Abstract
Objectives
The pericapsular nerve group (PENG) block was first described for analgesia of hip fracture in 2018. We hypothesised that the PENG block is safe and effective for patients with hip fracture when provided by emergency physicians and trainees in the ED.
Methods
This was an observational study of routine care. Consecutive patients receiving regional anaesthesia for hip fracture at a single ED were prospectively enrolled. Pain scores were assessed prior to regional anaesthesia then at 15, 30 and 60 min after administration. Maximal reduction in pain scores within 60 min were assessed using the Visual Analogue Scale (at rest and on movement) or the Pain Assessment IN Advanced Dementia tool (at rest). Patients were followed for opioid use for 12 h after regional anaesthesia and adverse events over the duration of admission.
Results
There were 67 eligible patients during the enrolment period, with 52 (78%) prospectively enrolled. Thirty‐three received femoral blocks (19 fascia iliaca compartment blocks, 14 femoral nerve blocks) and 19 received a PENG block. Inexperienced providers were able to successfully perform the PENG block. There was no difference in maximum pain score reduction between the groups. There was no difference in adverse effects between groups. Opioid use was similar between the groups. More patients were opioid‐free after a PENG block.
Conclusions
The present study demonstrated that the PENG block can be provided safely and effectively to patients with hip fracture in the ED. On the basis of this pilot study, a larger randomised controlled study should now be designed.
Keywords: hip fracture, neck of femur, PENG block, regional anaesthesia, ultrasound
The PENG block is a recently described regional anaesthetic technique for analgesia of hip fractures and hip surgery. This pilot study compares the PENG block to femoral nerve block and fascia iliaca block for patients with hip fracture in the ED. The PENG block is feasible, safe and effective when performed by emergency physicians.

Key findings.
The PENG block is safe and effective for hip fracture in the ED.
More patients were opioid‐free after a PENG block.
Introduction
Proximal femur fractures (including neck of femur fracture) simply referred to as hip fractures, are a common, painful condition of patients presenting to the ED who are typically elderly and frail. 1 , 2 Hip fractures are associated with significant morbidity and mortality and the disease burden is expected to increase. 1 , 2 ED management of these patients should incorporate multimodal analgesia, including regional anaesthesia, 3 which can improve comfort and reduce opioid‐related harm. 4
The fascia iliaca compartment block (FICB) and femoral nerve block (FNB), hereafter combined and referred to as femoral blocks (FBs), are both widely accepted as the current standard of care for regional anaesthesia of hip fractures in the ED. 3 Both of these blocks provide femoral nerve blockade for anaesthesia of the femur and cause lower limb motor block. 5 , 6 There is limited evidence that one is superior in effectiveness to the other. 7 , 8
The pericapsular nerve group (PENG) block is a recently described regional anaesthetic technique that may be superior to FB for elderly patients with hip fractures, given the potential for more complete anaesthesia of the joint capsule with motor sparing effects. 9 , 10 The technique utilises sonographic and tactile bony landmarks to inject local anaesthetic into the iliopsoas plane at a site distant from blood vessels (Fig. 1). The sensory branches of the femoral nerve (FN) and accessory obturator nerve (AON) that innervate the anterior hip capsule traverse the iliopsoas plane over the anterior surface of the ilium between the iliopubic eminence medially and the anterior inferior iliiac spine laterally 11 where they are anaesthetised by the PENG block. 12
Figure 1.
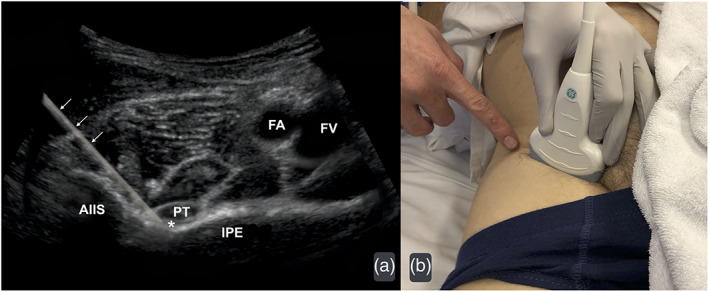
(a) Ultrasonographic view of right sided anatomical landmarks for the pericapsular nerve group block, with superimposed needle trajectory (arrows) and target injection site (*). (b) Demonstration of patient and probe positioning with needle insertion site indicated. AIIS, anterior inferior iliac spine; FA, femoral artery; FV, femoral vein; IPE, iliopubic eminence; PT, psoas tendon.
