Abstract
Objective
To identify and summarize the evidence about the extent of overuse of medications in low- and middle-income countries, its drivers, consequences and potential solutions.
Methods
We conducted a scoping review by searching the databases PubMed®, Embase®, APA PsycINFO® and Global Index Medicus using a combination of MeSH terms and free text words around overuse of medications and overtreatment. We included studies in any language published before 25 October 2021 that reported on the extent of overuse, its drivers, consequences and solutions.
Findings
We screened 3489 unique records and included 367 studies reporting on over 5.1 million prescriptions across 80 low- and middle-income countries – with studies from 58.6% (17/29) of all low-, 62.0% (31/50) of all lower-middle- and 60.0% (33/55) of all upper-middle-income countries. Of the included studies, 307 (83.7%) reported on the extent of overuse of medications, with estimates ranging from 7.3% to 98.2% (interquartile range: 30.2–64.5). Commonly overused classes included antimicrobials, psychotropic drugs, proton pump inhibitors and antihypertensive drugs. Drivers included limited knowledge of harms of overuse, polypharmacy, poor regulation and financial influences. Consequences were patient harm and cost. Only 11.4% (42/367) of studies evaluated solutions, which included regulatory reforms, educational, deprescribing and audit–feedback initiatives.
Conclusion
Growing evidence suggests overuse of medications is widespread within low- and middle-income countries, across multiple drug classes, with few data of solutions from randomized trials. Opportunities exist to build collaborations to rigorously develop and evaluate potential solutions to reduce overuse of medications.
Résumé
Objectif
Identifier et résumer les données démontrant l'ampleur de la surconsommation de médicaments dans les pays à revenu faible et intermédiaire, mais aussi les causes de cette surconsommation, ses conséquences et les pistes de solution.
Méthodes
Nous avons mené une analyse exploratoire en effectuant une recherche dans les bases de données PubMed®, Embase®, APA PsycINFO® et l'Index Medicus mondial à l'aide d'une combinaison de termes MeSH et de mots en texte libre liés à la surconsommation de médicaments et aux surtraitements. Nous avons inclus des études rédigées dans toutes les langues et publiées avant le 25 octobre 2021, qui mentionnaient l'ampleur de la surconsommation, ses causes, ses conséquences et les pistes de solution.
Résultats
Nous avons passé en revue 3489 documents uniques et conservé 367 études faisant état de plus de 5,1 millions d'ordonnances dans 80 pays à revenu faible et intermédiaire – ces études concernaient 58,6% (17/29) des pays à revenu faible, 62,0 % (31/50) de ceux à revenu intermédiaire de la tranche inférieure et 60,0% (33/55) de ceux à revenu intermédiaire de la tranche supérieure. Sur l'ensemble des études reprises, 307 (83,7%) signalaient l'ampleur de la surconsommation de médicaments, avec des estimations comprises entre 7,3% et 98,2% (écart interquartile: 30,2-64,5). Cette surconsommation s'observait principalement dans des catégories telles que les antimicrobiens, les substances psychotropes, les inhibiteurs de la pompe à protons et les antihypertenseurs. Plusieurs causes étaient évoquées: méconnaissance des dégâts liés à une surconsommation, polypharmacie, mauvaise réglementation et influences économiques. Les conséquences étaient surtout néfastes pour la santé des patients et les coûts engendrés. À peine 11,4% (42/367) des études examinaient des solutions, parmi lesquelles des réformes réglementaires, ainsi que des initiatives de sensibilisation, de déprescription et d'audit–feedback.
Conclusion
Un faisceau croissant de preuves indique que la surconsommation de médicaments est largement répandue dans les pays à revenu faible et intermédiaire, dans de nombreuses catégories de substances, et peu d'informations circulent quant aux solutions issues des essais randomisés. Il existe néanmoins des opportunités de collaboration qui permettraient de développer et d'évaluer rigoureusement des pistes de solution pour lutter contre la surconsommation de médicaments.
Resumen
Objetivo
Identificar y resumir la evidencia sobre el grado del uso excesivo de medicamentos en los países de ingresos bajos y medios, sus causas, consecuencias y posibles soluciones.
Métodos
Se realizó una revisión exploratoria mediante búsquedas en las bases de datos PubMed®, Embase®, APA PsycINFO® y Global Index Medicus a partir de una combinación de términos MeSH y palabras de texto libre sobre el uso excesivo de medicamentos y el sobretratamiento. Se incluyeron estudios en cualquier idioma publicados antes del 25 de octubre de 2021 y que informaran sobre el grado del uso excesivo, sus causas, consecuencias y soluciones.
Resultados
Se examinaron 3489 registros únicos y se incluyeron 367 estudios que informaron sobre más de 5,1 millones de recetas en 80 países de ingresos bajos y medios, con estudios del 58,6 % (17/29) de todos los países de ingresos bajos, el 62,0 % (31/50) de todos los países de ingresos medios bajos y el 60,0 % (33/55) de los países de ingresos medios altos. De los estudios incluidos, 307 (83,7 %) informaron sobre el grado de uso excesivo de medicamentos, con estimaciones que oscilaban entre el 7,3 % y el 98,2 % (rango intercuartil: 30,2-64,5). Las clases más usadas en exceso incluían los antimicrobianos, los psicofármacos, los inhibidores de la bomba de protones y los antihipertensores. Los factores causantes incluyeron el conocimiento limitado de los daños del uso excesivo, la polifarmacia, la falta de regulación y las influencias financieras. Las consecuencias incluían el daño a los pacientes y el coste. Solo el 11,4 % (42/367) de los estudios evaluaron las soluciones, entre las que se encontraban las reformas normativas, las iniciativas de educación, de desprescripción y de retroalimentación de auditorías.
Conclusión
Cada vez hay más evidencias de que el uso excesivo de medicamentos está muy extendido en los países de ingresos bajos y medios, en múltiples clases de medicamentos, y se dispone de datos insuficientes sobre soluciones procedentes de ensayos aleatorizados. Hay oportunidades de crear colaboraciones para desarrollar y evaluar con rigor posibles soluciones para reducir el uso excesivo de los medicamentos.
ملخص
الغرض تحديد وتلخيص الأدلة على مدى الاستخدام المفرط للأدوية في الدول ذات الدخل المنخفض والمتوسط، ودوافع هذا الاستخدام، وعواقبه، والحلول الممكنة له.
الطريقة لقد أجرينا مراجعة عن كثب عن طريق البحث في قواعد البيانات PubMed®، وEmbase®، وAPA PsycINFO®، وGlobal Index Medicus باستخدام مجموعة من مصطلحات MeSH، وكلمات نصية حرة بخصوص الاستخدام المفرط للأدوية والمعالجة المفرطة. وقمنا بتضمين دراسات نُشرت بأية لغة قبل 25 أكتوبر/تشرين أول 2021، وكنا نُبلغ عن مدى الاستخدام المفرط ودوافعه، وعواقبه، وحلوله.
النتائج قمنا بفحص 3489 سجلاً فريداً، وتضمين 367 دراسة كشفت عن أكثر من 5.1 مليون وصفة طبية في 80 دولة ذات دخل منخفض إلى متوسط - مع دراسات من %58.6 (17/29) من كل الدول ذات الدخل المنخفض، و%62.0 (31/50) من كل الدول ذات الدخل المتوسط الأدنى، و%60.0 (33/55) من الدول ذات الدخل المتوسط الأعلى. من بين الدراسات المشمولة، كشفت 307 (%83.7) عن مدى الاستخدام المفرط للأدوية، مع تقديرات تتراوح من %7.3 إلى %98.2 (المدى بين الشرائح الربعية: 30.2 إلى 64.5). وشملت الفئات الأكثر استخدامًا بشكل شائع مضادات الميكروبات، والعقاقير المؤثرة على العقل، ومثبطات مضخة البروتون، والأدوية الخافضة للضغط. تضمنت الدوافع معرفة محدودة بأضرار الاستخدام المفرط، وتعدد الأدوية، وسوء التنظيم، والتأثيرات المالية. كانت العواقب هي حدوث الضرر للمرضى، فضلًا عن التكلفة. قامت %11.4 فقط (42/367) من الدراسات بتقييم الحلول، والتي تضمنت الإصلاحات التنظيمية، والمبادرات التعليمية، ومبادرات الحد من الوصفات الطبية، ومبادرات التدقيق والمراجعة.
الاستنتاج تشير الدلائل المتزايدة إلى أن الاستخدام المفرط للأدوية هو ظاهرة منتشرة في الدول ذات الدخل المنخفض والدخل المتوسط، عبر فئات عديدة من الأدوية، مع بيانات قليلة عن الحلول من التجارب العشوائية. توجد فرص لبناء علاقات تعاون لتطوير، وتقييم الحلول الممكنة بشكل فعال للحد من الاستخدام المفرط للأدوية.
摘要
目的
旨在确定和概述关于中低收入国家药物滥用的程度、其驱动因素、后果和潜在解决方案的证据。
方法
我们通过搜索 PubMed®、Embase®、APA PsycINFO® 和 Global Index Medicus 数据库,结合使用 MeSH 主题词和自由词,对药物滥用和过度治疗情况进行了一项范围审查。我们纳入了 2021 年 10 月 25 日之前以任何语言发表的研究,并报告了药物滥用的程度、其驱动因素、结果和解决方案。
结果
我们筛选了 3489 项独特记录,纳入了 367 份研究,报告涉及 80 个中低收入国家的 510 多万份处方,其中所有低收入国家的研究占 58.6% (17/29)、所有中下收入国家的研究占 62.0% (31/50) 以及中上收入国家的研究占 60.0% (33/55)。纳入的研究中,307 (83.7%) 份研究报告了药物滥用的程度,估计范围为 7.3% 至 98.2%(四分位距:30.2–64.5)。常见的滥用药物包括抗菌药物、精神治疗药物、质子泵抑制剂和抗高血压药。驱动因素包括对药物滥用危害的认识有限、多重用药、监管不力以及财务影响。后果是患者受到伤害并承担费用。只有 11.4% (42/367) 研究评估了解决方案,其中包括监管改革、教育、取消处方和审查反馈方案。
结论
越来越多的证据表明中低收入国家普遍存在药物滥用情况,涉及多种药物类别,但有关随机试验中得出的解决方案的数据却很少。应创建机会建立合作,严格开发和评估潜在解决方案,以减少药物滥用情况。
Резюме
Цель
Определить и обобщить данные о масштабах чрезмерного использования лекарственных средств в странах с низким и средним уровнем дохода, его движущих факторах, последствиях и возможных способах решения проблемы.
Методы
Авторы провели предварительный обзор путем поиска данных в базах PubMed®, Embase®, APA PsycINFO® и Global Index Medicus, используя комбинацию терминов MeSH и слов произвольного текста, касающихся чрезмерного употребления лекарственных средств и передозировки ими. Были включены исследования на всех языках, опубликованные до 25 октября 2021 г., в которых сообщалось о масштабах чрезмерного употребления, его причинах, последствиях и способах решения проблемы.
Результаты
Авторы проанализировали 3489 уникальных записей и включили 367 исследований, в которых сообщалось о более чем 5,1 млн рецептов в 80 странах с низким и средним уровнем дохода. Среди них были исследования из 58,6% (17/29) всех стран с низким уровнем дохода, 62,0% (31/50) всех стран с уровнем дохода ниже среднего и 60,0% (33/55) стран с уровнем дохода выше среднего. Из включенных исследований в 307 (83,7%) сообщалось о степени чрезмерного использования лекарственных средств, при этом оценки колебались от 7,3 до 98,2% (межквартильный диапазон: 30,2–64,5). Как правило, к числу классов чрезмерно используемых лекарственных средств относятся: противомикробные препараты, психотропные средства, ингибиторы протонной помпы и антигипертензивные препараты. К движущим факторам относятся: ограниченные знания о вреде чрезмерного использования, полипрагмазия, слабое регулирование и финансовое влияние. Последствия для пациентов заключаются во вреде, причиненном их здоровью, и дополнительных затратах. Только в 11,4% (42/367) исследований оценивались способы решения проблемы, которые включали программу по реформированию нормативно-правовой базы, инициативы в области образования, а также в направлении постепенного прекращения использования определенных лекарственных средств и внедрения аудита с обратной связью.
Вывод
Все больше данных свидетельствуют о том, что чрезмерное использование лекарственных средств широко распространено в странах с низким и средним уровнем дохода в отношении нескольких классов лекарств, при этом данных о способах решения проблемы, полученных в ходе рандомизированных исследований, немного. Существуют возможности для налаживания сотрудничества с целью тщательной разработки и оценки потенциальных способов сокращения чрезмерного использования лекарственных средств.
Introduction
Overuse in health care is broadly defined as tests or treatments that are inappropriate, unnecessary or of low value and are likely to cause people more harm than benefit. Hence, health-care overuse is a recognized threat to both human health and health system sustainability.1,2
Estimates of global overuse suggest that 20–40% of health-care resources may be wasted and that these resources might be better invested tackling unmet need, including underuse.3–5 While much of the evidence for overuse arises from high-income countries, where there is greater access to care, the consequences due to overuse may be even more serious in low-resource settings.1 For example, medication overuse, a key component of health-care overuse, can threaten both the viability of public budgets, including the universal health coverage, and population health in low- and middle-income countries.1
Global initiatives such as Choosing Wisely6 and Preventing Overdiagnosis7 are increasingly interested in addressing the problem of overuse in low- and middle-income settings. To identify gaps in the evidence-base and develop an agenda for future research and actions, we conducted a scoping review to characterize the evidence about the extent of overuse of medications in these countries, its drivers, consequences and potential solutions to reduce it in low- and middle-income countries. The work has also contributed to building a new global network to take the new agenda forward.
Methods
We conducted this scoping review following the Joanna Briggs Institute guidance,8 using an accelerated approach,9 and reported it following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews.10 The protocol was prospectively developed and registered at Open Science Framework.11
Search strategy
We searched four electronic databases: PubMed®, Embase®, APA PsycINFO® and Global Index Medicus, from inception until 25 October 2021, using a low- and middle-country search filter from Cochrane12 and without language restrictions. We used a combination of MeSH terms and free text words for the following general concepts: overuse of medications/overtreatment (Box 1; available at: https://www.who.int/publications/journals/bulletin/). We searched reference lists of all included studies, and contacted experts in the field to identify relevant and important grey literature.
Box 1. Search strategy used to identify studies on overuse of medications in low- and middle-income countries.
Search on 21 October 2021
PubMed®
(“Medical Overuse”[Mesh] OR Overmedicalization[tiab] OR Overmedicalisation[tiab] OR Overtreatment[tiab] OR “Over-treatment”[tiab] OR ((Overuse[tiab] OR Unnecessary[ti] OR Unwarranted[tiab] OR Inappropriate[ti] OR Deprescribing[tiab] OR De-implementation[tiab] OR Deimplementation[tiab]) AND (Medication[tiab] OR Therapeutic[tiab] OR Therapeutics[tiab] OR Antibiotics[tiab] OR Medicine[ti] OR Medicines[tiab] OR Prescriptions[tiab] OR “Pharmacological treatment”[tiab] OR “Pharmacological treatments”[tiab])))
AND
(afghanistan[Text Word] OR albania[Text Word] OR algeria[Text Word] OR american samoa[Text Word] OR angola[Text Word] OR antigua[Text Word] OR barbuda[Text Word] OR argentina[Text Word] OR armenia[Text Word] OR armenian[Text Word] OR aruba[Text Word] OR azerbaijan[Text Word] OR bahrain[Text Word] OR bangladesh[Text Word] OR barbados[Text Word] OR belarus[Text Word] OR byelarus[Text Word] OR belorussia[Text Word] OR byelorussian[Text Word] OR belize[Text Word] OR british honduras[Text Word] OR benin[Text Word] OR dahomey[Text Word] OR bhutan[Text Word] OR bolivia[Text Word] OR bosnia[Text Word] OR herzegovina[Text Word] OR botswana[Text Word] OR bechuanaland[Text Word] OR brazil[Text Word] OR brasil[Text Word] OR bulgaria[Text Word] OR burkina faso[Text Word] OR burkina fasso[Text Word] OR upper volta[Text Word] OR burundi[Text Word] OR urundi[Text Word] OR cabo verde[Text Word] OR cape verde[Text Word] OR cambodia[Text Word] OR kampuchea[Text Word] OR khmer republic[Text Word] OR cameroon[Text Word] OR cameron[Text Word] OR cameroun[Text Word] OR central african republic[Text Word] OR ubangi shari[Text Word] OR chad[Text Word] OR chile[Text Word] OR china[Text Word] OR colombia[Text Word] OR comoros[Text Word] OR comoro islands[Text Word] OR mayotte[Text Word] OR congo[Text Word] OR zaire[Text Word] OR costa rica[Text Word] OR cote d’ivoire[Text Word] OR cote d’ ivoire[Text Word] OR cote divoire[Text Word] OR cote d ivoire[Text Word] OR Côte d'Ivoire[Text Word] OR croatia[Text Word] OR cuba[Text Word] OR cyprus[Text Word] OR czech republic[Text Word] OR czechoslovakia[Text Word] OR djibouti[Text Word] OR french somaliland[Text Word] OR dominica[Text Word] OR dominican republic[Text Word] OR ecuador[Text Word] OR egypt[Text Word] OR united arab republic[Text Word] OR el salvador[Text Word] OR equatorial guinea[Text Word] OR spanish guinea[Text Word] OR eritrea[Text Word] OR estonia[Text Word] OR eswatini[Text Word] OR swaziland[Text Word] OR ethiopia[Text Word] OR fiji[Text Word] OR gabon[Text Word] OR gabonese republic[Text Word] OR gambia[Text Word] OR georgia[Text Word] OR georgian[Text Word] OR ghana[Text Word] OR gold coast[Text Word] OR gibraltar[Text Word] OR greece[Text Word] OR grenada[Text Word] OR guam[Text Word] OR guatemala[Text Word] OR guinea[Text Word] OR guyana[Text Word] OR guiana[Text Word] OR haiti[Text Word] OR hispaniola[Text Word] OR honduras[Text Word] OR hungary[Text Word] OR india[Text Word] OR indonesia[Text Word] OR timor[Text Word] OR iran[Text Word] OR iraq[Text Word] OR isle of man[Text Word] OR jamaica[Text Word] OR jordan[Text Word] OR kazakhstan[Text Word] OR kazakh[Text Word] OR kenya[Text Word] OR korea[Text Word] OR kosovo[Text Word] OR kyrgyzstan[Text Word] OR kirghizia[Text Word] OR kirgizstan[Text Word] OR kyrgyz republic[Text Word] OR kirghiz[Text Word] OR laos[Text Word] OR lao pdr[Text Word] OR lao people's democratic republic[Text Word] OR latvia[Text Word] OR lebanon[Text Word] OR lesotho[Text Word] OR basutoland[Text Word] OR liberia[Text Word] OR libya[Text Word] OR libyan arab jamahiriya[Text Word] OR lithuania[Text Word] OR macau[Text Word] OR macao[Text Word] OR macedonia[Text Word] OR madagascar[Text Word] OR malagasy republic[Text Word] OR malawi[Text Word] OR nyasaland[Text Word] OR malaysia[Text Word] OR maldives[Text Word] OR indian ocean[Text Word] OR mali[Text Word] OR malta[Text Word] OR micronesia[Text Word] OR kiribati[Text Word] OR marshall islands[Text Word] OR nauru[Text Word] OR northern mariana islands[Text Word] OR palau[Text Word] OR tuvalu[Text Word] OR mauritania[Text Word] OR mauritius[Text Word] OR mexico[Text Word] OR moldova[Text Word] OR moldovian[Text Word] OR mongolia[Text Word] OR montenegro[Text Word] OR morocco[Text Word] OR ifni[Text Word] OR mozambique[Text Word] OR portuguese east africa[Text Word] OR myanmar[Text Word] OR burma[Text Word] OR namibia[Text Word] OR nepal[Text Word] OR netherlands antilles[Text Word] OR nicaragua[Text Word] OR niger[Text Word] OR nigeria[Text Word] OR oman[Text Word] OR muscat[Text Word] OR pakistan[Text Word] OR panama[Text Word] OR papua new guinea[Text Word] OR paraguay[Text Word] OR peru[Text Word] OR philippines[Text Word] OR philipines[Text Word] OR phillipines[Text Word] OR phillippines[Text Word] OR poland[Text Word] OR polish people's republic[Text Word] OR portugal[Text Word] OR portuguese republic[Text Word] OR puerto rico[Text Word] OR romania[Text Word] OR russia[Text Word] OR russian federation[Text Word] OR ussr[Text Word] OR soviet union[Text Word] OR union of soviet socialist republics[Text Word] OR rwanda[Text Word] OR ruanda[Text Word] OR samoa[Text Word] OR pacific islands[Text Word] OR polynesia[Text Word] OR samoan islands[Text Word] OR sao tome and principe[Text Word] OR saudi arabia[Text Word] OR senegal[Text Word] OR serbia[Text Word] OR seychelles[Text Word] OR sierra leone[Text Word] OR slovakia[Text Word] OR slovak republic[Text Word] OR slovenia[Text Word] OR melanesia[Text Word] OR solomon island[Text Word] OR solomon islands[Text Word] OR norfolk island[Text Word] OR somalia[Text Word] OR south africa[Text Word] OR south sudan[Text Word] OR sri lanka[Text Word] OR ceylon[Text Word] OR saint kitts and nevis[Text Word] OR st kitts and nevis[Text Word] OR saint lucia[Text Word] OR st lucia[Text Word] OR saint vincent[Text Word] OR st vincent[Text Word] OR grenadines[Text Word] OR sudan[Text Word] OR suriname[Text Word] OR surinam[Text Word] OR Syrian Arab Republic[Text Word] OR syrian arab republic[Text Word] OR tajikistan[Text Word] OR tadjikistan[Text Word] OR tadzhikistan[Text Word] OR tadzhik[Text Word] OR tanzania[Text Word] OR tanganyika[Text Word] OR thailand[Text Word] OR siam[Text Word] OR timor leste[Text Word] OR east timor[Text Word] OR togo[Text Word] OR togolese republic[Text Word] OR tonga[Text Word] OR trinidad[Text Word] OR tobago[Text Word] OR tunisia[Text Word] OR turkey[Text Word] OR turkmenistan[Text Word] OR turkmen[Text Word] OR uganda[Text Word] OR ukraine[Text Word] OR uruguay[Text Word] OR uzbekistan[Text Word] OR uzbek[Text Word] OR vanuatu[Text Word] OR new hebrides[Text Word] OR venezuela[Text Word] OR vietnam[Text Word] OR viet nam[Text Word] OR middle east[Text Word] OR west bank[Text Word] OR gaza[Text Word] OR palestine[Text Word] OR yemen[Text Word] OR yugoslavia[Text Word] OR zambia[Text Word] OR zimbabwe[Text Word] OR northern rhodesia[Text Word] OR global south[Text Word] OR africa south of the sahara[Text Word] OR sub-Saharan africa[Text Word] OR sub-Saharan africa[Text Word] OR central africa[Text Word] OR north africa[Text Word] OR northern africa[Text Word] OR magreb[Text Word] OR maghrib[Text Word] OR sahara[Text Word] OR southern africa[Text Word] OR east africa[Text Word] OR eastern africa[Text Word] OR west africa[Text Word] OR western africa[Text Word] OR west indies[Text Word] OR indian ocean islands[Text Word] OR caribbean[Text Word] OR central america[Text Word] OR latin america[Text Word] OR south america[Text Word] OR central asia[Text Word] OR north asia[Text Word] OR northern asia[Text Word] OR southeastern asia[Text Word] OR south eastern asia[Text Word] OR south-east asia[Text Word] OR south-east asia[Text Word] OR western asia[Text Word] OR east europe[Text Word] OR eastern europe[Text Word] OR developing country[Text Word] OR developing countries[Text Word] OR developing nation[Text Word] OR developing nations[Text Word] OR developing population[Text Word] OR developing populations[Text Word] OR developing world[Text Word] OR less developed country[Text Word] OR less developed countries[Text Word] OR less developed nation[Text Word] OR less developed nations[Text Word] OR less developed world[Text Word] OR lesser developed countries[Text Word] OR lesser developed nations[Text Word] OR under developed country[Text Word] OR under developed countries[Text Word] OR under developed nations[Text Word] OR under developed world[Text Word] OR underdeveloped country[Text Word] OR underdeveloped countries[Text Word] OR underdeveloped nation[Text Word] OR underdeveloped nations[Text Word] OR underdeveloped population[Text Word] OR underdeveloped populations[Text Word] OR underdeveloped world[Text Word] OR middle income country[Text Word] OR middle income countries[Text Word] OR middle income nation[Text Word] OR middle income nations[Text Word] OR middle income population[Text Word] OR middle income populations[Text Word] OR low income country[Text Word] OR low income countries[Text Word] OR low income nation[Text Word] OR low income nations[Text Word] OR low income population[Text Word] OR low income populations[Text Word] OR lower income country[Text Word] OR lower income countries[Text Word] OR lower income nations[Text Word] OR lower income population[Text Word] OR lower income populations[Text Word] OR underserved countries[Text Word] OR underserved nations[Text Word] OR underserved population[Text Word] OR underserved populations[Text Word] OR under served population[Text Word] OR under served populations[Text Word] OR deprived countries[Text Word] OR deprived population[Text Word] OR deprived populations[Text Word] OR poor country[Text Word] OR poor countries[Text Word] OR poor nation[Text Word] OR poor nations[Text Word] OR poor population[Text Word] OR poor populations[Text Word] OR poor world[Text Word] OR poorer countries[Text Word] OR poorer nations[Text Word] OR poorer population[Text Word] OR poorer populations[Text Word] OR developing economy[Text Word] OR developing economies[Text Word] OR less developed economy[Text Word] OR less developed economies[Text Word] OR underdeveloped economies[Text Word] OR middle income economy[Text Word] OR middle income economies[Text Word] OR low income economy[Text Word] OR low income economies[Text Word] OR lower income economies[Text Word] OR low gdp[Text Word] OR low gnp[Text Word] OR low gross domestic[Text Word] OR low gross national[Text Word] OR lower gdp[Text Word] OR lower gross domestic[Text Word] OR lmic[Text Word] OR lmics[Text Word] OR third world[Text Word] OR lami country[Text Word] OR lami countries[Text Word] OR transitional country[Text Word] OR transitional countries[Text Word] OR emerging economies[Text Word] OR emerging nation[Text Word] OR emerging nations[Text Word])
Embase®
(“Unnecessary Procedure”/exp/mj OR Overmedicalization:ti,ab OR Overmedicalisation:ti,ab OR Overtreatment:ti,ab OR Over-treatment:ti,ab OR ((Overuse:ti,ab OR Unnecessary:ti OR Unwarranted:ti,ab OR Inappropriate:ti OR Deprescribing:ti,ab OR De-implementation:ti,ab OR Deimplementation:ti,ab) AND (Medication:ti,ab OR Therapeutic:ti,ab OR Therapeutics:ti,ab OR Antibiotics:ti,ab OR Medicine:ti OR Medicines:ti,ab OR Prescriptions:ti,ab OR “Pharmacological treatment”:ti,ab OR “Pharmacological treatments”:ti,ab)))
AND
(afghanistan OR albania OR algeria OR “american samoa” OR angola OR antigua OR barbuda OR argentina OR armenia OR armenian OR aruba OR azerbaijan OR bahrain OR bangladesh OR barbados OR belarus OR byelarus OR belorussia OR byelorussian OR belize OR “british honduras” OR benin OR dahomey OR bhutan OR bolivia OR bosnia OR herzegovina OR botswana OR bechuanaland OR brazil OR brasil OR bulgaria OR “burkina faso” OR “burkina fasso” OR “upper volta” OR burundi OR urundi OR “cabo verde” OR “cape verde” OR cambodia OR kampuchea OR “khmer republic” OR cameroon OR cameron OR cameroun OR “central african republic” OR “ubangi shari” OR chad OR chile OR china OR colombia OR comoros OR “comoro islands” OR mayotte OR congo OR zaire OR “costa rica” OR “cote divoire” OR “cote d ivoire” OR “cote divoire” OR “cote d ivoire” OR “ivory coast” OR croatia OR cuba OR cyprus OR “czech republic” OR czechoslovakia OR djibouti OR “french somaliland” OR dominica OR “dominican republic” OR ecuador OR egypt OR “united arab republic” OR “el salvador” OR “equatorial guinea” OR “spanish guinea” OR eritrea OR estonia OR eswatini OR swaziland OR ethiopia OR fiji OR gabon OR “gabonese republic” OR gambia OR georgia OR georgian OR ghana OR “gold coast” OR gibraltar OR greece OR grenada OR guam OR guatemala OR guinea OR guyana OR guiana OR haiti OR hispaniola OR honduras OR hungary OR india OR indonesia OR timor OR iran OR iraq OR “isle of man” OR jamaica OR jordan OR kazakhstan OR kazakh OR kenya OR korea OR kosovo OR kyrgyzstan OR kirghizia OR kirgizstan OR “kyrgyz republic” OR kirghiz OR laos OR “lao pdr” OR “lao peoples democratic republic” OR latvia OR lebanon OR lesotho OR basutoland OR liberia OR libya OR “libyan arab jamahiriya” OR lithuania OR macau OR macao OR macedonia OR madagascar OR “malagasy republic” OR malawi OR nyasaland OR malaysia OR maldives OR “indian ocean” OR mali OR malta OR micronesia OR kiribati OR “marshall islands” OR nauru OR “northern mariana islands” OR palau OR tuvalu OR mauritania OR mauritius OR mexico OR moldova OR moldovian OR mongolia OR montenegro OR morocco OR ifni OR mozambique OR “portuguese east africa” OR myanmar OR burma OR namibia OR nepal OR “netherlands antilles” OR nicaragua OR niger OR nigeria OR oman OR muscat OR pakistan OR panama OR “papua new guinea” OR paraguay OR peru OR philippines OR philipines OR phillipines OR phillippines OR poland OR “polish peoples republic” OR portugal OR “portuguese republic” OR “puerto rico” OR romania OR russia OR “russian federation” OR ussr OR “soviet union” OR “union of soviet socialist republics” OR rwanda OR ruanda OR samoa OR “pacific islands” OR polynesia OR “samoan islands” OR “sao tome” AND principe OR “saudi arabia” OR senegal OR serbia OR seychelles OR “sierra leone” OR slovakia OR “slovak republic” OR slovenia OR melanesia OR “solomon island” OR “solomon islands” OR “norfolk island” OR somalia OR “south africa” OR “south sudan” OR “sri lanka” OR ceylon OR “saint kitts” AND nevis OR “st kitts” AND nevis OR “saint lucia” OR “st lucia” OR “saint vincent” OR “st vincent” OR grenadines OR sudan OR suriname OR surinam OR Syrian Arab Republic OR “syrian arab republic” OR tajikistan OR tadjikistan OR tadzhikistan OR tadzhik OR tanzania OR tanganyika OR thailand OR siam OR “timor leste” OR “east timor” OR togo OR “togolese republic” OR tonga OR trinidad OR tobago OR tunisia OR turkey OR turkmenistan OR turkmen OR uganda OR ukraine OR uruguay OR uzbekistan OR uzbek OR vanuatu OR “new hebrides” OR venezuela OR vietnam OR “viet nam” OR “middle east” OR “west bank” OR gaza OR palestine OR yemen OR yugoslavia OR zambia OR zimbabwe OR “northern rhodesia” OR “global south” OR “africa south of the sahara” OR “sub saharan africa” OR “subsaharan africa” OR “central africa” OR “north africa” OR “northern africa” OR magreb OR maghrib OR sahara OR “southern africa” OR “east africa” OR “eastern africa” OR “west africa” OR “western africa” OR “west indies” OR “indian ocean islands” OR caribbean OR “central america” OR “latin america” OR “south america” OR “central asia” OR “north asia” OR “northern asia” OR “southeastern asia” OR “south eastern asia” OR “southeast asia” OR “south east asia” OR “western asia” OR “east europe” OR “eastern europe” OR “developing country” OR “developing countries” OR “developing nation” OR “developing nations” OR “developing population” OR “developing populations” OR “developing world” OR “less developed country” OR “less developed countries” OR “less developed nation” OR “less developed nations” OR “less developed world” OR “lesser developed countries” OR “lesser developed nations” OR “under developed country” OR “under developed countries” OR “under developed nations” OR “under developed world” OR “underdeveloped country” OR “underdeveloped countries” OR “underdeveloped nation” OR “underdeveloped nations” OR “underdeveloped population” OR “underdeveloped populations” OR “underdeveloped world” OR “middle income country” OR “middle income countries” OR “middle income nation” OR “middle income nations” OR “middle income population” OR “middle income populations” OR “low income country” OR “low income countries” OR “low income nation” OR “low income nations” OR “low income population” OR “low income populations” OR “lower income country” OR “lower income countries” OR “lower income nations” OR “lower income population” OR “lower income populations” OR “underserved countries” OR “underserved nations” OR “underserved population” OR “underserved populations” OR “under served population” OR “under served populations” OR “deprived countries” OR “deprived population” OR “deprived populations” OR “poor country” OR “poor countries” OR “poor nation” OR “poor nations” OR “poor population” OR “poor populations” OR “poor world” OR “poorer countries” OR “poorer nations” OR “poorer population” OR “poorer populations” OR “developing economy” OR “developing economies” OR “less developed economy” OR “less developed economies” OR “underdeveloped economies” OR “middle income economy” OR “middle income economies” OR “low income economy” OR “low income economies” OR “lower income economies” OR “low gdp” OR “low gnp” OR “low gross domestic” OR “low gross national” OR “lower gdp” OR “lower gross domestic” OR lmic OR lmics OR “third world” OR “lami country” OR “lami countries” OR “transitional country” OR “transitional countries” OR “emerging economies” OR “emerging nation” OR “emerging nations”)
APA PsycINFO®
(Medical Overuse.ti,ab. OR Overmedicalization.ti,ab. OR Overmedicalisation.ti,ab. OR Overtreatment.ti,ab. OR Over-treatment.ti,ab. OR ((Overuse.ti,ab. OR Unnecessary.ti. OR Unwarranted.ti,ab. OR Inappropriate.ti. OR Deprescribing.ti,ab. OR De-implementation.ti,ab. OR Deimplementation.ti,ab.) AND (Medication.ti,ab. OR Therapeutic.ti,ab. OR Therapeutics.ti,ab. OR Antibiotics.ti,ab. OR Medicine.ti. OR Medicines.ti,ab. OR Prescriptions.ti,ab. OR “Pharmacological treatment.”ti,ab. OR “Pharmacological treatments.”ti,ab.)))
