Abstract
Coronary artery disease represents a leading cause of death worldwide, to which the coronary artery bypass graft (CABG) is the main method of treatment in advanced multiple vessel disease. The use of the internal mammary artery (IMA) as a graft insures an improved long-term survival, but impairment of chest wall perfusion often leads to surgical site infection and increased morbidity and mortality. Infrared thermography (IRT) has established itself in the past decades as a non-invasive diagnostic technique. The applications vary from veterinary to human medicine and from head to toe. In this study we used IRT in 42 patients receiving CABG to determine the changes in skin surface temperature preoperatively, two hours, 24 h and 6 days after surgery. The results showed a significant and independent drop of surface temperature 2 h after surgery on the whole surface of the chest wall, as well as a further reduction on the left side after harvesting the IMA. The temperature returned to normal after 24 h and remained so after 6 days. The study has shown that IRT is sufficiently sensitive to demonstrate the known, subtle reduction in chest wall perfusion associated with IMA harvesting.
Keywords: Infrared thermography, Tissue perfusion, Coronary artery bypass, Internal mammary artery, Chest wall perfusion
Introduction
Coronary artery disease (CHD) represents a leading cause of death worldwide, to which the coronary artery bypass graft (CABG) is the main method of treatment in advanced multiple vessel disease. The procedure implies the completion of a median sternotomy and bypassing the diseased coronary artery segments with autologous vessels. The use of the internal mammary artery (IMA) as a graft insures an improved long-term survival.12 Nevertheless, the combination of median sternotomy with the harvest of the sternal blood supply, the internal mammary arteries, leads to a decrease in the regional blood perfusion, which predisposes to postoperative wound healing disorders and deep sternal wound infections (DSWI).1 To minimize the occurence of these complications, the harvest of only the left internal mammary artery (LIMA) is currently favored in most heart surgery centers,15 while harvesting both internal mammary arteries (BIMA) is used only in chosen cases.4An alternative is the harvesting of a skeletonized IMA, leaving the collateral circulation around the artery intact and therefore preserving some of the sternal perfusion.6
Patient comorbidities like obesity, diabetes mellitus, heart failure or a history of smoking may favor the hypoperfusion of the anterior chest area postoperatively.19 Therefore, the perioperative diagnosis of perfusion impairment around the chest wall is of great importance, especially in patients at risk for developing wound complications. Nevertheless, standard measures to estimate chest wall perfusion have not been yet defined.
The measurement of thermal radiation has been proven so far to have useful applications in different domains like monitoring the heart rate and respiratory rates in experimental pigs,2 brain mapping,7,10,16 tumor detection,22 identifying the perforator vessels for flap surgery26,9 as well as for determining the skin perfusion postoperatively after flap harvest.20 Infrared thermography (IRT) implies a non-invasive, accessible and label-free technique. In patients undergoing CABG surgery, high resolution thermography of the chest wall may be valuable for identifying changes in perfusion, especially in patients at risk.
In our study we aimed at estimating changes in tissue perfusion by means of IRT after the harvest of the LIMA for bypass surgery. Patient-related risk factors, surgical technique, vital parameters and cutaneous blood volume pulse (CBVP) were investigated for additional effects on IRT.
Materials and Methods
Study Setting
Patients who underwent CABG were studied at our university center for cardiac surgery, after written informed consent was obtained. The study was conducted in accordance with the principles of the Declaration of Helsinki, fifth revision, and was approved by the Institutional Review Board of our institution (IRB00001473, EK168052013). This was a combined study to evaluate both high resolution thermographic imaging as well as contact-free photoplethysmographic imaging (PPGI)11 for monitoring purposes in major/cardiac surgery.
Thermography Setup
The chest wall surface temperature Ts was measured by the high resolution IRT system VarioCAM® (InfraTec GmbH, Dresden, Germany). VarioCAM® uses an uncooled microbolometric plane array with a resolution of 480 × 640 pixels. Its thermal resolution is 30 mK at 30 °C in a spectral range from 7.5 to 14 μm. Its spatial resolution reaches 0.25 mm with an object distance of 300 mm. Images are recorded with 30 frames per second.
Measurements and Image Processing
Measurements were performed the day before surgery (BL) as well as two hours (H2), 24 h (H24) and 6 days (D6) after surgery. Measurements were taken in supine position. Patients were in stable circulatory condition and weaned from mechanical ventilation during the measurements after surgery.
