Abstract
Anxiety is an adaptive emotional response to potentially threatening or dangerous situations; moderated by the sympathetic nervous system. Dental anxiety is common and presents before, during or after dental treatment. The physiological response includes an increase in heart rate, blood pressure, respiratory rate, and cardiac output. Consequently, extensive distress leads to avoidance of dental treatment and multiple failed appointments, impacting both oral and general health. Dental anxiety can generate a variety of negative consequences for both the dentist and the patient. Evidence‐based strategies are essential for mitigating and relieving anxiety in the dental clinic. Psychotherapeutic behavioural strategies can modify the patient's experience through a minimally invasive approach with nil or negligible side effects, depending on patient characteristics, anxiety level and clinical situations. These therapies involve muscle relaxation, guided imagery, physiological monitoring, utilizing biofeedback, hypnosis, acupuncture, distraction and desensitization. Pharmacological intervention utilizes either relative analgesia (nitrous oxide), conscious intravenous sedation or oral sedation, which can have undesirable side effects, risks and contraindications. These modalities increase the cost and availability of dental treatment.
Keywords: Anxiety, dental clinic, fear, management, strategies
Abbreviations and acronyms
- CBT
cognitive behavioural treatment
- GABA‐A
gamma‐aminobutyric acid
- HPA
hypothalamus–pituitary–adrenal axis
- HRV
heart rate variability
- IP
informational pamphlet
- IV
immersive visualization
- VAS
visual analogue scale
- VR
virtual reality
- VRET
Virtual Reality Exposure Therapy
INTRODUCTION
Anxiety is an adaptive emotional response to potentially threatening or dangerous situations; moderated by the sympathetic nervous system. 1 , 2 Dental anxiety relates to the fear, stress or dread induced before, during or after dental treatment. 3 Approximately 25% of the population suffers from dental anxiety, with some even fulfilling the criteria for dental anxiety. 4
Anxiety activates the autonomic nervous system, increasing involuntary body functions such as blood pressure, heart rate, respiratory rate, gastrointestinal tract motility and cardiac output. 1 , 2 , 4 When the hypothalamus–pituitary–adrenal (HPA) axis releases adrenaline, the sympathetic nervous system is activated, provoking the fight‐or‐flight response. 1 , 5 This response initiates various physiological changes, such as reducing pain threshold, increasing treatment complications, slowing recovery and increasing post‐treatment pain. 1 , 2 , 4 Evoking physical, cognitive, emotional and behavioural responses can make dentally anxious patients more challenging to manage, which is stressful for many dentists. 1 , 2 , 4
Substantial distress leads to avoidance of dental treatment and multiple failed appointments, negatively impacting oral and general health. 4 Evidence‐based strategies are essential for the appropriate management of dental anxiety, mitigating stress for both the dentist and patient. 4 Thus, improving dental attendance and quality of life. 4 This article will systematically review various current management strategies for adult patients with dental anxiety in the dental clinic. Although many articles focus on specific management strategies, there are a limited number of reviews that provide collated information on the current management of dental anxiety within the clinic for adults.
Searches were carried out using PubMed, Medline Ovid, Cochrane, Scopus and CINAHL, selecting articles published on dental anxiety management, with the following key terms; management, anxiety, adult, dental clinic, excluding children. Restrictions include articles published in English between 1 January 2011 and 5 October 2021.
There is no universally effective management for dental anxiety. 2 , 3 Psychotherapeutic strategies, pharmacological interventions or a combination of both can relieve anxiety in the dental clinic depending on patient characteristics, anxiety level and clinical situations. 2 , 3 Psychotherapeutic management strategies modify behaviour through learning and are minimally invasive with nil or negligible side effects. 2 , 3 These therapies involve muscle relaxation, guided imagery and physiological monitoring using biofeedback, hypnosis, acupuncture, distraction and desensitization.
Pharmacological interventions utilize relative analgesia (nitrous oxide), conscious intravenous sedation or oral sedation, which have a range of undesirable side effects, contraindications, and risks. Additionally, increasing the cost and availability of dental treatment. 5 The clinical relevance is the management of adult patients with dental anxiety within the dental clinic itself.
METHODS AND MATERIALS
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines and the PICO framework. 6 The following clinical statement was addressed “Management strategies for adult patients with dental anxiety in the dental clinic,” where (P = population) is adult patients with anxiety; (I = intervention) is anxiety management strategies; (C = comparison) is management vs no intervention and (O = outcome) is lower stress, fear or anxiety. This review protocol is registered with PROSPERO with a registration number: 278642. 7
Information sources and search strategy
Scopus, Ovid, PubMed, Cochrane and CINAHL databases were searched using different combinations of MeSH terms to retrieve the articles (Table 1). Only articles published in English and up to and including 1 January 2011, with no location restrictions. EndNote (Clarivate Analytics, EndNote X8.2, 2018) was used to store and sort articles. After 188 duplicates were removed, articles were excluded based on date, title, abstract and full text following the PRISMA guidelines. 7
Table 1.
Databases searched, search terms and corresponding MeSH terms used
| Database | Search terms |
|---|---|
| Medline (Ovid) |
|
| PubMed | ((((Dental Anxiety[MeSH Terms])) OR (anxiety OR fear OR phobia)) AND ((patient OR adult) OR (Adult[MeSH Terms])) AND ("Dental clinic" OR "dental practice" OR "dental procedure") AND (strateg* OR manag* OR therap* OR alleviate OR ease OR mitigate OR light* OR lessen OR decreas*) NOT ((child* OR infant OR adolescent OR youth))) |
| Cochrane |
|
| Scopus | ((anxiety OR fear OR phobia) AND ("dental clinic" OR "dental practice" OR "dental procedure*" OR "dental treatment") AND (strateg* OR manag* OR therap* OR alleviate OR ease OR mitigate OR light*OR lessen OR decreas*) AND (adult OR patient) AND NOT (child* OR infant OR adolescent OR youth)) |
| CINAHL |
|
Study selection process
The inclusion criteria for eligible studies included the following:
Type of Studies: All peer‐reviewed research articles, irrespective of study design; prospective, retrospective, and randomized controlled clinical trials on patients with dental anxiety or phobia; published in the English language, after and including 1 January 2011.
