Abstract
Objectives
To produce a best practice consensus guideline for the conduct of scrotal exploration for suspected testicular torsion using formal consensus methodology.
Materials and Methods
A panel of 16 expert urologists, representing adult, paediatric, general and andrological urology used the RAND Corporation / University of California, Los Angeles (RAND/UCLA) Appropriateness Consensus Methodology to score a 184‐statement pre‐meeting questionnaire on the conduct of scrotal exploration for suspected testicular torsion. The collated responses were presented at a face‐to‐face online meeting and each item was rescored anonymously after a group discussion, facilitated by an independent chair with expertise in consensus methodology. Items were scored for agreement and consensus and the items scored with consensus were used to derive a set of best practice guidelines.
Results
Statements scored with consensus increased from Round 1 (122/184, 66.3%) to Round 2 (149/200, 74.5%). Recommendations were generated in 10 categories: consent; assessment under anaesthetic; initial incision; intra‐operative decision making; fixation; medical photography; closure; operation note; logistics; and follow‐up after scrotal exploration. Our statements assume that the decision to operate has already been made. Key recommendations in the consent process included discussion of the possibility of orchidectomy and the possibility of subsequent infection of the affected testis or wound requiring antibiotic therapy. If after the examination under anaesthesia, the index of suspicion of testicular torsion is lower than previously thought, then the surgeon should still proceed to scrotal exploration as planned. A flow chart guiding decision making dependent on intra‐operative findings has been designed. If no torsion is present on exploration and bell clapper deformity is absent, the testis should not be fixed. When fixing a testis using sutures, a three‐ or four‐point method is acceptable and non‐absorbable sutures are preferred.
Conclusions
We have produced consensus recommendations to inform best practice in the conduct of scrotal exploration for suspected testicular torsion.
Keywords: testicular torsion, orchidopexy, surgical technique, fixation, scrotal exploration
Abbreviations
- BURST
British Urology Researchers in Surgical Training
- IPRAS
interpercentile range adjusted for symmetry
- NIHR
National Institute of Health Research
Introduction
Testicular torsion is a common urological emergency arising from acute twisting of the spermatic cord causing testicular ischaemia. The current ‘gold standard’ investigation and treatment is emergency scrotal exploration, ideally performed within 4–6 h of symptom onset, to untwist a torted testicle [1, 2]. If the testicle is found to be viable after untwisting, then it is fixed, usually along with the contralateral testicle. If it is found to be unviable then a simple orchidectomy is performed. However, findings during scrotal exploration can vary and may be ambiguous, meaning surgeons are required to make a series of potentially complex intra‐operative decisions.
Despite testicular torsion being an important emergency with potentially detrimental clinical and medicolegal consequences, there is a paucity of published work to inform best practice and guidelines. A recently published systematic review of seven studies and 182 patients detailing different surgical techniques highlighted a lack of strong evidence favouring any particular approach with respect to short‐term complications or longer‐term outcomes such as re‐torsion, fertility, or patient‐reported outcomes [3]. A previous survey of 29 English urologists also demonstrated wide variability in clinical practice [4]. Whilst all would perform bilateral orchidopexy in confirmed torsion, fixation technique differed. Responses also differed regarding which, if any, synchronous procedures to perform and, crucially, what to do intra‐operatively if torsion is excluded.
There is a lack of granular national or international guidance on intra‐operative decision making for surgeons. The European Association of Urology does not currently recommend any particular surgical technique or decision‐making process [5], and both the BAUS and AUA have not published any relevant guidelines.
In the absence of high‐quality clinical evidence and reported variation in practice [3, 4], robust consensus methodology is useful for outlining expert‐determined optimal surgical practice until comparative clinical studies can be performed. This approach also allows identification of areas of uncertainty that may form the basis of future research. Therefore, to provide a reference for standard practice, we aimed to use consensus methodology to produce a BAUS–British Urology Researchers in Surgical Training (BURST) consensus guideline for scrotal exploration technique and decision making.
Materials and Methods
Study Design
We conducted a two‐round consensus study using the RAND Corporation / University of California, Los Angeles (RAND/UCLA) appropriateness method [6]. This was a structured process that incorporated a series of statements with which panellists anonymously rated their agreement or disagreement. Further discussion, feedback, and amendments were then facilitated, and re‐scoring performed, to determine the presence or lack of consensus.
A protocol and list of statements related to the conduct of scrotal exploration was generated. Our statements assumed that the decision to operate had already been made. We did not include statements pertaining to neonatal torsion (defined here as patients younger than 1 month). For the purposes of this consensus document, ‘children’ refers to patients aged <16 years.
