Abstract
Background
Permanent hair dye is the most commonly used anti‐aging procedure used by both men and women. However, permanent hair dye can cause irritant contact dermatitis due to ammonia and allergic contact dermatitis due to paraphylenediamine (PPD).
Methods
This research examined an ammonia‐free and PPD‐free permanent hair dye in 50 ethnically diverse females 21–91 years of age who were current users of permanent hair dyes. Subjects were patch tested prior to dyeing. Two dye sessions were undertaken at baseline and 2–6 weeks post‐baseline depending on the dyeing habits of the subject.
Results
50/50 subjects successfully completed the study with no incidence of allergic or irritant contact dermatitis. After 2 dyeing procedures, the dermatologists rated an 87% improvement in hair shine, 90% improvement in hair color, 88% improvement in hair moisturization, 87% improvement in hair porosity, and 88% improvement in hair combability.
Conclusions
A MEA‐based ammonia‐free cream hair color without PPD or resorcinol was safe for use on the hair and scalp of females with diverse hair types and textures.
Keywords: allergic contact dermatitis, MEA, monoethanolamine, permanent hair dye
1. INTRODUCTION
Permanent hair dyeing is a commonly practiced procedure to cover gray hair and obtain hair shades different from the natural hair color of the individual. Traditional permanent hair dyeing can improve the cosmetic appearance of the hair, but has been associated with complaints of damage to the hair shaft and weakening of its mechanical properties. Carefully formulated permanent hair dyes can decrease hair damage while producing the hair color desired by the consumer.
Permanent hair dyes utilize oxidative chemistry requiring the initiation of a chemical reaction by mixing chemicals just prior to application. These dyes typically contain 6%–9% hydrogen peroxide and ammonia as an alkalizing agent to increase the pH of the final product. 1 This allows the hair dye to penetrate the cuticle and cortex, but also can produce hair shaft damage and scalp irritation and a pungent smell. This research examined a unique type of permanent hair dye without ammonia. The ammonia was replaced with monoethanolamine (MEA), which possesses less odor and may be less irritating. MEA still allows the hair dye to penetrate through the cuticle to the cortex. 2
Another problem with traditional permanent hair dyes is the possibility of allergic contact dermatitis to paraphenylenediamene (PPD). 3 PPD is used in many permanent hair dyes as a dye precursor in most black, brown, and blonde shades. The present study investigated whether an alternatively formulated, MEA‐based ammonia‐free permanent cream hair dye without PPD resulted in less hair damage. The safety‐in‐use, efficacy, and hair compatibility were assessed by a board‐certified dermatologist and licensed cosmetologist along with consumer perceptions in women with all colors and textures of hair.
2. METHODS
Fifty female subjects 18+ years of age across a diverse range of hair types, hair colors, ethnicities, hair shape (straight, wavy, curly, super curly, natural African American), Fitzpatrick skin types, and amounts of gray hair up to 75% were enrolled in this single site IRB approved (Allendale Institutional Review Board [AIRB], Old Lyme, CT) study to evaluate the safety and efficacy of a permanent MEA‐based hair dye system. Subjects were recruited from the database of the research center (Dermatology Consulting Services, PLLC, High Point, NC). Subjects who signed an IRB‐approved consent and were not pregnant or lactating were enrolled. All subjects were permanent hair dye users and had dyed their hair in the preceding 6 months. Subjects also agreed not to dye their hair or have any other chemical hair procedures performed during the study. An assessment was made by the dermatologist investigator of the hair history of each subject to ensure her appropriateness for study entry. No subjects with hair loss or other medical scalp or hair disorders were allowed in the study. No scalp medications were permitted. Subjects were not allowed to color their hair within 2 weeks of study entry or swim more than twice weekly.
Subjects were dispensed a shampoo and conditioner (Madison Reed, California) to use for at least 1 week prior to hair dyeing. Subjects picked out their desired hair shade from 56 shades available on a consumer website. The manufacturer provided the desired hair color (Madison Reed, California) to the research center.
Subjects returned to the research center for patch testing to minimize the incidence of allergic contact dermatitis, even though the test hair dye was PPD‐free. A small amount of hair dye was mixed following the hair dye instructions and applied to the neck at the hairline. Subjects returned to the research center in 48 h for patch test reading by the board‐certified dermatologist. If the patch test was positive, the subject was not enrolled in the study. If the patch test was negative, subjects continued on to baseline.
