Abstract
Objective
Many individuals with an eating disorder do not receive appropriate care. Low‐threshold interventions could help bridge this treatment gap. The study aim was to evaluate the effectiveness of Featback, a fully automated online self‐help intervention, online expert‐patient support and their combination.
Method
A randomized controlled trial with a 12‐month follow‐up period was conducted. Participants aged 16 or older with at least mild eating disorder symptoms were randomized to four conditions: (1) Featback, a fully automated online self‐help intervention, (2) chat or email support from a recovered expert patient, (3) Featback with expert‐patient support and (4) a waiting list control condition. The intervention period was 8 weeks and there was a total of six online assessments. The main outcome constituted reduction of eating disorder symptoms over time.
Results
Three hundred fifty five participants, of whom 43% had never received eating disorder treatment, were randomized. The three active interventions were superior to a waitlist in reducing eating disorder symptoms (d = −0.38), with no significant difference in effectiveness between the three interventions. Participants in conditions with expert‐patient support were more satisfied with the intervention.
Discussion
Internet‐based self‐help, expert‐patient support and their combination were effective in reducing eating disorder symptoms compared to a waiting list control condition. Guidance improved satisfaction with the internet intervention but not its effectiveness. Low‐threshold interventions such as Featback and expert‐patient support can reduce eating disorder symptoms and reach the large group of underserved individuals, complementing existing forms of eating disorder treatment.
Public significance statement
Individuals with eating‐related problems who received (1) a fully automated internet‐based intervention, (2) chat and e‐mail support by a recovered individual or (3) their combination, experienced stronger reductions in eating disorder symptoms than those who received (4) usual care. Such brief and easy‐access interventions play an important role in reaching individuals who are currently not reached by other forms of treatment.
Keywords: eating disorders, eHealth, expert patient, internet‐based intervention, randomized controlled trial, treatment gap
1. INTRODUCTION
On average, it takes people with an eating disorder several years before they receive help specifically for their eating disorder (Austin et al., 2021). While individuals with an eating disorder generally utilize more health care services than those without, only a minority seeks targeted treatment (Hart et al., 2011; Weissman & Rosselli, 2017), indicating that many do not receive the care they need. This is worrying, since a longer duration of untreated eating disorder seems to be indicative of poorer outcome (Andrés‐Pepiñá et al., 2020). The evident treatment gap (i.e., the discrepancy between people in need of help for their eating disorder and those actually receiving it) underscores the need to reach this underserved group, for example by using scalable, easily accessible, low‐threshold interventions (Aardoom, Dingemans, & Van Furth, 2016; Kazdin et al., 2017; Moessner & Bauer, 2017). Two possible ways of making interventions more accessible for a large audience are internet interventions and support from an expert (recovered) patient.
1.1. Internet interventions for eating disorders
As captured in multiple systematic reviews and meta‐analyses over the past decade (Aardoom et al., 2013; Beintner et al., 2012; Dölemeyer et al., 2013; Linardon et al., 2020, August 27; Loucas et al., 2014; Melioli et al., 2016; Pittock et al., 2018; Schlegl et al., 2015; Wade & Wilksch, 2018; Zeiler et al., 2021), internet interventions for eating disorders appear to have a beneficial effect on eating disorder symptoms and related complaints such as drive for thinness and weight and shape concerns compared to care as usual. Technological advancements have allowed internet‐based interventions to be increasingly personalized towards users. The internet intervention “Featback” is one such application that aims to provide low‐threshold and easily accessible care for people with (symptoms of) an eating disorder, through personalized feedback. It is a brief online self‐help program that works with an automated monitoring and feedback system. The main goal of Featback is to reduce eating disorder symptoms, by making users aware of their eating disorder symptoms, providing support and stimulating help‐seeking behaviors, both towards their direct environment and professional facilities. An earlier randomized controlled trial showed Featback to be (cost‐)effective in reducing symptoms of bulimia nervosa, depression and anxiety compared to a waiting list control condition (Aardoom, Dingemans, Spinhoven, et al., 2016; Aardoom, Dingemans, van Ginkel, et al., 2016). Interestingly, adding psychologist support once or three times a week increased satisfaction with the intervention, but not its (cost‐)effectiveness.
The impression is that personal guidance adds to the effectiveness of, adherence to and satisfaction with an online intervention, but this is mostly based on what we know from other disorders (Baumeister et al., 2014). Often, guidance is provided by therapists, but expert patients are increasingly involved in research and delivering support. Theoretically, expert‐patient support can be especially valuable in providing low‐threshold interventions, because a shared background and natural credibility enables them to establish a rapport, effectively model healthy behaviors and enhance self‐efficacy (Dennis, 2003; Simoni et al., 2011). They might also be easier to approach and confide in than health professionals. Only few studies have involved expert‐patient supporters (Fogarty et al., 2016; Lewis & Foye, 2022). Findings cautiously indicate that expert‐patient support can enhance quality of life, relationships, and adherence to an intervention (Cardi et al., 2019; McCarroll, 2012; Perez et al., 2014; Ramjan et al., 2017). Concordantly, guidance from an expert patient might be a strategic alternative to support from health professionals. However, its added value and effective ways of implementation are not yet established.
1.2. Aims
The aim of the study was to investigate the effectiveness of Featback, expert‐patient support and their combination. First, it was hypothesized that the three active interventions were more effective than a waiting list control condition. Secondly, the combination of Featback and expert‐patient support was expected to be more effective than the two interventions separately. Lastly, no differences in effectiveness were anticipated between separately receiving Featback or expert‐patient support.
2. METHODS
This study was preregistered at the Dutch Trial Register (trialregister.nl/trials; identifier NL7065) and a study protocol with elaborate descriptions of the hypotheses and methods has been published (Rohrbach et al., 2019). The described repeated measures ANOVAs in the study protocol were altered to mixed model analyses, since they were more versatile. Additionally, a sensitivity analysis controlling for all relevant prognostic variables was performed rather than only with variables that differed significantly at baseline, as this is statistically preferable (De Boer et al., 2015). No other changes to the analysis plan per protocol were made. An economic evaluation concerning this trial has been published elsewhere (Rohrbach et al., 2022). Results on prediction, moderation and mediation will not be addressed here.
2.1. Design
A randomized controlled trial with a two‐by‐two factorial design with planned contrasts was used, creating four conditions: (1) Featback only, (2) Featback plus weekly expert‐patient support, (3) weekly expert‐patient support only, and (4) a waiting list control condition. Participants were assessed at baseline (T0), postintervention (8 weeks after baseline; T1) and 3 (T2), 6 (T3), 9 (T4), and 12 (T5) months after postintervention. All assessments consisted of online self‐report questionnaires.
2.2. Participants and procedure
The majority of participants were recruited via Proud2Bme, a Dutch e‐community for people with eating related problems. Other sources were also used, such as the Featback website, a blog on a fashion and health website aimed at (female) teenagers, social media, Google Ads and the Dutch eating disorder patient organization. Eligible participants were aged 16 years or older and had at least mild self‐reported symptoms of an eating disorder; 52 or higher on the Weight Concerns Scale (Killen et al., 1993) or, as reported on the Short Evaluation of Eating Disorders (Bauer et al., 2005), a BMI of 18.5 or lower or at least weekly binge eating episodes or compensatory behaviors in the past 4 weeks. In the case of severe eating disorders, participants received the advice to seek professional help, but could still participate in the study as they may benefit from the offered interventions too. After expressing interest and filling out the screening questions, all eligible participants were asked to complete an online informed consent form and the baseline assessment (T0).
Participants were randomly allocated to one of the four conditions. An independent researcher created the allocation sequence using the SPSS function to produce random numbers. Hence, the randomization sequence, using blocks of 40 participants, was concealed from the principal investigator. The current design made it impossible to mask participants and expert patients to allocation. During the trial the principal investigator was not masked to the allocation, in order to send the appropriate information to participants. However, the content and timing of mails and reminders were standardized in order to avoid performance bias.