After initial design by K.D.C., A.L. and V.K., the statements were internally reviewed by the FIX‐IT working group, which included the panellists, an independent meeting chair with methodological consensus expertise, and involved expert peer review by non‐UK based expert urologists, and patient and public involvement representatives (this process is described in Appendix S1). After additions, removals and amendments, a list of 184 statement items was included in Round 1 for scoring by panellists. These statements were grouped into 10 broad categories: consent; assessment under anaesthetic; initial incision; intra‐operative decision making; fixation; medical photography; closure; operation note; logistics; and follow‐up after scrotal exploration.
Round 1 was conducted electronically between November 2020 and January 2021. All panel members were individually asked to score their agreement with each statement on a nine‐point Likert scale. On this scale, a score of 1 represented strong disagreement, a score of 5 uncertainty, and a score of 9 strong agreement. Panellists were permitted to abstain from scoring if they felt they did not have the required expertise pertaining to a particular statement to score it with confidence. Considering panellist scores collectively, a group median score of 1–3 indicated group disagreement with the statement, 4–6 indicated group uncertainty, and 7–9 indicated group agreement. Following this, statement scores were then assessed as being with or without consensus using the interpercentile range adjusted for symmetry (IPRAS) method [6]. Further details on this methodology are shown in Appendix S2. During Round 1, panellists were also given another opportunity to amend or delete statements or add additional statements.
Round 2 was conducted ‘virtually’ in March 2021 using the online meeting platform Zoom™. For each statement, the distribution of Round 1 scores was anonymized and presented graphically alongside the statement outcome for discussion amongst the panel (Appendix S3). Panellists also had access to their individual Round 1 scores. Following discussion, panellists were then asked to anonymously re‐score each statement in turn. As in Round 1, panellists were invited to suggest additions, removals, and amendments to statements during discussions. Thereafter, scores were collated, were quantitatively analysed as per the IPRAS method [6], and a qualitative analysis of the discussions was undertaken.
Panellists
Our panellists comprised 16 UK‐based surgeons in active practice with good experience of scrotal exploration (Appendix S4). All panellists participated in both scoring rounds. We invited panel members, prioritizing representation from a variety of subspecialties including paediatric urology and andrology, different geographical regions, and tertiary/non‐tertiary referral centres. We also prioritized inviting some panel members with experience in consensus meetings and guideline formation.
The Round 2 meeting was chaired by an independent, non‐scoring, health services researcher with expertise in chairing urological consensus meetings and consensus methodology (S.M.). Further support to the chair and necessary clarification of clinical discussions as required were provided by a neutral, non‐scoring member of the working group (V.K.).
Results
Following Round 1, six of the 184 statements were removed, 22 statements rephrased, and 22 statements added. This provided a final list of 200 statements that were discussed and scored in Round 2. During Round 1, 122/184 statements (66.3%) were scored with consensus. This proportion increased in Round 2, where 149/200 statements (74.5%) were scored with consensus. Table 1 shows the breakdown of statements after each round, scored as agreement with consensus, disagreement with consensus, or uncertain. A summary of results and Round 2 discussions are detailed below and in Appendix S5.
Table 1.
Proportion of statements scored as in agreement with consensus, in disagreement with consensus, and uncertain.
| Stage | Agreement with consensus, n (%) | Disagreement with consensus, n (%) | Uncertainty, n (%) |
|---|---|---|---|
| Post‐Round 1 | 68 (37.0) | 54 (29.3) | 62 (33.7) |
| Post‐Round 2 | 82 (41.0) | 67 (33.5) | 51 (25.5) |
‘Uncertainty’ also includes agreement or disagreement with no consensus. A total of 184 statements were scored in Round 1, and 200 statements in Round 2.
Consent
Patients and/or parents should be counselled regarding the possible following risks of scrotal exploration during the consent process:
• Orchidectomy;
• Decreased fertility;
• Contralateral testicular injury;
• Haematoma requiring secondary drainage;
• Anaesthetic complications and aspiration due to an unfasted anaesthetic induction (if applicable);
• Infection in the affected testis that may require antibiotics;
• Infection in the unaffected contralateral testis (if it is explored) that may require antibiotics;
• Infection in the wound that may require antibiotics or secondary drainage.
It was uncertain as to whether the possibility of decreased hormonal function and intra‐operative photography of the testis (routinely in all cases of scrotal exploration for suspected testicular torsion) should be included in the consent process.
Patients and/or parents should not be counselled to undergo unilateral fixation alone if there was no torsion evident on exploration. However, in this scenario, panellists agreed that patients and/or parents should be counselled that it is acceptable to perform a unilateral Jaboulay procedure alone, as this was not considered to be a fixation technique.
