Abstract
Background
Cutaneous melanomas are common cancers in white‐skinned populations, and early detection is promoted as a means of reducing morbidity and mortality. There is concern that increased skin screening is leading to overdiagnosis of indolent melanomas with low risk of lethality. The extent of melanoma overdiagnosis associated with screening is unknown.
Objectives
To estimate possible overdiagnosis by comparing subsequent melanoma incidence and biopsy rates among people subjected to skin screening those who were not.
Methods
We recruited 43 762 residents of Queensland, Australia, aged 40–69 years, with no prior history of melanoma, selected at random from a population register in 2010. At baseline, participants completed a comprehensive melanoma risk factor survey and were asked if their skin had been examined by a doctor in the 3 years prior to baseline. We calculated incidence and relative risk of histologically confirmed melanoma (invasive and in situ) in years 2–7 of follow‐up, obtained through linkage to the cancer registry. In secondary analyses, we measured biopsy rates in years 2–6 of follow‐up. We used propensity score analysis to calculate adjusted hazard ratios (aHRs) and 95% confidence intervals (CIs).
Results
In total, 28 155 participants underwent skin screening prior to baseline. We observed 967 first‐incident melanomas (381 invasive) during 197 191 person‐years of follow‐up. Those screened had higher rates of melanoma (aHR 1·29, 95% CI 1·02–1·63) and subsequent skin biopses (aHR 1·85, 95% CI 1·69–2·04) than unscreened participants. The higher risk associated with skin screening was evident for in situ melanoma (aHR 1·45, 95% CI 1·09–1·92) but not invasive melanoma (aHR 1·05, 95% CI 0·72–1·54). In secondary analyses, where screening was defined as having a skin biopsy in the first year after baseline, we observed significantly increased risks of melanoma (aHR 1·53, 95% CI 1·23–1·89) and subsequent biopsies (aHR 2·64, 95% CI 2·46–2·84) relative to those who did not have a biopsy.
Conclusions
People who undergo skin screening subsequently experience higher rates of biopsies and melanoma (especially in situ melanoma), even after adjusting for all known risk factors, consistent with overdiagnosis.
What is already known about this topic?
Cutaneous melanomas are common cancers in white‐skinned populations for which early detection is promoted as a means of reducing morbidity and mortality.
There is concern that increased surveillance is leading to the overdiagnosis of indolent melanomas that are not destined to be lethal.
The extent of melanoma overdiagnosis associated with surveillance is not known.
What does this study add?
People subjected to skin examinations by a doctor or who undergo skin biopsies subsequently have higher numbers of biopsies and higher rates of melanoma than people not subjected to either, even after adjusting for all known risk factors.
These findings suggest that heightened surveillance leads to a proportion of melanomas being diagnosed that otherwise may not have come to clinical attention.
Melanoma is a common cancer, for which skin examinations are promoted as an early detection tool. In a large, prospective cohort, we documented the incidence of melanoma among people who had and had not been screened. Melanoma incidence was about 29% higher in the screened group over more than 5 years of follow‐up, suggesting possible overdiagnosis among people undergoing skin examinations.
Linked Comment: K.J.L. Bell and T. Nijsten. Br J Dermatol 2022; 187:459–460.
Plain language summary available online
Cutaneous melanoma is a common and typically highly visible cancer, the incidence of which has been rising rapidly in many populations. 1 Melanoma survival is correlated inversely with tumour thickness. Early detection is promoted as a compelling strategy for reducing the burden of melanoma; 2 , 3 however, early‐detection programmes provide benefit only if they reduce morbidity or mortality from this disease. To date, Germany is the only country in which a population‐based programme has been introduced for the early detection of melanoma and other skin cancers, although it remains an open question whether or not the programme has delivered mortality benefits. 4 While there is no systematic programme for the early detection of melanoma in Australia, whole‐body skin examinations are commonly offered by primary care physicians, 5 and there are many medical practitioners whose sole clinical activity is ‘skin cancer detection and treatment’. 6 As such, a sizeable proportion of the Australian population undergoes regular screening for melanoma and skin cancer each year. 7
There is concern that increased diagnostic scrutiny (including frequent skin examinations, more biopsies and shifts in pathological thresholds) is leading to the detection of indolent melanomas that would not otherwise have come to clinical attention during the lifespan of the patient, a phenomenon described as the ‘cycle of melanoma overdiagnosis’. 8 Overdiagnosis leads to overtreatment, patient harm and inflated costs. In oncology, the strongest evidence for the existence of overdiagnosis comes from long‐term follow‐up of randomized controlled trials comparing cancer incidence and mortality among participants randomized to screening vs. no screening. Although a pilot trial for melanoma screening has been executed successfully, 9 no large‐scale trials with long‐term mortality follow‐up have yet been conducted, so indirect approaches have been taken to estimate the proportion of melanomas potentially overdiagnosed. For example, descriptive epidemiological analyses using administrative data suggest that up to 50% of melanomas detected may reflect overdiagnosis of otherwise indolent lesions. 8 , 10 , 11 , 12 While informative, investigations based on aggregate rather than individual‐level data can be difficult to interpret because they do not consider a person’s inherent risk of melanoma, and they cannot compare melanoma incidence among people exposed to screening or not.