In contrast, effective FB relies on cranial spread of anaesthetic to block proximal branches of the FN, which then travel caudally within the iliacus muscle via the iliopsoas plane to the anterior hip capsule. 11 FB does not block the AON, which is present in up to 54% of patients. 11 The anterior hip capsule is also innervated by articular branches of the obturator nerve (ON) in 83–98% of patients. 11 The articular branches of ON are not blocked by FB 13 but may be variably anaesthetised by the PENG block. 14 There have been no prior comparative studies of the PENG block in ED patients.
Existing literature supporting the PENG block for hip fractures is limited. 15 Comparative literature for the PENG block is limited to the investigation of perioperative use of the technique by anaesthetists. 10 , 16 , 17 , 18 , 19 A perioperative study showed the PENG block to be superior to suprainguinal FICB prior to patient positioning for spinal anaesthesia. 16
The objective of the present study was to confirm the feasibility of the PENG block in everyday ED practice and to compare the safety and effectiveness of the PENG block to FB for patients with hip fracture in the ED. We hypothesised that it is safe and effective for emergency medicine clinicians to provide the PENG block for patients presenting to ED with a hip fracture. The primary outcome was the maximal reduction in pain score (Visual Analogue Scale [VAS] and Pain Assessment IN Advanced Dementia [PAINAD]) assessed at rest within 60 min of administration of regional anaesthesia.
Methods
Study design and setting
This was a single‐centre prospective, pragmatic, observational cohort study of routine care conducted between October 2019 and July 2020 in the ED of a large regional centre in northern New South Wales, Australia. This regional hospital had an ED census of around 33 000 adult patients in 2019. The study was endorsed by emergency and anaesthetic specialists at the hospital and was approved by the North Coast New South Wales Human Research and Ethics Committee and prospectively registered in the Australian New Zealand Clinical Trials Registry (ACTRN12619001410145). We adhered to the STrengthening the Reporting of OBservational studies in Epidemiology statement (https://strobe-statement.org/).
Selection of participants
Patients were considered for the study if they had a suspected proximal femur fracture. To be eligible for inclusion, a proximal femur fracture (neck of femur, intertochanteric or peritrochanteric fracture), had to be confirmed on either radiograph or computed tomography reported by a radiologist, and the patient treated with regional anaesthesia (FICB, FNB or PENG block), performed by an emergency physician or trainee. In addition, patients had to be prospectively enrolled with pain scores recorded on a designated clinical research form (CRF). Exclusion criteria included age younger than 18 years, sub‐trochanteric fracture and regional anaesthesia provided at another location. Patients were screened 24 h a day, 7 days a week to ensure consecutive recruitment. Participant consent was waived for this observational study of routine practice. Clinicians were not masked to the study objectives.
Interventions
Patients were treated at the discretion of their treating clinician, without influence or specifications from the investigators. The experience of the clinician performing the regional anaesthesia technique was prospectively documented. All blocks were performed using US guidance and ropivacaine 75–150 mg. Lignocaine (up to 100 mg) was added to ropivacaine for three blocks in each group, which is known to accelerate the onset of regional anaesthesia. 20 No dexamethasone, or other anaesthetic adjunct medication, was added to injectate for any patient. FICB were performed using an infrainguinal technique. Injectate volume varied between groups, with providers mostly using 40 mL (range 20–40 mL) for FICB, 20 mL (20–30 mL) for FNB and 20 mL (15–40 mL) for PENG block.
Outcome measures
Pain scoring was scheduled immediately prior to regional anaesthesia, at 15, 30 and 60 min post regional anaesthesia, and then hourly until 12 h post regional anaesthesia or operative treatment. Clinicians asked patients to mark a 100 mm VAS on the CRF, or the PAINAD 21 tool was used for patients with severe cognitive impairment.
