Key Findings.
-
▪
Low-income countries could have several challenges in implementing a cardiac resynchronization therapy (CRT) program.
-
▪
Taking into consideration that heart transplantation is not readily available in many low- and middle-income countries, CRT could be the best solution to improve survival of the heart failure patients with left bundle branch block and reduced left ventricular ejection fraction.
-
▪
We note the smaller number of women compared with men receiving CRT.
-
▪
There are many improvements required over the following years: increased education regarding indications for CRT among the national cardiological community and increased training of new specialists who can perform CRT implantation.
Background
Cardiac resynchronization therapy (CRT) has become an established treatment modality for patients with advanced heart failure (HF) and left bundle branch block (LBBB). Despite CRT being available for over 2 decades in high-income countries, it has only been performed in the Republic of Moldova in recent years. In this brief report, we discuss the development of a CRT program for HF therapy and our outcomes.
The Republic of Moldova is a country in eastern Europe with about 3 million inhabitants. The health care system is organized according to the principles of universal access to basic health services assuring equity and solidarity. This public health care service was established in 1994 and is financed from both the state and individuals through a mandatory health insurance mechanism. Moldova now has a range of public and private medical facilities, public agencies, and authorities. The health care institutions could be primary, secondary, or tertiary level. Medical facilities at the tertiary level provide specialized and highly specialized medical care for the whole population of the country. In order to obtain free access to some specialized care, health care providers must be contracted with the National Health Insurance Company (NHIC).1 This is true regardless of state or private tertiary center.
Challenges to health care delivery in HF patients
Despite advances in the health care system, the Republic of Moldova is a low-income country, and specialized services are not readily available. The challenges to providing high levels of HF care are multifaceted. Many HF therapies are not available at the moment in our country, such as left ventricular (LV) assist devices and cardiac transplantation. The total number of implantable cardioverter-defibrillator (ICD) procedures has been low, and until recently CRT was not able to be offered. The patients who were in need of CRT were referred to neighbor countries such as Ukraine or Romania for implantation. The situation was caused by several factors. The 2 most important challenges in the implementation of the CRT implantation program were (1) the lack of experienced electrophysiologists who could perform the implantation and (2) the cost of the devices.
CRT implantation program
We started our CRT program in 2015 when a team of experienced electrophysiologists from Ankara, Turkey started to regularly visit our electrophysiology lab in Medpark International Hospital, Chisinau. We started to perform electrophysiology procedures and to recommend CRT implantation for patients with HF and LBBB. However, it was not until 2016 that we performed the first CRT implantation in our country. The patient received a non–magnetic resonance imaging (MRI) conditional CRT with defibrillator (CRT-D) device with a bipolar LV lead. In the next 2 years, there were no further implantations of CRT devices in our center because of the high cost of the procedure for our population. We considered using dual chamber pacemakers as an option to perform CRT using LV-only pacing.2 Fortunately, the situation changed in 2019, when we obtained a budget from the NHIC to cover the costs of the CRT procedures. In 2019, the number of procedures increased to 9 and continued to grow in the following years. Now, we can perform the procedures at no cost for the patient, completely covered by the NHIC, or totally covered by the patient. Only the first patient personally covered the cost of the procedure.
In 2020, CRT implantation was implemented in a second center, in the Institute of Cardiology; the main state cardiological center of our country.3
CRT implantation procedures outcomes
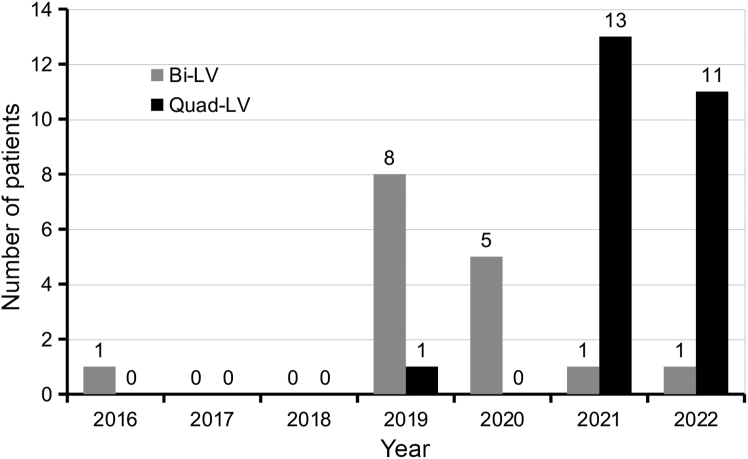
At our center, between April 2016 and July 2022, we performed CRT device implantation in a total of 41 patients, and all devices were CRT-Ds. The mean age of the patients was 61.6 ± 10.5 years. There were 36 (87.8%) men and 5 (12.2%) women, and all the patients had LV ejection fraction (LVEF) ≤35%, and the majority of the patients had LBBB (n = 39 [95%]). The number of implanted bipolar and quadripolar LV leads is represented in Figure 1.