To examine the impact of diagnostic scrutiny on melanoma incidence, we took advantage of a prospective cohort study that was established to explore the incidence and clinical course of cancers of the skin. We hypothesized that patients who underwent screening for melanoma prior to recruitment would subsequently experience higher rates of skin biopsies and melanomas than those who were not screened. We operationalized the screening exposure by categorizing as screened those who had had a skin examination prior to baseline (primary analysis) or a skin biopsy in the first year of follow‐up (secondary analysis).
Patients and methods
Participants
The QSkin Study comprises a prospective cohort of 43 762 men and women aged 40–69 years in 2010–11, randomly selected from a population register (full details of recruitment have been reported previously). 13 The study was approved by the Human Research Ethics Committee of the QIMR Berghofer Medical Research Institute (protocol number P1309). Patients or the public were not involved in the design, conduct, reporting or dissemination plans. All participants gave written or online consent to take part in the study and consented to their files being linked to the Queensland Cancer Registry; 40 438 (92·4%) further consented to linkage to the Medicare Benefits Schedule (MBS) supplied by Services Australia, which provides billing information for consultations and medical procedures that are provided to citizens and permanent residents of Australia outside public hospitals. We excluded 1817 participants with a confirmed diagnosis of melanoma prior to enrolment and 166 who were diagnosed with melanoma within 1 year of enrolment. After restricting to those of white European ancestry, the final cohort for the primary exposure analysis (from baseline survey data) comprised 38 682 melanoma‐free participants; the cohort for the secondary exposure analysis (from linked MBS data) comprised 35 825 participants (Figure S1; see Supporting Information).
At baseline, participants completed a risk factor survey (https://www.qimrberghofer.edu.au/qskin2‐research/) with high repeatability for most items. 14 , 15 The survey elicited information on risk factors for melanoma, including age, sex, education, ethnicity, place of birth (Australia/other), latitude of place of birth (< ±45°, ≥ ±45°), health insurance cover, phenotypic factors (eye, hair and unexposed skin colour; skin burning tendency and tanning ability; freckling density and naevus burden at 21 years of age), measures of sun exposure (sunburns as a child/teenager/adult, cumulative lifetime sun exposure), use of tanning beds, use of sun protection (sunscreen, hats), past medical history (number of skin cancers excised surgically, number of actinic skin lesions treated destructively, family history of melanoma), self‐assessed probability of developing melanoma, smoking status and alcohol consumption. We calculated the clinical risk score for each participant using our previously validated algorithm, categorized at the median as high vs. low risk. 16
Skin screening measures
The primary measure of skin cancer screening was the self‐reported skin examination by a doctor in the 3 years prior to enrolment (categorized as binary yes/no for analysis), a measure with good agreement on repeat testing [κ = 0·64, 95% confidence interval (CI) 0·53–0·75]. 14 We defined a second measure of skin screening as the occurrence of one or more skin biopsies during the first year of follow‐up, obtained through linkage to the MBS dataset (item 30071). We did not have consent to collect MBS data for the period prior to enrolment.
Outcomes
The primary outcome was incident, histologically confirmed melanoma (invasive and in situ combined) diagnosed in years 2–7 after enrolment, obtained through linkage to the mandatory Queensland Cancer Registry. We excluded melanomas arising in year 1 to avoid reverse causality bias that could have occured if respondents were being ‘worked‐up’ for suspicious lesions around the time of recruitment. We also separately analysed invasive vs. in situ melanomas. The secondary outcome was having one or more skin biopsies in years 2–6 after enrolment, obtained through linkage to the MBS. This outcome serves as a surrogate for subsequent screening activity.
Statistical analysis
We calculated person‐based age‐standardized rates (ASRs) of incident melanoma arising in years 2–7, and both person‐ and event‐based ASRs for biopsies arising in years 2–6. For the 65 participants who had both invasive and in situ melanomas during follow‐up, the first event was used to calculate the total melanoma ASR. We used the US 2000 population as our reference. We calculated ASRs for screened and unscreened participants.
