Abstract
Introduction
Recently, in the view of network analysis, depression has been conceptualized as a complex and dynamic network model combining individual symptoms. To date, no studies have systematically examined and compared depressive symptom networks across different populations.
Methods
A total of 36,105 participants were recruited and asked to complete the Patient Health Questionnaire-9 among junior high school students, senior high school students, college students, and elderly adults who were more susceptible to depression during the COVID-19 lockdown in China. In the analysis, we applied the optimal cutoff score ≥ 8 for students and a score ≥ 6 for elderly adults to identify 5830 participants who were likely to be depressed. The index of “strength” was used to identify central symptoms in the network structure.
Results
The results showed that Sad Mood was the most central symptom among junior high school students, senior high school students, and college students, but the most central symptom in the elderly was Guilt. Among the top three central symptoms, Suicide Ideation was unique to senior high school students, while Anhedonia was most prevalent among college students. Guilt - Suicide Ideation, Anhedonia – Energy, Anhedonia - Sad Mood, and Sleep – Energy showed the strongest association among junior and senior high school students, college students, and elderly adults, respectively. NCT (i.e., Network Comparison Test) suggested that the network's global connectivity was ultimately inconsistent, but the network structure remained roughly intact.
Conclusion
In treatment, targeting central symptoms may be critical to alleviating depression.
Keywords: Depression, Junior high school students, Senior high school students, College students, Elderly adults, Network analysis
1. Introduction
Depression is different from unhappiness or typical feelings of sadness and is, instead, a psychiatric illness combining cognitive, emotional and physical symptoms, including anhedonia, emptiness, hopelessness, and sleep disorders (American Psychiatric Association, 2013; Paunio et al., 2015). As a widely prevalent psychological disorder, depressive symptoms are associated with individuals' impaired social function in multiple domains, including work, school, family, and relationships (Altshuler et al., 2006; Bertha and Balázs, 2013). In severe cases, depressed patients may even hold suicidal ideation or attempt suicide (Balázs et al., 2013; Fergusson et al., 2005). Major depressive disorder, the principal form of depression, is a recurrent lifelong illness, and the most likely period for the onset of its first episode extends from mid-adolescence to one's mid-40s, but nearly 40 % experience their first episode before the age of 20 (Moffitt et al., 2010). To make matters worse, the lifetime risk of depression is approximately 15–18 % at a global level, with a peak prevalence occurring in the second and third decades of life and a subsequent but more modest peak in the fifth and sixth decades (Bromet et al., 2011; Moffitt et al., 2010; World Health Organization, 2017). As early as 2008, the WHO ranked major depression as the third leading cause of the global burden of disease and predicted that by 2030, the disease would become the leading cause of mortality and morbidity in the world (Malhi and Mann, 2018). Therefore, to reduce the risk of depression and provide effective interventions and treatments, it is crucial to understand the underlying pathological mechanism of depression.
From the traditional causal perspective of mental disorders, depression causes low mood and suicidality, just like infection causes fever (Borsboom and Cramer, 2013). Accordingly, traditional statistical approaches (i.e., the latent factor approach) assume that depression is an unobservable factor that generates observable specific symptoms. (Fried, 2015). That is, symptoms are loosely aggregated to describe the latent factor (Schmittmann et al., 2013). Hence, this approach cannot illustrate the dynamic interactions among indicators or symptoms assessed by the Patient Health Questionnaire-9 (PHQ-9) (Kroenke et al., 2001), a tool that can detect and assess the severity of depression (Dalege et al., 2016). A new approach called network analysis was proposed to conceptualize psychological phenomena in recent years (Borsboom and Cramer, 2013). According to network analysis theory, symptoms are not scattered points. Instead, they closely interact to form and maintain a unified pathological disease (Costantini and Perugini, 2018; Epskamp et al., 2018). These symptom-to-symptom interactions are clearly presented within the network, allowing researchers to identify the symptoms that play a major role in causing the onset of a syndrome. Thus, interventions targeting central symptoms may be more efficient (Borsboom and Cramer, 2013).
Since the outbreak of the COVID-19 pandemic at the end of 2019, countries, particularly China, have implemented active disease containment measures (e.g., lockdown and quarantine) to prevent this pandemic from harming people (Jin et al., 2022). On the other hand, however, a lack of normal public contacts or daily routines causes individuals to suffer from great anxiety and uncertainties, which in turn lead to psychological disorders, such as depression (Fancourt et al., 2021; Robb et al., 2020). Particularly, students (both from high school and college) (Cao et al., 2022; Wang et al., 2020) and elderly adults (Amicucci et al., 2021; Luo et al., 2021) reported higher rates of depression than adults during lockdowns in China, since these populations have particularly high needs for care and interpersonal relationships. Given their vulnerability to depression, these two groups warrant special attention and study.
A previous study showed that loneliness, sadness, self-hatred, fatigue, self-deprecation, and crying were prominent central symptoms in the depressive symptom network of American adolescents (Gijzen et al., 2021). In 2021, during the COVID-19 pandemic and political chaos in Hong Kong, a network was also used to examine the depressive symptoms of Hong Kong residents, revealing that guilt (i.e., feeling bad about yourself - or that you're a failure or have let yourself or your family down), sad mood (i.e., feeling down, depressed or hopeless), and energy (i.e., feeling tired or having little energy) were the three most prevalent central symptoms in adults aged between 18 and 59 years (Cheung et al., 2021). However, depression can be influenced by socioeconomic status and external affairs (Lorant et al., 2003). Therefore, as high-risk groups for depression during this pandemic period, mainland Chinese students and elderly adults may have different experiences due to differences in demographic information and social environment. Thus, the investigation of depressive symptoms in these groups is necessary.
To the best of our knowledge, no studies have comprehensively explored depressive symptom networks for a particular age group, especially for students and elderly adults. To address this knowledge gap, we conducted this study to (1) investigate the network structure of depressive symptoms for four groups during the COVID-19 pandemic lockdown period: junior high school students, senior high school students, college students, and elderly adults. (2) Clarifying the top central symptoms in the four different networks; and (3) presenting the strongest symptom-to-symptom interaction in each network. Moreover, previous studies using network analysis did not select participants who might have clinical depressive symptoms. A score above 5 on the PHQ-9 indicates that a person has a mild or higher level of depression severity (Kroenke et al., 2001). We applied population-specific cutoff scores to filter those who were likely to have depression in the current study.
2. Methods
2.1. Participants
This cross-sectional study was conducted in Harbin, China, between November and December 2021. A total of 13,999 junior high school students (male, 7056; female, 6943), 12,550 senior high school students (male, 6590; female, 5960), 6710 college students (male, 3074; female, 3636), and 2846 elderly adults whose ages are above 60 years (male, 878; female, 1968) completed the PHQ-9. According to previous studies, the optimal cutoff score of the PHQ-9 to screen probable positive cases for depression was ≥8 for students (Manea et al., 2012) and ≥ 6 for elderly adults (Chen et al., 2016). With this standard, 1793 (12.81 %) junior high school students, 2854 (22.74 %) senior high school students, 830 college students (12.37 %), and 353 (12.40 %) elderly adults were included in the study.
The research aim was clarified in the participants' electronic informed consent before starting the assessment. The research was examined and approved by the ethics committee of the first author's university (reference number: 202112220084).
