Abstract
Introduction
Uncertainty is an inevitable part of medical practice. An ability to tolerate uncertainty is viewed as a key competency across many health‐care systems. Poor uncertainty tolerance (UT) has been linked to negative outcomes including reduced psychological well‐being in medical students. A variety of medical education interventions have been developed with the intention of increasing medical students' UT. However, there is no synthesis of these studies available to inform education and research practice. Our aim was to conduct a scoping review of medical education interventions that evaluate their impact on UT.
Methods
Medline, PsycInfo, Embase and ERIC databases were searched for articles published from inception to December 2020. An extensive supplementary search was conducted and both quantitative and qualitative evaluations were included. For each intervention, we categorised the stimulus of uncertainty (ambiguity, complexity and/or probability) and mapped the students' reported cognitive, behavioural, and/or emotional response(s) to uncertainty onto an existing conceptual framework.
Results
Twenty‐two of 24 included studies reported a positive impact on medical student UT in at least one domain (cognitive, behavioural or emotional). Interventions included problem based learning‐based curricula, medical humanities, simulation, reflection and assessment. We found in four studies that a negative response in the emotional domain was reported despite positive responses also being reported in the cognitive and/or behavioural domains.
Conclusion
We identified a range of medical education interventions which report a positive impact on medical student UT. Further research is required to understand why a single intervention may stimulate a negative emotional response alongside a positive cognitive or behavioural response. In turn, this could support stakeholders such as policymakers and institutions to adapt the medical curriculum to better prepare their medical students for practice by enhancing their UT.
Short abstract
How can we improve medical students' uncertainty tolerance? This important question is addressed in the current issue through a review of existing interventions.
1. INTRODUCTION
Uncertainty, whether from increasingly complex disease states or conflicting clinical information, is inherent within the practice of medicine. 1 , 2 Subsequently, an ability for doctors to tolerate uncertainty is viewed as a key competency by regulating bodies in the UK, 3 US, 4 European Union, 5 Canada 6 and Australia. 7 There is growing evidence that medical students and doctors with lower tolerance of uncertainty are at higher risk of reduced psychological well‐being, including higher rates of burnout and stress. 8 , 9 Whilst the direct impact on patients is less clear, 9 studies suggest that reduced uncertainty tolerance (UT) in clinicians can be related to patients experiencing unnecessary investigations, distress and harm. 10 , 11
Whilst varying definitions of UT have been proposed, conceptual clarity has been offered by Hillen et al. 12 with Lee et al building on this and defining uncertainty as “the dynamic, subjective perception of not knowing what to think, feel, or do”. 13 Within this model uncertainty, experienced within an individual, can be the response to three principal sources: ambiguity (“lack of reliable, credible or adequate information”), probability (“randomness or indeterminacy of future outcomes”) or complexity (“features of information that limit understanding”). Uncertainty can then result in cognitive, emotional or behavioural responses which can be positive or negative. The model suggests that how an individual experiences uncertainty may be influenced by a range of moderators, which could include stimulus characteristics, individual characteristics and social factors. The strengths of this model include its comprehensive review of the existing literature and the subsequent development of conceptual clarity for this construct.
Undergraduate medical education has been suggested as a potential moderator to enhance medical students' UT. 10 , 12 , 13 Although a range of undergraduate medical educational interventions appear to have been described and their impact on UT evaluated, to the best of our knowledge none of these are built on existing theoretical frameworks, and there has been no comprehensive synthesis of such education interventions and their impact on UT.
The purpose of this study was to identify the range and type of interventions that have been developed to support UT in medical students and synthesise reported associations between the interventions and UT. The definitions within the Hillen et al. 12 model will be used to identify the source of uncertainty within interventions and consider the type of uncertainty response that interventions are provoking (cognitive, behavioural or emotional). This in turn would help to advance the research field by taking us closer to designing evidence‐based interventions that might support medical students in coping with the inherent uncertainty they will experience in their medical careers.
2. METHODS
This scoping review used Arksey and O′Malley's framework, 14 as updated by Levac et al. 15 We adhered to the Preferred Reporting Items for Systematic reviews and Meta‐Analyses Extension for Scoping Reviews (PRISMA‐ScR) guidelines. 16
2.1. Identifying the research question
The aims of this scoping review were to (a) to assess the nature and extent of the literature available to identify the range of medical education interventions that have been developed and evaluate their impact on UT and (b) to map the findings to Hillen et al.'s conceptual framework to inform future research. 12
2.2. Identifying relevant studies
Articles were included if they were (a) empirical and assessed the potential impact of a medical education intervention on tolerance of uncertainty or ambiguity and (b) were conducted within the medical student population. See Appendix S1 for the full inclusion criteria. The search strategy was developed by an iterative process with discussion among authors, including an information specialist. Medline (via OvidSp), PsycINFO (via OvidSp), Embase (via OvidSp) and ERIC (via EBSCOhost) were searched for articles published from inception to present day. The search was conducted on 9 December 2020. The full search strategy for each database is included in the Appendix S2. All retrieved citations were managed on EndNote X9.
Our supplementary search included searching the reference lists of the included studies, relevant studies identified by co‐authors, 8 , 9 , 12 , 13 non‐peer review databases and websites of relevant organisations, and professional bodies were searched for published or commissioned reports. Handsearching of key journals was conducted. We also contacted corresponding authors of relevant studies identified in the initial pilot search asking if they were aware of any further relevant articles. See Appendix S3 for the full supplementary search.
2.3. Study selection
After conducting the final search, duplicates were removed and the remaining articles were independently screened by two reviewers. After the initial title and abstract screening, author PP conducted a full‐text review of the remaining studies and excluded those studies which did not meet the inclusion criteria. All studies excluded by PP were discussed with either JH or MR, and any disagreements were resolved through discussion among both authors. The reasons for exclusion at this stage were recorded and are displayed in Figure 1.
FIGURE 1.
