Abstract
Aim
Type 1 diabetes mellitus has a large psychosocial impact on children and their families. This study's primary aim was to investigate whether the COVID‐19 pandemic affects the psychosocial impact of T1DM and glycaemic control.
Methods
During the 2020 lockdown, New South Wales residents were not allowed to leave home except for essential activities. After 3 months, children with T1DM and their parents were invited to complete online questionnaires. Data on glycaemic control were extracted from the children's clinical records with informed consent. Descriptive and comparative statistics were used to analyse the responses.
Results
Out of 149 families, 99 responses were received, with 92 participants identified. Comparable proportions of parents (56%) and children (45%) were anxious about the child's increased risk of contracting severe illness due to COVID‐19. Most responses from parents and children were closely correlated (r > 0.5, P ≤ 0.001) There was no consistent effect of lockdown on HbA1c levels, but there was a significant inverse correlation between HbA1c levels and parents' perception of the child having clear and concrete goals for diabetes care (r = −0.25, P < 0.05). The HbA1c also correlated positively with the child feeling depressed and alone with their diabetes when isolated (r = 0.36, P = 0.02).
Conclusions
Despite life‐style changes and a negative psychosocial impact, we did not find objective evidence of any detrimental impact of the lockdown on diabetic control. However, higher HbA1c correlated with children feeling more depressed and alone. There was a comparable frequency of anxiety concerning the risk of severe COVID illness in children and their parents.
Keywords: COVID‐19, psychosocial effects on children, psychosocial effects on parents, qualitative study, type 1 diabetes mellitus in children
What is already known on this topic
Type 1 diabetes exerts a significant psychosocial impact on affected individuals and their families.
In children with type 1 diabetes, psychosocial well‐being correlates with diabetic control.
Anxiety due to COVID‐19 may be associated with poorer psychosocial health in adults with diabetes.
What this paper adds
There was no discernible change in diabetic control, based on HbA1c levels before and after the lockdown.
Higher HbA1c after lockdown correlated with children feeling more depressed and alone.
Parents and children were comparably anxious about the risk of severe COVID illness.
Type 1 diabetes mellitus (T1DM) is the most common chronic endocrine disorder in childhood. 1 Treatment involves a multidisciplinary approach with the common goal of optimising glycaemic control. In the longer term, involving the child in self‐monitoring to prevent complications is also an essential part of the treatment plan. This should be achieved without compromising the child's mental health or placing undue stress on the family. 2 A child's diagnosis of T1DM can be stressful for parents, with some experiencing recurring episodes of grief and sorrow even 7–10 years after their children's diagnosis. 3 This shows the significance of the psychosocial impact of diabetes, which could become more pronounced during the COVID‐19 pandemic, contributed perhaps by social isolation and increased anxiety due to concerns about greater susceptibility to the infectious disease. 4 A study performed in Denmark found that people with diabetes might have COVID‐19‐specific worries related to their diabetes, which results in poorer psychosocial health. 5 For children with T1DM psychological well‐being may be particularly important because it may correlate with glycaemic control. A study carried out in Liberton Hospital, Edinburgh 6 found that better glycaemic control (lower HbA1c) was associated with less psychological impact in adolescents with T1DM. Researchers at the Children's Hospital in Goudi, Greece, had similar findings, identifying a link between better psychosocial health and the achievement of T1DM treatment goals. 7
During the COVID‐19 pandemic, lockdown restrictions were introduced in New South Wales (NSW) from March 2020 to control coronavirus spread. 8 This meant that residents were only allowed to leave home for essential activities. Many medical consultations were conducted via telehealth. The lockdown period lasted for approximately 3 months. The lockdown effect directly impacted life‐style, with lower exercise levels due to the cancellation of sporting events and lower incidental exercise due to being confined at home. There could also be changes in diet, perhaps with more fast‐food deliveries. The rapid shift to telemedicine was not associated with any additional psychosocial support from the clinic.
The aim of this study was first to investigate the psychosocial impact of T1DM from the perspective of the parents and children using a survey designed to screen for psychosocial well‐being. A second aim was to evaluate the glycaemic control by comparing the measurements of HbA1c taken before and after the lockdown and to correlate any changes with the survey results.
