Abstract
Background
The body index [body mass, body mass index (BMI), waist circumference and waist–height ratio] and functional fitness (aerobic capacity, muscular strength, balance, flexibility and functional ability) of people with Down syndrome (DS) are substantially lower than those in the general population, as DS has an overall negative impact on health.
Aims
This study explored the effect of a 24‐week basketball training programme on the body composition and functional fitness of adults with DS.
Methods and procedure outcomes
Twenty‐two adults with DS (24 ± 6 years; 25 ± 4 kg/m2) were randomly allocated to the experimental (n = 11, 67.04 kg) and control groups (n = 11, 69.36 kg). The experimental group performed 24 weeks of basketball programme training (3 times per week, 60 min per session), while the control group maintained their daily activities without any special physical training. Body composition and functional fitness parameters were measured before and after the intervention. To evaluate the differences between groups, an analysis of covariance (ANCOVA) was used while controlling for differences at baseline.
Results
Hip circumference and waist–height ratio were statistically different at baseline between the intervention and control groups. After the 24‐week basketball training programme, the results showed significant differences between the exercise and control groups for hip circumference, body mass, BMI, waist circumference, hip circumference, waist–height ratio, flexibility, aerobic capacity, static and dynamic balance, balance and basketball functional ability (P < 0.05). The exercise group showed significant improvements in all variables of body composition and functional fitness (P < 0.05) except for the waist–hip ratio. There was no statistical significance between all physical composition and functional health variables in the control group except for the standing long jump (P > 0.05), with effect sizes ranging from small to large.
Conclusions and implications
The basketball training programme improved body composition and functional fitness of adults with DS.
Keywords: basketball programme, body composition, Down syndrome, functional fitness, intellectual disability
Introduction
Down syndrome (DS) is a chromosomal anomaly produced by a partial or full extra copy of chromosome 21 that negatively impacts the physical and intellectual development of individuals, most of whom are born with or develop conditions or illnesses that affect their quality of life (Roizen & Patterson 2003; Pikora et al. 2014; de Asua et al. 2015; Ruiz‐González et al. 2019; Boer 2020). The majority of people with DS (70–75%) are only able to reach an intelligence quotient between 20 and 50 (Vicari 2006). DS affects about 1/1000 newborn babies worldwide and is the most common single intellectual disability (ID) (Menkes & Falk 2006; Presson et al. 2013; Suarez‐Villadat et al. 2020). Functional fitness components such as cardiorespiratory endurance, muscular strength and endurance, flexibility, balance, functional ability and appropriate body composition are important for the health and well‐being of any population group. Limitations in functional fitness hamper people's ability to live an independent and disease‐free life (Rikli & Jones 2013).
A literature review reveals that people with DS exhibit higher levels of overweight or obesity when compared with those with other IDs or without any ID (Bertapelli et al. 2016; Suarez‐Villadat et al. 2020). Moreover, studies on the body composition of people with DS have shown higher levels in most of the relevant body composition indicators [body mass index (BMI), waist circumference and waist‐to‐height ratio (WtHR)] compared with people without ID (González‐Agüero et al. 2010; Izquierdo‐Gomez et al. 2015; Suarez‐Villadat et al. 2019; Suarez‐Villadat et al. 2020). Improved physical fitness is also related to reduced body fat percentage in this population (Salaun & Berthouze‐Aranda 2012). Furthermore, a high body fat percentage has been linked to low physical and functional ability in DS (Salaun & Berthouze‐Aranda 2012). A study has suggested that a 36‐week swimming programme consisting of 3 sessions lasting 50 min each was able to improvement of body composition in a sample population of adolescents with DS (Suarez‐Villadat et al. 2020).
Although the life expectancy of these individuals has increased markedly as a consequence of improved medical treatment options, the population still ages prematurely, and their quality of life deteriorates even further with age (Torr et al. 2010; Arumugam et al. 2016). Besides, poor physical fitness and functional capacity are factors that further predispose people with DS to the early development of serious health problems (Gonzalez‐Aguero et al. 2010; Torr et al. 2010). One way to improve, delay or counter the numerous challenges for individuals with DS is to enhance their functional fitness. Functional fitness refers to possessing the physical capacity to perform normal everyday activities safely and independently without undue fatigue (Rikli & Jones 2013).
Recent studies on adults with DS showed that different forms of exercise improve functional fitness (aerobic fitness, balance, flexibility, function, muscle strength, weight or BMI), including walking, running, cycling, dragon boating or resistance training (Pieter & Beer 2019). Team sports, such as basketball, can be a popular way for individuals with ID to get involved in physical activity. Basketball is considered as a common activity for people with ID, because it incorporates both motor skills (e.g. running, jumping and shooting) and social aspects (Baldari et al. 2009). It is also a popular activity among people with ID as it allows quick participation in the activity. It is highly important that the players get involved in the personal–situational interaction of basketball, high decision‐making processes, understand the game and so forth. (Briere & Siegle 2008; Baldari et al. 2009; Baran et al. 2009; Alruwaih 2015). Basketball ability has been assessed in players with ID, and the tests established four levels of ability, each one characterised by four fundamental areas of this game: ball handling, reception, passing and shooting. Conducted basketball training also resulted in significant improvement in examined sport skills performance (Guidetti et al. 2009; Kocić et al. 2017).
One study demonstrated that 8 weeks of a specially adapted basketball training programme improved physical fitness in adolescents with ID. Such physical activity and the nature of basketball, which necessitates interaction and decision‐making in a variety of situations, can be a means of improving social interaction (Stanišić et al. 2012). However, to the best of our knowledge, no research has yet explored the effects of basketball training specifically on the physical composition and functional fitness of adults with DS. Therefore, there is a need for relevant experimental research to gather additional data. Our research team consists of experts from various disciplines, such as special medicine of sports science, and has designed the basketball programme in this study to provide more comprehensive support for adults with DS. Because some of the core features of DS are inadequate fitness and functional impairment, this study tries to explore the effect of a 24‐week basketball programme on the body composition and functional fitness containing sport skills performance in adults with DS.