AND
(afghanistan.mp. OR albania.mp. OR algeria.mp. OR “american samoa.”mp. OR angola.mp. OR antigua.mp. OR barbuda.mp. OR argentina.mp. OR armenia.mp. OR armenian.mp. OR aruba.mp. OR azerbaijan.mp. OR bahrain.mp. OR bangladesh.mp. OR barbados.mp. OR belarus.mp. OR byelarus.mp. OR belorussia.mp. OR byelorussian.mp. OR belize.mp. OR “british honduras.”mp. OR benin.mp. OR dahomey.mp. OR bhutan.mp. OR bolivia.mp. OR bosnia.mp. OR herzegovina.mp. OR botswana.mp. OR bechuanaland.mp. OR brazil.mp. OR brasil.mp. OR bulgaria.mp. OR “burkina faso.”mp. OR “burkina fasso.”mp. OR “upper volta.”mp. OR burundi.mp. OR urundi.mp. OR “cabo verde.”mp. OR “cape verde.”mp. OR cambodia.mp. OR kampuchea.mp. OR “khmer republic.”mp. OR cameroon.mp. OR cameron.mp. OR cameroun.mp. OR “central african republic.”mp. OR “ubangi shari.”mp. OR chad.mp. OR chile.mp. OR china.mp. OR colombia.mp. OR comoros.mp. OR “comoro islands.”mp. OR mayotte.mp. OR congo.mp. OR zaire.mp. OR “costa rica.”mp. OR “cote d’ivoire.”mp. OR “cote d’ ivoire.”mp. OR “cote divoire.”mp. OR “cote d ivoire.”mp. OR “ivory coast.”mp. OR croatia.mp. OR cuba.mp. OR cyprus.mp. OR “czech republic.”mp. OR czechoslovakia.mp. OR djibouti.mp. OR “french somaliland.”mp. OR dominica.mp. OR “dominican republic.”mp. OR ecuador.mp. OR egypt.mp. OR “united arab republic.”mp. OR “el salvador.”mp. OR “equatorial guinea.”mp. OR “spanish guinea.”mp. OR eritrea.mp. OR estonia.mp. OR eswatini.mp. OR swaziland.mp. OR ethiopia.mp. OR fiji.mp. OR gabon.mp. OR “gabonese republic.”mp. OR gambia.mp. OR georgia.mp. OR georgian.mp. OR ghana.mp. OR “gold coast.”mp. OR gibraltar.mp. OR greece.mp. OR grenada.mp. OR guam.mp. OR guatemala.mp. OR guinea.mp. OR guyana.mp. OR guiana.mp. OR haiti.mp. OR hispaniola.mp. OR honduras.mp. OR hungary.mp. OR india.mp. OR indonesia.mp. OR timor.mp. OR iran.mp. OR iraq.mp. OR “isle of man.”mp. OR jamaica.mp. OR jordan.mp. OR kazakhstan.mp. OR kazakh.mp. OR kenya.mp. OR korea.mp. OR kosovo.mp. OR kyrgyzstan.mp. OR kirghizia.mp. OR kirgizstan.mp. OR “kyrgyz republic.”mp. OR kirghiz.mp. OR laos.mp. OR “lao pdr.”mp. OR “lao people's democratic republic.”mp. OR latvia.mp. OR lebanon.mp. OR lesotho.mp. OR basutoland.mp. OR liberia.mp. OR libya.mp. OR “libyan arab jamahiriya.”mp. OR lithuania.mp. OR macau.mp. OR macao.mp. OR macedonia.mp. OR madagascar.mp. OR “malagasy republic.”mp. OR malawi.mp. OR nyasaland.mp. OR malaysia.mp. OR maldives.mp. OR “indian ocean.”mp. OR mali.mp. OR malta.mp. OR micronesia.mp. OR kiribati.mp. OR “marshall islands.”mp. OR nauru.mp. OR “northern mariana islands.”mp. OR palau.mp. OR tuvalu.mp. OR mauritania.mp. OR mauritius.mp. OR mexico.mp. OR moldova.mp. OR moldovian.mp. OR mongolia.mp. OR montenegro.mp. OR morocco.mp. OR ifni.mp. OR mozambique.mp. OR “portuguese east africa.”mp. OR myanmar.mp. OR burma.mp. OR namibia.mp. OR nepal.mp. OR “netherlands antilles.”mp. OR nicaragua.mp. OR niger.mp. OR nigeria.mp. OR oman.mp. OR muscat.mp. OR pakistan.mp. OR panama.mp. OR “papua new guinea.”mp. OR paraguay.mp. OR peru.mp. OR philippines.mp. OR philipines.mp. OR phillipines.mp. OR phillippines.mp. OR poland.mp. OR “polish people's republic.”mp. OR portugal.mp. OR “portuguese republic.”mp. OR “puerto rico.”mp. OR romania.mp. OR russia.mp. OR “russian federation.”mp. OR ussr.mp. OR “soviet union.”mp. OR “union of soviet socialist republics.”mp. OR rwanda.mp. OR ruanda.mp. OR samoa.mp. OR “pacific islands.”mp. OR polynesia.mp. OR “samoan islands.”mp. OR “sao tome” AND principe.mp. OR “saudi arabia.”mp. OR senegal.mp. OR serbia.mp. OR seychelles.mp. OR “sierra leone.”mp. OR slovakia.mp. OR “slovak republic.”mp. OR slovenia.mp. OR melanesia.mp. OR “solomon island.”mp. OR “solomon islands.”mp. OR “norfolk island.”mp. OR somalia.mp. OR “south africa.”mp. OR “south sudan.”mp. OR “sri lanka.”mp. OR ceylon.mp. OR “saint kitts” AND nevis.mp. OR “st kitts” AND nevis.mp. OR “saint lucia.”mp. OR “st lucia.”mp. OR “saint vincent.”mp. OR “st vincent.”mp. OR grenadines.mp. OR sudan.mp. OR suriname.mp. OR surinam.mp. OR Syrian Arab Republic.mp. OR “syrian arab republic.”mp. OR tajikistan.mp. OR tadjikistan.mp. OR tadzhikistan.mp. OR tadzhik.mp. OR tanzania.mp. OR tanganyika.mp. OR thailand.mp. OR siam.mp. OR “timor leste.”mp. OR “east timor.”mp. OR togo.mp. OR “togolese republic.”mp. OR tonga.mp. OR trinidad.mp. OR tobago.mp. OR tunisia.mp. OR turkey.mp. OR turkmenistan.mp. OR turkmen.mp. OR uganda.mp. OR ukraine.mp. OR uruguay.mp. OR uzbekistan.mp. OR uzbek.mp. OR vanuatu.mp. OR “new hebrides.”mp. OR venezuela.mp. OR vietnam.mp. OR “viet nam.”mp. OR “middle east.”mp. OR “west bank.”mp. OR gaza.mp. OR palestine.mp. OR yemen.mp. OR yugoslavia.mp. OR zambia.mp. OR zimbabwe.mp. OR “northern rhodesia.”mp. OR “global south.”mp. OR “africa south of the sahara.”mp. OR “sub saharan africa.”mp. OR “subsaharan africa.”mp. OR “central africa.”mp. OR “north africa.”mp. OR “northern africa.”mp. OR magreb.mp. OR maghrib.mp. OR sahara.mp. OR “southern africa.”mp. OR “east africa.”mp. OR “eastern africa.”mp. OR “west africa.”mp. OR “western africa.”mp. OR “west indies.”mp. OR “indian ocean islands.”mp. OR caribbean.mp. OR “central america.”mp. OR “latin america.”mp. OR “south america.”mp. OR “central asia.”mp. OR “north asia.”mp. OR “northern asia.”mp. OR “southeastern asia.”mp. OR “south eastern asia.”mp. OR “southeast asia.”mp. OR “south east asia.”mp. OR “western asia.”mp. OR “east europe.”mp. OR “eastern europe.”mp. OR “developing country.”mp. OR “developing countries.”mp. OR “developing nation.”mp. OR “developing nations.”mp. OR “developing population.”mp. OR “developing populations.”mp. OR “developing world.”mp. OR “less developed country.”mp. OR “less developed countries.”mp. OR “less developed nation.”mp. OR “less developed nations.”mp. OR “less developed world.”mp. OR “lesser developed countries.”mp. OR “lesser developed nations.”mp. OR “under developed country.”mp. OR “under developed countries.”mp. OR “under developed nations.”mp. OR “under developed world.”mp. OR “underdeveloped country.”mp. OR “underdeveloped countries.”mp. OR “underdeveloped nation.”mp. OR “underdeveloped nations.”mp. OR “underdeveloped population.”mp. OR “underdeveloped populations.”mp. OR “underdeveloped world.”mp. OR “middle income country.”mp. OR “middle income countries.”mp. OR “middle income nation.”mp. OR “middle income nations.”mp. OR “middle income population.”mp. OR “middle income populations.”mp. OR “low income country.”mp. OR “low income countries.”mp. OR “low income nation.”mp. OR “low income nations.”mp. OR “low income population.”mp. OR “low income populations.”mp. OR “lower income country.”mp. OR “lower income countries.”mp. OR “lower income nations.”mp. OR “lower income population.”mp. OR “lower income populations.”mp. OR “underserved countries.”mp. OR “underserved nations.”mp. OR “underserved population.”mp. OR “underserved populations.”mp. OR “under served population.”mp. OR “under served populations.”mp. OR “deprived countries.”mp. OR “deprived population.”mp. OR “deprived populations.”mp. OR “poor country.”mp. OR “poor countries.”mp. OR “poor nation.”mp. OR “poor nations.”mp. OR “poor population.”mp. OR “poor populations.”mp. OR “poor world.”mp. OR “poorer countries.”mp. OR “poorer nations.”mp. OR “poorer population.”mp. OR “poorer populations.”mp. OR “developing economy.”mp. OR “developing economies.”mp. OR “less developed economy.”mp. OR “less developed economies.”mp. OR “underdeveloped economies.”mp. OR “middle income economy.”mp. OR “middle income economies.”mp. OR “low income economy.”mp. OR “low income economies.”mp. OR “lower income economies.”mp. OR “low gdp.”mp. OR “low gnp.”mp. OR “low gross domestic.”mp. OR “low gross national.”mp. OR “lower gdp.”mp. OR “lower gross domestic.”mp. OR lmic.mp. OR lmics.mp. OR “third world.”mp. OR “lami country.”mp. OR “lami countries.”mp. OR “transitional country.”mp. OR “transitional countries.”mp. OR “emerging economies.”mp. OR “emerging nation.”mp. OR “emerging nations.”mp.)
Global Index Medicus (WPRIM (Western Pacific); LILACS (Americas); IMSEAR (South-East Asia); IMEMR (Eastern Mediterranean); AIM (Africa))
(“Medical Overuse” OR Overmedicalization OR Overmedicalisation OR (ti:(Overtreatment OR Over-treatment OR Overuse OR Deprescribing OR De-implementation OR Deimplementation)) AND (tw:(Medication OR Therapeutic OR Therapeutics OR Antibiotics OR Medicine OR Medicines OR Prescriptions OR “Pharmacological treatment” OR “Pharmacological treatments”)))
Eligibility criteria
We included studies from one or more low- and middle-income countries13 with a major focus on any of the four medication overuse themes: (i) extent of overuse; (ii) drivers and factors related to overuse; (iii) consequences of overuse; and (iv) solutions addressing the overuses. We included studies reporting data on low- and middle-income countries and high-income countries if data pertaining to low- and middle-income countries could be analysed separately, or the majority (≥ 75%) of reported data were from low- and middle-income countries. For this review, we used a broad commonly used definition of overuse of medications as the provision of medications which are unlikely to benefit the patient given the harms, cost, available alternatives or preferences of the patient – including unnecessary, inappropriate and potentially inappropriate medications.1,2 We also accepted operational definitions and assessments of primary study authors to estimate the extent of overuse of medications – including using Beers criteria® for Potentially Inappropriate Medication Use in Older Adults, or the screening tool of older persons’ prescriptions (STOPP), or appropriateness as judged by local guidelines.
We used the World Bank categorization from 202113 to define low- and middle-income countries (available in data repository).14
We included quantitative interventional and observational studies as well as qualitative studies, both primary and secondary studies, such as systematic reviews of eligible primary studies, and peer-reviewed articles or grey literature (e.g. eligible reports from governmental and nongovernmental organizations and conference abstracts). We included studies regardless of clinical setting (inpatient or outpatient, or the level of care), type of medications assessed (e.g. whether prescribed or nonprescription medications) and population type. We excluded case reports and case series, non-research opinion or analysis, literature reviews, conference abstracts with limited information to judge eligibility or to use for evidence synthesis, and studies where overuse of medications was not a major or primary focus or finding of the study.
Study selection
A total of nine pairs of reviewers independently screened titles and abstracts, and subsequently full text, using an open-access web-based tool.9 Any disagreements were resolved, at all stages, by discussion or reference to a third author.
Data extraction
We used a prospectively developed and piloted data extraction form. A single reviewer extracted data on (i) study characteristics including sample size and study design; (ii) overuse of medications including conditions and medication studied; (iii) main study themes (extent, drivers, consequences and solutions); and (iv) relevant key findings. For secondary studies (e.g. systematic reviews), we extracted data from summarized information of included studies and not directly from primary studies.
Data synthesis
We grouped studies by a priori defined groups: (i) the major focus or the four main themes; (ii) condition (i.e. per Global Burden of Disease classification); (iii) countries or country income level; and (iv) medication classes (i.e. by the major categories in the United States Pharmacopeial Medicare Model Guidelines v6.0).
Results
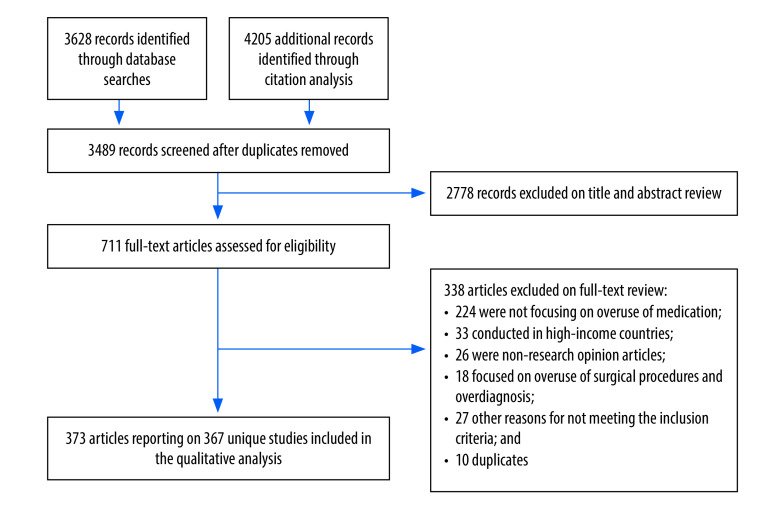
We identified a total of 3489 unique records. After screening titles and abstracts, we identified 711 records for full-text screening. Of the full-text articles screened, 338 were excluded with reasons recorded, and we included 373 articles15–387 reporting on a total of 367 unique studies (Fig. 1).15–381
Fig. 1.
Flowchart of the selection of articles included in study on overuse of medications in low- and middle-income countries
Characteristics of studies
The 367 included studies collectively reported on 5 120 468 prescribed or nonprescription medications (median: 1185; interquartile range, IQR: 333–3017) and more than 5 322 693 participants (median: 495; IQR: 222–1522) from 80 low- and middle-income countries. Of all 134 low- and middle-income countries, we found studies from 17 (58.6%) of all 29 low-income countries, 31 (62.0%) of all 50 lower-middle-income countries, and 33 (60.0%) of all 55 upper-middle-income countries. Twenty-one studies were multinational. Of the 346 studies originating from single countries, 232 (67.1%) were from upper-middle income countries and 99 (28.6%) from the East Asia and Pacific region (Table 1; Fig. 2).
Table 1. Characteristics of the 367 included studies in the scoping review on overuse of medications in low- and middle-income countries.
| Study characteristic | Study reference | No. (%) of studies |
|---|---|---|
|
Publication year
| ||
| 1990–2000 |
23
,
50
,
67
,
113
,
168
,
185
,
187
,
201
,
233
,
248
|
10 (2.7) |
| 2001–2010 |
18
,
22
,
49
,
54
,
56
,
57
,
71
,
85
,
95
,
110
,
145
,
159
,
169
,
172
,
181
,
193
,
195
,
202
,
213
,
256
,
264
,
270
,
285
,
289
,
291
,
295
,
318
|
27 (7.4) |
| 2011–2021 |
15
–
17
,
19
–
21
,
24
–
48
,
51
–
53
,
55
,
58
–
66
,
68
–
70
,
72
–
84
,
86
–
94
,
96
–
109
,
111
,
112
,
114
–
144
,
146
–
158
,
160
–
167
,
170
,
171
,
173
–
180
,
182
–
184
,
186
,
188
–
192
,
194
,
196
–
200
,
203
–
212
,
214
–
232
,
234
–
247
,
249
–
255
,
257
–
263
,
265
–
269
,
271
–
284
,
286
–
288
,
290
,
292
–
294
,
296
–
317
,
319
–
381
|
330 (89.9) |
|
Language of publication
| ||
| English |
15
,
17
–
21
,
24
–
49
,
51
–
66
,
68
–
91
,
93
–
132
,
134
–
165
,
167
,
168
,
170
–
213
,
215
–
224
,
226
,
228
–
235
,
238
–
266
,
268
–
270
,
272
,
273
,
275
–
289
,
291
–
329
,
331
–
381
|
347 (94.6) |
| Spanish |
50
,
90
,
133
,
169
,
227
,
236
,
237
,
267
,
271
,
274
,
290
|
11 (3) |
| French |
16
,
23
,
67
,
166
|
4 (1.1) |
| Portuguese |
22
,
92
,
214
,
225
|
4 (1.1) |
| Russian |
330
|
1 (0.3) |
|
No. of countries included in the study
| ||
| One |
15
–
23
,
25
–
52
,
54
–
57
,
59
–
72
,
74
–
82
,
84
,
85
,
87
–
138
,
141
–
147
,
149
–
169
,
171
–
179
,
181
–
200
,
202
–
208
,
211
–
221
,
223
–
331
,
334
–
346
,
348
–
381
|
346 (94.3) |
| Multiple countries |
24
,
53
,
58
,
73
,
83
,
86
,
139
,
140
,
148
,
170
,
180
,
201
,
209
,
210
,
222
,
242
,
297
,
326
,
332
,
333
,
347
|
21 (5.7) |
|
Country income level
| ||
| Low income |
18
,
20
,
21
,
38
,
67
,
75
,
77
,
111
,
127
,
129
,
144
,
146
,
166
,
183
,
230
,
231
,
245
,
249
,
256
,
262
,
316
,
329
,
335
,
337
,
343
|
25 (6.8) |
| Lower-middle income |
16
,
17
,
23
,
25
,
27
–
29
,
31
,
43
,
45
,
51
,
52
,
55
,
61
,
64
,
68
,
69
,
71
,
72
,
74
,
78
,
79
,
81
,
85
,
93
,
99
,
108
,
114
,
117
,
122
,
124
,
130
,
131
,
134
,
145
,
150
,
155
,
159
,
167
,
168
,
175
,
179
,
181
,
182
,
185
,
186
,
191
–
194
,
197
,
220
,
226
,
229
,
234
,
235
,
240
,
241
,
246
,
247
,
251
–
253
,
260
,
261
,
263
,
265
,
275
,
281
,
284
,
287
,
288
,
293
,
295
,
298
,
301
,
302
,
307
,
308
,
310
–
313
,
315
,
319
,
339
,
346
,
353
,
356
|
89 (24.3) |
| Upper-middle income |
15
,
19
,
22
,
26
,
30
,
32
–
37
,
39
–
42
,
44
,
46
,
47
,
49
–
51
,
54
,
56
,
57
,
59
,
60
,
62
,
63
,
65
,
66
,
70
,
76
,
80
,
82
,
84
,
87
–
92
,
94
–
98
,
100
–
107
,
109
,
110
,
112
,
113
,
115
,
116
,
118
–
121
,
123
,
125
,
126
,
128
,
132
,
133
,
135
–
138
,
141
–
143
,
147
,
149
,
151
–
154
,
156
–
158
,
160
–
165
,
169
,
171
–
174
,
176
–
178
,
184
,
187
–
190
,
195
,
196
,
198
–
200
,
202
–
208
,
211
–
219
,
221
,
223
–
225
,
227
,
228
,
232
,
233
,
236
–
239
,
243
,
244
,
248
,
250
,
254
,
255
,
257
–
259
,
264
,
266
–
274
,
276
–
280
,
282
–
286
,
289
–
292
,
294
,
296
,
299
,
300
,
303
–
306
,
309
,
314
,
317
,
318
,
320
–
325
,
327
,
328
,
330
,
331
,
334
,
336
,
338
,
340
–
342
,
344
,
345
,
348
–
352
,
354
,
355
,
357
–
381
|
232 (63.2) |
|
World Bank geographical regiona
| ||
| Sub-Saharan Africa |
20
,
21
,
25
,
27
,
28
,
31
,
45
,
55
,
67
,
75
–
77
,
108
,
111
,
122
,
124
,
127
,
129
–
131
,
135
,
144
,
146
,
166
,
168
,
183
,
185
,
197
,
220
,
226
,
228
,
230
,
231
,
245
,
249
,
256
,
261
–
263
,
282
,
287
,
288
,
295
,
316
,
329
,
335
,
337
,
343
,
349
|
49 (13.4) |
| East Asia and Pacific |
15
,
19
,
26
,
30
,
33
,
34
,
50
,
56
,
65
,
66
,
97
,
98
,
100
–
103
,
106
,
115
,
117
–
119
,
121
,
132
,
149
,
151
,
154
–
156
,
160
–
162
,
164
,
165
,
167
,
172
,
174
,
177
,
179
,
190
,
196
,
199
,
200
,
203
–
208
,
211
,
212
,
215
,
217
,
218
,
223
,
233
,
239
,
252
,
253
,
255
,
257
,
260
,
264
,
268
,
276
,
277
,
279
,
285
,
307
,
309
,
318
,
323
,
327
,
328
,
331
,
338
,
351
,
352
,
356
–
369
,
371
,
372
,
376
–
381
|
99 (27.0) |
| Europe and Central Asia |
32
,
35
,
39
,
51
,
54
,
59
,
60
,
62
,
70
,
80
,
84
,
91
,
94
,
95
,
107
,
125
,
126
,
128
,
150
,
152
,
157
,
158
,
176
,
178
,
187
–
189
,
198
,
202
,
250
,
265
,
266
,
276
,
283
,
296
,
303
,
304
,
306
,
310
,
317
,
320
,
322
,
324
,
325
,
330
,
334
,
336
,
340
,
342
,
344
,
345
,
350
,
370
,
373
|
54 (14.7) |
| Latin America and Caribbean |
22
,
37
,
40
,
42
,
44
,
63
,
82
,
87
,
88
,
90
,
92
,
104
,
105
,
109
,
110
,
112
,
113
,
116
,
120
,
133
,
136
–
138
,
141
–
143
,
147
,
169
,
171
,
184
,
195
,
213
,
214
,
216
,
219
,
221
,
224
,
225
,
227
,
236
–
238
,
243
,
248
,
254
,
258
,
259
,
267
,
269
,
270
,
273
,
274
,
286
,
289
,
290
,
299
,
300
,
305
,
341
,
348
,
354
,
355
|
62 (16.9) |
| Middle East and North Africa |
16
–
18
,
23
,
36
,
38
,
41
,
43
,
46
,
47
,
49
,
57
,
74
,
89
,
96
,
123
,
153
,
163
,
173
,
175
,
186
,
232
,
240
,
244
,
272
,
280
,
291
–
294
,
314
,
374
,
375
|
33 (9.0) |
| South Asia |
29
,
48
,
52
,
61
,
64
,
68
,
69
,
71
,
72
,
78
,
79
,
81
,
85
,
93
,
99
,
114
,
134
,
145
,
159
,
181
,
182
,
191
–
194
,
229
,
234
,
235
,
241
,
246
,
247
,
251
,
271
,
275
,
281
,
284
,
298
,
301
,
302
,
308
,
310
–
313
,
315
,
319
,
339
,
346
,
353
|
49 (13.4) |
|
Study design
| ||
| Interventional (e.g. RCT) |
37
,
45
,
50
,
52
,
55
,
65
,
66
,
98
,
106
,
108
,
114
,
117
,
176
,
186
,
189
,
192
,
201
,
215
,
231
,
234
,
236
,
240
,
249
,
260
,
267
,
299
,
313
,
329
,
341
,
347
,
356
,
359
,
363
,
368
,
369
,
378
|
36 (9.8) |
| Randomized trials (e.g. cluster RCTs) |
45
,
55
,
98
,
117
,
231
,
240
,
249
,
341
,
347
,
359
,
369
|
11 (3.0) |
| Controlled studies |
37
,
52
,
66
,
106
,
201
,
267
,
299
,
313
,
368
,
378
|
10 (2.7) |
| Before-and-after studies |
50
,
65
,
108
,
114
,
176
,
186
,
189
,
192
,
215
,
234
,
236
,
260
,
329
,
356
,
363
|
15 (4.1) |
| Observational |
15
–
23
,
25
–
36
,
38
,
40
,
42
–
44
,
46
,
48
,
51
,
54
,
56
–
64
,
67
–
72
,
74
–
77
,
79
–
85
,
87
–
97
,
99
–
105
,
107