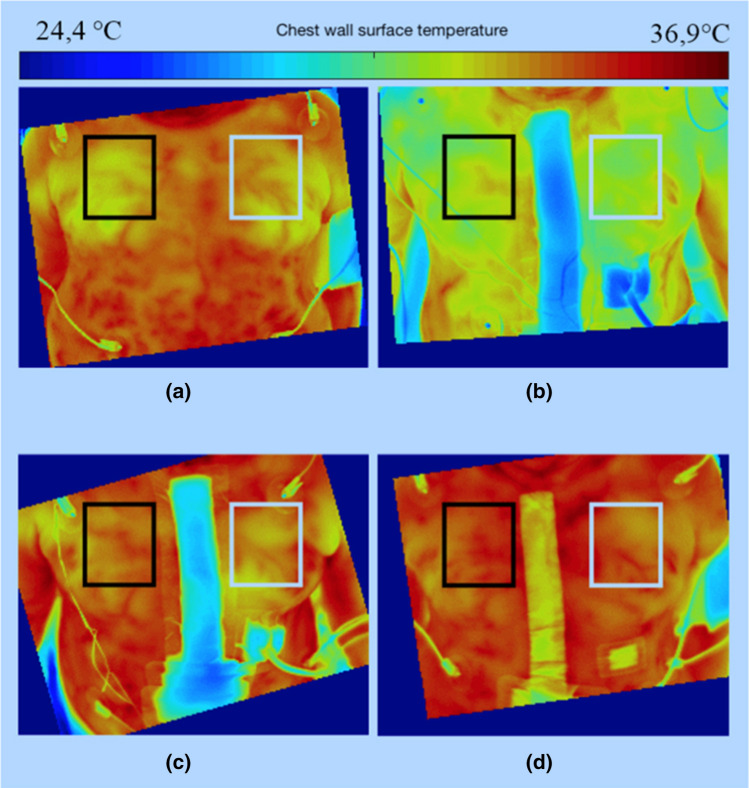
Before each measurement, an internal camera one-point non-uniformity correction (NUC) was performed for each microbolometer of the uncooled focal plane array to avoid a recalibration during data collection. A sequence of thermographic images of one minute duration was taken at each measurement. Data were processed offline after all measurements were completed. Consistent rectangular regions of interest (ROI) were defined for each side of the chest in the four videos, leaving out wound dressings and drains (Fig. 1). The temperatures within the ROI were averaged over time and space, leading to the two temperature values TS,L and TS,R for the left and right side of the anterior chest wall for each measurement. Blood pressure and heart rate, body (core) temperature and room temperature were taken for reference at each measurement. Surrogates of cutaneus perfusion were derived from the CBVP, which was estimated in non-contact photoplethysmograms of the accompanying study at the same time points.11
Figure 1.
Thermal images of the chest wall with left (white) and right (black) ROI. (a) before surgery, (b) 2 h after surgery, (c) 24 h after surgery, (d) 6 days after surgery. All temperature values were averaged over 18,000 frames, corresponding to a duration of 60 s.
Statistical Analysis
Effects of surgery and surgical techniques, vital parameters, and cofactors on Ts were investigated in random-intercept covariance models. Random effects were defined by patients. Fixed effects were defined by measurement time, chest wall side, vital signs, surgical factors and comorbidity. Maximal models containing covariates of any interest were constructed, pared down on the basis of stepwise deletion and compared by Likelihood ratio (LR) tests. Core temperature and room temperature variables were scaled to their grand mean. Heart rate was scaled to deviations of 10bpm from 80 bpm. Measurement time was defined as an ordinal variable in relation to surgery. Significance of fixed effects was t-tested after Satterthwaite´s approximation to degrees of freedom.13 The explanatory power of room and core temperature on Ts was taken as the reduction of the residual variance of Ts from the minimal adequate model through stepwise deletion of both predictors.
Results
Fortytwo patients undergoing CABG surgery were investigated. Patient characteristics and graft preparation are given in Table 1.
Table 1.