Type of participants: Healthy adult patients that suffer from dental anxiety or phobia.
Outcome measure: Qualitatively or quantitatively addressed the effect of a specific management strategy(s) on dental anxiety.
Excluded studies did not report dental anxiety, fear or phobia; did not evaluate management strategies as an outcome or involved children, adolescents, or medical conditions. Literature reviews, conference abstract(s), case studies, opinion papers or studies not available as full text or in English or published before 1 January 2011, were also excluded.
The PRISMA flow chart (Fig. 1) illustrates the selection process followed during this review. For screening and assessment of inclusion criteria, titles and abstracts were independently screened by four assessors (BH, KE and SN). Disagreements were resolved by a discussion moderated by one of the two independent assessors (DO and VF). Full‐text articles of the eligible studies were obtained and evaluated to confirm their eligibility for inclusion into this review.
Fig. 1.
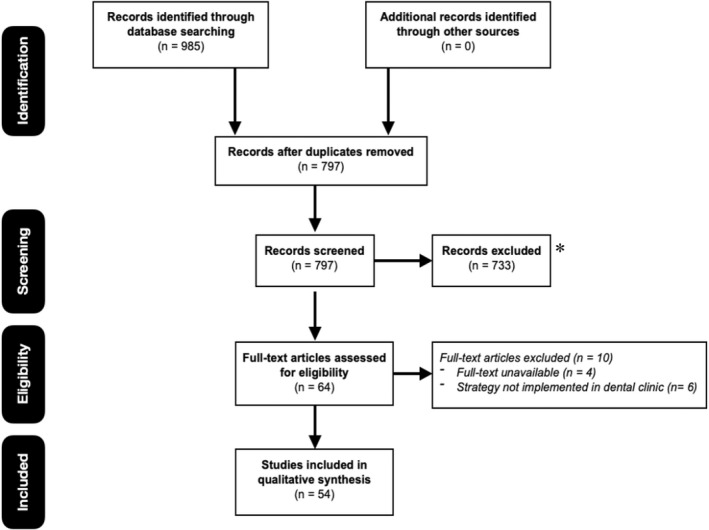
Flowchart of the systematic review according to preferred reporting items for systematic review guidelines. 6
Data collection and data synthesis
Extracted data was collated into a spreadsheet by three assessors independently using custom‐designed data extraction forms. The data included: study design, number of participants, intervention details, treatment outcomes, instrument or methodology utilized, initial findings, follow‐up period, funding source, location of the study and the outcome. The final data included was agreed upon by all the assessors. Group discussion resolved any differences, and two authors checked the accuracy.
RESULTS
Study characteristics
Fig. 1 outlines the details of the study selection process. The initial search returned 985 articles from the earlier databases; 188 duplicates were removed. The remaining 797 articles were screened for an appropriate date, title and then abstract. Sixty‐eight articles then underwent full‐text analysis to assess suitability based on the inclusion criteria. The final review included 54 articles as 10 articles did not meet the inclusion criteria (Table 2). Table 3 outlines the details of excluded studies.
Table 2.
Number of articles excluded by reason
| Database | Search results | Date | Title | Abstract | Language | Final no. of articles |
|---|---|---|---|---|---|---|
| Ovid | 301 | 163 | 57 | 5 | 0 | 19 |
| PubMed | 170 | 38 | 39 | 3 | 0 | 1 |
| Cochrane | 29 | 16 | 2 | 0 | 0 | 2 |
| Scopus | 598 | 257 | 273 | 25 | 1 | 32 |
| CINAHL | 75 | 0 | 39 | 0 | 1 | 0 |
Table 3.
Summary of papers excluded and reasons for exclusion, after accessing full text
| Author, year | Country | Objectives of study | Reasons for exclusion |
|---|---|---|---|
| Lindenberger et al. (2017) | Germany | Effect of aerobic exercise in dental phobia | Not applied in dental clinic |
| Arias et al. (2019) | USA | Smartphone‐based exposure treatment for dental phobia | Not applied in dental clinic |
| Heaton et al. (2013) | Unknown | Computerized dental injection fear treatment | Not applied in dental clinic |
| Doering et al. (2013) | Germany | Efficacy of a trauma‐focused treatment approach for dental phobia | Not applied in dental clinic |
| Elsesser et al. (2013) | Germany | Mental Retrieval of Treatment Context in Dental Phobia | Not applied in dental clinic |
| Yi‐Yueh et al. (2014) | China | Document details ‐ Comparative study of auxiliary effect on dental anxiety, pain and compliance during adult dental root canal treatment under therapeutic Chinese music or western classic music | Full‐text unavailable |
| Paul (2014) | USA | Dental phobia… How to overcome it. | Full‐text unavailable |
| Henry et al. (2018) | USA | Considerations for the management of patients with generalized anxiety disorder in the dental setting | Full‐text unavailable |
| Białoszewska et al., 2018 | Poland | Analysis of emotions related to dental treatment | Full‐text unavailable |
| Averley (2014) | United Kingdom | The GDC's new standards, and managing patients' pain, discomfort or anxiety. | Full‐text unavailable |
Quality assessment of included studies
Extracted data was collated into a spreadsheet by three assessors independently using custom‐designed data extraction forms. Two assessors (DO and KE) independently assessed the risk of bias and level of evidence for each of the studies included. Group discussions moderated by an independent assessor resolved any disagreements. The Oxford Centre for evidence‐based medicine's scale was utilized to assess the levels of evidence provided by each of the included studies. 8
DISCUSSION: MANAGEMENT STRATEGIES
Management strategies
Distraction therapy
Distraction with different technological interventions such as music, virtual reality and hypnosis, diverts attention away from negative stimuli by masking the fear‐generating noises that create an unpleasant experience. 1
Music therapy
Music listening utilizes neutral, relaxing music with a slow tempo; 60–80 beats per minute, repetitive rhythm, gentle contours and strings. 5 It can reduce blood pressure, heart rate, respiratory rate and cardiac output in anxious patients during dental treatment. 9 , 10 Music used in waiting areas or the dental chair can reduce anxiety and improve the patient experience. 11
Music listening has various effects on the body to manage anxiety:
