PURPOSE:
Financial hardship is a growing concern for patients with cancer. Patients with head and neck cancer (HNC) are particularly vulnerable, given that a third leave the workforce following treatment. The goal of our study was to characterize financial hardship in the psychologic response (response to increased expenses) and coping behaviors (behaviors patients adopt to manage their care in the setting of increased expenses) domains in patients with HNC compared with patients with other cancers.
METHODS:
This was a retrospective cohort study of nationally representative public survey data from 2013 to 2018 in the National Health Interviews Survey, an annual cross-sectional household survey. We included respondents age ≥ 18 years who reported a diagnosis of cancer and identified a subset of patients with HNC. Our main outcomes were financial hardship in the psychologic response and coping behaviors domains.
RESULTS:
Our sample included a weighted population of 357,052 patients with HNC and 21.4 million patients with other cancers. Compared with patients with other cancers, patients with HNC reported greater levels of coping behaviors hardship (31% v 23%, P = .015), but similar levels of psychologic financial hardship (73% v 72%, P = .787). Medicaid or uninsured patients more often reported coping behaviors hardship. On multivariable analysis, HNC (odds ratio, 1.51; 95% CI, 1.01 to 2.24) was independently associated with coping behaviors hardship.
CONCLUSION:
To our knowledge, this is the first study to evaluate financial hardship in patients with HNC compared with patients with other cancers that includes Medicaid and uninsured patients, who are more often to have financial hardship. Patients with HNC have greater levels of hardship in the coping behaviors domain compared with patients with other cancers, but similar levels in the psychologic response domain.
INTRODUCTION
Financial hardship is the excess financial strain a patient has as the result of a cancer diagnosis.1 Financial hardship in cancer survivors can be conceptualized in three domains: (1) the material conditions that emerge because of increased expenses and lowered income, (2) the psychologic response to the increased expenses, and (3) the coping behaviors patients adopt to manage their care in the setting of increased expenses.2 Financial hardship among patients with cancer is projected to rise because of the improved survival of these patients, increased utilization of expensive novel cancer therapies, and higher insurance premiums, deductibles, and copayments in the current health care system.3 Among patients with head and neck cancer (HNC), financial hardship has been associated with decreased quality of life, decreased treatment adherence, worse disease outcomes, and lower satisfaction with cancer care.3-6
The demographic and clinical features of patients with HNC may make them particularly vulnerable to financial hardship. Patients with HNC are disproportionately of lower socioeconomic status and have lower levels of education compared with patients with other cancers.7-9 Management of HNC furthermore consists of expensive multimodality therapy (radical surgery, radiotherapy, and chemotherapy) and support from ancillary providers, including speech therapists, dieticians, dentists, oral surgeons, supportive medicine physicians, and others, resulting in costs of care totaling upward of $100,000 US dollars (USD) per case, making it among the most costly cancers to treat in the United States.10 Moreover, given that HNC treatment can directly affect speaking and eating, may require numerous in-person visits totaling many hours per week, and often necessitates opioid use for pain management, continuing to work is often not feasible. In fact, up to a third of patients do not return to the workforce after treatment.11
Apart from financial analyses of claims data, treatment costs, or medical expenditures,9,10,12-14 prior studies on financial hardship in HNC have focused on patients' cost-coping strategies15 or caregiver distress.16 Only three studies have examined patient-reported financial hardship using validated measures, and all studies were limited to insured patients.4,17,18 Although one study has compared medical expenditures in patients with HNC to patients with other cancers,9 no study has examined potential differences in financial hardship within the psychologic response and coping behaviors domains. Through a retrospective review of nationally representative public survey data, our goal was to evaluate financial hardship in these two domains in patients with HNC compared with patients with other cancers.
METHODS
Data Source and Study Participants
We conducted a retrospective study using the National Health Interview Study (NHIS) data from 2013 to 2018. The NHIS is a Centers for Disease Control and Prevention–sponsored annual cross-sectional household survey with face-to-face interviews and a response rate of more than 70% of eligible households.19 The sample design uses a multistage area probability design, which accounts for nonresponse and allows for national representative sampling, including under-represented groups. The data are deidentified, so this study was exempt from review by the University of Michigan's Institutional Review Board. We followed the Strengthening the Reporting of Observational Studies in Epidemiology reporting guidelines.
