Abstract
The presence of multiple tracheal and bronchial diverticula is a rare condition. We present a case of a 22‐years old non‐smoker male with a history of pulmonary tuberculosis, having multiple tracheal and bronchial diverticula along with other common sequelae such as stenosed and collapsed upper lobe bronchi.
Keywords: bronchial stenosis, non‐smoker, tracheobronchial diverticula, tuberculosis, tuberculosis sequelae
Tracheobronchial diverticulosis is a uncommon entity in a young non‐smoking population. The presence of extensive bronchial diverticula along with sequelae of endobronchial tuberculosis in this patient poses a diagnostic and therapeutic challenge in a resource limited setting.

1. INTRODUCTION
Multiple tracheal and bronchial diverticula are uncommon entities and are often only detected incidentally by computed tomography (CT) or on autopsy specimens. 1 , 2 , 3 Tracheal diverticula are defined to be the condition with multiple sacs with narrow openings into the sac. 4 Though similar, bronchial diverticula are considered the cystic dilatation of the bronchial gland ducts. 5 A study by Polat et al. showed a 4% prevalence of paratracheal air cysts (PTACs) but the tracheal diverticulum (cysts with tracheal connections) comprised only 0.6%. 6 Combined bronchoscopic and bronchographic imaging estimated the presence of one or more bronchial diverticula among 30% of patients affected with chronic lung disease. 2 , 7 The diverticulum can be either congenital or acquired. 8 Clinically most are asymptomatic, and if symptomatic present with chronic cough, dyspnea, stridor, recurrent tracheobronchitis, etc. to list some. 9 , 10 CT scan and bronchoscopy are preferred for diagnosing the diverticula. 11 , 12 Herein we report a case of multiple tracheobronchial diverticula with a history of pulmonary tuberculosis in the past. This case report has been reported as per SCARE 2020 criteria. 13
2. CASE PRESENTATION
A 22‐year‐old non‐smoker, non‐alcoholic, Asian male, presented to the outpatient department of our hospital with complaints of chest pain, accompanied by shortness of breath and cough for about one and half years. He described having generalized chest pain without radiation, which was aggravated by activity, and gradually increased in intensity prompting him to seek care. The chest pain was associated with mild shortness of breath, occasional wheeze, and intermittent cough with scant non‐blood mixed sputum for the same duration. He has a significant history of pulmonary tuberculosis (sputum positive – no documents available), for which he was treated with antitubercular therapy (ATT) for 6 months 7 years back. He denied a history of fever, nasopharyngeal discharge, palpitations, significant weight changes, and had normal bowel and bladder habits. He did not have significant birth and genetic history. His family history was insignificant. Similarly, there were no surgical and psychosocial history.
On examination, he was normosthenic, with a body mass index (BMI) of 20.08 with a normal demeanor and posture. Grossly, he had no external deformity and no signs of pallor, icterus, cyanosis, lymphadenopathy, clubbing, edema, and dehydration. On examination of the respiratory system, bilateral diffuse wheeze along with diminished breath sound in the right upper lung region was heard on auscultation. His cardiovascular, gastrointestinal, and nervous system examinations were normal. Chest x‐ray revealed right upper lung collapse and pulmonary function test revealed moderate outflow limitations. Percentage changes in post bronchodilator was 4% in forced vital capacity (FVC), 7% in forced expiratory capacity in first second (FEV1), and 3% in ratio of FEV1/FVC. He was symptomatically managed with an inhaled bronchodilator, expectorant, and analgesics. Follow‐up on 3 months showed improvement.