Music listening suppresses the sympathetic nervous system, reducing adrenergic and neuromuscular activity lowers anxiety. 9
Body rhythms are synchronized with low (under 80 bpm) and predictable rhythm, resulting in lower adrenergic and neuromuscular arousal. 1
Music diverts attention away from negative stimuli by masking the fear‐generating noises of dental instruments. 1
Many studies have investigated the effect of music on physiological parameters and emotional anxiety levels. Mejia‐Rubalcava et al. (2015) investigated the impact of music therapy on physiologic parameters in patients with dental anxiety. 5 Following exposure to a local anaesthetic needle and noise of the high‐speed drill, patients listened to “soothing”, “calming”, “music instrumentals” for 20 minutes. Subsequently, decreasing anxiety, salivary cortisol concentrations and blood pressure; while improving patient experience. 5 A pilot study by Gupta and Ahmed (2017) investigated how listening to “instrumental music with earth sounds” through headphones during minor oral surgery affected dental anxiety. 11 Findings concluded; 92% of patients experienced reduced anxiety, pain and discomfort. 11 Anxiety levels reduced by 50% between pre‐and post‐operative recordings, and overall heart rate decreased along with the duration of treatment. 11 Overall, 90% of patients requested music for their next appointment, suggesting the intervention improved patient comfort and alleviated some anxiety. 11 Furthermore, Thoma et al. (2014) reported that patients who listened to music for ten minutes before dental hygiene treatment experienced less anxiety than participants who did not. 1 Similarly, Kavarthapu (2017) revealed that music reduces pain perception by alleviating anxiety in patients undergoing extraction. 12
Providing patients with more control might aid in anxiety reduction. 13 Saravanan (2018) investigated how listening to music through headphones affected dental anxiety during dental treatment. 13 Patients could manipulate the music volume, granting some control while simultaneously masking fear‐inducing noises from the dental drill. 13 Results suggest that music distraction effectively reduced the mean dental anxiety levels. 13 Conversely, Pintea et al. (2017) investigated the impact of symphonic and lounge music on anxiety and pain during treatment. 14 Irrespective of the use or type of background music, there was no significant reduction in anxiety or pain, and pulse rates were similar for all groups. 14 Therefore, questioning the efficacy of music in reducing anxiety and pain in dental patients. 14 However, this study did not utilize headphones, which is also likely to block out disturbing noises and improve distraction. These findings indicate that further research is required.
Different frequencies of music have various effects. 9 , 15 Music at 432 Hz is “neutral” and free from emotion avoiding physiological responses in patients. 9 , 15 Aravena et al. (2019) investigated how music listening at 432 and 440 Hz with headphones for fifteen minutes affects dental anxiety and salivary cortisol levels. 9 The study concluded, both 440 and 432 Hz reduced anxiety compared to the controlled group. 9 However, the emotional response and perception of anxiety showed no significant difference between frequencies. 9 Despite this, listening to 432 Hz produced significantly smaller cortisol concentrations, suggesting that the perception of a sound can be drastically modified when the frequency changes. 9 Nasso et al. (2016) supported this conclusion, adding that 432 Hz music significantly decreased blood pressure and heart rate during endodontic procedures. 15 Alternatively, binaural beats use two sounds with steady intensities but different frequencies in each ear. 2 A single tone results if the difference in frequencies is below 30 Hz. 2 The highly debated theory suggests that the frequency of external stimuli might synchronize neural activity. 2 Isik et al. (2017) investigated the effectiveness of listening to binaural beats for ten minutes through headphones in reducing preoperative anxiety. 2 Results revealed a significant anxiety reduction, suggesting that binaural beats might be valuable in reducing preoperative anxiety. 2 Again, more research is required. 2
Finally, Gulnahar (2020) investigated the effect of three different types of music: Turkish, classical and slow rock, on dental anxiety. 16 Blood pressure, heart rate, and oxygen saturation levels were measured during the experiment. 16 The study concluded; all groups with music treatment had a significant decrease in anxiety levels. There were no changes in blood pressure, but Turkish music improved heart rate stability compared with other kinds of music. 16 Regardless of the type of music, listening to music diminishes dental anxiety significantly, with Turkish and classical music being the most effective. 16
Music listening can distract the patient while suppressing the autonomic nervous system. 1 , 2 , 5 , 9 Subsequently, listening to slow tempo; 60–80 beats per minute, instrumental music is beneficial for managing dental anxiety before and during treatment in the dental clinic. 1 , 2 , 5 , 10 , 11 The use of headphones while in the dental chair is also recommended. 13 The duration of music listening before dental treatment shows no correlation thus far. 1 , 2 , 5 , 10 , 11 , 14 Research regarding the effect of different frequencies, the optimal moment to implement therapy and the impact on recovery would also be valuable.