Materials and methods
Participants
With the support and ethic approval of the researcher's university and local government, this research was initiated and collaborated with the Wuhu Intellectual Disabilities Association. Twenty‐eight participants aged 18–40 years were recruited from the Wuhu Intellectual Disabilities Association (Wuhu, P. R. China). Five adults were excluded or refused to attend due to the aforementioned reasons. The eligible participants were assigned to exercise group (n = 11) and control group (n = 12). Finally, one participant in the control group was unable to take the final test due to family reasons for withdrawing from this intervention, and 22 participants completed the entire intervention (Fig. 1).
Figure 1.
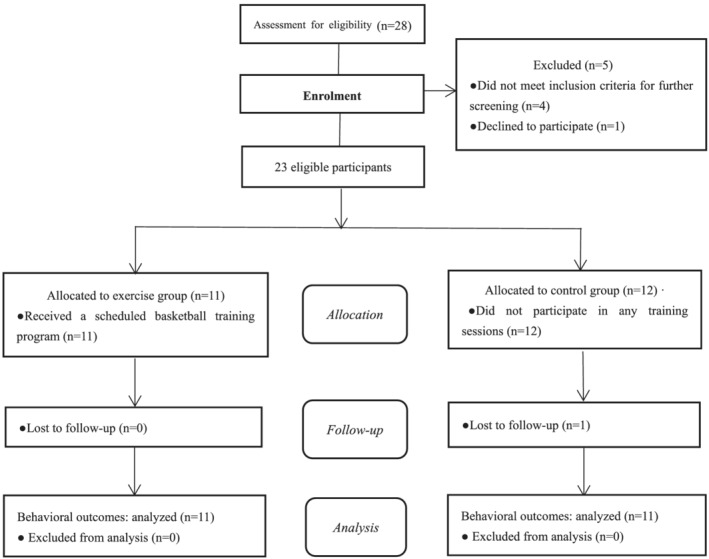
Participant flow characteristics. *One adult Down syndrome participant did not finish the post‐test assessment.
Our study, which has a quasi‐experimental design with the group defined as the inter‐subject factor and the time point as the intra‐subject factor, included 22 adults (18 men and 4 women) with DS (24.7 ± 6 years). The participants were randomly allocated to experimental and control groups (11 participants per group). Group allocation was determined by participants drawing a number from a hat. The study was approved by the institutional ethics committee (AHNU‐ET2021028), and the author ensured that the work described has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. Risk assessment analyses were conducted, and the obtained mitigation measures were provided to the ethical committee. All parents had to sign an informed consent form. All participants signed an adapted consent form written in a simpler language. The study was conducted in Wuhu (China) from December 2020 to June 2021.
Inclusion and exclusion criteria
Participants were excluded if (1) they had participated in basketball training or regular physical exercise in the past 6 months; (2) they had congenital heart disease or any other chronic physical and mental illness limiting their physical activity; or (3) they were diagnosed with cognitive execution and comprehension impairment.
Measurements
Assessment of body composition and functional fitness
Participants' body composition and functional fitness were measured twice, before and after the intervention, and variables were recorded as the mean of the two measurements before and after the intervention. The relevant procedures, such as the average of two measurements, have been validated for use in adolescents and adults with DS by multiple studies (Tejero‐Gonzalez et al. 2013; Boer & Moss 2016a; Ruiz‐González et al. 2019). The average of two measurements was validated by these researchers.
Body mass index
Stature and body mass measurements were conducted using a Seca scale and stadiometer (Seca, Hamburg, Germany). Each participants wore a shirt and light‐weight trouser only (Boer & Moss 2016b). Height was measured in the range of 70–200 cm, and weight was measured in the range of 5–200 kg, with measurement accuracies of 0.1 cm and 0.1 kg, respectively (Zhang et al. 2021). Body mass (kg) and height (cm) measurements were used to calculate BMI.
Waist and hip circumference, waist‐to‐hip ratio and waist‐to‐height ratio
In order to estimate central body fat, the candidates' abdomen was measured using a non‐elastic tape by taking the narrowest point between the iliac crest and the costal margin as a reference (Seca 200; Seca) (Savva et al. 2000). When measuring the weight circumference (WC), the subject was asked to breathe normally and wear thin clothes, and the measuring tape was placed to about 0.5–1.0 cm above the navel. For measuring the hips, the position of the greatest circumference at the buttocks was used. The measurement accuracy of WC and hips was required to be within 0.1 cm (Zhang et al. 2021).
Waist‐to‐hip ratio (WHR) is the ratio of waist to hip circumference and is a simple measure for assessing obesity. It is evaluated by dividing one's waist circumference by one's hip circumference (Zhang et al. 2021). WtHR is a simple measure of assessing overweight. WtHR is evaluated by dividing a person's waist by the person's height and is used to assess the body distribution of fat (Suarez‐Villadat et al. 2020).
Aerobic fitness
Cardiorespiratory endurance or aerobic capacity was assessed using the 16‐m modified shuttle‐run test or PACER test. It has been shown to be both feasible and reliable [intraclass correlation coefficient (ICC) = 0.99] in adults with DS (Boer & Moss 2016b). Moreover, it has been proved to be valid (R 2 = 0.86) when assessed with the gold standard maximal oxygen uptake test using a standardised treadmill protocol for adults with DS (Boer & Moss 2016c). In the test, to the sound of a tape‐recorded beep, participants ran between two lines that were 16 m apart. The final test score recorded was the number of successfully completed shuttles. The test instructor ran alongside the participant to help with turning and pacing.
Balance
Static balance was evaluated with the participants standing on one leg for as long as they could to a maximum period of 10 s while looking straight ahead and with their hands placed firmly on their hips. The knee of the free leg was bent such that the lower leg was parallel to the floor (Boer & Moss 2016b).
Dynamic balance was assessed by walking on a 3.05‐m balance beam that was 10.2 cm wide. Participants were instructed to walk with a normal stride while keeping their hands on their hips. The number of consecutive steps completed on the balance beam was recorded up to a maximum of six steps. Two trials were administered in both tests, and the best score was noted. Test–retest reliability for the balance tests was excellent (ICC for static balance = 0.98; the ICC for dynamic balance = 0.93), as shown in adults with DS (Boer & Moss 2016b).