However, 6 months later from the initial presentation, he then presented a recurrence of the symptoms, predominantly persistent cough with thick and purulent sputum production for the last 2 months. He also had associated shortness of breath, and occasional wheezing, and noticed some weight loss recently. On auscultation, he had bilaterally extensive wheezes. These findings required extensive workup, so laboratory samples for complete blood count (CBC), sputum for gram stain, nucleic acid amplification test (Xpert MTB/RIF assay) – as and culture & sensitivity were sent. In addition, contrast‐enhanced computed tomography (CT) and bronchoscopy was planned. Meanwhile, the patient was symptomatically managed with a bronchodilator, empiric antibiotic (ciprofloxacin), expectorant, mucolytics, and antitussive medications. No pathogenic organism was isolated in gram stain, culture and sensitivity. Acid fast bacilli was not seen in acid‐fast stain. Mycobacterium tuberculosis was not detected in the nucleic acid amplification test.
Contrast enhanced CT revealed complete collapse of the right upper lobe with bronchiectatic changes and bronchocele formation, bilateral tubular and varicose bronchiectatic changes with few bronchocele in the left lower lobe. There were multi‐septate cystic lesions in the mediastinum, some of which are communicating with the trachea and main‐stem bronchi, suggestive of tracheal and bronchial diverticula (Figures 1, 2, 3, 4).
FIGURE 1.

CT thorax shows the tracheal diverticula. (red arrows)
FIGURE 2.

CT thorax shows the tracheal diverticula. (red arrows)
FIGURE 3.

High resolution axial CT images of thorax show bronchial diverticula. (red arrows)
FIGURE 4.
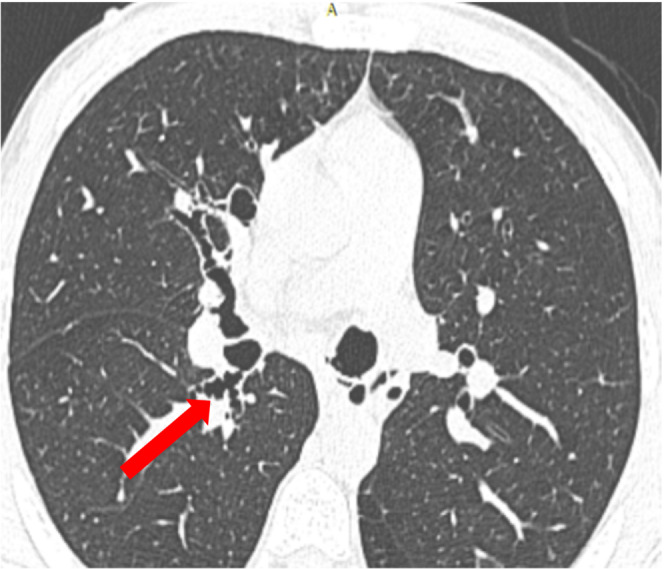
High resolution axial CT images of thorax show bronchial diverticula. (red arrows)
This was supported by the bronchoscopic findings shown in Figure 5. Bronchial wash was taken (from right main bronchus) and sent for cytology, acid fast bacilli (AFB) stain, gram stain, culture & sensitivity, tuberculosis culture and nucleic acid amplification test. The cytology of bronchoalveolar lavage (BAL) was negative for malignant cells, similarly gram stain, culture and nucleic acid amplification test turned out to be negative. Currently, the patient is asymptomatic and planned for follow‐up in 6 months for further assessment and management accordingly.
FIGURE 5.