When counselling patients about the possibility of orchidectomy for an unsalvageable testis, a prosthesis should not be offered during the initial scrotal exploration operation (in either children or adults) due to the risk of infection and prosthesis erosion.
Assessment Under Anaesthetic
If, after assessment under anaesthetic, the index of suspicion for testicular torsion is lower than previously thought, the surgeon should still proceed to scrotal exploration as planned.
Initial Incision
Both cranio‐caudal median raphe and transverse incisions (over the testis of concern) are acceptable, but it is uncertain which is preferred. It was uncertain as to whether a cranio‐caudal paramedian incision is acceptable (Fig. 1).
Fig. 1.
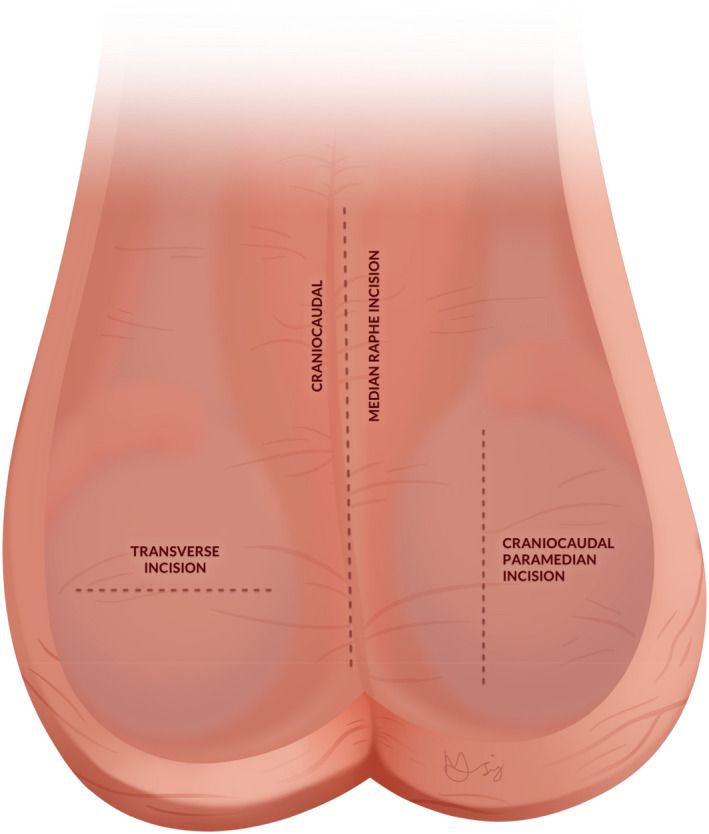
Visual representation of possible scrotal incisions. Following Round 2, it was agreed that both cranio‐caudal median raphe and transverse incisions (over the testis of concern) are acceptable, but it is uncertain which is preferred. It was uncertain as to whether a cranio‐caudal paramedian incision is acceptable. [Colour figure can be viewed at wileyonlinelibrary.com]
Intra‐operative Decision Making
Panellists were presented with three scenarios all pertaining to patients thought to have a torted testis preoperatively but with different intra‐operative findings: torsion found intra‐operatively; no torsion found intra‐operatively and no other pathology present; and no torsion found intra‐operatively but other pathology present to account for the presentation. A visual summary of recommendations is shown in Fig. 2.
Fig. 2.
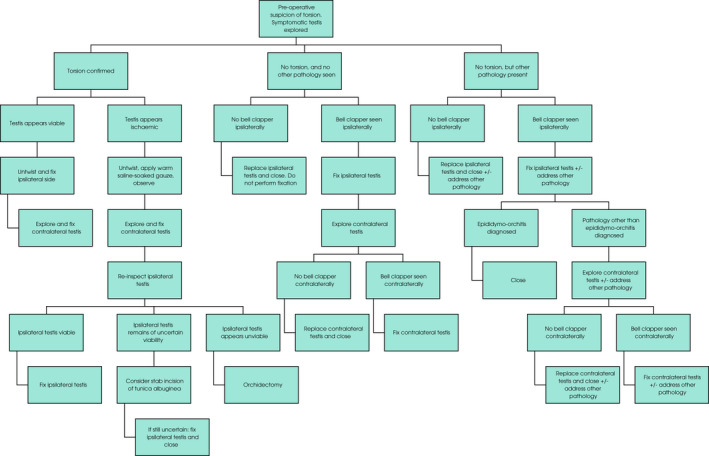
Flow chart for recommended decision making intra‐operatively, based on appearance of symptomatic testis. [Colour figure can be viewed at wileyonlinelibrary.com]
Scenario A: Torsion Found Intra‐operatively
Where torsion is found intra‐operatively, if viable, the testis should be untwisted and fixed to prevent future torsion. The contralateral side should be explored and fixed too, either by sutured or sutureless repair, such as a Dartos pouch.