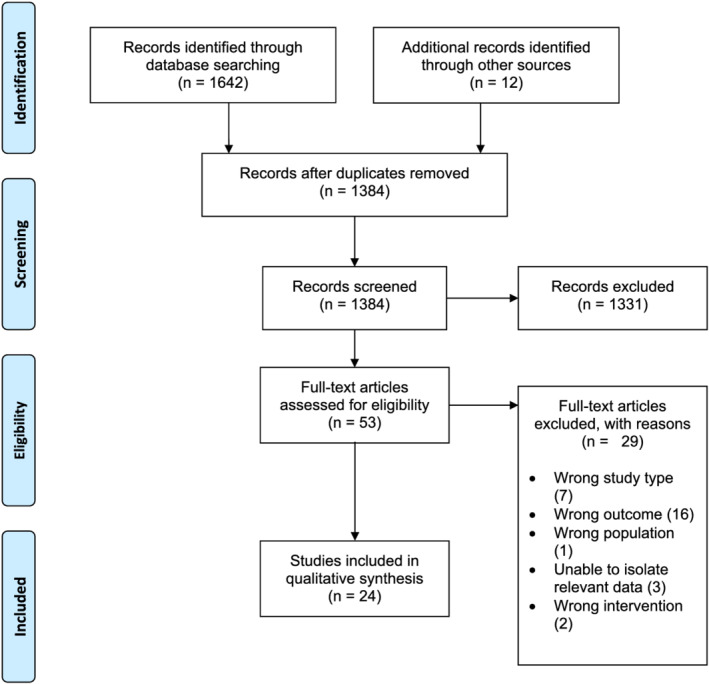
PRISMA flow diagram [Color figure can be viewed at wileyonlinelibrary.com]
2.4. Charting the data
A custom data extraction form was created by PP and was used to extract key information from each of the included studies. Information extracted included, but was not limited to, a brief description of the intervention, duration of intervention, stage and number of participants, outcome measures related to UT and the important findings.
2.5. Collating, summarising and reporting results
Each medical education intervention was categorised based on its description. This was done by PP, with input from authors JH, MR and SP.
Using Hillen et al.'s integrative model of UT and their published definitions, 12 authors PP and JH attempted to categorise the source(s) of uncertainty utilised in the included studies. Descriptions of the intervention, contained in the published papers, were used to do this. To understand the impact of the interventions on students' UT, we also mapped the outcomes reported within the published papers onto cognitive, behavioural, and/or emotional response(s) and their associated valency as either positive or negative where possible. The authors PP and JH independently reviewed each study to determine the reported uncertainty source(s) and response(s), with any disagreements resolved through discussion.
2.6. Undertaking consultation
Author PP facilitated an online consultation meeting with a medical student, medical educator and clinician on 10 June 2021. Author JH was also present. The purpose of this consultation was to present our preliminary results to aid the interpretation of our findings.
3. RESULTS
3.1. Search results
After removing duplicates, 1384 papers were screened using the inclusion and exclusion criteria (Appendix S3) resulting in 53 papers to include for full‐text review. After a full‐text review, 29 citations did not meet the inclusion criteria. A total of 24 studies were therefore included in this review which are summarised in Table 1. The PRISMA flowchart has been used to illustrate the search strategy used (see Figure 1).
TABLE 1.
Summary of 24 studies
| Author (s), year of publication (country) | Intervention description medical student population at time of delivery (n = total intervention population) | Evaluation of intervention (n = evaluated) | Author reported findings |
|---|---|---|---|
| Bartlett et al., 2018 17 (UK) | Simulation clinic session(s) Final year (Not reported) | Thematic analysis to explore the student's perceptions of the educational value of the session:
|
‘Students identified useful learning in time management, communication, decision making and managing uncertainty’ Some students ‘reported negative impacts on their perceptions of their ability to cope as a junior doctor’ |
| Bentwich and Gilbey, 2017 40 (Israel) | Lecture and discussion about art using visual thinking strategies 1st year (n = 120) | Self‐assessed Likert scale item related to UT: ‘Accept multiple possible meanings’ (n = 67/120 [55.8%]) | 67% of the students (n = 45) thought that the discussion of art works contributed to their acceptance of multiple possible meanings thereby implicitly recognising the existence of ambiguities |
| Bleakley and Brennan, 2011 18 (UK) | Curricula comparison All students throughout undergraduate training (n = 106) | Self‐assessed Likert scale item related to UT: ‘How well did your undergraduate course prepare you for coping with uncertainty’ (n = 146/198* [73.7%], intervention group n = 79, comparison group n = 67) | Significantly higher self‐assessed preparedness for coping with uncertainty in Peninsula college of medicine cohort compared with control (p = <0.001) |
| Del Vecchio et al., 2017 27 (US) | Lecture with interactive acting workshops 1st year (n = 50) | Self‐assessed Likert scale item related to UT: Item not reported (n = 12/50 [24%]) | Overall, n = 4 (33%) strongly agreed that the workshop helped improve their ability to deal with ambiguous situations |
| Drummond et al., 2016 19 (UK) | Activity using TDGs final year (n = 38) | Thematic analysis of focus group discussions (n = 28/38 [73.7%]) | Six key themes emerged from the data including ‘dealing with uncertainty and ambiguity’ |
| Fernandez et al., 2016 37 (Canada) | LbC question set 1st, 2nd and 3rd years (n = 900) | Thematic analysis of online qualitative feedback (n = 489/900 [54.3%]) |
‘Comments provided by students show that they reacted positively to being forced to position themselves about the uncertainty in the situation’ ‘1st year students found it hard to accept that there was no one right answer, 3rd year students very much appreciated the nuances separating expert opinions’ |
| Golden et al., 2018 28 (US) | Pilot phase: A simulation‐based education module 3rd and 4th years (n = 283) | Self‐assessed survey item related to UT: ‘I feel more comfortable speaking to families about medical uncertainties as a result of the session’ (n = 246/283 [86.9%]) | Pilot: 231/246 (94%) agree with survey item |
| Full implementation phase 3rd and 4th year medical students (n = 463) | Self‐assessed Likert scale item related to UT: ‘I feel better equipped to counsel patients when there is uncertainty about the clinical diagnosis or prognosis’ (n = 401/463 [86.6%]) | Full implementation: 395/401 (99%) agree or strongly agree with survey item | |
| Gowda et al., 2018 29 (US) | Facilitated museum‐based artwork reflection course 1st year (n = 47) |
Pre‐ and post‐intervention Tolerance for Ambiguity (TFA) scores (n = 35/47 [74.5%]) Narrative analysis of focus group (n = 18/47 [38.3%]) |
Though improvements were found on the TFA scale, the differences were not statistically significant Theme identified: ‘awareness of the subjectivity and uncertainty of perception’ |
| He et al., 2019 30 (US) | Museum‐based artwork course 1st, 2nd and 3rd years (n = 65) | Thematic analysis of qualitative self‐assessed survey developed by researchers (n = 65/65 [100%]) | Sub theme identified: ‘increased tolerance of ambiguity’ |
| Jones et al., 2002 20 (UK) | Curriculum comparison throughout undergraduate training for all students from 1994 (Not reported) |
Self‐assessed Likert scale item related to UT sent to graduates: ‘How well did the course prepare you for coping with uncertainty’? (n = 334/523* [63.7%], intervention graduates 163/267, comparison graduates 171/256) Supervisor assessed Likert scale item related to UT send to supervisors of graduates: “Please rate the Manchester PRHOs on their competence in Coping with uncertainty” (n = 320/412* [77.7%], intervention graduate supervisors 169/218, comparison graduate supervisors 151/194) |