The VAS tool was selected to assess pain in patients without cognitive impairment as it has been widely used in the existing literature comparing FICB to FNB. 8 , 22 , 23 PAINAD was employed to facilitate the inclusion of patients with significant cognitive impairment. The protocol planned for VAS and PAINAD scores to be used interchangeably for analysis of the primary outcome, similarly to the numerical rating scale (NRS) 24 and PAINAD scores being used interchangeably studies comparing FICB to FNB, 7 and assessing chemical denervation of the hip for patients with inoperable osteoarthritis. 25
Scores were documented by clinicians on the CRF on a scale from 0 to 10. When VAS was used, pain was scored at rest and on movement (attempted gentle hip flexion). PAINAD scores were only recorded at rest. When pain scores were documented on the CRF but the VAS tool had not been marked, the investigators assumed that the NRS had been used, in keeping with routine practice at this centre. NRS has been validated to correlate with VAS. 24 , 26
Opioid use was recorded pre‐hospital, including by the ambulance service or at the referring hospital, and in the ED during the pre‐block time period and until 12 h post block or the patient entered the operating theatre. These data were available to the investigators via the electronic medical record and ambulance service patient records. Opioid use was converted to oral morphine milligram equivalent (MME) using the Australian and New Zealand College of Anaesthetists Faculty of Pain Medicine Opioid Calculator. 27
Adverse events (AEs) were identified from the electronic medical record, using truncated keyword search within the admission date range for the following terms: ‘aspiration’, ‘delirium’, ‘sedation’, ‘naloxone’ and ‘constipation’. The electronic medication chart was searched within the admission date range for naloxone and antibiotic prescription and correlated with any association with iatrogenic opioid overdose or infections from regional anaesthesia.
The primary outcome was the maximal reduction in pain score at rest within 60 min of regional anaesthesia. Prespecified secondary outcomes included pain score reduction on movement, opioid use, onset time of regional anaesthesia (defined as the first recorded pain score of 1.5 less than the baseline score) and AEs.
Sample size
The sample size calculation was based on previous literature, which used VAS, 8 or PAINAD and NRS combined. 7 We aimed to detect a clinically significant difference in pain score reduction of 1.5 out of 10 points with a standard deviation of 2.4, a power of 80% and a two‐sided alpha of 0.05. Based on previous literature, 7 , 23 we assumed that the FICB and FNB groups would be sufficiently similar to combine as a single data set to compare to the PENG block, with a 2:1 allocation ratio. Therefore, the sample size calculated for the study was 74 patients, including at least 25 in the PENG block group. Consecutive patients were enrolled over 9 months from October 2019 to July 2020.
Data analysis
Data were entered into an Excel (version 2008; Microsoft, Redmond, WA, USA) spreadsheet and then analysed in IBM SPSS Statistics (version 26; IBM, Armonk, NY, USA). Normality of the data was assessed using the Shapiro–Wilk test. Basic descriptive statistics (counts, frequencies and mean and standard deviation (for normally distributed continuous variables) and median and interquartile range (IQR) for non‐normally distributed data. Graphs of the primary outcome were produced in Python v37.0, showing actual data points, medians and the 95% confidence intervals around the medians.
Results
Characteristics of study subjects
There were 67 eligible patients during the enrolment period, with 52 (78%) prospectively enrolled. Thirty‐three received femoral blocks (19 FICB and 14 FNB) and 19 received a PENG block (Fig. 2). Recruitment to the study was terminated early due to COVID‐19 restrictions impacting the investigators' ongoing access to the study site. All 52 eligible patients were included in the final analysis.
Figure 2.
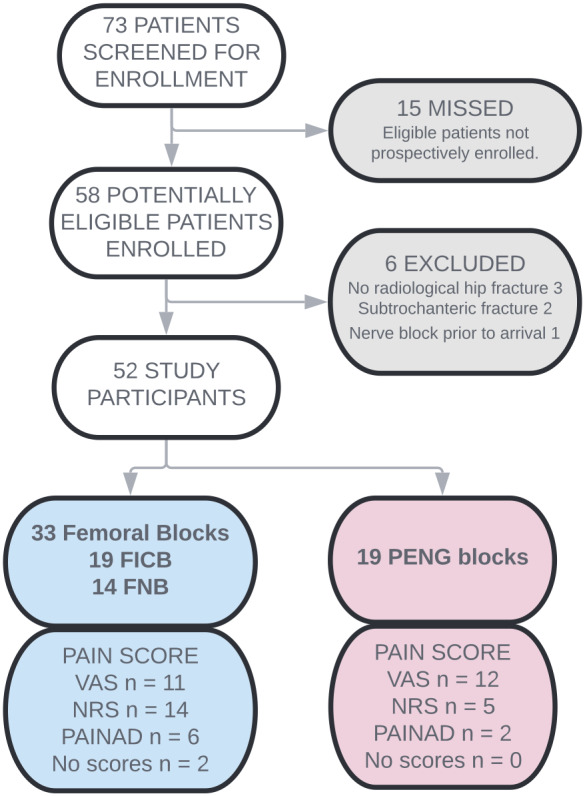
Patient enrolment flow chart. FICB, fascia iliaca compartment block; FNB, femoral nerve block; NRS, numerical rating scale; PENG, pericapsular nerve group; VAS, Visual Analogue Scale; PAINAD, Pain Assessment IN Advanced Dementia.