A small proportion (2·3%) of data were missing for our primary exposure variable (skin screening), although some covariates had higher proportions of missing data. We performed multiple imputation by chained equations using the MICE package in r. 17 We assumed data were missing at random, and generated 50 datasets.
Propensity score derivation
We used propensity score models to balance the distribution of confounding factors between the screened and unscreened groups. We first used the observed covariates to model the likelihood of reporting a physician skin examination in the 3 years prior to baseline for each participant, represented as a propensity score. We used the inverse of the propensity score to weight each observation in the standard regression model. We used a generalized boosted regression model (GBM) to estimate the propensity scores with a maximum of 10 000 iterations, two levels of interactions and 0·01 shrinkage with average treatment effect. 18 We assessed the balance between screened and unscreened groups overall, as well as across strata of age (≤ 60 years, > 60 years), sex (male, female) and clinical risk (low risk, high risk) subgroups, by comparing the pooled absolute standardized mean difference for each category of each variable across the dataset. We accepted up to a 5% difference as the balance threshold. The propensity score model included baseline survey data for 20 factors, including age, sex and pigmentation, and clinical, lifestyle and socio‐economic factors (Table S1; see Supporting Information). We calculated separate propensity scores using independent GBMs for each measure of skin screening (i.e. physician skin examinations; biopsy in year 1) and checked the balance of the standardized mean difference between the screened and unscreened groups for all categories of all factors following weighting. We used r packages ‘Weightthem’ and ‘Cobalt’ to fit the propensity score model and to produce the balance plots for multiply imputed datasets.
Regression models
We used inverse probability‐weighted Cox proportional hazards models to analyse melanoma outcomes, and inverse probability‐weighted Poisson regression models to analyse biopsy outcomes (i.e. event‐based analyses using count data). The follow‐up time for melanoma started on the first day of year 2 of follow‐up and stopped at the first event of either invasive or in situ melanoma diagnosis or at the end of follow‐up (date of death, date of last MBS record or 31 December 2017), whichever occurred first. The follow‐up time for incident biopsies started from the first day of year 2 and continued until either date of death, date of last MBS record or 31 December 2016. For each outcome, we performed separate regression analyses for each of the 50 imputed and weighted datasets and pooled the effect estimates using Rubin’s rule to derive an overall effect. 19 We estimated hazard ratios (HRs) and 95% CIs for the melanoma outcomes, and rate ratios (RRs) and 95% CIs for the biopsy outcome. For both outcomes we also conducted stratified analyses for subgroups, defined according to age group, sex and clinical risk score; we determined if differences between subgroups were statistically significant by including interaction terms in the regression models. We calculated absolute risk difference and number needed to treat, as described by Austin. 20 , 21 Finally, we conducted sensitivity analyses, which included all melanomas arising after recruitment (i.e. removing the 1‐year exclusion for controlling reverse causality).
We used the ‘Survey’ package in r for weighted Cox regression and Poisson regression.
Results
At baseline, 28 155 of 38 682 (72·8%) participants reported a skin examination by a doctor in the 3 years before enrolment and were classified as ‘screened’ for the primary analysis. In the first year of follow‐up, 3280 of 35 825 (9·2%) participants had at least one skin biopsy and were classified as ‘screened’ for the secondary analysis.
During follow‐up, 967 participants were newly diagnosed with at least one melanoma (316 with invasive melanoma only, 586 with in situ melanoma only, 65 with both; Table 1). The ASR of melanoma in the cohort overall was 430/100 000 person‐years at risk (PYAR; 156/100 000 PYAR for invasive melanoma and 292/100 000 PYAR for in situ melanoma). The age‐standardized incidence of melanoma in those who reported a prior skin examination was 2·2‐fold higher than in those with no prior skin examination [incidence RR (IRR) 2·21, P < 0·001]. During years 2–6 of follow‐up, 10 905 (30·4%) of 35 825 participants underwent skin biopsy for a total of 28 366 biopsies. The ASR of biopsies was 4·0‐fold higher in those who had a prior skin examination than those who did not (IRR 4·00, P < 0·001). The thickness distributions of invasive melanomas were similar for screened vs. unscreened participants (Table S2; see Supporting Information).
Table 1.