,
109
–
113
,
115
,
116
,
118
–
120
,
122
–
138
,
140
–
147
,
149
–
175
,
177
–
185
,
187
,
188
,
190
,
191
,
193
–
200
,
202
–
208
,
211
–
214
,
216
–
221
,
223
–
230
,
232
,
233
,
235
,
237
–
239
,
241
–
248
,
250
–
259
,
261
–
264
,
266
,
268
–
271
,
273
–
298
,
300
–
312
,
314
–
325
,
327
,
328
,
330
–
340
,
342
–
346
,
348
–
355
,
357
,
358
,
360
–
362
,
364
–
367
,
370
–
377
,
379
–
381
|
313 (85.3) |
| Cross sectional (e.g. survey) |
16
–
23
,
25
,
26
,
28
–
36
,
38
,
40
,
42
–
44
,
46
,
51
,
54
,
57
–
64
,
67
–
72
,
74
–
76
,
79
,
80
,
84
,
85
,
87
–
97
,
100
–
105
,
107
,
109
–
113
,
115
,
116
,
118
,
120
,
123
–
127
,
129
–
132
,
134
,
135
,
138
,
140
,
142
–
144
,
146
,
149
,
150
,
152
,
153
,
155
–
158
,
160
–
165
,
167
,
169
–
171
,
173
,
174
,
178
–
181
,
185
,
187
,
190
,
191
,
193
–
197
,
199
,
202
–
204
,
206
,
208
,
211
–
214
,
217
–
219
,
221
,
224
–
227
,
229
,
230
,
232
,
233
,
237
,
239
,
243
–
245
,
247
,
251
,
252
,
254
–
259
,
261
–
264
,
266
,
269
,
270
,
273
–
275
,
277
–
281
,
283
–
294
,
296
–
298
,
300
–
304
,
306
–
308
,
310
–
312
,
314
–
317
,
320
–
322
,
324
,
327
,
328
,
330
,
332
–
339
,
343
–
345
,
348
–
352
,
354
,
357
,
358
,
360
–
362
,
364
–
367
,
370
–
372
,
374
–
377
,
379
–
381
|
257 (70.0) |
| Cohort (prospective or retrospective) |
81
–
83
,
122
,
128
,
137
,
154
,
159
,
172
,
175
,
182
,
184
,
188
,
198
,
200
,
216
,
220
,
228
,
235
,
238
,
241
,
250
,
268
,
271
,
276
,
282
,
295
,
305
,
309
,
319
,
323
,
325
,
331
,
340
,
346
,
353
,
373
|
37 (10.1) |
| Others (e.g. Delphi or ecological studies) |
15
,
27
,
48
,
56
,
99
,
119
,
132
,
145
,
147
,
151
,
166
,
168
,
177
,
179
,
183
,
223
,
242
,
246
,
342
|
19 (5.2) |
| Secondary research (e.g. review) |
24
,
39
,
41
,
47
,
49
,
53
,
73
,
78
,
86
,
121
,
139
,
148
,
209
,
210
,
222
,
265
,
272
,
326
|
18 (4.9) |
|
Health-care settings
| ||
| Hospital-based or secondary care |
16
,
17
,
20
,
21
,
23
,
26
,
29
–
31
,
33
,
35
–
37
,
39
,
41
,
42
,
46
,
49
,
51
,
55
,
56
,
59
–
62
,
65
,
66
,
71
,
72
,
75
,
76
,
79
–
82
,
84
,
87
–
90
,
93
–
97
,
99
,
101
,
106
,
107
,
109
,
113
,
115
,
125
,
126
,
128
,
130
–
134
,
136
,
137
,
140
,
141
,
143
,
146
,
147
,
150
–
152
,
154
,
155
,
159
,
162
–
165
,
168
,
172
,
175
,
177
,
178
,
181
,
182
,
184
,
185
,
187
–
189
,
191
,
192
,
197
–
200
,
203
,
205
,
207
,
212
,
213
,
215
,
217
–
221
,
223
,
224
,
229
,
230
,
233
–
237
,
239
,
241
,
243
,
244
,
248
,
250
,
253
,
257
,
260
–
263
,
267
,
268
,
270
,
271
,
273
,
274
,
276
,
277
,
282
,
285
,
288
–
290
,
294
,
295
,
297
–
299
,
301
,
302
,
306
,
308
,
310
–
313
,
316
–
319
,
321
,
323
,
325
,
327
–
336
,
338
–
340
,
342
,
343
,
345
,
346
,
348
,
350
,
353
–
356
,
358
,
361
,
365
,
372
,
374
–
381
|
195 (53.1) |
| Home-based or community or primary care |
18
,
19
,
22
,
25
,
27
,
28
,
34
,
38
,
40
,
43
–
45
,
48
,
52
–
54
,
57
,
58
,
64
,
68
,
69
,
73
,
74
,
77
,
86
,
92
,
98
,
100
,
102
–
105
,
108
,
111
,
112
,
114
,
116
–
120
,
122
–
124
,
127
,
129
,
135
,
138
,
144
,
145
,
149
,
153
,
156
–
158
,
160
,
161
,
167
,
169
–
171
,
176
,
180
,
190
,
193
–
196
,
202
,
204
,
206
,
214
,
216
,
225
–
228
,
232
,
238
,
240
,
242
,
245
,
249
,
252
,
254
,
256
,
258
,
259
,
264
–
266
,
269
,
278
–
280
,
283
,
284
,
286
,
291
–
293
,
300
,
303
–
305
,
307
,
309
,
322
,
324
,
326
,
337
,
347
,
351
,
352
,
357
,
359
,
360
,
366
,
368
–
371
,
373
|
123 (33.5) |
| Mixed |
15
,
24
,
47
,
67
,
91
,
110
,
121
,
139
,
142
,
148
,
166
,
183
,
186
,
201
,
210
,
211
,
222
,
247
,
272
,
275
,
281
,
287
,
296
,
344
,
349
,
363
|
26 (7.1) |
| Unclear or not applicable |
32
,
50
,
63
,
70
,
78
,
83
,
85
,
173
,
174
,
179
,
208
,
209
,
231
,
246
,
251
,
255
,
314
,
315
,
320
,
341
,
362
,
364
,
367
|
23 (6.3) |
|
Analysis approach
| ||
| Quantitative |
15
–
17
,
19
–
23
,
25
,
26
,
29
–
32
,
34
–
42
,
44
–
46
,
49
–
51
,
53
–
66
,
70
,
72
–
91
,
93
–
95
,
97
–
104
,
106
–
117
,
120
,
122
–
147
,
149
–
165
,
167
–
170
,
172
–
185
,
187
–
192
,
195
–
200
,
202
–
208
,
211
–
230
,
232
–
243
,
245
,
246
,
248
–
250
,
253
–
255
,
257
–
259
,
261
,
263
,
264
,
266
–
268
,
270
–
274
,
276
–
282
,
284
–
313
,
315
–
331
,
334
,
336
–
338
,
340
–
353
,
355
–
361
,
364
,
365
,
367
–
370
,
372
–
381
|
316 (86.1) |
| Qualitative |
24
,
27
,
33
,
43
,
47
,
48
,
68
,
96
,
118
,
119
,
166
,
193
,
194
,
201
,
244
,
247
,
251
,
256
,
260
,
265
,
269
,
275
,
283
,
332
,
333
,
339
|
26 (7.1) |
| Mixed |
18
,
28
,
52
,
67
,
69
,
71
,
92
,
105
,
121
,
148
,
171
,
186
,
209
,
210
,
231
,
252
,
262
,
314
,
335
,
354
,
357
,
362
,
363
,
366
,
371
|
25 (6.8) |
|
Condition or systems treatedb
| ||
| Infectious |
15
,
18
,
21
,
24
,
26
,
29
,
30
,
37
,
38
,
43
,
45
,
53
,
55
,
58
,
64
,
67
,
73
,
75
,
87
,
95
,
97
,
101
,
108
,
110
,
114
,
117
,
120
,
127
–
129
,
141
,
144
,
147
,
148
,
154
,
155
,
163
,
170
,
172
,
178
,
181
–
183
,
186
,
187
,
190
,
192
–
194
,
202
,
203
,
207
,
210
,
213
,
220
,
223
,
228
,
230
,
231
,
233
–
235
,
241
,
246
,
249
,
255
,
256
,
260
,
261
,
282
,
284
,
295
,
307
,
314
–
316
,
319
,
327
,
329
,
332
,
339
,
347
,
364
,
367
,
369
,
380
|
86 (23.4) |
| Cardiovascular |
20
,
33
,
36
,
39
,
42
,
46
,
70
,
77
,
103
,
107
,
112
,
132
,
143
,
146
,
157
,
158
,
174
,
184
,
188
,
197
,
204
,
206
,
208
,
217
,
218
,
221
,
236
,
238
,
239
,
241
,
243
,
270
,
284
,
286
,
297
,
300
–
302
,
304
,
305
,
312
,
330
,
336
,
337
,
346
,
358
,
374
,
379
|
48 (13.1) |
| Respiratory |
23
,
56
,
88
,
100
,
103
,
123
,
132
,
143
,
152
,
157
,
179
,
180
,
184
,
204
,
208
,
221
,
257
,
265
,
268
,
273
,
302
,
306
,
309
,
312
,
325
,
330
,
336
,
344
–
346
,
350
,
358
|
32 (8.7) |
| Diabetes |
32
,
33
,
42
,
70
,
77
,
83
,
84
,
103
,
157
,
158
,
174
,
204
,
208
,
217
,
238
,
241
,
248
,
270
,
286
,
300
,
302
,
304
,
310
,
312
,
320
,
321
,
336
,
337
,
342
,
355
,
375
|
31 (8.4) |
| Mental health |
23
,
33
,
35
,
36
,
44
,
54
,
64
,
73
,
75
,
138
,
142
,
195
,
198
,
199
,
213
,
219
,
226
,
232
,
238
,
239
,
253
,
300
,
302
,
305
,
311
,
317
,
337
,
341
,
375
|
29 (7.9) |
| Gastrointestinal |
41
,
64
,
73
,
82
,
122
,
124
,
132
,
143
,
173
,
179
,
188
,
199
,
211
,
212
,
215
,
237
,
243
,
263
,
264
,
287
,
328
,
343
,
353
,
362
|
24 (6.5) |
| Genitourinary |
23
,
36
,
73
,
80
,
93
,
96
,
109
,
132
,
145
,
157
,
198
,
236
,
250
,
323
,
346
,
377
|
16 (4.4) |
| Other (e.g. cancer and skin) |
39
,
42
,
62
,
72
,
115
,
157
,
177
,
185
,
188
,
214
,
221
,
238
,
239
,
262
,
286
,
287
,
302
,
305
,
313
,
329
,
331
,
340
,
348
,
372
|
24 (6.5) |
| Not specified |
16
,
17
,
19
,
22
,
25
,
27
,
28
,
31
,
34
,
40
,
47
–
52
,
57
,
59
–
61
,
63
,
65
,
66
,
68
,
69
,
71
,
74
,
76
,
78
,
79
,
81
,
85
,
86
,
89
–
92
,
94
,
98
,
99
,
102
,
104
–
106
,
111
,
113
,
116
,
118
,
119
,
121
,
125
,
126
,
130
,
131
,
133
–
137
,
139
,
140
,
149
–
151
,
153
,
156
,
159
–
162
,
164
–
171
,
175
,
176
,
189
,
191
,
196
,
200
,
201
,
205
,
209
,
216
,
222
,
224
,
225
,
227
,
229
,
240
,
242
,
244
,
245
,
247
,
251
,
252
,
254
,
258
,
259
,
266
,
267
,
269
,
271
,
272
,
274
–
281
,
283
,
285
,
288
–
294
,
296
,
298
,
299
,
303
,
308
,
318
,
322
,
324
,
326
,
333
–
335
,
338
,
349
,
351
,
352
,
354
,
356
,
357
,
359
–
361
,
363
,
365
,
366
,
368
,
370
,
371
,
373
,
376
,
378
,
381
|
156 (42.5) |
|
Medication classb
| ||
| Antimicrobials |
15
,
17
,
18
,
21
–
30
,
38
,
45
,
48
–
50
,
52
,
53
,
55
,
56
,
58
,
61
,
64
,
65
,
67
–
71
,
73
,
75
,
80
,
81
,
84
,
87
,
88
,
91
,
95
–
101
,
103
,
108
,
110
,
111
,
113
,
114
,
117
–
129
,
135
,
141
,
144
,
147
,
149
,
156
,
163
,
167
–
169
,
171
,
175
,
179
,
185
,
187
,
192
,
202
,
203
,
205
,
209
,
222
,
223
,
228
,
230
,
231
,
234
–
236
,
245
–
247
,
249
,
251
,
252
,
255
,
256
,
260
,
263
–
265
,
269
,
272
,
274
,
279
,
282
,
283
,
285
,
287
,
288
,
290
,
293
–
296
,
298
–
300
,
307
,
309
,
313
–
316
,
319
,
326
–
328
,
331
,
332
,
339
,
343
,
347
,
350
,
353
,
357
,
360
,
362
–
364
,
366
–
369
,
371
,
376
,
380
,
381
|
152 (41.4) |
| Psychotropic drugsc |
19
,
31
,
34
–
37
,
40
,
42
,
44
,
54
,
57
,
60
,
63
,
70
,
92
,
102
,
104
,
106
,
107
,
116
,
131
–
133
,
136
–
138
,
142
,
143
,
157
,
158
,
160
,
161
,
168
,
169
,
174
,
176
,
178
,
181
,
182
,
184
,
188
,
196
,
198
,
199
,
204
,
206
,
208
,
213
,
216
–
219
,
221
,
225
,
227
,
232
,
238
,
239
,
241
,
243
,
248
,
250
,
253
,
266
,
270
–
272
,
276
,
286
,
289
,
297
,
300
,
302
,
304
,
305
,
311
,
312
,
317
,
318
,
330
,
336
,
348
,
349
,
352
,
354
,
356
,
358
,
361
,
374
,
375
,
379
|
91 (24.8) |
| Blood pressure lowering and cardiovascular medications |
20
,
25
,
33
,
34
,
36
,
39
,
42
,
44
,
54
,
77
,
80
,
89
,
92
,
104
,
107
,
112
,
132
,
138
,
143
,
146
,
150
,
158
,
160
–
162
,
165
,
169
,
182
,
188
,
196
,
197
,
199
,
204
,
206
,
208
,
213
,
216
–
218
,
221
,
225
,
227
,
229
,
236
,
238
,
239
,
243
,
248
,
250
,
258
,
266
,
272
,
277
,
291
,
297
,
300
,
302
,
305
,
317
,
320
–
322
,
324
,
330
,
334
,
337
,
338
,
341
,
346
,
349
,
352
,
353
,
370
,
374
,
375
,
379
|
76 (20.7) |
| Analgesics and steroids |
19
,
25
,
31
,
34
,
36
,
39
,
40
,
43
,
44
,
60
,
67
,
70
,
80
,
88
,
96
,
104
,
106
,
116
,
131
,
138
,
140
,
143
,
146
,
150
,
152
,
159
,
169
,
176
,
180
–
182
,
184
,
188
,
195
,
196
,
198
,
204
,
213
,
226
,
229
,
236
,
238
,
239
,
246
,
250
,
257
,
272
,
273
,
276
,
277
,
286
,
291
,
297
,
300
,
302
–
304
,
310
,
317
,
325
,
330
,
336
,
337
,
340
,
344
,
346
,
349
,
352
–
354
,
375
|
71 (19.3) |
| Proton pump inhibitors and antacids |
33
,
39
–
42
,
44
,
79
,
82
,
89
,
90
,
94
,
96
,
107
,
109
,
132
,
134
,
165
,
173
,
176
,
178
,
188
,
196
,
200
,
204
,
212
,
215
,
218
,
221
,
225
,
227
,
236
,
237
,
241
,
246
,
248
,
266
,
276
,
277
,
280
,
286
,
303
,
310
,
312
,
336
,
346
,
352
,
353
,
358
,
361
,
365
,
374
,
375
,
378
|
53 (14.4) |
| Hypoglycaemic and hormonal medications |
32
,
34
,
39
,
44
,
77
,
80
,
83
,
103
,
112
,
143
,
158
,
160
,
161
,
169
,
206
,
208
,
216
,
217
,
248
,
266
,
300
,
304
,
312
,
320
,
321
,
342
,
349
,
355
,
375
,
376
|
30 (8.2) |
| Others |
16
,
25
,
72
,
74
,
85
,
115
,
162
,
214
,
246
,
258
,
262
,
322
,
324
,
329
,
338
,
370
,
372
,
377
|
18 (4.9) |
| Not specified | 46 , 47 , 51 , 59 , 62 , 66 , 76 , 78 , 86 , 93 , 105 , 130 , 139 , 145 , 148 , 151 , 153 – 155 , 164 , 166 , 170 , 172 , 177 , 183 , 186 , 189 – 191 , 193 , 194 , 201 , 207 , 210 , 211 , 220 , 224 , 233 , 240 , 242 , 244 , 254 , 259 , 261 , 267 , 268 , 275 , 278 , 281 , 284 , 292 , 301 , 306 , 308 , 323 , 333 , 335 , 345 , 351 , 359 , 373 | 61 (16.6) |
RCT: randomized controlled trial.
a Twenty-one studies covered more than one region.
b Not mutually exclusive.
c Including anti-anxiety, antidepressant, anticonvulsant and antipsychotic.
Fig. 2.
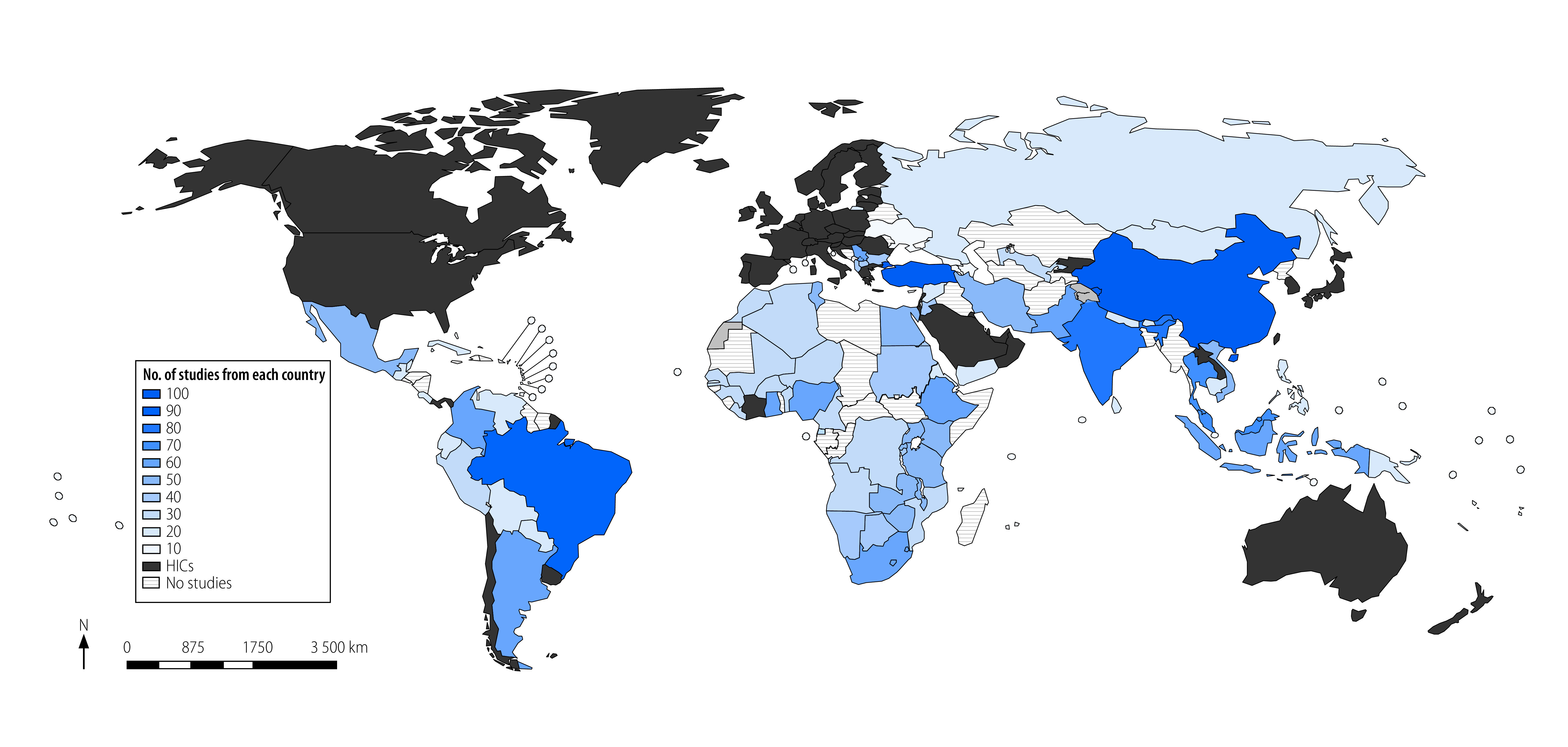
Studies of overuse of medications in low- and middle-income countries
Most studies (330; 89.9%) were published after 2010, with a marked increase in the number of studies per year. Most studies were written in English (347; 94.6%). In 195 studies (53.1%), the health-care setting was hospital-based. The study design in 313 (85.3%) studies was observational and in 26 (7.1%) studies was qualitative only. Twelve studies (3.3%) declared any funding from industry sources (Table 1; data repository).14
Extent of overuse
Of the included studies, 307 (83.7%; Table 2) reported on the extent of overuse of medications. Overall, the estimates of overuse of medications ranged from 7.3% in a study of 1264 older adults with diabetes in Türkiye (i.e. overtreated with blood pressure lowering and anti-diabetic medications)320 to 98.2% in a study of 599 critically ill older patients (i.e. ≥ 1 potentially inappropriate medications).141 The IQR of the estimates reported in 307 studies was 30.2–64.5% (Box 2; Fig. 3).
Table 2. Studies included on the extent of overuse of medications in low- and middle-income countries.
| Study characteristic | Study reference | No. (%) of studies |
|---|---|---|
| Total | 15 , 16 , 19 – 26 , 28 , 30 – 42 , 44 – 46 , 49 – 51 , 53 , 54 , 56 – 64 , 66 , 67 , 70 – 97 , 100 – 102 , 104 – 107 , 109 – 113 , 115 , 116 , 120 – 154 , 157 – 163 , 165 , 167 – 175 , 177 – 191 , 195 – 208 , 210 – 214 , 216 – 230 , 232 – 235 , 237 – 243 , 245 , 248 – 250 , 252 – 259 , 261 – 264 , 266 – 273 , 276 – 282 , 284 – 298 , 300 – 312 , 314 – 328 , 330 , 332 , 334 , 336 – 338 , 340 , 342 – 346 , 348 – 355 , 358 , 360 – 362 , 364 – 368 , 370 , 372 – 377 , 379 | 307 (83.7)a |
| Country income levelb | ||
| Low income | 20 , 21 , 38 , 67 , 75 , 77 , 111 , 127 , 129 , 144 , 146 , 170 , 183 , 230 , 245 , 249 , 256 , 262 , 316 , 337 , 343 | 21 (6.8) |
| Lower-middle income | 16 , 23 , 25 , 28 , 31 , 45 , 61 , 64 , 71 , 72 , 74 , 78 , 79 , 81 , 85 , 93 , 122 , 124 , 130 , 131 , 134 , 145 , 150 , 159 , 167 , 168 , 175 , 179 , 181 , 182 , 185 , 186 , 191 , 197 , 220 , 226 , 229 , 234 , 235 , 240 , 241 , 252 , 253 , 261 , 263 , 281 , 284 , 287 , 288 , 293 , 295 , 298 , 301 , 302 , 307 , 308 , 310 – 312 , 315 , 319 , 346 , 353 | 63 (20.5) |
| Upper-middle income | 15 , 19 , 22 , 26 , 30 , 32 – 37 , 39 – 42 , 44 , 46 , 49 – 51 , 54 , 56 , 57 , 59 , 60 , 62 , 63 , 66 , 70 , 76 , 80 , 82 , 84 , 87 – 90 , 92 , 94 – 97 , 100 – 102 , 104 – 107 , 109 , 110 , 112 , 113 , 115 , 116 , 120 , 121 , 123 , 125 , 126 , 128 , 132 , 133 , 135 – 138 , 141 – 143 , 147 , 149 , 151 – 154 , 157 , 158 , 160 – 163 , 165 , 169 , 171 – 174 , 177 , 178 , 184 , 187 – 190 , 195 , 196 , 198 – 200 , 202 – 208 , 211 – 214 , 216 – 219 , 221 , 223 – 225 , 227 , 228 , 232 , 233 , 237 – 239 , 243 , 248 , 250 , 254 , 255 , 257 – 259 , 264 , 266 – 270 , 272 , 273 , 276 – 280 , 282 , 285 , 286 , 289 – 292 , 294 , 296 , 300 , 303 – 306 , 309 , 314 , 317 , 318 , 320 – 325 , 327 , 328 , 330 , 334 , 336 , 338 , 340 , 342 , 344 , 345 , 348 – 352 , 354 , 355 , 358 , 360 – 362 , 364 – 368 , 370 , 372 – 377 , 379 | 205 (66.8) |
| Medication class | ||
| Antimicrobials | 15 , 21 – 26 , 28 , 30 , 38 , 45 , 49 , 50 , 53 , 56 , 58 , 61 , 64 , 67 , 70 , 71 , 73 , 75 , 80 , 81 , 84 , 87 , 88 , 95 – 97 , 100 , 101 , 110 , 111 , 113 , 120 – 129 , 135 , 141 , 144 , 147 , 149 , 163 , 167 – 169 , 171 , 175 , 179 , 185 , 187 , 202 , 203 , 205 , 222 , 223 , 228 , 230 , 234 , 235 , 245 , 249 , 252 , 255 , 256 , 263 , 264 , 269 , 272 , 279 , 282 , 285 , 287 , 288 , 290 , 293 – 296 , 298 , 300 , 307 , 309 , 314 – 316 , 319 , 326 – 328 , 332 , 343 , 350 , 353 , 360 , 362 , 364 , 366 – 368 , 376 | 110 (35.8) |
| Low-income country | 21 , 38 , 67 , 75 , 111 , 127 , 129 , 144 , 230 , 245 , 249 , 256 , 316 , 343 | 14 (12.7) |
| Lower-middle-income country | 23 , 25 , 28 , 45 , 61 , 64 , 71 , 81 , 122 , 124 , 167 , 168 , 175 , 179 , 185 , 234 , 235 , 252 , 263 , 287 , 288 , 293 , 295 , 298 , 307 , 315 , 319 , 353 | 28 (25.5) |
| Upper-middle income country | 15 , 22 , 26 , 30 , 49 , 50 , 56 , 70 , 80 , 84 , 87 , 88 , 95 – 97 , 100 , 101 , 110 , 113 , 120 , 121 , 123 , 125 , 126 , 128 , 135 , 141 , 147 , 149 , 163 , 169 , 171 , 187 , 202 , 203 , 205 , 223 , 228 , 255 , 264 , 269 , 272 , 279 , 282 , 285 , 290 , 294 , 296 , 300 , 309 , 314 , 327 , 328 , 350 , 360 , 362 , 364 , 366 – 368 , 376 | 61 (55.5) |
| Psychotropic drugsc | 19 , 31 , 34 – 37 , 40 , 42 , 44 , 54 , 57 , 60 , 63 , 70 , 92 , 102 , 104 , 106 , 107 , 116 , 131 – 133 , 136 – 138 , 142 , 143 , 157 , 158 , 160 , 161 , 168 , 169 , 174 , 178 , 181 , 182 , 184 , 188 , 196 , 198 , 199 , 204 , 206 , 208 , 213 , 216 – 219 , 221 , 225 , 227 , 232 , 238 , 239 , 241 , 243 , 248 , 250 , 253 , 266 , 270 – 272 , 276 , 286 , 289 , 297 , 300 , 302 , 304 , 305 , 311 , 312 , 317 , 318 , 330 , 336 , 348 , 349 , 352 , 354 , 358 , 361 , 374 , 375 , 379 | 89 (30.0) |
| Low-income country | N/A | 0 (0.0) |
| Lower-middle income country | 31 , 131 , 168 , 181 , 182 , 241 , 253 , 302 , 311 , 312 | 10 (11.2) |
| Upper-middle income country | 19 , 34 – 37 , 40 , 42 , 44 , 54 , 57 , 60 , 63 , 70 , 92 , 102 , 104 , 106 , 107 , 116 , 132 , 133 , 136 – 138 , 142 , 143 , 157 , 158 , 160 , 161 , 169 , 174 , 178 , 184 , 188 , 196 , 198 , 199 , 204 , 206 , 208 , 213 , 216 – 219 , 221 , 225 , 227 , 232 , 238 , 239 , 243 , 248 , 250 , 266 , 270 , 272 , 276 , 286 , 289 , 300 , 304 , 305 , 317 , 318 , 330 , 336 , 348 , 349 , 352 , 354 , 358 , 361 , 374 , 375 , 379 | 77 (86.5) |
| Antihypertensive | 20 , 25 , 33 , 34 , 36 , 39 , 42 , 44 , 54 , 77 , 80 , 89 , 92 , 104 , 107 , 112 , 132 , 138 , 143 , 146 , 150 , 158 , 160 – 162 , 165 , 169 , 182 , 188 , 196 , 197 , 199 , 204 , 206 , 208 , 213 , 216 – 218 , 221 , 225 , 227 , 229 , 238 , 239 , 243 , 248 , 250 , 258 , 266 , 272 , 277 , 291 , 297 , 300 , 302 , 305 , 317 , 320 – 322 , 324 , 330 , 334 , 337 , 338 , 346 , 349 , 352 , 353 , 370 , 374 , 375 , 379 | 74 (24.1) |
| Analgesics and steroids | 19 , 25 , 31 , 34 , 36 , 39 , 40 , 44 , 60 , 67 , 70 , 80 , 88 , 96 , 104 , 106 , 116 , 131 , 138 , 140 , 143 , 146 , 150 , 152 , 159 , 169 , 180 – 182 , 184 , 188 , 195 , 196 , 198 , 204 , 213 , 226 , 229 , 238 , 239 , 250 , 257 , 272 , 273 , 276 , 277 , 286 , 291 , 297 , 300 , 302 – 304 , 310 , 317 , 325 , 330 , 336 , 337 , 340 , 344 , 346 , 349 , 352 – 354 , 375 | 67 (21.8) |
| Proton pump inhibitors and antacids | 33 , 39 – 42 , 44 , 79 , 82 , 89 , 90 , 94 , 96 , 107 , 109 , 132 , 134 , 165 , 173 , 178 , 188 , 196 , 200 , 204 , 212 , 218 , 221 , 225 , 227 , 237 , 241 , 248 , 266 , 276 , 277 , 280 , 286 , 303 , 310 , 312 , 336 , 346 , 352 , 353 , 358 , 361 , 365 , 374 , 375 | 48 (15.6) |
| Methods for assessing overuse | ||
| Local professional norms or guidelines | 16 , 22 – 25 , 32 , 35 , 41 , 44 , 46 , 49 , 53 , 58 , 61 , 66 , 67 , 70 – 73 , 76 , 81 – 83 , 85 , 87 , 88 , 90 , 93 – 95 , 97 , 100 , 101 , 110 , 113 , 115 , 120 , 123 – 126 , 128 , 129 , 134 , 141 , 151 – 154 , 160 , 161 , 163 , 167 , 168 , 170 , 172 , 175 , 177 – 181 , 183 , 185 , 195 , 197 , 202 , 205 , 207 , 211 , 214 , 219 , 221 , 224 , 226 , 228 , 230 , 237 , 248 , 257 , 261 , 262 , 264 , 266 , 282 , 284 , 285 , 287 – 290 , 294 , 295 , 298 , 306 , 307 , 309 , 316 , 319 , 323 , 325 , 326 , 328 , 334 , 343 , 345 , 350 , 353 , 360 , 362 , 368 , 376 , 377 | 114 (37.1) |
| Beers criteria® for Potentially Inappropriate Medication Use in Older Adults | 19 , 31 , 36 , 39 , 40 , 51 , 54 , 57 , 60 , 63 , 77 – 79 , 89 , 92 , 96 , 102 , 104 – 106 , 109 , 112 , 116 , 130 , 131 , 133 , 136 – 138 , 142 , 143 , 150 , 158 – 161 , 165 , 169 , 182 , 184 , 191 , 196 , 198 , 199 , 206 , 213 , 216 , 218 , 225 , 227 , 229 , 238 , 239 , 253 , 254 , 258 , 259 , 270 , 271 , 281 , 286 , 291 , 297 , 301 , 302 , 305 , 310 – 312 , 324 , 330 , 337 , 346 , 349 , 352 , 354 , 358 , 361 , 373 , 375 | 80 (26.1) |
| Screening tool of older persons’ prescriptions | 20 , 33 , 34 , 59 , 60 , 78 , 102 , 107 , 130 , 132 , 133 , 142 , 146 , 161 , 184 , 188 , 196 , 199 , 204 , 217 , 218 , 225 , 229 , 243 , 250 , 253 , 254 , 258 , 311 , 317 , 337 , 352 | 32 (10.4) |
N/A: not applicable.
a The denominator is all 367 studies included in the scoping review.
b Including only single country studies.
c Including anti-anxiety, antidepressants and antipsychotics.