Demographic and baseline data.
| Patients (m:w) | 39:3 |
| Age (years) | 71.1 ± 7.5 |
| Weight (kg) | 87.3 ± 13.9 |
| Height (cm) | 174 ± 7.2 |
| Arterial hypertension (n) | 37 |
| Graft preparation (ped:scel) | 27:15 |
| NYHA (n) | |
| 1 | 2 |
| 2 | 18 |
| 3 | 22 |
| LVEF | |
| Normal | 26 |
| Borderline | 4 |
| Impaired | 8 |
| Severely impaired | 4 |
| Diabetes (n) | 18 |
| Hyperlipidemia (n) | 39 |
| Angina pectoris (n) | 18 |
| CCS 1 | 5 |
| CCS 2 | 6 |
| CCS 3 | 4 |
| CCS 4 | 3 |
Ped pedicled mammaria graft, scel skeletonized mammaria graft, NYHA New York heart Association functional class, LVEF preoperative left ventricular ejection fraction, CCS Canadian Cardiovascular Society grading of angina pectoris
Impact of Room and Core Temperature
TS varied between 28.8 and 35.8 °C and was on average 3.2 °C lower than core temperature (p < 0.001, U Test). TS significantly increased with room temperature or core temperature in univariable and multivariable analyses. A varying impact of both parameters on Ts during the study was not evident after adjustment for cofactors. Independently from surgery and physiological parameters, room temperature explained 8.3% of the variance of Ts, whereas body temperature explained 1.2% (p = 0.04) and both together explained 11.5% (p < 0.001).
Surgery, Vital Parameters and Comorbidity
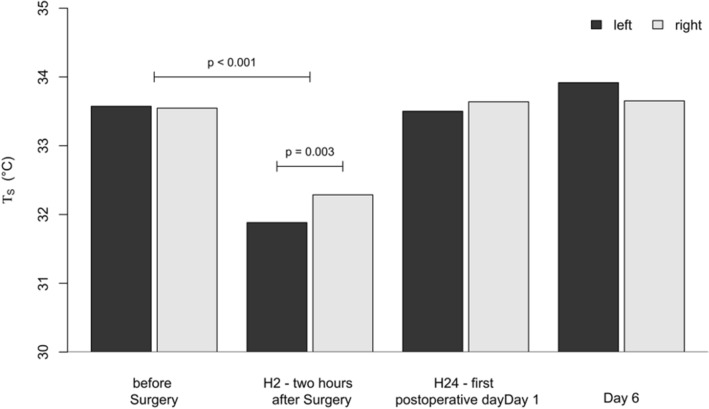
TS significantly decreased immediately after surgery (H2) by 1.7 K (from − 2.0 to − 1.4 K, p < 0.001) at the left side and by 1.3 K from (− 1.6 K to − 0.9 K, p < 0.001) at the right side. It recovered the day after surgery (H24) and slightly exceeded the preoperative level on day 6. A difference in TS of 404 mK (p = 0.015) between the left and right side was seen at H2, but neither before surgery nor at H24 or D6 (Fig. 2, Table 2). Core temperature also decreased after surgery (− 0.77 °C, p < 0.001). The measurement point per se remained significant after multivariable adjustment of related cofactors including core and room temperature.
Figure 2.
Surface Temperature TS of the left and right side of the anterior chest wall during the study.
Table 2.
TS of both sides of the chest during the study.
| left (°C) | SD | right (°C) | SD | |||
|---|---|---|---|---|---|---|
| Baseline | 33.6 | 0.9 | 33.5 | 0.8 | – | 0.869 |
| H2 | 31.9 | 1.1 | 32.3 | 1.0 | < 0.001 | 0.015 |
| H24 | 33.5 | 1.1 | 33.6 | 1.1 | 0.675 | 0.422 |
| Day6 | 33.9 | 0.9 | 33.7 | 0.9 | 0.045 | 0.119 |
SD standard deviation. p1 changes over time, p2 left side vs. right side of the chest wall
Table 3 shows the multivariable estimation of concurrent effects of vital parameters, surgery and comobidity on TS. A significant impact of surgery on global TS remains evident until the first postoperative day (H24). Heart rate affected TS at BL, H24 and D6, but not at H2. At heart rates higher than 80 bpm, TS increased by 0.3 °C (BL), 0.4 °C (H24) and 0.3 °C (D6) per 10 bpm increase of heart rate. A higher respiratory rate was associated with a slight decrease of TS. Sensitivity of TS to blood pressure was only seen in the subgroup of patients with documented angina pectoris before surgery. Among those, patients with angina of Canadian Cardiovascular Society (CCS) class 4 had a significant delay in postoperative recovery of TS, compared to lower classes (Table 4). Preoperative systolic cardiac function (ejection fraction) and heart failure according to the New York Heart Associacion (NYHA) classification had no influence on TS. Likewise, arterial hypertension, diabetes mellitus or lipid disorders did not exert a significant effect on TS. Surgical techniques (pedicled vs. skeletonized grafting) and ancillary measures like the use of stapler and gelaspone or intracutaneous suture were not systematically associated with TS.