Distribution of post‐1‐year melanoma incidence and skin biopsy status in QSkin participants by screening status (skin examination by physician; skin biopsy in first year of follow‐up)
| Screening measure | No. of participants | Melanoma‐free median follow‐up time (months)a |
No. of participants with melanoma (ASR × 10–5) |
No. of participants with an invasive melanoma (ASR × 10–5)b |
No. of participants with an in situ melanoma (ASR × 10–5)b |
Total biopsies post‐1‐year from baseline (ASR × 10–5)c |
|---|---|---|---|---|---|---|
| Skin examination in 3 years prior to baseline (n = 37 826)d | ||||||
| No | 10 267 | 64·9 | 149 (228) | 62 (77) | 95 (160) | 3168 (7183) |
| Yes | 27 559 | 64·8 | 818 (510) | 319 (188) | 556 (344) | 25 198 (20 578) |
| Skin biopsy in first year of follow‐up (n = 35 825)e | ||||||
| No | 32 545 | 65·0 | 748 (376) | 293 (138) | 507 (255) | 20 009 (13 385) |
| Yes | 3280 | 64·8 | 163 (887) | 70 (330) | 104 (584) | 8357 (54 643) |
Age standardized rate (ASR) standardized to US 2000. Melanoma ASR at individual levels (rate of new individual being diagnosed) and the total biopsies ASR includes multiple biopsies per person. aFollow‐up for melanoma started at 1 year and ended at either the date of first melanoma or date of last follow‐up (death/last contact date), whichever occurred first. bSixty‐five participants had both invasive and in situ melanomas and were counted in both ASR calculations. cFollow‐up for total biopsies ended at either first melanoma diagnosis or the last follow‐up (death/last contact data), whichever occurred first. ASR reflected overall rate of biopsies (including multiple events in individuals) during follow‐up. dIn total, 856 people had missing data for skin examination. eBiopsy information was only available for Medicare consented participants (n = 35 825).
As expected, the screened group differed substantially from the unscreened group for almost all risk factors measured in the baseline survey, for both the primary and secondary definitions of screened (Table S3; see Supporting Information). After propensity score weighting, the screened and unscreened samples for each analysis were evenly balanced with respect to observed risk factors (Figures S2 and S3; see Supporting Information).
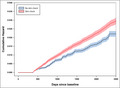
Table 2 presents the fully adjusted HRs (aHRs) from the propensity score‐weighted models for the melanoma and biopsy outcomes associated with the two measures of skin screening (physician skin examination and biopsy). We observed significantly higher rates of melanoma (aHR 1·29, 95% CI 1·02–1·63) and subsequent biopsies (aHR 1·85, 95% CI 1·69–2·04) in those who had undergone physician skin examination prior to enrolment; the higher rates of melanoma and biopsies were observed throughout the follow‐up period (Figure 1 and Table S4; see Supporting Information). In separate analyses of invasive and in situ melanoma, the higher risk associated with skin examination was evident only for in situ melanoma (aHR in situ 1·45, 95% CI 1·09–1·92; aHR invasive 1·05, 95% CI 0·72–1·54). When we included all melanomas arising within the first year following recruitment (n = 166), the aHRs increased slightly [all melanoma aHR 1·39 (95% CI 1·12–1·74); invasive melanoma aHR 1·12 (95% CI 0·79–1·58); in situ melanoma aHR 1·59 (95% CI 1·21–2·09)]. We estimated the absolute risk of melanoma at 5 years in the screened and unscreened groups to be 0·0194 and 0·0145, respectively, generating a risk difference of about 0·5% at 5 years. This equates to a number needed to screen to detect one excess melanoma of about 206. In secondary analyses in which skin screening was defined as skin biopsy in the first year of follow‐up, the melanoma hazard was about 50% higher among screenees; similarly high HRs were seen for both invasive (aHR 1·55, 95% CI 1·11–2·18) and in situ (aHR 1·50, 95% CI 1·14–1·98) melanomas. Using that secondary definition of screening, we observed about 2·6‐fold higher rates of skin biopsies in subsequent years (2–6 years of follow‐up) in the screened vs. the unscreened populations, after adjusting for all known confounders (Table 2).
Table 2.