Virtual reality
According to many studies, exposure therapy is the treatment of choice for specific fears and anxiety. 4 Exposure therapy can either be imaginal (in vitro) or real‐life (in vivo). 4 Virtual Reality Exposure Therapy (VRET) is a novel cognitive behavioural approach used to successfully treat specific anxieties through systematic and gradual desensitization until fear extinction occurs. 4 , 17 VRET creates a computer‐generated virtual environment where the patient can confront their fears at their own pace and in the privacy of the therapist's office or dental chair, thus providing a safer, less embarrassing and more cost‐effective treatment for anxieties. 4 As it is an in vitro exposure, as opposed to in vivo, the patient experiences less anticipatory anxiety and consequently, the rates of treatment acceptance and completion are higher. 4 VRET can be equally or slightly more effective than real‐life exposure therapy for anxiety treatment. However, the evidence of its effectiveness in treating dental anxiety is limited. 4
Guijar et al. (2018) investigated the effect of VRET on dental anxiety in ten randomized patients. 18 Patients received either an information pamphlet (IP) or VRET. 18 Heart rate and pre and post‐treatment anxiety levels were recorded. 18 Overall, the study suggested that VRET is a safe and feasible treatment option for patients with dental anxiety. 18 There was no evidence of increases in heart rate, no symptom exacerbations, and no participant drop‐outs. 18 Subsequently, VRET significantly reduced dental anxiety and behavioural avoidance. 18 The decrease in behavioural avoidances was seen as more patients in the VRET group scheduled follow‐up appointments than in the IP group. 18 Notably, more VRET patients no longer met the dental anxiety criteria when compared with the IP group. 18
Guijar et al. (2019) further assessed the effectiveness of VRET for the treatment of dental anxiety and addressed the limitations of previous studies. 17 The primary outcome compared post‐treatment state and dental anxiety scores between the VRET and IP groups. 17 Overall, VRET effectively decreased dental anxiety and behavioural avoidance. 17 Furthermore, a larger proportion of VRET patients underwent further dental treatment after six months and no longer fulfilled the diagnostic criteria for dental anxiety, further supporting the effectiveness of VRET. 17 VRET activates the underlying fear structure through controlled and realistic visual, olfactory and auditory cues, creating controlled confrontations in the absence of an adverse outcome, thus reducing the patient's fear response. 17 Interestingly, VRET does not increase heart rate but shows a downward trend with higher anxiety‐provoking virtual reality (VR) scenarios. 17
La Paglia et al. (2018) investigated the use of virtual reality as a distraction from anxiety and pain whilst patients are undergoing dental procedures. 19 The study supported the method of using different VR environments to allow patients to relax and be distracted, thus reducing anxiety, improving compliance, and achieving non‐disruptive behaviour during dental treatment. 19 Yamashita et al. (2020) also investigated the effect of VR in alleviating anxiety during impacted mandibular third molar extractions under local anaesthesia. 20 Anxiety was evaluated before and after treatment by measuring heart rate variability (HRV) and completing a pre and post‐treatment questionnaire involving a visual analogue scale (VAS). 20 The results found that anxiety had decreased amongst patients who had used VR, while anxiety increased in patients who had not used VR. 20 Furthermore, 92% of participants had reported a decrease in anxiety, 100% of the patients would want to use VR in future surgical treatments, and 96% would want to use VR in future dental treatments. 20 No patients showed symptoms of cybersickness. 20 Subsequently, VR effectively alleviated fear and anxiety during treatment. 20
Immersive visualization
Immersive visualization (IV) is a distraction technique that uses specialized eyewear to reduce stress, pain, anxiety and fear without interfering with treatment. 21 IV eyewear does not constrict the patient's peripheral vision, providing additional comfort. 21 Padrino‐Barrios et al. (2015) found that IV eyewear is an effective technique to help decrease or manage short‐term anxiety in adult patients during routine oral debridement. 21 IV eyewear is a safe, economical, easy‐to‐use, non‐pharmacological and portable approach to a short‐term reduction of dental anxiety. 21
HYPNOSIS
Hypnotherapy is an older, non‐invasive intervention that uses audio recordings with or without “relaxation music” to reduce fear and pain and improve relaxation during treatment. 3 , 22 Hypnotherapy is either used as a stand‐alone anxiolytic intervention or as an adjunct to other methods such as anaesthesia. 3
Glaesmer et al. (2015) state that hypnosis can be used in addition to other interventions in patients suffering from mild to moderate anxiety. 3 However, patients with severe dental anxiety require more complex and more effective psychotherapeutic interventions such as cognitive‐behavioural techniques. 3 Hypnosis is an easy‐to‐apply and economical method of reducing anxiety, as it can either be induced live or with a recording such as a CD. 3 Glaeser investigated the effect of hypnosis on dental anxiety in 102 patients. The study assessed patient attitudes regarding hypnosis and compared dental anxiety in both groups throughout dental extractions. 3 Hypnosis resulted in a lower level of dental anxiety during treatment, despite anxiety levels being similar between groups before and after treatment. 3 Additionally, 75% of patients found hypnosis pleasant, and more than 80% reported reduced anxiety during treatment. 3 Hypnosis is beneficial as an adjunct intervention. However, dental anxiety ranges from mild to dental anxiety and the findings did not apply to patients with severe anxiety. 3 Overall, the evidence regarding the efficacy of hypnosis is still limited, and more research is required. 3
Wannemueller et al. (2011) also investigated the effectiveness of hypnosis. 23 The treatment methods included; cognitive behavioural treatment (CBT), standardized hypnosis delivered by a CD recording, individualized hypnosis with imagery carried out by a hypnotist, and finally, general anaesthesia. 23 The findings concluded that CBT was more efficacious than standardized hypnosis treatment; only 35% of participants in the CBT group reported having significant anxiety compared to 70% in the standardized hypnosis group. 23 The standardized hypnosis group had a higher rate of premature treatment termination than the CBT group. 23 The individualized hypnosis treatment showed the best results second to CBT but had the highest drop‐out rate of 54%. 23 Overall, CBT was the most successful treatment method for dental anxiety, and individualized hypnosis was the second most successful. However, with a low patient acceptance. 23 Individualized hypnosis was also markedly more successful than standardized hypnosis. 23