Left main bronchus showing posterior diverticula, carina distorted with overlying diverticula, right bronchus opens directly into right upper lobe and bronchus intermedius separately. Stenosed right upper lobe bronchus and bronchus intermedius
3. DISCUSSION
According to Dorland's medical dictionary, a diverticulum is defined as a circumscribed pouch or sac of variable size occurring normally or created by herniation of the lining mucous membrane through a defect in the muscular coat of a tubular organ. 14 Tracheocele is considered to be a single sac entity with a wide opening whereas tracheal diverticula are defined to be the condition with multiple sacs with narrow openings into the sac. 4 Sayit et al. have defined multiple paratracheal conditions such as tracheocele, tracheal diverticula, lymphoepithelial cysts, and bronchogenic cysts under the heading of paratracheal cysts (PTACs). 15 However, some works of literature have used paratracheal air cysts and tracheal diverticulum interchangeably. 3 , 16 We would like to call for more research on these conditions. As like paratracheal air cysts, subcarinal air cysts are synonyms for small main bronchial diverticula. 17 We would suggest the concerned authorities for the standardized of these above‐mentioned terms and proper classification, which would help in better understanding the disease condition. Prevalence paratracheal cysts was found to be 1% in an autopsy series, 3 whereas in patients undergoing computed tomography (CT) scan was approximated to be in the range of 0.3–6.5%. 16 , 18 , 19 A study showed 4% prevalence of PTACs but the tracheal diverticulum (cysts with tracheal connections) comprised of only 0.6%. 6 The presence of multiple diverticula itself is a rare entity, as most case have a single paratracheal diverticulum, 1 so the presence of multiple tracheal as well as bronchial diverticula in our case is a rarity. Similarly, the presence of the bronchial diverticulosis in a smoker has been established, 2 but are very rare especially in non‐smoker as is the case in our patient. The postulated theory is the chronic inflammatory conditions including tuberculosis leads to erosion of the bronchial glands due to the infiltration resulting the dilation of the glands. 7 However, our patient was not actively infected with tuberculosis.
The differentiation of congenital and acquired diverticulum are based on the location, size, and histopathology, with acquired occurring at varying levels in the thoracic cavity usually with wide opening to the air sac. 8 Our patient had not had any symptoms prior to the initial presentation and has multi‐level diverticula, in addition the history of pulmonary tuberculosis in the past, likely suggest an acquired phenomenon. In addition, the scenario in our patient is that the post‐TB bronchostenosis on the right side likely led to chronic cough and prolonged stress on the posterior mucosal membrane on left bronchus, eventually forming the diverticulosis. However, labelling our case as a congenital condition cannot be ruled out completely as well.
Some literatures have mentioned about the association of tracheal diverticulum with Mounier‐Kuhn syndrome, 20 , 21 but our patient did not demonstrate dynamic airways collapse during respiration, which was further supported by measurements (transverse diameter) of airways in the CT scan. As the diverticula are usually an incidental finding, most remain asymptomatic, 9 but symptomatic patients have varied presentations such as chronic cough, dyspnea, stridor, recurrent tracheobronchitis, 10 recurrent hiccups and burping, 9 dysphonia from recurrent laryngeal nerve compression, 22 paratracheal abscess, 23 pneumomediastinum 24 etc. Our patient was initially bothered by chest pain rather than other accompanying symptom such as cough and dyspnea. Such cases can mimic chronic bronchitis. Commonly used diagnostic tools are CT scan 25 and bronchoscopy. 12 We also diagnosed the case with the use of both CT scan and further confirmation with bronchoscopy. Most diverticula are managed conservatively with mucolytic, antibiotics and physiotherapy. 15 Non‐medical management includes endoscopic laser cauterization or electrocoagulation, and surgery and these depends on the patients characteristics, symptomaticity and complications. 12 , 15 , 26 Currently our patient is asymptomatic with the mucolytics, inhaled bronchodilators and concurrent physiotherapy. Further plan is to review bronchoscopy in 6 months and plan further treatment accordingly.
4. CONCLUSION
Presence of multiple tracheal and bronchial diverticula is a rare entity. These diverticula can be the sequelae of pulmonary tuberculosis in a patient with a tuberculosis history. Tracheobronchial diverticula should be considered as a differential in a patient with a recurrent and chronic history of chest pain, cough, dyspnea, especially with prior history of tuberculosis infection. Tuberculosis diagnosis in resource limited setting like ours is based upon x‐ray and sputum acid fast stain which is not sufficient to diagnose the presence of congenital diverticula in this patient. However, the presence of post tuberculosis sequelae like stenosed and collapsed upper lobe bronchi along with tracheobronchial diverticula is suggestive of, although not confirmatory. Hence a post tuberculosis sequela is a presumptive diagnosis in this patient. We would also suggest the use of both imaging CT scan and if feasible bronchoscopy to diagnose the condition.