A comparative analysis was conducted of baseline characteristics of the two patient groups: FB and PENG blocks (Table 1). Patient demographics were similar between groups. Patients from the FB group were more likely to suffer chronic pain, although opioid use at baseline was similar. The groups differed in fracture type, with patients who received FB having a higher proportion of extracapsular fractures. Three patients had significant concurrent painful injuries, two from the PENG block group (contralateral Weber‐C ankle fracture and anterior shoulder dislocation) and one from the FB group (distal radius fracture). Operators providing the PENG block were significantly less experienced in the technique than operators providing FB.
TABLE 1.
Baseline characteristics of study cohort
| All (n = 52) | Femoral block (n = 33) | PENG block (n = 19) | ||||
|---|---|---|---|---|---|---|
| Characteristic | n | % | n | % | n | % |
| Sex = F | 33 | 63.0 | 22 | 66.7 | 11 | 58.0 |
| Fracture type = extracapsular | 23 | 44.0 | 18 | 54.5 | 5 | 26.3 |
| Comorbidities | ||||||
| Chronic pain | 10 | 19.2 | 8 | 24.2 | 2 | 11.0 |
| Regular opioid use at baseline | 5 | 10.0 | 2 | 6.1 | 3 | 15.8 |
| Cognitive impairment | 10 | 19.2 | 5 | 15.2 | 4 | 21.1 |
| Operator experience | ||||||
| First time | 9 | 17.3 | 2 | 6.1 | 7 | 36.8 |
| 1–4 | 17 | 32.7 | 9 | 27.3 | 8 | 42.1 |
| >4 | 26 | 50.0 | 22 | 66.7 | 4 | 21.1 |
| Opioid use prior to block (any) | 47 | 90.4 | 30 | 90.9 | 17 | 89.5 |
| Median (IQR) | Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | Mean (SD) | |
|---|---|---|---|---|---|---|
| Age | 84.5 (74.25–89) | 81.1 (11.7) | 83 (74.5–89) | 81.2 (9.7) | 86 (72–89) | 80.9 (14.8) |
| Pre‐block opioid dose (MME) | 30 (15–39) | 29.1 (20.9) | 30 (15–39) | 31.0 (21.1) | 16 (8–37.5) | 26.0 (20.9) |
| Baseline pain score at rest | 4 (0.9–6.0) | 4.1 (3.3) | 4.5 (0.9–6.5) | 4.3 (3.4) | 3.8 (0.8–6.0) | 3.7 (3.1) |
| Baseline pain score on movement | 9 (7.9–10) | 8.6 (1.8) | 10 (8–10) | 9.1 (1.2) | 8 (6–10) | 7.7 (2.4) |
| Time from triage to block (min) | 168.5 (119.8–310) | 241.3 (196.9) | 150 (119–235) | 213.8 (183.2) | 234 (138–369) | 288.9 (215.4) |
Femoral block, fascia iliaca compartment block or femoral nerve block; IQR, interquartile range; MME, oral morphine milligram equivalent; PENG, pericapsular nerve group; SD, standard deviation.
Main results
There was no difference in pain score reduction within 60 min between groups when measured at rest or when measured on movement (Table 2). Absolute pain scores at 60 min were similar (Fig. 3). Pain score recording in the first hour was good (85% of scheduled scores were recorded). However, from 2 to 12 h post block, only 3% of scheduled scores were recorded, this data is not presented. NRS was used in place of VAS in 19 of the 44 patients without significant cognitive impairment (Fig. 2). No patient was lost to follow up.
TABLE 2.