Eitner et al. (2011) conducted a prospective study to investigate the use of a novel audio pillow that could be attached to the dental chair. 22 The pillow provided the patient with hypnosis text and relaxation music, lowering dental anxiety by inducing a dissociated dream state. 22 Blood pressure, heart rate, and oxygen saturation levels were measured before, during and after surgery. 22 Results concluded; anxiety, intraoperative diastolic blood pressure and heart rate were substantially lower in the patients who listened to audio pillows compared with the control group. 21 Overall, the audio pillow's relaxation music and hypnotherapy had anxiolytic effects on patients undergoing dental implant surgery, potentially due to the patient's trance‐like state. 22 Patient feedback was positive, reporting improved comfort and dampening of stressful noises. 22 The study recommends further studies to confirm these findings. 22
AROMATHERAPY
Aromatherapy is one of the most effective non‐pharmacological techniques for anxiolysis and relaxation. 24 , 25 It uses essential oil aromas to alter a person's mind, mood/emotions, or cognitive function. 24 , 25 Aromatherapy can influence pain, anxiety relief and wound healing. 24 Therefore, a valuable, non‐pharmacological technique for dental anxiety management. 24 Many studies have investigated the effects of different types of essential oils on dental anxiety, such as; orange oil, chamomile oil, lavender oil and lemongrass oil. 24
In a randomized controlled trial, Baskran et al. (2019) assessed the effect of chamomile oil on dental anxiety for patients undergoing extractions. 26 Chamomile oil was placed in a diffuser, thus administering the oil through inhalation. 26 Results concluded; chamomile oil has aromatherapeutic properties, allowing patients to sustain a calm mental state and experience a significant decrease in dental anxiety levels. 26
Orange oil has sedative and anxiolytic properties as it is permeable through mucosal membranes, thus stimulating the central nervous system after passing through the blood‐brain barrier. 24 A study by Hasheminia et al. (2014) investigated the effect of ambient orange fragrance on patient anxiety during surgical removal of impacted third molars. 24 The results concluded that the mean blood pressure, pulse rate, and respiratory rate were significantly lower in the intervention group during surgery. 24 Therefore, orange fragrance effectively reduces anxiety during dental procedures. 24
Lavender oil is one of the most effective and preferable essential oils for aromatherapy. 27 Its sedative properties have been thoroughly researched and demonstrated in many studies. 27 Notably, Linalool is a key component in lavender oil, known to act on gamma‐aminobutyric acid (GABA‐A) receptors causing an inhibitory effect on the limbic system and autonomic transmission. 27 Subsequently, causing a decrease in blood pressure and anxiety levels. 27 Lavender oil has been shown to have similar effects to lorazepam but is considered more accessible and safer. 27
Karan (2019) investigated the influence of lavender oil inhalation on vital signs and anxiety in a randomized clinical trial. 27 The study involved inhaling lavender oil perioperatively versus no intervention. 27 The results showed a significant postoperative decrease in anxiety levels in both groups, possibly due to good patient communication and care. 27 Nevertheless, lavender oil produced a lower postoperative systolic blood pressure and intra‐operative respiratory rate. 27 This indicated reduced anxiety levels and a greater level of relaxation in the lavender group. 27 Overall, the study concluded that lavender oil inhalation provides a sedative effect based on the vital measurements and anxiety tests conducted and that it might be beneficial in patients with dental anxiety. 27 The study further suggests that it might reduce the need for anti‐psychotic medications. 27
Nardarajah et al. (2018) explored the anxiolytic effects of lavender oil, specifically for patients undergoing mandibular third molar removal. 25 The findings revealed a significant reduction in anxiety levels in the experimental group, concluding that lavender aromatherapy can reduce dental anxiety and be used as an adjunct treatment to control dental anxiety. 25 Additionally, lavender aromatherapy posed no adverse effects on the participants. 25 Lavender has antidepressant, sedative and calmative properties in addition to anti‐bacterial and anti‐fungal properties, supporting the use of lavender oil as an anxiolytic agent. 25 Upon inhalation, lavender oil stimulates the olfactory nerve cells, which alters GABA‐A receptors, thus stimulating the nervous and circulatory system much like benzodiazepines but with fewer side effects. 25
Lemongrass oil is another essential oil used in aromatherapy. 28 Rajaraman et al. (2019) conducted a prospective study, which evaluated the effectiveness of lemongrass aromatherapy on pain perception and anxiety levels during fixed prosthetic dental treatment. 28 The intervention group received diffused lemongrass oil in the room. 28 The results showed postoperative anxiety to be significantly lower than pre‐operative anxiety for the lemongrass intervention group. 28 Aromatherapy is a low cost and simple intervention that has proven to reduce dental anxiety, pain and improve emotional states in the dental setting. 28
ACUPUNCTURE
Auricular acupuncture is a minimally invasive technique that can reduce general and preoperative anxiety. 29 Anxiety occurs due to an imbalance in neurotransmitters such as GABA in the brain. 29 Auricular acupuncture relieves anxiety by modulating the autonomic nervous system, suppressing the sympathetic nervous system, and stimulating the parasympathetic nervous system, thus inhibiting noradrenaline production and reducing sympathetic hyperactivity. 29 Michalek‐Sauberer et al. (2012) investigated whether auricular acupuncture effectively reduced anxiety before dental treatment. 30 The results implied that auricular acupuncture at the relaxation, the tranquilizer and the master cerebral point, twenty minutes before ambulatory dental treatment, effectively reduces anxiety before dental treatment. 30 Hendrata et al. (2018) supported this conclusion, finding that auricular laser puncture in the same areas decreased the anxiety levels of patients undergoing dental procedures. 29 Laser acupuncture combines traditional acupuncture and modern treatment methods with lasers by stimulating acupuncture points with low‐intensity irradiated laser light. 29 The activation of GABA‐producing cells in the amygdala and hippocampus initiates the postsynaptic inhibitory transmission. 29 , 30 Subsequently, releasing serotonin, restoring balance and reducing anxiety. 29 , 30 Articular acupuncture is a simple and inexpensive treatment modality but requires special training and equipment. The limited but sound quality evidence indicated acupuncture is beneficial in reducing anxiety before treatment. 29
DOG‐ASSISTED THERAPY