2.3. Interventions
Participants in all four conditions were allowed to seek help from any source for their eating disorder symptoms or other complaints. In this sense, the waiting list control condition can be regarded as treatment as usual for the current sample.
2.3.1. Featback
Participants in this condition received an account for the weekly monitoring and feedback system. During 8 weeks participants received a weekly email with a link to a questionnaire with four questions on eating disorder related symptoms. On a 4‐point scale, participants rated how often the behavior or symptom occurred this week, ranging from “not at all,” “1–3 days,” “4–6 days”–“7 days.” The weekly feedback message was also dependent on whether participants indicated to have improved, deteriorated or stayed the same compared to previous week regarding the four monitoring questions. After completing the monitoring questionnaire, participants received a supportive feedback message that matched the participant's answers from a database with over 1250 different messages, written in collaboration with expert patients, scientists and psychologists. The supportive messages (on average 384 words) contain a summary of self‐reported eating problems and changes compared to the previous week, psychoeducation, and guidance on how to counter eating disorder related symptoms. Additionally, participants could access the Featback website with psycho‐educative material on eating disorders at their own convenience.
2.3.2. Expert‐patient support
Expert patients (N = 5) received an intervention protocol and one day of training on how to use their own experience to help others with eating disorder symptoms via chat and email. During the trial, expert patients received monthly supervision from an experienced expert patient and clinical psychologist (EvF). Expert patients scheduled 20‐minute slots flexibly across the week to give participants ample choice to access support. They worked 4–6 h a week, could maximally support 12 participants at any one time, and received monthly payment.
Participants in this condition were assigned to one of the expert patients for 8 weeks and received an account to schedule appointments. For each of the eight sessions, participants were able to choose between email and chat support. Chat sessions closed automatically after 20 min. For email sessions participants were asked to send an email to their expert patient before the scheduled appointment, so that the expert patient could respond during the 20‐minute appointment.
2.3.3. Featback with expert‐patient support
Participants in this condition were able to make use of both Featback and weekly 20‐minute chat or email support from an expert patient.
2.3.4. Waiting list control
Participants in this condition were placed on a waiting list for 14 months. The timing of the assessments was equal to that in the other conditions. After the waiting period, participants were offered 8 weeks of Featback with weekly expert‐patient support.
2.3.5. Intervention check
An intervention check, based on a checklist constructed before the trial started (Rohrbach et al., 2019), was performed to investigate whether and how sessions from expert patients were distinguishable from sessions by psychologists, as performed in the previous Featback trial by Aardoom, Dingemans, Spinhoven, et al. (2016). Two masked master‐level psychology students rated the structure, intervention content and methods of delivery of 30 chat and email sessions from expert patients and 30 chat and email sessions from psychologists.
2.4. Outcomes
The primary outcome measure was eating disorder symptomatology as assessed by the Eating Disorder Examination Questionnaire (EDE‐Q 6.0; Fairburn & Beglin, 2008). A total score of eating disorder pathology was computed by taking the average of 22 items presented as 7‐point Likert scale questions. Secondary outcomes measures included symptoms of anxiety and depression measured with the 4‐item Patient Health Questionnaire (PHQ‐4; Kroenke et al., 2009), general self‐efficacy measured with the General Self‐Efficacy Scale (GSES; Schwarzer & Jerusalem, 1995) and experienced social support measured with the 12‐item Social Support List (SSL‐12‐I; van Eijk et al., 1994). Additionally, motivation to change, user satisfaction with the automated messages and expert‐patient support, and help seeking intentions and behaviors were assessed with self‐developed questionnaires. At baseline, self‐esteem measured with the Rosenberg Self‐Esteem Scale (RSES; Rosenberg, 1965) was obtained, as well as demographic information including gender, age, educational level, country of origin, work situation, internet access, self‐reported severity of eating problems and eating disorder treatment history. Lastly, the Inclusion of Other in the Self scale (IOS scale; Aron et al., 1992) was used to assess, at week 3 of the intervention, the extent to which participants allocated to a condition with expert‐patient support perceived themselves to be similar to the expert patient they were paired with. Psychometric properties of all questionnaires were adequate and can be found in the published protocol (Rohrbach et al., 2019).
2.5. Statistical procedures
All participants who underwent randomization were included in the analyses, following the intention‐to‐treat approach. An a priori sample size calculation, finding the optimal sample size for the main research question with a power of 80% to detect a small effect (d = 0.30), indicated 88 participants per condition (N = 352) were needed.
Main analyses were conducted in R version 4.0.2 (R Core Team, 2018) using linear mixed models (lmer function from the lme4 package) including random intercepts. To analyze the effect of the intervention type, three condition contrast were created. Specifically, to investigate the main hypothesis that the active interventions (i.e., Featback, expert‐patient support and Featback plus expert‐patient support) were more effective than a waiting list in decreasing eating disorder symptomatology, the three active conditions (pooled) were contrasted against the waiting list (CC1). This contrast allowed to investigate whether offering one of the active interventions, on average, resulted in greater symptoms reductions compared to the waiting list. The second contrast (CC2) distinguished the expert‐patient support only and Featback only conditions (pooled) from the combination condition (i.e., Featback plus expert‐patient support) to examine whether the combination condition was superior in reducing eating disorder symptoms. The third contrast (CC3) consisted of the Featback only versus expert‐patient support only condition and informed on the relative effectiveness of offering only Featback and only expert‐patient support. Moreover, five time contrasts were included, being baseline versus postintervention (TC1), and postintervention versus 3 (TC2), 6 (TC3), 9 (TC4), and 12 (TC5) month follow‐up. Changes from baseline to postintervention (TC1) were of primary interest. The other time contrasts were used to inspect whether effects were maintained over time. All condition and time contrast combinations (15 in total) were tested separately to avoid noise in the models and improve interpretation. In other words, conditions or time points that were irrelevant for the effect of interest were removed from the model, as they may have introduced error variance, making the model less parsimonious. As recommended by (Cheng et al., 2010) when testing pre‐specified models, Bonferroni adjustment of the p‐values (α = .05/15) was applied to account for multiple testing and reduce type I errors. In summary, CC1*TC1 was the interaction of primary interest. CC2*TC1 and CC3*TC1 were used to test our second and third hypotheses. To see the long‐term effects of the interventions, TC5 (1‐year follow‐up) was deemed most informative. An overview of all statistical models can be found in the supplemental materials (S1). These main analyses were repeated for symptoms of anxiety and depression, general self‐efficacy and experienced social support.
Additionally, six linear regression analyses were conducted to investigate both the short (T1) and the long term (T5) relationship between perceived similarity ratings, and (1) eating disorder symptomatology, (2) self‐efficacy and (3) experienced social support. Multiple testing was accounted for using Holm's method (Holm, 1979).
2.5.1. Missing data
Missing data were multiply imputed (Rubin, 1987) using R. Logistic regression (multinomial) was used for imputing categorical variables, while predictive mean matching was used for most of the numerical variables (Rubin, 1986; Van Buuren, 2012). Variables constructed from other variables (e.g., BMI was determined by weight and length) were imputed using passive imputation (Van Buuren & Groothuis‐Oudshoorn, 2011). The number of predictors for each variable with missing data was determined by using a rule of thumb of 15 cases per predictor (Stevens, 2001). For a specific variable with missing data, the other variables that were most strongly related to this variable were chosen as predictors for the missing data. If the variable with missing data and a potential predictor were both numerical, then their absolute correlation was used as a measure of association. Partial η 2 was used as a measure of association if the variable with missing data was numerical and the potential predictor was categorical. Finally, if both the variable with missing data and a potential predictor were categorical, then Cramér's V was used. Missing data were imputed 100 times, creating 100 complete versions of the incomplete dataset.
