Abstract
Mediastinal tumours are commonly encountered in general thoracic surgery practice. Benign tumours like thymoma and teratoma often need direct surgical resection if resectable. Pre-operative biopsy is not recommended. We report 2 cases which were radiologically diagnosed as thymoma and teratoma turned out to be Ewing sarcoma and chondrosarcoma respectively after surgical excision. This has challenged the notion whether biopsy is really not needed. More elaborate studies are needed to find out tumour characteristics which would warrant a biopsy even if they are resectable. In our cases, pre-operative biopsy would have changed the line of management in both patients. This has led to a change in institutional protocol that now, we do biopsy for any mediastinal tumour more than 8 cm and abutting the chest wall.
Keywords: Thymoma, Teratoma, Ewing sarcoma, Chondrosarcoma, Mediastinum
Introduction
Thymomas and teratomas are the frequently encountered benign mediastinal tumours. Most of these tumours are diagnosed radiologically [1]. Most of them, even if they are large, rarely infiltrate the important mediastinal structures. So, the recommended treatment for most of these tumours is excision [2]. There is usually no need to confirm the histopathological diagnosis before surgery with an image guided biopsy. It is even contra-indicated in resectable thymomas as biopsy will upstage the tumour by causing capsular rupture [3]. We report two cases which were diagnosed as benign tumours arising from the mediastinum radiologically but turned out to be rib tumours intra-operatively. The post-operative histopathology was chondrosarcoma and Ewing sarcoma. This has led to a change in our institute protocol that we do image-guided biopsy for any mediastinal tumour exceeding 8 cm in size and abutting the chest wall. There should be more detailed studies to recommend guidelines.
Case report
Case 1
This 33-year-old gentleman presented with 2 months history of chest pain and breathlessness. Chest radiograph showed a huge mass lesion almost occupying the whole of the left hemi-thorax (Fig. 1a). Computed tomogram (CT) showed a heterogeneously enhancing large soft tissue density lesion (16 × 15 × 12 cm) arising from the anterior mediastinum (Fig. 1b, c). The lesion was radiologically benign probably a thymoma or teratoma. As tumour markers were not elevated, a provisional diagnosis of thymoma was made. A cine magnetic resonance imaging was done which showed preserved fat planes between all the major mediastinal structures (Fig. 1d). In a multidisciplinary meeting, it was decided to go ahead with surgical resection. Intra-operatively, the tumour was arising from the left second rib and was growing towards the mediastinum. The tumour was completely excised piecemeal along with a part of the second rib. Histopathology showed round cell sarcoma possibly Ewing sarcoma with CD 99 and NKX2.2 positivity (Fig. 2a–d). The patient was discharged uneventfully and was referred for systemic chemotherapy and radiotherapy.
Fig. 1.
a Chest radiograph showing a large mass in the left hemi-thorax (blue star). b Computed tomogram (CT) showing a large anterior mediastinal mass with possible infiltration of the pulmonary artery (white arrow). c CT showing no signs of the tumour arising from the rib (yellow arrow). d Magnetic resonance imaging (MRI) showing preserved fat planes between the tumour and the pulmonary artery (white arrow)
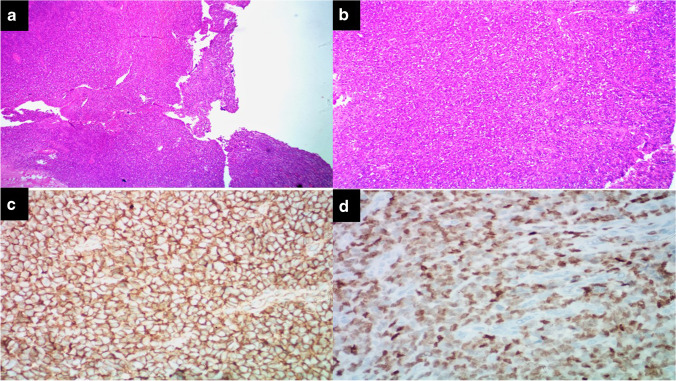
Fig. 2.
a Photomicrograph displaying sheets of round tumour cells, haematoxylin eosin (HE), 40 × . b Photomicrograph displaying sheets of round tumour cells, HE, 400 × . c Photomicrograph displaying sheets of round tumour cells showing membrane brown staining with CD99 immunohistochemistry (IHC), 400 × . d Photomicrograph displaying sheets of round tumour cells showing nuclear brown staining with NKX2.2 IHC, 400 ×
Case 2
This 34-year-old lady presented with 3 months history of chest pain and right shoulder pain. Chest radiograph showed a mass lesion in the right upper hemi-thorax. CT showed a heterogeneously enhancing lobulated soft tissue mass with fat, calcifications and few areas of necrosis seen arising from the right sided visceral space, measuring ~ 11 × 6 × 7 cm (Fig. 3a). This was radiologically diagnosed as a teratoma. There was significant compression on the trachea but no infiltration. Intra-operatively, it was noted that the tumour originated from the right second rib. It was completely excised along with part of the rib. Histopathology showed low grade chondrosarcoma for which she underwent volumetric modulated arc therapy (Fig. 3b, c). She was discharged without any events.