Dog‐assisted therapy can provide positive and calming therapeutic relief while improving the physical and mental health of patients. 31 Cruz‐Fierro et al. (2019) conducted a pilot study to evaluate the effect of dog‐assisted therapy for patients with a history of anxiety related to dental visits. 31 The findings concluded that dog‐assisted therapy improves blood pressure and neurohormone levels, aiding anxiety management. Subsequently, patients reported reducing discomfort and improved experience at dental visits. 31 Although dog‐assisted therapy indicates improvements in patient experience, more research is required. 31
BRIEF INFORMATION
Many patients become anxious due to a loss of control or absence of understanding during treatment. 32 Therefore, explaining the procedure and discussing expectations, concerns and safety measures can alleviate anxiety. Cabbar et al. (2019) investigated if providing brief information would calm patients during different oral surgical procedures. 32 Patients who received written information before oral surgery did not report lower anxiety than controls. However, these patients were less anxious during surgery than were patients who did not receive the written information. 32 The results indicated a minor intraoperative benefit, which might have improved patient cooperation. 32 Tang et al. (2015) investigated the effect of dental health instruction before treatment on anxious patients with acute pulpitis. 33 Patients reported reduced pressure and anxiety relief during the treatment. Therefore, providing both written and verbal explanations of the operative procedure might be beneficial in alleviating anxiety. 33
MUSCLE RELAXATION
Muscle relaxation therapy can suppress the sympathetic nervous system response to psychological and physiological stimulation. 34 This technique lowers heart rate, respiratory rate, and blood pressure while regulating the peripheral and central nervous systems. 34 Subsequently, reducing stress, anxiety, and depression, thus effectively alleviating dental anxiety. 34 Park et al. (2018) investigated if progressive muscle relaxation therapy relieved dental anxiety. 34 The results concluded that muscle relaxation therapy over four sessions effectively alleviated dental anxiety for at least three months following the intervention. 34 Additionally, the intervention significantly reduced depressive symptoms, blood pressure, pulse rate, and salivary cortisol levels. Therefore, muscle relaxation therapy might be beneficial to reduce dental anxiety. 34
BIOFEEDBACK
The use of biofeedback devices allows both the patient and dentist to monitor the patient's physiological information. 35 The data assists the patient to practice control and self‐regulate the monitored physiological processes and down‐regulate the sympathetic nervous system. 35 Morarend et al. (2011) conducted a pilot study to investigate the use of a novel biofeedback device to reduce preoperative general anxiety levels. 35 The results demonstrated effectiveness in reducing dental anxiety and negative feelings regarding a dental injection. Therefore, respiratory rate‐biofeedback devices can reduce preoperative anxiety levels in the dental clinic. 35 However, implementing this technology into practice would require special instruments. 35
STIMULATION
Process simulations can reduce anxiety in a field setting where an imminent threat of physical discomfort is present. 36 Mental simulations involve imagining the process of conducting the task. 36 Armitage and Reidy (2012) presented evidence that process simulations significantly reduce anxiety before and after consultations. 36 Results were consistent with previous research; process simulation is clinically and statistically effective in reducing state anxiety. 36 The simulation also produced a prolonged effect post‐consultation. Further research is required to refine the technique and identify the other active components of this intervention program. 36
BRIEF COGNITIVE BEHAVIOURAL INTERVENTION
Cognitive and behavioural therapy can effectively ease dental anxiety or anxiety in both the short and long term. 37 However, the number of sessions in each study varies. Previous studies also suggest that brief interventions involving one to three sessions might effectively reduce dental anxiety, even long term. 37 Furthermore, brief interventions based on cognitive‐behavioural techniques might be equal or superior to other forms of intervention, and that their benefits persist over time. 37 Spindler et al. (2015) conducted a study to investigate the effect of a brief dental fear intervention based on cognitive‐behavioural principles specifically designed for the dental practice. 37 Findings concluded, when compared with a waiting list condition, the immediate treatment group showed a significant reduction in dental anxiety. 37 However, after both groups had completed the intervention, reductions in dental anxiety were comparable, and results were maintained at two years follow‐up, demonstrating, a brief cognitive‐behavioural intervention performed by the practising dentist might be sufficient for a significant proportion of fearful patients in overcoming their anxiety and attend dental treatment regularly. 37
CONCLUSION
This systematic review has discussed various strategies for managing dental anxiety in adult patients in the dental setting. Implementing a combination of techniques discussed is recommended for dentally anxious patients. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 A large population of adults suffer from dental anxiety. 1 , 2 Without a current and updated collation of dental anxiety management for adult patients within the clinic, many dental practitioners might lack the knowledge and awareness of the variety of strategies available to relieve anxiety and provide much‐needed treatment. Additionally, this review promotes further research for those management strategies that lacked a quantity of evidence. Many studies discussed similarities to previous research, validation and support for future studies. Acknowledgement of transparency develops confidence within these articles. Certain studies also mentioned require further research for the future development of the management to ensure integration into dental clinics.
This systematic review presented several limitations. The strict nature of the search terms and inclusion criteria omitted discussion of pharmacological management strategies, narrowing the scope of this review. Additionally, several interventions provided limited supporting evidence. Therefore, many techniques would benefit from additional research. Case reports were disregarded from this review to improve evidence quality and validity. Four articles were also excluded due to unavailable full‐text print. Hence, not all eligible articles were incorporated into this review.
This article intends to provide dental practitioners with the knowledge and understanding to help create an environment suitable for dentally anxious patients. Reducing dental anxiety improves patient reception to treatment while improving treatment outcomes and success for future appointments. Therefore, improving oral and general health. This publication is the primary method of information delivery to dental practitioners.
DISCLOSURE
Nothing to declare.