2.5.2. Sensitivity analyses
The main analysis (CC1 and TC1) was repeated for participants with an adequate dose only. To be considered an adequate‐dose participant, a participant in the Featback only, expert‐patient support only and combination condition should have completed at least five out of eight monitoring assessments, five out of eight support sessions or both respectively. Secondly, the main analysis was repeated including covariates that were assumed to be prognostic for treatment outcome (i.e., age, baseline eating disorder symptoms, eating disorder duration, eating disorder treatment history, psychological health care visits, baseline self‐esteem, baseline motivation to recover from the eating disorder, baseline anxiety and depression symptoms, baseline self‐efficacy, baseline experienced social support and baseline BMI).
3. RESULTS
3.1. Participants
Participant flow throughout the study is presented in Figure 1 and baseline characteristics are summarized in Table 1. Recruitment went as planned and lasted from October 2018 until October 2019 with the last follow‐up measurement completed in December 2020. The baseline distributions of eating disorder symptoms across the sample are displayed in Figure 2. Study drop‐out rates did not differ between conditions at postintervention, χ 2 (3) = 3.99, p = .26, or other assessments. Most mentioned reasons for dropping out, based on 26 responses, were lost interest in the intervention or research, the feeling that participating took too much time and the feeling that the intervention or research was not helpful.
FIGURE 1.
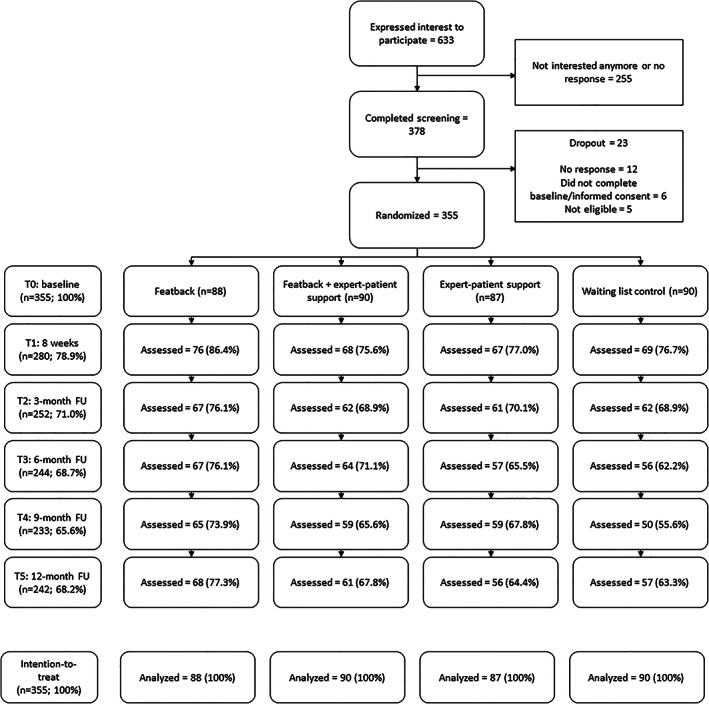
Participant flow during the study
TABLE 1.
Baseline characteristics of participants (N = 355)
| Characteristics | Featback (N = 88) | Featback + expert patient support (N = 90) | Expert patient support (N = 87) | Waiting list (N = 90) | Total sample (N = 355) |
|---|---|---|---|---|---|
| Gender | |||||
| Female (%) | 82 (93.2) | 89 (98.9) | 84 (96.6) | 88 (97.8) | 343 (96.7) |
| Male (%) | 5 (5.7) | 1 (1.1) | 1 (1.1) | 2 (2.2) | 9 (2.5) |
| Other (%) | 1 (1.1) | 0 (0.0) | 2 (2.3) | 0 (0.0) | 3 (0.8) |
| Nationality | |||||
| Dutch (%) | 78 (88.6) | 80 (88.9) | 80 (92.0) | 81 (90.0) | 319 (89.9) |
| Belgian (%) | 9 (10.0) | 9 (10.2) | 6 (6.9) | 8 (8.9) | 32 (9.0) |
| Other (%) | 1 (1.1) | 1 (1.1) | 1 (1.1) | 1 (1.1) | 4 (1.1) |
| Education | |||||
| Low (%) | 5 (5.6) | 12 (13.3) | 12 (13.7) | 18 (20.5) | 47 (13.3) |
| Middle (%) | 33 (37.5) | 31 (34.4) | 34 (39.0) | 35 (39.3) | 133 (37.6) |
| High (%) | 50 (56.8) | 47 (52.2) | 41 (47.1) | 36 (40.4) | 174 (49.2) |
| Marital status | |||||
| Married/living together (%) | 20 (22.7) | 22 (24.4) | 26 (29.9) | 30 (33.3) | 98 (27.6) |
| Living alone (%) | 68 (77.3) | 66 (73.3) | 58 (66.7) | 58 (64.4) | 250 (70.4) |
| Divorced (%) | 0 (0.0) | 1 (1.1) | 3 (3.4) | 2 (2.2) | 6 (1.6) |
| Widow (%) | 0 (0.0) | 1 (1.1) | 0 (0.0) | 0 (0.0) | 1 (0.2) |
| Treatment history for ED | |||||
| Yes (%) | 46 (52.3) | 54 (60.0) | 53 (60.9) | 49 (54.4) | 202 (56.9) |
| No (%) | 42 (47.7) | 36 (40.0) | 34 (39.1) | 41 (45.6) | 153 (43.1) |
| Self‐reported diagnosis status | |||||
| Officially diagnosed with ED | 52 (59.1) | 60 (66.7) | 52 (59.8) | 58 (64.4) | 222 (62.5) |
| No diagnosis, but assumed to have ED | 24 (27.3) | 22 (24.4) | 23 (26.4) | 22 (24.4) | 91 (25.6) |
| Eating problems, but likely no ED diagnosis | 12 (13.6) | 8 (8.9) | 12 (13.7) | 10 (11.1) | 42 (11.8) |
| Age (Years) | 28.0 (1.7) | 28.3 (10.4) | 26.8 (9.4) | 28.1 (12.4) | 27.8 (10.8) |
| BMI (kg/m2) | 22.2 (7.1) | 21.9 (6.2) | 22.0 (7.1) | 22.4 (7.7) | 22.1 (7.0) |
| Duration of eating problems (years) | 10.1 (9.1) | 10.3 (8.8) | 8.6 (8.2) | 11.4 (12.0) | 10.1 (9.7) |
| EDE‐Q | 3.9 (1.1) | 4.1 (1.1) | 4.3 (1.0) | 4.3 (1.0) | 4.1 (1.0) |
| PHQ‐4 | 7.6 (3.4) | 7.5 (3.3) | 8.2 (2.9) | 7.9 (3.3) | 7.8 (3.2) |
| GSES | 25.9 (5.8) | 27.4 (5.2) | 24.4 (5.4) | 26.7 (5.8) | 26.12 (5.6) |
| SSL‐12 | 29.4 (6.7) | 30.4 (7.5) | 30.0 (6.7) | 30.1 (7.0) | 30.0 (7.0) |
| RSES | 20.8 (5.5) | 21.6 (5.8) | 19.0 (4.5) | 20.6 (4.9) | 20.5 (5.3) |
| Motivation to change | 21.4 (4.5) | 22.6 (4.5) | 22.2 (4.5) | 22.0 (4.2) | 22.0 (4.5) |
| Internet usage (hours per day) | 4.2 (2.6) | 3.7 (2.2) | 3.9 (2.3) | 3.4 (2.8) | 3.8 (2.5) |
Note: Data are presented as means (SD) unless indicated otherwise.