At baseline, the dermatologist investigator, subjects, and licensed cosmetologist completed a scalp health and safety assessment. The dermatologist and cosmetologist assessed scalp redness, irritation, flaking, dryness, and swelling on a 5‐point ordinal scale (0 = none, 1 = minimal, 2 = mild, 3 = moderate, and 4 = severe). The subjects assessed scalp stinging, burning, itching, irritation, flaking, and dryness on the same 5‐point ordinal scale. In addition, an assessment was made of hair appearance by the investigator, cosmetologist, and subjects to include lack of hair shine, lack of hair color vibrancy, lack of hair moisturization, hair porosity, and hair combability on the same 5‐point ordinal scale. Finally, the dermatologist assessed hair performance in terms of hair shed, hair fall, and hair breakage by combing the hair and visually examining shed hairs. The loose hair removed by combing was collected and evaluated by the dermatologist investigator under the microscope for any structural abnormalities.
Following the baseline assessments, subjects underwent the permanent hair dye procedure and drying/styling by the licensed cosmetologist. Color was applied and processed at the roots for 35 min and pulled through the lengths and ends of the hair for the last 5 min. The subjects, cosmetologist, and dermatologist completed a post‐dyeing scalp health and safety assessment along with a hair appearance assessment. The dermatologist combed the subject's hair and evaluated loose hairs for structural changes, hair loss, and hair breakage after dyeing. The subjects were asked to continue using the provided shampoo and conditioner for the next 2–6 weeks until they returned to the research center for a second dyeing procedure when root show was sufficient for redyeing. The second dyeing procedure occurred 2–6 weeks after the first dyeing procedure.
Prior to the second dyeing procedure, a second patch test was performed using the same technique previously described. If the patch test was positive, the subject was released from their study participation. If the patch test was negative, subjects completed their hair assessment and second study dye procedure. The dermatologist investigator, subjects, and cosmetologist completed the same scalp health and safety assessment and hair appearance assessment prior to the second dyeing procedure. The licensed cosmetologist performed the second hair dyeing procedure using the same hair dye as the first dyeing procedure and dried/styled the hair.
Following the second dyeing procedure, the dermatologist investigator, subjects, and cosmetologist completed the same assessments as previously detailed. The subjects were asked to continue using the provided shampoo and conditioner for the next week. One week after the second dyeing procedure, the dermatologist investigator, subjects, and cosmetologist completed the same assessments and the subjects completed their study participation.
Along with descriptive statistics, investigator, cosmetologist, and subject ordinal nonparametric data were analyzed using the Wilcoxon signed rank test. Change was considered significant at a p value of less than or equal to 0.05.
3. RESULTS
50/50 subjects successfully completed the study. A diverse population of females was enrolled with ages 21–91 years to include 1 Hispanic, 1 American Indian, 2 Asians, 7 African Americans, and 39 Caucasians.
The licensed cosmetologist rated statistically significant (p < 0.001) hair appearance improvement in all criteria and at all time points after the first hair dyeing procedure (Figure 1A). No tolerability or safety issues were identified at any time during the study by the cosmetologist.