Significantly higher self‐assessed preparedness for coping with uncertainty in PBL cohort compared with traditional cohort (p = 0.00) Significantly higher supervisor assessment of competence for coping with uncertainty in PBL cohort: compared with traditional cohort (p = 0.002) |
| Liou et al., 2019 31 (US) | Workshop involving interactions with horses 1st and 4th years (n = 12) | Budner's tolerance of ambiguity scale (n = 12/12 [100%]) |
Statistically significant changes in 1st year medical student scores (n = 7) (p = 0.02) No statistically significant changes in 4th year student scores (n = 5) |
| Lutz et al., 2016 38 (Germany) | Facilitated clinical reflection training sessions final year (n = 30) | Thematic content analysis of semi‐structured interviews (n = 18/30 [60%]) | ‘Students felt more able to persevere and to tolerate ambiguity’ |
| McCartan‐Welch, 1997 32 (US) | Literature and medicine courses 5th and 6th years (n = 60) | Ethnographic methodology involving observation, transcripts of class discussions, researcher designed student surveys and journal essay extracts | In summary, because these medical students had ‘to read in the fullest sense,’ and learn how to ‘[tolerate] ambiguity’ during this medical humanities experience, they had to begin realistically preparing for actual ‘doctor/patient encounters’ |
| Mennin et al., 1996 33 (US) | Curricula comparison throughout 1st and 2nd years of undergraduate training between 1983 and 1986 (n = 40) | Self‐assessed Likert scale item related to UT sent to graduates: ‘How well did the undergraduate medical curriculum prepare you for coping with uncertainty’ (n = 120/140* [85.7%], intervention group 33/40, comparison group 87/100) | Statistically significantly higher self‐reported preparedness for coping with uncertainty (p = 0.0001) |
| Nevalainen et al., 2010 39 (Finland) | Reflective portfolio course 3rd year (n = 22) | Thematic content analysis of 79 reflective learning diaries and 95 writings on specific themes (n = 22/22 [100%]) | ‘Reflective writing showed to be an effective means for the students of both expressing and dealing with uncertainty, both with the difficult and the pleasant feelings and the experiences the students had with their first patient contacts’ |
| O'Neill et al., 2003 21 (UK) | Curricula comparison throughout undergraduate training for all students from 1994 (Not reported) | Thematic analysis of transcripts of semi‐structured interviews of graduates (n = 47, intervention group n = 23 and comparison group n = 24) | ‘Graduates of the new, integrated curriculum seemed to be much better at dealing with uncertainty’ |
| Sam et al., 2020 22 (UK) | Clinical Prioritisation Questions 3rd year (n = 245) |
Researcher adapted Physicians Response to Uncertainty scale Binary survey item related to UT: ‘Do you think your tolerance of uncertainty would change by answering CPQs?” (n = 234/245 [95.5%]) |
‘On all five questions a higher proportion of students reported feeling more anxious when answering CPQs compared to SBAs’ ‘Significantly more students felt that continued use of CPQs would improve their tolerance of uncertainty compared to continued use of SBAs (66% (n = 154) versus 42% ([n = 98], p < 0.01)’ |
| Scott et al., 2020 23 (UK) | Uncertainty Simulation or standard simulation (control) Final year (n = 45) |
Thematic analysis of structured debrief: (n = 45/45 [100%], intervention group 12, comparison group 33) |
‘Students found that the “uncertainty simulation” helped them to develop clinical reasoning skills, such as gathering and weighing up information to form differential diagnoses’ ‘Students reported unease with the lack of an answer’ |
| Stephens et al., 2020 36 (Australia) | A core anatomy course 1st year (n = 608) | Framework analysis
|
Within anatomy education, student's tolerance of uncertainty appeared to be either facilitated or impeded by perceptions related to: (a) peers; (b) experts; (c) society and patients, and (d) grey case contexts. |
| Strohbehn et al., 2020 34 (US) | Museum‐based arts, hospital‐based arts or case‐based conferences (control) Clinical medical students (museum based n = 11, hospital based n = 10) | Tolerance of ambiguity scale (TOAS) (n = 35/35 [100%]) | No statistically significant difference in TOAS score from baseline |
| Watmough et al., 2006 (UK) 24 | Curricula comparison throughout undergraduate training (Not reported) | Supervisor assessed Likert scale item related to UT of graduates: Competence rating of ‘Coping with uncertainty’ (not reported) | Statistically significant improvement in ‘Coping with uncertainty’ in RMC compared with TMC (p = 0.03) |
| Watmough et al., 2006 (UK) 25 | Curricula comparison throughout undergraduate training (Not reported) | Self‐assessed Likert scale item related to UT sent to graduates: Competence rating of ‘Coping with uncertainty’ (376/639* [58.8%], intervention group n = 186/323, comparison group n = 190/316) | No significant difference in self‐reported perceived competence of ‘Coping with uncertainty’ between RMC and TMC graduates |
| Whitehouse et al., 2002 26 (UK) | Curricula evaluation Final year (Not reported) | Self‐assessed Likert scale items related to UT: ‘I believe I can cope with uncertainty in medical practice’ (n = 626/632) | 438 (70%) students agree or strongly agree that they can cope with uncertainty in medical practice. This was significantly associated with feelings of confidence |
| Wolpaw et al., 2009 35 (US) | Clinical feedback training using SNAPPS, feedback training group or usual‐and‐customary group (control) 3rd year (n = 162) | Quantitative content analysis of audiotaped student case presentations (n = 64/162 [39.5%], 215 presentations), SNAPPS group n = 21 (66 presentations), feedback training group n = 23 (67 presentations), usual‐and‐customary group n = 20 [82 presentations]) | ‘Students in the SNAPPS group formulated nearly eight times more questions and uncertainties than the students in the comparison group and more than twice as many as the students in the usual‐and‐customary groups (84.38 versus 10.77 and 33.33, χ 2(2) = 75.75, p < .000)’ |
(* = number of survey items sent by researchers; UT = Uncertainty Tolerance; TDGs = Tactical Decision Games; LbC = Learning by Concordance; PBL = Problem‐Based Learning; CPQs = Clinical Prioritisation Questions; SBAs = Single Best Answers; SNAPPS = Summarise history and findings, Narrow the differential, Analyse the differential, Probe preceptor about uncertainties, Plan management, Select case‐related issues for self‐study; RMC = Reformed Medical Curricula; TMC = Traditional Medical Curricula).