If the appearance of the torted testis indicates ischaemia, the testis should be untwisted and wrapped in warm, saline‐soaked gauze. The anaesthetist should not be asked to administer an increased concentration of oxygen. The surgeon should allow some time to assess interval change in appearance. It was uncertain how long to wait, but it was agreed that the delay should be at least as long as the time taken to fix the contralateral side. A stab incision of the tunica albuginea to assess for bleeding should be performed only if the testis remains of uncertain viability following other efforts to maximize reperfusion as detailed above.
If a testis remains of uncertain viability (e.g., is dusky in colour but not black or purple), the testis should be replaced and orchidectomy avoided. The panellists discussed incision in the tunica albuginea to reduce intra‐testicular pressure, followed by a graft such as a vaginalis patch [7]. It was agreed that this was not a widely used technique and there was uncertainty about its role in scrotal exploration. There may be rare cases where this is indicated but it should only be performed by those familiar with the technique.
Scenario B: No Torsion Found intra‐operatively and No Other Pathology to Account for Presentation is Evident
If no torsion is found intra‐operatively and no other pathology is evident to account for the presentation, the symptomatic testis should not be fixed, and the contralateral testis should neither be explored nor fixed.
If no torsion is found but a bell clapper deformity (Fig. 3) is evident ipsilaterally, the testis should be fixed to prevent future torsion. The contralateral side should also be explored and if the bell clapper deformity is again evident, the contralateral testis should also be fixed.
Fig. 3.
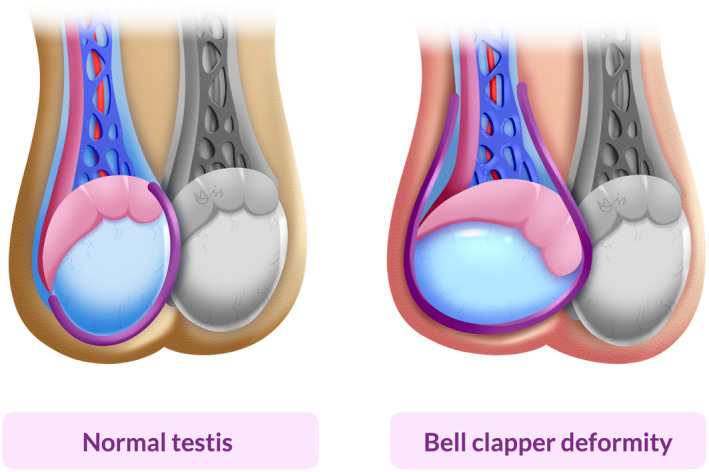
Visual illustration of a normal testis vs a testis with a bell clapper deformity. In the bell clapper deformity, the tunica vaginalis (denoted by the purple line) does not attach normally to the epididymis to create a ‘mesentery’, thereby making it more prone to torsion. [Colour figure can be viewed at wileyonlinelibrary.com]
Scenario C: No Torsion Found Intra‐operatively But Other Pathology to Account for Presentation is Evident
Where no torsion is found intra‐operatively but other pathology is evident, such as epididymo‐orchitis or a torted testicular appendage, the testis should not be routinely fixed. If a bell clapper deformity is evident on the symptomatic side, the testis should be fixed in place to prevent future torsion. In the presence of a bell clapper deformity, if the pathology is anything other than epididymo‐orchitis (to prevent seeding of infection), the contralateral side should then be explored to investigate for a bell clapper on the contralateral side.
For each scenario above, it was agreed that, in children, healthy testicular appendages should routinely be removed to prevent future torsion. In adults it was agreed that it is acceptable to do this, but it was uncertain whether this should be performed routinely.
Fixation
In children, both a Dartos pouch (sutureless fixation; Fig. 4) and suture fixation (Fig. 5) are equally acceptable. Surgeons should only undertake fixation techniques in which they are competent. If using a Dartos pouch, supplemental sutures should not be used to fix the testis within the Dartos pouch. Furthermore, for suture fixation, the testes should not be fixed to each other through the midline scrotal septum using sutures. If suture fixation is being undertaken, there was uncertainty as to whether the tunica vaginalis should be everted as per a Jaboulay repair.
Fig. 4.