Hazard ratios (HRs) and 95% confidence intervals (CIs) for melanoma‐related outcomes associated with measures of skin screening.
| Melanoma | Biopsy in years 2–6 | |||
|---|---|---|---|---|
| All | Invasivea | In situ b | ||
| Screening measure | HR (95% CI) | HR (95% CI) | HR (95% CI) | RR (95% CI) |
| Physician skin examination | ||||
| No | 1·0 | 1·0 | 1·0 | 1·0 |
| Yes (overall) | 1·29 (1·02–1·63) | 1·05 (0·72–1·54) | 1·45 (1·09–1·92) | 1·85 (1·69–2·04) |
| Skin biopsy in the first year of follow‐up | ||||
| No | 1·0 | 1.0 | 1.0 | 1·0 |
| Yes (overall) | 1·53 (1·23–1·89) | 1·55 (1·11–2·18) | 1·50 (1·14–1·98) | 2·64 (2·46–2·84) |
RR, rate ratio. aOf the 381 individuals diagnosed with invasive melanoma, 17 had an earlier diagnosis of in situ melanoma and were censored at that first event. bOf the 651 individuals diagnosed with in situ melanoma, 35 had an earlier diagnosis of invasive melanoma and were censored at that first event.
Figure 1.

Fully adjusted cumulative incidence of melanoma among screened and unscreened participants in years 2–7 of follow‐up. (a) Physician skin examination; (b) biopsy in year 1. [Colour figure can be viewed at wileyonlinelibrary.com]
In analyses stratified by age group, sex and clinical risk score, the risk of subsequent melanoma (Figure S4a; see Supporting Information) and biopsies (Figure S4b) in those undergoing skin examination remained elevated and broadly similar in magnitude across all strata. For the biopsy definition of skin screening, there were statistically significant differences by sex, but the differences in risk between the strata were modest and the overall pattern of elevated risks of subsequent melanoma or biopsies in those undergoing biopsies remained strong (Figure S5; see Supporting Information).
Discussion
We compared the melanoma incidence and rate of skin biopsies between people screened for skin cancer and those not screened, using two different definitions of skin screening: self‐reported whole‐body skin examination by a physican prior to baseline; and record of a skin biopsy in the first year of follow‐up. Our analyses suggest that, after considering known risk factors, people undergoing physician‐based screening for skin cancer have melanoma detection rates at least 29% higher than those not undergoing screening. While our primary analyses suggest that this effect is largely driven by increased detection of in situ melanomas, our secondary analyses observed similarly increased rates of invasive melanomas among screened vs. unscreened participants.
Chance is unlikely to explain these associations, given the precision of the risk estimates and that increased risks were observed with both measures of skin screening. Systematic information bias is also unlikely, as the primary definition of screening was reported at the baseline survey, before incident melanomas were captured through data linkage. Random misclassification of prior physician skin examinations is possible, although this would, on average, tend to bias the estimates towards the null. Moreover, this self‐reported measure is open to some interpretation by respondents; we have no way of assessing the extent or quality of the skin examinations that were conducted. The secondary definition of screening, biopsy in the first year of follow‐up, was highly unlikely to be misclassified as it was captured through record linkage with high validity, 22 , 23 although we acknowledge it suffers low sensitivity as a measure of true ‘skin screening’. It is also possible that participants changed their screening behaviour over time. In a subsequent survey during follow‐up, participants were asked if they had undergone a skin examination in the past year. About 33% of participants who were unscreened at baseline reported having a skin check at follow‐up, suggesting a reasonable ‘drop‐in’ rate. Conversely, about 23% of screened participants did not report a skin check at follow‐up (although the exposure period on the follow‐up survey was shorter than the baseline questionnaire). Taken together, these ‘drop ins’ and ‘drop outs’ would likely lead to underestimation of the effect of screening.
It is possible that residual confounding may explain the higher incidence of melanoma and biopsies in the screened groups, although we used propensity score weights to balance for all known risk factors. To reduce the observed effect to the null, unmeasured confounders that were distributed differently between screened and unscreened groups would need to exist. We estimate the e‐value for unmeasured confounders to require a risk ratio of 1·88‐fold associated with both screening and melanoma. 24 , 25 Although conceivable, we consider the existence of unknown and umeasured confounders of this magnitude to be unlikely, especially as the plots showed that the screened and unscreened groups were balanced even for factors that did not contribute to the propensity scores. While propensity score models seek to emulate randomized trials, we accept that statistical methods for removing possible confounding are imperfect. However, in the absence of randomized trial data, estimates generated from propensity score models are arguably closest to those that would arise from a trial conducted in the same setting.