Acknowledgement
Open access publishing facilitated by James Cook University, as part of the Wiley ‐ James Cook University agreement via the Council of Australian University Librarians.
REFERENCES
- 1. Thoma M, Zemp M, Kreienbühl L, et al. Effects of music listening on pre‐treatment anxiety and stress levels in a dental hygiene recall population. Int J Behav Med 2015;22:498–505. 10.1007/s12529-014-9439-x [DOI] [PubMed] [Google Scholar]
- 2. Isik B, Esen A, Buyukerkmen B, Kilinc A, Menziletoglu D. Effectiveness of binaural beats in reducing preoperative dental anxiety. Br J Oral Maxillofac Surg 2017;55:571–574. 10.1016/j.bjoms.2017.02.014 [DOI] [PubMed] [Google Scholar]
- 3. Glaesmer H, Geupel H, Haak R. A controlled trial on the effect of hypnosis on dental anxiety in tooth removal patients. Patient Educ Couns 2015;98:1112–1115. 10.1016/j.pec.2015.05.007 [DOI] [PubMed] [Google Scholar]
- 4. Gujjar K, Sharma R, Jongh A. Virtual reality exposure therapy for treatment of dental phobia. Dent Update 2017;44:423–435. 10.12968/denu.2017.44.5.423.x [DOI] [PubMed] [Google Scholar]
- 5. Mejía‐Rubalcava C, Alanís‐Tavira J, Mendieta‐Zerón H, Sánchez‐Pérez L. Changes induced by music therapy to physiologic parameters in patients with dental anxiety. Complement Ther Clin Pract 2015;21:282–286. 10.1016/j.ctcp.2015.10.005 [DOI] [PubMed] [Google Scholar]
- 6. Moher D, Liberati A, Tetzlaff J, Altman D, The PRISMA Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. PROSPERO . International Prospective Register of Systemic Reviews. University of York Centre for Reviews and Dissemination Website. 2021. Available at: https://www.crd.york.ac.uk/prospero/#loginpage. Accessed 21 June 2021.
- 8. The University of Oxford. Oxford Centre for Evidence‐Based Medicine: Levels of Evidence (March 2009) . Centre for Evidence‐Based Medicine. 2009. https://www.cebm.ox.ac.uk/resources/levels‐of‐evidence/oxford‐centre‐for‐evidence‐based‐medicine‐levels‐of‐evidence‐march‐2009. Accessed 22 June 2021.
- 9. Aravena P, Almonacid C, Mancilla M. Effect of music at 432 Hz and 440 Hz on dental anxiety and salivary cortisol levels in patients undergoing tooth extraction: a randomized clinical trial. J App Oral Sci 2020;28:e20190601. 10.1590/1678-7757-2019-0601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mathivadani V, Anjali AK, Arivarasu L. Awareness regarding impact of music on patients anxiety during dental treatments. Eur J Mol Clin Med 2020;7:1032‐1042. https://www.scopus.com/inward/record.uri?eid=2‐s2.0‐85096895387&partnerID=40&md5=142565ba548e6565fa33856c8cc6b340. Accessed June 11 2021. [Google Scholar]
- 11. Gupta A, Ahmed B. Experience of listening to music on patient anxiety during minor oral surgery procedures: a pilot study. Brit Dent J 2020;228:89–92. 10.1038/s41415-019-1162-1 [DOI] [PubMed] [Google Scholar]
- 12. Kavarthapu A, Sharmila H, Reddy S. To compare the efficacy of alternative techniques in reduction of stress during dental extraction. J Adv Pharm Educ Res 2017;7:120‐123. https://www.scopus.com/inward/record.uri?eid=2‐s2.0‐85033410996&partnerID=40&md5=12c2ab465f2eda2058cdd84b2e2ca79f. Accessed 12 June 2021. [Google Scholar]
- 13. Wong CY, Saravanan C, Musawi A, Gan S. Effects of a combination of non‐pharmaceutical psychological interventions on dental anxiety. J Clin Transl Res 2018;3:311‐317. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6426253/. Accessed 3 June, 2021. [PMC free article] [PubMed] [Google Scholar]
- 14. Pintea S, Gatlan D, Kállay É, Jucan A. The effect of symphonic and lounge music upon anxiety and pain in a sample of Romanian dental patients. Cogn Brain Behav 2017;21:85–99. 10.24193/cbb.2017.21.06 [DOI] [Google Scholar]
- 15. Di Nasso L, Nizzardo A, Pace R, Pierleoni F, Pagavino G, Giuliani V. Influences of 432 Hz music on the perception of anxiety during endodontic treatment: a randomized controlled clinical trial. J Endod 2016;42:1338–1343. 10.1016/j.joen.2016.05.015 [DOI] [PubMed] [Google Scholar]
- 16. Gulnahar Y, Kupeli I. Effect of different kinds of music on anxiety during implant surgery in Turkey: randomized controlled study. Int J Oral Maxillofac Implants 2020;35:762–766. 10.11607/jomi.8329 [DOI] [PubMed] [Google Scholar]
- 17. Gujjar K, Van Wijk A, Sharma R, De Jongh A. Virtual reality exposure therapy for the treatment of dental phobia: a controlled feasibility study. Behav Cogn Psychother 2018;46:367–373. 10.1017/S1352465817000534 [DOI] [PubMed] [Google Scholar]
- 18. Gujjar K, van Wijk A, Kumar R, de Jongh A. Efficacy of virtual reality exposure therapy for the treatment of dental phobia in adults: a randomized controlled trial. J Anxiety Disord 2019;62:100–108. 10.1016/j.janxdis.2018.12.001 [DOI] [PubMed] [Google Scholar]
- 19. Yamashita Y, Shimohira D, Aijima R, Mori K, Danjo A. Clinical effect of virtual reality to relieve anxiety during impacted mandibular third molar extraction under local anesthesia. J Oral Maxillofac Surg 2020;78:545.e541–545.e546. 10.1016/j.joms.2019.11.016 [DOI] [PubMed] [Google Scholar]