FIGURE 1.
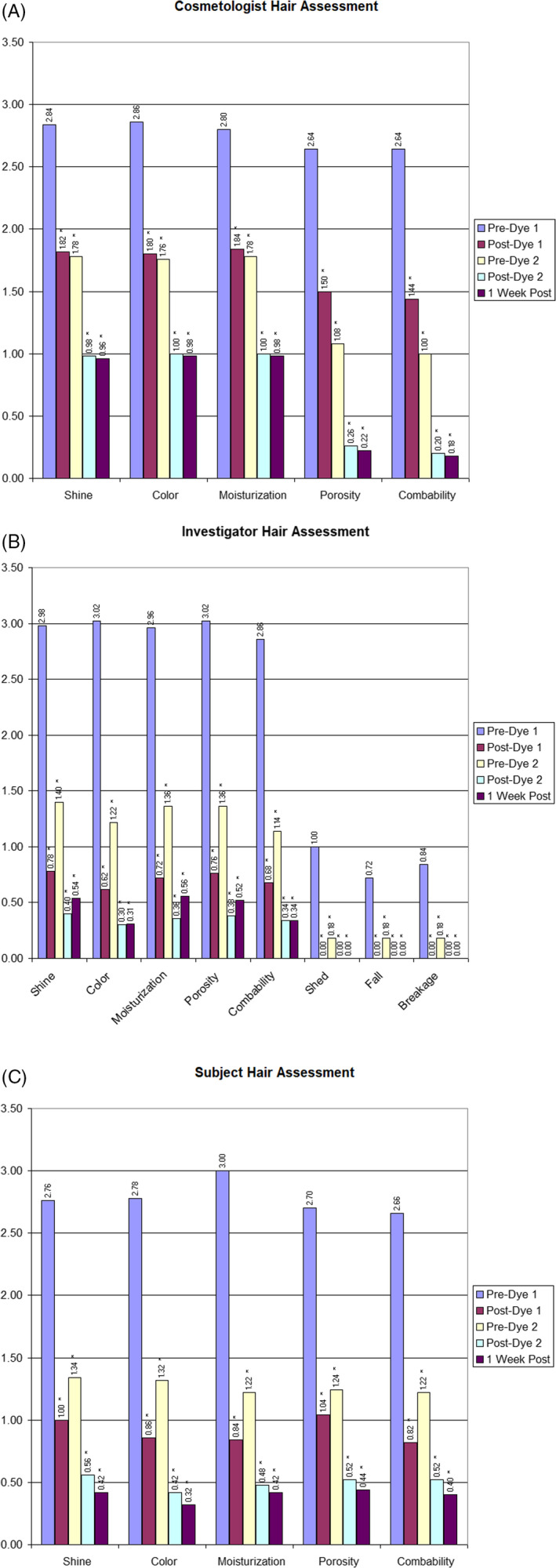
Hair assessments for each criteria at each of the time points are presented. All data points are statistically significant as compared to baseline. (A) Cosmetologist Hair Assessments. (B) Dermatologist Hair Assessments. (C) Subject Hair Assessments
The dermatologist investigator findings mirrored the cosmetologist findings, noting a statistically significant improvement at all time points in all parameters (Figure 1B). These findings indicate the hair dye improved the condition of the hair. The scalp, hairline, ears, neck, and forehead were examined, and no tolerability or safety issues were noted.
The subjects rated highly statistically significant (p < 0.001) perceived improvement in all parameters at all assessment times as compared to baseline (Figure 1C). The improvement was continuous and cumulative throughout the study. After the second hair dyeing procedure, improvement continued. Thus, rather than damaging the hair, the subjects felt the two hair coloring procedures actually improved the performance of their hair. No tolerability issues were identified by the subjects.
The dermatologist did not note any issues with hair shed, hair fall, hair breakage, or structural abnormalities by combing the hair and visually examining shed hairs with and without microscope magnification.
4. DISCUSSION
Permanent hair dyeing can damage the hair shafts if a poorly formulated product is improperly applied to the hair. 4 Two chemical processes occur during permanent hair dye. First, oxidation of the melanin pigment occurs, lightening the natural hair color. Second, oxidation of the dye precursors forms the actual colored chromophores that impart the new hair color. Only chromophores retained within the hair shaft are permanent; the rest are washed away following dye application. Thus, the dye precursors must diffuse into the hair and the oxidation reaction must occur based on hydrogen peroxide oxidation of the dye precursors, also known as intermediates. These intermediates are typically p‐diames and p‐aminophenols. The permanent dye studied did not contain PPD, but rather toluene‐2,5‐diamine sulfate (PTD).
All permanent hair dyes contain primary intermediates, which are oxidized by hydrogen peroxide and produce reactive species, which in turn react with couplers to produce dye molecules. Most permanent hair dye products use PPD as the primary intermediate; however, the study hair dye utilized PTD as the primary intermediate. Coupling agents or color couplers are also essential to permanent hair dyes. Couplers react with primary intermediates in the presence of hydrogen peroxide to produce dye molecules. Permanent hair dye formulations typically contain a mix of coupling agents. Primary intermediates can, in some cases, couple to themselves to produce coloration. Self‐coupling of a primary intermediate is undesirable and when the primary intermediate is PPD, self‐coupling increases the risk of an allergic reaction. 5 To minimize such risk, PTD was used in the study hair dye because it is less prone to self‐coupling. Moreover, the study hair dye was formulated with coupler excess to inhibit PTD self‐coupling.
The permanent hair dye process is optimal at an alkaline pH. A raised pH causes the hair cuticle to swell thereby enabling hydrogen peroxide and primary intermediates to pass into the hair cortex. 6 Ammonia is often used in hair dye formulations as the alkaline agent; however, the study hair dye used MEA to create an alkaline pH inducing less hair damage.