Fig. 3.
a Computed tomogram (CT) showing a large tumour arising from the mediastinum with fat and calcific densities suggestive of teratoma (yellow star). The trachea is significantly compressed. b Photomicrograph displaying cartilaginous tumour arranged in varying sized lobules (400 ×). c Photomicrograph displaying tumour lobules entrapping the bony trabeculae (400 ×). d CT showing the tumour in close contact with the second rib but with no evidence suggesting that it is the origin (yellow arrow)
Discussion
The International Thymic Malignancy Interest Group separates the mediastinum into the prevascular, visceral and para-vertebral compartments which is the recently accepted classification [4]. Thymomas and teratomas are the common mediastinal tumours. The National Comprehensive Cancer Network (NCCN) guidelines clearly say that pre-operative biopsy should not be done for resectable thymomas [3]. The tumour in case 1 was huge but radiologically benign with no infiltration of mediastinal structures. So, it was decided to proceed with surgical resection. Post-operatively, it turned out to be an Ewing sarcoma. If this diagnosis was known pre-operatively, the patient would have been offered systemic chemotherapy first [5]. This would have reduced the tumour burden and size which would have made the subsequent resection easier and safe for the patient. Retrospective scrutiny of the radiological images did not reveal any signs of rib involvement like erosion, scalloping which would suggest the tumour origin as bony.
There was a multidisciplinary meeting including the radiologists, oncologists and surgeons to discuss the radiological images of case 2. The position of the tumour was unique as it looked like it was arising from the visceral compartment (middle mediastinum). After elaborate discussions, it was diagnosed as a teratoma due to the contents of the lesion which were fat and calcific densities [1, 6]. Teratomas usually arise from the prevascular compartment but can arise anywhere as they are from the multi-potent embryonic cells. Pericardial teratomas are a known entity [7]. Intra-operatively, it was clear that it was a rib tumour with absolutely no adhesions with the mediastinum. A complete excision with part of the rib was done. Post-operative histopathology was low-grade chondrosarcoma. If this was known pre-operatively, a wider excision involving the adjacent ribs would have been done. Retrospective analysis of the radiological images showed that the tumour was very close to the second rib but there was no evidence of the tumour arising from it (Fig. 3d).
In both these cases, pre-operative biopsy would have either changed the line of management or altered the surgical plan. Although both were benign radiologically, they turned out to be malignant tumours. There are no clear-cut guidelines as to when to go for a pre-operative biopsy. NCCN guidelines state that biopsy should be done in unresectable lesions only. In our cases, both were resectable. Following these 2 cases, we have changed our institutional protocol. Any mediastinal tumour more than 8 cm and abutting the chest wall will be undergoing a pre-operative biopsy. There was one study in which a tumour size more than 8 cm resulted in more recurrences and so they suggested biopsy to identify candidates for pre-operative therapy [8]. More elaborate studies are needed to recommend these guidelines.
Conclusion
Thymoma and teratoma are commonly encountered benign mediastinal tumours. The treatment of choice is surgical resection for resectable tumours without pre-operative biopsy. Our cases challenge this notion and raises a question: is pre-operative biopsy really not required? More studies are needed to find out what are the characteristics to look out in these lesions, which would warrant a biopsy even if they are resectable.
Author contribution
All authors contributed to the study conception and design. The manuscript was written by Santhosh Regini Benjamin. The surgeries were done by Santhosh Regini Benjamin and Vinay Murahari Rao. The histopathology reporting was done by Thomas Alex Kodiatte and Twisha Adhikari. All authors read and approved the final manuscript.
Funding
None.
Declarations
The manuscript is original and has not been submitted to any other journal for simultaneous consideration and never been published elsewhere in any form or language.
Ethics approval
The approval of the institutional review board is not required.
Informed consent
Written consent for studies and publication were obtained from the patients prior to the surgery.
Conflict of interest
There was no conflict of interest in this study.
Statement of human and animal rights
The study has been performed in accordance with the ethical standards as laid down in the 1964 declaration of Helsinki and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Carter BW, Okumura M, Detterbeck FC, Marom EM. Approaching the patient with an anterior mediastinal mass: a guide for radiologists. J Thorac Oncol. 2014;9:S110–S118. doi: 10.1097/JTO.0000000000000295. [DOI] [PubMed] [Google Scholar]
- 2.Almeida PT, Heller D. Anterior Mediastinal Mass. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546608/. [PubMed]
- 3.National Comprehensive Cancer Network. Thymomas and thymic carcinomas (version 2.2019). https://www2.tri-kobe.org/nccn/guideline/lung/english/thymic.pdf. Accessed 14 Aug 2022.
- 4.Carter BW, Tomiyama N, Bhora FY, et al. A modern definition of mediastinal compartments. J Thorac Oncol. 2014;9:S97–101. doi: 10.1097/JTO.0000000000000292. [DOI] [PubMed] [Google Scholar]
- 5.Biswas B, Bakhshi S. Management of Ewing sarcoma family of tumors: current scenario and unmet need. World J Orthop. 2016;7:527–538. doi: 10.5312/wjo.v7.i9.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levitt RG, Husband JE, Glazer HS. CT of primary germ-cell tumors of the mediastinum. AJR Am J Roentgenol. 1984;142:73–78. doi: 10.2214/ajr.142.1.73. [DOI] [PubMed] [Google Scholar]
- 7.Cohen RA, Loarte P, Navarro V, Mirrer B. Mature cardiac teratoma in an adult. Cardiol Res. 2012;3:97–99. doi: 10.4021/cr182w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wright CD, Wain JC, Wong DR, et al. Predictors of recurrence in thymic tumors: importance of invasion, World Health Organization histology, and size. J Thorac Cardiovasc Surg. 2005;130:1413–1421. doi: 10.1016/j.jtcvs.2005.07.026. [DOI] [PubMed] [Google Scholar]