Box 2. Examples of key findings in the scoping review on overuse of medications in low- and middle-income countries.
Estimation of overuse (307 studies; Table 2)
For low-income countries (21 studies), the IQR of overuse estimates was 48.2–82.5%.
A cross-sectional study evaluating the appropriateness of antibiotic use for acute diarrhoeal disease among 303 inpatients in a large Ethiopian hospital serving 1.2 million people showed that 86.8% (263) of patients had received at least one antibiotic drug (92.6%; 174/188 of children younger than five years).343 The rate of overuse of antibiotics was 72.3%,343 which is a high level of overuse of antibiotics according to the recommendations of WHO for treating diarrhoeal disease.
For lower-middle-income countries (63 studies), the IQR of overuse estimates was 26.8–66.2%.
A retrospective analysis evaluating the use of potentially inappropriate medicines in 676 elderly patients in an Indian teaching hospital showed that 590 (87.3%) patients received at least one inappropriate medicine according to Beers criteria®, with metoclopramide being the most commonly used inappropriate medication (54.3%; 367 patients).179
For upper-middle-income countries (205 studies), the IQR of overuse estimates was 29.0–62.5.
A cross-sectional study evaluating the prevalence of potentially inappropriate medications among geriatric inpatients in a 3000-bed teaching hospital in China showed that the proportion of potentially inappropriate medications was 64.8% (4163/6424) according to Beers 2019 criteria® and 64.3% (4131/6424) according to Beers 2015 criteria®. Proton pump inhibitors were the most commonly prescribed inappropriate medications.162
Drivers of overuse (139 studies; Table 3)
A qualitative study explored the drivers of antibiotics overuse in Médecins Sans Frontières projects located in four low-income African countries. The study included 384 people who participated in semi-structured in-depth interviews, focus group discussions, and field observations. System-level drivers included failing health-care systems, such as underdeveloped and understaffed primary and secondary health-care systems. Individual-level drivers included strong patient demands for antibiotics that influenced prescription decisions, and high proportions of self-medication.383
Researchers of a qualitative study to identify drivers of potentially inappropriate medication use interviewed 417 geriatric patients in 22 public primary care facilities in Brazil, an upper-middle-income country. Important patient-related drivers included short consultation times (< 10 minutes) and polypharmacy. Clinician-related drivers included the number of patients attended and number of prescriptions per clinician.43
Consequences of overuse (31 studies; Table 3)
A cross-sectional study examined the costs and appropriateness of prophylactic preoperative antibiotic use among 1000 consecutive patients in six teaching hospitals in the Islamic Republic of Iran, an upper-middle-income country. Antibiotics were prescribed for 85 out of 87 (97.7%) procedures in which an antibiotic was not indicated. The average cost of antibiotic prescription per surgical procedure was US$ 100 and the estimated total cost of inappropriate prescription of cefazoline alone (the most frequently prescribed antibiotic) was US$ 4623; the GDP per capita is US$ 4802.160
A cross-sectional analysis was conducted of the economic impact of unnecessary proton pump inhibitors in Lebanon, an upper-middle-income country. The proportion of overuse was 71.4% (714/1000 individuals), with an estimated annual waste of US$ 25 million.170
Solutions for the problem of overuse (42 studies; Table 3)
A before-and-after study evaluated the effect of an intervention (training and pulse oximeters) on the appropriate use of oxygen among 1765 patients in a teaching hospital in Rwanda, a low-income country. Oxygen use in the emergency department decreased from a median of 32.0 (IQR: 28.0–35.0) tanks per day to 16.0 (IQR: 12.5–21.0) tanks per day at week 12. The proportion of appropriate use of oxygen therapy increased from 18.7% (34/182) at baseline to 42.0% (42/100) at 12 weeks.329
A multicentre RCT of the effect of point-of-care CRP testing on the inappropriate use of antibiotics for non-severe acute respiratory infections among 2037 patients in 10 Vietnamese primary health-care centres showed that the number of patients who used antibiotics within 14 days was 581 (64.4%) of 902 patients in the CRP group versus 738 (77.9%) of 947 patients in the control group (OR: 0.49; 95% CI: 0.40–0.61).115
CI: confidence interval; CRP: C-reactive protein; GDP: gross domestic product; IQR: interquartile range; OR: odds ratio; RCT: randomized controlled trial; US$: United States dollars; WHO: World Health Organization.
Note: Results reported in the box are based on key studies that we have selected to represent different countries (i.e. income group or WHO region) and main theme or focus (e.g. solution or estimate). However, these studies were conducted in local settings and might not be representative to the wider low- and middle-income countries context. Therefore, generalizability of these findings to the low- and middle-income countries context is limited and should be done with extreme caution.
Fig. 3.
Average percentage of overuse of medications in low- and middle-income countries
Note: We obtained the data from studies reporting on the extent of overuse of medications.
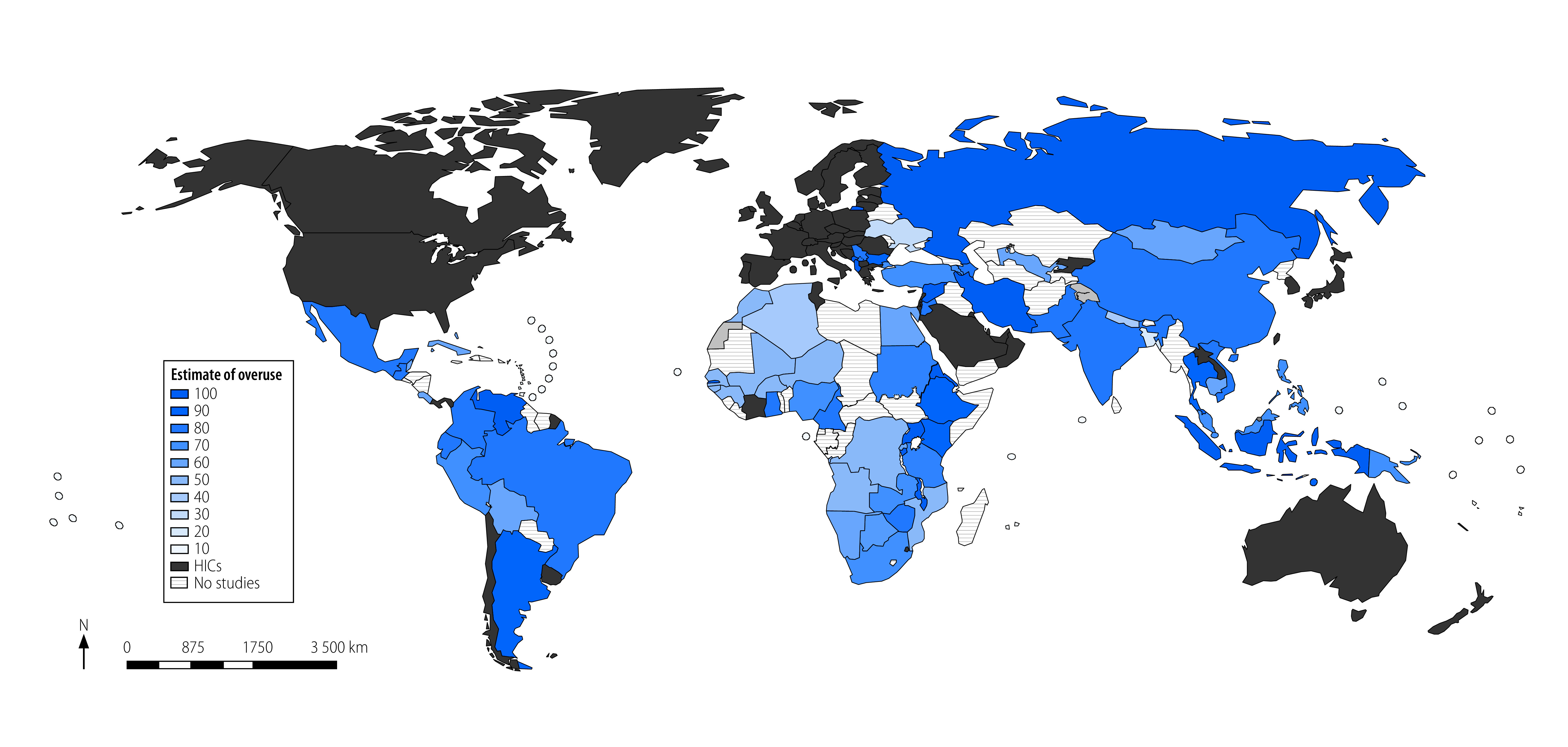
The top five classes of medications that were most frequently examined and reported in the 307 studies were (i) antimicrobials (110 studies; 35.8%); (ii) anti-anxiety, antidepressants and antipsychotics (89 studies; 30.0%); (iii) antihypertensive drugs (74 studies; 24.1% ); (iv) analgesics and steroids (67 studies; 21.8%); and (v) proton pump inhibitors and antacids (48 studies; 15.6%; Table 2).
The three most common methods for assessing overuse of medications were: comparing existing prescribing practices with what would be considered appropriate under local professional norms or guidelines (114 studies; 37.1%); using Beers criteria® to identify potentially inappropriate medications (80 studies; 26.1%); and using STOPP (32 studies; 10.4%; Table 2).
Antimicrobials
The estimate of the overuse of antibiotics in the 110 studies range from 18.4% (40/217 prescriptions) in a retrospective evaluation of the inappropriateness of antibiotics prescribed for 735 patients in three primary health care clinics in Malaysia309 to 97.0% (194) of 200 pharmacies inappropriately dispensing antibiotics without prescriptions in the Syrian Arab Republic.36 A 2019 Chinese survey of more than 74 648 antibiotics prescriptions in 16 rural primary care health centres found that only 8.8% (6567) of prescriptions were appropriate and 84.1% (62 780) of prescriptions were deemed unnecessary, according to guidelines.96 A 2021 systematic review of 23 studies estimated the proportion of nonprescription inappropriate dispensing of antibiotics in sub-Saharan African countries at 69.0% (95% confidence interval, CI: 58.0–80.0).73 The IQR of the estimates reported in the 110 studies was 34.3–66.5%. In the 14 low-income countries included, the estimates ranged between 53.9% and 85.4%; the ranges were 30.5–64.3% and 34.3–60.9% for 28 lower-middle- and 61 upper-middle-income countries, respectively (Table 2).
Psychotropic drugs
The estimates of the overuse of anti-anxiety and antidepressant medications in the 89 studies range from 10.0 % in a survey of 1048 Chilean adults 65 years or older according to Beers criteria®269 to 91.0 % in a cross-sectional analysis of 456 older adults in a tertiary hospital in India using both Beers® and STOPP criteria.311 The IQR of the estimates reported in the 89 studies was 30.1–61.7%. There was no study for a low-income country. For 10 lower-middle- and 77 upper-middle-income countries, the estimate ranges were 28.6–87.3% and 31.2–61.4%, respectively (Table 2).
Analgesics, proton pump inhibitors and antihypertensive drugs
A cross-sectional analysis of medical records of 13 274 elderly patients in four community hospitals in Thailand found that 79.0% (10486) of patients were prescribed one or more potentially inappropriate medications, using the Lists of Risk Drugs for Thai Elderly criteria, with antihypertensive drugs, proton pump inhibitors and analgesics being the most frequently prescribed potentially inappropriate medications.274 Another cross-sectional analysis of medical records of 6337 older adults in China found 79.4% (5033) prescribed one or more potentially inappropriate medications according to either Beers criteria® or STOPP, with antihypertensive, anti-anxiety and non-steroidal anti-inflammatory drugs among the most common potentially inappropriate medications.201
Drivers
Drivers and factors related to the overuse of medications in low- and middle-income countries were reported in 139 (37.9%) studies, with 74 studies reporting on individual-level (i.e. clinician or patient, e.g. knowledge and skills or preferences) and 40 on system-level drivers or factors (i.e. institutional or organization, e.g. resource allocation, staffing and national guidelines; Table 3). Only 10 of these studies were from low-income countries,20,77,111,127,129,144,166,183,262,337 and we did not observe clear associations between country income levels and drivers (Box 2), nor could we observe any geographical variations in the drivers.
Table 3. Studies included on the drivers, solutions and consequences of medication overuse in low- and middle-income countries.
| Study characteristic | Study reference | No. (%) of studies |
|---|---|---|
| Drivers | 15 , 18 , 20 , 27 – 30 , 32 , 36 , 40 , 43 , 44 , 47 , 48 , 52 – 54 , 60 , 63 , 68 , 69 , 71 , 77 , 79 , 82 , 86 , 88 – 92 , 96 , 99 , 102 , 104 , 105 , 111 , 113 , 115 , 118 , 119 , 121 , 127 , 129 , 130 , 132 , 135 – 139 , 144 , 151 , 153 , 155 , 156 , 159 , 162 , 164 – 166 , 173 – 175 , 183 , 190 , 193 , 194 , 196 , 198 , 199 , 204 , 206 , 208 , 210 , 213 , 216 – 218 , 221 , 222 , 226 , 228 , 229 , 234 , 235 , 238 , 239 , 244 , 246 , 247 , 250 – 252 , 260 , 262 , 275 , 277 , 278 , 283 , 284 , 286 , 291 , 292 , 295 , 297 , 300 , 302 – 304 , 307 , 309 , 310 , 312 , 317 , 319 , 321 , 322 , 326 , 327 , 332 , 333 , 337 – 340 , 342 , 346 , 350 , 352 , 354 , 357 , 358 , 362 , 364 , 366 , 368 , 371 , 379 | 139 (37.9)a |
| Individual-level factors | 27 , 29 , 40 , 43 , 47 , 48 , 53 , 60 , 63 , 69 , 71 , 77 , 79 , 82 , 86 , 88 – 90 , 92 , 96 , 99 , 102 , 104 , 105 , 118 , 119 , 121 , 127 , 130 , 136 – 139 , 144 , 151 , 153 , 155 , 156 , 159 , 165 , 166 , 173 – 175 , 190 , 193 , 196 , 208 , 210 , 213 , 229 , 238 , 247 , 250 , 251 , 260 , 283 , 286 , 291 , 300 , 302 – 304 , 310 , 312 , 332 , 337 , 339 , 354 , 357 , 358 , 366 , 371 , 379 | 74 (53.2) |
| Polypharmacy and/or multimorbidity | 27 , 40 , 60 , 63 , 77 , 79 , 86 , 88 – 90 , 92 , 96 , 102 , 104 , 105 , 130 , 136 – 139 , 159 , 165 , 174 , 196 , 208 , 213 , 229 , 250 , 286 , 291 , 300 , 303 , 304 , 310 , 337 , 354 , 358 , 379 | 38 (51.4) |
| Limited knowledge | 29 , 47 , 48 , 69 , 82 , 99 , 118 , 119 , 121 , 127 , 144 , 166 , 175 , 190 , 210 , 238 , 250 , 251 , 283 , 302 , 312 , 332 , 357 , 371 | 24 (32.4) |
| Patient demand | 43 , 47 , 48 , 53 , 71 , 193 , 210 , 247 , 260 , 339 , 366 , 371 | 12 (16.2) |
| System-level factors | 15 , 18 , 28 , 40 , 43 , 47 , 48 , 52 , 68 , 69 , 71 , 89 , 92 , 99 , 111 , 113 , 119 , 127 , 130 , 139 , 151 , 156 , 164 , 166 , 190 , 193 , 196 , 210 , 213 , 246 , 247 , 251 , 260 , 283 , 310 , 332 , 333 , 357 , 366 , 371 | 40 (28.8) |
| Constrained resources | 18 , 28 , 48 , 68 , 69 , 71 , 111 , 139 , 166 , 190 , 210 , 247 , 251 , 260 , 333 , 357 | 16 (40.0) |
| Financial factors | 15 , 47 , 48 , 119 , 164 , 166 , 193 , 210 , 247 , 251 , 283 , 366 , 371 | 13 (32.5) |
| Regulatory issues | 15 , 43 , 48 , 69 , 99 , 119 , 127 , 193 , 251 , 332 , 371 | 11 (27.5) |
| Other | 18 , 40 , 52 , 89 , 92 , 113 , 130 , 151 , 156 , 196 , 213 , 246 , 310 | 13 (32.5) |
| Consequences | 21 , 23 , 33 – 35 , 37 , 39 , 46 , 74 , 81 , 103 , 112 , 116 , 142 , 143 , 179 , 203 , 242 , 265 , 268 , 274 , 280 , 294 , 308 , 315 , 318 , 331 , 361 , 365 , 374 , 380 | 31 (8.4)a |
| Potential solutions | 17 , 25 , 43 , 48 , 55 , 64 , 66 , 98 , 99 , 106 , 114 , 117 , 141 , 147 , 170 , 176 , 186 , 189 , 193 , 200 , 201 , 205 , 209 , 215 , 231 , 236 , 240 , 249 , 274 , 276 , 299 , 305 , 313 , 329 , 335 , 341 , 347 , 356 , 359 , 363 , 378 , 381 | 42 (11.4)a |
| Study design | ||
| Interventional | 55 , 66 , 98 , 106 , 114 , 117 , 176 , 186 , 189 , 201 , 215 , 231 , 236 , 240 , 249 , 299 , 313 , 329 , 341 , 347 , 356 , 359 , 363 | 23 (54.8) |
| Observational | 17 , 25 , 43 , 48 , 64 , 99 , 141 , 147 , 170 , 193 , 200 , 205 , 209 , 274 , 276 , 305 , 335 , 378 , 381 | 19 (45.2) |
| Medicine focus | ||
| Antibiotics | 17 , 25 , 48 , 55 , 64 , 98 , 99 , 114 , 117 , 141 , 147 , 205 , 209 , 231 , 236 , 249 , 274 , 299 , 313 , 347 , 363 , 381 | 22 (52.4) |
| Others | 43 , 66 , 106 , 170 , 176 , 186 , 189 , 193 , 200 , 201 , 215 , 240 , 276 , 305 , 329 , 335 , 341 , 356 , 359 , 378 | 20 (47.6) |
a The denominator is all 367 studies included in the scoping review.
Individual-level drivers
Of the studies reporting on individual-level drivers, 24 studies cited limited knowledge among clinicians or patients on the harms of overuse, 12 studies pointed to perceived or actual patients’ demands, while polypharmacy and/or multimorbidity was found as a factor in 38 studies, largely studies of potentially inappropriate medications among elderly people (Table 3). For example, a study of 6400 hospitalized older patients in China found that 64.8% (4147) of prescriptions were inappropriate based on Beers criteria®, with proton pump inhibitors the most common potentially inappropriate medication, and polypharmacy was the most important factor associated with potentially inappropriate medications.162 In a qualitative study with clinicians and older adults in Burkina Faso, a low-income country, drivers of overuse included poor patient–clinician communication, limited clinician knowledge, and incentives from pharmaceutical companies.163
System-level drivers
Of the studies reporting on system-level drivers and factors, 11 studies cited regulatory issues such as poorly enforced regulations or policies; 16 studies cited constrained resources, including limited access to diagnostic facilities, and problematic access in rural or regional places; and 13 studies cited financial factors such as profitability of health-care providers and industry influence (Table 3). For example, a nationwide Malaysian study of 5810 antibiotic prescriptions in 545 clinics (129 public and 416 private clinics) found much higher proportions of antibiotic prescriptions (30.8%; 5055/16 415 vs 6.8%; 755/11 172), and antibiotic prescriptions for respiratory tract infections (16.7%; 49/293 vs 57.7%; 1479/2564) in private clinics versus public, most of which were considered unnecessary.15
Consequences
Consequences of overuse of medications were reported in 31 studies (8.4%), including just one from a low-income country (Table 3).21 The two most commonly identified consequences of overuse were harms – such as adverse drug reactions, impacts on quality of life or mortality – and costs. For example, a study among 125 heart-failure patients in Lebanon found a moderate correlation between potentially inappropriate medications and reduced quality of life,374 while another small study of 127 older adults in Brazil found no impact of potentially inappropriate medications on mortality, during a 10-year follow-up.111 In relation to costs, a study in the Islamic Republic of Iran estimated that almost 1 million United States dollars (US$) was wasted within a year in one teaching hospital on unnecessary antibiotics, measured as use not adherent to local guidelines.292 In 2020, a survey in Lebanon found widespread overuse of proton pump inhibitors and estimated that the nation may be wasting US$ 25 million annually as a result.170 No studies in low-income countries assessed costs of overuse.
Potential solutions
Evaluations of potential solutions were reported in 42 studies (11.4%), with 23 studies reporting on interventional rather than observational studies (Table 3). Only four studies of solutions were based in low-income countries231,249,329,335 (data repository).14
Twenty-two studies of solutions focused on antibiotics (Table 3). For example, a review identified multiple interventions that successfully reduced inappropriate antibiotics in low- and middle-income countries, including national action plans, educational campaigns, wider use of audit–feedback initiatives and regulatory or legal changes to reduce self-purchasing of antibiotics.145 Similarly, a large study of long-term antibiotic use in 55 low- and middle-income countries, using World Health Organization databases, found that having national policies and/or strategies on rational antibiotic use was associated with an estimated 20% reduction in antibiotic use for upper respiratory tract infections and an estimated 30% reduction in antibiotic use for acute diarrhoeal illness.167
For non-antibiotic overuse, 20 studies evaluated potential solutions, including educational interventions, deprescribing initiatives, new technologies and interventions involving pharmacists (Table 3). In Uganda, a low-income country, two cluster randomized controlled trials of 127 villages and 381 community health workers found dramatic reductions in the overuse of antimalarial drugs following the introduction of rapid diagnostic tests (48.5% absolute reduction: from 79.3%; 520/656; to 30.8%; 215/699).247,388 In Argentina, a multifaceted intervention including educational workshops, deprescribing algorithms and automated email alerts was found to successfully reduce inappropriate medications among 900 older adults (overall absolute reduction of 8.5% across eight classes of potentially inappropriate medications – relative reduction of 73% for non-steroidal anti-inflammatory drugs and 31% for benzodiazepines).303 Also in Argentina, an email-linked behavioural intervention underpinned by social-norm feedback reduced inappropriate prescriptions and cost for cognitively impaired older adults. Physicians in the intervention group made fewer inappropriate prescriptions than physicians in the control group, mean 93.25 prescriptions (95% CI: 89.27–97.24) versus 98.99 (95% CI: 95.00–102.98).341 In Thailand, a large study of 11 915 patients across four community hospitals found that computerized decision support systems that detect potentially inappropriate medications were associated with 13.3 percentage points decrease (from 87.7% to 74.4%) in potentially inappropriate medications.275
A 2021 Chinese study found that an intervention by clinical pharmacists halved the rate of inappropriate prescriptions of proton pump inhibitors (from 48.9 to 22.7 prescriptions per 100 patient-days), with no harmful impacts.378 Encouragingly, a 2018 survey in Ethiopia, a low-income country, assessing attitudes to deprescribing, found that 81.6% (258/316) of people asked were willing to stop one or more medications if possible and if agreed by their doctors.335
Discussion
We found widespread evidence of high proportions of overuse of medications in low- and middle-income countries. Classes of commonly overused medications included antibiotics, benzodiazepines, non-steroidal anti-inflammatory drugs, proton pump inhibitors and antihypertensive medicines. Drivers of overuse included a lack of knowledge of overuse among patients or clinicians, insufficient resources to access optimum care, polypharmacy, financial factors including the profit motive, and weak or poorly enforced regulations. Consequences were harms from adverse drug reactions and high costs of inappropriate use of scarce resources. While only a small number of studies evaluated potential solutions, we identified feasible and effective interventions, even for the lowest income settings, to tackle the problem of overuse.
Almost 90% of the included studies were published in the past 10 years, emphasizing the growing interest in understanding and addressing overuse of medications in low- and middle-income countries. We observed wide dispersions of the proportion of overuse of medications; this finding might be attributed to the differences in the population, settings, medications and methods used among included studies. Only a few studies evaluated the consequences, such as financial wasting. Wasting of resources is catastrophic for health-care systems in low- and middle-income countries that are already fragmented and fragile.389 Future research should not only estimate the extent of overuse of prescribed medications, but also estimate the extent and drivers of the overuse from nonprescription medications. Furthermore, studies should evaluate the potential physical, psychological and social consequences, both at individual and health-care system levels. Further research should also include improving the methods to evaluate the harms and consequences associated with overuse of medications.
The finding that only a tenth of studies evaluated potential solutions points to a gap in the literature and the need to intensify research evaluating innovative solutions to reduce overuse, while at the same time improving the rigor of the science assessing the extent and nature of the problem. Our review finds evidence from low- and middle-income countries of significant reductions in inappropriate medications, using for example multifaceted interventions or deprescribing initiatives, which suggests such interventions are practical as well as desirable. However, future studies replicating successful interventions from high-income countries need to include more robust evaluations of individual-level (e.g. educational interventions, audit and feedback, and clinical decision support system) and system-level solutions (e.g. changes in payment and incentives and changes in regulations and policies).390
We also found strong evidence of very high levels of overprescription of antibiotics across many low- and middle-income countries. Such overprescription is associated with antibiotic resistance,391 however, there are hopeful signs that those overprescription rates can be reduced with national policies and local initiatives.145,167 Research evaluating potential solutions for unnecessary prescription needs to focus on nonprescription antibiotic dispensing in drug shops and antibiotic prescriptions by private health-care providers. This research might include multicomponent interventions combining educational programmes to improve public awareness; engagement of pharmacists in patient education and consumer guideline development; audit and feedback; and more incisive regulations and policies to reduce inappropriate antibiotic use in low- and middle-income countries.392
Our finding that only 7% of studies were from low-income countries suggests that either the problem of overuse may not be so pressing in places where underuse is a clear priority for stakeholders, or that the problem of overuse is understudied.
Our review has limitations. To achieve the breadth required of a scoping review, we have necessarily included studies using a range of definitions and methods, from assessing adherence to guidelines for appropriate use, to the potentially inappropriate medications assessments using the Beers criteria®, STOPP and other criteria. While we broadly accepted the definitions used by authors of the studies, if our review team could find no evidence in the study of an explicit method to measure overuse, the study was excluded. Generally, definitions of inappropriate use equate to use when a medication is not clinically indicated, or the overuse of a medication which may bring more harm than benefit, but in some studies, use of the term inappropriate also included finer details relating to dosage, frequency or duration of use. A further limitation arises from our subjective categorization of system- versus individual-level drivers, where there may be clear overlap among these drivers. Another minor limitation arises from applying the World Bank income level list from 2021 to studies conducted over many previous years, however, the income level has not changed for most low- and middle-income countries.13
The findings of this review suggest the time has arrived to build a global community of researchers, clinicians, policy-makers and citizens who will share, build and improve the science of overuse in low- and middle-income countries. The global community should have a focus on scaling up effective solutions to reduce harm and save wasted resources. Initiatives to tackle overuse of medications in low- and middle-income countries are currently limited and of a particular focus – such as the Global Antimicrobial Resistance Partnership.393–395 This review’s broad findings confirm the need for global discussions to prioritize research and action agendas. Global initiatives which have largely arisen in high-income countries to tackle overuse, such as Right Care, Preventing Overdiagnosis and Choosing Wisely, will only be strengthened through developing links with, and learning from, colleagues in low- and middle-income countries.
Acknowledgements
EO is also affiliated with the Centre for Evidence-Based Health Care, Faculty of Medicine and Health Sciences, Stellenbosch University, Stellenbosch, South Africa.
The Overdiagnosis and Overuse of Healthcare Services in LMICs Network consists of Karen Born (University of Toronto, Toronto, Canada), Minna Johansson (Cochrane Sustainable Healthcare, Lund, Sweden), Luis Correia (Medical and Public Health School of Bahia, Bahia, Brazil), Bishal Gyawali (Queen's University Cancer Research Institute, Kingston, Canada), Sumanth Gandra (Washington University School of Medicine, St Louis, USA), Suzana Alves da Silva (Hcor Hospital, São Paulo, Brazil), Giorgia Sulis (McGill University, Montreal, Canada), Ashraf Nabhan (Ain Shams University, Cairo, Egypt), Verna Vanderpuye (Korle Bu Teaching Hospital, Accra, Ghana), Daniel Morgan (University of Maryland School of Medicine, Baltimore, USA), Deborah Korenstein (Memorial Sloan Kettering Cancer Center, New York, USA) and Eddy Lang (University of Calgary, Calgary, Canada).
Funding:
LA is supported by a research fellowship funded by the National Health and Medical Research Council (NHMRC) Investigator grant (grant no. 2008379). RM is supported by a research fellowship funded by NHMRC (grant no. 1124207) and is a chief investigator on a Centre for Research Excellence (grant no. 1104136).
Competing interests:
RM has helped organize Preventing Overdiagnosis conferences. All other authors declare no competing interests.