Assuming error does not explain higher rates of biopsies and higher rates of melanoma in screened patients, the ‘cycle of overdiagnosis’ 8 offers a plausible explanation. Such an interpretation would be in agreement with recent trends, including the rapidly rising incidence of in situ and very thin invasive melanomas, 26 , 27 , 28 and population‐level correlations observed between the rates of skin biopsy and melanoma incidence. 8 , 10 , 11 Indeed, based on those reports, one might anticipate the effect of overdetection to be considerably higher than the 29% we estimated. In reconciling these lines of evidence, it is important not to conflate the magnitude of temporal trends observed in entire populations over many decades (i.e. large‐scale effects) with effect estimates derived in the setting of a trial over a short interval (i.e. smaller‐scale effects). Moreover, trials (and pseudo‐trials) can only measure the difference in melanoma rates between those screened and not screened, and cannot quantify any prevailing trend of overdetection that may have occurred in the background during the conduct of the study. As such, if overdetection is a consequence of population‐wide changes in the ways in which pigmented lesions present to and are managed by clinicians and pathologists, then those forces will likely be occuring in the unscreened group, as well as the screened group, albeit to a lesser extent.
It might be argued that we overadjusted our analysis by including terms for factors that may be associated with diagnostic scrutiny (such as previous excisions for skin cancer). We contend that a screening trial for melanoma would seek to ensure that the intervention and control arms were balanced for past history of skin cancer excisions; indeed, a trial that was unbalanced for this factor would be open to criticism. Nevertheless, we recalculated propensity score weights leaving out the term for previous history of skin cancer and then re‐analysed the data. The revised HR was 1·39 (95% CI 1·11–1·74).
A unique feature of our investigation into the detection of melanoma was having individual‐level data from a large prospective cohort with validated measures of phenotypic and clinical risk factors, coupled with complete follow‐up information through medical claims and cancer registration data. The number of melanoma events was sufficiently high for our primary and secondary outcome analyses, although we had limited statistical power for analyses separately by melanoma behaviour (invasive/in situ, or melanoma thickness).
In summary, these data lend plausibility to the argument that overdetection is occurring among the section of the population undergoing skin screening. Our analyses suggest that the excess fraction of melanomas at 5 years in the screened group is 0·5% after adjusting for all known risk factors, equating to a number needed to screen of 206. If those effects were generalized to the entire Australian population aged 40–69 years (6·47 million people), and assuming the same period prevalence of skin examination as observed here (0·73), we crudely estimate that about 6400 additional melanomas (mostly in situ lesions) would be diagnosed each year in those screened that might otherwise not come to clinical attention. Whether detecting those additional melanomas confers a mortality benefit remains an open question.
Funding sources
This work was supported by grants from the National Health and Medical Research Council (NHMRC) of Australia [APP1073898; APP1063061; APP1185416]. D.C.W. is supported by a NHMRC Research Fellowship [APP1155413]. S.M. is supported by a NHMRC Research Fellowship [APP1154543]. The funders played no role in the design, execution, analysis or interpretation of this study.
Conflicts of interest
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare grant and salary support only from the organizations listed above. D.C.W. has received honoraria and travel reimbursements for speaking at dermatology and oncology conferences. The authors declare no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; and no other relationships or activities that could appear to have influenced the submitted work.
Author contributions
David Whiteman: Conceptualization (lead); funding acquisition (lead); methodology (equal); project administration (supporting); resources (equal); supervision (lead); writing – original draft (lead); writing – review and editing (lead). Catherine Olsen: Conceptualization (supporting); data curation (supporting); formal analysis (supporting); funding acquisition (supporting); project administration (lead); resources (supporting); supervision (supporting); writing – original draft (supporting); writing – review and editing (supporting). Stuart MacGregor: Funding acquisition (supporting); methodology (supporting); resources (supporting); writing – review and editing (supporting). Matthew H. Law: Conceptualization (supporting); formal analysis (supporting); funding acquisition (supporting); resources (supporting); writing – review and editing (supporting). Bridie Thompson: Formal analysis (supporting); methodology (supporting); project administration (supporting); writing – review and editing (supporting). Jean Claude Dusingize: Data curation (supporting); formal analysis (supporting); writing – review and editing (supporting). Adele Green: Conceptualization (supporting); supervision (supporting); writing – review and editing (supporting). Rachel E Neale: Conceptualization (supporting); formal analysis (supporting); funding acquisition (supporting); methodology (supporting); writing – original draft (supporting); writing – review and editing (supporting). Nirmala Pandeya: Conceptualization (supporting); data curation (lead); formal analysis (lead); funding acquisition (supporting); methodology (lead); project administration (supporting); software (lead); writing – original draft (supporting); writing – review and editing (supporting).
Ethics statement
The study was approved by the Human Research Ethics Committee of the QIMR Berghofer Medical Research Institute (protocol number P1309). Patients or the public were not involved in the design, conduct, reporting or dissemination plans. All participants gave written or online consent to take part in the study and consented to their files being linked to the Queensland Cancer Registry.