Outcomes by block type
| Characteristic | All (n = 52) | Femoral block (n = 33) | PENG block (n = 19) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Scale and continuous variables | Valid, n | Median (IQR) | Mean (SD) | Valid, n | Median (IQR) | Mean (SD) | Valid, n | Median (IQR) | Mean (SD) |
| Maximum pain score reduction at rest | 50 | 2 (0–5.13) | 2.8 (3.0) | 31 | 2 (0–6) | 2.9 (3.0) | 19 | 2 (0–5) | 2.6 (3.1) |
| Maximum pain score reduction on movement | 40 | 3.2 (2.0–5.0) | 3.7 (2.7) | 24 | 3.2 (2.0–5.0) | 3.8 (2.7) | 16 | 3.4 (1.0–5.1) | 3.5 (2.9) |
| Time of onset assessed at rest (min) | 28 | 15 (15–30) | NA | 17 | 15 (15–60) | NA | 11 | 15 (15–30) | NA |
| Time of onset assessed on movement (min) | 32 | 15 (15–30) | NA | 21 | 30 (15–30) | NA | 11 | 15 (15–30) | NA |
| Post block opioid use 6 h post block (MME) | 52 | 7.5 (0–15) | 8.8 (11.1) | 33 | 7.5 (0–15) | 9.9 (10.7) | 19 | 0 (0–10) | 7.0 (11.8) |
| Post block opioid use 12 h post block (MME) | 52 | 21.25 (7.5–37.5) | 16.1(13.9) | 33 | 23 (15–37.5) | 18.1 (12.3) | 19 | 8 (0–25.75) | 12.7 (16.0) |
| Total opioid use at 6 h (MME) | 52 | 32 (21–46.5) | 37.9 (28.4) | 33 | 37.5 (22.5–52) | 40.8 (27.6) | 19 | 30 (8–37.5) | 33.0 (29.8) |
| Total opioid use at 12 h (MME) | 52 | 44.25 (30.0–68.25) | 54.1 (40.0) | 33 | 52.5 (31–82.5) | 58.9 (37.2) | 19 | 39 (8–45.5) | 45.7 (44.2) |
| Duration of admission (days) | 52 | 9 (6–11.75) | 10.8 (8.6) | 33 | 8 (6–10) | 8.9 (5.1) | 19 | 10 (6–15) | 14 (12.1) |
| Yes or no variables | Valid, n | n (%) | Valid, n | n (%) | Valid, n | n (%) | |||
| Opioid free for 6 h post block | 52 | 21 (40.4) | 33 | 11 (33.3) | 19 | 10 (52.6) | |||
| Opioid free for 12 h post block | 52 | 9 (17.3) | 33 | 3 (9.1) | 19 | 6 (31.6) | |||
| Rescue block during first 6 h | 52 | 2 (3.8) | 33 | 1 (3.0) | 19 | 1 (5.3) | |||
| New onset delirium during admission | 52 | 11 (21.2) | 33 | 9 (27.3) | 19 | 2 (10.5) | |||
| New onset constipation during admission | 52 | 9 (17.3) | 33 | 7 (21.2) | 19 | 2 (10.5) | |||
Femoral block, fascia iliaca compartment block or femoral nerve block; IQR, interquartile range; MME, oral morphine milligram equivalent; PENG, pericapsular nerve group; SD, standard deviation.
Figure 3.
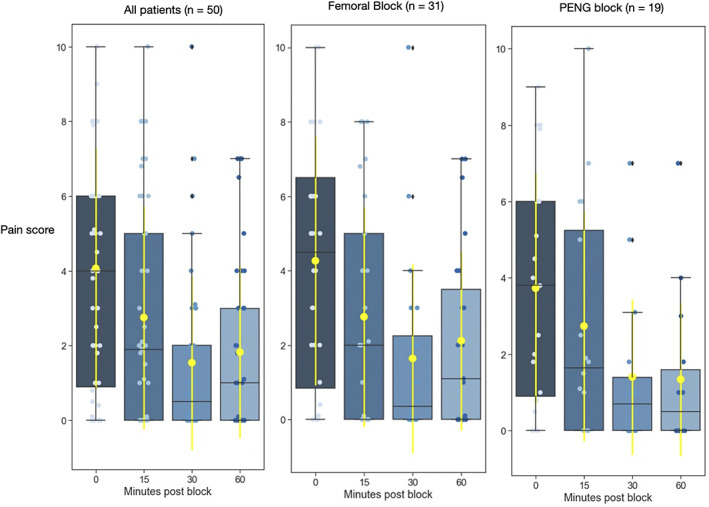
Pain scores over time. Boxes indicate the interquartile range bisected at the median. Black whiskers show the distribution, excluding outliers. Yellow dots and lines show mean and standard deviation. Blue dots are individual data points. Femoral block, femoral nerve block or fascia iliaca compartment block; PENG, pericapsular nerve group.