2.2. Measures
2.2.1. Patient Health Questionnaire-9 (PHQ-9)
The PHQ-9 comprises nine items (Kroenke et al., 2001). Each item is graded on a scale from 0 (not at all) to 3 (nearly every day) to assess depressive symptoms, including anhedonia, sad mood, sleep, energy, appetite, guilt, concentration, motor function, and suicide ideation in the last two weeks (Löwe et al., 2004). Higher scores indicate higher levels of depression severity. In China, the PHQ-9 has been proven to be valid (Wang et al., 2014; Zhang et al., 2013).
2.3. Data analysis
All statistical analyses were conducted in R (R Core Team, 2021).
2.3.1. Item selection
In the network analysis, nodes represent symptoms, and edges represent relationships between two nodes. The association between two nodes was calculated by partial correlation analysis, keeping other nodes' interference constant.
First, the mean, standard deviation, kurtosis, and skewness of all PHQ-9 items were examined. Standard deviation was used to evaluate the informativeness of each item, and potential item redundancy was checked (Mullarkey et al., 2019). Following the manual (Jones, 2021), if the polychoric correlation between two variables and other items was significantly different, the proportion of which falls below 25 %, it would be confirmed that these two items measured the same feature/symptom (i.e., redundancy). The R package ‘networktools 1.3.0’ (Jones, 2021) was used for the item redundancy test.
2.3.2. Network estimation
Second, in accordance with current guidelines, an extended Bayesian information criterion (EBIC) graphical least absolute shrinkage and selection operator (LASSO) network model containing all items was estimated (Epskamp and Fried, 2018). After controlling for all other symptoms in the network, the association between each pair of symptoms was calculated using polychoric correlation. Small correlations were shrunk to exactly zero by using LASSO, with the related tuning parameter set using the EBIC. All nonzero correlations were conditionally dependent (i.e., not spuriously due to any other network variable), and the network became sparser and easier to understand. In the current study, blue and red represent positive and negative correlations, respectively. More saturated and thicker edges indicated stronger connections between two nodes. The R packages qgraph 1.6.9 and bootnet 1.4.3 were used for network estimation and visualization (Epskamp et al., 2018; Epskamp et al., 2012).
Third, the R packages qgraph 1.6.9 (Epskamp et al., 2012) and mgm 1.2–12 (Haslbeck and Waldorp, 2020) were used to assess network properties by computing two metrics: strength (i.e., the sum of absolute edge weights between one node and all other nodes connected to it) (Valente, 2012) and predictability (i.e., how well one node can be predicted by its neighboring nodes) (Epskamp et al., 2018; Haslbeck and Waldorp, 2018). Previous research has shown that assessments of closeness and betweenness are unreliable in determining nodes' importance (Bringmann et al., 2019; Epskamp et al., 2016). Hence, strength was chosen as the metric in the current study.
2.3.3. Estimation of network stability
Fourth, we used a case-dropping bootstrap procedure to ensure the robustness of node strength (Epskamp et al., 2018). Dropping a proportion of data does not result in significant changes in the existing network, ensuring its stability. The index used to assess network stability is the correlation stability coefficient (CS-C). The CS-C indicates the maximum number of cases that might be removed from the sample when centrality indices in the subset correlate with centrality indices in the original network at the 0.7 level with a probability of 95 % (Epskamp et al., 2018). Generally, the value of CS-C should be >0.25, preferably >0.5.
Finally, we computed confidence intervals (Cls) using nonparametric bootstrapping to examine the accuracy of edge weights and the nodes' centrality. Meanwhile, bootstrap tests based on 0.95 CIs were performed to analyze the difference between the strengths of two edges or two nodes; if CIs did not include zero, there was a significant difference between the strengths of two edges or two nodes.
All analyses of network stability were performed by the R package bootnet (Version 1.4.3) (Epskamp et al., 2018).
2.3.4. Comparison of network characteristics among the four groups
Finally, we used the network comparison test (NCT) to assess the difference between two networks based on several invariance measures (e.g., network structure invariance, global strength invariance, edge invariance). This assessment was performed with the R package NetworkComparisonTest (Version 2.2.1) (van Borkulo et al., 2021). The network structure conveys the maximum difference between two networks' pairwise edges. Edge invariance means the difference between two networks' individual edge weights, and global strength refers to the sum of all edge weights in each network. The Holm–Bonferroni correction was used for multiple comparisons between two networks at the individual edge level. Previous studies have not systematically examined depressive symptom network structures among different groups (Abdul Karim et al., 2021; Cheung et al., 2021). The current study compared network structure invariance, edge invariance, and global strength among different subgroups (i.e., junior high school students, senior high school students, college students, and elderly adults).
3. Results
3.1. Item check and descriptive statistics
Item informativeness (i.e., the standard deviation of the item) and item redundancy were checked first. No item was found to be poorly informative (i.e., 2.5 SD below the mean level of informativeness), and no item was found to be redundant with any other item (i.e., < 25 % of significantly different correlations). The mean, SD, skewness, and kurtosis of depressive symptoms measured by the PHQ-9 are shown in Table 1 .
Table 1.
Descriptive statistics for the network variables.