Supporting information
Figure S1 Flow diagram depicting QSkin participant selection and endpoints.
Figure S2 Covariate balance plots (standardized mean difference of unadjusted and propensity score weight‐adjusted distribution) for the primary exposure measure: physician skin check.
Figure S3 Covariate balance plots (standardized mean difference of unadjusted and propensity score weight‐adjusted distribution) for the secondary exposure measure: biopsy in year 1.
Figure S4 Subgroup analyses for the association between physician skin examination and subsequent melanoma in years 2–7 and subsequent number of biopsies in years 2–6.
Figure S5 Subgroup analyses for the association between biopsy in year 1 and subsequent melanoma in years 2–7 and subsequent number of biopsies in years 2–6.
Table S1 List of variables included in propensity score models.
Table S2 Thickness distributions of invasive melanomas among unscreened vs. screened participants.
Table S3 Distribution of melanoma risk factors by screening status (skin examination by physician; skin biopsy status during the first year of follow‐up) among QSkin participants.
Table S4 Numbers of melanomas and numbers of participants at risk over time, by screening status (physician skin examination; biopsy in year 1).
Acknowledgments
We wish to thank Drs Noah Griefer and Farhad Pishgar from the Johns Hopkins School of Public Health for their kind assistance with propensity score models. We also wish to thank Professor Karen Canfell from the Cancer Council NSW, who provided critical feedback during the writing of this manuscript. Open access publishing facilitated by The University of Queensland, as part of the Wiley ‐ The University of Queensland agreement via the Council of Australian University Librarians.
Plain language summary available online
Data availability statement
The authors will make the de‐identified, relevant data from these analyses available to requestors, subject to approval from the requestor’s institutional ethics committee and the human research ethics committee of QIMR Berghofer Medical Research Institute.
References
- 1. Whiteman DC, Green AC, Olsen CM. The growing burden of invasive melanoma: projections of incidence rates and numbers of new cases in six susceptible populations through 2031. J Invest Dermatol 2016; 136:1161–71. [DOI] [PubMed] [Google Scholar]
- 2. Adler NR, Kelly JW, Guitera P et al. Methods of melanoma detection and of skin monitoring for individuals at high risk of melanoma: new Australian clinical practice. Med J Aust 2019; 210:41–7. [DOI] [PubMed] [Google Scholar]
- 3. Petrie T, Samatham R, Witkowski AM et al. Melanoma early detection: big data, bigger picture. J Invest Dermatol 2019; 139:25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Datzmann T, Schoffer O, Meier F et al. Patients benefit from participating in the German skin cancer screening program? A large cohort study based on administrative data. Br J Dermatol 2022; 186:69–77. [DOI] [PubMed] [Google Scholar]
- 5. Smith AL, Watts CG, Robinson S et al. GPs’ involvement in diagnosing, treating, and referring patients with suspected or confirmed primary cutaneous melanoma: a qualitative study. BJGP Open 2020; 4(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wilkinson D, Askew DA, Dixon A. Skin cancer clinics in Australia: workload profile and performance indicators from an analysis of billing data. Med J Aust 2006; 184:162–4. [DOI] [PubMed] [Google Scholar]
- 7. Reyes‐Marcelino G, Tabbakh T, Espinoza D et al. Prevalence of skin examination behaviours among Australians over time. Cancer Epidemiol 2021; 70:101874. [DOI] [PubMed] [Google Scholar]
- 8. Welch HG, Mazer BL, Adamson AS. The rapid rise in cutaneous melanoma diagnoses. N Engl J Med 2021; 384:72–9. [DOI] [PubMed] [Google Scholar]
- 9. Aitken JF, Youl PH, Janda M et al. Increase in skin cancer screening during a community‐based randomized intervention trial. Int J Cancer 2006; 118:1010–16. [DOI] [PubMed] [Google Scholar]
- 10. Welch HG, Woloshin S, Schwartz LM. Skin biopsy rates and incidence of melanoma: population based ecological study. BMJ 2005; 331:481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Weinstock M, Lott J, Wang Q et al. Skin biopsy utilization and melanoma incidence among Medicare beneficiaries. Br J Dermatol 2017; 176:949–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Glasziou PP, Jones MA, Pathirana T et al. Estimating the magnitude of cancer overdiagnosis in Australia. Med J Aust 2020; 212:163–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Olsen CM, Green AC, Neale RE et al. Cohort profile: the QSkin Sun and Health Study. Int J Epidemiol 2012; 41:929–29i. [DOI] [PubMed] [Google Scholar]