3.2. Characteristics of included studies
The characteristics of the 24 included studies are summarised in Table 1. Studies were conducted in the UK (10), 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 USA (9), 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 Australia (1), 36 Canada (1), 37 Germany (1), 38 Finland (1) 39 and Israel (1). 40 Twelve studies involved a single year group, 17 , 19 , 22 , 23 , 26 , 27 , 29 , 35 , 36 , 38 , 39 , 40 six involved a mixture of year groups, 28 , 30 , 31 , 32 , 34 , 37 five involved interventions employed throughout undergraduate training, 18 , 20 , 21 , 24 , 25 and one intervention was throughout the first and second years of training. 33 The total number of participants per educational intervention ranged from 12 31 to 900. 37 The total number of students participating was not reported for six of the studies. 17 , 20 , 21 , 24 , 25 , 26 The duration of interventions varied significantly, ranging from isolated sessions to spanning across multiple points of undergraduate medical training. It was therefore not possible to determine the median length of the medical education interventions. Attendance to the interventions were compulsory (10), 19 , 22 , 23 , 27 , 31 , 34 , 35 , 38 , 39 voluntary (9), 17 , 18 , 20 , 21 , 24 , 25 , 26 , 33 , 36 , 40 elective (i.e., a chosen module within the compulsory curricula) (2) 30 , 32 or mixed (3). 28 , 29 , 37 The intervention schedule varied; nine were single session exposures, 17 , 19 , 22 , 23 , 27 , 28 , 31 , 37 , 40 seven involved multiple sessions, 29 , 30 , 32 , 34 , 35 , 38 , 39 and eight were curricula wide. 18 , 20 , 21 , 24 , 25 , 26 , 33 , 36 In 22 of 24 included studies, the authors reported a positive impact on UT.
3.3. Characteristics of interventions and framework application
A range of intervention types were identified, which have been separated into nine categories using information provided in the published paper and discussions between the authors: Problem Based Learning (PBL) curricula (n = 7), 18 , 20 , 21 , 24 , 25 , 26 , 33 medical humanities (n = 6), 27 , 29 , 30 , 32 , 34 , 40 simulation (n = 3), 17 , 23 , 28 assessment (n = 2), 22 , 37 reflection (n = 2), 38 , 39 anatomy course (n = 1), 36 clinical feedback tool (n = 1), 35 equine facilitated learning (n = 1) 31 and Tactical Decision Games (n = 1). 19
None of the identified studies explicitly stated the source of uncertainty utilised according to any existing theory or definition. Subsequently, authors PP and JH used the reported intervention descriptions to determine this, where sufficient detail had been provided. In 11 of 24 studies, the sources of uncertainty were categorised using the definitions published within the Hillen et al. model. 12 These included ambiguity (n = 8), 19 , 23 , 29 , 30 , 31 , 32 , 36 , 40 probability (n = 4) 19 , 22 , 28 , 37 and complexity (n = 2). 23 , 37
Using the conceptual framework for UT developed by Hillen et al., 12 the reported student response(s) to uncertainty were mapped where possible, including whether the response was positive or negative. Ten studies did not report the students' responses to uncertainty in enough detail to allow mapping. 18 , 20 , 24 , 25 , 26 , 27 , 30 , 31 , 33 , 34 One study provided rich qualitative data regarding the moderating factors of UT within an anatomy course. 36 The authors felt this study could not be appropriately mapped using our binary approach to assessing the valency of response(s). Of the 13 mapped studies, we identified cognitive (n = 12), emotional (n = 8) and behavioural (n = 5) responses. All 13 studies reported positive responses to uncertainty, with four studies reporting a negative response in the emotional domain despite positive responses being reported in the cognitive and/or behavioural domains. 17 , 22 , 23 , 37 The response(s) to uncertainty for each mapped study within their intervention category are summarised in Table 2, which was constructed using feedback from the consultation meeting with stakeholders.
TABLE 2.