| Group (N) | Item | Node | M | SD | Skewness | Kurtosis | Strengtha | Predictability |
|---|---|---|---|---|---|---|---|---|
| JH (1793) | PHQ1 | Anhedonia | 1.68 | 0.88 | 0.07 | −0.88 | −0.17 | 0.24 |
| PHQ2 | Sad Mood | 1.46 | 0.91 | 0.29 | −0.77 | 1.78 | 0.31 | |
| PHQ3 | Sleep | 1.47 | 1.02 | 0.18 | −1.10 | −1.59 | 0.16 | |
| PHQ4 | Energy | 1.67 | 0.93 | 0.09 | −1.05 | 0.74 | 0.25 | |
| PHQ5 | Appetite | 1.40 | 1.02 | 0.21 | −1.08 | −0.83 | 0.13 | |
| PHQ6 | Guilt | 1.53 | 0.96 | 0.17 | −0.98 | 0.73 | 0.27 | |
| PHQ7 | Concentration | 1.46 | 1.00 | 0.17 | −1.05 | −0.29 | 0.16 | |
| PHQ8 | Motor | 1.28 | 0.99 | 0.33 | −0.90 | −0.61 | 0.18 | |
| PHQ9 | Suicide | 0.88 | 0.99 | 0.88 | −0.36 | 0.23 | 0.24 | |
| SH (2854) | PHQ1 | Anhedonia | 1.80 | 0.90 | −0.01 | −1.09 | −0.18 | 0.32 |
| PHQ2 | Sad Mood | 1.52 | 0.92 | 0.26 | −0.86 | 1.82 | 0.41 | |
| PHQ3 | Sleep | 1.59 | 1.11 | −0.03 | −1.35 | −1.12 | 0.18 | |
| PHQ4 | Energy | 1.89 | 0.90 | −0.08 | −1.22 | 0.56 | 0.31 | |
| PHQ5 | Appetite | 1.55 | 1.05 | 0.05 | −1.22 | −1.27 | 0.17 | |
| PHQ6 | Guilt | 1.64 | 0.99 | 0.02 | −1.11 | 0.10 | 0.31 | |
| PHQ7 | Concentration | 1.60 | 1.04 | −0.03 | −1.20 | −0.94 | 0.20 | |
| PHQ8 | Motor | 1.30 | 1.09 | 0.33 | −1.18 | 0.37 | 0.29 | |
| PHQ9 | Suicide | 0.83 | 1.02 | 1.01 | −0.21 | 0.67 | 0.34 | |
| College (830) | PHQ1 | Anhedonia | 1.50 | 0.77 | 0.57 | −0.39 | 0.53 | 0.28 |
| PHQ2 | Sad Mood | 1.35 | 0.72 | 0.71 | 0.26 | 1.74 | 0.40 | |
| PHQ3 | Sleep | 1.33 | 0.88 | 0.39 | −0.53 | −0.56 | 0.16 | |
| PHQ4 | Energy | 1.47 | 0.74 | 0.73 | −0.19 | 0.87 | 0.32 | |
| PHQ5 | Appetite | 1.33 | 0.88 | 0.44 | −0.47 | −1.66 | 0.11 | |
| PHQ6 | Guilt | 1.30 | 0.81 | 0.49 | −0.15 | −0.42 | 0.24 | |
| PHQ7 | Concentration | 1.44 | 0.86 | 0.37 | −0.56 | −0.74 | 0.15 | |
| PHQ8 | Motor | 1.00 | 0.85 | 0.67 | −0.00 | −0.11 | 0.27 | |
| PHQ9 | Suicide | 0.61 | 0.80 | 1.23 | 0.86 | 0.34 | 0.26 | |
| Elderly (353) | PHQ1 | Anhedonia | 1.49 | 0.94 | 0.27 | −0.89 | −0.94 | 0.62 |
| PHQ2 | Sad Mood | 1.28 | 0.88 | 0.52 | −0.38 | 0.82 | 0.68 | |
| PHQ3 | Sleep | 1.56 | 0.97 | 0.17 | −1.04 | −0.93 | 0.56 | |
| PHQ4 | Energy | 1.60 | 0.89 | 0.33 | −0.94 | 0.27 | 0.66 | |
| PHQ5 | Appetite | 1.38 | 0.88 | 0.37 | −0.57 | −1.04 | 0.63 | |
| PHQ6 | Guilt | 1.24 | 0.95 | 0.42 | −0.71 | 2.07 | 0.68 | |
| PHQ7 | Concentration | 1.41 | 0.94 | 0.32 | −0.82 | −0.32 | 0.59 | |
| PHQ8 | Motor | 1.36 | 0.93 | 0.43 | −0.69 | 0.17 | 0.66 | |
| PHQ9 | Suicide | 1.01 | 0.96 | 0.62 | −0.60 | −0.11 | 0.56 |
Note. JH, Junior high school students. SH, Senior high school students. a The values of node strength were standardized z scores from the network.
3.2. Network structure and centrality measures analysis
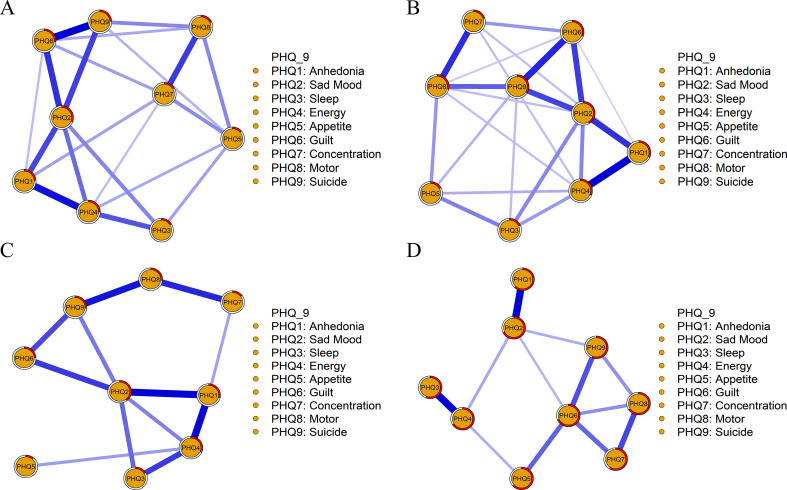
Four depressive symptom networks are shown in Fig. 1 and Fig. S1, and the corresponding partial correlation matrix is presented in Tables S2-S5. The edge of Guilt - Suicide Ideation (PHQ6-PHQ9) showed the strongest association, followed by the edge of Anhedonia - Energy (PHQ1-PHQ4) and the edge of Sad Mood - Guilt (PHQ2-PHQ6), among junior high school students. The edge of Anhedonia - Energy (PHQ1-PHQ4) showed the strongest association, followed by the edge of Guilt - Suicide Ideation (PHQ6-PHQ9) and the edge of Anhedonia - Sad Mood (PHQ1-PHQ2), among senior high school students.
Fig. 1.
The network structure of the major depressive symptoms among junior high school students, senior high school students, college students, and elderly adults.
The edge of Anhedonia - Sad Mood (PHQ1-PHQ2) showed the strongest association, followed by the edge of Anhedonia - Energy (PHQ1-PHQ4) and the edge of Motor Function- Suicide Ideation (PHQ8-PHQ9), among college students. The edge of Sleep - Energy (PHQ3-PHQ4) showed the strongest association, followed by the edge of Anhedonia - Sad Mood (PHQ1-PHQ2) and Concentration - Motor Function (PHQ7-PHQ8), among elderly adults.
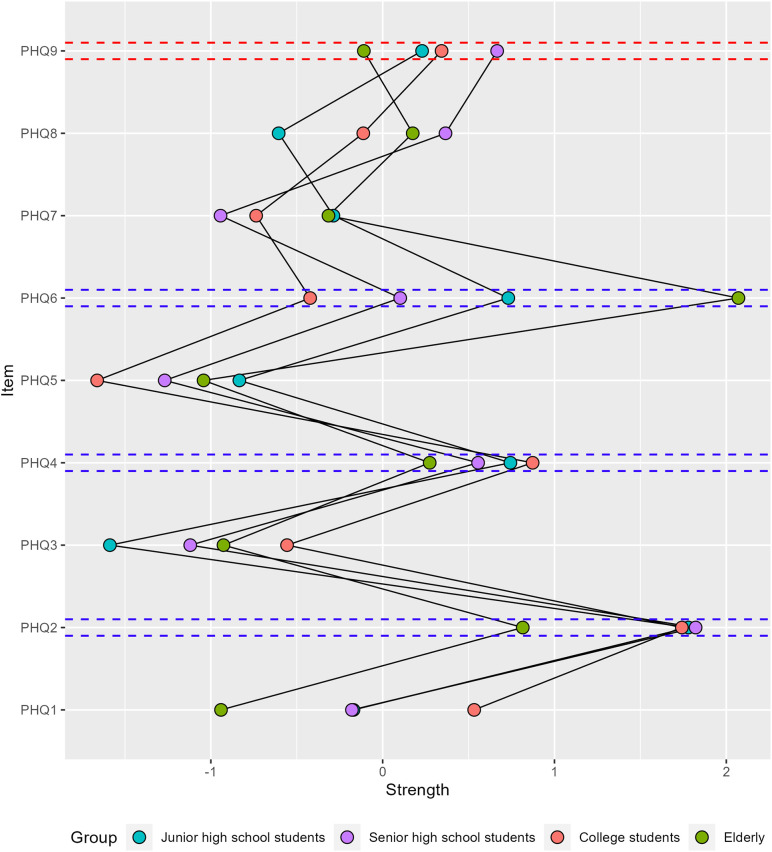
In Table 1, Fig. 2 and Fig. S2, Sad Mood (PHQ2) had the highest node strength in the depressive symptom network among junior high school students, followed by Energy (PHQ4) and Guilt (PHQ6), and an average of 21.5 % of the variance could be potentially accounted for by each node's neighbors (M predictability = 0.215 ± 0.059). Sad Mood (PHQ2) had the highest node strength in the depressive symptom network among senior high school students, followed by Suicide Ideation (PHQ9) and Energy (PHQ4), and an average of 28.1 % of the variance could be potentially accounted for by each node's neighbors (M predictability = 0.281 ± 0.082). Sad Mood (PHQ2) had the highest node strength in the depressive symptom network of college students, followed by Energy (PHQ4) and Anhedonia (PHQ1), and an average of 24.4 % of the variance could be potentially accounted for by each node's neighbors (M predictability = 0.244 ± 0.089). Guilt (PHQ6) had the highest node strength in the depressive symptom network among elderly adults, followed by Sad Mood (PHQ2) and Energy (PHQ4), and an average of 62.7 % of the variance could be potentially accounted for by each node's neighbors (M predictability = 0.627 ± 0.048).