Muscular strength
Participants laid in a supine position with the knees bent, feet flat on the floor and their hands on their thighs. They slid their fingers up along the upper legs to the kneecap while performing a curl‐up and then returned to the initial starting position. The participants performed as many curl‐ups as possible (up to a maximum of 75) for as long as required by doing one curl‐up approximately every 3 s. The test feasibility and test–retest reliability were shown to be excellent (ICC = 0.99) for adults with DS (Terblanche & Boer 2013; Boer & Moss 2016b).
The standing long jump mainly measures the explosive force of the lower limbs. A line was drawn on clean, flat ground and the participants with DS were required to stand on the line with their feet, keep their feet apart, cooperate with their arms and jump forward from the ground, and then to land on the ground at the same time. We measured the distance between the line to the heel twice consecutively and then recorded the best result (Guidetti et al. 2010). The test feasibility and test–retest reliability were shown to be excellent (ICC range 0.90–0.99) (Mac Donncha et al. 1999).
Flexibility
The sit‐and‐reach test assesses lower body flexibility. Each leg needs to be extended straight out in front of the hip, with the heel kept on the floor and the ankle flexed at 90° (the other leg is bent off to the side with the foot flat on the floor). With the hands overlapped and the middle fingers even, the participant had to reach as far as possible to the toes. If the tip of the middle finger did not touch the toe, the distance short of the middle toe was measured and recorded as a negative score; when the middle finger reached beyond the toes, the distance of overlap was measured and recorded as a positive score. The same procedure was followed with the other leg. The test–retest reliability of this test item revealed an ICC value of 0.95 in an elderly population (Rikli & Jones 2013). The measurement of hamstring flexibility estimated the standard correlation effectiveness in older men (r = 0.76) and older women (r = 0.81) (Rikli & Jones 2013). The discriminant validity of this test has been reported in adults with DS between age categories (18–25, 26–35, 36–45 and >45) (Terblanche & Boer 2013).
Basketball programme
Number of single‐handed dribbles in 1 min
When Coach A said ‘start’, the subject began to bounce the ball (dribbled) at their fastest speed. Coach B measured the number of bounces. When Coach A said ‘stop’, the tester stopped dribbling the ball, and Coach B stopped counting and reported the count to Coach C for recording.
One‐minute free shot
When Coach A said ‘start’, the subject could choose any position below the basket to shoot. Coach B measured the number of shots that went into the basket. When Coach A said ‘stop’, the subject had to stop shooting, and Coach B stopped counting and reported the result to Coach C for recording.
During the pilot phase of the study, the maximum reliability of single‐handed dribbles per minute and free shots in a minute was determined. Two practice trials were administered, and the tests were conducted 1 week apart. For the single‐handed dribble in 1 min and free shots in 1‐min tests, ICCs of 0.922 and 0.946 and a standard error of the mean (SEM) of 2.228 and 0.217, respectively, were shown.
Training programme
The basketball training programme of this study was based on previously described protocols (Bagherly & Ghasemi 2012; Zhu et al. 2017; Cai et al. 2020). The programme was conducted primarily in a collective class, providing much interaction and communication for DS. All training interventions were structured to achieve physical health benefits. Both groups continued with their normal everyday activities during the intervention period. Their daily routine did not include structured physical activity. Participants in the control group performed no structured exercises.
All of the activities were strictly supervised. The basketball programme comprised 3 days of exercise per week for 24 consecutive weeks (72 sessions in total). Each session lasted 60 min and comprised the following three stages: (1) warm up with various games for 10 min; (2) 45 min of basic basketball skill learning (shooting, passing and handling) and physical training; and (3) relaxing exercises for 5 min. The 24‐week basketball programme was divided into three phases to achieve different targets: (a) Phase I (3 weeks) – arousing the interest of participants with DS in basketball and standardised classroom routines; for participants with DS and their parents, the main content was simple but interesting basketball training. At this stage, participants with DS learned standard behaviour and classroom routines such as taking turns, waiting, listening to and carrying out instructions, familiarity with basic shooting and dribbling techniques. (b) Phase II (15 weeks) – improving the skills and physical fitness of adults with DS. (c) Phase III (6 weeks) – improving basketball actual game ability and physical fitness of adults with DS. See the descriptive information for basketball training in Tables 1 and 2.
Table 1.
Basketball programme content and goals for each session
| Category | Content | Goal | Duration |
|---|---|---|---|
| Classroom routine | Line up, classroom greetings, roll call etc. | Standardise classroom routines | 2 min |
| Warm‐up activities | Jogging, stretching, game, limb exercises etc. | Warm‐up | 8 min |
| Basketball training programme |
Phase I: basic basketball training Phase II: basketball skill learning and game Phase III: physical fitness training |
Basketball skills development and improvement of physical fitness | 45 min |
| Cool‐down activities | Relaxation exercise and summary | Review, summary, reward, stretching | 5 min |
Table 2.
Basketball programme protocol
| Phase | Goal | Content | Duration |
|---|---|---|---|
| Phase I |
Raise the interest of adults with DS in fun‐packed basketball standardised classroom routines |
Classroom routines (taking turns, waiting, carrying out instructions etc.) Basic basketball skills‐training along with music (roll and throw the ball, dribbling, passing, shooting relay racing etc.) |
3 weeks |
| Phase II | Improve basketball skills and physical quality of adults with DS |
Peer coordination training (basket‐moving shooting, rebounds passing, catching the ball, relay racing etc.) Basketball game (one on one and two on two) |
15 weeks |
| Phase III |
Improve strength and physical fitness of adults with DS |
Physical fitness training (continuous jump, 1‐min high‐lift and kick practice, duck walking etc.) Basketball game (three on three, five on five etc.) |
6 weeks |
DS, Down syndrome.
The basketball programme was conducted in a 28‐m long, 15‐m wide, international standard basketball court of Basketball Qixing Sports Club in Yijiang District, Wuhu City, China. Participants could rest in the middle of the class. Continuous basketball training was strictly controlled by basketball coaches using body language, demonstrations and whistle signals. Three qualified basketball coaches (FIBA‐certified coaches) assisted in all training activities. The purpose of the basketball programme was to include varying degrees of difficulty, so that the coach could give training at the appropriate level. This may also have motivated adult DS participants to move towards a higher level in the course of the training programmes.