References
- 1.Brownlee S, Chalkidou K, Doust J, Elshaug AG, Glasziou P, Heath I, et al. Evidence for overuse of medical services around the world. Lancet. 2017. Jul 8;390(10090):156–68. 10.1016/S0140-6736(16)32585-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morgan DJ, Dhruva SS, Coon ER, Wright SM, Korenstein D. 2019 update on medical overuse: a review. JAMA Intern Med. 2019. Nov 1;179(11):1568–74. 10.1001/jamainternmed.2019.3842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tackling wasteful spending on health. Paris: Organisation for Economic Co-operation and Development Publishing; 2017. [Google Scholar]
- 4.Glasziou P, Straus S, Brownlee S, Trevena L, Dans L, Guyatt G, et al. Evidence for underuse of effective medical services around the world. Lancet. 2017. Jul 8;390(10090):169–77. 10.1016/S0140-6736(16)30946-1 [DOI] [PubMed] [Google Scholar]
- 5.Delivering quality health services: a global imperative for universal health coverage. Geneva: World Health Organization; 2018. Available from: https://apps.who.int/iris/handle/10665/272465 [cited 2022 Mar 8].
- 6.Rubagumya F, Mitera G, Ka S, Manirakiza A, Decuir P, Msadabwe SC, et al. Choosing wisely Africa: ten low-value or harmful practices that should be avoided in cancer care. JCO Glob Oncol. 2020. Jul;6(6):1192–9. 10.1200/GO.20.00255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pathirana T, Wang Yu M, Martiny F, Rupasinghe M, Kottahachchi D, Wijewickrama A, et al. 8 Drivers and potential solutions for overdiagnosis: perspectives from the low and middle income countries. BMJ Evid Based Med. 2019;24:A6–7. [Google Scholar]
- 8.Aromataris E, Munn Z. JBI manual for evidence synthesis. 2020. Available from: https://jbi-global-wiki.refined.site/space/MANUAL [cited 2022 Feb 22].
- 9.Clark J, Glasziou P, Del Mar C, Bannach-Brown A, Stehlik P, Scott AM. A full systematic review was completed in 2 weeks using automation tools: a case study. J Clin Epidemiol. 2020. May;121:81–90. 10.1016/j.jclinepi.2020.01.008 [DOI] [PubMed] [Google Scholar]
- 10.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018. Oct 2;169(7):467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 11.Albarqouni L, Arab-Zozani M, Scott A, Bakhit M, Pathirana T, Cardona M, et al. Overuse of medications in low- and middle- Income countries (LMICs): a protocol for a scoping review. Charlottesville: Center for Open Science; 2021. Available from: https://osf.io/tcgwm [cited 2022 Oct 19]. [Google Scholar]
- 12.The Cochrane Effective Practice and Organisation of Care. LMIC filter. London: The Cochrane Collaboration; 2020. Available from: https://epoc.cochrane.org/lmic-filters [cited 2022 Oct 19].
- 13.World Bank country and lending groups. Washington, DC: The World Bank; 2021. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups [cited 2021 May 27].
- 14.Albarqouni L, Palagama S, Chai J, Sivananthajothy P, Pathirana T, Moynihan R, et al. Overuse of medications in low- and middle-income countries (LMICs): a scoping review of the extent, drivers, consequences, and solutions [data repository]. Charlottesville: Center for Open Science; 2022. 10.17605/OSF.IO/72HYM [DOI] [Google Scholar]
- 15.Ab Rahman N, Teng CL, Sivasampu S. Antibiotic prescribing in public and private practice: a cross-sectional study in primary care clinics in Malaysia. BMC Infect Dis. 2016. May 17;16(1):208. 10.1186/s12879-016-1530-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abbassi A, Ben Cheikh Brahim A, Bokri E, Salem M, Ouahchi Z. [Inappropriate use of human albumin in a gastroenterology service of a university hospital: frequency and cost]. Pharm Hosp Clin. 2021;56(1):44–51. French. 10.1016/j.phclin.2020.09.004 [DOI] [Google Scholar]
- 17.Abdeljelil M, Aouam A, Kooli I, Marrakchi W, Toumi A, Chakroun M. Duration of antibiotic treatment in an infectious diseases department: comparison with guidelines. J Infect Public Health. 2020;13(2):337. 10.1016/j.jiph.2020.01.085 [DOI] [Google Scholar]
- 18.Abdo-Rabbo A. Household survey of treatment of malaria in Hajjah, Yemen. East Mediterr Health J. 2003. Jul;9(4):600–6. 10.26719/2003.9.4.600 [DOI] [PubMed] [Google Scholar]
- 19.Abdulah R, Insani WN, Destiani DP, Rohmaniasari N, Mohenathas ND, Barliana MI. Polypharmacy leads to increased prevalence of potentially inappropriate medication in the Indonesian geriatric population visiting primary care facilities. Ther Clin Risk Manag. 2018. Sep 4;14:1591–7. 10.2147/TCRM.S170475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abegaz TM, Birru EM, Mekonnen GB. Potentially inappropriate prescribing in Ethiopian geriatric patients hospitalized with cardiovascular disorders using START/STOPP criteria. PLoS One. 2018. May 3;13(5):e0195949. 10.1371/journal.pone.0195949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abera B, Kibret M, Mulu W. Knowledge and beliefs on antimicrobial resistance among physicians and nurses in hospitals in Amhara Region, Ethiopia. BMC Pharmacol Toxicol. 2014. May 19;15(1):26. 10.1186/2050-6511-15-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abrantes PdeM, Magalhães SM, Acúrcio Fde A, Sakurai E. [Quality assessment of antibiotic prescriptions dispensed at public health units in Belo Horizonte, Minas Gerais, Brazil, 2002]. Cad Saude Publica. 2007;23(1):95–104. Portuguese. 10.1590/S0102-311X2007000100011 [DOI] [PubMed] [Google Scholar]
- 23.Abroug F, Belghuith M, Nouira S, Bouchoucha S. [Antibiotic survey in a Tunisian hospital]. Med Mal Infect. 1990;20(12):595–9. French. 10.1016/S0399-077X(05)80348-8 [DOI] [Google Scholar]
- 24.Adedayo T, O’Mahony D, Adeleke O, Mabunda S. Doctors’ practice and attitudes towards red blood cell transfusion at Mthatha Regional Hospital, Eastern Cape, South Africa: a mixed methods study. Afr J Prim Health Care Fam Med. 2021. Jun 24;13(1):e1–8. 10.4102/phcfm.v13i1.2889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Adrizain R, Setiabudi D, Chairulfatah A. The inappropriate use of antibiotics in hospitalized dengue virus-infected children with presumed concurrent bacterial infection in teaching and private hospitals in Bandung, Indonesia. PLoS Negl Trop Dis. 2019. Jun 21;13(6):e0007438. 10.1371/journal.pntd.0007438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Afari-Asiedu S, Hulscher M, Abdulai MA, Boamah-Kaali E, Asante KP, Wertheim HFL. Every medicine is medicine; exploring inappropriate antibiotic use at the community level in rural Ghana. BMC Public Health. 2020. Jul 14;20(1):1103. 10.1186/s12889-020-09204-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Afari-Asiedu S, Oppong FB, Tostmann A, Ali Abdulai M, Boamah-Kaali E, Gyaase S, et al. Determinants of inappropriate antibiotics use in rural central Ghana using a mixed methods approach. Front Public Health. 2020. Mar 24;8:90. 10.3389/fpubh.2020.00090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Agarwal S, Yewale VN, Dharmapalan D. Antibiotics use and misuse in children: a knowledge, attitude and practice survey of parents in India. J Clin Diagn Res. 2015. Nov;9(11):SC21–4. 10.7860/JCDR/2015/14933.6819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ahmad A, Nor J, Abdullah AA, Tuan Kamauzaman TH, Yazid MB. Patient factors in inappropriate antibiotic prescribing for upper respiratory tract infection in the emergency department. Malays J Med Sci. 2021. Apr;28(2):72–83. 10.21315/mjms2021.28.2.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ahmed I, Rabbi MB, Sultana S. Antibiotic resistance in Bangladesh: a systematic review. Int J Infect Dis. 2019. Mar;80:54–61. 10.1016/j.ijid.2018.12.017 [DOI] [PubMed] [Google Scholar]
- 31.Akande-Sholabi W, Adebusoye LA, Olowookere OO. Potentially inappropriate medication use among older patients attending a geriatric centre in south-west Nigeria. Pharm Pract (Granada). 2018. Jul-Sep;16(3):1235. 10.18549/PharmPract.2018.03.1235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Akin S, Bölük C, Ozgur Y, Aladağ N, Geçmez G, Keskin O, et al. Overtreatment and hypoglycemia prevalence in geriatric patients with type-2 diabetes in the Turkish population. Acta Endocrinol (Bucur). 2019. Jul-Sep;15(3):311–16. 10.4183/aeb.2019.311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Akkawi ME, Nik Mohamed MH, Md Aris MA. Does inappropriate prescribing affect elderly patients’ quality of life? A study from a Malaysian tertiary hospital. Qual Life Res. 2019. Jul;28(7):1913–20. 10.1007/s11136-019-02153-5 [DOI] [PubMed] [Google Scholar]
- 34.Al Aqqad SM, Chen LL, Shafie AA, Hassali MA, Tangiisuran B. The use of potentially inappropriate medications and changes in quality of life among older nursing home residents. Clin Interv Aging. 2014. Jan 22;9:201–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Al-Azayzih A, Alamoori R, Altawalbeh SM. Potentially inappropriate medications prescribing according to Beers criteria among elderly outpatients in Jordan: a cross sectional study. Pharm Pract (Granada). 2019. Apr-Jun;17(2):1439. 10.18549/PharmPract.2019.2.1439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Al-Faham Z, Habboub G, Takriti F. The sale of antibiotics without prescription in pharmacies in Damascus, Syria. J Infect Dev Ctries. 2011. May 28;5(5):396–9. 10.3855/jidc.1248 [DOI] [PubMed] [Google Scholar]
- 37.Alexandre V Jr, Monteiro EA, Freitas-Lima P, Pinto KD, Velasco TR, Terra VC, et al. Addressing overtreatment in patients with refractory epilepsy at a tertiary referral centre in Brazil. Epileptic Disord. 2011. Mar;13(1):56–60. 10.1684/epd.2011.0411 [DOI] [PubMed] [Google Scholar]
- 38.Alkan A, Yaşar A, Karcı E, Köksoy EB, Ürün M, Şenler FC, et al. Severe drug interactions and potentially inappropriate medication usage in elderly cancer patients. Support Care Cancer. 2017. Jan;25(1):229–36. 10.1007/s00520-016-3409-6 [DOI] [PubMed] [Google Scholar]
- 39.Almeida TA, Reis EA, Pinto IVL, Ceccato MDGB, Silveira MR, Lima MG, et al. Factors associated with the use of potentially inappropriate medications by older adults in primary health care: an analysis comparing AGS Beers, EU(7)-PIM List, and Brazilian Consensus PIM criteria. Res Social Adm Pharm. 2019. Apr;15(4):370–7. 10.1016/j.sapharm.2018.06.002 [DOI] [PubMed] [Google Scholar]
- 40.Alqudah MA, Al-Azzam S, Alzoubi K, Alkhatatbeh M, Rawashdeh N. Overuse of proton pump inhibitors for stress ulcer prophylaxis in Jordan. Int J Clin Pharmacol Ther. 2016. Aug;54(8):597–602. 10.5414/CP202533 [DOI] [PubMed] [Google Scholar]
- 41.Alvarez PA, Castro V, Santini F, Soler C, Gutierrez R, Bril F, et al. Pharmacovigilance on hospital admission: medication lists and beyond. Drug Saf. 2011;34(10):959. [Google Scholar]
- 42.Amin MEK, Amine A, Newegy MS. Perspectives of pharmacy staff on dispensing subtherapeutic doses of antibiotics: a theory informed qualitative study. Int J Clin Pharm. 2017. Oct;39(5):1110–8. 10.1007/s11096-017-0510-y [DOI] [PubMed] [Google Scholar]
- 43.Amorim WW, Passos LC, Gama RS, Souza RM, Graia LT, Macedo JC, et al. Physician and patient-related factors associated with inappropriate prescribing to older patients within primary care: a cross-sectional study in Brazil. Sao Paulo Med J. 2021. Apr 5;139(2):107–16. 10.1590/1516-3180.2020.0411.r1.18112020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ansah EK, Narh-Bana S, Affran-Bonful H, Bart-Plange C, Cundill B, Gyapong M, et al. The impact of providing rapid diagnostic malaria tests on fever management in the private retail sector in Ghana: a cluster randomized trial. BMJ. 2015. Mar 4;350 mar04 8:h1019. 10.1136/bmj.h1019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Arab-Zozani M, Pezeshki MZ, Khodayari-Zarnaq R, Janati A. Balancing overuse and underuse in the Iranian healthcare system: a force field theory analysis. Ethiop J Health Sci. 2019. Mar;29(2):231–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Arabyat RM, Nusair MB, Al-Azzam SI, Alzoubi KH. Analysis of prevalence, risk factors, and potential costs of unnecessary drug therapy in patients with chronic diseases at the outpatient setting. Expert Rev Pharmacoecon Outcomes Res. 2020. Feb;20(1):125–32. 10.1080/14737167.2019.1612243 [DOI] [PubMed] [Google Scholar]
- 47.Asghar S, Atif M, Mushtaq I, Malik I, Hayat K, Babar Z-U-D. Factors associated with inappropriate dispensing of antibiotics among non-pharmacist pharmacy workers. Res Social Adm Pharm. 2020. Jun;16(6):805–11. 10.1016/j.sapharm.2019.09.003 [DOI] [PubMed] [Google Scholar]
- 48.Askarian M, Moravveji AR, Mirkhani H, Namazi S, Weed H. Adherence to American Society of Health-System Pharmacists surgical antibiotic prophylaxis guidelines in Iran. Infect Control Hosp Epidemiol. 2006. Aug;27(8):876–8. 10.1086/506405 [DOI] [PubMed] [Google Scholar]
- 49.Aswapokee N, Vaithayapichet S, Komoltri C. The failure of a preprinted order form to alter physicians’ antimicrobial prescribing pattern. J Med Assoc Thai. 1992. Apr;75(4):223–30. [PubMed] [Google Scholar]
- 50.Atif M, Asghar S, Mushtaq I, Malik I, Amin A, Babar ZU, et al. What drives inappropriate use of antibiotics? A mixed methods study from Bahawalpur, Pakistan. Infect Drug Resist. 2019. Mar 26;12:687–99. 10.2147/IDR.S189114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Auta A, Hadi MA, Oga E, Adewuyi EO, Abdu-Aguye SN, Adeloye D, et al. Global access to antibiotics without prescription in community pharmacies: a systematic review and meta-analysis. J Infect. 2019. Jan;78(1):8–18. 10.1016/j.jinf.2018.07.001 [DOI] [PubMed] [Google Scholar]
- 52.Ay P, Akici A, Harmanc H. Drug utilization and potentially inappropriate drug use in elderly residents of a community in Istanbul, Turkey. Int J Clin Pharmacol Ther. 2005. Apr;43(4):195–202. 10.5414/CPP43000 [DOI] [PubMed] [Google Scholar]
- 53.Ayieko P, Ntoburi S, Wagai J, Opondo C, Opiyo N, Migiro S, et al. A multifaceted intervention to implement guidelines and improve admission paediatric care in Kenyan district hospitals: a cluster randomised trial. PLoS Med. 2011. Apr;8(4):e1001018. 10.1371/journal.pmed.1001018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ayuthya SK, Matangkasombut OP, Sirinavin S, Malathum K, Sathapatayavongs B. Utilization of restricted antibiotics in a university hospital in Thailand. Southeast Asian J Trop Med Public Health. 2003. Mar;34(1):179–86. [PubMed] [Google Scholar]
- 55.Azmy MT, Loganathan M, Hassan Y, Muhammad NA, Lee C, Rosman A. Inappropriate prescribing defined by START and STOPP criteria and association with adverse drug events in elderly hospitalized patients. Pharmacoepidemiol Drug Saf. 2014;23:234.24741695 [Google Scholar]
- 56.Azoulay L, Zargarzadeh A, Salahshouri Z, Oraichi D, Bérard A. Inappropriate medication prescribing in community-dwelling elderly people living in Iran. Eur J Clin Pharmacol. 2005. Dec;61(12):913–9. 10.1007/s00228-005-0036-4 [DOI] [PubMed] [Google Scholar]
- 57.Bagger K, Nielsen AB, Siersma V, Bjerrum L. Inappropriate antibiotic prescribing and demand for antibiotics in patients with upper respiratory tract infections is hardly different in female versus male patients as seen in primary care. Eur J Gen Pract. 2015. Jun;21(2):118–23. 10.3109/13814788.2014.1001361 [DOI] [PubMed] [Google Scholar]
- 58.Bahat G, Bay I, Tufan A, Tufan F, Kilic C, Karan MA. Prevalence of potentially inappropriate prescribing among older adults: a comparison of the Beers 2012 and Screening Tool of Older Person’s Prescriptions criteria version 2. Geriatr Gerontol Int. 2017. Sep;17(9):1245–51. 10.1111/ggi.12850 [DOI] [PubMed] [Google Scholar]
- 59.Bahat G, Ilhan B, Bay I, Kilic C, Kucukdagli P, Oren MM, et al. Explicit versus implicit evaluation to detect inappropriate medication use in geriatric outpatients. Aging Male. 2020. Sep;23(3):179–84. 10.1080/13685538.2018.1464552 [DOI] [PubMed] [Google Scholar]
- 60.Bahat G, Ilhan B, Erdogan T, Halil M, Savas S, Ulger Z, et al. Turkish inappropriate medication use in the elderly (TIME) criteria to improve prescribing in older adults: TIME-to-STOP/TIME-to-START. Eur Geriatr Med. 2020. Jun;11(3):491–8. 10.1007/s41999-020-00297-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Baig MT, Sial AA, Huma A, Ahmed M, Shahid U, Syed N. Irrational antibiotic prescribing practice among children in critical care of tertiary hospitals. Pak J Pharm Sci. 2017. Jul;30(4(Suppl.)):1483–9. [PubMed] [Google Scholar]
- 62.Balci MA, Oksuz MF, Donmez S, Ozen T, Dalkilic E, Tufan AN, et al. Comparison of adherence to disease modifying antirheumatic drugs in psoriatic arthritis and other rheumatic disease. Arthritis Rheumatol. 2016;68:2169–71. [Google Scholar]
- 63.Baldoni AO, Ayres LR, Martinez EZ, Dewulf NL, Dos Santos V, Pereira LR. Factors associated with potentially inappropriate medications use by the elderly according to Beers criteria 2003 and 2012. Int J Clin Pharm. 2014. Apr;36(2):316–24. 10.1007/s11096-013-9880-y [DOI] [PubMed] [Google Scholar]
- 64.Ban B, Hodgins S, Thapa P, Thapa S, Joshi D, Dhungana A, et al. A national survey of private-sector outpatient care of sick infants and young children in Nepal. BMC Health Serv Res. 2020. Jun 16;20(1):545. 10.1186/s12913-020-05393-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bao L, Peng R, Wang Y, Ma R, Ren X, Meng W, et al. Significant reduction of antibiotic consumption and patients’ costs after an action plan in China, 2010-2014. PLoS One. 2015. Mar 13;10(3):e0118868. 10.1371/journal.pone.0118868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bao Z, Ji C, Hu J, Luo C, Fang W. Clinical and economic impact of pharmacist interventions on sampled outpatient prescriptions in a Chinese teaching hospital. BMC Health Serv Res. 2018. Jul 4;18(1):519. 10.1186/s12913-018-3306-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Baribwira C, Kalambay K, Niyuhire F, Solofo R. [Burundi: knowledge and practices of physicians and nursing personnel about acute respiratory infections in children]. Med Trop (Mars). 1996;56(1):95–8. [French. ] [PubMed] [Google Scholar]
- 68.Barker AK, Brown K, Ahsan M, Sengupta S, Safdar N. What drives inappropriate antibiotic dispensing? A mixed-methods study of pharmacy employee perspectives in Haryana, India. BMJ Open. 2017. Mar 2;7(3):e013190. 10.1136/bmjopen-2016-013190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Barker AK, Brown K, Ahsan M, Sengupta S, Safdar N. Social determinants of antibiotic misuse: a qualitative study of community members in Haryana, India. BMC Public Health. 2017. Apr 19;17(1):333. 10.1186/s12889-017-4261-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Başaran Ö, Dogan V, Beton O, Tekinalp M, Aykan AC, Kalaycioğlu E, et al. ; and Collaborators. Suboptimal use of non-vitamin K antagonist oral anticoagulants: results from the RAMSES study. Medicine (Baltimore). 2016. Aug;95(35):e4672. 10.1097/MD.0000000000004672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Başaran Ö, Dogan V, Biteker M, Karadeniz FÖ, Tekkesin Aİ, Çakıllı Y, et al. ; Collaborators. Guideline-adherent therapy for stroke prevention in atrial fibrillation in different health care settings: results from RAMSES study. Eur J Intern Med. 2017. May;40:50–5. 10.1016/j.ejim.2017.02.011 [DOI] [PubMed] [Google Scholar]
- 72.Basu S, Chatterjee M, Chandra PK, Basu S. Antibiotic misuse in children by the primary care physicians–an Indian experience. Niger J Clin Pract. 2008. Mar;11(1):52–7. [PubMed] [Google Scholar]
- 73.Belachew SA, Hall L, Selvey LA. Non-prescription dispensing of antibiotic agents among community drug retail outlets in Sub-Saharan African countries: a systematic review and meta-analysis. Antimicrob Resist Infect Control. 2021. Jan 14;10(1):13. 10.1186/s13756-020-00880-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ben Cheikh Brahim A, Abbassi A, Khaireddine R, Bokri E, Dridi H, Ouahchi Z. Inappropriate use of human albumin in a teaching hospital. Eur J Hosp Pharm. 2020;27 Suppl 1:A54–5. Available from: https://ejhp.bmj.com/content/ejhpharm/27/Suppl_1/A54.2.full.pdf [cited 2022 Oct 19]. [Google Scholar]
- 75.Berhe YH, Amaha ND, Ghebrenegus AS. Evaluation of ceftriaxone use in the medical ward of Halibet National Referral and teaching hospital in 2017 in Asmara, Eritrea: a cross sectional retrospective study. BMC Infect Dis. 2019. May 24;19(1):465. 10.1186/s12879-019-4087-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bester BH, Sobuwa S. Utilisation of prehospital intravenous access. S Afr Med J. 2014. Jul 22;104(9):615–18. 10.7196/SAMJ.7969 [DOI] [PubMed] [Google Scholar]
- 77.Bhagavathula AS, Seid MA, Adane A, Gebreyohannes EA, Brkic J, Fialová D. Prevalence and determinants of multimorbidity, polypharmacy, and potentially inappropriate medication use in the older outpatients: findings from EuroAgeism H2020 ESR7 project in Ethiopia. Pharmaceuticals (Basel). 2021. Aug 25;14(9):844. 10.3390/ph14090844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bhagavathula AS, Vidyasagar K, Chhabra M, Rashid M, Sharma R, Bandari DK, et al. Prevalence of polypharmacy, hyperpolypharmacy and potentially inappropriate medication use in older adults in India: a systematic review and meta-analysis. Front Pharmacol. 2021. May 19;12:685518. 10.3389/fphar.2021.685518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bhatt AN, Paul SS, Krishnamoorthy S, Baby BT, Mathew A, Nair BR. Potentially inappropriate medications prescribed for older persons: a study from two teaching hospitals in southern India. J Family Community Med. 2019. Sep-Dec;26(3):187–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bilge U, Yavuz E, Culhaci A, Keskin A, Korkut Y, Alacali M, et al. Inappropriate use of aspirin and its concomitant use with nonsteroidal antiinflammatory drugs. Acta Med Mediter. 2015;31(3):621–5. Available from: https://www.actamedicamediterranea.com/archive/2015/medica-3/inappropriate-use-of-aspirin-and-its-concomitant-use-with-nonsteroidalantiinflammatory-drugs/document [cited 2022 Oct 19]. [Google Scholar]
- 81.Bin YB, Rozina A, Junaid M, Saima K, Farhan N, Maham T. A study of unnecessary use of antibiotics at a tertiary care hospital: urgent need to implement antimicrobial stewardship programs. J Young Pharm. 2015;7(4):311–9. Available from: https://cdn.emanuscript.tech/jyp/v7/i4/JYoungPharm-7-4-311.pdf [cited 2022 Oct 19]. [Google Scholar]
- 82.Bischoff LM, Faraco LSM, Machado LV, Bialecki AVS, Almeida GM, Becker SCC. Inappropriate usage of intravenous proton pump inhibitors and associated factors in a high complexity hospital in Brazil. Arq Gastroenterol. 2021. Jan-Mar;58(1):32–8. 10.1590/s0004-2803.202100000-07 [DOI] [PubMed] [Google Scholar]
- 83.Bostan H, Sencar ME, Calapkulu M, Hepsen S, Duger H, Ozturk Unsal I, et al. Two important issues in subacute thyroiditis management: delayed diagnosis and inappropriate use of antibiotics. Eur Thyroid J. 2021. Jul;10(4):323–9. 10.1159/000513745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bray TJ, Salil P, Weiss HA, Porter JD. Transfusion medicine in India: a survey of current practice. Transfus Med. 2003. Feb;13(1):17–23. 10.1046/j.1365-3148.2003.00417.x [DOI] [PubMed] [Google Scholar]
- 85.Brkic J, Fialova D, Reissigova J, Apostoli P, Bobrova V, Capiau A, et al. Potentially inappropriate medication use in older patients in 8 central and eastern Europe countries participating in the Horizon 2020 EUROAGEISM project: a narrative literature review. Int J Clin Pharm. 2020;42(1):233–4. 10.1007/s11096-019-00945-w [DOI] [Google Scholar]
- 86.Buendía JA, Patiño DG. Costs of respiratory syncytial virus hospitalizations in Colombia. Pharmacoeconom Open. 2021. Mar;5(1):71–6. 10.1007/s41669-020-00218-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Buendía JA, Rodríguez CA. A predictive model of inappropriate use of medical tests and medications in bronchiolitis. Pan Afr Med J. 2020. Sep 25;37:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bulatova N, Elayeh E, Abdullah S, Halaseh L, Abuloha S, Raqeeq MA, et al. Assessment of inappropriate medication use in Jordanian elderly hospitalized patients using 2015 Beers criteria. Turk Geriatri Derg. 2019;22(3):258–68. 10.31086/tjgeri.2019.101 [DOI] [Google Scholar]
- 89.Bustamante Robles KY, Ticse Aguirre R, Cánepa Rondo IF, Costta Herrera CG, Vasquez Kunze S, Soto Arquiñigo L, et al. [Frequency of proton pump inhibitor prescription based in clinical practice guidelines in hospitalized patients in two academic hospitals in Lima, Peru]. Rev Gastroenterol Peru. 2012. Jan-Mar;32(1):44–9. Spanish. [PubMed] [Google Scholar]
- 90.Camcioglu Y, Sener Okur D, Aksaray N, Darendeliler F, Hasanoglu E. Factors affecting physicians’ perception of the overuse of antibiotics. Med Mal Infect. 2020. Nov;50(8):652–7. 10.1016/j.medmal.2020.01.006 [DOI] [PubMed] [Google Scholar]
- 91.Cassoni TC, Corona LP, Romano-Lieber NS, Secoli SR, Duarte YA, Lebrão ML. [Use of potentially inappropriate medication by the elderly in São Paulo, Brazil: SABE Study]. Cad Saude Publica. 2014. Aug;30(8):1708–20. Portuguese. 10.1590/0102-311X00055613 [DOI] [PubMed] [Google Scholar]
- 92.Castelino RL, Sathvik BS, Parthasarathi G, Gurudev KC, Shetty MS, Narahari MG. Prevalence of medication-related problems among patients with renal compromise in an Indian hospital. J Clin Pharm Ther. 2011. Aug;36(4):481–7. 10.1111/j.1365-2710.2011.01266.x [DOI] [PubMed] [Google Scholar]
- 93.Çelik F, Aypak C, Özdemir A, Görpelioğlu S. Inappropriate prescribing of proton pump inhibitors in outpatient clinics. Gastroenterol Nurs. 2021. Mar-Apr 01;44(2):84–91. 10.1097/SGA.0000000000000500 [DOI] [PubMed] [Google Scholar]
- 94.Ceyhan M, Yildirim I, Ecevit C, Aydogan A, Ornek A, Salman N, et al. Inappropriate antimicrobial use in Turkish pediatric hospitals: a multicenter point prevalence survey. Int J Infect Dis. 2010. Jan;14(1):e55–61. 10.1016/j.ijid.2009.03.013 [DOI] [PubMed] [Google Scholar]
- 95.Chahine B. Potentially inappropriate medications prescribing to elderly patients with advanced chronic kidney by using 2019 American Geriatrics Society Beers criteria. Health Sci Rep. 2020. Dec 7;3(4):e214. 10.1002/hsr2.214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Chang Y, Chusri S, Sangthong R, McNeil E, Hu J, Du W, et al. Clinical pattern of antibiotic overuse and misuse in primary healthcare hospitals in the southwest of China. PLoS One. 2019. Jun 26;14(6):e0214779. 10.1371/journal.pone.0214779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chang Y, Sangthong R, McNeil EB, Tang L, Chongsuvivatwong V. Effect of a computer network-based feedback program on antibiotic prescription rates of primary care physicians: a cluster randomized crossover-controlled trial. J Infect Public Health. 2020. Sep;13(9):1297–303. 10.1016/j.jiph.2020.05.027 [DOI] [PubMed] [Google Scholar]
- 98.Chatterjee D, Sen S, Begum SA, Adhikari A, Hazra A, Das AK. A questionnaire-based survey to ascertain the views of clinicians regarding rational use of antibiotics in teaching hospitals of Kolkata. Indian J Pharmacol. 2015. Jan-Feb;47(1):105–8. 10.4103/0253-7613.150373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chen J, Wang Y, Chen X, Hesketh T. Widespread illegal sales of antibiotics in Chinese pharmacies - a nationwide cross-sectional study. Antimicrob Resist Infect Control. 2020. Jan 15;9(1):12. 10.1186/s13756-019-0655-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Chen L, Zhou F, Li H, Xing X, Han X, Wang Y, et al. ; CAP-China network. Disease characteristics and management of hospitalised adolescents and adults with community-acquired pneumonia in China: a retrospective multicentre survey. BMJ Open. 2018. Feb 15;8(2):e018709. 10.1136/bmjopen-2017-018709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chen LL, Tangiisuran B, Shafie AA, Hassali MA. Evaluation of potentially inappropriate medications among older residents of Malaysian nursing homes. Int J Clin Pharm. 2012. Aug;34(4):596–603. 10.1007/s11096-012-9651-1 [DOI] [PubMed] [Google Scholar]