Categorised summary of studies mapped to their response(s) to uncertainty
| Cognitive | Emotional | Behavioural | |
|---|---|---|---|
| PBL‐based curricula 21 |

|

|
|
| Medical humanities 29 , 32 , 40 |

|

|
|
| Simulation 17 , 23 , 28 |

|

|

|
| Assessment 22 , 27 , 37 |

|

|
|
| Reflection 38 , 39 |

|

|
|
| Clinical feedback tool 35 |

|
||
| Tactical Decision Games 19 |

|

|
Positive response 
Negative response 
Both positive and negative response 
Number in circle refers to the papers reference
Seven studies explored PBL curricula as an intervention to increase UT in medical students. The authors were unable to determine the source(s) of uncertainty in any of these interventions due to insufficient detail being included in the published papers. It is difficult to determine if the observed increases in UT reported in these studies are directly due to the PBL components of the curriculum or due to other characteristics of the course, such as a community‐based learning emphasis. 20 , 21 , 26 , 33 O'Neill et al. was the only study from this category for which it was possible to map the assessed student responses to uncertainty onto the framework. 21 This qualitative study analysed semi‐structured interviews exploring challenging clinical situations of both PBL and traditional curricula graduates, finding that exposure to a PBL curricula was associated with positive cognitive and behavioural responses to uncertainty. 21
Six included interventions identified medical humanities as a potential means for improving UT. This review identified medical humanities programmes involving visual arts (four), 29 , 30 , 34 , 40 literature (one) 32 and drama (one). 27 In all four of the studies where it was possible to categorise the source of uncertainty, this was ambiguity. Two studies reported positive cognitive responses to uncertainty, 32 , 40 whilst one study found positive cognitive and emotional responses to uncertainty. 29
Three included studies used simulation‐based training which incorporated elements of uncertainty, 17 , 23 , 28 building upon suggestions to encourage confrontation and subsequent reflection of uncertain experiences. 41 For example, Scott et al. adapted a simulation scenario to replicate clinical uncertainty. 23 The simulated patient was confused with long and complex medical notes and had no unifying diagnosis. The sources of uncertainty were categorised in two simulation studies. Scott et al.'s scenario involved both ambiguity and complexity, 23 whereas Golden et al.'s communication simulation appeared to use probability as a source of uncertainty. 28 All three identified interventions appeared to provoke responses to uncertainty across the three domains. 17 , 23 , 28 Although cognitive and behavioural responses were positive in all three simulation studies, two studies reported negative emotional responses. 17 , 23
Both Learning by Concordance (LbC) 37 and Clinical Prioritisation Questions (CPQs) 22 were identified as potential alternative assessment strategies to improve student's response to uncertainty. Both interventions used probability as the source of uncertainty, with the LbC intervention also including complexity as a source. Although LbC and CPQs resulted in initial negative emotional responses, both studies suggest that students recognised the long‐term benefits of these alternative assessment styles. 22 , 37
3.4. Characteristics of evaluation approaches
Evaluation approaches to measuring UT included 13 quantitative studies, 18 , 20 , 22 , 24 , 25 , 26 , 27 , 28 , 31 , 33 , 34 , 35 , 40 10 qualitative studies, 17 , 19 , 21 , 23 , 30 , 32 , 36 , 37 , 38 , 39 and 1 study with mixed outcome measures. 29 Of the 14 studies with quantitative outcome measures, 9 used a single survey item, 18 , 20 , 21 , 22 , 23 , 24 , 28 , 33 , 40 3 used validated scales, 29 , 31 , 34 1 used a survey adapted from a validated scale 22 and 1 used a quantitative content analysis. 35 Of the 11 studies using qualitative methodologies, data collection methods included focus groups (n = 3), 17 , 19 , 29 semi‐structured interviews (n = 3), 21 , 36 , 38 qualitative written feedback (n = 3), 17 , 30 , 37 reflective diary entries and essays (n = 1), 39 structured debriefing (n = 1), 23 online discussion forums (n = 1) 36 and ethnography (n = 1). 32 As a result of the significant variation between these evaluation measures of UT, it is challenging to compare the outcomes of the identified studies. Of the 24 studies, 18 were post‐intervention evaluations only, 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 30 , 33 , 35 , 37 , 38 , 40 3 were pre‐ and post‐intervention evaluations 29 , 31 , 34 and 3 were recurrent longitudinal. 32 , 36 , 39 Of the 18 post‐intervention evaluation‐only studies, 1 was a 3‐group randomised control trial, 35 7 were 2‐group non‐randomised studies, 18 , 20 , 21 , 23 , 24 , 25 , 33 and 10 were single group only. 17 , 19 , 22 , 26 , 27 , 28 , 30 , 37 , 38 , 40 All but 2 25 , 34 of the 24 studies suggested, there was an impact on the medical students' UT. The reported findings of each study are summarised in Table 1.
For those studies utilising a quantitative approach single‐item scale, items were used in the majority of cases (9 of 13). For example, in 6 of 7 studies evaluating the impact of PBL curricula, a single item Likert scale was used to evaluate UT. In a smaller number of studies (n = 4), previously validated scales were used; however, it was not clear if two of these scales were valid for the population studied. 42 , 43 The quantitative measurements approaches used are summarised in S4 of the Appendix.
4. DISCUSSION
This review identified a range of medical education interventions that have been developed and their impact on UT in medical students evaluated. The most common interventions described included PBL‐based curricula and medical humanities. Twenty‐two of 24 studies reported a positive impact on medical student UT in at least one of the cognitive, behavioural or emotional domains. However, a single medical education intervention may be associated with a negative emotional response alongside a positive cognitive or behavioural response. Further research is required to understand the reasons for this disparity but may include the high stakes nature of these interventions (simulation and assessment). In time, this research will support institutions to better prepare their students for uncertainty in medicine by reviewing and adapting their current curricula.
The aims of this scoping review were to (a) to assess the nature and extent of the literature available to identify the range of medical education interventions that have been developed and evaluate their impact on UT and (b) to map the findings to Hillen et al.'s conceptual framework to inform future research. 12 This is the first paper to comprehensively review and synthesise undergraduate medical education interventions and their impact on UT in this population.
Our first key finding was that most studies (22 of 24) reported a positive impact on medical student UT. This suggests that a range of medical education interventions may facilitate improvements in medical student UT. Five studies explored student perceptions of UT development and found that students viewed this as a continual process that may be influenced, or moderated, by the described interventions. 22 , 23 , 36 , 37 , 39 This appears to be broadly consistent with the current body of literature regarding the development of personal epistemologies in medical education for constructs such as UT. It has been argued that during undergraduate training, medical students develop from a position where they view science as being based on ‘truths’ to an understanding that is much more contextualised and fluid. 44 In particular, it has been argued that this progression can be different for different components of the undergraduate curriculum. For example, students may view anatomy as certain, whilst accepting that much more fluidity exists for social sciences. Our findings therefore provide further evidence for the claim that UT may increase during undergraduate training in part due to education interventions acting as moderators of UT. Furthermore, our review suggests that there are a range of educational methods which may support students to develop improved UT, including PBL curricula, medical humanities and simulation.