Procedures
Before the training programme, all participants completed the 12‐body composition and functional fitness tests. During the first assessment day, body mass, height, waist and hip circumference, balance (static: standing on one leg; dynamic: walking on a balance beam) and flexibility (sit‐and‐reach test) were measured. On the second day, the two muscular strength tests (modified curl‐up and standing long jump) and the aerobic capacity test (16‐m PACER) were performed. One‐minute single‐handed dribble and 1‐min shooting tests were also conducted. The same tests were repeated after 24 weeks in the same order and at the same time of day as the initial assessments. Familiarisation sessions were conducted before the commencement of the study for all baseline tests. All tests were visually demonstrated and explained step by step to the participants. The participants practised each test on their own under the supervision of the test instructor. A healthcare doctor and three basketball coaches were always on the premises during training and testing.
All testing procedures and methods, including technique and number of trials and demonstrations, were followed exactly as outlined in the Bruininks–Oseretsky, BPFT and the SFT manuals. All tests allowed two familiarisation and practice sessions 1 week prior to testing. Sufficient rest was allocated during testing days.
Statistical analysis
Data were analysed by the Statistical Package for the Social Sciences (SPSS 25.0, Chicago, IL, USA). A significance level of P < 0.05 was used. The study followed an ‘intention to treat’ and not the ‘effect of treatment’ procedure (Lewis & Machin 1993). All data were screened for normality and homogeneity of variance using the Shapiro–Wilk statistic and Levene's test, respectively. Analysis of variables that violated the assumption of normality (Shapiro–Wilk) was assessed by the Mann–Whitney (inter‐group) and Wilcoxon signed‐rank (intra‐group) non‐parametric tests. Data were presented as mean (standard deviation). Significant differences between groups before the intervention were analysed with an independent samples T‐test. To evaluate differences between groups, an analysis of covariance (ANCOVA) was used, controlling for differences at baseline. A paired sample T‐test was assessed within groups, before and after the intervention. Statistically significant differences were presented in bold (P < 0.05). The test–retest relative reliability of data for the 1‐min single‐handed dribble and free shots in 1‐min tests was assessed with the ICC by using ANOVA. This model treats all sources of measurement variation as error, providing an accurate estimate of the reliability of stability. The test–retest absolute variability was measured by using the SEM to calculate the minimal detectable change at 90% confidence interval (MDC90) (Stratford 2004).
The Cohen's d effect sizes were calculated. The magnitude of the effect sizes was classified as small (0.10 to <0.30), medium (0.30 to <0.50) or large (≥0.50), as per Cohen (1988). Effect sizes were calculated between groups as well as pre‐training to post‐training within groups.
Results
All enrolled participants were able to complete the 12‐body composition and functional fitness test items. No serious or adverse events occurred during baseline, intervention or post‐testing. The intervention period saw excellent adherence, as 10 of the 11 participants attended more than 90% of the exercise sessions (nine had 100% attendance). The participant with the lowest adherence attended 67% of all sessions. The average attendance rate of participants was 96.7% for all courses. The test–retest reliability analysis for single shots in 1 min and free shots in 1‐min tests revealed ICC values of 0.922 and 0.946, SEM values of 2.228 and 0.217 and MDC90 values of 2.09 and 93.18, respectively, for the single shots in 1 min and free shots in 1‐min tests.
The assumption of homogeneity of variances (Levene's test) was violated for none of the variables, and the assumption of normality (Shapiro–Wilk) was violated for the two balance tests, modified curl‐up test, sit‐and‐reach test and the two basketball tests. As a result, the analysis for these variables was performed by the Mann–Whitney (between‐group) and Wilcoxon signed‐rank (within‐group) non‐parametric tests. After 24 weeks of following in the basketball programme, the results showed a statistically significant improvement in all body composition and functional health variables in the exercise group except WHR (all featured P < 0.05). The control group showed no statistically significant difference between all body composition and functional health variables except for the standing long jump (all featured P > 0.05). The comparisons between the two groups on the post‐test, based on the results of the ANCOVA, revealed statistical significance (P < 0.05) for all indicators except waist–hip ratio. On the post‐test, the exercise group had a significantly lower body mass, BMI, waist circumference, hip circumference and WtHR and better flexibility, sit‐and‐reach and modified curl‐up, aerobic capacity, static and dynamic balance and functional basketball ability than the control group (P < 0.05). The aforementioned information is shown in Table 3.
Table 3.
Influence of basketball programme on parameters of body composition and functional fitness
| Body composition | Exercise group (n = 11) | Control group (n = 11) | |||
|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||
| Body mass (kg) | 67.04 (10.21) | 63.68 (10.62)* , † | 69.36 (7.52) | 69.60 (6.93) | |
| BMI (kg/m2) | 25.58 (3.43) | 24.28 (3.55)* , † | 24.84 (2.45) | 24.93 (2.30) | |
| Waist circumference (cm) | 92.91 (6.99) | 87.55 (6.49)* , † | 87.18 (9.56) | 87.40 (8.53) | |
| Hip circumference (cm) | 99.73 (5.27) | 96.91 (5.92)* , † | 99.95 (4.31) | 100.18 (4.45) | |
| Waist–hip ratio (%) | 0.94 (0.05) | 0.92 (0.05) | 0.99 (0.10) | 0.99 (0.10) | |
| Waist–height ratio (%) | 0.58 (0.06) | 0.54 (0.05)* , † | 0.52 (0.06) | 0.52 (0.05) | |
| Sit‐and‐reach test (cm) | −2.69 (11.58) | 6.00 (8.99)* , † | −6.68 (12.00) | −5.00 (11.30) | |
| Modified curl‐up (n) | 10.18 (5.81) | 16.00 (8.83)* , † | 8.82 (4.58) | 9.36 (3.47) | |
| Standing long jump (cm) | 93.64 (23.19) | 108.73 (21.97)* , † | 92.73 (11.01) | 92.57 (10.74) | |
| Standing on one leg (s) | 3.17 (1.46) | 5.43 (1.12)* , † | 3.79 (0.65) | 4.45 (0.78) | |
| WOBB (steps) | 3.26 (1.11) | 5.24 (0.96)* , † | 3.17 (0.87) | 3.30 (0.58) | |
| 16‐m PACER (shuttles) | 19.16 (2.04) | 24.16 (1.96)* , † | 19.07 (1.58) | 19.08 (1.12) | |
| One‐minute single‐handed dribble (n) | 93.18 (18.93) | 155.91 (23.49)* , † | 83.27 (18.10) | 84.36 (12.99) | |
| One‐minute shot (n) | 2.09 (1.14) | 4.91 (1.97)* , † | 1.82 (0.87) | 1.91 (0.70) | |
P < 0.05 significant difference within group.
