INTRODUCTION
Each year, tens of millions of patients are admitted to US hospitals. 1 Among older adults who are hospitalized, 30%–50% will become unable to complete one or more activities of daily living (ADLs) after discharge—a condition termed hospital‐associated disability (HAD). 2 , 3 Over a quarter of those with HAD will experience prolonged in ADL disability. 4 Older adults with low mobility during hospitalization are six times more likely to be institutionalized at the time of discharge and 34 times more likely to die. 5 In spite of these detrimental, life‐altering, and sometimes permanent effects, hospitalists remain largely unaware of how to manage HAD and other addressable but often overlooked antecedent functional mobility impairments that can occur during acute hospitalization. So how can we begin to formalize our understanding and management of these common, yet nuanced clinical conditions? The answer may be easier than you think: we treat them like any other disease we manage in the hospital. For inpatient functional mobility impairments this will require clarifying (1) terminology, (2) risk assessment and diagnostics, and (3) treatment strategies.
IS IT TIME FOR A CLINICAL GUIDELINE?
Imagine a 78‐year‐old patient with hypertension, well controlled insulin‐dependent diabetes, and history of hip replacement surgery 3 years ago is admitted to your service for community‐acquired pneumonia requiring 2 L of supplemental oxygen. The patient is independent with ADLs prior to admission and ambulates without an assistive device. After 5 days, the patient is on room air and planned for discharge. However, the nurse notes that the patient has been in bed nearly 100% of the time despite not being considered a fall risk. She is now requiring significant assistance just to get out of bed. You consult physical and occupational therapy for disposition recommendations and they suggest subacute rehabilitation due to development of HAD and physical deconditioning.
Disability leading to a nonhome discharge represents a poor outcome for a patient who was independent prior to admission and, with proper risk assessment and mobilization, may have returned home at discharge. However, since HAD and physical deconditioning are not commonly thought of as medical conditions, they can be forgotten while addressing primary problems during hospitalization. This is compounded by the absence of standardized guidance on how to recognize, diagnose, or prescribe treatment for functional mobility impairments in the medical acute care setting. Therefore, our primary purpose is to propose the development of a clinical practice guideline (CPG) for the “Management of HAD and Physical Deconditioning in Patients Hospitalized for Acute Medical Illness” to initiate a paradigm shift in how we prioritize, diagnose, and intervene upon functional mobility impairments during hospitalization.
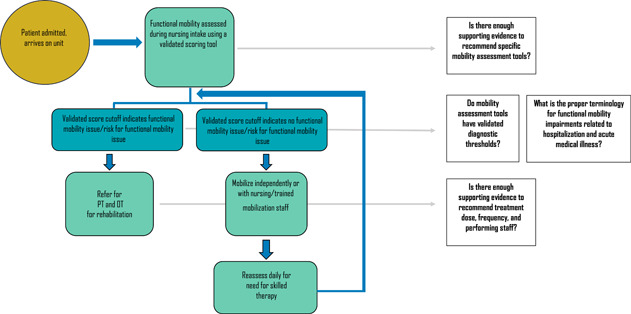
It is critical that the CPG be evidence‐based and free from bias in the process of its creation and within its evidence base. We did not complete a formal literature review, but employed the Appraisal of Guidelines for Research and Evaluation (AGREE II) instrument 6 to guide our assessment of whether there is data to support a medical inpatient mobility CPG. The instrument's “Rigour of Development” domain states that there be “an explicit link between the recommendations and the supporting evidence.” We, therefore, developed the following framework to outline ideal management and areas in need of evidence to support a CPG:
TERMINOLOGY
Which terms should be used to describe functional mobility impairments in the hospital?
This may be the most important step toward compelling clinicians to see these conditions as diseases that require attention during hospitalization. Functional mobility impairments are alternatively and inconsistently labeled as physical deconditioning, HAD, debility, functional decline, generalized weakness, and more. However, HAD is a condition specifically related to hospitalization and can reasonably be applied to a decrease in abilties related to acute illness and bedrest. For consistency, we will refer to acute ADL impairments as “HAD” since an impairment in one's ability to care for oneself may be considered a “disability” and development in the setting of acute illness while in the hospital implies “hospital‐associated,” making this term quite precise. New impairments in physical performance will be referred to as “physical deconditioning.” These may or not be the exact terms used by an expert panel in a CPG but making this distinction would be a crucial first step for guideline developers.
POPULATION
Who should be assessed?
For patients hospitalized for acute medical conditions, there are no validated scores that combine risk factors to create an overall risk score for development of HAD or physical deconditioning. There is a large body of literature describing risk factors for HAD and many can be assessed at the time of admission. Age is one major risk factor 3 but cognitive and mood disorders can also confer very high risk. 7 , 8 , 9 A patient's level of function prior to admission and their need for assistive devices with ambulation can be clues to whether they require mobility assessment as these are also potent risk factors. 10 , 11 Most experts agree that mobility assessment should be done for all patients at the time of admission since bedrest is harmful for nearly everyone. It is likely that guideline developers would make this recommendation based on “expert opinion.” Future research focusing on prediction scores for development of HAD or physical deconditioning could strengthen this recommendation by adding a validated screening tool. Screening, however, would likely continue to be recommended in all hospitalized patients.