Fig. 2.
The strength (centrality) value (standardized Z scores) of the major depressive symptoms among junior high school students, senior high school students, college students, and elderly adults. The red dashed line indicates the core symptoms newly identified in this study (Top three). The blue dashed line denotes core symptoms that have been found in previous studies (Top three). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
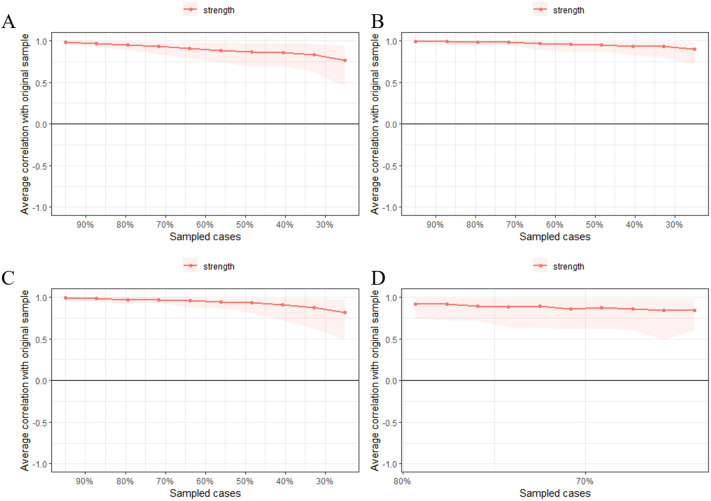
3.3. Network and stability
In Fig. 3 , the case-dropping bootstrap procedure shows that CS-C was 0.60, 0.75, 0.59, and 0.28 among junior high school students, senior high school students, college students, and elderly adults, respectively. The results of the nonparametric bootstrap procedure revealed that most comparisons among edge weights and node strength were statistically significant (Figs. S4, S5). Additionally, bootstrapped 95 % of CIs were narrow, representing edges that were trustworthy (Fig. S3).
Fig. 3.
The x-axis indicates the percentage of cases of the original sample included at each step. The y-axis indicates the average of correlations between the centrality indices from the original network and the centrality indices from the networks that were re-estimated after excluding increasing percentages of cases. A for junior high school students. B for senior high school students. C for college students. D for elderly adults.
3.4. Network comparison among junior high school students, senior high school students, college students and elderly
NCT revealed the network structure invariance and global strength invariance among the four groups (see Table 2 ).
Table 2.
Internetwork similarity indexes and network comparison tests across four groups.
| Comparison | Edge weights similarity | Strength similarity | Predictability similarity | Global strength invariance | Network structure invariance |
|---|---|---|---|---|---|
| JH - SH | rs = 0.882⁎⁎ | rs = 0.817⁎ | rs = 0.850⁎⁎ | p = 0.003 | p = 0.398 |
| JH - College | rs = 0.816⁎⁎ | rs = 0.783⁎ | rs = 0.783⁎ | p = 0.086 | p = 0.082 |
| JH - Elderly | rs = 0.599⁎⁎ | rs = 0.750⁎ | rs = 0.583 | p = 0.017 | p = 0.005 |
| SH - College | rs = 0.784⁎⁎ | rs = 0.850⁎⁎ | rs = 0.767⁎ | p = 0.000 | p = 0.744 |
| SH - Elderly | rs = 0.555⁎⁎ | rs = 0.733⁎ | rs = 0.233 | p = 0.086 | p = 0.000 |
| College - Elderly | rs = 0.621⁎⁎ | rs = 0.517 | rs = 0.417 | p = 0.000 | p = 0.038 |
Note. JH, Junior high school students. SH, Senior high school students. Spearman correlations (rs) were computed; p-values were adjusted for Bonferroni-Holm correction.
p < 0.050.
p < 0.010.
Specifically, there was a significant group difference in network global strength among junior high school students - senior high school students (3.19 vs. 3.50, global strength difference (S = 0.31, p = 0.003)), junior high school students- elderly (3.19 vs. 3.86, S = 0.66, p = 0.017), senior high school students – college students (3.50 vs. 2.92, S = 0.58, p = 0.000), college students – elderly (2.92 vs. 3.86, S = 1.37, p = 0.000). Junior high school, senior high school, and college students' networks, in terms of their network structure, were substantially different from those of elderly adults (M = 0.23, p = 0.005, M = 0.28, p = 0.000, and M = 0.21, p = 0.038, respectively). In combination, these findings suggested that networks' global connectivity was ultimately inconsistent, but structures remained roughly intact.
4. Discussion
To our knowledge, this is the first study to systematically investigate depressive symptoms among junior high school students, senior high school students, college students, and elderly adults during the COVID-19 pandemic lockdown in China. Several findings are worth discussing.
Sad mood was the most central symptom of students' depression networks, which was consistent with a previous study (Beard et al., 2016), and the inclusion of sadness as a prerequisite for major depressive disorder in the clinical diagnosis (Bernstein et al., 2007). The COVID-19 pandemic is unprecedented for everyone, especially for students. Students had to take online courses, had to stay at home or alone, and were forced to overcome a multitude of learning and relationship challenges at a phase when they were supposed to construct and maintain peer relationships in real life (Wu et al., 2022). Without catharsis, students' feelings of gloominess accumulated into depression (Lee and Jeong, 2018). One point to emphasize is that sad mood is the hallmark symptom needed to meet a diagnosis of major depression (Fried et al., 2016). Fortunately, Tao et al. (2022) have revealed through network analysis that the level of hopelessness among college students is significantly reduced once the lockdown ending. Therefore, to intervene in depression development, parents or communities need to understand the situation of students in the lockdown period and address their distorted perceptions.