Methods
This was a qualitative cross‐sectional cohort study involving families of children and adolescents with T1DM attending the Nepean Diabetes Service Centre. The hospital is a metropolitan teaching hospital in Western Sydney and has been providing a multidisciplinary team approach to paediatric diabetes care since 2007. Inclusion criteria were children and adolescents aged between 2 and 16 years with a formal diagnosis of T1DM of more than 6 months and who attended more than two visits to the diabetes centre. Their parents were emailed the link to two online surveys, one for the parent and one for the child to complete. The surveys addressed multiple psychosocial aspects, including depression, anxiety, and social restrictions. Life‐style changes (diet and exercise) during the lockdown were addressed in the additional five parent questions. The survey took the form of statements to which parents and children could respond using a 5‐point Likert scale, scored numerically (strongly agree = 5; agree = 4; neither agree nor disagree = 3; disagree = 2; and strongly disagree = 1); additional space for free text comment was provided for every question. The child survey comprised 10 multiple‐choice questions; the parent survey comprised 9 of the same 10 questions plus another 5. The responses were collected anonymously, but participants were invited to identify themselves so that parent/child correlations could be made. Clinical and demographic details were retrieved from the child's medical record. Reminders were sent out weekly between July and August 2020 for 4 consecutive weeks via email to those not known to have already responded.
Clinical and demographic details included the child's mode of insulin delivery, age, gender, ethnicity, and postcode. HbA1c levels taken before (prior to 15th March 2020) and after the lockdown period (from June to September 2020), were also extracted for evidence of changes in glycaemic control. Some participants (32%, n = 31) did not have their HbA1c levels taken shortly after the pandemic period. Hence, the HbA1c levels were either estimated based on the data taken from their continuous glucose monitors (CGM), between June and September 2020 (39%, n = 12) or using those taken closest to the end of the investigation period after September 2020 (61%, n = 19). The socio‐economic status (SES) (based on postcode) was obtained from the Australian Bureau of Statistics 2016 9 and classified using the Index of Relative Socio‐economic Advantage and Disadvantage (IRSAD) centile with 1 being the lowest and 10 being the highest.
SPSS version 24 (IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp) was used to analyse the data. Differences in parent and child responses were evaluated using independent sample t‐tests. The Pearson correlation was used to test for association between variables. Statistical significance was assumed at P < 0.05.
This study complied with the Helsinki Declaration and relevant national guidelines and was approved by the Human Research Ethics Committee of the Nepean Blue Mountains Local Health District (Ethics number: 2020/ETH01544). Completing the survey implied consent to participate in the study; giving the child's identity indicated consent to access the clinical records.
Results
Out of 149 families (152 children) attending the clinic, responses were received from 99 parents and 49 children (Fig. 1); a total of 92 children were identifiable. In three cases, both parents returned surveys for the same child. Eight parents and four children chose not to identify themselves. There was no significant difference in the ages of the children who did and did not complete the questionnaire for themselves (P = 0.5).
Fig. 1.
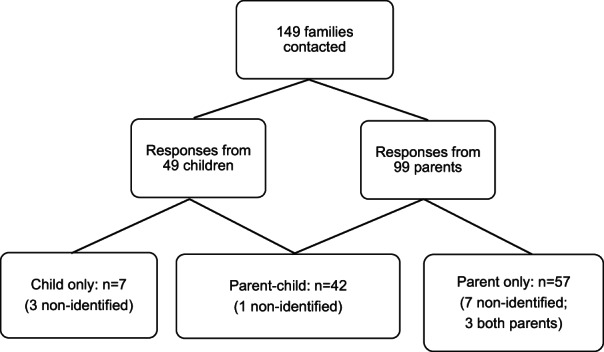
Responses received from diabetes services in Nepean Blue Mountains Local Health District.
The 92 identifiable participants comprised 37 males (40%) and 55 females (60%) with a mean age of 11.6 ± 3.4 years. There were no significant differences in age, gender, SES, or mode of insulin delivery between the identified respondents (61%) and the rest of the clinic population (Table 1).
Table 1.