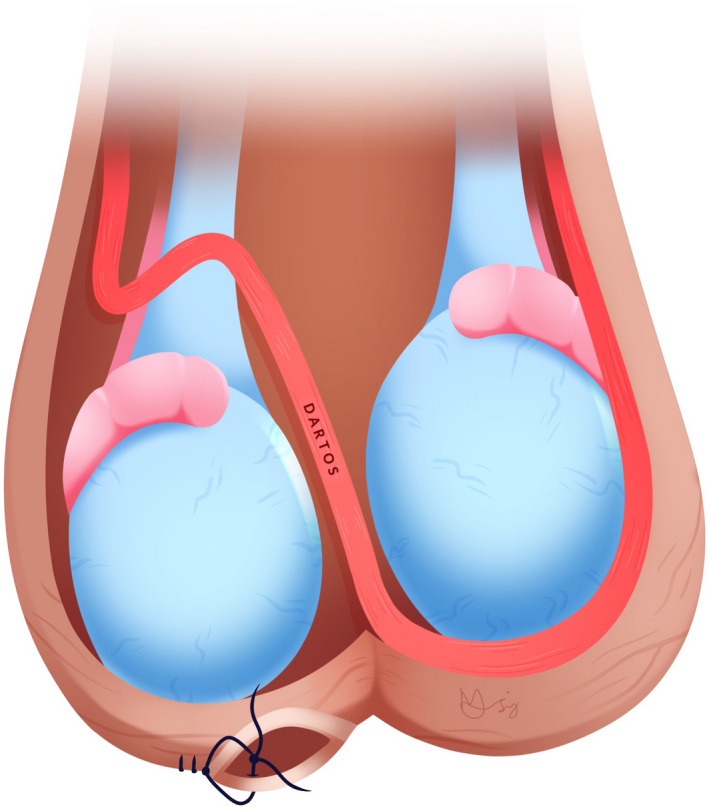
Visual illustration of a sutureless fixation of the right testis within a Dartos pouch. [Colour figure can be viewed at wileyonlinelibrary.com]
Fig. 5.
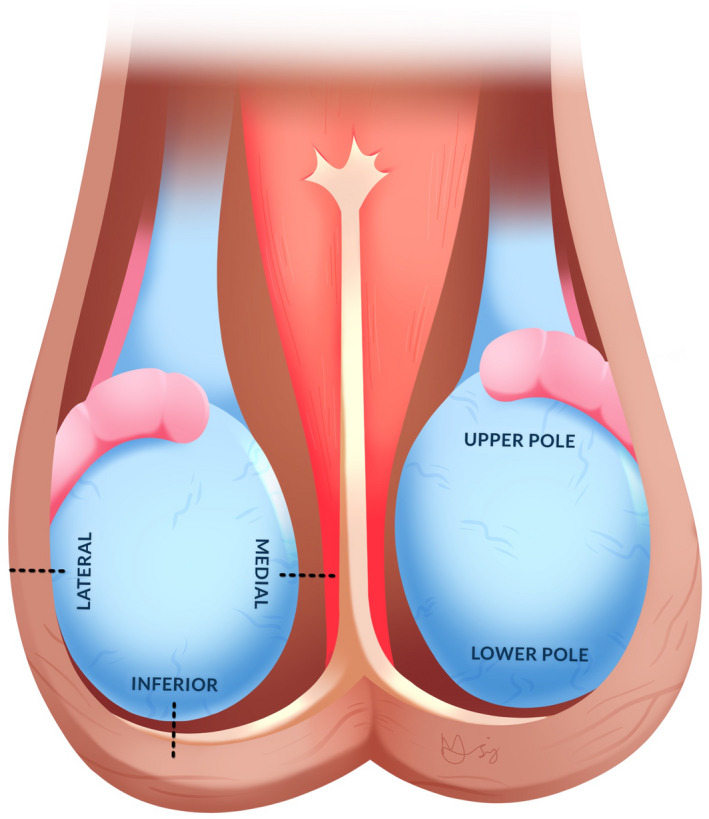
Visual illustration of a three‐point suture fixation of the right testis. [Colour figure can be viewed at wileyonlinelibrary.com]
In adults, suture fixation should be performed. The testes should not be fixed to each other through the midline scrotal septum using sutures. The tunica vaginalis should be everted as per a Jaboulay repair [8].
For suture fixation, non‐absorbable sutures, for example, polypropylene, were the preferred option. As a second choice, if surgeons were to use absorbable sutures, prolonged‐absorption absorbable sutures such as polydioxanone (approximate absorption time of 200 days) was the only suture type deemed acceptable. Theoretically, this may reduce the likelihood of micro‐abscesses and development of chronic scrotal pain when compared to non‐absorbable sutures. It was agreed there may be important medicolegal implications if absorbable sutures are used regarding the possibility of re‐torsion once the sutures have been absorbed. Irrespective of type of suture or fixation method used, panellists felt that, should a patient re‐present with pain in a testis previously documented as fixed, and the history and examination findings are consistent with testicular torsion, it is reasonable to undertake further scrotal exploration to investigate for recurrent testicular torsion.