Moreover, from the elderly adults' network, we found that Guilt was the most central symptom. An investigation of Hong Kong adult residents' depressive symptom network revealed the same phenomenon as ours (Cheung et al., 2021). Guilt is a negative evaluation of one's own behavior (Cândea and Szentagotai-Tătar, 2018), which is closely associated with self-blame (Peterson et al., 1981), worthlessness (Zahn et al., 2015), low self-esteem (Battle, 1978), and hopelessness (Abramson et al., 1989). A previous study stated that guilt levels were positively associated with depression (Li et al., 2018). During the lockdown period, elderly adults paused their activities, such as purchasing food for the family or seeing doctors. Instead, they had to depend heavily on their family members or communities. In this situation, it is easy for elders to feel that they are useless or even a burden to their surroundings. Losing body control or getting sick could further intensify guilty feelings (Pedroso-Chaparro et al., 2021). Hence, we believe that if communities or families can offer elderly adults chances to regain control of their bodies and lives, their depressive symptoms will be alleviated.
Another finding that should not be overlooked is senior high school students' Suicide Ideation, the second most central symptom in their depression networks. Until now, no studies have revealed this result. As we applied optimal cutoff scores to screen for those who were likely to have depression, suicide ideation was a prominent symptom in depressed senior high school students. In terms of the escape theory of suicide (Baumeister, 1990), suicide ideation is a motivation to eliminate acrimonious self-evaluation and internal inadequacies. Senior high school students are under tremendous academic pressure to prepare for the competitive college entrance examinations (named “Gaokao”) that decide whether students can enter a key university, and the magnitude of this pressure exceeds that felt by other students (Zhang et al., 2019). During the lockdown period, however, the shift to online learning made it difficult to guarantee the efficacy of teaching, which in turn led to a decline in students' learning efficiency or academic achievements (Wang and Yu, 2021). Once one's or parents' expectations are not met (Liu and Tein, 2005), these students tend to attribute these failures internally (Baumeister, 1990). Consequently, these continuous aversive assessments gradually led to depression (Unger et al., 2001), and made them have a relatively high prevalence of suicide plans or attempts (Anderson et al., 2015). More seriously, senior high school students might rely on the ultimate step, suicide, to escape from agony (Cao et al., 2022; Hou et al., 2020). In recent years, China has launched several hotlines to prevent suicides. If a student is found to have suicidal ideation or attempts, people can call a hotline or seek a professional psychotherapist for help.
In addition, the results showed that the symptom-to-symptom relationship differed across groups. Specifically, the strongest correlations were found between Guilt - Suicide Ideation, Anhedonia - Energy, and Anhedonia - Sad Mood in junior high school students, senior high students and college students, respectively. These findings were partly similar to a previous study performed in the United States, suggesting that the strongest edge was between ‘Sad Mood' and ‘Anhedonia’ (Beard et al., 2016). Adolescence is a dynamic period of life characterized by marked changes in physical maturation, drive for independence, and increased salience of social and peer interactions (Whittle et al., 2016). Increased self-consciousness during adolescence results in an increase in the frequency and intensity of the experience of negative emotions such as guilt and shame (Zeman et al., 2006). However, poor emotion regulation ability in adolescents makes them prone to risky behavior, such as nonsuicidal self-injury or even suicide (Brausch et al., 2022). Hence, in the present study, the strongest correlation was between guilt and suicide ideation in junior high school students. With increasing age, individuals' cognition maturation is further developed, and hence, the improvement of cognitive reappraisal strategies (changing the meaning of a stimulus to alter its emotional impact) leads to less impulsive actions (Cardi et al., 2021). On the other hand, COVID-19 lockdown measures may be especially difficult for adolescents given the particular importance of peer interaction during this period of life (Skumlien et al., 2021). Students were prevented from engaging in many activities, including social, professional and physical activities (Martines et al., 2021), which restricted interaction with environmental rewards and then contributed to psychological symptoms such as anhedonia (Wieman et al., 2022). Senior high school students were unable to release their pressure through exercise as before (Shepherd et al., 2021), while college students may have been sad about the economic recession and increased unemployment (Nicola et al., 2020), making them lose their passion for imagining the future like before (Duplaga and Grysztar, 2021; Li et al., 2021). Taken together, the strongest symptom-to-symptom relationship varied among these different groups.
For the elderly, Sleep was most strongly associated with energy. First, the prevalence of sleep-related disorders usually increases with age, including obstructive sleep apnea (especially for males aged over 60) and insomnia (Pires et al., 2021). Social isolation, home confinement, anxiety, fear of getting infected and stress during the COVID-19 pandemic period can further damage the sleep quality of the elderly (De Mello et al., 2020; Xue et al., 2020). Furthermore, energy refers to the feeling of unwillingness or incompetence to complete physical and mental activities (O'Connor, 2004). Moreover, in the lockdown period, elderly adults had to stay at home without gaining access to entertainment facilities. A study has shown that a lack of regular exercise can cause fatigue (Wielopolski et al., 2015), which may further develop into sedentariness and lead to depression (Kandola et al., 2019). From this perspective, it is important to improve people's level of physical activity at home during the pandemic to lower the likelihood of depression. Alternatively, duloxetine is prevalent in helping depressed patients regain energy (Harada et al., 2015).
4.1. Limitation
Several limitations should be mentioned in the current study. We performed a cross-sectional study during the COVID-19 lockdown period. Long-term changes in networks should be investigated in further research. Second, based on adults' depressive symptom networks (Cheung et al., 2021), we performed further research on students and elderly adults. However, we could not merge the previous data with that obtained in our study, although we mentioned that socioeconomic factors might impact depression development. In further research, more factors should be taken into account (Hou et al., 2021).
5. Conclusion
In summary, for four age group networks, Sad Mood, Energy, Guilt and Suicide Ideation were highly associated with depression. Furthermore, Sad Mood was the most central symptom among junior high school students, senior high school students, and college students, while Guilt was the most central symptom among elderly adults. Suicide Ideation and Anhedonia were two unique symptoms in senior high school students' and college students' networks, respectively.
Moreover, NCT suggested that the network's global connectivity was ultimately inconsistent, but the network structure remained roughly intact. These findings provide an empirical investigation into depressive symptoms that may occur in different groups during lockdowns in China. Our results may shed some light on depression treatment.
Funding statement
No funding.
Ethics statement
The study was approved by Beijing Normal University Institutional Review Board (202112220084).
CRediT authorship contribution statement
Yanqiang Tao took the lead in writing the manuscript.
Liang Zhang and Xiangping Liu conceived the study design and supervised the data collection.
Yanqiang Tao and Zijuan Ma performed the data analysis.
Wenxin Hou, Haiqun Niu, Shujian Wang, and Zeqing Zheng provided critical feedback and helped shape the research, analysis, and manuscript.
Conflict of interest
The authors declare no conflicts of interest.
Acknowledgement
This study thanks Qiubai Li, a member of the political and legal Committee of Xiangfang district in Harbin.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jad.2022.12.120.
Appendix A. Supplementary data
Supplementary material for all results mentioned in the article.
Data availability
Data are available upon request from the first author.