P < 0.05 significant difference between exercise and control groups.
Data are presented as mean (standard deviation).
BMI, body mass index; n, amount; WOBB, walking on balance beam.
The between‐group effect sizes were larger for body mass, hip circumference, waist–hip ratio, sit‐and‐reach test, modified curl‐up and standing long jump, static and dynamic balance, and 16‐m PACER and basketball functional ability. The between‐group effect sizes for WtHR were medium, and effect sizes were smaller for BMI and waist circumference. In the exercise group, the effect sizes were large for all indicators except WHR, which had a medium effect size. In the control group, the effect sizes were larger for hip circumference and single leg stance, the effect sizes were medium for the sit‐and‐reach test and walking on balance beam and the effect sizes were small for all other indicators (Table 4).
Table 4.
Effect sizes of functional body composition and functional fitness parameters (between and within groups)
| Variable | Between groups | Exercise group (within) | Control group (within) | |||
|---|---|---|---|---|---|---|
| Effect size | Magnitude | Effect size | Magnitude | Effect size | Magnitude | |
| Body composition | ||||||
| Body mass | 0.66 | Large | 4.818 | Large | 0.253 | Small |
| BMI | 0.219 | Small | 3.657 | Large | 0.281 | Small |
| Waist circumference | 0.019 | Small | 1.347 | Large | 0.066 | Small |
| Hip circumference | 0.687 | Large | 1.916 | Large | 0.564 | Large |
| Waist–hip ratio | 0.923 | Large | 0.320 | Medium | 0.060 | Small |
| Waist–height ratio | 0.389 | Medium | 1.242 | Large | 0.062 | Small |
| Flexibility | ||||||
| Sit‐and‐reach test | 1.077 | Large | 2.705 | Large | 0.470 | Medium |
| Muscular strength | ||||||
| Modified curl‐up | 0.989 | Large | 0.916 | Large | 0.285 | Small |
| Standing long jump | 0.701 | Large | 2.052 | Large | 0.228 | Small |
| Static and dynamic balance | ||||||
| Standing on one leg | 1.017 | Large | 2.747 | Large | 0.597 | Large |
| WOBB | 2.438 | Large | 3.683 | Large | 0.362 | Medium |
| Aerobic capacity | ||||||
| 16‐m PACER | 3.183 | Large | 3.274 | Large | 0.016 | Small |
| One‐minute single ball and shot | ||||||
| One‐minute single‐handed dribble | 3.77 | Large | 3.185 | Large | 0.087 | Small |
| One‐minute shot | 2.027 | Large | 2.871 | Large | 0.087 | Small |
BMI, body mass index; WOBB, walking on balance beam.
Discussion
This study analysed the effect of a 24‐week basketball programme on the body composition and functional fitness of adults with DS. Both groups continued with their normal everyday activities during the intervention period. The control group performed no structured exercises. No serious or adverse events transpired during the study. The main findings were that adults with DS in the exercise group showed a decrease in all body composition indicators and an increase in all functional body indicators after 24 weeks of basketball training. Meanwhile, the control group had essentially no changes, with the exception of the standing long jump and the sit‐and‐reach tests. Hip circumference and waist–height ratio were statistically different at the baseline.
This study used three phases: the first phase used basic basketball skills learning (shooting, passing and handling) and physical training to increase adult DS patients' interest in fun basketball; the second phase used peer coordination training (basket moving, rim passing, catching, relay races etc.) basketball games (one on one and two on two) to improve their skills and fitness; and the third phase used physical training (continuous jumping, 1‐min high lifts, kicking exercises, duck walking etc.) basketball games (three on three, five on five etc.) aimed at improving their strength and fitness. The fact that so many parameters of body composition and functional fitness showed significant improvement is promising, given that many studies conducted on adults with DS reported considerable improvements on certain components of body composition and functional fitness (Rimmer et al. 2004; Mendonca et al. 2011, 2013; Lin & Wuang 2012; Boer & Moss 2016a; Suarez‐Villadat et al. 2020). Basketball is a common sport for people with mental disabilities (Baldari et al. 2009). It is a popular activity among people with DS as it allows them to participate quickly and gets them involved in personal–situational interactions, high decision‐making processes, understanding the game and so forth (Briere & Siegle 2008; Baldari et al. 2009; Baran et al. 2009; Alruwaih 2015).
These research data showed that the basketball training programme was effective in significantly decreasing most indicators of body composition (BMI, waist circumference, hip circumference and WtHR) in adults with DS after they followed the programme for 24 weeks. These findings are in good agreement with other studies performed in the DS population (Bertapelli et al. 2016). A study that compared ‘intermittent sprint training’ with ‘aerobic continuous training’ showed no significant difference in BMI between the two groups after the intervention, although it reported a significant reduction in body fat and that intermittent sprint training was more effective (Boer et al. 2014). BMI decreased less in this study, which essentially agreed with our results. Subject height changes before and after the intervention could be ignored; therefore, weight changes before and after the intervention determined the BMI changes.
Our study showed that, compared with the control group, the interventional group apparently improved through basketball activity, especially in five indicators: body mass, BMI, waist circumference, hip circumference and waist–height ratio. This may be because the basketball programme contains group games (basketball‐dribbling‐relay, basketball‐passing relays, basket‐moving shooting etc.) including ‘intermittent sprint training’ and ‘aerobic continuous training’, as basketball is considered both ‘interval sprint training’ and ‘aerobic continuous training’, thus involves both kinds of exercise.