AUTHOR CONTRIBUTIONS
Bibek Timilsina: Literature review, writing the initial draft, case information, revising, editing, and submission of the manuscript. Raju Prasad Pangeni: Concept of study, writing, case information, revising of the manuscript. Sulochana Khadka: Literature review and writing the draft, editing, and revising the manuscript. Pradeep Raj Regmi: Literature review, imaging descriptions, revising, and editing the manuscript. Binaya Dhakal: Literature review, imaging descriptions, and editing the manuscript. All authors were involved in manuscript drafting, revising, and approved the final version.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST
No conflict of interest.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor‐in Chief of this journal on request.
GUARANTOR
Dr Bibek Timilsina, Nepalese Army Institute of Health Sciences – College of Medicine, Kathmandu, Nepal. Email: bibek.timilsina72@gmail.com, Phone +977–9846140918.
PROVENANCE AND PEER REVIEW
Not commissioned, externally peer reviewed.
ACKNOWLEDGMENT
Dr Dhan Bahadur Shrestha, Dr Saurab Karki, Dr Sunil Shahi, Dr Suhail Sapkota.
Timilsina B, Pangeni RP, Khadka S, Regmi PR, Dhakal B. Multiple tracheobronchial diverticula in a post‐TB patient: A case report. Clin Case Rep. 2022;10:e06787. doi: 10.1002/ccr3.6787
DATA AVAILABILITY STATEMENT
Data openly available in a public repository that issues datasets with DOIs
REFERENCES
- 1. Madan K, Das CJ, Guleria R. Posterior tracheal diverticulosis. J Bronchology Interv Pulmonol. 2014;21(4):338‐341. [DOI] [PubMed] [Google Scholar]
- 2. Sverzellati N, Ingegnoli A, Calabrò E, et al. Bronchial diverticula in smokers on thin‐section CT. Eur Radiol. 2010;20(1):88‐94. [DOI] [PubMed] [Google Scholar]
- 3. Mackinnon D. Tracheal diverticula. J Pathol Bacteriol. 1953;65(2):513‐517. [DOI] [PubMed] [Google Scholar]
- 4. Madana J, Yolmo D, Saxena SK, Gopalakrishnan S. Giant tracheocele with multiple congenital anomalies. Ear Nose Throat J. 2012;91(5):E13‐E15. [DOI] [PubMed] [Google Scholar]
- 5. Duprez A, Mampuys R. Cystic enlargement of the mucous glands of the bronchus associated with chronic bronchitis. Thorax. 1953;8(2):141‐147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Polat AV, Elmali M, Aydin R, Ozbay A, Celenk C, Murat N. Paratracheal air cysts: prevalence and correlation with lung diseases using multi‐detector CT. J Med Imaging Radiat Oncol. 2014;58(2):144‐148. [DOI] [PubMed] [Google Scholar]
- 7. Hirschfeld JH. Dilated bronchial mucous glands in chronic bronchitis, a neglected morphologic finding. Correlation of bronchoscopic and bronchographic appearance. Am Rev Respir Dis. 1961;83:16‐25. [DOI] [PubMed] [Google Scholar]
- 8. Lee SY, Joo S, Lee GD, Ham SJ, Park CH, Lee S. A case of symptomatic tracheal diverticulum and surgical resection as a treatment modality. Korean J Thorac Cardiovasc Surg. 2016;49(5):405‐407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Srivastava A, Guitron J, Williams VA. Tracheal diverticulum: an atypical presentation. J Thorac Cardiovasc Surg. 2014;148(6):3244‐3245. [DOI] [PubMed] [Google Scholar]
- 10. Early EK, Bothwell MR. Congenital tracheal diverticulum. Otolaryngol Head Neck Surg. 2002;127(1):119‐121. [DOI] [PubMed] [Google Scholar]