Our second key finding was that a single intervention (simulation 17 , 23 and assessment 22 , 37 ) may be associated with a negative emotional response alongside a positive cognitive or behavioural response. It is important to note that in all of the studies that identified a negative emotional response, students reported that they viewed engagement with the intervention (simulation or assessment) valuable for longer‐term development of UT. It may be that external social factors, such as achievement pressures from institutions, could help to explain the observed immediate negative emotional responses in these high stakes (assessment) and or/high fidelity (simulation) interventions. For example, including elements of uncertainty within simulation training or written assessments, which generally involve unambiguous clinical presentations, may cause students acute feelings of discomfort or even distress. This is supported by two included simulation studies, 17 , 23 where some students expressed feelings of reduced self‐efficacy and “unease with the lack of an answer” despite finding it beneficial for their longer‐term learning. This exposure to uncertainty during medical education may therefore influence the development of student's personal epistemologies regarding the nature of clinical medicine, better preparing them for their future practice.
4.1. Strengths and limitations
Whilst other reviews have looked more broadly at how a range of health professional students engage with uncertainty, 45 this is the first scoping review focussed on medical education interventions in the medical undergraduate population. A strength of this review is its extensive and systematic search strategy involving a double screening process. Input from the authorship team throughout the formation of this paper harnessed a range of experiences including that of an information specialist, PBL tutor and medical education academic in the field. Additionally, the inclusion of a consultation stage helped us to interpret our findings and inform our results and discussion.
Our findings must be interpreted considering the limitations of the studies identified. Some of the deficiencies of the studies include the use of limited (single Likert item) and novel or new quantitative assessment methods where their validity for the populations studied have not been considered. 8 A further limitation is that many studies did not explore UT in depth and did not make their own definition of UT, or the source utilised (ambiguity, probability and complexity) explicit. The majority of studies did not appear to be underpinned by careful consideration of the existing theory or existing conceptual models. This is not a challenge unique to this construct but a common challenge encountered in the field of medical education. 46
Finally, our use of a binary approach to assess the valency of the response to uncertainty, as either positive or negative, may fail to appreciate more indistinct responses. It may be, for example, that using qualitative data collection methods 36 produces much richer data than quantitative studies alone when investigating this construct.
4.2. Implications for practice: Regulating bodies and medical institutions
Further research is needed before implications for policy changes to medical education can be discussed with confidence. Our findings suggest that medical education interventions such as PBL, reflective practice, medical humanities and assessment methods have the potential to improve students' UT. Institutions could consider how these existing elements of their curricula can be developed to better prepare students for uncertainty in clinical practice, for example, through meaningful exposure and supported reflection.
4.2.1. Priorities for educators
In thinking of implementing these insights into practice using the existing literature, theory and our own insights, we recommend that medical educators consider the importance of both the intervention and the environment that the intervention exists within. In particular, rather than placing an emphasis on the intervention in isolation, interventions should be offered to students within a wider supportive educational environment that promotes psychological safety. In turn, this could support students to engage with metacognition through reflection, where the intervention is acting as the stimulus, ultimately resulting in improved UT. These priorities are illustrated in the model for practice seen in Figure 2. Methods to implement this may include post‐intervention debriefing or feedback sessions around potentially distressing experiences. For example, Bartlett et al. altered their simulation session structure by allowing greater reflection during the debriefing and supporting staff to signpost to students where appropriate. 17 Results from these amendments are yet to be published.
FIGURE 2.
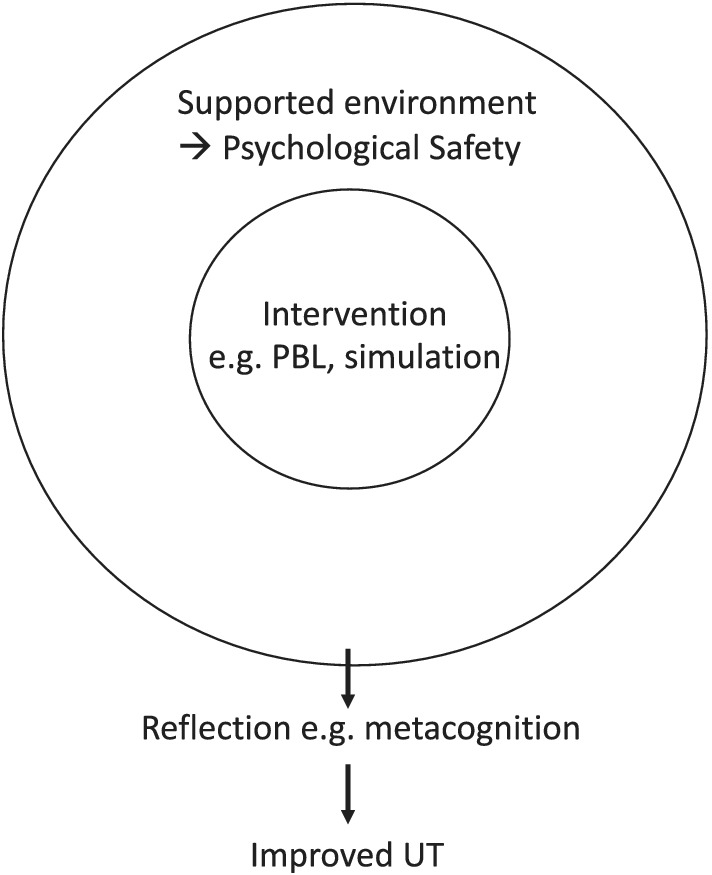
Model for practice
4.3. Future research
Further exploration of the negative emotional responses to uncertainty experienced following engagement with medical education interventions, such as assessment and simulation, is required. In particular, why negative emotional responses were in some cases seen alongside positive cognitive or behavioural responses. This should also include consideration of the strategies that could be employed to either mitigate this negative response or to support students to reflect on the reason(s) for this response.