Abbreviations: BMI, body mass index; ED, eating disorder; EDE‐Q, Eating Disorder Examination Questionnaire; GSES, General Self‐Efficacy Scale; PHQ‐4 = 4‐item Patient Health Questionnaire; RSES, Rosenberg Self‐Esteem Scale; SD, standard deviation; SSL‐12, 12‐item Social Support List.
FIGURE 2.
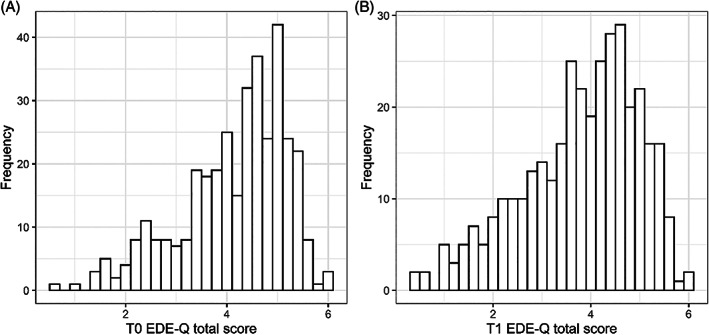
Distribution of eating disorder examination questionnaire (EDE‐Q) total scores at baseline (a) and postintervention (b)
3.2. Eating disorder psychopathology
Main results can be found in Table 2 and all mixed model results can be found in the supplemental materials (S2). First, the three active interventions were compared with the waiting list control condition (CC1*TC1). A statistically significant medium effect of condition on changes in EDE‐Q total scores between baseline and postintervention was found, favoring the active interventions. There were no significant condition‐by‐time interaction terms for the other time contrasts, indicating that there were no differences in longer‐term eating disorder symptom changes between the three active interventions and the waitlist. No other significant results were found regarding eating disorder symptomatology. Specifically, the combination condition did not outperform the Featback only and expert‐patient support only conditions pooled together in the short term (CC2*TC1) or any other time contrast. Similarly, no difference in effectiveness between the Featback only and expert‐patient support only conditions were found in the short term (CC3*TC1) or any other time contrast.
TABLE 2.
Pooled results of linear mixed models analyses over 100 multiple imputed datasets
| Measure | CC | TC | Time effects | Time‐condition interaction effects | |||
|---|---|---|---|---|---|---|---|
| B (95% CI) | t (p) | B (95% CI) | t (p) | Cohen's d | |||
| Eating disorder symptoms (EDE‐Q global) | CC1 | TC1 |
−0.18 (−0.22; −0.14) |
−8.12 (<.001) |
−0.15 (−0.22; −0.07) |
−3.66 (<.001) | 0.38 |
| CC1 | TC5 |
−0.27 (−0.35; −0.19) |
−6.67 (<.001) |
0.16 (0.02; 0.29) |
2.26 (.02) | 0.25 | |
| CC2 | TC1 |
−0.23 (−0.28; −0.18) |
−8.81 (<.001) | −0.04 (−0.12; 0.03) | −1.17 (.24) | 0.12 | |
| CC2 | TC5 |
−0.22 (−0.31; −0.13) |
−4.87 (<.001) |
−0.04 (−0.18; 0.09) |
−0.64 (.52) | −0.09 | |
| CC3 | TC1 |
−0.21 (−0.26; −0.15) |
−6.73 (<.001) |
0.01 (−0.06; 0.07) |
0.17 (.87) | 0.02 | |
| CC3 | TC5 |
−0.2 (−0.31; −0.09) |
−3.66 (<.001) |
0.01 (−0.09; 0.12) |
0.25 (.80) | 0.04 | |
| Depression and anxiety symptoms (PHQ‐4) | CC1 | TC1 |
−0.41 (−0.58; −0.23) |
−4.61 (<.001) |
−0.22 (−0.52; 0.08) |
−1.43 (.15) | 0.12 |
| CC1 | TC5 |
−0.42 (−0.63; −0.2) |
−3.85 (<.001) |
0.16 (0.02; 0.29) |
2.26 (.02) | 0.25 | |
| General self‐efficacy (GSES) | CC1 | TC1 |
0.09 (−0.18; 0.35) |
0.65 (.52) |
0.09 (−0.4; 0.59) |
0.37 (.71) | 0.04 |
| CC1 | TC5 |
0.38 (0.07; 0.69) |
2.4 (.02) |
−0.15 (−0.73; 0.43) |
−0.50 (.62) | 0.06 | |
| Experienced social support (SSL‐12) | CC1 | TC1 |
−0.04 (−0.35; 0.26) |
−0.28 (.78) |
−0.19 (−0.72; 0.35) |
−0.69 (.49) | 0.07 |
| CC1 | TC5 |
0.35 (−0.1; 0.80) |
1.52 (.13) |
0.20 (−0.58; 0.97) |
0.50 (.62) | 0.06 | |
Abbreviations: CC, condition contrast; CC1, three active interventions (Featback only, expert‐patient support only and Featback plus expert‐patient support) versus waiting list control condition; CC2, Featback plus expert‐patient support condition versus Featback only and expert‐patient support only; CC3, Featback only versus expert‐patient support only; CI, confidence interval; TC, time contrast; TC1, baseline versus postintervention; TC5, postintervention versus 12‐month follow‐up.
To further explore change in participants on EDE‐Q scores between baseline and postintervention, the reliable change index (RCI) was calculated (Jacobson & Truax, 1992). Based on the EDE‐Q reliability in the current sample (Cronbach's α = .90) and the standard deviation of baseline EDE‐Q total scores (1.04), the RCI was 0.89. Derived from the RCI, the number of participants (averaged across 100 imputed datasets) showing reliable deterioration, no change and reliable improvement was 14, 261 and 80 respectively. No significant difference in these frequencies between conditions was found, χ 2 (6) = 11.14, p = .08. Details can be found in the supplemental materials (S3).
3.3. Secondary outcomes
For symptoms of anxiety and depression, social support and self‐efficacy, no time‐by‐condition interaction effects were found, indicating that for these variables trajectories over time were similar across conditions. Between baseline and postintervention, participants improved regarding symptoms of anxiety and depression. Between postintervention and 12‐month follow‐up participants improved regarding self‐efficacy. Results were non‐significant across other condition and time contrasts.
3.4. Intervention check
Raters could distinguish sessions correctly in 94% of the cases (agreement between the two raters was 95%), confirming the expectation that differences exist between the psychologist sessions of the previous trial (Aardoom, Dingemans, Spinhoven, et al., 2016) and expert‐patient sessions of the current trial. Details on the intervention check can be found in the supplemental materials (S4).
3.5. Similarity ratings
Of the 177 participants who had the option to receive expert‐patient support, 144 (81.4%) completed the IOS‐scale. Answers on the IOS‐scale were not imputed, since only participants in the two expert‐patient support conditions received this questionnaire. Perceived similarity ratings were low with a median of 2 and mean of 2.7 (SD = 1.5). Perceived similarity was not predictive of eating disorder symptoms at postintervention, β = .002, F(1, 126) < 0.001, p = .98, and, after correcting for multiple testing, at 12‐month follow‐up, β = −.19, F(1, 107) = 4.05, p = .05. Similar non‐significant results were found for the predictive value of perceived similarity ratings on experienced social support and self‐efficacy.