References
- Abdul Karim M., Ouanes S., Reagu S.M., Alabdulla M. Network analysis of anxiety and depressive symptoms among quarantined individuals: cross-sectional study. BJPsych Open. 2021;7(6) doi: 10.1192/bjo.2021.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abramson L.Y., Metalsky G.I., Alloy L.B. Hopelessness depression: a theory-based subtype of depression. Psychol. Rev. 1989;96(2):358–372. doi: 10.1037/0033-295X.96.2.358. [DOI] [Google Scholar]
- Altshuler L.L., Post R.M., Black D.O., Keck P.E., Nolen W.A., Frye M.A., Suppes T., Grunze H., Kupka R.W., Leverich G.S., McElroy S.L., Walden J., Mintz J. Subsyndromal depressive symptoms are associated with functional impairment in patients with bipolar disorder: results of a large, multisite study. J. Clin. Psychiatry. 2006;67(10):1551–1560. doi: 10.4088/jcp.v67n1009. [DOI] [PubMed] [Google Scholar]
- Amicucci G., Salfi F., D’Atri A., Viselli L., Ferrara M. The differential impact of COVID-19 lockdown on sleep quality, insomnia, depression, stress, and anxiety among late adolescents and elderly in Italy. Brain Sci. 2021;11(10):1336. doi: 10.3390/brainsci11101336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. 2013. p. 21. [DOI] [Google Scholar]
- Anderson, Lowry L.S., Wuensch K.L. Racial differences in adolescents' answering questions about suicide. Death Stud. 2015;39(10):600–604. doi: 10.1080/07481187.2015.1047058. [DOI] [PubMed] [Google Scholar]
- Balázs J., Miklósi M., Keresztény Á., Hoven C.W., Carli V., Wasserman C., Apter A., Bobes J., Brunner R., Cosman D. Adolescent subthreshold-depression and anxiety: psychopathology, functional impairment and increased suicide risk. J. Child Psychol. Psychiatry. 2013;54(6):670–677. doi: 10.1111/jcpp.12016. [DOI] [PubMed] [Google Scholar]
- Battle J. Relationship between self-esteem and depression. Psychol. Rep. 1978;42(3):745–746. doi: 10.2466/pr0.1978.42.3.745. [DOI] [PubMed] [Google Scholar]
- Baumeister R.F. Suicide as escape from self. Psychol. Rev. 1990;97(1):90–113. doi: 10.1037/0033-295x.97.1.90. [DOI] [PubMed] [Google Scholar]
- Brausch A.M., Clapham R.B., Littlefield A.K. Identifying specific emotion regulation deficits that associate with nonsuicidal self-injury and suicide ideation in adolescents. J. Youth Adolesc. 2022;51(3):556–569. doi: 10.1007/s10964-021-01525-w. 556-569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard C., Millner A.J., Forgeard M.J., Fried E.I., Hsu K.J., Treadway M., Leonard C.V., Kertz S., Björgvinsson T. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychol. Med. 2016;46(16):3359–3369. doi: 10.1017/S0033291716002300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein I.H., Rush A.J., Carmody T.J., Woo A., Trivedi M.H. Clinical vs. self-report versions of the quick inventory of depressive symptomatology in a public sector sample. J. Psychiatr. Res. 2007;41(3–4):239–246. doi: 10.1016/j.jpsychires.2006.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertha E.A., Balázs J. Subthreshold depression in adolescence: a systematic review. Eur. Child Adolesc. Psychiatry. 2013;22(10):589–603. doi: 10.1016/j.jad.2013.06.010. [DOI] [PubMed] [Google Scholar]
- Borsboom D., Cramer A.O. Network analysis: an integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Bringmann L., Elmer T., Epskamp S., Krause R., Schoch D., Wichers M., Wigman J., Snippe E. What do centrality measures measure in psychological networks? J. Abnorm. Psychol. 2019;128(8):892–903. doi: 10.1037/abn0000446. [DOI] [PubMed] [Google Scholar]
- Bromet E., Andrade L.H., Hwang I., Sampson N.A., Alonso J., de Girolamo G., de Graaf R., Demyttenaere K., Hu C., Iwata N., Karam A.N., Kaur J., Kostyuchenko S., Lépine J.-P., Levinson D., Matschinger H., Mora M.E.M., Browne M.O., Posada-Villa J., Viana M.C., Williams D.R., Kessler R.C. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011;9(1) doi: 10.1186/1741-7015-9-90. 90-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cândea D.-M., Szentagotai-Tătar A. Shame-proneness, guilt-proneness and anxiety symptoms: a meta-analysis. J. Anxiety Disord. 2018;58:78–106. doi: 10.1016/j.janxdis.2018.07.005. [DOI] [PubMed] [Google Scholar]
- Cao C., Wang L., Fang R., Liu P., Bi Y., Luo S., Grace E., Olff M. Anxiety, depression, and PTSD symptoms among high school students in China in response to the COVID-19 pandemic and lockdown. J. Affect. Disord. 2022;296:126–129. doi: 10.1016/j.jad.2021.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardi V., Albano G., Gentili C., Sudulich L. The impact of emotion regulation and mental health difficulties on health behaviours during COVID19. J. Psychiatr. Res. 2021;143:409–415. doi: 10.1016/j.jpsychires.2021.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen I.-P., Liu S.-I., Huang H.-C., Sun F.-J., Huang C.-R., Sung M.-R., Huang Y.-P. Validation of the patient health questionnaire for depression screening among the elderly patients in Taiwan. Int. J. Gerontol. 2016;10(4):193–197. doi: 10.1016/j.ijge.2016.05.002. [DOI] [Google Scholar]
- Cheung T., Jin Y., Lam S.C., Zhaohui S., Hall B., Xiang Y.-T., Suen L., Chan S., Ho H.S.W., Lam K.B.H., Huang E., Xiao Y., Pereira-Ávila F., Gir E., Yildirim M., Seren Intepeler S., Lantta T., Kyungmi L., Shin N., Fong T. Network analysis of depressive symptoms in Hong Kong residents during the COVID-19 pandemic. Transl. Psychiatry. 2021;11(1):1–8. doi: 10.1038/s41398-021-01543-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costantini G., Perugini M. A framework for testing causality in personality research. Eur. J. Personal. 2018;32(3):254–268. doi: 10.1002/per.2150. [DOI] [Google Scholar]
- Dalege J., Borsboom D., Van Harreveld F., Van den Berg H., Conner M., Van der Maas H.L. Toward a formalized account of attitudes: the causal attitude network (CAN) model. Psychol. Rev. 2016;123(1):2–22. doi: 10.1037/a0039802. [DOI] [PubMed] [Google Scholar]
- De Mello M.T., Silva A., Guerreiro R.C., da-Silva F.R., Esteves A.M., Poyares D. Sleep and COVID-19: considerations about immunity, pathophysiology, and treatment. Sleep Sci. 2020;13(3):199–209. doi: 10.5935/1984-0063.20200062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duplaga M., Grysztar M. The association between future anxiety, health literacy and the perception of the COVID-19 pandemic: a cross-sectional study. Healthcare. 2021;9(1):1–18. doi: 10.3390/healthcare9010043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S., Borsboom D., Fried E.I. Estimating psychological networks and their accuracy: a tutorial paper. Behav. Res. Methods. 2018;50(1):195–212. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S., Cramer A.O., Waldorp L.J., Schmittmann V.D., Borsboom D. Qgraph: network visualizations of relationships in psychometric data. J. Stat. Softw. 2012;48(4):1–18. doi: 10.18637/jss.v048.i04. [DOI] [Google Scholar]