Characteristics of 92 identifiable children
| Parent and child, n = 41 | Parent only, n = 47 | Child only, n = 4 | Totals | ||
|---|---|---|---|---|---|
| Gender | Male | 18 | 17 | 2 | 37 (40%) |
| Female | 23 | 30 | 2 | 55 (60%) | |
| Mode of insulin delivery | Insulin pump | 27 | 30 | 2 | 59 (64%) |
| MDI | 14 | 17 | 2 | 33 (36%) | |
| Ethnicity | Caucasian | 37 | 42 | 4 | 83 (90%) |
| Asian | 3 | 3 | 0 | 6 (7%) | |
| ATSI | 1 | 2 | 0 | 3 (3%) | |
| Age in years (SD), range | 12.0 (2.8), 5.4–16.2 | 11.1 (3.9), 5.4–16.2 | 12.6 (2.2), 10.1–14.7 | ||
|
Socio‐economic status (SD), range † |
6.4 (2.2), 2–10 | 5.9 (2.4), 1–10 | 5.7 (2.0), 4–9 | ||
1 = Lowest SES, 10 = Highest SES.
ATSI, Aboriginal and Torres Strait Islander; MDI, multiple daily injection.
Table 2 describes the survey response. The COVID‐19 pandemic was associated with the cessation of regular sport for 72% and a reduction in outdoor physical exercise when compared to the pre‐lockdown period in 78% of children. Some parents reported a change in diet (31%) and a change in insulin requirement (48%), making comments such as: ‘Less active, so needs more’; ‘She needs way more insulin, but I think this is mainly because of growth, not inactivity (her day off basal pattern has needed a lot of adjusting, and when she went back to school her school day pattern also needed adjusting). She is always inactive on her days off school’; and ‘Only minor adjustments, but I do not feel these are COVID‐related’.
Table 2.
Parents' and children's survey responses
| Question | Parent score, n = 99 (mean ± SD) | Child score, n = 49 (mean ± SD) | Significance (unpaired t‐test) |
|---|---|---|---|
| 1. I am worried that [my child/I] may get severe COVID illness due to diabetes during the COVID‐19 pandemic | 3.5 ± 1.1 | 3.2 ± 1.1 | 0.14† |
| 2. I feel more anxious generally due to the added health risks because of [my child's/my] diabetes during the COVID‐19 pandemic | 3.8 ± 1.0 | 3.0 ± 1.1 | <0.001† |
| 3. I am concerned or anxious about what [my child eats/I eat] due to diabetes when isolated during the COVID‐19 pandemic | 3.0 ± 1.0 | 2.4 ± 1.0 | 0.001 |
| 4. I feel depressed and alone with [my child's/my] diabetes when isolated during the COVID‐19 pandemic | 2.4 ± 1.0 | 2.4 ± 1.2 | 0.98† |
| 5. I am worried about [my child] having complications of diabetes such as diabetic ketoacidosis or low blood sugar reactions during the COVID‐19 pandemic | 3.3 ± 1.1 | 2.8 ± 1.1 | 0.01† |
| 6. I am happy that [my child has/I have] clear and concrete goals for diabetes care during the COVID‐19 pandemic | 3.5 ± 0.8 | 3.5 ± 0.7 | 0.94 |
| 7. I feel like diabetes has severely affected [my child's/my] daily living activities or social interactions especially when isolated during the COVID‐19 pandemic | 3.1 ± 1.2 | 3.1 ± 1.3 | 0.88† |
| 8. I am comfortable [bringing my child/coming] to visit the diabetes service during the COVID‐19 pandemic | 3.4 ± 1.1 | 3.4 ± 1.1 | 0.86 |
| 9. I prefer telehealth (phone/video consult) compared to face to face consultation during the COVID‐19 pandemic | 3.1 ± 1.2 | 2.7 ± 1.2 | 0.04† |
| 10. I am satisfied with my body weight and shape with the diabetes management especially during COVID‐19 pandemic when activities are limited | – | 3.2 ± 1.1 | |
| 11. I feel guilty when my child gets off track with diabetes management during the COVID‐19 pandemic | 3.3 ± 1.2 | – | – |
| 12. Before the lockdown my child was engaged in regular exercise (sport, dance and drama) | 3.9 ± 1.0 | – | – |
| 13. Before the lockdown, in addition to the regular exercise listed in question 12, my child was physically active (e.g. playing outside at home, playing outside at recess and lunch breaks at school, walking or cycling to school) for an hour or more per day | 3.9 ± 0.9 | – | – |
| 14. During the lockdown, my child's diet has changed | 2.8 ± 1.1 | – | – |
| 15. During the lockdown, my child's insulin requirement has changed | 3.3 ± 1.0 | – | – |
Pearson correlation between parent and child responses, r > 0.5, P < 0.001.