3.6. Per protocol analyses
The number of adequate‐dose participants was 74 (84.1%) in the Featback, 34 (37.8%) in the combination and 48 (55.2%) in the expert‐patient support condition. The main analysis, concerning the comparison of the effect of the three active interventions and the waitlist condition on eating disorder symptoms for the period between baseline and postintervention, was repeated with adequate‐dose participants (N = 156). The result was similar to the main analysis and favoring the three active interventions, t(323) = −3.23, p = .001. The number of intervention sessions was not prognostic of eating disorder symptoms at postintervention, β = −.02, t(665) = −1.10, p = .27. Furthermore, adding covariates to the model yielded similar results to the main analysis, with a significant time‐by‐condition interaction favoring the three active interventions, t(405) = −3.57, p < .001. Lastly, severity of eating disorder symptoms was explored as a moderator, by entering it as a fixed effect in the CC1*TC1 model. Based on Mond et al. (2006), severity was considered high or low depending on whether a participant's baseline EDE‐Q score was higher or lower than 4.0. No evidence for moderation of eating disorder symptom severity was found, t(447) = 0.80, p = .42.
Table 3 presents information on intervention usage, satisfaction and initiation of professional help. Further details can be found in the supplemental materials (S5). On average, participants made more use of Featback sessions than expert‐patient support sessions. Intervention satisfaction was significantly higher in conditions with expert‐patient support compared to the Featback only condition. Furthermore, of the 150 participants seeking help at postintervention, 33 (22%) indicated that the 8‐week intervention stimulated them to request professional help. However, there was no difference between the four conditions in initiating professional help for eating‐related problems (e.g., with general practitioner or psychologist). Lastly, of the 90 participants randomized to the waiting list, 38 (42%) made use of the option to use Featback and expert‐patient support after study completion.
TABLE 3.
Intervention usage, satisfaction and help initiation of participants per condition
| Category | Featback (N = 88) | Featback + expert‐patient support (N = 90) | Expert‐patient support (N = 87) | Waiting list (N = 90) | Total (N = 265; excludes waitlist) | Statistics | |
|---|---|---|---|---|---|---|---|
|
Adequate‐dose participants (%) |
74 (84.1) | 34 (37.8) | 48 (55.2) | NA | 156 (58.9) | χ2(2) = 40.00, p < .001 | |
|
Indicated to stop with the intervention (%) |
4 (4.6) | 3 (3.3) | 6 (6.9) | NA | 13 (4.9) | χ2(2) = 1.24, p = .54 | |
| Mean amount of sessions (SD; median) | 6.5 (2.1; 7.0) | 9.2 (5.2; 10.0) | 4.4 (3.1; 5.0) | NA | 6.7 (4.2) | F(2, 262) = 37.67, p < .001 | |
| Featback | 5.6 (2.7; 7.0) | NA | 6.0 (3.0) | t(176) = 2.28, p = .024 | |||
| Support |
3.6 (2.9; 3.0) |
NA | 4.0 (3.0) | t(175) = 1.86, p = .066 | |||
|
Proportion of possible sessions used (SD) |
80.7% (26.1) | 57.4% (32.2) | 54.9% (38.3) | NA | 64.3% (34.5) |
F(2, 262) = 16.80, p < .001 |
|
| 0 sessions (%) | 2 (2.3) | 6 (6.7) | 17 (19.5) | NA | χ2(2) = 16.43, p < .001 | ||
| Featback | 6 (6.7) | NA | |||||
| Support | 23 (25.6) | NA | |||||
| 1 session (%) | 4 (4.5) | 4 (4.4) | 7 (8.0) | NA | χ2(2) = 1.38, p = .50 | ||
| Featback | 6 (6.7) | NA | |||||
|
Support |
5 (5.6) | NA | |||||
| All sessions (%) | 40 (45.5) | 11 (12.2) | 14 (16.1) | NA | χ2(2) = 28.20, p < .001 | ||
| Featback | 34 (37.8) | NA | |||||
| Support | 12 (13.3) | NA | |||||
| Intervention satisfaction a (SD) | 5.8 (1.8) | 7.1 (1.7) | 7.4 (1.6) | NA | 6.7 (1.8) | F(2, 192) = 15.98, p < .001 | |
| Initiated professional help b (%) | 22 (25.0) | 17 (18.9) | 15 (17.2) | 20 (22.2) | 74 (20.8) | F(3,351) = 0.64, p = .59 | |
Abbreviation: SD = standard deviation.
On a scale from 1 (completely unsatisfied) to 10 (completely satisfied); based on 70, 63, and 62 (195 total) responses in the Featback, Featback + expert‐patient support and expert patient support conditions respectively.
Indicates the number of participants who had never received eating disorder related treatment at baseline, but sought professional help (e.g., with a general practitioner, psychologist or psychiatrist) on at least one of the follow‐up measures (T1–T5); total based on 355 participants.
4. DISCUSSION
The main aim of the current study was to investigate the effectiveness of Featback, expert‐patient support and the combination of both compared to care as usual (waitlist) for eating disorders. Of the 355 participants, 22.5% (25.3% in the three active conditions and 13.3% in the waitlist) experienced reliable improvement in eating disorder symptoms. Results showed that participants in the three active conditions had larger improvements in eating disorder symptoms over the 8‐week intervention period than participants in the waitlist condition. Contrary to expectations, the three active interventions were equally effective. The conditions with support from an expert patient were rated as more satisfactory than Featback alone. The results are similar to a previous randomized controlled trial on the effectiveness of Featback (Aardoom, Dingemans, Spinhoven, et al., 2016), where active interventions outperformed a waiting list control condition and adding support from a psychologist to the automated monitoring system enhanced intervention satisfaction, but not its effectiveness. Results are also in line with other research that found internet‐based interventions to be effective in reducing eating disorder symptoms (Linardon et al., 2020, August 27; Melioli et al., 2016). The interventions in the current trial did not lead to more professional treatment initiation compared to the waitlist condition, but over 30 participants indicated the intervention had stimulated them to seek professional help. That a brief intervention such as Featback and expert‐patient support can improve eating disorder symptoms and might stimulate help‐seeking behaviors is promising, especially when considering its potential reach. Featback is free to use and easily accessible 24 h a day. Therefore, it can exist next to and complement current treatment options for eating disorders, by reaching underserved individuals (Bauer & Goldschmidt, 2019). This is supported by the fact that 43% of the current study sample had, at baseline, never received treatment while having a very long average duration of eating disorder problems. This suggests that others in similar positions might also profit from Featback or expert‐patient support, even if they do not (yet) receive other forms of treatment. Apart from individuals not currently reached by regular treatment, Featback could also be used in the period between intake and commencement of treatment. Waiting times for eating disorder treatment in the Netherlands have increased to an average of 11 weeks (Nederlandse Zorgautoriteit, 2021). Although further research is necessary, offering self‐help interventions in this period might keep individuals motivated for recovery and prepare them for future care (Vollert et al., 2019). In general, based on findings from this and other studies, low‐threshold and innovative interventions like Featback and expert‐patient support are not only likely to reduce the burden for individuals with eating disorders, but also to bridge the treatment gap by reaching underserved people.