Our study included respondents age 18 years and older with a self-reported diagnosis of cancer by answering yes to the following survey question: Have you ever been told by a doctor or other health professional that you had cancer or malignancy of any kind? Of these patients with cancer, we identified a subset of patients with HNC who reported having larynx, mouth, tongue, lip, throat, or pharyngeal cancers. The malignancies included in the all other cancers group included skin (nonmelanoma and unknown skin), breast, genitourinary (prostate, bladder, renal, and testicular), gynecologic (ovarian, uterine, and cervical), gastrointestinal (colorectal, esophageal, stomach, gallbladder, pancreas, and liver), melanoma, hematologic (leukemia, lymphoma, and blood), thyroid, lung, other, and those with multiple cancers.
Study Variables
The baseline variables included sex, marital status, age, race, insurance, income, federal poverty level (FPL), and region. Marital status was grouped into married/living together, widowed/divorced/separated, and never married. Age was categorized into 18-50, 51-64, 65-84, and ≥ 85 years and also evaluated as a continuous variable. Race was classified as White, Black, and Other. Insurance status was categorized as private, Medicaid, Medicare, other state, and other/uninsured. Total combined family income was grouped into $0-$34,999 USD, $35,000-$74,999 USD, $75,000-$99,999 USD, and ≥ $100,000 USD. Family income as a percent of the federal poverty limit from the Census Bureau was classified as < 100%, 100%-199%, 200%-399%, and ≥ 400%. Geographic regions included the Northeast, Midwest, South, and West.
Study Outcomes
Our main outcomes were financial hardship in the psychologic response and coping behaviors domains. Psychologic financial hardship was defined by any evidence of worry about paying medical bills, paying medical costs of a serious illness/accident, not being able to pay medical costs for normal health care, maintaining one's current standard of living, having money for retirement, paying monthly bills, and paying for housing costs (Appendix Table A1, online only). Patients without psychologic financial hardship expressed no worry about any of these factors. Financial hardship in the coping behaviors domain was defined by responding yes to problems paying or unable to pay any medical bills or to needing prescription medications, dental, mental health, or vision services but being unable to afford them.
Statistical Analysis
Baseline characteristics were compared using chi-squared tests, and weighted totals and weighted proportions were reported. Financial hardship in the psychologic response and coping behaviors domains were compared between patients with HNC and patients with other cancers. Univariable and multivariable logistic regression was used to evaluate the relationship between demographic, socioeconomic, and clinical variables and financial hardship. Statistical significance was defined as a two-sided P < .05. Analysis was performed using STATA version 16.1 (StataCorp LLC, College Station, TX). The person weights and variance estimates were used with Stata's svy function to account for the NHIS's complex survey design to achieve nationally representative results. All person weights were pooled and divided by the number of years studied in accordance with NHIS guidelines, given that multiple years of data were aggregated for analysis.
