Recent advances in technical aspects and surgical techniques have made anatomical endoscopic enucleation of the prostate (AEEP) a much more attractive surgical option for the treatment of benign prostatic obstruction (BPO). Technological improvements such as fast morcellators, slimmer scopes [1], and new energy sources that offer better hemostasis have helped AEEP to evolve to become a much faster surgical procedure that can be even performed in an ambulatory setting [2], [3]. In addition, a better understanding of the endoscopic anatomy of the sphincter [4] and ejaculatory mechanism [5] is reducing the morbidity classically attributed to the procedure, making it more attractive for patients, urologists, and hospitals.
AEEP is rapidly gaining in popularity around the world. Logically, centers that are considering adoption of this technique wonder what tool to choose, as there is now evidence that the good results with AEEP are driven mainly by the anatomical completeness of removal of the adenoma rather than by the energy source used (enucleation is enucleation) [6].
Despite the feasibility of performing AEEP with various energy sources, their different physical properties in their interaction with prostatic tissue might result in substantial differences in the ability to develop and remain in the correct plane of dissection and the quality of first-pass hemostasis, which can in turn potentially influence critical clinical parameters such as intraoperative visibility, ease of learning, surgical procedure time, catheterization time, safety, and ability to perform the procedure as a day case [3].
The holmium laser was introduced in urology in 1992 and is currently the most widely used laser worldwide. It is versatile, as it allows for the treatment of stone disease, strictures, urothelial tumors and bladder outlet obstruction, with substantial scientific evidence supporting its use to treat these conditions, especially stones and benign prostatic hyperplasia.
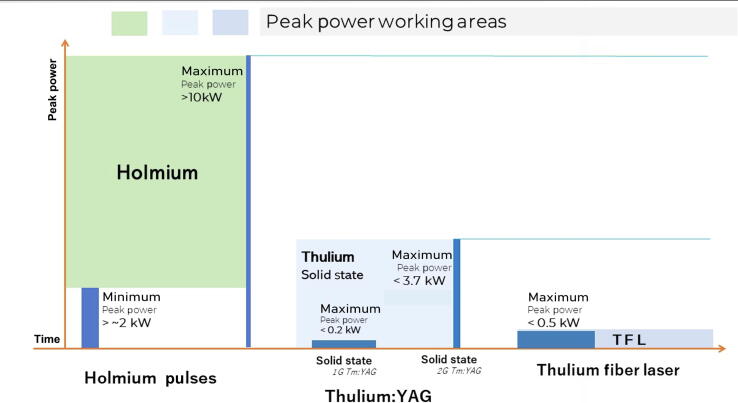
The holmium laser emits pulses at 2100 nm with very high peak power of ∼10 kW (peak power = pulse power/pulse duration), which can also be defined as the maximum instantaneous optical power output by the laser (Fig. 1). Owing to the affinity of water for this wavelength, the pulse violently heats the water medium so that a cavitation bubble is formed, emitting a shockwave and exerting local pressure. When this bubble and the accompanying shockwave are pointed at the interface between the surgical capsule and the adenoma, they behave similarly to two scissor blades opening between the two layers, dissecting the virtual plane and thus helping urologists to perform enucleation following the actual anatomical plane [7] (Table 1). Holmium laser in regular mode has a good dissection effect during enucleation, but with irregular and suboptimal coagulation. Thulium fiber laser (TFL) produce bubbles that are four times smaller owing to its lower peak power (up to 3.7 kW) [8] and tenfold lower local pressure in comparison to Ho:YAG; its effect would be more similar to a surgical blade, which cuts very well, but does not particularly help in dissecting the anatomical plane, and might actually facilitate cutting out of the plane [9].
Fig. 1.
Schematic representation of pulses, peak power, and the working area of holmium and thulium lasers. The peak power and working area are considerably greater for holmium than for thulium. 1G = first-generation; 2G = second-generation.
Table 1.
Effect of different lasers on tissue when performing anatomical endoscopic enucleation of the prostate
| Characteristic | ThuLEP-ThuVEP (Tm:YAG, old TFL) | ThuFLEP-SoLEP (SP-TFL) | HoLEP with short pulse | HoLEP with pulse modulationa |
|---|---|---|---|---|
| Shockwave dissection | Absent | Low effect | High effect | Medium effect |
| Tissue color | Charring (brown/dark) | White-light brown | White | White-light brown |
| Distance from tissue | Contact | Contact/near contact | Near contact/distance | Near contact/distance |
| Hemostatic capability | Very good | Very good | Good | Very good |
| Cutting properties | Excellent | Excellent | Good | Very good |
HoLEP = holmium LEP; LEP = laser enucleation of the prostate; SoLEP = SOLTIVE (Olympus, Hamburg, Germany) LEP; SP = superpulsed; TFL = thulium fiber laser; ThuFLEP = thulium fiber LAP; ThuLEP = thulium LEP; ThuVEP = thulium vapor enucleation of the prostate.