Panellists agreed that suture size is an important decision, however, there was no agreement as to the most appropriate size. Discussion highlighted that intra‐operative assessment of testicular volume may influence this, especially regarding children, and therefore suture size choice should be at the discretion of the surgeon.
Interrupted sutures should be used for suture fixation. Three‐ or four‐point fixation methods are both acceptable, but a three‐point fixation is preferred (Fig. 5). Sutures should be placed on three surfaces of the testis: lateral, medial and inferior. It does not matter if sutures are placed in the upper or lower pole.
Medical Photography
Intra‐operative medical photography of a torted testis should not be performed routinely, for example, to document appearances pre‐ and post‐untwisting.
Closure
The Dartos layer should be closed separately to the skin. For the Dartos layer, a continuous suture is preferred. For the skin, interrupted sutures are preferred. The scrotum should be held in a compressive fashion postoperatively, for example, using a scrotal support.
Operation Note
The following should be documented in the operation note:
• Technique of testicular fixation, if performed;
• If suture fixation was performed, the size and type of suture used;
• If a testis is torted, the degree to which it was twisted;
• If a testis is torted, its appearance pre‐ and post‐untwisting;
• If observed, the presence of other pathology, where a testis is non‐torted.
A copy of the operation note and/or discharge summary containing the above details should be given to the patient. This may be helpful for patients to bring with them if they were to re‐present with acute scrotal pain.
There was uncertainty whether the approximate time of onset of symptoms, time of symptom onset to hospital presentation, or time from symptom onset to theatre should be recorded in the operation note specifically. However, all of the above should be documented elsewhere in the medical notes.
Logistics
The priority should be ensuring urgent exploration as soon as possible, thereby providing the best chance of organ salvage in a suspected torsion. There was no agreement on a minimum or maximum acceptable time delay. Discussions highlighted the need for some pragmatism when local circumstances, surgeon workload (e.g., managing other life‐threatening emergencies) and availability of the emergency theatre (e.g., another emergency currently in emergency theatre) may vary. If an emergency operating theatre is not available within a reasonable time frame, an additional emergency theatre with appropriate staffing should be opened to accommodate this operation. In such a scenario, there was uncertainty as to whether a patient should be transferred to the nearest centre where there is emergency theatre availability, highlighting concerns about further delays when transferring patients.
Any appropriately trained surgeon should be permitted to perform scrotal exploration, which includes urologists, general surgeons and paediatric surgeons. Due to concerns about delays in transfer, there was uncertainty regarding the appropriateness of transferring patients to another site if there is no appropriately trained surgeon at the index site, or if the surgeon covering the index site on call is based at another centre.
Panellists agreed that if there was likely to be no significant delay, ultrasonography may add further information to help decision making and is acceptable but not mandatory. However, if the clinician felt that scrotal ultrasonography would be likely to lead to significant delay in the possibility of taking a patient to theatre, it should be omitted.
Follow‐up after Scrotal Exploration
Routine follow‐up of patients is influenced by both intra‐operative findings and individual patient characteristics. Certain scenarios were raised where follow‐up should be particularly encouraged, for example, the intra‐operative finding of epididymo‐orchitis in a child, which is far less common than in an adult and may warrant further investigation. Whilst it was accepted that final decisions should be made dependent on local resource availability, panellists discussed aspirational follow‐up arrangements for four broad scenarios.
Scenario A: No Torsion Identified
There was no consensus regarding whether patients with no torsion identified required follow‐up.
Scenario B: Torsion Found and Testis Appeared Viable After Untwisting and Fixation
Patients in whom torsion is found and where the testis appears viable after untwisting and fixation should be assessed in an outpatient clinic to assess routine postoperative recovery.
Scenario C: Torsion Found and Testis of Uncertain Viability After Untwisting and Fixation
Patients in whom torsion is found and where the testis is of uncertain viability after untwisting and fixation do not require routine admission postoperatively to hospital to observe deterioration in symptoms. However, these patients should be assessed in an outpatient clinic to assess routine postoperative recovery. Doppler ultrasonography should only be used if the patient is symptomatic, for example, with pain beyond what one might expect. It was uncertain whether orchidectomy should be performed routinely if postoperative ultrasonography demonstrates no flow in the affected testis but the patient is asymptomatic. However, orchidectomy is an acceptable course of action following discussion with the patient. If follow‐up ultrasonography demonstrates no flow in the affected testis and the patient is in persistent pain, the option for orchidectomy should be discussed with the patient.