- 20. La Paglia F, Daino M, Guarino D, et al. Virtual reality environments to reduce dental anxiety. Annu Rev Cyber Ther Telemed 2018;2018:175–178. https://www.scopus.com/inward/record.uri?eid=2‐s2.0‐85067860417&partnerID=40&md5=7a928ed68098632206197ff586563578 [Google Scholar]
- 21. Padrino‐Barrios C, McCombs G, Diawara N, De Leo G. The use of immersive visualization for the control of dental anxiety during oral debridement. J Dent Hyg 2015;89:372–377. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=med12&AN=26684994 [PubMed] [Google Scholar]
- 22. Eitner S, Sokol B, Wichmann M, Bauer J, Engels D. Clinical use of a novel audio pillow with recorded hypnotherapy instructions and music for anxiolysis during dental implant surgery: a prospective study. Int J Clin Exp Hypn 2011;59:180–197. 10.1080/00207144.2011.546196 [DOI] [PubMed] [Google Scholar]
- 23. Wannemueller A, Joehren P, Haug S, Hatting M, Elsesser K, Sartory G. A practice‐based comparison of brief cognitive behavioural treatment, two kinds of hypnosis and general anaesthesia in dental phobia. Psychother Psychosom 2011;80:159–165. 10.1159/000320977 [DOI] [PubMed] [Google Scholar]
- 24. Hasheminia D, Kalantar Motamedi M, Karimi Ahmadabadi F, Hashemzehi H, Haghighat A. Can ambient orange fragrance reduce patient anxiety during surgical removal of impacted mandibular third molars? J Oral Maxillofac Surg 2014;72:1671–1676. 10.1016/j.joms.2014.03.031 [DOI] [PubMed] [Google Scholar]
- 25. Nardarajah D, Dhanraj M, Jain A. Effects of lavender aromatherapy on anxiety levels of patients undergoing mandibular third molar extraction. Drug Invent Today 2018;10:1318–1322. https://www.scopus.com/inward/record.uri?eid=2‐s2.0‐85054931450&partnerID=40&md5=a18b5fdbd4dbf82d0b1fcb24618da00e [Google Scholar]
- 26. Baskran R, Lakshmanan R. Assessment of effect of chamomile oil on dental anxiety for patients undergoing extraction – a randomized controlled trial. Drug Invent Today 2019;11:1875–1879. https://www.scopus.com/inward/record.uri?eid=2‐s2.0‐85071514115&partnerID=40&md5=8fba174e3ae3590a1ba00c35f377f1a3 [Google Scholar]
- 27. Karan N. Influence of lavender oil inhalation on vital signs and anxiety: a randomized clinical trial. Physiol Behav 2019;211:112676. 10.1016/j.physbeh.2019.112676 [DOI] [PubMed] [Google Scholar]
- 28. Rajaraman V, Nallaswamy D, Ganapathy D, Manoharan S. Effect of aroma on pain perception and anxiety levels in patients undergoing fixed prosthetic dental treatment in dental clinic – a prospective study. Drug Invent Today 2019;11:98–103. https://www.scopus.com/inward/record.uri?eid=2‐s2.0‐85087205652&partnerID=40&md5=311ce1116e741fe5052317ca7338f1bf [Google Scholar]
- 29. Hendrata CJ, Mihardja H, Srilestari A, Amir N, Suhartoyo C. Effects of auricular laser puncture at the depressing, tranquilizer, and master cerebral points in patients with dental anxiety. 2nd Phys and Technol Med Dent Symposium. doi: 10.1088/1742-6596/1073/6/062040 [DOI]
- 30. Michalek‐Sauberer A, Gusenleitner E, Gleiss A, Tepper G, Deusch E. Auricular acupuncture effectively reduces state anxiety before dental treatment‐a randomised controlled trial. Clin Oral Invest 2012;16:1517–1522. 10.1007/s00784-011-0662-4 [DOI] [PubMed] [Google Scholar]
- 31. Cruz‐fierro N, Vanegas‐farfano M, González‐ramírez MT. Dog‐assisted therapy and dental anxiety: a pilot study. Animals 2019;9. 10.3390/ani9080512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cabbar F, Burdurlu M, Tomruk C. Does giving brief information keep patients calm during different oral surgical procedures? Quintessence Int 2018;49:817–828. 10.3290/j.qi.a40245 [DOI] [PubMed] [Google Scholar]
- 33. Tang Y, Du R. The effect of dental health instruction before treatment on anxiety of patients with acute pulpitis. J Stomatol 2015;24:483–485. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=med12&AN=26383577 [PubMed] [Google Scholar]
- 34. Park E, Yim H, Lee K. Progressive muscle relaxation therapy to relieve dental anxiety: a randomized controlled trial. Eur J Oral Sci 2019;127:45–51. 10.1111/eos.12585 [DOI] [PubMed] [Google Scholar]
- 35. Morarend Q, Spector M, Dawson D, Clark S, Holmes D. The use of a respiratory rate biofeedback device to reduce dental anxiety: an exploratory investigation. Appl Psychophysiol Biofeed 2011;36:63–70. 10.1007/s10484-011-9148-z [DOI] [PubMed] [Google Scholar]
- 36. Armitage C, Reidy J. Evidence that process simulations reduce anxiety in patients receiving dental treatment: randomized exploratory trial. Anxiety Stress Coping 2012;25:155–165. 10.1080/10615806.2011.604727 [DOI] [PubMed] [Google Scholar]
- 37. Spindler H, Staugaard S, Nicolaisen C, Poulsen R. A randomized controlled trial of the effect of a brief cognitive‐behavioral intervention on dental fear. J Publ Health Dent 2015;75:64–73. 10.1111/jphd.12074 [DOI] [PubMed] [Google Scholar]