- Epskamp S., Fried E.I. A tutorial on regularized partial correlation networks. Psychol. Methods. 2018;23(4):617–634. doi: 10.1037/met0000167. [DOI] [PubMed] [Google Scholar]
- Epskamp S., Rhemtulla M., Borsboom D. Generalized network psychometrics: combining network and latent variable models. Psychometrika. 2016;82:904–927. doi: 10.1007/s11336-017-9557-x. [DOI] [PubMed] [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2021;8(2):141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson D.M., Horwood L.J., Ridder E.M., Beautrais A.L. Subthreshold depression in adolescence and mental health outcomes in adulthood. Arch. Gen. Psychiatry. 2005;62(1):66–72. doi: 10.1001/archpsyc.62.1.66. [DOI] [PubMed] [Google Scholar]
- Fried E.I. Problematic assumptions have slowed down depression research: why symptoms, not syndromes are the way forward. Front. Psychol. 2015;6 doi: 10.3389/fpsyg.2015.00309. 309-309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried E.I., Epskamp S., Nesse R.M., Tuerlinckx F., Borsboom D. What are 'good' depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. J. Affect. Disord. 2016;189:314–320. doi: 10.1016/j.jad.2015.09.005. [DOI] [PubMed] [Google Scholar]
- Gijzen M.W.M., Rasing S.P.A., Creemers D.H.M., Smit F., Engels R., De Beurs D. Suicide ideation as a symptom of adolescent depression. A network analysis. J. Affect. Disord. 2021;278:68–77. doi: 10.1016/j.jad.2020.09.029. [DOI] [PubMed] [Google Scholar]
- Harada E., Kato M., Fujikoshi S., Wohlreich M., Berggren L., Tokuoka H. Changes in energy during treatment of depression: an analysis of duloxetine in double-blind placebo-controlled trials. Int. J. Clin. Pract. 2015;69(10):1139–1148. doi: 10.1111/ijcp.12658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslbeck J., Waldorp L. Mgm: estimating time-varying mixed graphical models in high-dimensional data. J. Stat. Softw. 2020;93(8):1–46. doi: 10.18637/jss.v093.i08. [DOI] [Google Scholar]
- Haslbeck J.M.B., Waldorp L.J. How well do network models predict observations? On the importance of predictability in network models. Behav. Res. Methods. 2018;50(2):853–861. doi: 10.3758/s13428-017-0910-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou T.-Y., Mao X.-F., Dong W., Cai W.-P., Deng G.-H. Prevalence of and factors associated with mental health problems and suicidality among senior high school students in rural China during the COVID-19 outbreak. Asian J. Psychiatr. 2020;54 doi: 10.1016/j.ajp.2020.102305. 102305-102305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou W.K., Hall B.J., Liang L., Li T.W., Liu H., Galea S. Probable depression and suicidal ideation in Hong Kong amid massive civil unrest. Ann. Epidemiol. 2021;54:45–51. doi: 10.1016/j.annepidem.2020.09.006. [DOI] [PubMed] [Google Scholar]
- Jin H., Li B., Jakovljevic M. How China controls the Covid-19 epidemic through public health expenditure and policy? J. Med. Econ. 2022:1–23. doi: 10.1080/13696998.2022.2054202. [DOI] [PubMed] [Google Scholar]
- Jones P. networktools: tools for identifying important nodes in networks. R package version 1.3.0. 2021. https://CRAN.R-project.org/package=networktools
- Kandola A., Ashdown-Franks G., Hendrikse J., Sabiston C.M., Stubbs B. Physical activity and depression: towards understanding the antidepressant mechanisms of physical activity. Neurosci. Biobehav. Rev. 2019;107:525–539. doi: 10.1016/j.neubiorev.2019.09.040. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H.R., Jeong E.J. Do therapeutic interventions exist in online games? Effects of therapeutic catharsis, online game self-efficacy, and life self-efficacy on depression, loneliness, and aggression. Int. J. Contents. 2018;14(1):12–17. doi: 10.5392/IJOC.2018.14.1.012. [DOI] [Google Scholar]
- Li J., Tendeiro J., Stroebe M.S. Guilt in bereavement: its relationship with complicated grief and depression. Int. J. Psychol. 2018;54(4):454–461. doi: 10.1002/ijop.12483. [DOI] [PubMed] [Google Scholar]
- Li, Zhao J., Ma Z., McReynolds L.S., Lin D., Chen Z., Wang T., Wang D., Zhang Y., Zhang J., Fan F., Liu X. Mental health among college students during the COVID-19 pandemic in China: a 2-wave longitudinal survey. J. Affect. Disord. 2021.;281:597–604. doi: 10.1016/j.jad.2020.11.109. [DOI] [PubMed] [Google Scholar]
- Liu X., Tein J.Y. Life events, psychopathology, and suicidal behavior in chinese adolescents. J. Affect. Disord. 2005;86(2–3):195–203. doi: 10.1016/j.jad.2005.01.016. [DOI] [PubMed] [Google Scholar]
- Lorant V., Deliège D., Eaton W., Robert A., Philippot P., Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am. J. Epidemiol. 2003;157(2):98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Löwe B., Kroenke K., Herzog W., Gräfe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the patient health questionnaire (PHQ-9) J. Affect. Disord. 2004;81(1):61–66. doi: 10.1016/S0165-0327(03)00198-8. [DOI] [PubMed] [Google Scholar]
- Luo W., Zhong B.-L., Chiu H.F.-K. Prevalence of depressive symptoms among Chinese university students amid the COVID-19 pandemic: a systematic review and meta-analysis. Epidemiol. Psychiatr. Sci. 2021;30:e31–e50. doi: 10.1017/S2045796021000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malhi G.S., Mann J.J. Depression. Lancet (Br. Ed.) 2018;392:2299–2312. doi: 10.1016/S0140-6736(18)31948-2. [DOI] [PubMed] [Google Scholar]
- Manea L., Gilbody S., McMillan D. Optimal cutoff score for diagnosing depression with the patient health questionnaire (PHQ-9): a meta-analysis. Can. Med. Assoc. J. 2012;184(3):E191–E196. doi: 10.1503/cmaj.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martines F.R.V., Toppa R.H., Assunção L.M., Desjardins M.R., Delmelle E.M. Detecting space–time clusters of COVID-19 in Brazil: mortality, inequality, socioeconomic vulnerability, and the relative risk of the disease in Brazilian municipalities. J. Geogr. Syst. 2021;23(1):7–36. doi: 10.1007/s10109-020-00344-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt T.E., Caspi A., Taylor A., Kokaua J., Milne B.J., Polanczyk G., Poulton R. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol. Med. 2010;40(6):899–909. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullarkey M.C., Marchetti I., Beevers C.G. Using network analysis to identify central symptoms of adolescent depression. J. Clin. Child Adolesc. Psychol. 2019;48(4):656–668. doi: 10.1080/15374416.2018.1437735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C., Agha R.… The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int. J. Surg. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor P.J. Evaluation of four highly cited energy and fatigue mood measures. J. Psychosom. Res. 2004;57(5):435–441. doi: 10.1016/j.jpsychores.2003.12.006. [DOI] [PubMed] [Google Scholar]