Consumer purchased permanent hair dyes are sold as two component kits. One component, which is the colorant, contains the dye precursor and an alkalizer, such as ammonia; however, the study hair dye reduced hair shaft damage by employing the gentler MEA. MEA‐based hair dyes have been sold to consumers for over two decades without safety issues. The dye precursor and alkalizer are contained in a surfactant base, such as cocamidopropyl betaine, which is a mild surfactant to minimize hair shaft damage. The other component, known as the developer, contains a stabilized solution of hydrogen peroxide. The two components are mixed immediately prior to dyeing and applied to the hair.
In most cases, the two liquid components are mixed. In the case of the study dye, the colorant was a cream. The cream creates a barrier on the scalp to minimize irritation and provide hair conditioning benefits, thus reducing mechanical stress and subsequent hair breakage. The cream consistency stays in place on the area of new root outgrowth and does not drip, minimizing dye contact with previously dyed hair. Less hair damage occurs if the dye is only applied to new growth as redyeing previously dyed hair causes cumulative damage.
The study hair dye was successful in reducing scalp irritation, as the cosmetologist, dermatologist, and subjects assessed no tolerability issues. Improvements in hair shine, hair color, hair moisturization, decrease in hair porosity, and improvement in hair combability were noted. Hair shine refers to the light reflection from the hair shafts and correlates with an intact cuticle while hair color refers to the ability of the dye to reach the cortex. Hair moisturization refers to how frizzy the hair appears, which can be related to the porosity or holes in the cuticle allowing humidity to enter the hair shaft and create frizz. Finally, combability refers to how easy it is to pull a comb through the hair indirectly assessing friction. Hair with a damaged cuticle will snag and snarl when combined from increased friction due to an uplifted cuticle. Damage from permanent hair dye should be minimized, which was achieved with the study hair dye formulation.
Hair dye is one of the most successful and commonly used anti‐aging cosmetic procedures. The ability to recolor gray hair in an hour and return to a more youthful or more desirable hair color is appealing. Permanent hair dyes are used by men and women of all ages sometimes to cover gray hairs and other times to create a new hair color for personal preference. The goal is to create the new color without unnecessarily damaging the hair shaft. The study hair dye was not observed by the dermatologist to increase hair shedding, falling, or breakage. Thus, safety was established allowing this important anti‐aging procedure to improve the cosmetic appearance of the hair without excessive structural damage.
4.1. Summary
A MEA‐based ammonia‐free cream hair color without PPD or resorcinol was safe for use on the scalp and hair of females with a diverse representation of hair types and textures. The permanent hair dye did not precipitate hair loss or shed, did not increase hair fall, and did not increase hair breakage.
CONFLICT OF INTEREST
Zoe Diana Draelos, MD, received an educational grant from Madison Reed to conduct the research detailed in this manuscript.
ETHICAL APPROVAL
This research was IRB approved by the Allendale Institutional Review Board, Old Lyme, CT. All subjects were consented prior to study entry. The study was conducted in accordance with Good Clinical Practices for studies involving human subjects.
Draelos ZD. A clinical evaluation of a permanent hair dye designed to reduce allergic contact dermatitis and hair damage. J Cosmet Dermatol. 2022;21:3925‐3928. doi: 10.1111/jocd.15212
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Jachowicz J. Hair damage and attempts to its repair. J Soc Cosmet Chem. 1987;38:326‐386. [Google Scholar]
- 2. Aprecida da Franca S, Dario MR, Esteves VB, Baby AR, Velasco MVR. Types of hair dye and their mechanism of action. Cosmet. 2015;2:110‐126. [Google Scholar]
- 3. DeLeo V. p‐Phenylenediamine. Dermatitis. 2006;17:53‐55. [PubMed] [Google Scholar]
- 4. Schlatter H, Long T, Gray J. An overview of hair dye safety. J Cosmet Dermatol. 2007;6:32‐36. [Google Scholar]
- 5. Schnuch A, Lessmann H, Prosch PJ, Uter W. Para‐phenylenediamine: the profie of an important allergen. Results of the IVDK. Br J Dermatol. 2006;159(2):379‐386. [DOI] [PubMed] [Google Scholar]
- 6. Takada I, Nakamura A, Matsua N, Inoue A, Someya K, Shimogaki H. Influence of oxidative and/or reductive treatment on human hair I: analysis of hair damage after oxidative and/or reductive treatment. J Oleo Sci. 2003;52:541‐548. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