Longitudinal research would also be required to assess whether long‐term UT is improved with such interventions in concordance with the perceptions of the students. It appears likely that using qualitative approaches to evaluate interventions and their impact on UT may provide much richer and detailed findings than using quantitative approaches alone. Finally, we echo the recommendations of a recent commentary that calls for medical education researchers to be clearer about the definitions and theory that underpins their intervention development, and to consider making use of a complex interventions framework to guide this. 46
FUNDING
Not applicable.
CONFLICTS OF INTEREST
None.
ETHICS STATEMENT
No human subjects were involved. Ethical approval for this project was granted under low‐risk typology A ethics route by the Clinical Education Independent Research project ethics committee.
AUTHOR CONTRIBUTIONS
All authors were involved from the conception and design of the project through multiple team meetings. PP wrote the main body of the paper with substantial amendments made by JH, MR and SP. All authors reviewed and approved the final paper before submission.
We have all agreed to be accountable for all aspects of the paper.
Supporting information
TABLE S1 Inclusion and exclusion criteria
TABLE S2 Search terms
TABLE S3 Supplementary search strategy
TABLE S4 Quantitative scales used to assess tolerance of uncertainty
ACKNOWLEDGEMENTS
The authors would like to thank Professor Karen Mattick for reviewing draft copies of the manuscript and providing thoughtful and insightful feedback. The authors would also like to thank Dr Rory Conn, Dr Stephanie Bull and Dr Ellie Moxey for providing valuable feedback during a focus group session for the consultation stage of this review.
Patel P, Hancock J, Rogers M, Pollard SR. Improving uncertainty tolerance in medical students: A scoping review. Med Educ. 2022;56(12):1163‐1173. doi: 10.1111/medu.14873
REFERENCES
- 1. Fox RC. The evolution of medical uncertainty. Milbank Mem Fund Q Health Soc. 1980;58(1):1‐49. doi: 10.2307/3349705 [DOI] [PubMed] [Google Scholar]
- 2. Geller G, Faden RR, Levine DM. Tolerance for ambiguity among medical students: implications for their selection, training and practice. Soc Sci Med. 1990;31(5):619‐624. doi: 10.1016/0277-9536(90)90098-D [DOI] [PubMed] [Google Scholar]
- 3. General Medical Council: outcomes for graduates. 2018. https://www.gmc-uk.org/-/media/documents/dc11326-outcomes-for-graduates-2018_pdf-75040796.pdf
- 4. National Academies of Sciences EaM , National Academy of Medicine , Committee on Systems Approaches to Improve Patient Care by Supporting Clinician W‐B . Taking Action Against Clinician Burnout: A Systems Approach to Professional Well‐Being. National Academies Press (US); 2019. [PubMed] [Google Scholar]
- 5. Cumming A, Ross M. The tuning project for medicine—learning outcomes for undergraduate medical education in Europe. Med Teach. 2007;29(7):636‐641. doi: 10.1080/01421590701721721 [DOI] [PubMed] [Google Scholar]
- 6. Medical Council of Canada . Examination objectives overview: Scholar. https://mcc.ca/objectives/scholar/
- 7. Toohey S, Ham J, Hughes C, Harris P, McNeil P. Expectations for level of achievement of the graduate capabilities in each phase of the curriculum. 2005.
- 8. Hancock J, Mattick K. Tolerance of ambiguity and psychological well‐being in medical training: a systematic review. Med Educ. 2020;54(2):125‐137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Strout TD, Hillen M, Gutheil C, et al Tolerance of uncertainty: a systematic review of health and healthcare‐related outcomes. Patient Educ Couns. 2018;101(9):1518‐1537. [DOI] [PubMed] [Google Scholar]
- 10. Hall KH. Reviewing intuitive decision‐making and uncertainty: the implications for medical education. Med Educ. 2002;36(3):216‐224. [DOI] [PubMed] [Google Scholar]
- 11. Lysdahl KB, Hofmann BM. What causes increasing and unnecessary use of radiological investigations? A survey of radiologists perceptions. BMC Health Serv Res. 2009;9:155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hillen MA, Gutheil CM, Strout TD, Smets EMA, Han PKJ. Tolerance of uncertainty: conceptual analysis, integrative model, and implications for healthcare. Soc Sci Med. 2017;180:62‐75. [DOI] [PubMed] [Google Scholar]
- 13. Lee C, Hall K, Anakin M, Pinnock R. Towards a new understanding of uncertainty in medical education. J Eval Clin Pract. 2020;27(5):1195‐1204. [DOI] [PubMed] [Google Scholar]
- 14. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19‐32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 15. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA‐ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467‐473. doi: 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 17. Bartlett M, Gay SP, Kinston R, McKinley R. Taking on the doctor role in whole‐task simulation. Clin Teach. 2018;15(3):236‐239. [DOI] [PubMed] [Google Scholar]
- 18. Bleakley A, Brennan N. Does undergraduate curriculum design make a difference to readiness to practice as a junior doctor? Med Teach. 2011;33(6):459‐467. [DOI] [PubMed] [Google Scholar]
- 19. Drummond I, Sheikh G, Skinner J, Wood M. Exploring the feasibility and acceptability of using tactical decision games to develop final year medical students non‐technical skills. Med Teach. 2016;38(5):510‐514. [DOI] [PubMed] [Google Scholar]
- 20. Jones A, McArdle PJ, O'Neill PA Perceptions of how well graduates are prepared for the role of pre‐registration house officer: a comparison of outcomes from a traditional and an integrated PBL curriculum. Med Educ. 2002;36(1):16‐25. doi: 10.1046/j.1365-2923.2002.01105.x [DOI] [PubMed] [Google Scholar]
- 21. O'Neill PA, Jones A, Willis SC, McArdle PJ Does a new undergraduate curriculum based on Tomorrows Doctors prepare house officers better for their first post? A qualitative study of the views of pre‐registration house officers using critical incidents. Med Educ. 2003;37(12):1100‐1108. doi: 10.1046/j.1365-2923.2003.01714.x [DOI] [PubMed] [Google Scholar]