4.1. Expert‐patient guidance
It was expected that individuals with an eating disorder would bond quickly with expert patients, making them receptive to interventions aimed at changing destructive behavior and increasing self‐efficacy and experienced social support (Dennis, 2003; Simoni et al., 2011). Contradictorily, adding expert‐patient support to Featback did not increase effectiveness. This is not in line with a meta‐analysis, covering multiple disorders, suggesting a small beneficial effect of guidance (Baumeister et al., 2014). Guidance in the pooled studies varied considerably and mostly covered support by therapists. An explanation of the discrepancy might thus be that expert patients are less effective in reducing symptoms through online support than health professionals. However, even though expert‐patient and psychologist support appear to be distinct interventions, a previous Featback trial found no increased effectiveness of adding online psychologist support (Aardoom, Dingemans, Spinhoven, et al., 2016). Alternatively, results on the effectiveness of online guidance of Baumeister et al. (2014) may not generalize to eating disorder interventions, where evidence seems mixed (Yim & Schmidt, 2019b). Accordingly, in a meta‐analysis studying the effect of individual components on effectiveness of e‐health interventions for eating disorders, guidance did not moderate intervention effectiveness (Barakat et al., 2019). Regardless of effectiveness, individuals with eating disorders are repeatedly found to value support in the context of internet interventions highly (Linardon et al., 2021; Yim & Schmidt, 2019a). It suggests that intervention effectiveness does not require satisfaction. Surprisingly, despite the higher satisfaction, there were relatively fewer adequate‐dose participants in conditions with expert‐patient support. For the combination condition, this may partly be explained by the fact that an adequate dose required 10 completed sessions instead of 5 in the other conditions. Nonetheless, many participants in the current study did not make (full) use of the option to receive weekly support, indicating they still experienced barriers to engage with the online support. These barriers were thought to be lower when guidance was offered by expert patients compared to health professionals. Specifically, perceived similarity between the participant and expert patient was proposed to be an important ingredient for the effectiveness of expert‐patient support, but no proof for this was found. Possibly, the perceived similarity was too low and little varied to detect any effect or 3 weeks were too few to build a rapport.
4.2. Future directions
Considering the ambiguity around guidance for internet‐based eating disorder interventions, more research specifically devoted to how it works and under which circumstances is warranted. Additionally, investigating predictors and moderators of internet‐based interventions like Featback and expert‐patient support might clarify who benefits from what kind of intervention, leading to more personalized treatment. Thirdly, an interesting next step might be to see if Featback and expert‐patient support can be improved by incorporating more innovative technologies, as there is still much ground to cover (Burger et al., 2020). For example, gamification, videos or Virtual Agents in addition to text alone show potential in improving mental health and engagement (Abd‐Alrazaq et al., 2020; Fleming et al., 2017). This is in line with evidence indicating that using multiple features that address different modalities has a positive influence on the effectiveness of technology‐enhanced eating disorder treatments (Barakat et al., 2019). Lastly, to better understand the effect of intervention usage on effectiveness, it might be valuable to investigate different durations of Featback and expert‐patient support.
4.3. Strengths and limitations
Strengths of the study are recruitment of a large sample size, the design including randomized allocation of participants, obtaining 12‐month follow‐up measures in all conditions with adequate retention of participants and maintaining an intent‐to‐treat approach making use of multiple imputations of the data. A limitation is the sole use of self‐report measures, which are subject to socially acceptable answers, misinterpretation and recall bias. Nevertheless, using self‐report allowed for maintaining the low‐threshold character of the intervention and participating in the study. Similarly, broad inclusion criteria were used to ensure the sample represented intended end users, improving generalization to real‐world settings. However, it is difficult to generalize the results to individuals with specific diagnoses, as rates of improvement may differ across diagnostic groups. A last consideration pertains to the number of planned contrasts. While they were conform the hypotheses as stated in the protocol, performing several tests increased the family‐wise error rate, which was mitigated by a Bonferroni correction of the p‐values. Nevertheless, a different statistical approach (e.g., factorial design with main and interaction effects of treatment) might have involved fitting fewer models, while still informing on the (relative) effectiveness of the internet interventions.
5. CONCLUSION
A fully automated low‐threshold internet‐based self‐help program for eating disorders (Featback), weekly chat or email support from an expert patient and the combination of both were effective in reducing eating disorder symptoms compared to a waiting list control condition. Although expert‐patient support improved satisfaction ratings, it did not improve the effectiveness. Now that beneficial effects of Featback have been confirmed in two randomized controlled trials, a next step is to implement the program and make it widely available. The current study highlights the potential of internet interventions such as Featback and expert‐patient support to reach the large group of undetected and underserved individuals with an eating disorder and help them address their problems, complementing the existing pallet of treatment options that currently exists for eating disorders.
AUTHOR CONTRIBUTIONS
Pieter Rohrbach: Conceptualization; data curation; formal analysis; investigation; methodology; project administration; software; validation; visualization; writing – original draft; writing – review and editing. Alexandra E. Dingemans: Conceptualization; funding acquisition; methodology; project administration; supervision; writing – original draft; writing – review and editing. Philip Spinhoven: Conceptualization; funding acquisition; methodology; project administration; supervision; writing – review and editing. Joost R. van Ginkel: Conceptualization; data curation; formal analysis; methodology; resources; software; validation; writing – review and editing. Marjolein Fokkema: Conceptualization; data curation; formal analysis; methodology; resources; software; validation; visualization; writing – review and editing. Tom F. Wilderjans: Formal analysis; methodology; resources; software; validation; writing – review and editing. Stephanie Bauer: Resources; software; writing – review and editing. Eric F. van Furth: Conceptualization; funding acquisition; methodology; project administration; supervision; writing – review and editing.
CONFLICT OF INTEREST
P. Rohrbach reports a grant from ZonMw during the conduct of the study. No other disclosures were reported.
Supporting information
Appendix S1 Supplementary Information
ACKNOWLEDGMENTS
The work was funded by ZonMw (636310001). First, the authors would like to thank Masja and Jiska for their contribution to the Featback program. Second, thanks goes out to all expert patients for supporting individuals throughout the study duration, and all participants for their contribution to the research. Third, the authors are grateful to Stefan Böhringer for his expert advice on the statistical analyses.
Rohrbach, P. J. , Dingemans, A. E. , Spinhoven, P. , Van Ginkel, J. R. , Fokkema, M. , Wilderjans, T. F. , Bauer, S. , & Van Furth, E. F. (2022). Effectiveness of an online self‐help program, expert‐patient support, and their combination for eating disorders: Results from a randomized controlled trial. International Journal of Eating Disorders, 55(10), 1361–1373. 10.1002/eat.23785
Action Editor: Tracey Wade
Funding information ZonMw, Grant/Award Number: 636310001
DATA AVAILABILITY STATEMENT
Data, materials and code are available upon reasonable request.