Scenario D: Torsion Found and Orchidectomy Performed
Patients in whom torsion is found and orchidectomy performed should be assessed in an outpatient clinic to assess routine postoperative recovery. If the contralateral testis is of small volume or appears atrophic, they should also be offered semen analysis with a view to sperm banking where fertility preservation is appropriate. At this appointment it can be discussed whether a testicular prosthesis is desired. In children, placement of a prosthesis should be delayed until post‐puberty and the prosthesis can be sized based on their adult‐size testis. During discussions, it was agreed that a prosthesis should ideally be placed inguinally rather than through the initial scrotal incision.
Discussion
Acute scrotal pain is a common presentation at the emergency department and one of the most important urological emergencies. Despite this, there is an absence of high‐certainty evidence for the decision making and conduct of scrotal exploration [3]. In this context, expert‐based consensus to guide practice is valuable. These guidelines represent the first expert‐consensus‐derived set of best practice recommendations for the conduct of emergency scrotal exploration for suspected testicular torsion. Clinicians can use these recommendations to guide their daily practice.
A recent systematic review highlighted both a paucity of work and limited evidence favouring one particular operating technique, with only 182 patients from seven relevant studies identified between 1975 and 2012 [3]. There was significant variability in practice regarding fixation technique, the type of sutures used, synchronous procedures, contralateral orchidopexy, and whether to perform orchidopexy in negative explorations. Ultimately there was limited evidence supporting any one technique and, importantly, there was a lack of long‐term clinical, fertility and patient‐reported outcomes presented.
A previous UK survey of practice in scrotal exploration also highlighted considerable variation in clinical practice regarding scrotal exploration [4]. Of the 29 respondents, all would perform bilateral orchidopexy in confirmed torsion with viable testes. However, fixation technique was varied, although the use of polyglactin 910 sutures (57%) and three‐point fixation were the most common (66%). The majority of respondents (62%) would not perform a synchronous procedure, such as excision of an appendix testis or a Jaboulay procedure. Lastly, in the case of a diagnosis other than torsion, 31% would still perform ipsilateral orchidopexy (contrary to the results of this consensus meeting), although all would omit contralateral orchidopexy.
Despite torsion being a common emergency, and despite the lack of high‐certainty evidence in this space, there has been no previous attempt at deriving consensus‐based guidelines for clinical practice. This work therefore fills an important gap in the literature. The high degree of consensus achieved in this meeting, which increased after Round 2, highlighted that, despite high variation in practice, when considered in more detail using consensus methodology, it is possible to successfully agree on a reference set of guidelines.
This study has some limitations. Expert consensus recommendations are prone to bias, especially when taken in the context of a lack of robust, randomized evidence. Views of the panellists may not be fully representative of all surgeons who perform scrotal exploration. Furthermore, individual dominant personalities could have disproportionately influenced discussions in Round 2. We minimized this bias by performing a systematic review as a basis for discussions [3], by including a range of surgeons from a variety of specialist and subspecialist backgrounds, different geographical areas and tertiary and non‐tertiary centre backgrounds, and lastly by facilitating anonymized scoring, chaired by an independent expert methodologist.
Our recommendations are made for a typical patient and the most typical scenarios with which a surgeon may be faced, although it is acknowledged that there may be circumstances that arise that are not accounted for in these guidelines, particularly in varied healthcare settings. In each case, individual surgeon judgement is important to evaluate the relevance of these guidelines to their patients.
Previous work has identified that there is no strong evidence favouring any particular operating technique with respect to clinical, fertility and patient‐reported outcomes [3]. One of the issues is that there are limited published data available relating outcomes after exploration to surgical technique. In studies that do report this, long‐term outcomes are usually lacking. Future studies could first focus on collecting these data more robustly in a national registry, as is performed in the UK for other urological conditions [9, 10, 11].
Whilst these guidelines focus on decision making once a decision for scrotal exploration has already been made, one area for future research would be to investigate the value of point‐of‐care testicular ultrasonography, in addition to clinical evaluation, for evaluating suspected torsion and reducing the negative exploration rate. This was considered a high priority by our patient and public involvement group and the panellists felt that this may be of value in decision making in acute scrotal pain providing it would not significantly delay a patient's pathway to surgery.
In conclusion, these consensus recommendations provide best‐practice guidelines for the conduct of scrotal exploration for suspected testicular torsion and can be used by clinicians in the management of this important urological emergency.
Disclosure of Interests
All authors have nothing to declare.
Supporting information
Appendix S1 Study design flowchart.
Appendix S2 Explanation of the interpercentile range adjusted for symmetry (IPRAS) method, with a worked example.