- 14. Morze CJ, Olsen CM, Perry SL et al. Good test–retest reproducibility for an instrument to capture self‐reported melanoma risk factors. J Clin Epidemiol 2012; 65:1329–36. [DOI] [PubMed] [Google Scholar]
- 15. Mortimore A, Pandeya N, Olsen CM, Whiteman DC. “Repeatability of Repeatability”: the stability of self‐reported melanoma risk factors in two independent samples. Aust N Z J Public Health 2021; 45:469–73. [DOI] [PubMed] [Google Scholar]
- 16. Olsen CM, Pandeya N, Thompson BS et al. Risk stratification for melanoma: models derived and validated in a purpose‐designed prospective cohort. J Natl Cancer Inst 2018; 110:1075–83. [DOI] [PubMed] [Google Scholar]
- 17. van Buuren S, Groothuis‐Oudshoorn K. mice: Multivariate imputation by chained equations in R. J Stat Softw 2010; 45:1–68. [Google Scholar]
- 18. McCaffrey DF, Ridgeway G, Morral AR. Propensity score estimation with boosted regression for evaluating causal effects in observational studies. Psychol Methods 2004; 9:403. [DOI] [PubMed] [Google Scholar]
- 19. Rubin DB. Multiple Imputation for Survey Nonresponse. New York: John Wiley, 1987. [Google Scholar]
- 20. Austin PC. Absolute risk reductions and numbers needed to treat can be obtained from adjusted survival models for time‐to‐event outcomes. J Clin Epidemiol 2010; 63:46–55. [DOI] [PubMed] [Google Scholar]
- 21. Zhang Z, Ambrogi F, Bokov AF et al. Estimate risk difference and number needed to treat in survival analysis. Ann Transl Med 2018; 6:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Perera E, Gnaneswaran N, Perera M, Sinclair R. Validating the use of Medicare Australia billing data to examine trends in skin cancer. F1000Res 2015; 4:1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Thompson BS, Olsen CM, Subramaniam P et al. Medicare claims data reliably identify treatments for basal cell carcinoma and squamous cell carcinoma: a prospective cohort study. Aust N Z J Public Health 2016; 40:154–8. [DOI] [PubMed] [Google Scholar]
- 24. Mathur MB, Ding P, Riddell CA, VanderWeele TJ. Web site and R package for computing E‐values. Epidemiology 2018; 29:e45–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E‐value. Ann Intern Med 2017; 167:268–74. [DOI] [PubMed] [Google Scholar]
- 26. Coory M, Baade P, Aitken J et al. Trends for in situ and invasive melanoma in Queensland, Australia, 1982–2002. Cancer Causes Control 2006; 17:21–7. [DOI] [PubMed] [Google Scholar]
- 27. Lipsker DM, Hedelin G, Heid E et al. Striking increase of thin melanomas contrasts with stable incidence of thick melanomas. Arch Dermatol 1999; 135:1451–6. [DOI] [PubMed] [Google Scholar]
- 28. van der Leest RJ, Zoutendijk J, Nijsten T et al. Increasing time trends of thin melanomas in The Netherlands: what are the explanations of recent accelerations? Eur J Cancer 2015; 51:2833–41. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Flow diagram depicting QSkin participant selection and endpoints.
Figure S2 Covariate balance plots (standardized mean difference of unadjusted and propensity score weight‐adjusted distribution) for the primary exposure measure: physician skin check.
Figure S3 Covariate balance plots (standardized mean difference of unadjusted and propensity score weight‐adjusted distribution) for the secondary exposure measure: biopsy in year 1.
Figure S4 Subgroup analyses for the association between physician skin examination and subsequent melanoma in years 2–7 and subsequent number of biopsies in years 2–6.
Figure S5 Subgroup analyses for the association between biopsy in year 1 and subsequent melanoma in years 2–7 and subsequent number of biopsies in years 2–6.
Table S1 List of variables included in propensity score models.
Table S2 Thickness distributions of invasive melanomas among unscreened vs. screened participants.
Table S3 Distribution of melanoma risk factors by screening status (skin examination by physician; skin biopsy status during the first year of follow‐up) among QSkin participants.
Table S4 Numbers of melanomas and numbers of participants at risk over time, by screening status (physician skin examination; biopsy in year 1).
Data Availability Statement
The authors will make the de‐identified, relevant data from these analyses available to requestors, subject to approval from the requestor’s institutional ethics committee and the human research ethics committee of QIMR Berghofer Medical Research Institute.