All responses were scored on a 5‐point Likert scale: (strongly agree = 5; agree = 4; neither agree nor disagree = 3; disagree = 2; strongly disagree = 1).
The majority of parents (55%) were happy that there were clear goals for their child's diabetes management, although this was less important to the children (47% neither agreed nor disagreed); parents and children were comfortable attending the diabetes service during lockdown (62% and 55%, respectively). Most parents (52%) admitted to feeling guilty when their child's diabetes management was off track.
The parents agreed with most of the survey questions eliciting negative psychosocial consequences of COVID‐19 (Table 2). Parents and children were comparably anxious about the child's increased risk of contracting severe illness due to COVID‐19. This worried 56% of parents and 45% of children. The parents' highest mean scores were for feeling more anxious generally about their child's diabetes during the pandemic; for this, the mean score for the parents was significantly higher than the children's (P < 0.001) (Table 2, Fig. 2). Children were significantly less anxious than their parents about their diet (P = 0.001) and the complications of diabetes, such as low blood sugar or diabetic ketoacidosis (DKA) (P = 0.01). One parent commented, ‘I worry about the possibility of DKA due to getting the virus’. Parents made comments such as, ‘I hold concern for my child getting any illness, not solely COVID‐19 due to the added complexity of T1DM when unwell’.; ‘It is complicated as I (the parent) have diabetes and comorbidity so am quite concerned generally about COVID’.; and ‘I feel my child is at a higher risk compared to other people, and a lot of teenagers have become quite complacent with COVID‐19’. Children commented: ‘Well I think COVID will be a bit more severe because I am a diabetic’.; ‘They say that diabetes has a higher death rate if they get COVID’; ‘I agree mainly because I think diabetes weakens my immune system’.
Fig. 2.
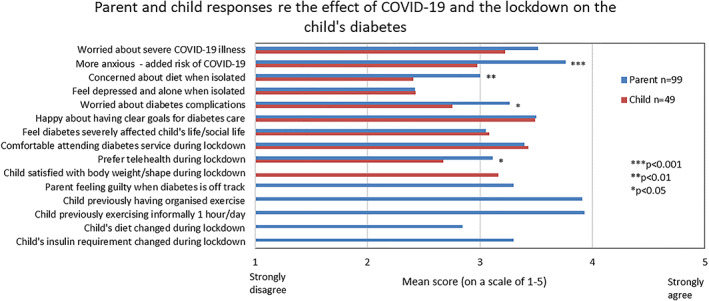
Parent and child responses regarding the effect of COVID‐19 and the lockdown on the child's diabetes. For questions in full see Table 2.
Most parents and children disagreed that they felt depressed and alone with the child's diabetes (83% and 82%, respectively). One parent commented that her husband was off work during the pandemic; hence she obtained more help at home from him. One child commented: ‘No, how dare you I have supporting friends I have no reason to feel depressed’. However, one parent commented on changes in their child's daily living activities: ‘She seems more withdrawn and yet tells me she is fine. She does not want to talk about diabetes, but I know it is depressing her’. Most children (63%) were not anxious about what they ate when isolated, with comments such as ‘No, I just eat less because mum restricts me from eating everything in the fridge’; and ‘No I do not care’. Some children (29%) expressed dissatisfaction with their body weight and shape with the diabetes management and restricted activities due to COVID‐19.
About 38% of parents and 27% of children preferred telehealth, with the parents scoring this significantly higher than the children (P = 0.04). Regarding the change to telehealth, parent comments included: ‘I feel face‐to‐face has more impact, as my son was not interested in the phone and I was the one who had to relay what was discussed’; ‘I prefer a face‐to‐face appointment as I feel they are more effective for both myself and my child’; and ‘I am happy to use the phone service if it is the only option however we prefer the face‐to‐face’.
For six of the nine questions that they had in common, the responses from parents and their children were highly correlated (r > 0.5, P ≤ 0.001). The correlation was slightly less significant for questions 8 and (r = 0.47, P = 0.002) and 3 (r = 0.35, P = 0.023), which related to being comfortable attending the diabetes service and anxiety about diet, respectively. There was no significant correlation between parents and children about having clear goals for diabetes management (r = 0.04, P = 0.8): only the parents prioritised this.