Opioid use was statistically similar in the 12 h period after regional anaesthesia (median MME of 8 mg for PENG block vs 23 mg in the FB group) (Table 2). However, more patients were opioid‐free for 6 h after regional anaesthesia in the PENG block group (53% vs 33% FB) and for the duration of follow up (31% vs 9% FB). The median onset times were similar.
AEs were similar between groups (Table 2). No regional anaesthesia associated infections were detected during admission. One patient from each group required a rescue block provided by an anaesthetist prior to operative fixation. One patient with a FICB had a repeat FICB using landmark technique. One patient with a PENG block had a femoral nerve catheter inserted. Three patients were checked in to the operating theatre prior to 12 h post regional anaesthesia (one PENG block and two FBs).
Discussion
In this pragmatic, single‐centre observational study of patients with hip fracture in ED, there was no difference observed in maximal pain score reduction within 60 min for the PENG block compared to FB. This pilot study demonstrates that the PENG block is feasible, safe and effective when provided in the ED by a group of providers relatively inexperienced in the technique. This is the first study to report on routine use of the PENG block in ED and the first prospective comparison to other techniques (FICB and FNB) in the ED.
Opioid‐sparing is important in the elderly population because of its potential morbidity. In our study, more patients were opioid‐free after a PENG block, although we did not detect a significant difference in median opioid use. The data on opioid use had excellent capture because of the strict mandatory recording of these regulated medications. In addition, we were able to account for potential confounders between groups, including concurrent injuries, baseline opioid tolerance or attending the operating theatre less than 12 h from regional anaesthesia.
The PENG block has several characteristics highlighted by the present study that make it attractive to ED clinicians. First, it was straightforward for inexperienced providers to perform successfully, which is likely because of bony sonographic landmarks and tactile bony endpoint of needle insertion. Also, the risk of local anaesthetic systemic toxicity is innately minimised as the target injection site is distant from vascular structures, and there were no reported differences in AEs compared to FB.
A strength of the present study was use of VAS and PAINAD, allowing inclusion of patients with cognitive impairment, who are often excluded from regional anaesthesia research 28 despite representing a third of the disease burden for hip fracture. 23 , 28 Having clinicians, rather than research assistants, enrol patients and record data allowed for a 78% prospective recruitment rate with consecutive (24/7) screening. However, this resulted in a heterogeneous data set as NRS was often used in place of VAS. Combining FICB and FNB as a single treatment arm for data analysis was reasonable based on previously established similar effectiveness. 7 , 23 However, when our data were divided into three treatment arms, we found the FICB and FNB group differed significantly in baseline pain scores and pain score reduction was not equal (Tables S1 and S2).
There were several limitations to the present study. First, it was a single‐centre, non‐randomised study, subject to potential selection bias. Clinicians were unable to be blinded and, given the open‐label nature of the study, clinicians were aware of the intervention of interest and could be subject to the Hawthorne effect. 29 Pain score recording after 60 min was too sparse to provide any information on the duration of action of any of the regional anaesthetic techniques provided. However, there was excellent capture of opioid use from the time of injury until 12 h post regional anaesthesia, which provides another objective measure of pain. AEs were reviewed retrospectively, although all the important AEs were likely to have been captured.
Conclusions
This first comparative study of the PENG block versus FICB and FNB demonstrates the PENG block to be feasible, safe and effective when provided by everyday ED clinicians. A larger multi‐centre randomised controlled study should now be designed to determine whether the PENG block is superior to FICB or FNB for patient‐centred outcomes in patients with hip fracture in ED.
Supporting information
Appendix S1. Raw data.
Table S1. Baseline characteristics of three way‐comparison study cohort. FICB, fascia iliaca compartment block; FNB, femoral nerve block; IQR, interquartile range; MME, oral morphine milligram equivalent; PENG, pericapsular nerve group block.
Table S2. Outcomes by block type – three treatment arms. FICB, fascia iliaca compartment block; FNB, femoral nerve block; IQR, interquartile range; MME, oral morphine milligram equivalent; PENG, pericapsular nerve group block.