- 22. Sam AH, Wilson RK, Lupton M, et al Clinical prioritisation questions: a novel assessment tool to encourage tolerance of uncertainty? Med Teach. 2020;42(4):416‐421. [DOI] [PubMed] [Google Scholar]
- 23. Scott A, Sudlow M, Shaw E, Fisher J. Medical education, simulation and uncertainty. Clin Teach. 2020;17(5):497‐502. [DOI] [PubMed] [Google Scholar]
- 24. Watmough S, Taylor DC, Garden A, Ryland I. Educational supervisors views on the competencies of preregistration house officers. Br J Hosp Med (Lond). 2006;67(2):92‐95. [DOI] [PubMed] [Google Scholar]
- 25. Watmough S, Ryland I, Taylor DC. Preregistration house officer skill and competency assessment through questionnaires. Bri J Hosp Med (Lond). 2006;67(9)487‐490. [DOI] [PubMed] [Google Scholar]
- 26. Whitehouse CR, O'Neill P, Dornan T Building confidence for work as house officers: student experience in the final year of a new problem‐based curriculum. Med Educ. 2002;36(8):718‐727. doi: 10.1046/j.1365-2923.2002.01287.x [DOI] [PubMed] [Google Scholar]
- 27. Del Vecchio A, Pfennig C, Moschella P. Medical student response to improvisation and acting training: Novel curriculum pilot study. Ann Emerg Med. 2017;70(4):S34‐S35. [Google Scholar]
- 28. Golden WC, Patel SC, Chou B, et al Development and evaluation of a simulation‐based, medical student teaching session for communicating bad news and uncertainty along the obstetric‐neonatal continuum. Medical Sci Educ. 2018;28(1):211‐219. [Google Scholar]
- 29. Gowda D, Dubroff R, Willieme A, Swan‐Sein A, Capello C. Art as sanctuary: a four‐year mixed‐methods evaluation of a visual art course addressing uncertainty through reflection. Acad Med. 2018;93:S8‐S13. [DOI] [PubMed] [Google Scholar]
- 30. He B, Prasad S, Higashi RT, Goff HW. The art of observation: a qualitative analysis of medical students experiences. BMC Med Educ. 2019;19(1):234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Liou KT, Jamorabo DS, Geha RM, Crawford CM, George P, Schiffman FJ. Foreign bodies: is it feasible to develop tolerance for ambiguity among medical students through Equine‐Facilitated learning? Med Teach. 2019;41(8):960‐962. [DOI] [PubMed] [Google Scholar]
- 32. McCartan‐Welch KM. Resistance and Reflection: The Humanities Experience for Medical Students . Ph.D. University of Missouri; ‐ Columbia; 1997. ProQuest. [Google Scholar]
- 33. Mennin SP, Kalishman S, Friedman M, Pathak D, Snyder J,. A survey of graduates in practice from the University of New Mexicos conventional and community‐oriented, problem‐based tracks. Acad Med. 1996;71(10)1079‐1089. [DOI] [PubMed] [Google Scholar]
- 34. Strohbehn GW, Hoffman SJK, Tokaz M, et al. Visual arts in the clinical clerkship: a pilot cluster‐randomised, controlled trial. BMC Med Educ. 2020;20(1):481. doi: 10.1186/s12909-020-02386-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wolpaw T, Klara K. Papp, Bordage G Using SNAPPS to facilitate the expression of clinical reasoning and uncertainties: a randomised comparison group trial. Acad Med. 2009;84(4):517‐524. doi: 10.1097/ACM.0b013e31819a8cbf [DOI] [PubMed] [Google Scholar]
- 36. Stephens GC, Rees CE, Lazarus MD. Exploring the impact of education on preclinical medical students tolerance of uncertainty: a qualitative longitudinal study. Adv Health Sci Educ. 2020;26(1)53‐77. [DOI] [PubMed] [Google Scholar]
- 37. Fernandez N, Foucault A, Dube S, et al Learning‐by‐Concordance (LbC): introducing undergraduate students to the complexity and uncertainty of clinical practice. Can Med Educ J. 2016;7(2):e104‐e113. [PMC free article] [PubMed] [Google Scholar]
- 38. Lutz G, Roling G, Berger B, Edelhauser F, Scheffer C. Reflective practice and its role in facilitating creative responses to dilemmas within clinical communication—a qualitative analysis. BMC Med Educ. 2016;16(1):301. doi: 10.1186/s12909-016-0823-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Nevalainen MK, Mantyranta T, Pitkala KH. Facing uncertainty as a medical student—a qualitative study of their reflective learning diaries and writings on specific themes during the first clinical year. Patient Educ Couns. 2010;78(2):218‐223. [DOI] [PubMed] [Google Scholar]
- 40. Bentwich ME, Gilbey P. More than visual literacy: art and the enhancement of tolerance for ambiguity and empathy. BMC Med Educ. 2017;17(1):200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Merrill JM, Camacho Z, Laux LF, Lorimor R, Thornby JI, Vallbona C. Uncertainties and ambiguities: measuring how medical students cope. Med Educ. 1994;28(4):316‐322. [DOI] [PubMed] [Google Scholar]
- 42. Herman JL, Stevens MJ, Bird A, Mendenhall M, Oddou G. The tolerance for ambiguity scale: towards a more refined measure for international management research. Int J Intercult Relat. 2010;34(1):58‐65. [Google Scholar]
- 43. Geller G, Tambor ES, Chase GA, Holtzman NA. Measuring physicians tolerance for ambiguity and its relationship to their reported practices regarding genetic testing. Med Care. 1993;31(11):989‐1001. [DOI] [PubMed] [Google Scholar]
- 44. Knight LV, Mattick K. ‘When I first came here, I thought medicine was black and white’: making sense of medical students ways of knowing. Soc Sci Med. 2006;63(4):1084‐1096. [DOI] [PubMed] [Google Scholar]
- 45. Moffett J, Hammond J, Murphy P, Pawlikowska T. The ubiquity of uncertainty: a scoping review on how undergraduate health professions students engage with uncertainty. Adv Health Sci Educ. 2021;26(3):913‐958. doi: 10.1007/s10459-021-10028-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hancock J, Mattick K. Mindfulness, complex interventions and conceptual clarity. Med Educ. 2020;54(9):774‐776. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
TABLE S1 Inclusion and exclusion criteria
TABLE S2 Search terms
TABLE S3 Supplementary search strategy
TABLE S4 Quantitative scales used to assess tolerance of uncertainty