REFERENCES
- Aardoom, J. J. , Dingemans, A. E. , Spinhoven, P. , & van Furth, E. F. (2013). Treating eating disorders over the internet: A systematic review and future research directions. International Journal of Eating Disorders, 46(6), 539–552. 10.1002/eat.22135 [DOI] [PubMed] [Google Scholar]
- Aardoom, J. J. , Dingemans, A. E. , Spinhoven, P. , van Ginkel, J. R. , de Rooij, M. , & van Furth, E. F. (2016). Web‐based fully automated self‐help with different levels of therapist support for individuals with eating disorder symptoms: A randomized controlled trial. Journal of Medical Internet Research, 18(6), e159. 10.2196/jmir.5709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aardoom, J. J. , Dingemans, A. E. , & van Furth, E. F. (2016). E‐health interventions for eating disorders: Emerging findings, issues, and opportunities. Current Psychiatry Reports, 18(4), 1–8. 10.1007/s11920-016-0673-6 [DOI] [PubMed] [Google Scholar]
- Aardoom, J. J. , Dingemans, A. E. , van Ginkel, J. R. , Spinhoven, P. , van Furth, E. F. , & van den Akker‐Van Marle, M. E. (2016). Cost‐utility of an internet‐based intervention with or without therapist support in comparison with a waiting list for individuals with eating disorder symptoms: A randomized controlled trial. International Journal of Eating Disorders, 49(12), 1068–1076. 10.1002/eat.22587 [DOI] [PubMed] [Google Scholar]
- Abd‐Alrazaq, A. A. , Rababeh, A. , Alajlani, M. , Bewick, B. M. , & Househ, M. (2020). Effectiveness and safety of using chatbots to improve mental health: Systematic review and meta‐analysis. Journal of Medical Internet Research, 22(7), e16021. 10.2196/16021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrés‐Pepiñá, S. , Plana, M. T. , Flamarique, I. , Romero, S. , Borràs, R. , Julià, L. , Gárriz, M. , & Castro‐Fornieles, J. (2020). Long‐term outcome and psychiatric comorbidity of adolescent‐onset anorexia nervosa. Clinical Child Psychology and Psychiatry, 25(1), 33–44. 10.1177/1359104519827629 [DOI] [PubMed] [Google Scholar]
- Aron, A. , Aron, E. N. , & Smollan, D. (1992). Inclusion of other in the self scale and the structure of interpersonal closeness. Journal of Personality and Social Psychology, 63, 596–612. 10.1037/0022-3514.63.4.596 [DOI] [Google Scholar]
- Austin, A. , Flynn, M. , Richards, K. , Hodsoll, J. , Duarte, T. A. , Robinson, P. , Kelly, J. , & Schmidt, U. (2021). Duration of untreated eating disorder and relationship to outcomes: A systematic review of the literature. European Eating Disorders Review, 29(3), 329–345. 10.1002/erv.2745 [DOI] [PubMed] [Google Scholar]
- Barakat, S. , Maguire, S. , Smith, K. E. , Mason, T. B. , Crosby, R. D. , & Touyz, S. (2019). Evaluating the role of digital intervention design in treatment outcomes and adherence to eTherapy programs for eating disorders: A systematic review and meta‐analysis. International Journal of Eating Disorders, 52(10), 1077–1094. 10.1002/eat.23131 [DOI] [PubMed] [Google Scholar]
- Bauer, S. , & Goldschmidt, A. B. (2019). Introduction to the special issue on advancing assessment of, and interventions for, eating disorders via innovative uses of technology. International Journal of Eating Disorders, 52, 1073–1076. 10.1002/eat.23164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer, S. , Winn, S. , Schmidt, U. , & Kordy, H. (2005). Construction, scoring and validation of the short evaluation of eating disorders (SEED). European Eating Disorders Review, 13, 191–200. 10.1002/erv.637 [DOI] [Google Scholar]
- Baumeister, H. , Reichler, L. , Munzinger, M. , & Lin, J. (2014). The impact of guidance on internet‐based mental health interventions: A systematic review. Internet Interventions, 1(4), 205–215. 10.1016/j.invent.2014.08.003 [DOI] [Google Scholar]
- Beintner, I. , Jacobi, C. , & Taylor, C. B. (2012). Effects of an internet‐based prevention programme for eating disorders in the USA and Germany: A meta‐analytic review. European Eating Disorders Review, 20(1), 1–8. 10.1002/erv.1130 [DOI] [PubMed] [Google Scholar]
- Burger, F. , Neerincx, M. A. , & Brinkman, W. P. (2020). Technological state of the art of electronic mental health interventions for major depressive disorder: Systematic literature review. Journal of Medical Internet Research, 22(1), e12599. 10.2196/12599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardi, V. , Albano, G. , Ambwani, S. , Cao, L. , Crosby, R. D. , Macdonald, P. , Schmidt, U. , & Treasure, J. (2019). A randomised clinical trial to evaluate the acceptability and efficacy of an early phase, online, guided augmentation of outpatient care for adults with anorexia nervosa. Psychological Medicine, 1‐12, 2610–2621. 10.1017/S0033291719002824 [DOI] [PubMed] [Google Scholar]
- Cheng, J. , Edwards, L. J. , Maldonado‐Molina, M. M. , Komro, K. A. , & Muller, K. E. (2010). Real longitudinal data analysis for real people: Building a good enough mixed model. Statistics in Medicine, 29(4), 504–520. 10.1002/sim.3775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Boer, M. R. , Waterlander, W. E. , Kuijper, L. D. , Steenhuis, I. H. M. , & Twisk, J. W. R. (2015). Testing for baseline differences in randomized controlled trials: An unhealthy research behavior that is hard to eradicate. International Journal of Behavioral Nutrition and Physical Activity, 12(4), 4. 10.1186/s12966-015-0162-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis, C. (2003). Peer support within a health care context: A concept analysis. International Journal of Nursing Studies, 40, 321–332. 10.1016/S0020-7489(02)00092-5 [DOI] [PubMed] [Google Scholar]
- Dölemeyer, R. , Tietjen, A. , Kersting, A. , & Wagner, B. (2013). Internet‐based interventions for eating disorders in adults: A systematic review. BMC Psychiatry, 13(1), 207. 10.1186/1471-244X-13-207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn, C. G. , & Beglin, S. J. (2008). Assessment of eating disorders: Interview or self‐report questionnaire? International Journal of Eating Disorders, 16(4), 363–370. [DOI] [PubMed] [Google Scholar]
- Fleming, T. M. , Bavin, L. , Stasiak, K. , Hermansson‐Webb, E. , Merry, S. N. , Cheek, C. , Lucassen, M. , Lau, H. M. , Pollmuller, B. , & Hetrick, S. (2017). Serious games and gamification for mental health: Current status and promising directions. Frontiers in Psychiatry, 7, 215. 10.3389/fpsyt.2016.00215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fogarty, S. , Ramjan, L. , & Hay, P. (2016). A systematic review and meta‐synthesis of the effects and experience of mentoring in eating disorders and disordered eating. Eating Behaviors, 21, 66–75. 10.1016/j.eatbeh.2015.12.004 [DOI] [PubMed] [Google Scholar]
- Hart, L. M. , Granillo, M. T. , Jorm, A. F. , & Paxton, S. J. (2011). Unmet need for treatment in the eating disorders: A systematic review of eating disorder specific treatment seeking among community cases. Clinical Psychology Review, 31(5), 727–735. 10.1016/j.cpr.2011.03.004 [DOI] [PubMed] [Google Scholar]
- Holm, S. (1979). A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics, 6(2), 65–70. [Google Scholar]
- Jacobson, N. S. , & Truax, P. (1992). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. In Kazdin A. E. (Ed.), Methodological issues & strategies in clinical research (pp. 631–648). American Psychological Association. 10.1037/10109-042 [DOI] [PubMed] [Google Scholar]
- Kazdin, A. E. , Fitzsimmons‐Craft, E. E. , & Wilfley, D. E. (2017). Addressing critical gaps in the treatment of eating disorders. International Journal of Eating Disorders, 50(3), 170–189. 10.1002/eat.22670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killen, J. D. , Taylor, C. B. , Hammer, L. D. , Litt, I. , Wilson, D. M. , Rich, T. , Hayward, C. , Simmonds, B. , Kraemer, H. , & Varady, A. (1993). An attempt to modify unhealthful eating attitudes and weight regulation practices of young adolescent girls. International Journal of Eating Disorders, 13(4), 369–384. [DOI] [PubMed] [Google Scholar]
- Kroenke, K. , Spitzer, R. L. , Williams, J. B. W. , & Löwe, B. (2009). An ultra‐brief screening scale for anxiety and depression: The PHQ‐4. Psychosomatics, 50(6), 613–621. 10.1176/appi.psy.50.6.613 [DOI] [PubMed] [Google Scholar]