There was a small but significant reduction in HbA1c over the entire clinic population (mean −0.25, SD 1.44, P = 0.039), but the reduction was not significant when the non‐respondents were excluded (mean −0.23, SD 1.36, P = 0.11). The HbA1c concentrations before and after the lockdown were closely correlated (r = 0.59, P < 0.001).
The parents' perceptions of the impact of lockdown on their child's diet and insulin requirement (questions 14 and 15) were significantly correlated with HbA1c (r = 0.21, P = 0.04, and r = 0.58, P < 0.001), respectively). The HbA1c after the lockdown correlated positively with the child feeling depressed and alone with their diabetes when isolated (r = 0.36, P = 0.02) and inversely with the parents' perception of the child having clear and concrete goals for diabetes care (r = −0.25, P = 0.02). The pre‐lockdown HbA1c and the change in HbA1c did not correlate significantly with any survey responses. There was a significant inverse correlation between SES and the parent's perception of the severity of the impact of the pandemic on their child's daily living and social interactions (r = −0.24, P = 0.018).
Discussion
Our study has demonstrated an insignificant effect of lockdown on HbA1c. Higher HbA1c was correlated with children feeling more depressed and alone, whereas lower HbA1c was correlated with parents having a better perception of targets. There was a comparable frequency of anxiety concerning to the risk of contracting severe COVID illness in children and their parents, although parents were more anxious than children about the added health risk imposed by COVID‐19, including the risks of hypoglycaemia and DKA. Children showed little concern about their diet during the lockdown, one stating that this was under parental control. There was a suggestion of poorer diabetes control in association with changes in diet and insulin. Although parents and children did not generally feel that the child's daily living activities or social life had been greatly affected, those with lower SES may have suffered more. Parents and children were happy overall about the clear goals for diabetes management and comfortable attending the diabetes service, although parents showed a significantly greater preference than children for telemedicine.
The strength of this study was its qualitative research design and associated correlation with objective data on diabetic control. This provided us with an understanding of the psychosocial impact of living through the pandemic with T1DM and the correlations with HbA1c.
There are limitations to the study that should be considered. First, this is a small, single‐centre study. Although we had identifiable responses from 61% of our clinic cohort, the responders may not represent the clinic cohort as a whole, for example, having a higher rate of insulin pump use. Not all had HbA1c levels performed after the pandemic from June to September 2020, as face‐to‐face consultations were not always available. In addition, although we may infer lower exercise levels in those who ceased their regular sport and outdoor activities, time spent exercising in the home was not assessed.
The findings in this study are consistent with the results of a Denmark Study, which also utilised online surveys and concluded that people with diabetes had COVID‐19‐specific worries related to their diabetes associated with poorer psychosocial health. 6 The Denmark study had a much larger sample size of 2430 participants but was restricted to adults and did not include other family members' responses. An Italian study, which surveyed parents and children, found pronounced psychological symptoms during the first wave of the pandemic due to the quarantine and lack of support. 10 Multiple measures were utilised in the study, including the COVID‐contact risk index, home environment risk index, parent's dyadic parenting stress (perception of parent's stress in the parent–child interaction), parents' stress and children's psychological problems, which provided a broader view of psychological impact as compared to our study. However, only parents' perceptions were taken into the analysis compared to our study, where both the children's and parents' perceptions were captured. They were, therefore, unable to document any correlation between parental anxiety and the anxiety experienced by their children. Furthermore, they were not investigating children with chronic health conditions.
Parental mental well‐being, consistent positive parenting and low levels of hostile parenting are important factors for maintaining and improving a child's socio‐emotional well‐being. 11 T1DM is known to have a psychosocial impact on children and their families, and we thought this might become more evident during the COVID‐19 pandemic. However, we found that parental feelings of guilt about poor diabetes management were associated only with poorer pre‐pandemic diabetes control and did not significantly correlate with HbA1c after the pandemic. Families may have felt better supported during the pandemic by the clinic staff's efforts to maintain continuity of care via telemedicine.
Interestingly, Predieri's study in Italy has suggested improvement in glycaemic control in children and adolescents with T1DM during the lockdown due to the use of real‐time CGM, continuous parental management and telemedicine care, despite home quarantine and limitations to exercise. 12 A similar study has also suggested a comparable outcome in Italian children and adults with CGM metrics, though not in teenagers. 13 Our findings are not consistent with the outcome of the Italian studies, perhaps because fewer participants with poor pre‐lockdown diabetes control answered the survey.