Acknowledgements
This trial was made possible with the support of the Northern NSW Health Service and Lismore Base Hospital. The authors thank Justin Dryden for conducting the retrospective analysis preceding the present study and for data collection and entry. The authors thank Neil Stokes, Gerben Keijzers and Alexandre Stephens for their guidance in moving the present study from an idea to a reality, and Morwenna Haywood for Figure 1a. The authors thank Stefan Jantschulev for his enthusiasm for the project and teaching us the PENG block. Open access publishing facilitated by Bond University, as part of the Wiley ‐ Bond University agreement via the Council of Australian University Librarians.
Competing interests
None declared.
Abridged results were presented as a poster at the Australian and New Zealand College of Anaesthetists (ANZCA) special interest group rural practice meeting on 13 June 2021 at Airlie Beach, Queensland, Australia. Awarded Mackay Institute of Research and Innovation Rolling Trophy.
Data availability statement
The data that supports the findings of this study are available in Appendix S1 of this article.
References
- 1. Dyer SM, Crotty M, Fairhall N et al. A critical review of the long‐term disability outcomes following hip fracture. BMC Geriatr. 2016; 16: 158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lystad RP, Cameron CM, Mitchell RJ. Mortality risk among older Australians hospitalised with hip fracture: a population‐based matched cohort study. Arch. Osteoporos. 2017; 12: 67. [DOI] [PubMed] [Google Scholar]
- 3. Australian Commission on Safety and Quality in Health Care . Hip Fracture Care Clinical Care Standard. Sydney: Australian Commission on Safety and Quality in Health Care, 2016. [Google Scholar]
- 4. Guay J, Parker MJ, Griffiths R, Kopp SL. Peripheral nerve blocks for hip fractures: A Cochrane review. Anesth. Analg. 2018; 126: 1695–704. [DOI] [PubMed] [Google Scholar]
- 5. Ilfeld BM, Duke KB, Donohue MC. The association between lower extremity continuous peripheral nerve blocks and patient falls after knee and hip arthroplasty. Anesth. Analg. 2010; 111: 1552–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Xing JG, Abdallah FW, Brull R et al. Preoperative femoral nerve block for hip arthroscopy: A randomized, triple‐masked controlled trial. Am. J. Sports Med. 2015; 43: 2680–7. [DOI] [PubMed] [Google Scholar]
- 7. Cooper AL, Nagree Y, Goudie A, Watson PR, Arendts G. Ultrasound‐guided femoral nerve blocks are not superior to ultrasound‐guided fascia iliaca blocks for fractured neck of femur. Emerg. Med. Australas. 2019; 31: 393–8. [DOI] [PubMed] [Google Scholar]
- 8. Newman B, McCarthy L, Thomas PW, May P, Layzell M, Horn K. A comparison of pre‐operative nerve stimulator‐guided femoral nerve block and fascia iliaca compartment block in patients with a femoral neck fracture. Anaesthesia 2013; 68: 899–903. [DOI] [PubMed] [Google Scholar]
- 9. Kukreja P, Avila A, Northern T, Dangle J, Kolli S, Kalagara H. A retrospective case series of pericapsular nerve group (PENG) block for primary versus revision total hip arthroplasty analgesia. Cureus 2020; 12: e8200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Allard C, Pardo E, de la Jonquière C et al. Comparison between femoral block and PENG block in femoral neck fractures: a cohort study. PLoS One 2021; 16: e0252716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Short AJ, Barnett JG, Gofeld M et al. Anatomic study of innervation of the anterior hip capsule: Implication for image‐guided intervention. Reg. Anesth. Pain Med. 2018; 43: 186–92. [DOI] [PubMed] [Google Scholar]
- 12. Giron‐Arango L, Peng PWH, Chin KJ et al. Pericapsular nerve group (PENG) block for hip fracture. Reg. Anesth. Pain Med. 2018; 43: 859–63. [DOI] [PubMed] [Google Scholar]
- 13. Swenson JD, Davis JJ, Stream JO, Crim JR, Burks RT, Greis PE. Local anesthetic injection deep to the fascia iliaca at the level of the inguinal ligament: The pattern of distribution and effects on the obturator nerve. J. Clin. Anesth. 2015; 27: 652–7. [DOI] [PubMed] [Google Scholar]