Table 3.
Multivariable estimation of the effects of surgery vital parameters and comorbidity on TS.
| CI low | CI high | |||
|---|---|---|---|---|
| Effect of surgery | ||||
| H2 | − 2.2 | − 2.9 | − 1.5 | <0.001 |
| H24 | − 0.7 | − 1.3 | − 0.2 | 0.015 |
| D6 | 0.1 | − 0.3 | 0.6 | 0.612 |
| Side effect | ||||
| BL | 0.0 | − 0.3 | 0.3 | 1 |
| H2 | 0.5 | 0.2 | 0.9 | 0.004 |
| H24 | 0.3 | − 0.1 | 0.6 | 0.208 |
| D6 | − 0.2 | − 0.6 | 0.1 | 0.219 |
| Heart rate (10 × min−1) | ||||
| BL | 0.3 | 0.07 | 0.45 | 0.013 |
| H2 | 0.1 | − 0.2 | 0.42 | 0.515 |
| H24 | 0.4 | 0.07 | 0.67 | 0.023 |
| D6 | 0.2 | 0.01 | 0.43 | 0.049 |
| Respiratory rate (min−1) | − 0.04 | − 0.07 | 0.00 | 0.037 |
| Core temperature (°C) | 0.2 | 0.0 | 0.3 | 0.047 |
| Room temperature (°C) | 0.2 | 0.1 | 0.4 | < 0.001 |
CI 95% confidence interval. Side effect denotes the difference of TS between the right and left side of the chest wall
Table 4.
TS in patients with documented angina pectoris.
| CI low | CI high | |||
|---|---|---|---|---|
| CCS 1–3 | ||||
| H2 | − 1.8 | − 2.3 | − 1.2 | < 0.001 |
| H24 | − 0.2 | − 0.7 | 0.4 | 0.587 |
| D6 | 0,0 | − 0.4 | 0.44 | 0.946 |
| CCS 4 vs. CCS 1–3 | ||||
| H2 | − 1.3 | − 2.1 | − 0.54 | 0.002 |
| H24 | − 1.6 | − 2.44 | − 0.68 | < 0.001 |
| D6 | − 1.8 | − 2.53 | − 0.98 | < 0.001 |
| Heart rate | 0.3 | 0.14 | 0.39 | < 0.001 |
| Systolic blood pressure (10 × mmHg−1) | 0.1 | 0.03 | 0.2 | 0.01 |
For patients with CCS1-3, TS was compared to baseline. For patients with CCS4, Ts deviation from patients with CCS1–3 is shown (CCS 4 vs. CCS 1–3)
Relation Between Chest Wall Temperature and Cutaneous Blood Volume Pulse
TS significantly increased with higher CBVP estimated by non-contact photoplethysmography, albeit the association was moderate (Fig. 3). 25.8% of the variability of TS was explained by changes of CBVP. Taking into account vital signs and measurement time, the independent effect of CBVP consistently remained. It was not dependent on measurement time (p = 0.98 for the interaction).
Figure 3.
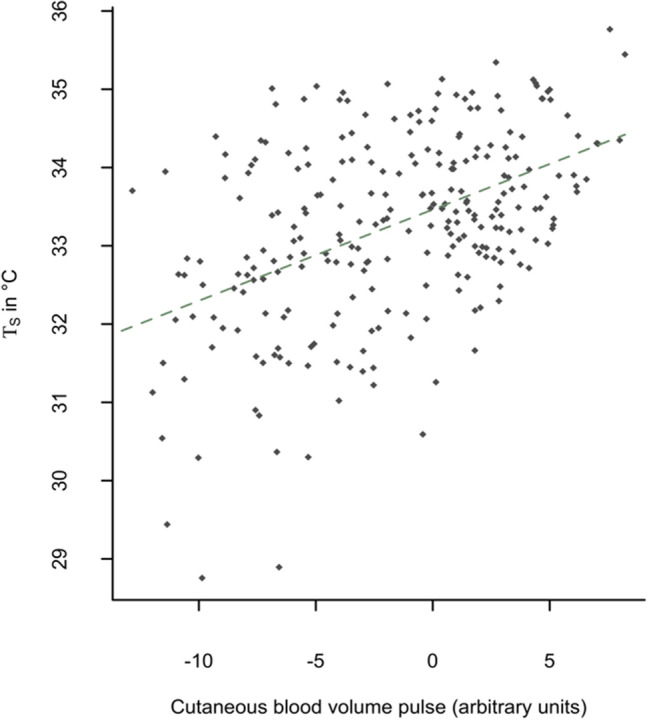
Association between cutaneous blood volume pulse (CVP) and chest wall surface temperature (TS). The dotted line shows the linear fit of TS to CBVP.