DIAGNOSIS
How do we diagnose HAD and physical deconditioning?
In 2018, the American Geriatrics Society released a white paper 12 stating their recommendations for mobility assessment in older adults, which highlighted 14 validated tools for evaluating functional mobility and physical performance in older patients. Of these, seven were validated in the acute care setting and, five took only a few minutes to complete and, importantly, could be performed by either rehabilitation therapists or nursing staff. Two of these assessments, the Activity Measure Post‐Acute Care (AM‐PAC) 13 score and the Johns Hopkins Highest Level of Mobility (JH‐HLM) score, have since had further evidence supporting their reliability and construct validity for assessments done by nurses and therapists. 14 The AM‐PAC score would thus be important to include in a CPG for HAD diagnosis while physical performance tools such as JH‐HLM and even gait speed, 15 which is validated and has established diagnostic cutpoints, may be used for diagnosis of physical deconditioning. Future research may then focus on the predictive precision of the cutpoints that are used as thresholds to prescribe varying intensities of treatment.
TREATMENT
How do we treat functional mobility impairments in the medical acute care setting?
The best way to treat and prevent HAD and physical deconditioning is with mobilization beginning early in admission. This can be accomplished by physical and occupational therapists, nursing staff, or other properly trained staff. There are myriad studies describing the association of early mobilization and rehabilitation of ADL loss with decreases in length‐of‐stay, functional decline, institutionalization, disability, and mortality in hospitalized patients. 16 , 17 , 18 , 19 , 20 , 21 As with other medical conditions, treatment should be tailored to the patient and consider “severity of illness.” There is also longstanding evidence that amount and duration of rehabilitation matter, 22 , 23 so an optimal CPG would not only recommend mobilization but would specify “dose,” “frequency,” and “mode of delivery” (e.g., skilled therapy vs. ambulate with nursing staff).
IF NOT NOW, THEN WHEN?
One might argue that we don't yet have enough evidence to support official recommendations. But given the existing literature on diagnosis, treatment, and consequences of functional mobility impairments, it seems unacceptable that hospitalists are given no systematic way to manage these conditions. Imagine if all elderly patients admitted for sepsis due to a urinary tract infection received a cardiology consult to ensure they were not inadvertently discharged to home with any cardiac conditions. Because of the lack of understanding of functional mobility impairments, physical or occupational therapists are frequently consulted in this way. Their dual responsibility as therapists administering treatment and experts providing recommendations for safe discharge levels of care means therapists are frequently saddled with triaging, diagnosing, and treating mobility issues regardless of a patient's functional status. In fact, PT referrals occur for hospitalized patients with no need for skilled therapy as much as 38% of the time. 24 But given they are a constrained resource in most hospital settings, like other consultants, their services should be reserved for the appropriate patients. Targeting allocation of skilled therapy to vulnerable patients is key for treating and preventing HAD and physical deconditioning in hospitalized patients but cannot be achieved with the current standards of practice.
It is possible that current evidence supports only level 2B recommendations (weak recommendation, moderate‐quality evidence). However, any guidelines could significantly improve how hospitalists manage functional mobility impairments. They would also serve to focus future research, getting us closer to 1A recommendations (strong recommendation, high‐quality evidence). It is simply critical that we comprehend that our patients present with and develop distinct “mobility maladies” and “ability ailments” related to their acute illness and hospitalization. Formal framing of these conditions and their life‐changing effects will help clinicians begin to manage them like other conditions, which is an essential step toward home and functional independence for our patients.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ACKNOWLEDGMENTS
Dr. Maylyn Martinez and Dr. Jason R. Falvey are funded by National Institute on Aging (M.M.: NIA P30 AG066619; JRF: NIA K76AG074926).