- 102.Chen M, Wang L, Chen W, Zhang L, Jiang H, Mao W. Does economic incentive matter for rational use of medicine? China’s experience from the essential medicines program. Pharmacoeconomics. 2014. Mar;32(3):245–55. 10.1007/s40273-013-0068-z [DOI] [PubMed] [Google Scholar]
- 103.Chiapella LC, Menna JM, Mamprin ME. Potentially inappropriate medications in elderly ambulatory patients: a comparative study between a primary health care center and a community pharmacy. Value Health Reg Issues. 2018. Dec;17:119–25. 10.1016/j.vhri.2017.12.009 [DOI] [PubMed] [Google Scholar]
- 104.Chiapella LC, Montemarani Menna J, Marzi M, Mamprin ME. Prevalence of potentially inappropriate medications in older adults in Argentina using Beers criteria and the IFAsPIAM List. Int J Clin Pharm. 2019. Aug;41(4):913–9. 10.1007/s11096-019-00858-8 [DOI] [PubMed] [Google Scholar]
- 105.Chivapricha W, Srinonprasert V, Suansanae T. Impact of geriatric pharmacy specialist interventions to reduce potentially inappropriate medication among hospitalized elderly patients at medical wards: a prospective quasi-experimental study. Drugs Real World Outcomes. 2021. Mar;8(1):39–47. 10.1007/s40801-020-00214-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Cuba Fuentes MS, Zegarra Zamalloa CO, Reichert S, Gill D. Attitudes, perceptions and awareness concerning quaternary prevention among family doctors working in the social security system, Peru: a cross-sectional descriptive study. Medwave. 2016. Apr 27;16(3):e6433. 10.5867/medwave.2016.03.6433 [DOI] [PubMed] [Google Scholar]
- 107.Cvetković Z, Perić A, Dobrić S. Potentially inappropriate prescribing and potential clinically significant drug-drug interactions in older outpatients: is there any association? Medicina (Kaunas). 2019. Jul 3;55(7):332. 10.3390/medicina55070332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.da Costa IHF, Silva RME, Carlos JO, Silva MCA, Pinheiro MKC, Martins BCC, et al. Potentially inappropriate medications in older kidney transplant recipients: a Brazilian prevalence study. Int J Clin Pharm. 2019. Aug;41(4):888–94. 10.1007/s11096-019-00842-2 [DOI] [PubMed] [Google Scholar]
- 109.da Cunha AJ, Amaral J, e Silva MA. Inappropriate antibiotic prescription to children with acute respiratory infection in Brazil. Indian Pediatr. 2003. Jan;40(1):7–12. [PubMed] [Google Scholar]
- 110.Dache A, Dona A, Ejeso A. Inappropriate use of antibiotics, its reasons and contributing factors among communities of Yirgalem town, Sidama regional state, Ethiopia: a cross-sectional study. SAGE Open Med. 2021. Sep 3;9:20503121211042461. 10.1177/20503121211042461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.de Araújo NC, Silveira EA, Mota BG, Neves Mota JP, de Camargo Silva AEB, Alves Guimarães R, et al. Potentially inappropriate medications for the elderly: incidence and impact on mortality in a cohort ten-year follow-up. PLoS One. 2020. Oct 28;15(10):e0240104. 10.1371/journal.pone.0240104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.de Castro MS, Kopittke L, Fuchs FD, Tannhauser M. Evidence of inappropriate use of vancomycin in a university affiliated hospital in Brazil. Pharmacoepidemiol Drug Saf. 1999. Oct;8(6):405–11. [DOI] [PubMed] [Google Scholar]
- 113.Dehn Lunn A. Reducing inappropriate antibiotic prescribing in upper respiratory tract infection in a primary care setting in Kolkata, India. BMJ Open Qual. 2018. Nov 20;7(4):e000217. 10.1136/bmjoq-2017-000217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.do Nascimento MM, Mambrini JV, Lima-Costa MF, Firmo JO, Peixoto SW, de Loyola Filho AI. Potentially inappropriate medications: predictor for mortality in a cohort of community-dwelling older adults. Eur J Clin Pharmacol. 2017. May;73(5):615–21. 10.1007/s00228-017-2202-x [DOI] [PubMed] [Google Scholar]
- 115.Do NT, Ta NT, Tran NT, Than HM, Vu BT, Hoang LB, et al. Point-of-care C-reactive protein testing to reduce inappropriate use of antibiotics for non-severe acute respiratory infections in Vietnamese primary health care: a randomised controlled trial. Lancet Glob Health. 2016. Sep;4(9):e633–41. 10.1016/S2214-109X(16)30142-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Donertas B, Gelal A, Alkan A, Mollahaliloglu S, Akici A. Pattern of parenteral drug prescription for children under the age of 6 in Turkey. Clin Ther. 2013;35(8):e91. 10.1016/j.clinthera.2013.07.270 [DOI] [Google Scholar]
- 117.Donsamak S, Weiss MC, John DN. PNS110 barriers to compliance with antibiotic treatment guidelines in community pharmacies in Thailand. Value Health. 2020;23:S304. 10.1016/j.jval.2020.04.1113 [DOI] [Google Scholar]
- 118.Donsamak S, Weiss MC, John DN. Exploring the use of antibiotics by Thai citizens supplied from community pharmacies in Thailand. Int J Pharm Pract. 2020;28:(52 Suppl 1). [Google Scholar]
- 119.Doubova SV, Perez-Cuevas R, Balandrán-Duarte DA, Rendón-Macías ME. Quality of care for children with upper respiratory infections at Mexican family medicine clinics. Bol Méd Hosp Infant México. 2015. Jul - Aug;72(4):235–41. 10.1016/j.bmhimx.2015.07.003 [DOI] [PubMed] [Google Scholar]
- 120.Duan L, Liu C, Wang D. The general population’s inappropriate behaviors and misunderstanding of antibiotic use in China: a systematic review and meta-analysis. Antibiotics (Basel). 2021. Apr 26;10(5):497. 10.3390/antibiotics10050497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Efunshile AM, Ezeanosike O, Nwangwu CC, König B, Jokelainen P, Robertson LJ. Apparent overuse of antibiotics in the management of watery diarrhoea in children in Abakaliki, Nigeria. BMC Infect Dis. 2019. Mar 21;19(1):275. 10.1186/s12879-019-3899-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.El Khoury G, Ramia E, Salameh P. Misconceptions and malpractices toward antibiotic use in childhood upper respiratory tract infections among a cohort of Lebanese parents. Eval Health Prof. 2018. Dec;41(4):493–511. 10.1177/0163278716686809 [DOI] [PubMed] [Google Scholar]
- 123.El-Khoury M, Banke K, Sloane P. Improved childhood diarrhea treatment practices in Ghana: a pre-post evaluation of a comprehensive private-sector program. Glob Health Sci Pract. 2016. Jun 27;4(2):264–75. 10.9745/GHSP-D-16-00021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Erdeniz EH, Dursun A. Evaluation of inappropriate antibiotic use in pediatric patients: point-prevalence study. Çocuk Enfeks Derg. 2020;14(2):e63–8. 10.5578/ced.202024 [DOI] [Google Scholar]
- 125.Ergül AB, Gökçek İ, Çelik T, Torun YA. Assessment of inappropriate antibiotic use in pediatric patients: point-prevalence study. Turk Pediatri Ars. 2018. Mar 1;53(1):17–23. 10.5152/TurkPediatriArs.2018.5644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Erku DA, Mekuria AB, Belachew SA. Inappropriate use of antibiotics among communities of Gondar town, Ethiopia: a threat to the development of antimicrobial resistance. Antimicrob Resist Infect Control. 2017. Nov 7;6(1):112. 10.1186/s13756-017-0272-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Evirgen O, Onlen Y, Ertan O. The intensity of antibiotic usage in the university hospital and the investigation of an inappropriate use of antibiotics. Bratisl Lek Listy. 2011;112(10):595–8. [PubMed] [Google Scholar]
- 128.Ewing AC, Davis NL, Kayira D, Hosseinipour MC, van der Horst C, Jamieson DJ, et al. ; Breastfeeding, Antiretrovirals and Nutrition study team. Prescription of antibacterial drugs for HIV-exposed, uninfected infants, Malawi, 2004-2010. Emerg Infect Dis. 2019. Jan;25(1):103–12. 10.3201/eid2501.180782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Fadare JO, Agboola SM, Opeke OA, Alabi RA. Prescription pattern and prevalence of potentially inappropriate medications among elderly patients in a Nigerian rural tertiary hospital. Ther Clin Risk Manag. 2013;9:115–20. 10.2147/TCRM.S40120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Fadare JO, Desalu OO, Obimakinde AM, Adeoti AO, Agboola SM, Aina FO. Prevalence of inappropriate medication prescription in the elderly in Nigeria: a comparison of Beers and STOPP criteria. Int J Risk Saf Med. 2015;27(4):177–89. 10.3233/JRS-150660 [DOI] [PubMed] [Google Scholar]
- 131.Fajreldines AV, Insua JT, Schnitzler E. [Inappropriate prescription in elderly inpatients]. Medicina (B Aires). 2016;76(6):362–8. Spanish. [PubMed] [Google Scholar]
- 132.Fareed G, Abid S. Inappropriate use of proton pump inhibitors, time to reconsider indications before it will cause more harm than benefits. Turk J Gastroenterol. 2019;30:S706–7. [Google Scholar]
- 133.Farley E, Stewart A, Davies MA, Govind M, Van den Bergh D, Boyles TH. Antibiotic use and resistance: knowledge, attitudes and perceptions among primary care prescribers in South Africa. S Afr Med J. 2018. Aug 28;108(9):763–71. 10.7196/SAMJ.2018.v108i9.12933 [DOI] [PubMed] [Google Scholar]
- 134.Faustino CG, Martins MA, Jacob Filho W. Potentially inappropriate medication prescribed to elderly outpatients at a general medicine unit. Einstein (Sao Paulo). 2011. Mar;9(1):18–23. 10.1590/s1679-45082011ao1844 [DOI] [PubMed] [Google Scholar]
- 135.Faustino CG, Passarelli MC, Jacob-Filho W. Potentially inappropriate medications among elderly Brazilian outpatients. Sao Paulo Med J. 2013;131(1):19–26. 10.1590/S1516-31802013000100004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ferreira TR, Lopes LC, Motter FR, de Cássia Bergamaschi C. Potentially inappropriate prescriptions to Brazilian older people with Alzheimer disease: a cross-sectional study. Medicine (Baltimore). 2021. Mar 26;100(12):e25015. 10.1097/MD.0000000000025015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Fialova D, Tasic L, Skowron A, Soos G, Vlček J, Doro P, et al. Eastern and central European perspectives in potentially inappropriate medication use and polypharmacy in older patients (EU COST initiative IS 1402). Int J Clin Pharm. 2016;38(6):478. [Google Scholar]
- 138.Find NL, Terlizzi R, Munksgaard SB, Bendtsen L, Tassorelli C, Nappi G, et al. ; COMOESTAS Consortium. Medication overuse headache in Europe and Latin America: general demographic and clinical characteristics, referral pathways and national distribution of painkillers in a descriptive, multinational, multicenter study. J Headache Pain. 2015;17(1):20. 10.1186/s10194-016-0612-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Flores TG, Costa GS, Oliveira R, Pedro FL, Cruz IBMd, Lampert MA. Prescription of antimicrobials for hospitalized elderly: benefit analysis and association with implementation of therapeutic effort limitation and palliative care. Rev Epidemiol control infec. 2019;9(4):292–8. 10.17058/.v9i4.13006 [DOI] [Google Scholar]
- 140.Fulone I, Lopes LC. Potentially inappropriate prescriptions for elderly people taking antidepressant: comparative tools. BMC Geriatr. 2017. Dec 2;17(1):278. 10.1186/s12877-017-0674-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Galli TB, Reis WC, Andrzejevski VM. Potentially inappropriate prescribing and the risk of adverse drug reactions in critically ill older adults. Pharm Pract (Granada). 2016. Oct-Dec;14(4):818. 10.18549/PharmPract.2016.04.818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Gebeyehu E, Bantie L, Azage M. Inappropriate use of antibiotics and its associated factors among urban and rural communities of Bahir Dar City administration, northwest Ethiopia. PLoS One. 2015. Sep 17;10(9):e0138179. 10.1371/journal.pone.0138179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.George R, Thomas K, Thyagarajan SP, Jeyaseelan L, Peedicayil A, Jeyaseelan V; STD Study Group. Genital syndromes and syndromic management of vaginal discharge in a community setting. Int J STD AIDS. 2004. Jun;15(6):367–70. 10.1258/095646204774195191 [DOI] [PubMed] [Google Scholar]
- 144.Getachew H, Bhagavathula AS, Abebe TB, Belachew SA. Inappropriate prescribing of antithrombotic therapy in Ethiopian elderly population using updated 2015 STOPP/START criteria: a cross-sectional study. Clin Interv Aging. 2016. Jun 20;11:819–27. 10.2147/CIA.S107394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Godman B, Haque M, McKimm J, Abu Bakar M, Sneddon J, Wale J, et al. Ongoing strategies to improve the management of upper respiratory tract infections and reduce inappropriate antibiotic use particularly among lower and middle-income countries: findings and implications for the future. Curr Med Res Opin. 2020. Feb;36(2):301–27. 10.1080/03007995.2019.1700947 [DOI] [PubMed] [Google Scholar]
- 146.Gong Y, Jiang N, Chen Z, Wang J, Zhang J, Feng J, et al. Over-the-counter antibiotic sales in community and online pharmacies, China. Bull World Health Organ. 2020. Jul 1;98(7):449–57. 10.2471/BLT.19.242370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Grintsova O, Moroz V. Inappropriate medication in elderly patients in the university clinic. Int J Clin Pharm. 2019;41(2):608. [Google Scholar]
- 148.Guan X, Ni B, Zhang J, Man C, Cai Z, Meng W, et al. The impact of physicians’ working hours on inappropriate use of outpatient medicine in a tertiary hospital in China. Appl Health Econ Health Policy. 2020. Jun;18(3):443–51. 10.1007/s40258-019-00544-w [DOI] [PubMed] [Google Scholar]
- 149.Gunen H, Yilmaz M, Aktas O, Ergun P, Ortakoylu MG, Demir A, et al. Categorization of COPD patients in Turkey via GOLD 2013 strategy document: ALPHABET study. Int J Chron Obstruct Pulmon Dis. 2015. Nov 13;10:2485–94. 10.2147/COPD.S87464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Haddadin RN, Alsous M, Wazaify M, Tahaineh L. Evaluation of antibiotic dispensing practice in community pharmacies in Jordan: a cross sectional study. PLoS One. 2019. Apr 29;14(4):e0216115. 10.1371/journal.pone.0216115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Han X, Zhou F, Li H, Xing X, Chen L, Wang Y, et al. ; CAP-China network. Effects of age, comorbidity and adherence to current antimicrobial guidelines on mortality in hospitalized elderly patients with community-acquired pneumonia. BMC Infect Dis. 2018. Apr 24;18(1):192. 10.1186/s12879-018-3098-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Hang PT, Anh DPP. Awareness survey regarding antibiotic among healthcare workers in Hungvuong hospital. Antimicrob Resist Infect Control. 2017;6(Suppl2):AS10. 10.1186/s13756-017-0176-1 [DOI] [Google Scholar]
- 153.Haque M, Rahman NAA, McKimm J, Binti Abdullah SL, Islam MZ, Zulkifli Z, et al. A cross-sectional study evaluating the knowledge and beliefs about, and the use of antibiotics amongst Malaysian university students. Expert Rev Anti Infect Ther. 2019. Apr;17(4):275–84. 10.1080/14787210.2019.1581607 [DOI] [PubMed] [Google Scholar]
- 154.Harasani K, Xhafaj D, Begolli A, Olvera-Porcel MC. Prevalence of potentially inappropriate prescriptions in primary care and correlates with mild cognitive impairment. Pharm Pract (Granada). 2020. Jul-Sep;18(3):2017. 10.18549/PharmPract.2020.3.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Harasani K, Xhafaj D, Qipo O. Prevalence and types of potentially inappropriate prescriptions among older and middle-aged community-dwelling Albanian patients. Int J Risk Saf Med. 2020;31(1):5–13. 10.3233/JRS-195052 [DOI] [PubMed] [Google Scholar]
- 156.Harugeri A, Joseph J, Parthasarathi G, Ramesh M, Guido S. Potentially inappropriate medication use in elderly patients: a study of prevalence and predictors in two teaching hospitals. J Postgrad Med. 2010. Jul-Sep;56(3):186–91. 10.4103/0022-3859.68642 [DOI] [PubMed] [Google Scholar]
- 157.Hasan SS, Kow CS, Thiruchelvam K, Chong DWK, Ahmed SI. An evaluation of the central nervous system medication use and frailty among residents of aged care homes in Malaysia. Neuroepidemiology. 2017;49(1-2):82–90. 10.1159/000480433 [DOI] [PubMed] [Google Scholar]
- 158.Hasan SS, Kow CS, Verma RK, Ahmed SI, Mittal P, Chong DWK. An evaluation of medication appropriateness and frailty among residents of aged care homes in Malaysia: a cross-sectional study. Medicine (Baltimore). 2017. Sep;96(35):e7929. 10.1097/MD.0000000000007929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Hashemzaei M, Afshari M, Koohkan Z, Bazi A, Rezaee R, Tabrizian K. Knowledge, attitude, and practice of pharmacy and medical students regarding self-medication, a study in Zabol University of Medical Sciences; Sistan and Baluchestan province in south-east of Iran. BMC Med Educ. 2021. Jan 14;21(1):49. 10.1186/s12909-020-02374-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Hatam N, Askarian M, Moravveji AR, Assadian O. Economic burden of inappropriate antibiotic use for prophylactic purpose in shiraz, Iran. Iran Red Crescent Med J. 2011. Apr;13(4):234–8. [PMC free article] [PubMed] [Google Scholar]
- 161.He AJ. The doctor-patient relationship, defensive medicine and overprescription in Chinese public hospitals: evidence from a cross-sectional survey in Shenzhen city. Soc Sci Med. 2014. Dec;123:64–71. 10.1016/j.socscimed.2014.10.055 [DOI] [PubMed] [Google Scholar]
- 162.He D, Zhu H, Zhou H, Dong N, Zhang H. Potentially inappropriate medications in Chinese older adults: a comparison of two updated Beers criteria. Int J Clin Pharm. 2021. Feb;43(1):229–35. 10.1007/s11096-020-01139-5 [DOI] [PubMed] [Google Scholar]
- 163.Hien H, Konaté B, Berthé A, Somé T, Drabo KM, Tougouma JB, et al. [Potentially inappropriate medication use in elderly care in Burkina Faso]. Sante Publique. 2016. Nov 25;28(5):677–86. French. 10.3917/spub.165.0677 [DOI] [PubMed] [Google Scholar]
- 164.Hoa NQ, Thi Lan P, Phuc HD, Chuc NTK, Stalsby Lundborg C. Antibiotic prescribing and dispensing for acute respiratory infections in children: effectiveness of a multi-faceted intervention for health-care providers in Vietnam. Glob Health Action. 2017;10(1):1327638. http://10.1080/16549716.2017.1327638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Holdsworth G, Garner PA, Harphan T. Crowded outpatient departments in city hospitals of developing countries: a case study from Lesotho. Int J Health Plann Manage. 1993. Oct-Dec;8(4):315–24. 10.1002/hpm.4740080407 [DOI] [PubMed] [Google Scholar]
- 166.Holguín-Hernández E, Orozco-Díaz JG. [Potentially inappropriate medication in elderly in a first level hospital, Bogota 2007]. Rev Salud Publica (Bogota). 2010. Apr;12(2):287–99. Spanish. [DOI] [PubMed] [Google Scholar]
- 167.Holloway KA, Rosella L, Henry D. The impact of WHO essential medicines policies on inappropriate use of antibiotics. PLoS One. 2016. Mar 22;11(3):e0152020. 10.1371/journal.pone.0152020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Homedes N, Ugalde A. Mexican pharmacies and antibiotic consumption at the US-Mexico border. South Med Rev. 2012. Dec;5(2):9–19. [PMC free article] [PubMed] [Google Scholar]
- 169.Hooi PY, Yong CM, Cheong I. A study of the appropriateness of antibiotic use in the medical wards of a tertiary teaching hospital in Malaysia. Int J Clin Pract. 2001. May;55(4):272–4. [PubMed] [Google Scholar]
- 170.Hoteit M, Mattar E, Allaw R, Abou Rached A. Epidemiological study assessing the overuse of proton pump inhibitors in lebanese population. Middle East J Dig Dis. 2020. Oct;12(4):265–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Huang Y, Zhang L, Huang X, Liu K, Yu Y, Xiao J. Potentially inappropriate medications in Chinese community-dwelling older adults. Int J Clin Pharm. 2020. Apr;42(2):598–603. 10.1007/s11096-020-00980-y [DOI] [PubMed] [Google Scholar]
- 172.Ibrahim OM, Saber-Ayad M. Antibiotic misuse in different hospital wards (a pilot study in an Egyptian hospital). Asian J Pharm Clin Res. 2012;5(2):95–7. [Google Scholar]
- 173.Ilić D, Bukumirić Z, Janković S. Impact of educational intervention on prescribing inappropriate medication to elderly nursing homes residents. Srp Arh Celok Lek. 2015. Mar-Apr;143(3-4):174–9. 10.2298/SARH1504174I [DOI] [PubMed] [Google Scholar]
- 174.Ingkapairoj N, Luanratanakorn S, Chumworathayi B, Kietpeerakool C, Supoken A. Incidences of cervical intraepithelial neoplasia 2-3 or cancer pathologic diagnoses in patients with a high grade squamous intraepithelial lesion pap smear attending a colposcopy clinic at Srinagarind hospital. Asian Pac J Cancer Prev. 2012;13(12):6203–6. 10.7314/APJCP.2012.13.12.6203 [DOI] [PubMed] [Google Scholar]
- 175.Isik MN, Dalgic N, Okuyan B, Yildirmak ZY, Kose G, Urganci N, et al. Clinical pharmacist-led medication review to evaluate inappropriate prescriptions in pediatric patients. Int J Clin Pharm. 2019;41(1):344. [Google Scholar]
- 176.James CD, Hanson K, Solon O, Whitty CJ, Peabody J. Do doctors under-provide, over-provide or do both? Exploring the quality of medical treatment in the Philippines. Int J Qual Health Care. 2011. Aug;23(4):445–55. 10.1093/intqhc/mzr029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Jardim JR, Stirbulov R, Moreno D, Zabert G, Lopez-Varela MV, Montes de Oca M. Respiratory medication use in primary care among COPD subjects in four Latin American countries. Int J Tuberc Lung Dis. 2017. Apr 1;21(4):458–65. 10.5588/ijtld.16.0633 [DOI] [PubMed] [Google Scholar]
- 178.Jhaj R, Bhargava VK, Uppal R, Lekha S, Reeta K, Kaur N. Use of cold medications for upper respiratory tract infections in children. Pharmacoepidemiol Drug Saf. 2001. Jun-Jul;10(4):323–7. 10.1002/pds.617 [DOI] [PubMed] [Google Scholar]
- 179.Jhaveri BN, Patel TK, Barvaliya MJ, Tripathi C. Utilization of potentially inappropriate medications in elderly patients in a tertiary care teaching hospital in India. Perspect Clin Res. 2014. Oct;5(4):184–9. 10.4103/2229-3485.140562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Johansson EW, Selling KE, Nsona H, Mappin B, Gething PW, Petzold M, et al. Integrated paediatric fever management and antibiotic over-treatment in Malawi health facilities: data mining a national facility census. Malar J. 2016. Aug 4;15(1):396. 10.1186/s12936-016-1439-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Juliano ACDSRS, Lucchetti ALG, Silva JTSD, Santos LG, Nunes JBT, Fernandes GC, et al. Inappropriate prescribing in older hospitalized adults: a comparison of medical specialties. J Am Geriatr Soc. 2018. Feb;66(2):383–8. 10.1111/jgs.15138 [DOI] [PubMed] [Google Scholar]
- 182.Kahabuka FK, Willemsen W, van’t Hof M, Ntabaye MK, Burgersdijk R, Frankenmolen F, et al. Initial treatment of traumatic dental injuries by dental practitioners. Endod Dent Traumatol. 1998. Oct;14(5):206–9. 10.1111/j.1600-9657.1998.tb00839.x [DOI] [PubMed] [Google Scholar]
- 183.Kandeel A, Palms DL, Afifi S, Kandeel Y, Etman A, Hicks LA, et al. An educational intervention to promote appropriate antibiotic use for acute respiratory infections in a district in Egypt- pilot study. BMC Public Health. 2019. May 10;19(S3) Suppl 3:498. 10.1186/s12889-019-6779-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Kandemir S, Ergül N. Grievances in cases using antibiotics due to orodental problems and assessment of the need for antibiotics. Int Dent J. 2000. Apr;50(2):73–7. 10.1002/j.1875-595X.2000.tb00802.x [DOI] [PubMed] [Google Scholar]
- 185.Kara Ö, Arık G, Kızılarslanoglu MC, Kılıc MK, Varan HD, Sümer F, et al. Potentially inappropriate prescribing according to the STOPP/START criteria for older adults. Aging Clin Exp Res. 2016. Aug;28(4):761–8. 10.1007/s40520-015-0475-4 [DOI] [PubMed] [Google Scholar]
- 186.Karaali C, Emiroglu M, Atalay S, Sert I, Dursun A, Kose S, et al. A new antibiotic stewardship program approach is effective on inappropriate surgical prophylaxis and discharge prescription. J Infect Dev Ctries. 2019. Nov 30;13(11):961–7. 10.3855/jidc.11734 [DOI] [PubMed] [Google Scholar]
- 187.Karuniawati H, Hassali MAA, Suryawati S, Ismail WI, Taufik T, Hossain MS. Assessment of knowledge, attitude, and practice of antibiotic use among the population of Boyolali, Indonesia: a cross-sectional study. Int J Environ Res Public Health. 2021. Aug 4;18(16):8258. 10.3390/ijerph18168258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Kashyap M, D’Cruz S, Sachdev A, Tiwari P. Evidence-based information leads to reduction in inappropriate drug prescribing: results from Indian older inpatients. Int J Risk Saf Med. 2015;27(4):209–17. 10.3233/JRS-150665 [DOI] [PubMed] [Google Scholar]
- 189.Kommalur A, Baddadka V, Devadas S, Kariyappa M, Dakshayani B, Krishnapura Lakshminarayana S, et al. Decreasing antibiotic over-use by implementation of an antibiotic stewardship programme in preterm neonates in resource limited settings - a quality improvement initiative. Paediatr Int Child Health. 2021. May;41(2):103–11. 10.1080/20469047.2021.1886545 [DOI] [PubMed] [Google Scholar]
- 190.Kotwani A, Joshi PC, Jhamb U, Holloway K. Prescriber and dispenser perceptions about antibiotic use in acute uncomplicated childhood diarrhea and upper respiratory tract infection in New Delhi: qualitative study. Indian J Pharmacol. 2017. Nov-Dec;49(6):419–31. 10.4103/ijp.IJP_508_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Kotwani A, Wattal C, Katewa S, Joshi PC, Holloway K. Factors influencing primary care physicians to prescribe antibiotics in Delhi India. Fam Pract. 2010. Dec;27(6):684–90. 10.1093/fampra/cmq059 [DOI] [PubMed] [Google Scholar]
- 192.Krymchantowski AV. Overuse of symptomatic medications among chronic (transformed) migraine patients: profile of drug consumption. Arq Neuropsiquiatr. 2003. Mar;61(1):43–7. 10.1590/S0004-282X2003000100007 [DOI] [PubMed] [Google Scholar]
- 193.Kua KP, Hamzah NN, Lee SWH. Potentially inappropriate medication prescribed among older patients in a primary care setting in Malaysia. Pharmacoepidemiol Drug Saf. 2020. Mar;29(3):363–4. 10.1002/pds.4945 [DOI] [PubMed] [Google Scholar]
- 194.Kuate-Tegueu C, Dongmo-Tajeuna JJ, Doumbe J, Mapoure-Njankouo Y, Noubissi G, Djientcheu VDP. Management of blood pressure in acute stroke: comparison of current prescribing patterns with AHA/ASA guidelines in a sub-Saharan African referral hospital. J Neurol Sci. 2017. Nov 15;382:137–41. 10.1016/j.jns.2017.10.002 [DOI] [PubMed] [Google Scholar]
- 195.Kucukdagli P, Bahat G, Bay I, Kilic C, Oren MM, Turkmen BO, et al. The relationship between common geriatric syndromes and potentially inappropriate medication use among older adults. Aging Clin Exp Res. 2020. Apr;32(4):681–7. 10.1007/s40520-019-01239-x [DOI] [PubMed] [Google Scholar]
- 196.Kumar S, Wong PS, Hasan SS, Kairuz T. The relationship between sleep quality, inappropriate medication use and frailty among older adults in aged care homes in Malaysia. PLoS One. 2019. Oct 17;14(10):e0224122. 10.1371/journal.pone.0224122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Lai PS, Wong YY, Low YC, Lau HL, Chin KF, Mahadeva S. Unexplained abdominal pain as a driver for inappropriate therapeutics: an audit on the use of intravenous proton pump inhibitors. PeerJ. 2014. Jun 26;2:e451. 10.7717/peerj.451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.le Grand A, Hogerzeil HV, Haaijer-Ruskamp FM. Intervention research in rational use of drugs: a review. Health Policy Plan. 1999. Jun;14(2):89–102. 10.1093/heapol/14.2.89 [DOI] [PubMed] [Google Scholar]
- 199.Leblebicioglu H, Canbaz S, Peksen Y, Gunaydin M. Physicians’ antibiotic prescribing habits for upper respiratory tract infections in Turkey. J Chemother. 2002. Apr;14(2):181–4. 10.1179/joc.2002.14.2.181 [DOI] [PubMed] [Google Scholar]
- 200.Li H, Deng J, Yu P, Deng L, Ren X. Gaining insight into irrational off-label use of vidarabine through analysis of a spontaneous reporting system in China. J Clin Pharm Ther. 2020. Dec;45(6):1301–11. 10.1111/jcpt.13209 [DOI] [PubMed] [Google Scholar]
- 201.Li H, Pu S, Liu Q, Huang X, Kuang J, Chen L, et al. Potentially inappropriate medications in Chinese older adults: the Beers criteria compared with the screening tool of older persons’ prescriptions criteria. Geriatr Gerontol Int. 2017. Nov;17(11):1951–8. 10.1111/ggi.12999 [DOI] [PubMed] [Google Scholar]