Discussion
The present study measured the chest wall surface temperature (TS) using high resolution thermographic imaging in 42 heart surgery patients. Although expectedly TS was correlated to core temperature and room temperature, multivariable analysis confirmed that both temperatures only explained a minor part of TS variance and that an independent residual effect of surgery on its own was present. Two hours after surgery, TS significantly decreased compared to the preoperative measurement. The expected drop in TS on the left compared to the right side, where the main blood supply to the chest wall was removed, was also statistically significant at this point. At the next measurement, 24 h after surgery, the difference between TS and core temperature as well as between the chest wall sides had disappeared. While the surgical trauma and the operating room temperature had probably an effect on the core temperature, the further drop in TS may be attributed on the one hand to the postoperative peripheral vasoconstriction21 and on the other hand to the surgical interruption of the local skin and soft tissue perfusion, which is emphasized on the less perfused left side. Until the next measurement, 24 h after surgery, compensatory mechanisms had gradually reversed these changes, including the difference between sides. Here might come into role the redistribution of circulation with opening of choke vessels, which connect different vascular zones.3,5 The fact that TS was independent of the heart rate only at H2 sustains the idea, that the local perfusion impairment due to surgery was responsible for the TS drop all together and on the left side. After reestablishement of local perfusion, the heart rate could influence again TS.
The physiological parameters had a minimal impact on TS. While the respiratory rate was slightly and inversely associated with TS, blood pressure had an impact on TS only in patients with preoperative angina pectoris. The delayed recovery in Class 4 CCS patients may be attributed to a pronounced general vascular injury and successively reduced flow-mediated dilation in these patients, which could delay the opening of choke vessels and the reorganization of circulation.14 The absent effects of preoperative ejection fraction and NYHA stage on TS are in accordance with the compensated resting hemodynamics of all patients. Although an improvement in ejection fraction is expected within 30 days after CABG8 and therefore an improvement in peripheral tissue perfusion, the measurement interval in our study was possibly too short for these changes to take place. Out of the surgical factors, while the use of stapler, gelaspone or intracutaneous sutures were not expected to have a direct impact on tissue perfusion and TS, the skeletonization of the IMA also didn’t systematically show an impact on TS. While on the long-term this technique has shown to improve the chest wall perfusion,6 the surgical preparation with vessel spasm probably impede the rapid reestablishement of tissue perfusion immediately postoperative. Diabetes mellitus, hypertension and lipid disorders had no influence on TS, showing that these factors do not affect the rapid circulation changes described above.
The systematic link between TS and CBVP proves that the perfusion of superficial skin vessels partly determines TS. Owing to the limited propagation of light into the skin, CBVP is mainly determined by blood volume changes in the outer skin layers. However, there is only a weak relation between both measures (explanatory power 25.8%). These data support the notion that high resolution thermal imaging depends to some extend on peripheral perfusion, as expected, but also on thermal effects of deeper regions of the chest wall, that are more affected by IMA severance and are critical for wound healing.
The results of this study show, that perfusion alterations after cardiac surgery and even local effects of IMA harvesting can be early detected by means of high resolution IRT. The limited explanatory value of core or room temperature for TS emphasizes the specific physiologic significance of IRT monitoring in the context of peripheral perfusion. If the method allows to discriminate between expected and pathological changes in chest wall blood flow, i.e., if it could serve as an early indicator of complications associated to malperfusion, remains to be seen in further studies.