Pulse modulation = Virtual Basket (Quanta System) or MOSES (Boston Scientific).
A contemporary sophistication of the holmium laser has been the development of pulse modulation (MOSES, Boston Scientific, Marlborough, MA, USA; Virtual Basket, Quanta System, Samarate, Italy) [10], [11], [12], in which two consecutive rapid pulses are emitted. The first pulse interacts with water, generating violent deposition of heat and a cavitation bubble accompanied by a pressure wave, while the second pulse travels through the bubble and interacts with water over a greater distance than when a single pulse is emitted. This makes it possible to preserve the excellent dissection properties with the first pulse and improve the coagulation and cutting effect with the second pulse (Table 1). This translates into a better balance between dissection and coagulation, improving first-pass hemostasis, visibility, ablation efficiency, and surgical time, and reducing surgeon stress [13], [14].
The efficiency of a laser enucleation procedure relies on various factors, including surgeon experience, energy source, water flow, scope size, and smooth movements (or not as soft during mechanical dissection with the endoscope tip), as well as characteristics related to the laser and its interaction with the tissue, such as the peak power, shape, bubble size, working distance, wavelength, and absorption coefficient. Undoubtedly, the most outstanding feature of the holmium laser for enucleation is in aiding the surgeon in dissecting the anatomical plane owing to its high peak power (Fig. 1) [15], [16], which is much higher than that of thulium, pulsed thulium, and TFL lasers.
There is scarce evidence comparing holmium and thulium fiber laser enucleation (HoLEP and ThuFLEP). Both ThuFLEP and HoLEP are efficient ways of treating BPO and showed no apparent differences in functional outcomes in a recent study [17].
However, after using all of the laser types for prostate enucleation in our institution, our feeling is that the holmium laser facilitates staying in the anatomical plane more efficiently thanks to the effect described. Thulium, pulsed thulium, and TFL lasers provide excellent hemostasis; they have a significant cutting effect, with an even thin layer of coagulation and charring of the tissue, making the dissection in the proper plane less intuitive.
Of course, a seasoned surgeon can perform enucleation with all the laser sources mentioned and achieve excellent results, and gaining surgical experience with a particular wavelength allows surgeons to compensate for the differences in tissue effects and dissection versus cutting of the different lasers.
It also seems clear that the classic thulium and single-pulse holmium lasers have been significantly improved with the newer generation of thulium-based and pulse-modulation holmium lasers. These more recent lasers undoubtedly represent a significant leap forward in the features we need to perform AEEP safely and more efficiently and are already contributing to boosting interest in and adoption of this excellent surgical technique.
There is still not enough evidence to say that one laser is the best; large, randomized studies are needed to compare if there is a winner in providing measurable clinical advantages for surgeons, patients, or hospitals.
The new pulse-modulation holmium lasers are already delivering clinical advantages, with shorter surgical times, lower complication rates, easier learning curves, economic savings, and daycare possibilities, so we can confidently say, long live holmium!
Conflicts of interest: Fernando Gómez Sancha is a consultant for Lumenis, Quanta System, and Lisa Laser. The remaining authors have nothing to disclose.
