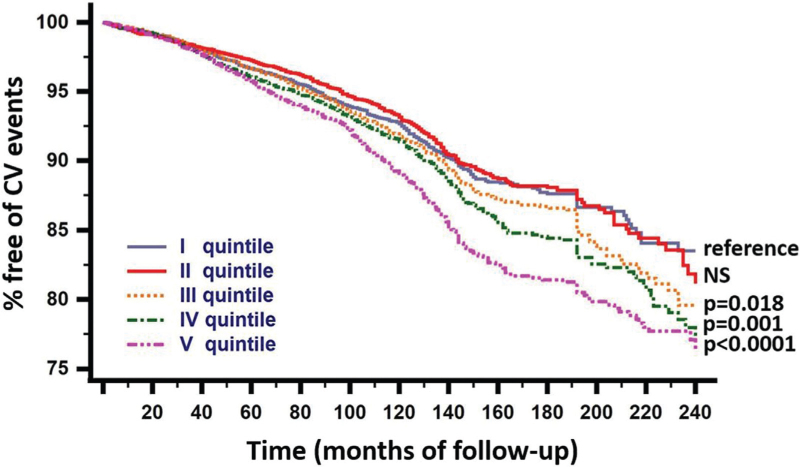
Kaplan–Meier curves in after stratification according to cut-off of SUA/sCr in quintiles of SUA/sCr, in men and in women are shown in Fig. 4. The curves of participants having SUA/sCr ≤ cut-off and SUA/sCr > cut-off were clearly separate.
FIGURE 4.
Kaplan–Maier curves of survival according to being or being not over the cut-off of SUA/sCr for each quintile of SUA/sCr. Values of P represent rejection of the null hypothesis vs. the reference. NS: nonsignificant difference. sCr, serum creatinine; SUA, serum uric acid.
DISCUSSION
First of all, the results of this present analysis confirm that SUA is an independent risk factor for CV events in a long follow-up also after indexing for renal function. This is consistent with a series of studies showing a positive association of incident CV events with SUA as a continuous variable, as well as with being over a well defined prognostic value of SUA [3–8].
This paper particularly takes into consideration the indexing of SUA to renal function represented by sCr. Since both SUA and sCr are expressed in the same unit of measurement (mg/dl), the SUA/sCr derivative variable is a-dimensional, that is purely numerical. SUA/sCr represents not only the result of an indexing but a novel item that can be treated in epidemiological setting as a new variable. We demonstrated SUA/sCr, when used as a continuous item, was a CV risk indicator both in men and women. This focused on the importance of taking into account renal function when using SUA as a risk factor in epidemiological setting. Neglecting this detail represents a severe bias and can lead to misleading results.
More importantly, up to date no prognostic cut-off values of SUA/sCr were known, that is, it was impossible to know if being over a certain value of SUA/sCr could lead to premature incident CV events. We demonstrated that precise cut-off values of SUA/sCr exist in the whole cohort, and separately in men and women. Participants being over the cut-off show higher prevalence of CV events during the follow-up. Not only this, but different (and increasing) cut-off exist with increasing SUA/sCr.
In the present analysis, the prognostic cut-off value of SUA/sCr able to identify the Participants at risk of developing premature CV events was more than 5.35 in the whole cohort, in men and in women: being over the cut-off, significantly led to HR >1 of developing a CV event in both sexes. This is undoubtedly the first report of a defined prognostic cut-off value of SUA predicting CV risk. Although it has been suggested that SUA is a better predictor of CV events than the SUA/sCr ratio [15], our protocol does not allow to clarify if there is any therapeutic implication to apply SUA/sCr rather than SUA for detection of CV risk in clinical setting.
On the contrary, this simply means that indexing for renal function is the right and necessary way to proceed when considering SUA a risk indicator, and that not indexing it to sCr, that is, not considering renal function, leads to falsely more optimistic results when using SUA as a CV prognostic marker.
Concerning sex, the literature suggests that a difference exists between men and women as regards SUA [1]. In our data, SUA/sCr >5.35 was the prognostic cut-off in the whole database, in men in women, confirming that, also after indexing for renal function, gender is a nonsignificant source of heterogeneity when SUA is considered as a risk factor.
In the continuation of the analysis, we wanted to see if SUA/sCr ratio was a constant value or if it varied with varying SUA/sCr. As a matter of fact, the cut-off values increased as the ratio increased, being higher in the higher than in the lower quintiles. Not only that, but when the cut-off values were used to divide, in every quintile, the participants destined and those not destined to develop a higher incidence of CV events in Cox models, we observed that the specific cut-off was valid only for the three higher quintiles, i.e. for values of SUA/sCr >5.35 (third quintile), while in the second quintile the risk was that of the first used as reference. In other words, being over the cut-off represents an increasing CV risk if the SUA/sCr ratio is over 5.35.