Conclusions
Despite reports of psychosocial issues including increased anxiety, together with life‐style changes during the COVID‐19 pandemic and lockdown, we did not find objective evidence of any detrimental impact on diabetic control, as indicated by HbA1c levels before and after the lockdown. Future research is warranted to investigate the effectiveness of using psychosocial assessment tools and interventions on the psychosocial impact of T1DM during times of additional environmental stress, particularly in families with lower SES.
Acknowledgements
We would like to acknowledge and thank all the participants, patients and parents of patients who participated in this study. We would also like to acknowledge and thank Associate Professor Gary Leong, Paediatric endocrinologist, Ms Julie Longson, Credentialled diabetes educator; Ms Renee Kennedy, Dietician and Ms Cassandra Noake, Admin officer of Nepean Paediatric diabetes service, for their assistance in this project.
Grants: None.
Conflict of interest: None declared.
References
- 1. Henríquez‐Tejo R, Cartes‐Velásquez R. Psychosocial impact of type 1 diabetes mellitus in children, adolescents and their families. Literature review. Rev. Chil. Pediatr. 2018; 89: 391–8. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29999147. [DOI] [PubMed] [Google Scholar]
- 2. Cooke D, Plotnick L. Type 1 diabetes mellitus in pediatrics. Pediatr. Rev. 2008; 29: 374–85. [DOI] [PubMed] [Google Scholar]
- 3. Bowes S, Lowes L, Warner J, Gregory JW. Chronic sorrow in parents of children with type 1 diabetes. J. Adv. Nurs. 2009; 65: 992–1000. [DOI] [PubMed] [Google Scholar]
- 4. Liu JJ, Bao Y, Huang X, Shi J, Lu L. Mental health considerations for children quarantined because of COVID‐19. Lancet Child Adolesc. Health 2020; 4: 347–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Joensen LE, Madsen KP, Holm L et al. Diabetes and COVID‐19: Psychosocial consequences of the COVID‐19 pandemic in people with diabetes in Denmark—What characterizes people with high levels of COVID‐19‐related worries? Diabet. Med. 2020; 37: 1146–54. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/dme.14319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ashraff S, Siddiqui MA, Carline TE. The psychosocial impact of diabetes in adolescents: A review. Oman Med. J. 2013; 28: 159–62. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3679608/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kakleas K, Kandyla B, Karayianni C, Karavanaki K. Psychosocial problems in adolescents with type 1 diabetes mellitus. Diabetes Metab. 2009; 35: 339–50. [DOI] [PubMed] [Google Scholar]
- 8. Australia's coronavirus lockdown – The first 50 days [internet]. The Guardian. Guardian News and Media; 2020 [cited 2020 Oct 26]. Available from: https://www.theguardian.com/world/2020/may/02/australias-coronavirus-lockdown-the-first-50-days
- 9. Main Features – Socio‐Economic Advantage and Disadvantage [Internet]. Australian Bureau of Statistics, Australian Government. [cited 2020 Nov 10]. Available from: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2071.0~2016~Main%20Features~Socio-Economic%20Advantage%20and%20Disadvantage~123
- 10. Spinelli M, Lionetti F, Pastore M, Fasolo M. Parents' stress and children's psychological problems in families facing the COVID‐19 outbreak in Italy. Front. Psychol. 2020; 11: 1713. Available from: https://www.frontiersin.org/articles/10.3389/fpsyg.2020.01713/full. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Parsons J. COVID‐19 children and anxiety in 2020. Aust. J. Gen. Pract. 2020: 49. Available from: https://www1.racgp.org.au/ajgp/coronavirus/covid-19-children-and-anxiety-in-2020. doi: 10.31128/AJGP-COVID-27 [DOI] [PubMed] [Google Scholar]
- 12. Predieri B, Leo F, Candia F et al. Glycemic control improvement in Italian children and adolescents with type 1 diabetes followed through telemedicine during lockdown due to the COVID‐19 pandemic. Front. Endocrinol. 2020; 7: 595735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Di Dalmazi G, Maltoni G, Bongiorno C et al. Comparison of the effects of lockdown due to COVID‐19 on glucose patterns among children, adolescents, and adults with type 1 diabetes: CGM study. BMJ Open Diabetes Res. Care 2020; 8: e001664. [DOI] [PMC free article] [PubMed] [Google Scholar]