Associate Editor: Véronique Phé
References
- 1.Figueiredo F.C.A., Cracco C.M., Marins R.L., Scoffone C.M. Holmium laser enucleation of the prostate: problem-based evolution of the technique. Andrologia. 2020;52:e13582. doi: 10.1111/and.13582. [DOI] [PubMed] [Google Scholar]
- 2.Large T., Nottingham C., Stoughton C., Williams J., Krambeck A. Comparative study of holmium laser enucleation of the prostate with MOSES enabled pulsed laser modulation. Urology. 2020;136:196–201. doi: 10.1016/j.urology.2019.11.029. [DOI] [PubMed] [Google Scholar]
- 3.Agarwal D.K., Large T., Tong Y., et al. Same day discharge is a successful approach for the majority of patients undergoing holmium laser enucleation of the prostate. Eur Urol Focus. 2022;8:228–234. doi: 10.1016/j.euf.2020.12.018. [DOI] [PubMed] [Google Scholar]
- 4.Saitta G., Becerra J.E.A., Del Álamo J.F., et al. “En bloc” HoLEP with early apical release in men with benign prostatic hyperplasia. World J Urol. 2019;37:2451–2458. doi: 10.1007/s00345-019-02671-4. [DOI] [PubMed] [Google Scholar]
- 5.Bozzini G., Berti L., Maltagliati M., et al. Ejaculation-sparing thulium laser enucleation of the prostate (ES-ThuLEP): outcomes on a large cohort. World J Urol. 2021;39:2029–2035. doi: 10.1007/s00345-020-03442-2. [DOI] [PubMed] [Google Scholar]
- 6.Herrmann T.R.W. Enucleation is enucleation is enucleation is enucleation. World J Urol. 2016;34:1353–1355. doi: 10.1007/s00345-016-1922-3. [DOI] [PubMed] [Google Scholar]
- 7.Piesche S., Keller H. MP26-16 The “scalpel and scissors effect” using infrared lasers – visiualisation of a principle and deduction of operative consequences in transurethral prostate enucleation. J Endourol. 2015;29:A200. doi: 10.1089/end.2015.29003.abstracts. [DOI] [Google Scholar]
- 8.Petzold R., Miernik A., Suarez-Ibarrola R. In vitro dusting performance of a new solid state thulium laser compared to holmium laser lithotripsy. J Endourol. 2021;35:221–225. doi: 10.1089/end.2020.0525. [DOI] [PubMed] [Google Scholar]
- 9.Martov A.G., Ergakov D.V., Guseynov M., Andronov A.S., Plekhanova O.A. Clinical comparison of super pulse thulium fiber laser and high-power holmium laser for ureteral stone management. J Endourol. 2021;35:795–800. doi: 10.1089/end.2020.0581. [DOI] [PubMed] [Google Scholar]
- 10.Rodríguez Socarrás M.E., Llanes González L., Reinoso J., et al. Pulse modulation for holmium laser: Vapor Tunnel-Virtual Basket–Bubble Blast. Videourology. 2020;34 doi: 10.1089/vid.2020.0018. [DOI] [Google Scholar]
- 11.Elhilali M.M., Badaan S., Ibrahim A., Andonian S. Use of the Moses technology to improve holmium laser lithotripsy outcomes: a preclinical study. J Endourol. 2017;31:598–604. doi: 10.1089/end.2017.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bozzini G., Maltagliati M., Besana U., et al. Holmium laser enucleation of the prostate with Virtual Basket mode: faster and better control on bleeding. BMC Urol. 2021;21:28. doi: 10.1186/s12894-021-00797-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nevo A., Faraj K.S., Cheney S.M., et al. Holmium laser enucleation of the prostate using Moses 2.0 vs non-Moses: a randomised controlled trial. BJU Int. 2021;127:553–559. doi: 10.1111/bju.15265. [DOI] [PubMed] [Google Scholar]
- 14.Assmus M.A., Ganesh M.B., Lee M.S., Large T., Krambeck A.E. Contemporary outcomes for patients undergoing concurrent surgeries at the time of holmium laser enucleation of the prostate before and after Moses 2.0 BPH mode. J Endourol. 2021;35:S8–S. doi: 10.1089/end.2021.0531. [DOI] [PubMed] [Google Scholar]
- 15.Levin B.A., Aldoukhi A.H., Black K.M., Hall T.L., Roberts W.W., Ghani K.R. Burnback: the role of pulse duration and energy on fiber-tip degradation during high-power laser lithotripsy. Lasers Med Sci. 2021;36:1817–1822. doi: 10.1007/s10103-020-03199-5. [DOI] [PubMed] [Google Scholar]
- 16.Ventimiglia E., Villa L., Doizi S., et al. Laser lithotripsy: the importance of peak power and pulse modulation. Eur Urol Focus. 2021;7:22–25. doi: 10.1016/j.euf.2021.01.012. [DOI] [PubMed] [Google Scholar]
- 17.Enikeev D., Taratkin M., Babaevskaya D., et al. Randomized prospective trial of the severity of irritative symptoms after HoLEP vs ThuFLEP. World J Urol. 2022;40:2047–2053. doi: 10.1007/s00345-022-04046-8. [DOI] [PubMed] [Google Scholar]