It is noteworthy that, when eGFR as a further marker of renal function was added to the Cox models having SUA/sCr as predictive variable, the results did not change significantly. This demonstrates that sCr is a sufficient and adequate indicator of the function of the kidneys. This is good, because sCr is easier to use in clinical practice and, unlike eGFR, it is directly measured variable, not calculated using other parameters according to empirical algorithms.
The main strength of the study described here is to have determined for the first time on a large population sample a prognostic cut-off of the SUA/sCr variable capable of predicting the incidence of cardiovascular events, and to have shown that it is dynamic and increases when SUA/sCr increases. A weakness of the study is that it did not take into account the eco-genetic context [23], which will have to be considered in subsequent studies, and that the URRAH is not strictly a population-based study, but rather a cohort study of data collected on a regional basis in the entire Italian territory. On the other hand, the collected database represents the largest number of Italian cases ever collected, and to our knowledge there is no one more representative of the Italian situation. Furthermore, the present analysis was limited to Italian people and its results cannot be directly applied to other ethnicities. In Chinese [24,25] and Japanese people [26], a simple association between the continuous variable SUA/sCr ratio and other CV risk factors was found, and Mazidi et al.[12], in a paper then withdrawn, described in the United States an association between the ratio as a continuous variable and mortality. On the other hand, to our knowledge, no paper defined cut-off values of the SUA/sCr ratio able to identify individuals at higher cardiovascular risk. A strength of our study is to have defined clear prognostic cut-off identified by the ROC curves methods and validated in multivariate models, able to stratify participants at higher CV risk.
In conclusion, the SUA/sCr ratio is more complete than SUA alone in predicting CV risk, as it includes the weight of renal function which is intimately linked to SUA. A clear and defined cut-off exists for SUA/sCr (>5.35), and in the frame of a nationwide study is able to stratify individuals destined to experience incident CV events during a long-lasting follow-up from those destined to be events-free. This cut-off, good for the whole cohort, is a dynamic value which tends to increase with increasing SUA/sCr when over 5.35. The SUA/sCr ratio is therefore qualifying itself as a low-cost reliable marker of CV risk and should be used systematically in epidemiological setting as well as in clinical practice to screen individuals at higher risk.
ACKNOWLEDGEMENTS
Sources of Funding: none.
Conflicts of interest
There are no conflicts of interest.
Supplementary Material
Edoardo Casiglia and Valérie Tikhonoff contributed equally to this work.
Abbreviations: CI, confidence interval(s); CV, cardiovascular; HR, hazard ratio(s); ICD-10, International Classification of Diseases – 10th Revision; OR, odds ratio(s); ROC, receiver operating characteristic; sCr, serum creatinine; SUA, serum uric acid; URRAH, Uric Acid Right for Heart Health
Supplemental digital content is available for this article.
REFERENCES
- 1.Culleton BF, Larson MG, Kannel WB, Levy D. Serum uric acid and risk for cardiovascular disease and death: the Framingham Heart Study. Ann Intern Med 1999; 131:7–13. [DOI] [PubMed] [Google Scholar]
- 2.Desideri G, Virdis A, Casiglia E, Borghi C. Exploration into uric and cardiovascular disease: Uric Acid Right for Heart Health (URRAH) project. A study protocol for a retrospective observational study. High Blood Press Cardiovasc Prev 2018; 25:197–202. [DOI] [PubMed] [Google Scholar]
- 3.Virdis A, Masi S, Casiglia E, Tikhonoff V, Cicero AFG, Ungar A, et al. Identification of the uric acid thresholds predicting an increased total and cardiovascular mortality over 20 years. Hypertension 2020; 75:302–308. [DOI] [PubMed] [Google Scholar]
- 4.Casiglia E, Tikhonoff V, Virdis A, Masi S, Barbagallo CM, Bombelli M, et al. Serum uric acid and fatal myocardial infarction: detection of prognostic cut-off values: the URRAH (Uric Acid Right for Heart Health) study. J Hypertens 2020; 38:412–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tikhonoff V, Casiglia E, Spinella P, Barbagallo CM, Bombelli M, Cicero AFG, et al. Identification of a plausible serum uric acid cut-off value as prognostic marker of stroke: the Uric Acid Right for Heart Health (URRAH) study. J Hum Hypertens 2021; doi: 10.1038/s41371-021-00613-5. [DOI] [PubMed] [Google Scholar]