Appendix S3 Graphic representation of the group response for four statements showing (A) agreement and consensus (group median score: 9); (B) uncertainty and consensus (group median score: 4); (C) agreement and no consensus (group median score: 7.5); (D) disagreement and no consensus (group median score: 3). Please see Appendix S1 for more information.
Appendix S4 List of participants, and their characteristics, who took part in both Round 1 and 2.
Appendix S5 Final list of statements discussed and scored.
Acknowledgements
The authors would like to thank Jacqueline Emkes and Rachel Jury for their contribution to our protocol development with respect to patient and public involvement. Similarly, the authors would like to thank Dr Matthew Coward, Department of Urology, University of North Carolina, and Dr Selcuk Sarikaya, Department of Urology, University of Ankara, for their international perspectives and input to our study protocol. We would like to acknowledge the BAUS Trustees for allowing this collaboration. Unrelated to this work, The BURST Research Collaborative would like to acknowledge funding from the BJUI, the Urology Foundation, Ferring Pharmaceuticals Ltd, Rosetrees Trust and Action Bladder Cancer UK. Veeru Kasivisvanathan is an Academic Clinical Lecturer funded by the United Kingdom National Institute for Health Research (NIHR). The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. PubMed Indexed Collaborative Authors: Matthew Coward, Selcuk Sarikaya, Jacqueline Emkes, Rachel Jury.
K.D.C. and A.L. are joint first authors.
References
- 1. Dajusta DG, Granberg CF, Villanueva C, Baker LA. Contemporary review of testicular torsion: New concepts, emerging technologies and potential therapeutics. J Pediatr Urol 2013; 9(6 PART A): 723–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mellick LB, Sinex JE, Gibson RW, Mears K. A systematic review of testicle survival time after a torsion event. Pediatr Emerg Care 2019; 35: 821–5 [DOI] [PubMed] [Google Scholar]
- 3. Moore SL, Chebbout R, Cumberbatch M et al. Orchidopexy for testicular torsion: A systematic review of surgical technique. Eur Urol Focus 2020; 7: 1493–503 [DOI] [PubMed] [Google Scholar]
- 4. Pearce I, Islam S, McIntyre IG, O'Flynn KJ. Suspected testicular torsion: A survey of clinical practice in north West England. J R Soc Med 2002; 95: 247–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. European Association of Urology . Paediatric urology. 2020. Available at: https://uroweb.org/guideline/paediatric‐urology/. Accessed 21 March 2021
- 6. Fitch K, Bernstein SJ, Aguilar MD, Burnand B, LaCalle JR. The RAND/UCLA appropriateness method user's manual. Rand Corp Santa Monica CA 2001. https://www.rand.org/pubs/monograph_reports/MR1269.html [Google Scholar]
- 7. Figueroa V, Salle JLP, Braga LHP et al. Comparative analysis of detorsion alone versus detorsion and tunica albuginea decompression (fasciotomy) with tunica vaginalis flap coverage in the surgical management of prolonged testicular ischemia. J Urol 2012; 188: 1417–23 [DOI] [PubMed] [Google Scholar]
- 8. Jaboulay M. Chirurgie des centres nerveux des viscères et des membres, Vol. 2. Lyon/Paris: Storck, 1902: 192 [Google Scholar]
- 9. Devlin CM, Fowler S, Biyani CS, Forster JA. Changes in UKrenal oncological surgical practice from 2008 to 2017: Implications for cancer service provision and surgical training. BJU Int 2021; 128: 206–17 [DOI] [PubMed] [Google Scholar]
- 10. Aning JJ, Parry MG, van der Meulen J et al. How reliable are surgeon‐reported data? A comparison of the British Association of Urological Surgeons radical prostatectomy audit with the National Prostate Cancer Audit Hospital Episode Statistics‐linked database. BJU Int; 2021; 124: 482–9 [DOI] [PubMed] [Google Scholar]
- 11. Payne SR, Fowler S, Mundy AR. Analysis of a 7‐year national online audit of the management of open reconstructive urethral surgery in men. BJU Int 2020; 125: 304–13 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Study design flowchart.
Appendix S2 Explanation of the interpercentile range adjusted for symmetry (IPRAS) method, with a worked example.
Appendix S3 Graphic representation of the group response for four statements showing (A) agreement and consensus (group median score: 9); (B) uncertainty and consensus (group median score: 4); (C) agreement and no consensus (group median score: 7.5); (D) disagreement and no consensus (group median score: 3). Please see Appendix S1 for more information.
Appendix S4 List of participants, and their characteristics, who took part in both Round 1 and 2.
Appendix S5 Final list of statements discussed and scored.