IRT has established itself in the past decades as a non-invasive diagnostic technique. The applications vary from veterinary to human medicine and head to toe.24 Around the chestwall, IRT can be used as an adjunctive to mammography to detect breast cancer. The higher tumoral metabolism rate enables the detection within breast thermal maps.22 Zhang et al.27 showed that the temperature difference between the two anterior chest wall sides can reliably predict the succces of the regional anesthetical block. The blockade of small unmyelinated fibers in this case causes a vasodialation and interferes with the physiological thermoregulation, compared to the control side. This sustains the findings of our study, that local changes in blood perfusion have a thermographic effect.
IRT is furthermore used in the mapping of skin perforators in flap surgery. According to the angiosome principle, a perforator vessel supplies blood flow to a vascular territory and has anastomoses to other neighbouring vascular territories.25 Currently, dynamic IRT is being used preoperatively in identifying the appropriate perforator vessel to be transplanted as well as in flap monitoring after free flap transplantation, where changes in arterial or venous perfusion influence the skin temperature.17,23,28 The sensitivities lie between 89.6 and 99.6% and specificities between 96 and 99.9%.20
After supplying blood to the chest wall, IMA continues to the abdomen wall as the superior epigastric artery, where it anastomosises itself to the inferior epigastric artery to supply the perfusion to the abdominal wall. In breast reconstruction using abdominal flaps, the inferior epigastric artery is elevated together with the fasciocutaneous tissues and the vessel anastomosis is usually performed to the IMA and vein. Nergård et al.18 investigated the abdominal wall perfusion using dynamic IRT in 17 female patients after receiving a breast reconstruction as described before. They recorded a loss of hot spots corresponding to the perforator vessels not only in the undermined median regions, but also in the submammary region on the side where the internal mammary vessels were severed at the level of the third or fourth rib. This sustains the results of the present study, that the harvest of the IMA results in a decline in skin perfusion immediately postoperative. According to Dhar et al.,5 after a 3 h period of vasoconstriction, the chocke vessels connecting different angiosomes start progressively dilating to reach a normal diameter within 24 h and a maximal dilation at 48–72 h. This was confirmed in the study of Nergård et al.,18 where the hot spots reappeared within the first postoperative days, as well as in our study, where the chest wall temperature equalized within 24 h of surgery.
The present study was performed in a rather limited amount of patients and did not investigate the impact of harvesting BIMA on the chest wall pefusion. The investigation resumed to a quantitative measurement of the temperature, without identifying the individual perforators. The planning of future studies could include a dynamic investigation with the identification of hot spots. This could show more accurately the impact of thoracotomy and the harvesting of the IMA, as direct perforators could be either closed or show less flow.
In the present study, we showed that the high resolution thermography is suitable to detect early perfusion changes of the chest wall and even local effects of IMA harvesting after CABG. We also showed, that the harvest of LIMA has an additive impact on the hemithoracic blood supply in the first day after surgery. Further studies should aim at establishing a quantitative threshold, in order to predict the wound healing disorders according to the measurement of local blood supply.
Acknowledgments
No funds, Grants, or other support was received. The authors have no relevant financial or non-financial interests to disclose.
Abbreviations
- BIMA
Bilateral internal mammary artery
- BL
Before surgery
- CABG
Coronary artery bypass graft
- CCS
Canadian Cardiovascular Society grading of angina pectoris