- 11. Haghi Z, Towhidi M, Fattahi H, Lari SM. Right Paratracheal air cyst (tracheal diverticulum). Respir Care. 2009;54(10):1409‐1411. [PubMed] [Google Scholar]
- 12. Soto‐Hurtado EJ, Peñuela‐Ruíz L, Rivera‐Sánchez I, Torres‐Jiménez J. Tracheal diverticulum: a review of the literature. Lung. 2006;184(6):303‐307. [DOI] [PubMed] [Google Scholar]
- 13. Agha RA, Franchi T, Sohrabi C, Mathew G, Kerwan A, SCARE Group . The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int J Surg. 2020;84:226‐230. [DOI] [PubMed] [Google Scholar]
- 14. Dorland WAN. Dorland's Illustrated Medical Dictionary. 32nd ed. Elsevier/Saunders; 2012. [Google Scholar]
- 15. Tanrivermis Sayit A, Elmali M, Saglam D, Celenk C. The diseases of airway‐tracheal diverticulum: a review of the literature. J Thorac Dis. 2016;8(10):E1163‐E1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Goo JM, Im JG, Ahn JM, et al. Right paratracheal air cysts in the thoracic inlet: clinical and radiologic significance. AJR Am J Roentgenol. 1999;173(1):65‐70. [DOI] [PubMed] [Google Scholar]
- 17. Weerakkody Y. Subcarinal air cyst | Radiology Reference Article | Radiopaedia.org [Internet]. Radiopaedia. https://radiopaedia.org/articles/subcarinal‐air‐cyst?lang=us#nav_radiographic‐features. Accessed 21 July, 2022.
- 18. Buterbaugh JE, Erly WK. Paratracheal air cysts: a common finding on routine CT examinations of the cervical spine and neck that may mimic pneumomediastinum in patients with traumatic injuries. AJNR Am J Neuroradiol. 2008;29(6):1218‐1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cheng HM, Chang PY, Chiang KH, Huang HW, Lee CC. Prevalence and characteristics of paratracheal air cysts and their association with emphysema in a general population. Eur J Radiol. 2012;81(10):2673‐2677. [DOI] [PubMed] [Google Scholar]
- 20. Kachhawa S, Meena M, Jindal G, Jain B. Case report: Mounier‐Kuhn syndrome. Indian J Radiol Imaging. 2008;18(4):316‐318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jaiswal AK, Munjal S, Singla R, Jain V, Behera D. A 46‐year‐old man with tracheomegaly, tracheal diverticulosis, and bronchiectasis: Mounier‐Kuhn syndrome. Lung India. 2012;29(2):176‐178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Caversaccio MD, Becker M, Zbären P. Tracheal diverticulum presenting with recurrent laryngeal nerve paralysis. Ann Otol Rhinol Laryngol. 1998;107(4):362‐364. [DOI] [PubMed] [Google Scholar]
- 23. Akabane S, Kawachi J, Fukai R, et al. A rare case of an infected tracheal diverticulum requiring emergency intervention: a case report. Int J Surg Case Rep. 2016;24:7‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Möller GM, ten Berge EJ, Stassen CM. Tracheocele: a rare cause of difficult endotracheal intubation and subsequent pneumomediastinum. Eur Respir J. 1994;7(7):1376‐1377. [PubMed] [Google Scholar]
- 25. Kwong JS, Müller NL, Miller RR. Diseases of the trachea and main‐stem bronchi: correlation of CT with pathologic findings. Radiographics. 1992;12(4):645‐657. [DOI] [PubMed] [Google Scholar]
- 26. Kim MJ, Jung H, Park CS. Incidental paratracheal air cyst in papillary thyroid cancer patient: a case report. Gland Surg. 2021;10(7):2334‐2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data openly available in a public repository that issues datasets with DOIs