- 202.Li H, Yan S, Li D, Gong Y, Lu Z, Yin X. Trends and patterns of outpatient and inpatient antibiotic use in China’s hospitals: data from the Center for Antibacterial Surveillance, 2012-16. J Antimicrob Chemother. 2019. Jun 1;74(6):1731–40. 10.1093/jac/dkz062 [DOI] [PubMed] [Google Scholar]
- 203.Li Y, Hu J, Gao YZ, Zhou F, Zhu ZH, Zhang BF, et al. Prevalence and determinants of potentially inappropriate medications prescribing in elderly patients in Chinese communities. Ann Palliat Med. 2021. Feb;10(2):2072–9. 10.21037/apm-21-32 [DOI] [PubMed] [Google Scholar]
- 204.Liang X, Jin C, Wang L, Wei L, Tomson G, Rehnberg C, et al. Unnecessary use of antibiotics for inpatient children with pneumonia in two counties of rural China. Int J Clin Pharm. 2011. Oct;33(5):750–4. 10.1007/s11096-011-9535-9 [DOI] [PubMed] [Google Scholar]
- 205.Liew NY, Chong YY, Yeow SH, Kua KP, Saw PS, Lee SWH. Prevalence of potentially inappropriate medications among geriatric residents in nursing care homes in Malaysia: a cross-sectional study. Int J Clin Pharm. 2019. Aug;41(4):895–902. 10.1007/s11096-019-00843-1 [DOI] [PubMed] [Google Scholar]
- 206.Lim JM, Singh SR, Duong MC, Legido-Quigley H, Hsu LY, Tam CC. Impact of national interventions to promote responsible antibiotic use: a systematic review. J Antimicrob Chemother. 2020. Jan 1;75(1):14–29. 10.1093/jac/dkz348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Lin L, Sun R, Yao T, Zhou X, Harbarth S. Factors influencing inappropriate use of antibiotics in outpatient and community settings in China: a mixed-methods systematic review. BMJ Glob Health. 2020. Nov;5(11):e003599. 10.1136/bmjgh-2020-003599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Liu X, Tong X, Jin L, Ha M, Cao F, Xu F, et al. Prospective study on the overuse of blood test-guided antibiotics on patients with acute diarrhea in primary hospitals of China. Patient Prefer Adherence. 2017. Mar 14;11:537–45. 10.2147/PPA.S123294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Liu Y, Zhu X, Li R, Zhang J, Zhang F. Proton pump inhibitor utilisation and potentially inappropriate prescribing analysis: insights from a single-centred retrospective study. BMJ Open. 2020. Nov 26;10(11):e040473. 10.1136/bmjopen-2020-040473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Locatelli J, Lira AR, Torraga LK, Paes AT. Inappropriate medications using the Beers criteria in Brazilian hospitalized elderly patients. Consult Pharm. 2010. Jan;25(1):36–40. 10.4140/TCP.n.2010.36 [DOI] [PubMed] [Google Scholar]
- 211.Lunardi-Maia T, Schuelter-Trevisol F, Galato D. [Medication use during the first trimester of pregnancy: drug safety and adoption of folic acid and ferrous sulphate]. Rev Bras Ginecol Obstet. 2014. Dec;36(12):541–7. Portuguese. 10.1590/So100-720320140005051 [DOI] [PubMed] [Google Scholar]
- 212.Luo H, Fan Q, Xiao S, Chen K. Impact of clinical pharmacist interventions on inappropriate prophylactic acid suppressant use in hepatobiliary surgical patients undergoing elective operations. PLoS One. 2017. Oct 18;12(10):e0186302. 10.1371/journal.pone.0186302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Lutz BH, Miranda VIA, Bertoldi AD. Potentially inappropriate medications among older adults in Pelotas, Southern Brazil. Rev Saude Publica. 2017. Jun 22;51(0):52. 10.1590/s1518-8787.2017051006556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Ma Z, Tong Y, Zhang C, Liu L. Potentially inappropriate medications and potentially prescribing omissions in Chinese older patients: comparison of two versions of STOPP/START. J Clin Pharm Ther. 2020. Dec;45(6):1405–13. 10.1111/jcpt.13237 [DOI] [PubMed] [Google Scholar]
- 215.Ma Z, Zhang C, Cui X, Liu L. Comparison of three criteria for potentially inappropriate medications in Chinese older adults. Clin Interv Aging. 2018. Dec 28;14:65–72. 10.2147/CIA.S190983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Machado-Duque ME, Valladales-Restrepo LF, Ospina-Cano JA, Londoño-Serna MJ, Machado-Alba JE. Potentially inappropriate prescriptions of antipsychotics for patients with dementia. Front Pharmacol. 2021. May 31;12:695315. 10.3389/fphar.2021.695315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Madut DB, Rubach MP, Bonnewell JP, Cutting ER, Carugati M, Kalengo N, et al. Trends in fever case management for febrile inpatients in a low malaria incidence setting of Tanzania. Trop Med Int Health. 2021. Dec;26(12):1668–76. 10.1111/tmi.13683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Magalhães MS, Santos FSD, Reis AMM. Factors associated with the use of potentially inappropriate medication by elderly patients prescribed at hospital discharge. Einstein (Sao Paulo). 2019. Oct 28;18:eAO4877. 10.31744/einstein_journal/2020AO4877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Mao W, Jiang W, Hamilton C, Zhang H, Huang F, Lucas H, et al. Over- and under-treatment of TB patients in eastern China: an analysis based on health insurance claims data. Trop Med Int Health. 2019. Sep;24(9):1078–87. 10.1111/tmi.13287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Mao W, Vu H, Xie Z, Chen W, Tang S. Systematic review on irrational use of medicines in China and Vietnam. PLoS One. 2015. Mar 20;10(3):e0117710. 10.1371/journal.pone.0117710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Marques GFM, Rezende DMRP, Silva IPD, Souza PC, Barbosa SRM, Penha RM, et al. Polypharmacy and potentially inappropriate medications for elder people in gerontological nursing. Rev Bras Enferm. 2018. Sep-Oct;71(5):2440–6. 10.1590/0034-7167-2017-0211 [DOI] [PubMed] [Google Scholar]
- 222.Martins GA, Acurcio FA, Franceschini SC, Priore SE, Ribeiro AQ. [Use of potentially inappropriate medications in the elderly in Viçosa, Minas Gerais State, Brazil: a population-based survey]. Cad Saude Publica. 2015. Nov;31(11):2401–12. Portuguese. 10.1590/0102-311X00128214 [DOI] [PubMed] [Google Scholar]
- 223.Marume A, Muvirimi TG, Chitindingu K, Mutingwende I. Inappropriate use of promethazine and promethazine-containing products in children under the age of three years in Harare, Zimbabwe. Cent Afr J Med. 2011. Sep-Dec;57(9-12):39–43. [PubMed] [Google Scholar]
- 224.Marzi M M, Diruscio A V, Núñez H M, Pires S M, Quaglia B N. [Analysis of medication prescription in an Argentinian geriatric hospital]. Rev Med Chil. 2013. Feb;141(2):194–201. Spanish. 10.4067/S0034-98872013000200008 [DOI] [PubMed] [Google Scholar]
- 225.Mathibe LJ, Zwane NP. Unnecessary antimicrobial prescribing for upper respiratory tract infections in children in Pietermaritzburg, South Africa. Afr Health Sci. 2020. Sep;20(3):1133–42. 10.4314/ahs.v20i3.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Mazhar F, Akram S, Malhi SM, Haider N. A prevalence study of potentially inappropriate medications use in hospitalized Pakistani elderly. Aging Clin Exp Res. 2018. Jan;30(1):53–60. 10.1007/s40520-017-0742-7 [DOI] [PubMed] [Google Scholar]
- 227.Mbonye AK, Birungi J, Yanow S, Magnussen P. Prescription patterns and drug use among pregnant women with febrile Illnesses in Uganda: a survey in out-patient clinics. BMC Infect Dis. 2013. May 23;13(1):237. 10.1186/1471-2334-13-237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Mbonye AK, Magnussen P, Lal S, Hansen KS, Cundill B, Chandler C, et al. A cluster randomised trial introducing rapid diagnostic tests into registered drug shops in Uganda: impact on appropriate treatment of malaria. PLoS One. 2015. Jul 22;10(7):e0129545. 10.1371/journal.pone.0129545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Memari AH, Ziaee V, Beygi S, Moshayedi P, Mirfazeli FS. Overuse of psychotropic medications among children and adolescents with autism spectrum disorders: perspective from a developing country. Res Dev Disabil. 2012. Mar-Apr;33(2):563–9. 10.1016/j.ridd.2011.10.001 [DOI] [PubMed] [Google Scholar]
- 230.Meng Q, Liu X, Shi J. Comparing the services and quality of private and public clinics in rural China. Health Policy Plan. 2000. Dec;15(4):349–56. 10.1093/heapol/15.4.349 [DOI] [PubMed] [Google Scholar]
- 231.Menon VB, Ramesh M, Pereira P, Chilkunda Raviprakash V, Undela K. Inappropriate prescribing of antimalarial therapy for the treatment of undifferentiated febrile illness among the elderly. J Pharm Pract Res. 2018;48(6):530–6. 10.1002/jppr.1452 [DOI] [Google Scholar]
- 232.Menon VB, Ramesh M, Pereira P, Cr V, Undela K, Hathur BG. Cost implications of inappropriate prescribing of anti-malarial therapy for treatment of undifferentiated febrile illness among elderly. Value Health. 2016;19(7):A402. 10.1016/j.jval.2016.09.320 [DOI] [Google Scholar]
- 233.Merlano SU, Marimón RC, Puentes NC. Pharmaceutical intervention to potentially inappropriate prescriptions according to STOPP/START criteria on geriatric patients hospitalized in a third level institution of Cartagena Colombia. Arch Venez Farmacol Ter. 2020;39(6):685–8. [Google Scholar]
- 234.Milone MC, Olocco ME, Vidal Guitart X. Sobre utilización de Inhibidores de la acidez gástrica en pacientes pediátricos. Rev Salud Publica (Córdoba). 2012;16(1):27–35. Spanish. [Google Scholar]
- 235.Mino-León D, Sánchez-García S, Giraldo-Rodríguez L, Reyes-Morales H. Potentially inappropriate prescribing to older adults in ambulatory care: prevalence and associated patient conditions. Eur Geriatr Med. 2019. Aug;10(4):639–47. 10.1007/s41999-019-00181-5 [DOI] [PubMed] [Google Scholar]
- 236.Mo L, Ding D, Pu SY, Liu QH, Li H, Dong BR, et al. Patients aged 80 years or older are encountered more potentially inappropriate medication use. Chin Med J (Engl). 2016. Jan 5;129(1):22–7. 10.4103/0366-6999.172558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Mohamed Ibrahim O, Al Mazrouei N, Al Meslamani AZ, Kassem AB, El-Bassiouny NA, Mohammed Ebaed SB, et al. Assessment of a new strategy for catalyzing deprescribing in community pharmacies. J Am Pharm Assoc (Wash DC). 2022. Jan-Feb;62(1):125–33. 10.1016/j.japh.2021.09.003 [DOI] [PubMed] [Google Scholar]
- 238.Molina GJ. Sobreusos de tecnologías medicas: racionalidad en la formulacion de lincosaminas. Acta Med Colomb. 1984;9(4):139–45. Spanish. [Google Scholar]
- 239.Momin TG, Pandya RN, Rana DA, Patel VJ. Use of potentially inappropriate medications in hospitalized elderly at a teaching hospital: a comparison between Beers 2003 and 2012 criteria. Indian J Pharmacol. 2013. Nov-Dec;45(6):603–7. 10.4103/0253-7613.121372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Mongkhon P, Tanasombat T, Jeenapongsa R, Kongkaew C. The association between inappropriate medication use and health-related outcomes among nursing home residents: a systematic review and meta-analysis. Drug Saf. 2018;41(11):1171–2. [Google Scholar]
- 241.Mori AL, Carvalho RC, Aguiar PM, de Lima MG, Rossi MD, Carrillo JF, et al. Potentially inappropriate prescribing and associated factors in elderly patients at hospital discharge in Brazil: a cross-sectional study. Int J Clin Pharm. 2017. Apr;39(2):386–93. 10.1007/s11096-017-0433-7 [DOI] [PubMed] [Google Scholar]
- 242.Mortazavi SS, Shati M, Malakouti SK, Khankeh HR, Mehravaran S, Ahmadi F. Physicians’ role in the development of inappropriate polypharmacy among older adults in Iran: a qualitative study. BMJ Open. 2019. May 22;9(5):e024128. 10.1136/bmjopen-2018-024128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Mustafa IEMA. The inappropriate prescribing of antibacterial medicines in Sudan; a national study at national health insurance fund setting. Pharmacoepidemiol Drug Saf. 2014;23(Suppl1):60.23913654 [Google Scholar]
- 244.Nafade V, Huddart S, Sulis G, Daftary A, Miraj SS, Saravu K, et al. Over-the-counter antibiotic dispensing by pharmacies: a standardised patient study in Udupi district, India. BMJ Glob Health. 2019. Nov 1;4(6):e001869. 10.1136/bmjgh-2019-001869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Nair M, Tripathi S, Mazumdar S, Mahajan R, Harshana A, Pereira A, et al. “Without antibiotics, I cannot treat”: a qualitative study of antibiotic use in Paschim Bardhaman district of West Bengal, India. PLoS One. 2019. Jun 27;14(6):e0219002. 10.1371/journal.pone.0219002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Nappo SA, de Oliveira EM, Morosini S. Inappropriate prescribing of compounded antiobesity formulas in Brazil. Pharmacoepidemiol Drug Saf. 1998. May;7(3):207–12. [DOI] [PubMed] [Google Scholar]
- 247.Ndyomugyenyi R, Lal S, Hansen K, Chandler C, Magnussen P, Clarke S. Adherence to rapid diagnostic test results among community medicine distributors in rural Ugandan communities. Trop Med Int Health. 2013;18(Suppl1):73–4. 10.1111/tmi.12162 [DOI] [Google Scholar]
- 248.Nedin Ranković G, Janković SM, Veličković Radovanović R, Jović Z, Pešić G, Pavlović S, et al. Potentially inappropriate prescribing of drugs in elderly patients on chronic hemodialysis treatment. Clin Nephrol. 2018. Jun;89(6):453–60. 10.5414/CN109095 [DOI] [PubMed] [Google Scholar]
- 249.Nepal A, Hendrie D, Selvey LA, Robinson S. Factors influencing the inappropriate use of antibiotics in the Rupandehi district of Nepal. Int J Health Plann Manage. 2021. Jan;36(1):42–59. 10.1002/hpm.3061 [DOI] [PubMed] [Google Scholar]
- 250.Nguyen QH, Nguyen TK, Ho D, Larsson M, Eriksson B, Lundborg CS. Unnecessary antibiotic use for mild acute respiratory infections during 28-day follow-up of 823 children under five in rural Vietnam. Trans R Soc Trop Med Hyg. 2011. Nov;105(11):628–36. 10.1016/j.trstmh.2011.07.015 [DOI] [PubMed] [Google Scholar]
- 251.Nguyen TA, Pham T, Vu HTT, Nguyen TX, Vu TT, Nguyen BTT, et al. Use of Potentially Inappropriate Medications in People With Dementia in Vietnam and Its Associated Factors. Am J Alzheimers Dis Other Demen. 2018. Nov;33(7):423–32. 10.1177/1533317518768999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Novaes PH, da Cruz DT, Lucchetti ALG, Leite ICG, Lucchetti G. Comparison of four criteria for potentially inappropriate medications in Brazilian community-dwelling older adults. Geriatr Gerontol Int. 2017. Oct;17(10):1628–35. 10.1111/ggi.12944 [DOI] [PubMed] [Google Scholar]
- 253.Novan Y I P, Primadi A, Mahfudz, Suharjono. Comparison of antibiotic prescriptions in adults and children with upper respiratory tract infections in Bangka Tengah primary health care centers. J Basic Clin Physiol Pharmacol. 2020. Jan 11;30(6):/j/jbcpp.2019.30.issue-6/jbcpp-2019-0248/jbcpp-2019-0248.xml. 10.1515/jbcpp-2019-0248 [DOI] [PubMed] [Google Scholar]
- 254.Okebe JU, Walther B, Bojang K, Drammeh S, Schellenberg D, Conway DJ, et al. Prescribing practice for malaria following introduction of artemether-lumefantrine in an urban area with declining endemicity in West Africa. Malar J. 2010. Jun 24;9(1):180. 10.1186/1475-2875-9-180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Okonogi K, Pothirat C, Bumroongkit C, Deesomchok A, Theerakittikul T, Limsukon A, et al. Adverse outcomes associated with physician’s adherence to gold guideline for management of stable COPD patients. Respirology. 2016;21 S3:175. 10.1111/resp.12939_1527005391 [DOI] [Google Scholar]
- 256.Oliveira MG, Amorim WW, de Jesus SR, Heine JM, Coqueiro HL, Passos LC. A comparison of the Beers and STOPP criteria for identifying the use of potentially inappropriate medications among elderly patients in primary care. J Eval Clin Pract. 2015. Apr;21(2):320–5. 10.1111/jep.12319 [DOI] [PubMed] [Google Scholar]
- 257.Oliveira MG, Amorim WW, de Jesus SR, Rodrigues VA, Passos LC. Factors associated with potentially inappropriate medication use by the elderly in the Brazilian primary care setting. Int J Clin Pharm. 2012. Aug;34(4):626–32. 10.1007/s11096-012-9656-9 [DOI] [PubMed] [Google Scholar]
- 258.Om C, Daily F, Vlieghe E, McLaughlin JC, McLaws ML. “If it’s a broad spectrum, it can shoot better”: inappropriate antibiotic prescribing in Cambodia. Antimicrob Resist Infect Control. 2016. Dec 20;5(1):58. 10.1186/s13756-016-0159-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Onchiri FM, Pavlinac PB, Singa BO, Naulikha JM, Odundo EA, Farquhar C, et al. Frequency and correlates of malaria over-treatment in areas of differing malaria transmission: a cross-sectional study in rural Western Kenya. Malar J. 2015. Mar 1;14(1):97. 10.1186/s12936-015-0613-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Opoka RO, Ssemata AS, Oyang W, Nambuya H, John CC, Tumwine JK, et al. High rate of inappropriate blood transfusions in the management of children with severe anemia in Ugandan hospitals. BMC Health Serv Res. 2018. Jul 18;18(1):566. 10.1186/s12913-018-3382-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Opondo C, Ayieko P, Ntoburi S, Wagai J, Opiyo N, Irimu G, et al. Effect of a multi-faceted quality improvement intervention on inappropriate antibiotic use in children with non-bloody diarrhoea admitted to district hospitals in Kenya. BMC Pediatr. 2011. Nov 25;11(1):109. 10.1186/1471-2431-11-109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Osatakul S, Puetpaiboon A. Appropriate use of empirical antibiotics in acute diarrhoea: a cross-sectional survey in southern Thailand. Ann Trop Paediatr. 2007. Jun;27(2):115–22. 10.1179/146532807X192480 [DOI] [PubMed] [Google Scholar]
- 263.Østergaard MS, Kjærgaard J, Kristensen MM, Reventlow S, Poulsen A, Isaeva E, et al. Recurrent lower respiratory illnesses among young children in rural Kyrgyzstan: overuse of antibiotics and possible under-diagnosis of asthma. A qualitative FRESH AIR study. NPJ Prim Care Respir Med. 2018. Apr 10;28(1):13. 10.1038/s41533-018-0081-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Öztürk GZ, Ardiç C, Toprak D. Frequency of polypharmacy and use of potentially inappropriate medications in the elderly. Turk Geriatri Derg. 2017;20(4):296–305. [Google Scholar]
- 265.Palacios-Saucedo GDC, de la Garza-Camargo M, Briones-Lara E, Carmona-González S, García-Cabello R, Islas-Esparza LA, et al. [Assessment of antibiotic use and impact of an intervention intended to modify the prescribing behavior in surgical prophylaxis in 6hospitals in the metropolitan area of Monterrey, Mexico]. Cir Cir. 2017. Nov–Dec;85(6):459–70. Spanish. [DOI] [PubMed] [Google Scholar]
- 266.Panumatrassamee C, Kawamatawong T, Samarnkongsak T, Pongcharoensuk P, Pattanaprateep O. Rationalized medication prescribing for COPD patients following gold guideline in RAMATHIBODI hospital. Respirology. 2014;19 S3:122. 10.1111/resp.1241724372635 [DOI] [Google Scholar]
- 267.Paredes JL, Navarro R, Riveros M, Picon V, Conde F, Suito-Ferrand M, et al. Parental antibiotic use in urban and peri-urban health care centers in Lima: a cross-sectional study of knowledge, attitudes, and practices. Clin Med Insights Pediatr. 2019. Aug 21;13:1179556519869338. 10.1177/1179556519869338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Passarelli MC, Jacob-Filho W, Figueras A. Adverse drug reactions in an elderly hospitalised population: inappropriate prescription is a leading cause. Drugs Aging. 2005;22(9):767–77. 10.2165/00002512-200522090-00005 [DOI] [PubMed] [Google Scholar]
- 269.Passi A, Margozzini P, Valenzuela E, Hoyl T, Marin PP, Carrasco M, et al. [Inappropriate medication use among Chilean older people]. Rev Med Chil. 2016. Apr;144(4):417–25. Spanish. 10.4067/S0034-98872016000400001 [DOI] [PubMed] [Google Scholar]
- 270.Pezeshki MZ, Janati A, Arab-Zozani M. Medical overuse in the Iranian healthcare system: a systematic scoping review and practical recommendations for decreasing medical overuse during unexpected COVID-19 pandemic opportunity. Risk Manag Healthc Policy. 2020. Aug 11;13:1103–10. 10.2147/RMHP.S262908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Pinto CR, Lemos ACM, Assunção-Costa L, Alcântara AT, Yamamura LLL, Souza GS, et al. Management of COPD within the Brazilian Unified Health Care System in the state of Bahia: an analysis of real-life medication use patterns. J Bras Pneumol. 2019. Feb 11;45(1):e20170194. 10.1590/1806-3713/e20170194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Pisonero Socias JJ, Guanche Garcell H, Mir Narbona I, Enseñat Sánchez R, Fiterre Lancis I, García Arzola B. Implementación de un programa de control de antibióticos a nivel hospitalario: efecto económico. Rev Cuba Cir. 2014;53(1):52–9. Spanish. [Google Scholar]
- 273.Porter G, Grills N. Medication misuse in India: a major public health issue in India. J Public Health (Oxf). 2016. Jun;38(2):e150–7. 10.1093/pubmed/fdv072 [DOI] [PubMed] [Google Scholar]
- 274.Prasert V, Akazawa M, Shono A, Chanjaruporn F, Ploylearmsang C, Muangyim K, et al. Applying the Lists of Risk Drugs for Thai Elderly (LRDTE) as a mechanism to account for patient age and medicine severity in assessing potentially inappropriate medication use. Res Social Adm Pharm. 2018. May;14(5):451–8. 10.1016/j.sapharm.2017.05.012 [DOI] [PubMed] [Google Scholar]
- 275.Prasert V, Shono A, Chanjaruporn F, Ploylearmsang C, Boonnan K, Khampetdee A, et al. Effect of a computerized decision support system on potentially inappropriate medication prescriptions for elderly patients in Thailand. J Eval Clin Pract. 2019. Jun;25(3):514–20. 10.1111/jep.13065 [DOI] [PubMed] [Google Scholar]
- 276.Projovic I, Vukadinovic D, Milovanovic O, Jurisevic M, Pavlovic R, Jacovic S, et al. Risk factors for potentially inappropriate prescribing to older patients in primary care. Eur J Clin Pharmacol. 2016. Jan;72(1):93–107. 10.1007/s00228-015-1957-1 [DOI] [PubMed] [Google Scholar]
- 277.Puspitasari HP, Faturrohmah A, Hermansyah A. Do Indonesian community pharmacy workers respond to antibiotics requests appropriately? Trop Med Int Health. 2011. Jul;16(7):840–6. 10.1111/j.1365-3156.2011.02782.x [DOI] [PubMed] [Google Scholar]
- 278.Rababa M, Rababa’h A. The inappropriate use of proton pump inhibitors and its associated factors among community-dwelling older adults. Heliyon. 2021. Jul 15;7(7):e07595. 10.1016/j.heliyon.2021.e07595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Rambhade S, Chakarborty A, Shrivastava A, Patil UK, Rambhade A. A survey on polypharmacy and use of inappropriate medications. Toxicol Int. 2012. Jan;19(1):68–73. 10.4103/0971-6580.94506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Ramsamy Y, Muckart DJ, Han KS. Microbiological surveillance and antimicrobial stewardship minimise the need for ultrabroad-spectrum combination therapy for treatment of nosocomial infections in a trauma intensive care unit: an audit of an evidence-based empiric antimicrobial policy. S Afr Med J. 2013. Mar 15;103(6):371–6. 10.7196/SAMJ.6459 [DOI] [PubMed] [Google Scholar]
- 281.Raspopovic K, Jankovic S, Opancina V. Factors affecting inappropriate prescription of antibiotics and the emergence of antibiotic resistance in patients in primary health care. Medicinski Casopis. 2016;50(3):85–90. 10.5937/mckg50-12699 [DOI] [Google Scholar]
- 282.Rasu RS, Iqbal M, Hanifi S, Moula A, Hoque S, Rasheed S, et al. Level, pattern, and determinants of polypharmacy and inappropriate use of medications by village doctors in a rural area of Bangladesh. Clinicoecon Outcomes Res. 2014. Dec 3;6:515–21. 10.2147/CEOR.S67424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Rattanaumpawan P, Thamlikitkul V, Chokepaibulkit K, Lohsiriwat D, Aswapokee N. Vancomycin overuse in Siriraj Hospital. J Med Assoc Thai. 2006. Nov;89 Suppl 5:S125–32. [PubMed] [Google Scholar]
- 284.Reis CM, Dos Santos AG, de Jesus Souza P, Reis AMM. Factors associated with the use of potentially inappropriate medications by older adults with cancer. J Geriatr Oncol. 2017. Jul;8(4):303–7. 10.1016/j.jgo.2017.05.003 [DOI] [PubMed] [Google Scholar]
- 285.Rhee C, Aol G, Ouma A, Audi A, Muema S, Auko J, et al. Inappropriate use of antibiotics for childhood diarrhea case management - Kenya, 2009-2016. BMC Public Health. 2019. May 10;19(S3) Suppl 3:468. 10.1186/s12889-019-6771-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Roberts AA, Fajolu I, Oshun P, Osuagwu C, Awofeso O, Temiye E, et al. Feasibility study of prospective audit, intervention and feedback as an antimicrobial stewardship strategy at the Lagos university teaching hospital. Niger Postgrad Med J. 2020. Jan-Mar;27(1):54–8. 10.4103/npmj.npmj_115_19 [DOI] [PubMed] [Google Scholar]
- 287.Rozenfeld S, Fonseca MJ, Acurcio FA. Drug utilization and polypharmacy among the elderly: a survey in Rio de Janeiro City, Brazil. Rev Panam Salud Publica. 2008. Jan;23(1):34–43. 10.1590/S1020-49892008000100005 [DOI] [PubMed] [Google Scholar]
- 288.Ruvinsky S, Mónaco A, Pérez G, Taicz M, Inda L, Kijko I, et al. [Reasons for inappropriate prescribing of antibiotics in a high-complexity pediatric hospital]. Rev Panam Salud Publica. 2011. Dec;30(6):580–5. Spanish. [PubMed] [Google Scholar]
- 289.Saab YB, Hachem A, Sinno S, El-Moalem H. Inappropriate medication use in elderly Lebanese outpatients: prevalence and risk factors. Drugs Aging. 2006;23(9):743–52. 10.2165/00002512-200623090-00004 [DOI] [PubMed] [Google Scholar]
- 290.Saboor M, Kamrani AA, Momtaz YA, Sahaf R. Prevalence and associated factors of potentially inappropriate medications among Iranian older adults. Med Glas (Zenica). 2019. Feb 1;16(1):121–7. [DOI] [PubMed] [Google Scholar]
- 291.Sabry NA, Farid SF, Dawoud DM. Antibiotic dispensing in Egyptian community pharmacies: an observational study. Res Social Adm Pharm. 2014. Jan-Feb;10(1):168–84. 10.1016/j.sapharm.2013.03.004 [DOI] [PubMed] [Google Scholar]
- 292.Sadatsharifi A, Davarpanah MA, Namazi S, Mottaghi S, Mahmoudi L. Economic burden of inappropriate empiric antibiotic therapy: a report from southern Iran. Risk Manag Healthc Policy. 2019. Dec 12;12:339–48. 10.2147/RMHP.S222200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Sadoh WE, Akinsete AM. Physicians management of sore throat in children in Benin City, Nigeria. Niger J Clin Pract. 2009. Dec;12(4):407–11. [PubMed] [Google Scholar]
- 294.Šahman-Zaimović M, Vukmirović S, Tomić N, Stilinović N, Horvat O, Tomić L. Relationship between outpatient antibiotic use and the prevalence of bacterial infections in Montenegro. Vojnosanit Pregl. 2017. Jan;74(1):46–50. 10.2298/VSP150626146S [DOI] [PubMed] [Google Scholar]
- 295.Saka SA, Oosthuizen F, Nlooto M. Potential inappropriate prescribing and associated factors among older persons in Nigeria and South Africa. Int J Clin Pharm. 2019. Feb;41(1):207–14. 10.1007/s11096-018-0770-1 [DOI] [PubMed] [Google Scholar]
- 296.Saleem Z, Saeed H, Hassali MA, Godman B, Asif U, Yousaf M, et al. Pattern of inappropriate antibiotic use among hospitalized patients in Pakistan: a longitudinal surveillance and implications. Antimicrob Resist Infect Control. 2019. Nov 21;8(1):188. 10.1186/s13756-019-0649-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Sánchez X, Orrico M, Morillo T, Manzano A, Jimbo R, Armijos L. Reducing unnecessary antibiotic prescription through implementation of a clinical guideline on self-limiting respiratory tract infections. PLoS One. 2021. Apr 1;16(4):e0249475. 10.1371/journal.pone.0249475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Santos Garcia T, Simas da Rocha B, De Jezus Castro SM, Heineck I. Potentially inappropriate medications for older adults in a primary healthcare unit in southern Brazil. Int J Clin Pharm. 2020. Jun;42(3):911–22. 10.1007/s11096-020-01048-7 [DOI] [PubMed] [Google Scholar]
- 299.Saqlain M, Ali H, Kamran S, Munir MU, Jahan S, Mazhar F. Potentially inappropriate medications use and its association with health-related quality of life among elderly cardiac patients. Qual Life Res. 2020. Oct;29(10):2715–24. 10.1007/s11136-020-02530-5 [DOI] [PubMed] [Google Scholar]
- 300.Sarwar MR, Iftikhar S, Sarfraz M. Influence of education level of older patients on polypharmacy, potentially inappropriate medications listed in Beer’s criteria, and unplanned hospitalization: a cross-sectional study in Lahore, Pakistan. Medicina (Kaunas). 2018. Aug 24;54(4):57. 10.3390/medicina54040057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Sayin Z, Sancar M, Ozen Y, Okuyan B. Medication review in elderly patients at community pharmacy setting: the association between occurrence of potentially inappropriate prescribing and medication regimen complexity. Int J Clin Pharm. 2020;42(1):243. [Google Scholar]