Figure 1.
Types of left ventricular leads. Bi-LV = bipolar left ventricular lead; Quad-LV = quadripolar left ventricular lead.
There were 39 (95.1%) primary implantations and 2 (4.9%) upgrades: 1 from a dual chamber pacemaker to a CRT-D and 1 from an ICD to a CRT-D.
Our target area for LV lead placement is posterolateral or lateral branches. If there are no suitable branches in that area, we aim for anterolateral branches. If there are no suitable vessels for LV lead placement, we choose between epicardial implantation of the bipolar lead on the LV lateral wall or consider left bundle branch area pacing.4
Our implantation success rate was 38 (92.7%) of 41 patients. We had 3 (7.3%) failures of LV lead implantation in the first procedure: in one patient, the lead was implanted during a second procedural session; in a second patient, the lead was implanted in a fourth procedural session; and in a third patient, there were no suitable vessels for LV lead placement, and we performed nonselective left bundle branch area pacing.
Complication rates were the following. One (2.4%) patient had a cardiac arrest during the procedure and died 1 week later. One (2.4%) patient had a coronary sinus perforation, and the LV lead was successfully implanted in another session. Four (9.8%) patients developed a postprocedural hematoma, and 2 (4.9%) patients developed pocket infection. Of the 2 patients with infection, one developed pocket infection at day 377 after primary implantation and required complete removal of the system, and the other developed pocket infection at day 112 after an upgrade from ICD to CRT-D, and we performed revision with creation of a new subpectoral pocket. During a mean follow-up of 374 ± 362 days, we did not have any LV lead dislodgement.
Discussion
The Republic of Moldova is a low-income country, and the access to CRT devices has been drastically affected by the high cost of these devices. When the procedure cost in our hospital became covered by the NHIC, the number of procedures increased from 0 or 1 per year from 2014 to 2018 to 14 per year by 2021. While this has been a significant improvement, the number of the procedures will need to be increased to cover the needs of the HF population.
Do patients have equal access to these therapies, including CRT regardless of economic status? Yes and no: yes because any patient with mandatory health insurance has free access to a CRT procedure if indicated; no because there is not an established mechanism to regulate the choice of device type (CRT with pacemaker vs CRT-D; non–MRI conditional vs MRI conditional) at the national level. The decision is made either by administration of the institution or by the implanting physician.
Also, we note the smaller number of women compared with men in our experience (Figure 2). Prior reports have highlighted sex disparities in ICD and CRT implantation rates.5 Whether or not there is a sex disparity of HF treatments in Moldova will require future analysis of our HF patient population.
Figure 2.
Distribution by sex.
There are many improvements required in the coming years: (1) increased education regarding indications for CRT among the national cardiological community, (2) an increase in the number of procedures to better meet the needs of our HF patients, (3) implementation of remote monitoring (not yet available in the Republic of Moldova), and (4) increased training of new specialists who can perform CRT implantation.
Conclusions
CRT is an important tool in HF management that has been used routinely and worldwide in high-income countries. We have outlined the challenges to implementing a CRT program in our country and what the future needs are to provide this life-saving therapy to our HF patients. It is well established that CRT in correctly selected patients decreases mortality, increases quality of life, improves LVEF, and may postpone the need for heart transplantation.
Taking into consideration that heart transplantation is not readily available in many low- and middle-income countries, CRT could be the best solution to improve survival of the HF patient with LBBB and reduced LVEF.
Acknowledgments
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosures
The authors have no conflicts to disclose.
Authorship
All authors attest they meet the current ICMJE criteria for authorship.
References
- 1.Turcanu G., Domente S., Buga M., Richardson E. Republic of Moldova health system review. Health Syst Transit. 2012;14:1–151. [PubMed] [Google Scholar]
- 2.Rai M.K., Prabhu M.A., Sharma A., et al. ‘Optimized’ LV only pacing using a dual chamber pacemaker as a cost effective alternative to CRT. Indian Pacing Electrophysiol J. 2017;17:72–77. doi: 10.1016/j.ipej.2017.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moscalu V., Racila V., Rizov M., Gutan I., Vataman E. Device and surgical treatment of patients with heart failure based on the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Bull Acad Sci Moldova. 2022;72:82–90. [Google Scholar]
- 4.Padala S.K., Ellenbogen K.A. Left bundle branch pacing is the best approach to physiological pacing. Heart Rhythm O2. 2020;1:59–67. doi: 10.1016/j.hroo.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ingelaere S., Hoffmann R., Guler I., et al. Inequality between women and men in ICD implantation. Int J Cardiol Heart Vasc. 2022;41 doi: 10.1016/j.ijcha.2022.101075. [DOI] [PMC free article] [PubMed] [Google Scholar]