RESULTS
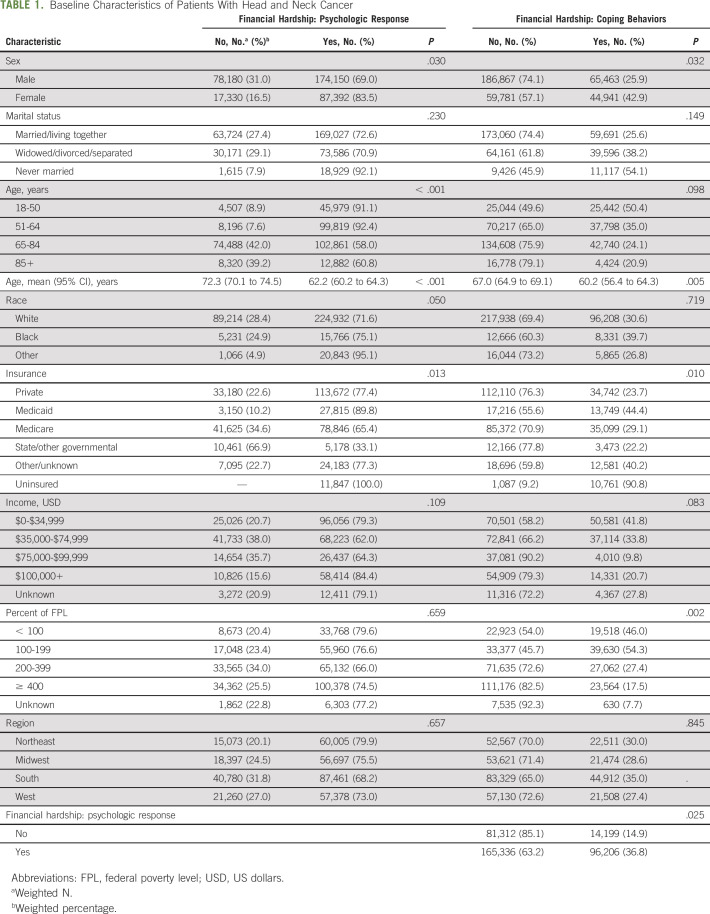
The analysis included a total of 19,442 respondents: 311 had a history of HNC and 19,131 had a history of other cancers, resulting in a weighted population of 357,052 patients with HNC and 21.4 million patients with other cancers (Table 1). Descriptive statistics for the factors used to build the aggregate measures of psychologic financial hardship and coping behaviors are in Appendix Table A2 (online only). Among patients with HNC, those who were female (84% of females v 69% of males, P = .030) and of younger age (91% of those 18-50 years v 61% of 85+ years, P < .001) more often reported psychologic financial hardship. Patients with Medicaid reported the highest levels of psychologic financial hardship compared with other insured patients (90% v 77% for privately insured patients, 77% for those with other insurance, and 65% for Medicare patients, P < .013). Marital status, region, income, and FPL were not significant for differences in psychologic financial hardship.
TABLE 1.
Baseline Characteristics of Patients With Head and Neck Cancer
Similarly, female patients more often reported financial hardship in the coping behaviors domain compared with males (43% v 26%, P = .032). Patients at a lower FPL percentage more often reported coping behavior measures (46% of < 100%, 54% of 100%-199%, 27% of 200%-399%, v 18% of ≥ 400%, P = .002). Nearly all uninsured patients reported coping behavior measures (91%), whereas among insured patients, those with Medicaid (44%) or other insurance status (40%) more often reported coping behavior measures than those with private (24%) or state/other insurance (22%; P = .010). Compared with those without any psychologic financial hardship, patients with HNC who perceived themselves to have psychologic financial hardship more often expressed coping behavior measures (15% v 37%, P = .025).
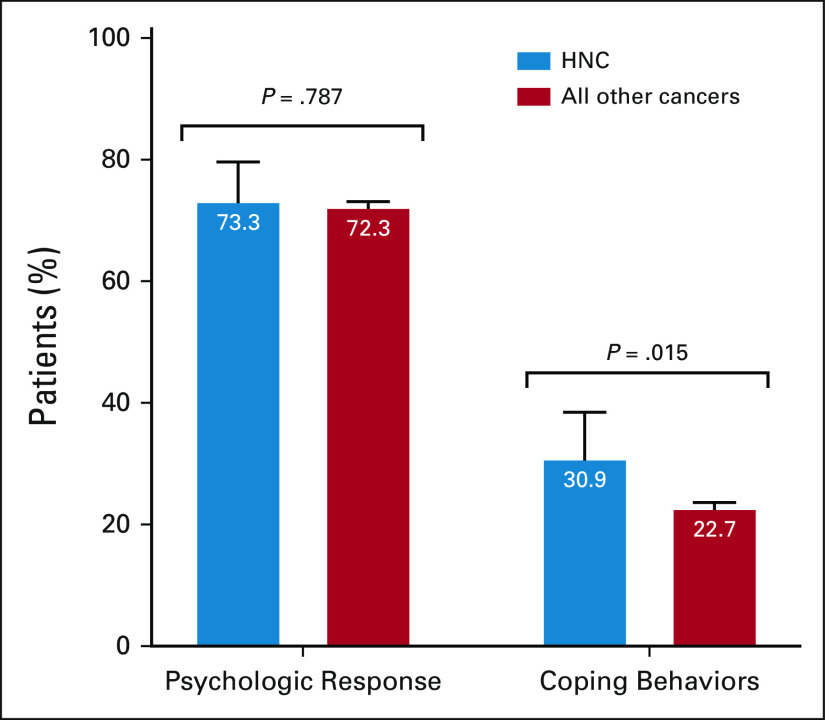
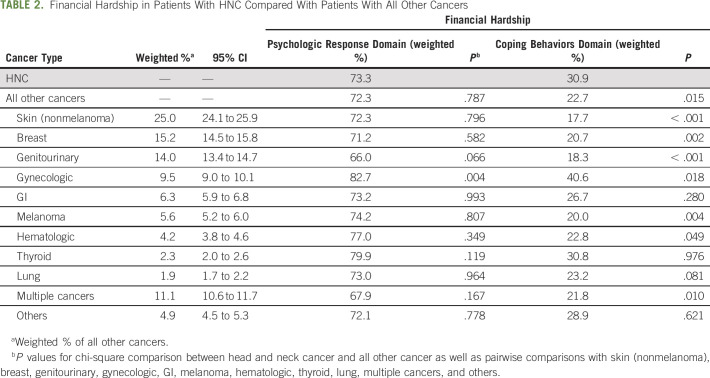
Compared with patients with other cancer types, patients with HNC were more often in the lowest income bracket (34% v 27% with annual incomes of $0-$34,999 USD, P = .045; Appendix Table A3, online only). Patients with HNC more often expressed coping behavior measures relative to other patients with cancer (31% v 23%, P = .015); however, they reported similar levels of psychologic financial hardship (73% v 72%, P = .787; Fig 1). The only subgroup of patients with cancer with more coping behavior measures were patients with gynecologic cancers (41% v 31%, P = .018; Table 2).