- 14. Nielsen ND, Bendtsen TF. In response: Motor blockade after iliopsoas plane (IPB) and pericapsular nerve group (PENG) blocks: A little may go a long way. Acta Anaesthesiol. Scand. 2021; 65: 137–8. [DOI] [PubMed] [Google Scholar]
- 15. Morrison C, Brown B, Lin DY, Jaarsma R, Kroon H. Analgesia and anesthesia using the pericapsular nerve group block in hip surgery and hip fracture: A scoping review. Reg. Anesth. Pain Med. 2021; 46: 169–75. [DOI] [PubMed] [Google Scholar]
- 16. Jadon A, Mohsin K, Sahoo RK, Chakraborty S, Sinha N, Bakshi A. Comparison of supra‐inguinal fascia iliaca versus pericapsular nerve block for ease of positioning during spinal anaesthesia. Ind. J. Anaesth. 2021; 65: 572–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Aliste J, Layera S, Bravo D et al. Randomized comparison between pericapsular nerve group (PENG) block and suprainguinal fascia iliaca block for total hip arthroplasty. Reg. Anesth. Pain Med. 2021; 46: 874–8. [DOI] [PubMed] [Google Scholar]
- 18. Lin DY, Morrison C, Brown B et al. Pericapsular nerve group (PENG) block provides improved short‐term analgesia compared with the femoral nerve block in hip fracture surgery: A single‐center double‐blinded randomized comparative trial. Reg. Anesth. Pain Med. 2021; 46: 398–403. [DOI] [PubMed] [Google Scholar]
- 19. Pascarella G, Costa F, Del Buono R et al. Impact of the pericapsular nerve group (PENG) block on postoperative analgesia and functional recovery following total hip arthroplasty: A randomised, observer‐masked, controlled trial. Anaesthesia 2021; 76: 1492–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Valery P, Aliaksei M. A comparison of the onset time of complete blockade of the sciatic nerve in the application of ropivacaine and its equal volumes mixture with lidocaine: A double‐blind randomized study. Korean J. Anaesthesiol. 2013; 65: 42–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Warden V, Hurley AC, Volicer L. Development and psychometric evaluation of the pain assessment in advanced dementia (PAINAD) scale. J. Am. Med. Dir. Assoc. 2003; 4: 9–15. [DOI] [PubMed] [Google Scholar]
- 22. Ritcey B, Pageau P, Woo MY, Perry JJ. Regional nerve blocks for hip and femoral neck fractures in the emergency department: A systematic review. CJEM 2016; 18: 37–47. [DOI] [PubMed] [Google Scholar]
- 23. Wang X, Sun Y, Wang L, Hao X. Femoral nerve block versus fascia iliaca block for pain control in total knee and hip arthroplasty: A meta‐analysis from randomized controlled trials. Medicine 2017; 96: e7382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bijur PE, Latimer CT, Gallagher EJ. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad. Emerg. Med. 2003; 10: 390–2. [DOI] [PubMed] [Google Scholar]
- 25. Kwun‐Tung Ng T, Chan WS, Peng PWH, Sham P, Sasaki S, Tsui HF. Chemical hip denervation for inoperable hip fracture. Anesth. Analg. 2020; 130: 498–504. [DOI] [PubMed] [Google Scholar]
- 26. Bahreini M, Safaie A, Mirfazaelian H, Jalili M. How much change in pain score does really matter to patients? Am. J. Emerg. Med. 2020; 38: 1641–6. [DOI] [PubMed] [Google Scholar]
- 27. Australian and New Zealand College of Anaesthetists . Opioid Calculator; 2020. Available from URL: http://www.opioidcalculator.com.au/opioidsource.html
- 28. Mundi S, Chaudhry H, Bhandari M. Systematic review on the inclusion of patients with cognitive impairment in hip fracture trials: a missed opportunity? Can. J. Surg. 2014; 57: 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J. Clin. Epidemiol. 2014; 67: 267–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Raw data.
Table S1. Baseline characteristics of three way‐comparison study cohort. FICB, fascia iliaca compartment block; FNB, femoral nerve block; IQR, interquartile range; MME, oral morphine milligram equivalent; PENG, pericapsular nerve group block.
Table S2. Outcomes by block type – three treatment arms. FICB, fascia iliaca compartment block; FNB, femoral nerve block; IQR, interquartile range; MME, oral morphine milligram equivalent; PENG, pericapsular nerve group block.
Data Availability Statement
The data that supports the findings of this study are available in Appendix S1 of this article.