- Paunio T., Korhonen T., Hublin C., Partinen M., Koskenvuo K., Koskenvuo M., Kaprio J. Poor sleep predicts symptoms of depression and disability retirement due to depression. J. Affect. Disord. 2015;172:381–389. doi: 10.1016/j.jad.2014.10.002. [DOI] [PubMed] [Google Scholar]
- Pedroso-Chaparro M.D.S., Márquez-González M., Vara-García C., Cabrera I., Romero-Moreno R., Barrera-Caballero S., Losada A. Guilt for perceiving oneself as a burden in healthy older adults. Associated factors. Aging Ment. Health. 2021;25(12):2330–2336. doi: 10.1080/13607863.2020.1822291. [DOI] [PubMed] [Google Scholar]
- Peterson C., Schwartz S.M., Seligman M.E. Self-blame and depressive symptoms. J. Pers. Soc. Psychol. 1981;41(2):253–259. doi: 10.1037/0022-3514.41.2.253. [DOI] [PubMed] [Google Scholar]
- Pires G.N., Ishikura I.A., Xavier S.D., Petrella C., Piovezan R.D., Xerfan E.M.S., Tufik S.… Sleep in older adults and its possible relations with COVID-19. Front. Aging Neurosci. 2021;13 doi: 10.3389/fnagi.2021.647875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robb C.E., de Jager C.A., Ahmadi-Abhari S., Giannakopoulou P., Udeh-Momoh C., McKeand J., Price G., Car J., Majeed A., Ward H. Associations of social isolation with anxiety and depression during the early COVID-19 pandemic: a survey of older adults in London, UK. Front Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.591120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmittmann V.D., Cramer A.O., Waldorp L.J., Epskamp S., Kievit R.A., Borsboom D. Deconstructing the construct: a network perspective on psychological phenomena. New Ideas Psychol. 2013;31(1):43–53. doi: 10.1016/j.newideapsych.2011.02.007. [DOI] [Google Scholar]
- Skumlien M., Langley C., Lawn W., Voon V., Sahakian B.J. Apathy and anhedonia in adult and adolescent cannabis users and controls before and during the COVID-19 pandemic lockdown. Int. J. Neuropsychopharmacol. 2021;24(11):859–866. doi: 10.1093/ijnp/pyab033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepherd, Evans T., Gupta S., McDonough M.H., Doyle-Baker P., Belton K.L., Karmali S., Pawer S., Hadly G., Pike I., Adams S.A., Babul S., Yeates K.O., Kopala-Sibley D.C., Schneider K.J., Cowle S., Fuselli P., Emery C.A., Black A.M. The impact of COVID-19 on high school student-athlete experiences with physical activity, mental health, and social connection. Int. J. Environ. Res. Public Health. 2021;18(7):3515. doi: 10.3390/ijerph18073515. (1-14) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao Y., Niu H., Hou W., Zhang L., Ying R. Hopelessness during and after the COVID-19 pandemic lockdown among chinese college students: a longitudinal network analysis. J. Clin. Psychol. 2022:1–14. doi: 10.1002/jclp.23439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; 2021. R: a language and environment for statistical computing.https://www.r-project.org/ [Google Scholar]
- Unger J.B.L.Y., Johnson C.A., Gong J., Chen X., Li C. Stressful life events among adolescents in Wuhan, China. Int. J. Behav. Med. 2001;8:1–18. doi: 10.1207/S15327558IJBM0801_01. [DOI] [Google Scholar]
- Valente T.W. Network interventions. Science. 2012;337(6090):49–53. doi: 10.1126/science.1217330. [DOI] [PubMed] [Google Scholar]
- van Borkulo C., van Bork R., Boschloo L., Kossakowski J., Tio P., Schoevers R., Borsboom D., Waldorp L. Comparing network structures on three aspects: a permutation test. Psychol. Methods. 2021 doi: 10.1037/met0000476. [DOI] [PubMed] [Google Scholar]
- Wang W., Bian Q., Zhao Y., Li X., Wang W., Du J., Zhang G., Zhou Q., Zhao M. Reliability and validity of the chinese version of the patient health questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry. 2014;36(5):539–544. doi: 10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- Wang X., Hegde S., Son C., Keller B., Smith A., Sasangohar F. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J. Med. Internet Res. 2020;22(9) doi: 10.2196/22817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Yu N. Education data-driven online course optimization mechanism for college student. Mob. Inf. Syst. 2021;2021 doi: 10.1155/2021/5545621. [DOI] [Google Scholar]
- Whittle S., Liu K., Bastin C., Harrison B.J., Davey C.G. Neurodevelopmental correlates of proneness to guilt and shame in adolescence and early adulthood. Dev. Cogn. Neurosci. 2016;19(C):51–57. doi: 10.1016/j.dcn.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wieman S.T., Fields J.S., Arditte Hall K.A., MacDonald H.Z., Liverant G.I. Effects of the COVID-19 pandemic on anhedonia, reward exposure and responsiveness, and sleep in college students. J. Am. Coll. Heal. 2022;1–5 doi: 10.1080/07448481.2022.2047705. [DOI] [PubMed] [Google Scholar]
- Wielopolski J., Reich K., Clepce M., Fischer M., Sperling W., Kornhuber J., Thuerauf N. Physical activity and energy expenditure during depressive episodes of major depression [Article] J. Affect. Disord. 2015;174:310–316. doi: 10.1016/j.jad.2014.11.060. [DOI] [PubMed] [Google Scholar]
- World Health Organization Depression and other common mental disorders, global health estimates. 2017. http://apps.who.int/iris/bitstream/10665/254610/1/WHO-MSD
- Wu Y., Yin G., Zhang Y. Experience and perceptions of chinese university students regarding the COVID-19 pandemic: a qualitative analysis. Front. Public Health. 2022;10 doi: 10.3389/fpubh.2022.872847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue Z., Lin L., Zhang S., Gong J., Liu J., Lu J. Sleep problems and medical isolation during the SARS-CoV-2 outbreak. Sleep Med. 2020;70:112–115. doi: 10.1016/j.sleep.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahn R., Lythe K.E., Gethin J.A., Green S., Deakin J.F.W., Young A.H., Moll J. The role of self-blame and worthlessness in the psychopathology of major depressive disorder. J. Affect. Disord. 2015;186:337–341. doi: 10.1016/j.jad.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeman J., Cassano M., Perry-Parrish C., Stegall S. Emotion regulation in children and adolescents. J. Dev. Behav. Pediatr. 2006;27(2):155–168. doi: 10.1097/00004703-200604000-00014. [DOI] [PubMed] [Google Scholar]
- Zhang Y.Y., Lei Y.T., Song Y., Lu R.R., Duan J.L., Prochaska J.J. Gender differences in suicidal ideation and health-risk behaviors among high school students in Beijing, China. J. Glob. Health. 2019;9(1) doi: 10.7189/jogh.09.010604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y.L., Liang W., Chen Z.M., Zhang H.M., Zhang J.H., Weng X.Q., Yang S.C., Zhang L., Shen L.J., Zhang Y.L. Validity and reliability of patient health Questionnaire-9 and patient health Questionnaire-2 to screen for depression among college students in China. Asia Pac. Psychiatry. 2013;5(4):268–275. doi: 10.1111/appy.12103. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material for all results mentioned in the article.
Data Availability Statement
Data are available upon request from the first author.