- 6.Muiesan ML, Salvetti M, Virdis A, Masi S, Casiglia E, Tikhonoff V, et al. Serum uric acid predicts heart failure in a large Italian cohort: search for a cut-off value the Uric Acid Right for Heart Health study. J Hypertens 2021; 39:62–69. [DOI] [PubMed] [Google Scholar]
- 7.Masulli M, D’Elia L, Angeli F, Barbagallo CM, Bilancio G, Bombelli M, et al. Serum uric acid levels threshold for mortality in diabetic individuals: the Uric Acid Right for Heart Health (URRAH) project. Nutr Metab Cardiovasc Dis 2022; 32:1245–1252. [DOI] [PubMed] [Google Scholar]
- 8.Ungar A, Rivasi G, Di Bari M, Virdis A, Casiglia E, Masi S, et al. The association of uric acid with mortality modifies at old age: data from the Uric Acid Right for Heart Health (URRAH) study. J Hypertens 2022; 40:704–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Praught ML, Shlipak MG. Are small changes in serum creatinine an important risk factor? Curr Opin Nephrol Hypertens 2005; 14:265–270. [DOI] [PubMed] [Google Scholar]
- 10.Tikhonoff V, Casiglia E. Metabolic syndrome: nothing more than a constellation? Eur Heart J 2007; 28:780–781. [DOI] [PubMed] [Google Scholar]
- 11.Wang A, Tian X, Wu S, Zuo Y, Chen S, Mo D, et al. Metabolic factors mediate the association between serum uric acid to serum creatinine ratio and cardiovascular disease. J Am Heart Assoc 2021; 10:e023054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mazidi M, Katsiki N, Banach M. A higher ratio of serum uric acid to serum creatinine could predict the risk of total and cause specific mortality – insight from a US national survey. Int J Cardiol 2021; 326:189–193. this paper was then retired. [DOI] [PubMed] [Google Scholar]
- 13.Al-Daghri NM, Al-Attas OS, Wani K, Sabico S, Alokail MS. serum uric acid to creatinine ratio and risk of metabolic syndrome in Saudi type 2 diabetic patients. Scientific Rep 2017; 7:12104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ding Z, Fan Y, Yao C, Gu L. The association between the serum uric acid to creatinine ratio and all-cause mortality in elderly hemodialysis patients. BMC Nephrol 2022; 23:177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ephraim RKD, Awuku YA, Numekevor P, Felix Botchway R, Adoba P, et al. Serum Uric acid is a better indicator of kidney impairment than serum uric acid to creatine ratio; a cross sectional study of type 2 diabetes mellitus patients. J Diab Metab Dis 2021; 20:313–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kocak ND, Sasak G, Akturk UA, Akgun M, Boga S, Sengul A, et al. Serum uric acid levels and uric acid/creatinine ratios in stable chronic obstructive pulmonary disease (COPD) patients: are these parameters efficient predictors of patients at risk for exacerbation and/or severity of disease? Med Sci Monit 2016; 22:4169–4176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tao J, Shen X, Li J, Cha E, Gu PP, Liu J, et al. Serum uric acid to creatinine ratio and metabolic syndrome in postmenopausal Chinese women. Medicine 2020; 99: 17 (e19959). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levey AS, Inker LA, Coresh J. GFR estimation: from physiology to public health. Am J Kidney Dis 2014; 63:820–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988; 44:837–845. [PubMed] [Google Scholar]
- 20.Kamarudin AN, Cox T, Kolamunnage-Dona R. Time-dependent ROC curve analysis in medical research: current methods and applications. BMC Med Res Methodol 2017; 17:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Youden WJ. Index for rating diagnostic tests. Cancer 1950; 3:32–35. [DOI] [PubMed] [Google Scholar]
- 22.Schisterman EF, Perkins NJ, Liu A, Bondell H. Optimal cut-point and its corresponding Youden index to discriminate individuals using pooled blood samples. Epidemiology 2005; 16:73–81. [DOI] [PubMed] [Google Scholar]
- 23.Stolarz K, Staessen JA, Kawecka-Jaszcz K, Brand E, Bianchi G, Kuznetsova T, et al. Genetic variation in CYP11B2 and AT1R influences heart rate variability conditional on sodium excretion. Hypertension 2004; 44:156–162. [DOI] [PubMed] [Google Scholar]
- 24.Li R, Luo SY, Zuo ZG, Yu Z, Chen WN, Ye YX, Xia M. Association between serum uric acid to creatinine ratio and metabolic syndrome based on community residents in Chashan town, Dongguan city. Zhonghua Yu Fang Yi Xue Za Zhi 2021; 55:1449–1455. [DOI] [PubMed] [Google Scholar]
- 25.Liu S, Song J, Peng J, Tang Z, Zhang J, Zhang L. Association of serum uric acid /creatinine ratio and metabolic syndrome in euthyroid population. Wei Sheng Yan Jiu 2020; 49:374–380. [PubMed] [Google Scholar]
- 26.Kawamoto R, Ninomiya D, Akase T, Kikuchi A, Kasai Y, Kusunoki T, et al. Serum uric acid to creatinine ratio independently predicts incident metabolic syndrome among community-dwelling persons. Metab Syndr Relat Disord 2019; 17:81–89. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.