As shown by the muscle strength and flexibility tests, improvements in adult participants with DS in the exercise group were found. The increments observed in physical fitness were consistent with previous studies demonstrating improvements in physical fitness after regular exercise. Studies performed on individuals with DS have demonstrated the importance of adequate muscle strength, due to its relationship with functional performance and everyday living activities (Cowley et al. 2010; Terblanche & Boer 2013). Our study showed that standing long jumps and modified curl‐us apparently improved and resulted in large effect sizes. Because the basketball programme was the main content of the training programme in the present study, it comprised much of the practice in basketball with a focus on speed–agility and muscle strength (i.e. basic basketball skills) as well as physical fitness training, such as lower limb strength training, using continuous jumps, duck walking, 1‐min high lifts and kick practice training methods. Intensity and exercise gradually improved in the study participants with DS doing the training programme. Subject to the tolerance range of participants, coaches could monitor their performance in real time. Flexibility was greatly improved, which may be related to stretching the whole body during basketball warm‐up and the relaxing stretching at the end. In contrast, the improvement in the standing long jump and seated forward bend in the control group may be due to the fact that the participants with DS had not fully mastered the test technique at the initial test but they had got accustomed to the technique by the second test.
The results of this study revealed a significant improvement with a large effect size for both static and dynamic balance. Dynamic balance has also been shown to improve with swimming or aquatic training performed by elderly individuals and children with cerebral palsy (Hsu et al. 2010; Zverev & Kurnikova 2016). Studies have reported that appropriate balance skills are one of the most difficult sets of skills to acquire but are a major factor in the safety and independence of children with DS (Jung et al. 2017). Unfortunately, many individuals with DS exhibit poor static and dynamic balance as compared with the general population (Carmeli et al. 2002; Tsimaras & Fotiadou 2004; Villamonte et al. 2010). Static and dynamic balance are also essential for individuals with DS, as revealed by an association between these measures and physical independence, along with the ability to participate in leisure and social activities (Villamonte et al. 2010). Our study demonstrated significant improvement in both static and dynamic balance, which may be attributed to the need for coordination skills in basketball training (passing and catching the ball, shooting, relay racing etc.) as well as part of the game involving the warm‐up process that includes balancing training.
The aerobic capacity abilities of the participants increased significantly with a large effect size, which may be related to the direct encounters in the basketball game (one on one, three on three and five on five). Many studies using a combination of aerobic and resistance training reported significant improvements in aerobic capacity for individuals with DS (Rimmer et al. 2004; Lewis & Fragala‐Pinkham 2005; Mendonca et al. 2011, 2013). Basketball is an intermittent team sport, which requires a high level of anaerobic and aerobic fitness (Delextrat et al. 2018). The last two basketball training tests revealed a significant improvement with a large effect size for both dribble and shot. These results were very similar to the study of assessing basketball ability in players with ID (Guidetti et al. 2009; Kocić et al. 2017). However, the increase in the number of single‐handed dribbles in 1 min was greater than the increase in shots in 1 min. One reason for this finding may be that, during the intervention period, the number of participants was large, and the number of shots and time for each participant was small in comparison, such that the grasp of shooting technique could not develop appropriately.
The success of this study provides evidence for easy and manageable sports interventions that can be administered even by non‐professionals and can be promoted across cultures and countries to meet the needs of DS globally applicable intervention models for adults. A limitation of this study is that the level of intellectual impairment could not be determined, as no intelligence quotient records were available for the participants. However, all participants in the current study fully understood the test instructions, test procedures, correct technique and training procedures. Secondly, generalisation of results is also limited by the small number of participants and sample structure (subjects were of similar age and gender ratio varies). Thirdly, while the basketball coach encouraged the participants to exercise at the highest possible intensity and to conduct pre‐basketball activities, there was no guarantee that all participants did their best (i.e. no endpoint of maximum performance was established). Future tests should take a larger sample size and design more comprehensive tests for body composition and functional adaptability indicators while monitoring exercise intensity and heart rate.
Conclusions
In this work, a basketball programme intervention was implemented to assess its potential effects on body composition and functional fitness parameters of young adults with DS. The programme was met with excellent adherence without any serious or adverse events. Participation in the basketball programme significantly improved many of the studied parameters, some of which previously shown to be improved when studied individually in adults with DS.
Source of funding
This research was supported by the Anhui Provincial Philosophy and Social Science Foundation (AHSKY2020D78) and University Natural Science Research Project of Anhui Province (KJ2020A0059).
Conflict of interest
No conflicts of interest have been declared.
Acknowledgements
The authors want to thank all participants and their parents that participated in the study for their understanding and dedication.
Cai, W. , and Baek, S.‐S. (2022) Effects of 24‐week basketball programme on body composition and functional fitness on adults with Down syndrome. Journal of Intellectual Disability Research, 66: 939–951. 10.1111/jir.12951.
Data availability statement
The data (descriptive statistics) used to support the findings of this study are included within the article. The source data (SPSS table with original measurements; testing and activities videos) used to support the findings of this study are available from the author upon request.