- CHD
Coronary heart disease
- CVP
Cutaneous blood volume pulse
- D6
6 Days after surgery
- DSWI
Deep sternal wound infection
- H2
Two hours after surgery
- H24
24 Hours after surgery
- IMA
Internal mammary artery
- LIMA
Left internal mammary artery
- LR
Likelihood ratio
- LVEF
Ejection fraction
- NUC
Non-uniformity correction
- NYHA
New York heart Association functional class
- ped
Pedicled mammaria graft
- PPGI
Photoplethysmographic imaging
- ROI
Regions of interest
- scel
Skeletonized mammaria graft
- Ts
Chest wall surface temperature
- TS,L
Left chest wall surface temperature
- TS,R
Right chest wall surface temperature
Funding
Open Access funding enabled and organized by Projekt DEAL.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Andreas, M., M. Zeitlinger, M. Hoeferl, W. Jaeger, D. Zimpfer, J.-M. Hiesmayr, G. Laufer, and D. Hutschala. Internal mammary artery harvesting influences antibiotic penetration into presternal tissue. Ann Thorac Surg 95(4):1323–9; Discussion 1329–30, 2013. 10.1016/j.athoracsur.2012.10.088 [DOI] [PubMed]
- 2.Barbosa Pereira, C., H. Dohmeier, J. Kunczik, N. Hochhausen, R. Tolba, and M. Czaplik. Contactless monitoring of heart and respiratory rate in anesthetized pigs using infrared thermography. PLoS ONE 14(11):e0224747, 2019. 10.1371/journal.pone.0224747 [DOI] [PMC free article] [PubMed]
- 3.Bota O, Josten C, Borger MA, Spindler N, Langer S. Standardized musculocutaneous flap for the coverage of deep sternal wounds after cardiac surgery. Ann. Thorac. Surg. 2019;107(3):802–808. doi: 10.1016/j.athoracsur.2018.09.017. [DOI] [PubMed] [Google Scholar]
- 4.Buttar SN, Yan TD, Taggart DP, Tian DH. Long-term and short-term outcomes of using bilateral internal mammary artery grafting versus left internal mammary artery grafting: a meta-analysis. Heart (British Cardiac Society) 2017;103(18):1419–1426. doi: 10.1136/heartjnl-2016-310864. [DOI] [PubMed] [Google Scholar]
- 5.Dhar SC, Taylor GI. The delay phenomenon: the story unfolds. Plast. Reconstr. Surg. 1999;104(7):2079–2091. doi: 10.1097/00006534-199912000-00021. [DOI] [PubMed] [Google Scholar]
- 6.Ejiofor JI, Kaneko T, Aranki SF. Current readings: single vs bilateral internal mammary artery in coronary artery bypass grafting. Sem Thorac Cardiovasc Surg. 2018;30(4):398–405. doi: 10.1053/j.semtcvs.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 7.Font-Réaulx, E. de, J. T. Lluch, R. L. López, P. S. Bialik, M. Á. C. Corona, L. G. D. López, E. A. Tirado, E. R. Navarrete, and A. G. Astiazarán. Thermography mapping patterns in temporal lobe epilepsy surgery. Surg Neurol Int 11:30, 2020. 10.25259/SNI_549_2019 [DOI] [PMC free article] [PubMed]
- 8.Haxhibeqiri-Karabdic I, Hasanovic A, Kabil E, Straus S. Improvement of ejection fraction after coronary artery bypass grafting surgery in patients with impaired left ventricular function. Med. Arch. (Sarajevo, Bosnia and Herzegovina) 2014;68(5):332–334. doi: 10.5455/medarh.2014.68.332-334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hennessy O, Potter SM. Use of infrared thermography for the assessment of free flap perforators in autologous breast reconstruction: a systematic review. JPRAS Open. 2020;23:60–70. doi: 10.1016/j.jpra.2019.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoffmann N, Koch E, Petersohn U, Kirsch M, Steiner G. Cerebral cortex classification by conditional random fields applied to intraoperative thermal imaging. Curr Direct Biomed Eng. 2016;2(1):475–478. doi: 10.1515/cdbme-2016-0105. [DOI] [Google Scholar]
- 11.Kukel I, Trumpp A, Plötze K, Rost A, Zaunseder S, Matschke K, Rasche S. Contact-free optical assessment of changes in the chest wall perfusion after coronary artery bypass grafting by imaging photoplethysmography. Appl. Sci. 2020;10(18):6537. doi: 10.3390/app10186537. [DOI] [Google Scholar]
- 12.Kusu-Orkar T-E, Kermali M, Oguamanam N, Bithas C, Harky A. Coronary artery bypass grafting: Factors affecting outcomes. J Cardiac Surg. 2020;35(12):3503–3511. doi: 10.1111/jocs.15013. [DOI] [PubMed] [Google Scholar]