- 302.Sayın Z, Sancar M, Özen Y, Okuyan B. Polypharmacy, potentially inappropriate prescribing and medication complexity in Turkish older patients in the community pharmacy setting. Acta Clin Belg. 2022. Apr;77(2):273–9. 10.1080/17843286.2020.1829251 [DOI] [PubMed] [Google Scholar]
- 303.Schapira M, Calabró P, Montero-Odasso M, Osman A, Guajardo ME, Martínez B, et al. A multifactorial intervention to lower potentially inappropriate medication use in older adults in Argentina. Aging Clin Exp Res. 2021. Dec;33(12):3313–20. 10.1007/s40520-020-01582-4 [DOI] [PubMed] [Google Scholar]
- 304.Sen E, Guclu SZ, Kibar I, Ocal U, Yilmaz V, Celik O, et al. Adherence to GOLD guideline treatment recommendations among pulmonologists in Turkey. Int J Chron Obstruct Pulmon Dis. 2015. Dec 10;10(1):2657–63. 10.2147/COPD.S85324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Senn N, Rarau P, Salib M, Manong D, Siba P, Rogerson S, et al. Use of antibiotics within the IMCI guidelines in outpatient settings in Papua New Guinean children: an observational and effectiveness study. PLoS One. 2014. Mar 13;9(3):e90990. 10.1371/journal.pone.0090990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Shah KN, Joshi HM, Christian RP, Patel KP, Malhotra SD. Prevalence of potentially inappropriate medications and prescription cost analysis among older cardiac patients in an outpatient department of a tertiary care hospital in India. J Basic Clin Pharm. 2016. Sep;7(4):110–5. 10.4103/0976-0105.189434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Shamshirian A, Mohseni AR, Pourfathollah AA, Mehdipour S, Hosseini S, Ghorbanpour A, et al. A review of blood usage and wastage in a tertiary heart center. Acta Clin Belg. 2020. Apr;75(2):96–103. 10.1080/17843286.2018.1555113 [DOI] [PubMed] [Google Scholar]
- 308.Broom J, Broom A, Kenny K, Chittem M. Antimicrobial overuse in India: a symptom of broader societal issues including resource limitations and financial pressures. Glob Public Health. 2021. Jul;16(7):1079–87. 10.1080/17441692.2020.1839930 [DOI] [PubMed] [Google Scholar]
- 309.Shamsuddin S, Akkawi ME, Zaidi STR, Ming LC, Manan MM. Antimicrobial drug use in primary healthcare clinics: a retrospective evaluation. Int J Infect Dis. 2016. Nov;52:16–22. 10.1016/j.ijid.2016.09.013 [DOI] [PubMed] [Google Scholar]
- 310.Sharma R, Bansal P, Garg R, Ranjan R, Kumar R, Arora M. Prevalence of potentially inappropriate medication and its correlates in elderly hospitalized patients: a cross-sectional study based on Beers criteria. J Family Community Med. 2020. Sep-Dec;27(3):200–7. 10.4103/jfcm.JFCM_175_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Sharma R, Bansal P, Sharma A, Chhabra M, Bansal N, Arora M. Clonazepam tops the list of potentially inappropriate psychotropic (PIP) medications in older adults with psychiatric illness: a cross-sectional study based on Beers criteria 2019 vs STOPP criteria 2015. Asian J Psychiatr. 2021. Apr;58:102570. 10.1016/j.ajp.2021.102570 [DOI] [PubMed] [Google Scholar]
- 312.Sharma R, Chhabra M, Vidyasagar K, Rashid M, Fialova D, Bhagavathula AS. Potentially inappropriate medication use in older hospitalized patients with type 2 diabetes: a cross-sectional study. Pharmacy (Basel). 2020. Nov 17;8(4):E219. 10.3390/pharmacy8040219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Sharma S, Kumari N, Sengupta R, Malhotra Y, Bhartia S. Rationalising antibiotic use after low-risk vaginal deliveries in a hospital setting in India. BMJ Open Qual. 2021. Jul;10 Suppl 1:e001413. 10.1136/bmjoq-2021-001413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Shehadeh M, Suaifan G, Darwish RM, Wazaify M, Zaru L, Alja’fari S. Knowledge, attitudes and behavior regarding antibiotics use and misuse among adults in the community of Jordan. A pilot study. Saudi Pharm J. 2012. Apr;20(2):125–33. 10.1016/j.jsps.2011.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Shet A, Sundaresan S, Forsberg BC. Pharmacy-based dispensing of antimicrobial agents without prescription in India: appropriateness and cost burden in the private sector. Antimicrob Resist Infect Control. 2015. Dec 11;4(1):55. 10.1186/s13756-015-0098-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Shimels T, Bilal AI, Mulugeta A. Evaluation of Ceftriaxone utilization in internal medicine wards of general hospitals in Addis Ababa, Ethiopia: a comparative retrospective study. J Pharm Policy Pract. 2015. Nov 9;8(1):26. 10.1186/s40545-015-0047-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Silay K, Yalcin A, Akinci S, Gursoy FG, Sener Dede D. Charlson comorbidity index, inappropriate medication use and cognitive impairment: Bermuda Triangle. Wien Klin Wochenschr. 2017. Nov;129(21-22):799–804. 10.1007/s00508-017-1253-4 [DOI] [PubMed] [Google Scholar]
- 318.Sirijit S, Manit S, Peerasak L. Benzodiazepine overuse in an internal medicine outpatient department: a prospective study. ASEAN J Psychiatr. 2007;8:106–10. [Google Scholar]
- 319.Sonkar SC, Wasnik K, Kumar A, Mittal P, Saluja D. Comparative analysis of syndromic and PCR-based diagnostic assay reveals misdiagnosis/ overtreatment for trichomoniasis based on subjective judgment in symptomatic patients. Infect Dis Poverty. 2016. May 5;5(1):42. 10.1186/s40249-016-0133-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Sonmez A, Tasci I, Demirci I, Haymana C, Barcin C, Aydin H, et al. ; TEMD Study Group. A cross-sectional study of overtreatment and deintensification of antidiabetic and antihypertensive medications in diabetes mellitus: the TEMD overtreatment study. Diabetes Ther. 2020. May;11(5):1045–59. 10.1007/s13300-020-00779-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Sonmez A, Tasci I, Demirci I, Haymana C, Barcin C, Aydin H, et al. The rates of overtreatment and deintensification of antidiabetic and antihypertensive medications in patients with diabetes mellitus. Diabetes. 2018;67(Supplement_1):191-LB. 10.2337/db18-191-LB [DOI] [Google Scholar]
- 322.Sönmez Y, Aşci H, Izmeirli Olgun G, Gündoğar D, Cankara FN, Yeşilot S. Evaluation of potentially inappropriate drug use and medical non-adherence in a community-dwelling elderly population: a cross-sectional study. Turk Geriatri Derg. 2014;17(2):125–33. [Google Scholar]
- 323.Srisuwan S, Hamontri S, Kongsomboon K, Bhamarapravatana K, Suwannarurk K. See-and-treat approach to cervical intraepithelial lesions in HRH Princess Maha Chakri Sirindhorn Medical Center. Asian Pac J Cancer Prev. 2014;15(8):3483–6. 10.7314/APJCP.2014.15.8.3483 [DOI] [PubMed] [Google Scholar]
- 324.Stojanović M, Vuković M, Jovanović M, Dimitrijević S, Radenković M. Potentially inappropriate medications in Belgrade, Serbia nursing home residents: a comparison of two approaches. Eval Health Prof. 2021. Jun;44(2):180–5. 10.1177/0163278719900653 [DOI] [PubMed] [Google Scholar]
- 325.Suerdem M, Gunen H, Akyildiz L, Cilli A, Ozlu T, Uzaslan E, et al. Demographic, clinical and management characteristics of newly diagnosed COPD patients in Turkey: a real-life study. Int J Chron Obstruct Pulmon Dis. 2020. Feb 4;15:261–7. 10.2147/COPD.S211838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Sulis G, Daniels B, Kwan A, Gandra S, Daftary A, Das J, et al. Antibiotic overuse in the primary health care setting: a secondary data analysis of standardised patient studies from India, China and Kenya. BMJ Glob Health. 2020. Sep;5(9):e003393. 10.1136/bmjgh-2020-003393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Sun Q, Dyar OJ, Zhao L, Tomson G, Nilsson LE, Grape M, et al. Overuse of antibiotics for the common cold - attitudes and behaviors among doctors in rural areas of Shandong Province, China. BMC Pharmacol Toxicol. 2015. Mar 31;16(1):6. 10.1186/s40360-015-0009-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Supcharassaeng S, Suankratay C. Antibiotic prescription for adults with acute diarrhea at King Chulalongkorn Memorial Hospital, Thailand. J Med Assoc Thai. 2011. May;94(5):545–50. [PubMed] [Google Scholar]
- 329.Sutherland T, Moriau V, Niyonzima JM, Mueller A, Kabeja L, Twagirumugabe T, et al. The “just right” amount of oxygen. improving oxygen use in a Rwandan emergency department. Ann Am Thorac Soc. 2019. Sep;16(9):1138–42. 10.1513/AnnalsATS.201811-763QI [DOI] [PubMed] [Google Scholar]
- 330.Sychev DА, Danilina KS, Golovina ОV. [The frequency of potentially inappropriate medication use according to the Beers’ criteria in elderly people at the therapy departments of a multidisciplinary hospital]. Russian. Ter Arkh. 2015;87(1):27–30. 10.17116/terarkh201587127-30 [DOI] [PubMed] [Google Scholar]
- 331.Tang Y, Wu X, Cheng Q, Li X. Inappropriate initial antimicrobial therapy for hematological malignancies patients with Gram-negative bloodstream infections. Infection. 2020. Feb;48(1):109–16. 10.1007/s15010-019-01370-x [DOI] [PubMed] [Google Scholar]
- 332.Tarrant C, Colman AM, Jenkins DR, Chattoe-Brown E, Perera N, Mehtar S, et al. Drivers of broad-spectrum antibiotic overuse across diverse hospital contexts-a qualitative study of prescribers in the UK, Sri Lanka and South Africa. Antibiotics (Basel). 2021. Jan 19;10(1):94. 10.3390/antibiotics10010094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Tarrant C, Krockow EM, Nakkawita WMID, Bolscher M, Colman AM, Chattoe-Brown E, et al. Moral and contextual dimensions of “inappropriate” antibiotic prescribing in secondary care: a three-country interview study. Front Sociol. 2020. Feb 20;5:7. 10.3389/fsoc.2020.00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Tatlisu MA, Ozcan KS, Gungor B, Zengin A, Karatas MB, Nurkalem Z. Inappropriate use of digoxin in patients presenting with digoxin toxicity. J Geriatr Cardiol. 2015. Mar;12(2):143–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Tegegn HG, Tefera YG, Erku DA, Haile KT, Abebe TB, Chekol F, et al. Older patients’ perception of deprescribing in resource-limited settings: a cross-sectional study in an Ethiopia university hospital. BMJ Open. 2018. Apr 20;8(4):e020590. 10.1136/bmjopen-2017-020590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Temrel T, Şahin S. Polypharmacy and potentially inappropriate medication use in geriatric patients presenting to the emergency department. Turk Geriatri Derg. 2019;22(1):25–31. 10.31086/tjgeri.2019150569 [DOI] [Google Scholar]
- 337.Tesfaye BT, Tessema MT, Yizengaw MA, Bosho DD. Potentially inappropriate medication use among older adult patients on follow-up at the chronic care clinic of a specialized teaching hospital in Ethiopia. A cross-sectional study. BMC Geriatr. 2021. Oct 7;21(1):530. 10.1186/s12877-021-02463-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Tian F, Li H, Chen Z, Xu T. Potentially inappropriate medications in Chinese older outpatients in tertiary hospitals according to Beers criteria: a cross-sectional study. Int J Clin Pract. 2021. Aug;75(8):e14348. 10.1111/ijcp.14348 [DOI] [PubMed] [Google Scholar]
- 339.Tillekeratne LG, Bodinayake CK, Dabrera T, Nagahawatte A, Arachchi WK, Sooriyaarachchi A, et al. Antibiotic overuse for acute respiratory tract infections in Sri Lanka: a qualitative study of outpatients and their physicians. BMC Fam Pract. 2017. Mar 16;18(1):37. 10.1186/s12875-017-0619-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Tolu S, Rezvani A, Karacan İ, Buğdayci D, Küçük HC, Bucak ÖF, et al. Self-reported medication adherence in patients with ankylosing spondylitis: the role of illness perception and medication beliefs. Arch Rheumatol. 2020. Feb 7;35(4):495–505. 10.46497/ArchRheumatol.2020.7732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Torrente F, Bustin J, Triskier F, Ajzenman N, Tomio A, Mastai R, et al. Effect of a social norm email feedback program on the unnecessary prescription of nimodipine in ambulatory care of older adults: a randomized clinical trial. JAMA Netw Open. 2020. Dec 1;3(12):e2027082. 10.1001/jamanetworkopen.2020.27082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Tuhan H, Abaci A, Cicek G, Anik A, Catli G, Demir K, et al. Levothyroxine replacement in primary congenital hypothyroidism: the higher the initial dose the higher the rate of overtreatment. J Pediatr Endocrinol Metab. 2016. Feb;29(2):133–8. 10.1515/jpem-2015-0047 [DOI] [PubMed] [Google Scholar]
- 343.Tulu S, Tadesse T, Alemayehu Gube A. Assessment of antibiotic utilization pattern in treatment of acute diarrhoea diseases in Bishoftu General Hospital, Oromia Ethiopia. Adv Med. 2018. May 2;2018:2376825. 10.1155/2018/2376825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Turan O, Emre JC, Deniz S, Baysak A, Turan PA, Mirici A. Adherence to current COPD guidelines in Turkey. Expert Opin Pharmacother. 2016;17(2):153–8. 10.1517/14656566.2016.1115482 [DOI] [PubMed] [Google Scholar]
- 345.Turan PA, Turan O, Güldaval F, Anar C, Polat G, Büyükşirin M. Transitions between COPD groups: a cross-sectional study in Turkey. Respir Med. 2021. Mar;178:106310. 10.1016/j.rmed.2021.106310 [DOI] [PubMed] [Google Scholar]
- 346.Undela K, Bansal D, D’Cruz S, Sachdev A, Tiwari P. Prevalence and determinants of use of potentially inappropriate medications in elderly inpatients: a prospective study in a tertiary healthcare setting. Geriatr Gerontol Int. 2014. Apr;14(2):251–8. 10.1111/ggi.12081 [DOI] [PubMed] [Google Scholar]
- 347.Urbiztondo I, Bjerrum L, Caballero L, Suarez MA, Olinisky M, Córdoba G. Decreasing inappropriate use of antibiotics in primary care in four countries in South America-cluster randomized controlled trial. Antibiotics (Basel). 2017. Dec 14;6(4):38. 10.3390/antibiotics6040038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Valladales-Restrepo LF, Machado-Alba JE. Potentially inappropriate anticholinergic drug prescriptions for patients with Sjögren’s syndrome. J Transl Autoimmun. 2019. Jun 27;2:100007. 10.1016/j.jtauto.2019.100007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Van Heerden JA, Burger JR, Gerber JJ. Inappropriate medicine prescribing in older South africans: a cross-sectional analysis of medicine claims data. S Afr Med J. 2016. Sep 9;106(10):1010–6. 10.7196/SAMJ.2016.v106i10.10627 [DOI] [PubMed] [Google Scholar]
- 350.Varol Y, Karakurt Z, Çırak AK, Şahin HD, Kıraklı C, Kömürcüoğlu B. Inappropriate utilization of antibiotics in COPD exacerbations. Turk Thorac J. 2020. Nov;21(6):397–403. 10.5152/TurkThoracJ.2020.19074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Vatcharavongvan P, Puttawanchai V. Potentially inappropriate medications among the elderly in primary care in Thailand from three different sets of criteria. Pharm Pract (Granada). 2019. Jul-Sep;17(3):1494. 10.18549/PharmPract.2019.3.1494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Vatcharavongvan P, Puttawanchai V. Elderly patients in primary care are still at risks of receiving potentially inappropriate medications. J Prim Care Community Health. 2021. Jan-Dec;12:21501327211035088. 10.1177/21501327211035088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Venkataraman R, Rashid M, Shrestha H. Inappropriate medication use and cost comparison analysis of proton pump inhibitors: evidence from an Indian tertiary care facility. Curr Drug Saf. 2020;15(2):147–55. 10.2174/1574886315666200311120151 [DOI] [PubMed] [Google Scholar]
- 354.Vieira de Lima TJ, Garbin CA, Garbin AJ, Sumida DH, Saliba O. Potentially inappropriate medications used by the elderly: prevalence and risk factors in Brazilian care homes. BMC Geriatr. 2013. May 30;13(1):52. 10.1186/1471-2318-13-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Vigário PS, Vaisman F, Coeli CM, Ward L, Graf H, Carvalho G, et al. Inadequate levothyroxine replacement for primary hypothyroidism is associated with poor health-related quality of life-a Brazilian multicentre study. Endocrine. 2013. Oct;44(2):434–40. 10.1007/s12020-013-9886-1 [DOI] [PubMed] [Google Scholar]
- 356.Vu TX, Huong QBT. The effect of the pharmacist’s intervention on potentially inappropriate medication prescription in older adults in a Vietnamese hospital. Pharm Sci Asia. 2019;46(1):54–61. 10.29090/psa.2019.01.017.0023 [DOI] [Google Scholar]
- 357.Wang D, Liu C, Zhang X, Liu C. Identifying antibiotic prescribing patterns through multi-level latent profile analyses: a cross-sectional survey of primary care physicians. Front Pharmacol. 2020. Nov 11;11:591709. 10.3389/fphar.2020.591709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Wang F, Ma Z, Liu M, Wu X. Potentially inappropriate medications at admission and discharge in older adults: a comparison of the Beers 2019 and 2015 criteria. Int J Clin Pharmacol Ther. 2020. Jun;58(6):299–309. 10.5414/CP203638 [DOI] [PubMed] [Google Scholar]
- 359.Wang H, Zhang L, Yip W, Hsiao W. An experiment in payment reform for doctors in rural China reduced some unnecessary care but did not lower total costs. Health Aff (Millwood). 2011. Dec;30(12):2427–36. 10.1377/hlthaff.2009.0022 [DOI] [PubMed] [Google Scholar]
- 360.Wang J, Wang P, Wang X, Zheng Y, Xiao Y. Use and prescription of antibiotics in primary health care settings in China. JAMA Intern Med. 2014. Dec;174(12):1914–20. 10.1001/jamainternmed.2014.5214 [DOI] [PubMed] [Google Scholar]
- 361.Wang P, Wang Q, Li F, Bian M, Yang K. Relationship between potentially inappropriate medications and the risk of hospital readmission and death in hospitalized older patients. Clin Interv Aging. 2019. Nov 4;14:1871–8. 10.2147/CIA.S218849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Wang X, Xuan Z, Storella TH, Zhou X. Determinants of non-prescription antibiotic dispensing in Chinese community pharmacies from socio-ecological and health system perspectives. Soc Sci Med. 2020. Jul;256:113035. 10.1016/j.socscimed.2020.113035 [DOI] [PubMed] [Google Scholar]
- 363.Wei X, Zhang Z, Hicks JP, Walley JD, King R, Newell JN, et al. Long-term outcomes of an educational intervention to reduce antibiotic prescribing for childhood upper respiratory tract infections in rural China: follow-up of a cluster-randomised controlled trial. PLoS Med. 2019. Feb 5;16(2):e1002733. 10.1371/journal.pmed.1002733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Widayati A, Suryawati S, de Crespigny C, Hiller JE. Self medication with antibiotics in Yogyakarta City Indonesia: a cross sectional population-based survey. BMC Res Notes. 2011. Nov 11;4(1):491. 10.1186/1756-0500-4-491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Wijaya D, Padolo E, Ardianto C, Sumarno, Matulatan F, Alderman CP,Suharjono . Analysis of the use and cost of stress ulcer prophylaxis for surgical inpatients. J Basic Clin Physiol Pharmacol. 2020. Jan 11;30(6):/j/jbcpp.ahead-of-print/jbcpp-2019-0306/jbcpp-2019-0306.xml. 10.1515/jbcpp-2019-0306 [DOI] [PubMed] [Google Scholar]
- 366.Wulandari LPL, Khan M, Liverani M, Ferdiana A, Mashuri YA, Probandari A, et al. Prevalence and determinants of inappropriate antibiotic dispensing at private drug retail outlets in urban and rural areas of Indonesia: a mixed methods study. BMJ Glob Health. 2021. Aug;6(8):e004993. 10.1136/bmjgh-2021-004993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Xu Y, Lu J, Sun C, Wang X, Hu YJ, Zhou X. A cross-sectional study of antibiotic misuse among Chinese children in developed and less developed provinces. J Infect Dev Ctries. 2020. Feb 29;14(2):129–37. 10.3855/jidc.11938 [DOI] [PubMed] [Google Scholar]
- 368.Xue H, Shi Y, Huang L, Yi H, Zhou H, Zhou C, et al. Diagnostic ability and inappropriate antibiotic prescriptions: a quasi-experimental study of primary care providers in rural China. J Antimicrob Chemother. 2019. Jan 1;74(1):256–63. [DOI] [PubMed] [Google Scholar]
- 369.Yang L, Liu C, Wang L, Yin X, Zhang X. Public reporting improves antibiotic prescribing for upper respiratory tract infections in primary care: a matched-pair cluster-randomized trial in China. Health Res Policy Syst. 2014. Oct 10;12(1):61. 10.1186/1478-4505-12-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Yilmaz F, Colak MY. Evaluation of inappropriate medication use and compliance in elderly people. Curr Drug Saf. 2018;13(2):122–7. 10.2174/1574886313666180321120036 [DOI] [PubMed] [Google Scholar]
- 371.Yin J, Dyar OJ, Yang P, Yang D, Marrone G, Sun M, et al. Pattern of antibiotic prescribing and factors associated with it in eight village clinics in rural Shandong Province, China: a descriptive study. Trans R Soc Trop Med Hyg. 2019. Nov 1;113(11):714–21. 10.1093/trstmh/trz058 [DOI] [PubMed] [Google Scholar]
- 372.Yu X, Pang H, Xu Z, Yan H, Xu L, Du J, et al. Multicentre evaluation of perioperative red blood cells transfusions in China. Br J Anaesth. 2014. Dec;113(6):1055–6. 10.1093/bja/aeu392 [DOI] [PubMed] [Google Scholar]
- 373.Yucel A, Clark PM, Ozbay L, Yucel E. Prevalance of inappropriate medication use in elderly in a community pharmacy. Value Health. 2013;16(3):A78. 10.1016/j.jval.2013.03.355 [DOI] [Google Scholar]
- 374.Zahwe M, Skouri H, Rachidi S, Khoury M, Noureddine S, Isma’eel H, et al. Potentially inappropriate medications in elderly patients with heart failure: Beers Criteria-based study. Int J Pharm Pract. 2020. Dec;28(6):652–9. 10.1111/ijpp.12651 [DOI] [PubMed] [Google Scholar]
- 375.Zeenny R, Wakim S, Kuyumjian YM. Potentially inappropriate medications use in community-based aged patients: a cross-sectional study using 2012 Beers criteria. Clin Interv Aging. 2017. Jan 4;12:65–73. 10.2147/CIA.S87564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Zeng S, Wang D, Yan Y, Zhu M, Liu W, Gong Z, et al. Single-center analysis of the potential inappropriate use of intravenous medications in hospitalized patients in China. Clin Ther. 2019. Aug;41(8):1631–1637.e4. 10.1016/j.clinthera.2019.05.009 [DOI] [PubMed] [Google Scholar]
- 377.Zhang J, Zhang Z, Shi T. Single-center analysis of the inappropriate use of human albumin and nutritional support in hospitalized patients with hypoproteinemia in China. J Int Med Res. 2021. Mar;49(3):300060520987731. 10.1177/0300060520987731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Zhang Y, Yang H, Kong J, Liu L, Ran L, Zhang X, et al. Impact of interventions targeting the inappropriate use of proton-pump inhibitors by clinical pharmacists in a hepatobiliary surgery department. J Clin Pharm Ther. 2021. Feb;46(1):149–57. 10.1111/jcpt.13273 [DOI] [PubMed] [Google Scholar]
- 379.Zhao M, Song JX, Zheng FF, Huang L, Feng YF. Potentially inappropriate medication and associated factors among older patients with chronic coronary syndrome at hospital discharge in Beijing, China. Clin Interv Aging. 2021. Jun 9;16:1047–56. 10.2147/CIA.S305006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Zhu H, Chen Y, Hang Y, Luo H, Fang X, Xiao Y, et al. Impact of inappropriate empirical antibiotic treatment on clinical outcomes of urinary tract infections caused by Escherichia coli: a retrospective cohort study. J Glob Antimicrob Resist. 2021. Sep;26:148–53. 10.1016/j.jgar.2021.05.016 [DOI] [PubMed] [Google Scholar]
- 381.Zou XX, Fang Z, Min R, Bai X, Zhang Y, Xu D, et al. Is nationwide special campaign on antibiotic stewardship program effective on ameliorating irrational antibiotic use in China? Study on the antibiotic use of specialized hospitals in China in 2011-2012. J Huazhong Univ Sci Technolog Med Sci. 2014. Jun;34(3):456–63. 10.1007/s11596-014-1300-6 [DOI] [PubMed] [Google Scholar]
- 382.Fahrni ML, Azmy MT, Usir E, Aziz NA, Hassan Y. Inappropriate prescribing defined by STOPP and START criteria and its association with adverse drug events among hospitalized older patients: a multicentre, prospective study. PLoS One. 2019. Jul 26;14(7):e0219898. 10.1371/journal.pone.0219898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Bahat G, Ilhan B, Erdogan T, Halil M, Savas S, Ulger Z, et al. Turkish inappropriate medication use in the elderly (TIME) criteria to improve prescribing in older adults: TIME-to-STOP/TIME-to-START. Eur Geriatr Med. 2020. Jun;11(3):491–8. 10.1007/s41999-020-00297-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384.Basaran O, Dogan V, Biteker M, Beton O, Tekinalp M, Bolat I, et al. Guideline adherence of non-vitamin K antagonist oral anticoagulant therapy: results from RAMSES study. Thromb Res. 2016;141:S7–8. [Google Scholar]
- 385.Brkic J, Fialova D, Okuyan B, Kummer I, Sesto S, Capiau A, et al. Prevalence of potentially inappropriate prescribing in older adults in Central and Eastern Europe: a systematic review and synthesis without meta-analysis. Sci Rep. 2022. Oct 6;12(1):16774. 10.1038/s41598-022-19860-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Donsamak S, Weiss MC, John DN. Evaluation of antibiotic supply decisions by community pharmacists in Thailand: a vignette study. Antibiotics (Basel). 2021. Feb 3;10(2):154. 10.3390/antibiotics10020154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Ergül AB, Gökçek İ, Çelik T, Torun YA. Assessment of inappropriate antibiotic use in pediatric patients: point-prevalence study. Turk Pediatri Ars. 2018. Mar 1;53(1):17–23. 10.5152/TurkPediatriArs.2018.5644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Ndyomugyenyi R, Magnussen P, Lal S, Hansen K, Clarke SE. Appropriate targeting of artemisinin-based combination therapy by community health workers using malaria rapid diagnostic tests: findings from randomized trials in two contrasting areas of high and low malaria transmission in south-western Uganda. Trop Med Int Health. 2016. Sep;21(9):1157–70. 10.1111/tmi.12748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Hanson K, Brikci N, Erlangga D, Alebachew A, De Allegri M, Balabanova D, et al. The Lancet Global Health Commission on financing primary health care: putting people at the centre. Lancet Glob Health. 2022. May;10(5):e715–72. 10.1016/S2214-109X(22)00005-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390.Latifi N, Redberg RF, Grady D. The next frontier of less is more-from description to implementation. JAMA Intern Med. 2022. Feb 1;182(2):103–5. 10.1001/jamainternmed.2021.6908 [DOI] [PubMed] [Google Scholar]
- 391.Sulis G, Adam P, Nafade V, Gore G, Daniels B, Daftary A, et al. Antibiotic prescription practices in primary care in low- and middle-income countries: a systematic review and meta-analysis. PLoS Med. 2020. Jun 16;17(6):e1003139. 10.1371/journal.pmed.1003139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Jacobs TG, Robertson J, van den Ham HA, Iwamoto K, Bak Pedersen H, Mantel-Teeuwisse AK. Assessing the impact of law enforcement to reduce over-the-counter (OTC) sales of antibiotics in low- and middle-income countries; a systematic literature review. BMC Health Serv Res. 2019. Jul 31;19(1):536. 10.1186/s12913-019-4359-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Pierce J, Apisarnthanarak A, Schellack N, Cornistein W, Maani AA, Adnan S, et al. Global antimicrobial stewardship with a focus on low- and middle-income countries. Int J Infect Dis. 2020. Jul;96:621–9. 10.1016/j.ijid.2020.05.126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394.Eibs T, Koscalova A, Nair M, Grohma P, Kohler G, Bakhit RG, et al. Qualitative study of antibiotic prescription patterns and associated drivers in Sudan, Guinea-Bissau, Central African Republic and Democratic Republic of Congo. BMJ Open. 2020. Sep 24;10(9):e036530. 10.1136/bmjopen-2019-036530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Do NTT, Ta NTD, Tran NTH, Than HM, Vu BTN, Hoang LB, et al. Point-of-care C-reactive protein testing to reduce inappropriate use of antibiotics for non-severe acute respiratory infections in Vietnamese primary health care: a randomised controlled trial. Lancet Glob Health. 2016. Sep;4(9):e633–41. 10.1016/S2214-109X(16)30142-5 [DOI] [PMC free article] [PubMed] [Google Scholar]