- Lewis, H. K. , & Foye, U. (2022). From prevention to peer support: A systematic review exploring the involvement of lived‐experience in eating disorder interventions. Mental Health Review Journal, 27(1), 1–17. 10.1108/MHRJ-04-2021-0033 [DOI] [Google Scholar]
- Linardon, J. , Messer, M. , Lee, S. , & Rosato, J. (2021). Perspectives of e‐health interventions for treating and preventing eating disorders: Descriptive study of perceived advantages and barriers, help‐seeking intentions, and preferred functionality. Eating and Weight Disorders‐Studies on Anorexia, Bulimia and Obesity, 26(4), 1097–1109. 10.1007/s40519-020-01005-3 [DOI] [PubMed] [Google Scholar]
- Linardon, J. , Shatte, A. , Messer, M. , Firth, J. , & Fuller‐Tyszkiewicz, M. (2020, August 27). E‐mental health interventions for the treatment and prevention of eating disorders: An updated systematic review and meta‐analysis. Journal of Consulting and Clinical Psychology, 88, 994–1007. 10.1037/ccp0000575 [DOI] [PubMed] [Google Scholar]
- Loucas, C. E. , Fairburn, C. G. , Whittington, C. , Pennant, M. E. , Stockton, S. , & Kendall, T. (2014). E‐therapy in the treatment and prevention of eating disorders: A systematic review and meta‐analysis. Behaviour Research and Therapy, 63, 122–131. 10.1016/j.brat.2014.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarroll, M. (2012). A pilot study on the effects of mentoring on disorderd eating behavior. Master's Theses and Doctoral Dissertations http://commons.emich.edu/theses/388
- Melioli, T. , Bauer, S. , Franko, D. L. , Moessner, M. , Ozer, F. , Chabrol, H. , & Rodgers, R. F. (2016). Reducing eating disorder symptoms and risk factors using the internet: A meta‐analytic review. International Journal of Eating Disorders, 49(1), 19–31. 10.1002/eat.22477 [DOI] [PubMed] [Google Scholar]
- Moessner, M. , & Bauer, S. (2017). Maximizing the public health impact of eating disorder services: A simulation study. International Journal of Eating Disorders, 50(12), 1378–1384. 10.1002/eat.22792 [DOI] [PubMed] [Google Scholar]
- Mond, J. M. , Hay, P. J. , Rodgers, B. , & Owen, C. (2006). Eating disorder examination questionnaire (EDE‐Q): Norms for young adult women. Behaviour Research and Therapy, 44(1), 53–62. 10.1016/j.brat.2004.12.003 [DOI] [PubMed] [Google Scholar]
- Nederlandse Zorgautoriteit . (2021). Informatiekaart wachttijden ggz 2021 https://puc.overheid.nl/nza/doc/PUC_648825_22/1/
- Perez, M. , Kroon van Diest, A. , & Cutts, S. (2014). Preliminary examination of a mentor‐based program for eating disorders. Journal of Eating Disorders, 2(1), 24. 10.1186/s40337-014-0024-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pittock, A. , Hodges, L. , & Lawrie, S. M. (2018). The effectiveness of internet‐delivered cognitive behavioural therapy for those with bulimic symptoms: A systematic review. BMC Research Notes, 11, 748. 10.1186/s13104-018-3843-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . (2018). R: a language and environment for statistical . www.R-project.org
- Ramjan, L. , Hay, P. , & Fogarty, S. (2017). Benefits of a mentoring support program for individials with an eating disorder: A proof of concept pilot program. BMC Research Notes, 10(1), 709. 10.1186/s13104-017-3026-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohrbach, P. J. , Dingemans, A. E. , Spinhoven, P. , van den Akker‐Van Marle, E. , van Ginkel, J. R. , Fokkema, M. , Moessner, M. , Bauer, S. , & van Furth, E. F. (2019). A randomized controlled trial of an internet‐based intervention for eating disorders and the added value of expert‐patient support: Study protocol. Trials, 20(1), 1–17. 10.1186/s13063-019-3574-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohrbach, P. J. , Dingemans, A. E. , van Furth, E. F. , Spinhoven, P. , van Ginkel, J. R. , Bauer, S. , & van den Akker‐Van Marle, M. E. (2022). Cost‐effectiveness of three internet‐based interventions for eating disorders: Results from a randomized controlled trial. International Journal of Eating Disorders, 1‐13. 10.1002/eat.23763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg, M. (1965). Society and the adolescent self‐image. Princeton: Princeton University Press. 10.1515/9781400876136 [DOI] [Google Scholar]
- Rubin, D. B. (1986). Statistical matching using file concatenation with adjusted weights and multiple imputations. Journal of Business and Economic Statistics, 4(1), 87–94. 10.1080/07350015.1986.10509497 [DOI] [Google Scholar]
- Rubin, D. B. (1987). Multiple imputation for nonresponse in surveys. Wiley. [Google Scholar]
- Schlegl, S. , Bürger, C. , & Voderholzer, U. (2015). The potential of technology‐based psychological interventions for anorexia and bulimia nervosa: A systematic review and recommendations for future research. Journal of Medical Internet Research, 17(3), e85. 10.2196/jmir.3554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzer, R. , & Jerusalem, M. (1995). Generalized self‐efficacy scale. In Weinman I. J., Wright S., & Johnston M. (Eds.), Measures in health psychology, a user's portfolio: Causal and control beliefs (pp. 35–37). Nfer‐Nelson. [Google Scholar]
- Simoni, J. M. , Franks, J. C. , Lehavot, K. , & Yard, S. S. (2011). Peer interventions to promote health: Conceptual considerations. American Journal of Orthopsychiatry, 81(3), 351–359. 10.1111/j.1939-0025.2011.01103.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens, I. (2001). Applied multivariate statistics for the social sciences (4th ed.). Psychology Press. 10.4324/9781410604491 [DOI] [Google Scholar]
- van Buuren, S. (2012). Flexible imputation of missing data (1st Edition). New York: Chapman &Hall/CRC Press. 10.1201/b11826 [DOI] [Google Scholar]
- van Buuren, S. , & Groothuis‐Oudshoorn, C. G. M. (2011). MICE: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45, 1–67. 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- van Eijk, L. M. , Kempen, G. I. J. M. , & van Sonderen, F. L. P. (1994). Een korte schaal voor het meten van sociale steun bij ouderen: de SSL‐12‐I. Tijdschrift voor Gerontologie en Geriatrie, 25(5), 192–196. [PubMed] [Google Scholar]
- Vollert, B. , Beintner, I. , Musiat, P. , Gordon, G. , Görlich, D. , Nacke, B. , Schmidt‐Hantke, J. , Potterton, R. , Spencer, L. , Grant, N. , Schmidt, U. , & Jacobi, C. (2019). Using internet‐based self‐help to bridge waiting time for face‐to‐face outpatient treatment for bulimia nervosa, binge eating disorder and related disorders: Study protocol of a randomized controlled trial. Internet Interventions, 16, 26–34. 10.1016/j.invent.2018.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade, T. D. , & Wilksch, S. M. (2018). Internet eating disorder prevention. Current Opinion in Psychiatry, 31(6), 456–461. 10.1097/YCO.0000000000000450 [DOI] [PubMed] [Google Scholar]
- Weissman, R. S. , & Rosselli, F. (2017). Reducing the burden of suffering from eating disorders: Unmet treatment needs, cost of illness, and the quest for cost‐effectiveness. Behaviour Research and Therapy, 88, 49–64. 10.1016/j.brat.2016.09.006 [DOI] [PubMed] [Google Scholar]
- Yim, S. H. , & Schmidt, U. (2019a). Experiences of computer‐based and conventional self‐help interventions for eating disorders: A systematic review and meta‐synthesis of qualitative research. International Journal of Eating Disorders, 52(10), 1108–1124. 10.1002/eat.23142 [DOI] [PubMed] [Google Scholar]
- Yim, S. H. , & Schmidt, U. (2019b). Self‐help treatment of eating disorders. Psychiatric Clinics, 42(2), 231–241. 10.1016/j.psc.2019.01.006 [DOI] [PubMed] [Google Scholar]
- Zeiler, M. , Kuso, S. , Nacke, B. , Klesges, L. M. , & Waldherr, K. (2021). Evaluating reach, adoption, implementation and maintenance of internet‐based interventions to prevent eating disorders in adolescents: A systematic review. The European Journal of Public Health, 31(1), i38–i47. 10.1093/eurpub/ckz130 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Supplementary Information
Data Availability Statement
Data, materials and code are available upon reasonable request.