References
- Alruwaih M. E. (2015) Effects of soccer unified program on adaptive behavioral for children with Intellectual disability. Ovidius University Annals, Physical Education and Sport/Science, Movement and Health Series 15, 436–441. [Google Scholar]
- Arumugam A., Raja K., Venugopalan M., Chandrasekaran B., Kovanur S. K., Muthusamy H. et al. (2016) Down syndrome – a narrative review with a focus on anatomical features. Clinical Anatomy 29, 568–577. [DOI] [PubMed] [Google Scholar]
- Bagherly J. & Ghasemi A. (2012) The compensatory impact of mini‐basketball skills on the progress of fundamental movements in children. Procedia ‐ Social and Behavioral Sciences 46, 5206–5210. [Google Scholar]
- Baldari C., Franciosi E., Gallotta M. C., Emerenziani G. P., Machado Reis V. & Guidetti L. (2009) Using basketball test battery to monitor players with intellectual disability across two sports seasons. Journal of Strength and Conditioning Research 23, 2345–2350. [DOI] [PubMed] [Google Scholar]
- Baran F., Top E., Aktop A., Özer D. & Nalbant S. (2009) Evaluation of unified football program by Special Olympics athletes, partners, parents, and coaches. European Journal of Adapted Physical Activity 2, 51–61. [Google Scholar]
- Bertapelli F., Pitetti K., Agiovlasitis S. & Guerra‐Junior G. (2016) Overweight and obesity in children and adolescents with Down syndrome – prevalence, determinants, consequences, and interventions: a literature review. Research in Developmental Disabilities 57, 181–192. [DOI] [PubMed] [Google Scholar]
- Boer P. H. (2020) The effect of 8 weeks of freestyle swim training on the functional fitness of adults with Down syndrome. Journal of Intellectual Disability Research 64, 770–781. [DOI] [PubMed] [Google Scholar]
- Boer P. H., Meeus M., Terblanche E., Boer P. H., Rombaut L., Wandele I. D. et al. (2014) The influence of sprint interval training on body composition, physical and metabolic fitness in adolescents and young adults with intellectual disability: a randomised controlled trial. Clinical Rehabilitation 28, 221–231. [DOI] [PubMed] [Google Scholar]
- Boer P. H. & Moss S. J. (2016a) Effect of continuous aerobic vs. interval training on selected anthropometrical, physiological and functional parameters of adults with Down syndrome. Journal of Intellectual Disability Research 60, 322–334. [DOI] [PubMed] [Google Scholar]
- Boer P. H. & Moss S. J. (2016b) Test‐retest reliability and minimal detectable change scores of twelve functional fitness tests in adults with Down syndrome. Research in Developmental Disabilities 48, 176–185. [DOI] [PubMed] [Google Scholar]
- Boer P. H. & Moss S. J. (2016c) Validity of the 16‐metre PACER and six‐minute walk test in adults with Down syndrome. Disability and Rehabilitation 38, 2575–2583. [DOI] [PubMed] [Google Scholar]
- Briere D. E. I. & Siegle D. (2008) The effects of the unified sports basketball program on special education students' self‐concepts: four students' experiences. Teaching Exceptional Children Plus 5, 1–12. [Google Scholar]
- Cai K. L., Wang J. G., Liu Z. M., Zhu L. N., Xiong X., Klich S. et al. (2020) Mini‐basketball training program improves physical fitness and social communication in preschool children with autism spectrum disorders. Journal of Human Kinetics 73, 267–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmeli E., Kessel S., Coleman R. & Ayalon M. (2002) Effects of a treadmill walking program on muscle strength and balance in elderly people with Down syndrome. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 57, M106–M110. [DOI] [PubMed] [Google Scholar]
- Cohen J. (1988) Statistical Power Analysis for the Behavioural Sciences. Routledge, London. [Google Scholar]
- Cowley P. M., Ploutz‐Snyder L. L., Baynard T., Heffernan K., Jae S. Y., Hsu S. et al. (2010) Physical fitness predicts functional tasks in individuals with Down syndrome. Medicine and Science in Sports and Exercise 42, 388–393. [DOI] [PubMed] [Google Scholar]
- de Asua D. R., Quero M., Moldenhauer F. & Suarez C. (2015) Clinical profile and main comorbidities of Spanish adults with Down syndrome. European Journal of Internal Medicine 26, 385–391. [DOI] [PubMed] [Google Scholar]
- Delextrat A., Gruet M. & Bieuzen F. (2018) Effects of small‐sided games and high‐intensity interval training on aerobic and repeated sprint performance and peripheral muscle oxygenation changes in elite junior basketball players. Journal of Strength and Conditioning Research 32, 1882–1891. [DOI] [PubMed] [Google Scholar]
- González‐Agüero A., Vicente‐Rodríguez G., Moreno L. A., Guerra‐Balic M., Ara I. & Casajus J. A. (2010) Health‐related physical fitness in children and adolescents with Down syndrome and response to training. Scandinavian Journal of Medicine and Science in Sports 20, 716–724. [DOI] [PubMed] [Google Scholar]
- Guidetti L., Franciosi E., Emerenziani G. P., Gallotta M. C. & Baldari C. (2009) Assessing basketball ability in players with intellectual disability. British Journal of Sports Medicine 43, 208–212. [DOI] [PubMed] [Google Scholar]
- Guidetti L., Franciosi E., Gallotta M. C., Emerenziani G. P. & Baldari C. (2010) Could sport specialization influence fitness and health of adults with mental retardation? Research in Developmental Disabilities 31, 1070–1075. [DOI] [PubMed] [Google Scholar]
- Hsu H. C., Chou S. W., Chen C. P. C., Wong A. M. K., Chen C K. & Hong J. P. (2010) Effects of swimming on eye hand coordination and balance in the elderly. The Journal of Nutrition, Health and Aging 14, 692–695. [DOI] [PubMed] [Google Scholar]
- Izquierdo‐Gomez R., Martinez‐Gomez D., Villagra A., Fernhall B. & Veiga Ó. L. (2015) Associations of physical activity with fatness and fitness in adolescents with Down syndrome: the UP&DOWN study. Research in Developmental Disabilities 36C, 428–436. [DOI] [PubMed] [Google Scholar]
- Jung H. K., Chung E. & Lee B. H. (2017) A comparison of the balance and gait function between children with Down syndrome and typically developing children. Journal of Physical Therapy Science 29, 123–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocić M., Bojić I., Aleksandrović M., Ignjatović A. & Radovanović D. (2017) Physical activity in adolescent with mental retardation: is adapted basketball training adequate stimulus to improve cardiorespiratory fitness and sport skills performance? Acta Facultatis Medicae Naissensis 34, 159–168. [Google Scholar]
- Lewis C. L. & Fragala‐Pinkham M. A. (2005) Effects of aerobic conditioning and strength training on a child with Down syndrome: a case study. Paediatric Physical Therapy 17, 30–36. [DOI] [PubMed] [Google Scholar]