- 13.Kuznetsova, A., P. B. Brockhoff, R. H. B. Christensen. lmerTest package: tests in linear mixed effects models. J. Stat. Soft. 2017. 10.18637/jss.v082.i13
- 14.Lekakis JP, Papamichael CM, Vemmos CN, Voutsas AA, Stamatelopoulos SF, Moulopoulos SD. Peripheral vascular endothelial dysfunction in patients with angina pectoris and normal coronary arteriograms. J. Am. Coll. Cardiol. 1998;31(3):541–546. doi: 10.1016/s0735-1097(97)00542-1. [DOI] [PubMed] [Google Scholar]
- 15.McNichols B, Spratt JR, George J, Rizzi S, Manning EW, Park K. Coronary artery bypass: review of surgical techniques and impact on long-term revascularization outcomes. Cardiol Therapy. 2021;10(1):89–109. doi: 10.1007/s40119-021-00211-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muller J, Muller J, Chen F, Tetzlaff R, Muller J, Bohl E, Kirsch M, Schnabel C. Registration and fusion of thermographic and visual-light images in neurosurgery. IEEE Trans Biomed Circ Syst. 2018;12(6):1313–1321. doi: 10.1109/TBCAS.2018.2856407. [DOI] [PubMed] [Google Scholar]
- 17.Muntean MV, Strilciuc S, Ardelean F, Pestean C, Lacatus R, Badea AF, Georgescu A. Using dynamic infrared thermography to optimize color Doppler ultrasound mapping of cutaneous perforators. Med. Ultrasonograph. 2015;17(4):503–508. doi: 10.11152/mu.2013.2066.174.dyn. [DOI] [PubMed] [Google Scholar]
- 18.Nergård S, Mercer JB, de Weerd L. Internal mammary vessels’ impact on abdominal skin perfusion in free abdominal flap breast reconstruction. Plast Reconstr. Surg. 2017;5(12):e1601. doi: 10.1097/GOX.0000000000001601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Phoon PHY, Hwang NC. Deep sternal wound infection: diagnosis, treatment and prevention. J Cardiothorac Vasc Anesth. 2020;34(6):1602–1613. doi: 10.1053/j.jvca.2019.09.019. [DOI] [PubMed] [Google Scholar]
- 20.Raheman FJ, Rojoa DM, Patel NG. Performance of infrared thermography and thermal stress test in perforator mapping and flap monitoring: a meta-analysis of diagnostic accuracy. J. Plast. Reconstruct. Aesthet. Surg. 2021;74(9):2013–2025. doi: 10.1016/j.bjps.2021.03.088. [DOI] [PubMed] [Google Scholar]
- 21.Sessler DI. Perioperative thermoregulation and heat balance. Lancet (London, England) 2016;387(10038):2655–2664. doi: 10.1016/S0140-6736(15)00981-2. [DOI] [PubMed] [Google Scholar]
- 22.Singh D, Singh AK. Role of image thermography in early breast cancer detection- Past, present and future. Comput. Methods Programs Biomed. 2020;183:105074. doi: 10.1016/j.cmpb.2019.105074. [DOI] [PubMed] [Google Scholar]
- 23.Sjøberg T, Mercer JB, Weum S, de Weerd L. The value of dynamic infrared thermography in pedicled thoracodorsal artery perforator flap surgery. Plast. Reconstr. Surg. 2020;8(7):e2799. doi: 10.1097/GOX.0000000000002799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tattersall GJ. Infrared thermography: a non-invasive window into thermal physiology. Compar. Biochem. Physiol. A. 2016;202:78–98. doi: 10.1016/j.cbpa.2016.02.022. [DOI] [PubMed] [Google Scholar]
- 25.Taylor GI, Chubb DP, Ashton MW. True and ‘choke’ anastomoses between perforator angiosomes: part I. anatomical location. Plast. Reconstr. Surg. 2013;132(6):1447–1456. doi: 10.1097/PRS.0b013e3182a80638. [DOI] [PubMed] [Google Scholar]
- 26.Thiessen FEF, Tondu T, Cloostermans B, Dirkx YAL, Auman D, Cox S, Verhoeven V, Hubens G, Steenackers G, Tjalma WAA. Dynamic infrared thermography (DIRT) in DIEP-flap breast reconstruction: a review of the literature. Eur. J. Obstetr. Gynecol. Reprod. Biol. 2019;242:47–55. doi: 10.1016/j.ejogrb.2019.08.008. [DOI] [PubMed] [Google Scholar]
- 27.Zhang S, Liu Y, Liu X, Liu T, Li P, Mei W. Infrared thermography for assessment of thoracic paravertebral block: a prospective observational study. BMC Anesthesiol. 2021;21(1):168. doi: 10.1186/s12871-021-01389-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang Y, Xiao W, Ng S, Zhou H, Min P, Xi W, Masia J, Blondeel P, Feng S. Infrared thermography-guided designing and harvesting of pre-expanded pedicled flap for head and neck reconstruction. J. Plast. Reconstr. Aesthet. Surg. 2021;74(9):2068–2075. doi: 10.1016/j.bjps.2020.12.102. [DOI] [PubMed] [Google Scholar]