Martinez M, Falvey JR, Cifu A. Deconditioned, disabled, or debilitated? Formalizing management of functional mobility impairments in the medical inpatient setting. J Hosp Med. 2022;17:843‐846. 10.1002/jhm.12910
REFERENCES
- 1. Freeman W, Weiss AJ, Heslin KC. Overview of U.S. Hospital stays in 2016: variation by geographic region. Accessed April 4, 2022. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb246-Geographic-Variation-Hospital-Stays.jsp [PubMed]
- 2. Loyd C, Markland AD, Zhang Y, et al. Prevalence of hospital‐associated disability in older adults: a meta‐analysis. J Am Med Dir Assoc. 2020;21(4):455‐461. 10.1016/j.jamda.2019.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51:451‐458. [DOI] [PubMed] [Google Scholar]
- 4. Gill TM, Gahbauer EA, Han L, Allore HG. Functional trajectories in older persons admitted to a nursing home with disability after an acute hospitalization. J Am Geriatr Soc. 2009;57(2):195‐201. 10.1111/j.1532-5415.2008.02107.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brown CJ, Friedkin RJ, Inouye SK. Prevalence and outcomes of low mobility in hospitalized older patients. J Am Geriatr Soc. 2004;52(8):1263‐1270. 10.1111/j.1532-5415.2004.52354.x [DOI] [PubMed] [Google Scholar]
- 6. Brouwers M, Kho ME, Browman GP, et al. AGREE II: advancing guideline development, reporting and evaluation in healthcare. Can Med Assoc J. 2010;182:E839‐E842. 10.1503/cmaj.090449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Covinsky KE, Fortinsky RH, Palmer RM, Kresevic DM, Landefeld CS. Relation between symptoms of depression and health status outcomes in acutely ill hospitalized older persons. Ann Intern Med. 1997;126(6):417‐425. [DOI] [PubMed] [Google Scholar]
- 8. Sands LP, Yaffe K, Covinsky K, et al. Cognitive screening predicts magnitude of functional recovery from admission to 3 months after discharge in hospitalized elders. J Gerontol A Biol Sci Med Sci. 2003;58(1):M37‐M45. [DOI] [PubMed] [Google Scholar]
- 9. Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23(10):433‐441. [DOI] [PubMed] [Google Scholar]
- 10. Lindenberger EC, Landefeld CS, Sands LP, et al. Unsteadiness reported by older hospitalized patients predicts functional decline. J Am Geriatr Soc. 2003;51(5):621‐626. [DOI] [PubMed] [Google Scholar]
- 11. Mahoney JE, Sager MA, Jalaluddin M. Use of an ambulation assistive device predicts functional decline associated with hospitalization. J Gerontol A Biol Sci Med Sci. 1999;54(2):M83‐M88. [DOI] [PubMed] [Google Scholar]
- 12. Wald HL, Ramaswamy R, Perskin MH, et al, Quality and Performance Measurement Committee of the American Geriatrics Society . The case for mobility assessment in hospitalized older adults: American Geriatrics Society white paper executive summary. J Am Geriatr Soc. 2019;67(1):11‐16. 10.1111/jgs.15595 [DOI] [PubMed] [Google Scholar]
- 13. Jette DU, Stilphen M, Ranganathan VK, Passek SD, Frost FS, Jette AM. Validity of the AM‐PAC “6‐Clicks” inpatient daily activity and basic mobility short forms. Phys Ther. 2014;94(3):379‐391. 10.2522/ptj.20130199 [DOI] [PubMed] [Google Scholar]
- 14. Hoyer EH, Young DL, Klein LM, et al. Toward a common language for measuring patient mobility in the hospital: reliability and construct validity of interprofessional mobility measures. Phys Ther. 2018;98(2):133‐142. 10.1093/ptj/pzx110 [DOI] [PubMed] [Google Scholar]
- 15. Kim HJ, Park I, Lee HJ, Lee O. The reliability and validity of gait speed with different walking pace and distances against general health, physical function, and chronic disease in aged adults. J Exerc Nutrition Biochem. 2016;20(3):46‐50. 10.20463/jenb.2016.09.20.3.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Martínez‐Velilla N, Casas‐Herrero A, Zambom‐Ferraresi F, et al. Effect of exercise intervention on functional decline in very elderly patients during acute hospitalization: a randomized clinical trial. JAMA Inter Med. 2019;1791:28‐36. 10.1001/jamainternmed.2018.4869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Baztán JJ, Suárez‐García FM, López‐Arrieta J, Rodríguez‐Mañas L, Rodríguez‐Artalejo F. Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta‐analysis. BMJ. 2009;338:b50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bachmann S, Finger C, Huss A, Egger M, Stuck AE, Clough‐Gorr KM. Inpatient rehabilitation specifically designed for geriatric patients: systematic review and meta‐analysis of randomised controlled trials. BMJ. 2010;340:c1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Inouye SK, Bogardus ST, Jr. , Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669‐676. [DOI] [PubMed] [Google Scholar]
- 20. Reuben DB, Borok GM, Wolde‐Tsadik G, et al. A randomized trial of comprehensive geriatric assessment in the care of hospitalized patients. N Engl J Med. 1995;332(20):1345‐1350. [DOI] [PubMed] [Google Scholar]
- 21. Leff B, Burton L, Mader SL, et al. Comparison of functional outcomes associated with hospital at home care and traditional acute hospital care. J Am Geriatr Soc. 2009;57(2):273‐278. [DOI] [PubMed] [Google Scholar]
- 22. Roach KE, Ally D, Finnerty B, et al. The relationship between duration of physical therapy services in the acute care setting and change in functional status in patients with lower‐extremity orthopedic problems. Phys Ther. 1998;78(1):19‐24. 10.1093/ptj/78.1.19 [DOI] [PubMed] [Google Scholar]
- 23. Peiris CL, Taylor NF, Shields N. Extra physical therapy reduces patient length of stay and improves functional outcomes and quality of life in people with acute or subacute conditions: a systematic review. Arch Phys Med Rehabil. 2011;92(9):1490‐1500. 10.1016/j.apmr.2011.04.005 [DOI] [PubMed] [Google Scholar]
- 24. Martinez M, Cerasale M, Baig M, et al. Defining potential overutilization of physical therapy consults on hospital medicine services. J Hosp Med. 2021;16:553‐555. [DOI] [PubMed] [Google Scholar]