- Lewis J. A. & Machin D. (1993) Intention to treat – who should use ITT? British Journal of Cancer 68, 647–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H. C. & Wuang Y. P. (2012) Strength and agility training in adolescents with Down syndrome: a randomized controlled trial. Research in Developmental Disabilities 33, 2236–2244. [DOI] [PubMed] [Google Scholar]
- Mendonca G. V., Pereira F. D. & Fernhall B. (2011) Effects of combined aerobic and resistance exercise training in adults with and without Down syndrome. Archives of Physical Medicine and Rehabilitation 92, 37–45. [DOI] [PubMed] [Google Scholar]
- Mendonca G. V., Pereira F. D. & Fernhall B. (2013) Heart rate recovery and variability following combined aerobic and resistance exercise training in adults with and without Down syndrome. Research in Developmental Disability 34, 353–361. [DOI] [PubMed] [Google Scholar]
- Mac Donncha C., Watson A., McSweeney T. & O'Donovan D. (1999) Reliability of Eurofit physical fitness items for adolescent males with and without mental retardation. Adapted Physical Activity Quarterly 16, 86–95. [Google Scholar]
- Menkes J. H. & Falk R. E. (2006) Cerebral palsy due to chromosomal anomalies and continuous‐gene syndromes. Clinics in Perinatology. Journal of Intellectual Disability Research 32, 481–501. [DOI] [PubMed] [Google Scholar]
- Pieter H. B. & de Beer Z. (2019) The effect of aquatic exercises on the physical and functional fitness of adults with Down syndrome: A non‐randomised controlled trial. Journal of Intellectual Disability Research 63, 1453–1463. [DOI] [PubMed] [Google Scholar]
- Pikora T. J., Bourke J., Bathgate K., Foley K. R., Lennox N. & Leonard H. (2014) Health conditions and their impact among adolescents and young adults with Down syndrome. PLoS ONE 9, e96868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Presson A. P., Partyka G., Jensen K. M., Devine O. J., Rasmussen S. A., McCabe L. L. et al. (2013) Current estimate of Down syndrome population prevalence in the United States. The Journal of Pediatrics 163, 1163–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rikli R. E. & Jones C. J. (2013) Development and validation of criterion‐referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist 53, 255–267. [DOI] [PubMed] [Google Scholar]
- Rimmer J. H., Heller T., Wang E. & Valerio I. (2004) Improvements in physical fitness in adults with Down syndrome. American Journal of Mental Retardation 109, 165–174. [DOI] [PubMed] [Google Scholar]
- Roizen N. & Patterson D. (2003) Down syndrome. The Lancet 361, 1281–1289. [DOI] [PubMed] [Google Scholar]
- Ruiz‐González L., Lucena‐Antón D., Salazar A., Martín‐ Valero R. & Moral‐Munoz J. A. (2019) Physical therapy in Down syndrome: systematic review and meta‐analysis. Journal of Intellectual Disability Research 63, 1041–1067. [DOI] [PubMed] [Google Scholar]
- Salaun L. & Berthouze‐Aranda S. E. (2012) Physical fitness and fatness in adolescents with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities 25, 231–239. [DOI] [PubMed] [Google Scholar]
- Savva S. C., Tornaritis M., Savva M. E., Kourides Y., Panagi A., Silikiotou N. et al. (2000) Waist circumference and waist‐to‐height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. International Journal of Obesity and Related Metabolic Disorders 24, 1453–1458. [DOI] [PubMed] [Google Scholar]
- Stanišić Z., Kocić M., Aleksandrović M., Stanković N. & Radovanović D. (2012) The effects of an adapted basketball training program on the physical fitness of adolescents with mental retardation: a pilot study. Serbian Journal of Experimental and Clinical Research 13, 103–107. [Google Scholar]
- Stratford P. W. (2004) Getting more from the literature: estimating the standard error of measurement from reliability studies. Physiotherapy Canada 56, 27–30. [Google Scholar]
- Suarez‐Villadat B., Veiga O. L., Villagra A. & Izquierdo‐Gomez R. (2019) Changes in body composition and physical fitness in adolescents with Down syndrome. Childhood Obesity 15, 397–405. [DOI] [PubMed] [Google Scholar]
- Suarez‐Villadat B., Luna‐Oliva L., Acebes C. & Villagra A. (2020) The effect of swimming program on body composition levels in adolescents with Down syndrome. Research in Developmental Disabilities 102, 103643. [DOI] [PubMed] [Google Scholar]
- Tejero‐Gonzalez C. M., Martinez‐Gomez D., Bayon‐Serna J., Izquierdo‐Gomez R., Castro‐Pinero J. & Veiga O. L. (2013) Reliability of the ALPHA health‐related fitness test battery in adolescents with Down syndrome. Journal of Strength and Conditioning Research: November 27, 3221–3224. [DOI] [PubMed] [Google Scholar]
- Terblanche E. & Boer P. (2013) The functional fitness capacity of adults with Down syndrome in South Africa. Journal of Intellectual Disability Research 57, 826–836. [DOI] [PubMed] [Google Scholar]
- Torr J., Strydom A., Patti P. & Jokinen N. (2010) Aging in Down syndrome: morbidity and mortality. Practise in Intellectual Disabilities 7, 70–81. [Google Scholar]
- Tsimaras V. K. & Fotiadou E. G. (2004) Effect of training on the muscle strength and dynamic balance ability of adults with Down syndrome. Journal of Strength and Conditioning Research 18, 343–347. [DOI] [PubMed] [Google Scholar]
- Vicari S. (2006) Motor development and neuropsychological patterns in persons with Down syndrome. Behavior Genetics 36, 355–364. [DOI] [PubMed] [Google Scholar]
- Villamonte R., Vehrs P. R., Feland J. B., Johnson A. W., Seeley M. K. & Eggett D. (2010) Reliability of 16 balance tests in individuals with Down syndrome. Perceptual and Motor Skills 111, 530–542. [DOI] [PubMed] [Google Scholar]
- Zhang F.‐L., Ren J.‐X., Zhang P., Jin H., Qu Y., Yu Y. et al. (2021) Strong association of waist circumference (WC), body mass index (BMI), waist‐to‐height ratio (WHtR), and waist‐to‐hip ratio (WHR) with diabetes: a population‐based cross‐sectional study in Jilin Province, China. Journal of Diabetes Research 14, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Xu C., Wan Q. & Guo L. Y. (2017) Effects of adapted physical exercise intervention on visual working memory in children with autism spectrum disorder. China Sport Sci. Technol 53, 55–62. [Google Scholar]
- Zverev Y. & Kurnikova M. (2016) Adapted community‐based group aquatic program for developing balance: a pilot intervention study involving children and adolescents with cerebral palsy. Journal of Physical Education and Sport 16, 1258–1265. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data (descriptive statistics) used to support the findings of this study are included within the article. The source data (SPSS table with original measurements; testing and activities videos) used to support the findings of this study are available from the author upon request.