FIG 1.
Financial hardship in patients with HNC compared with patients with all other cancers. HNC, head and neck cancer.
TABLE 2.
Financial Hardship in Patients With HNC Compared With Patients With All Other Cancers
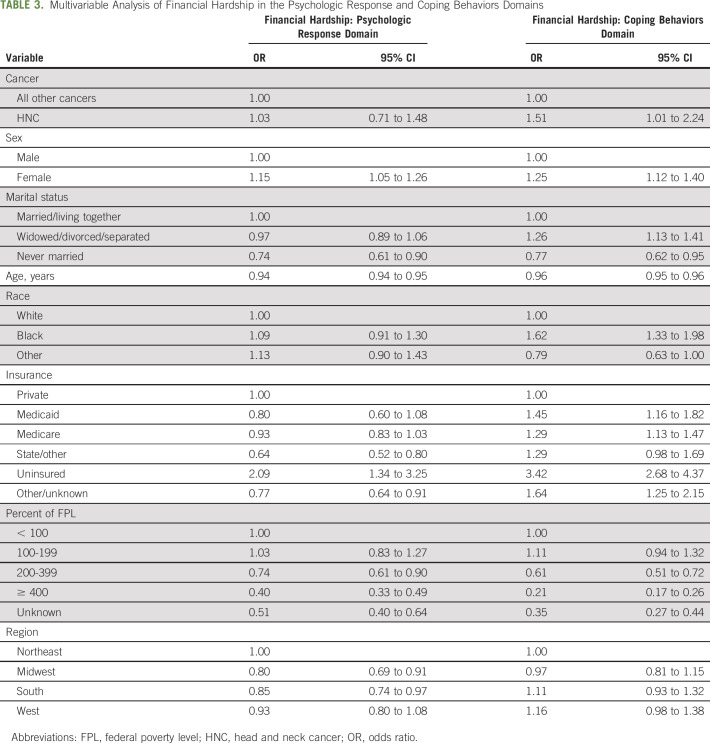
On multivariable analysis across all cancers, having an HNC diagnosis (reference, all cancers; odds ratio [95% CI], 1.51 [1.01 to 2.24]) was associated with increased odds of having financial hardship coping behavior measures, but not psychologic financial hardship (Table 3). Other factors associated with coping behavior measures across all cancers included being female (reference: male; 1.25 [1.12 to 1.40]), Black race (reference: White race; 1.62 [1.33 to 1.98]), widowed/divorced/separated (reference: married/living together; 1.26 [1.13 to 1.41]), and having nonprivate insurance or no insurance (reference: private insurance; 1.45 [1.16 to 1.82] for Medicaid; 1.29 [1.13 to 1.47] for Medicare; 3.42 [2.68 to 4.37] for uninsured; 1.64 [1.25 to 2.15] for other/unknown). Patients of increasing age (0.96 [0.95 to 0.96]), patients who were never married (reference: married/living together; 0.77 [0.62 to 0.95]), and those in ≥ 200% of the FPL (reference: < 100%; 0.61 [0.51 to 0.72] for 200%-399%; 0.21 [0.17- to 0.26] for ≥ 400%; 0.35 [0.27 to 0.44] for unknown) less often expressed coping behavior measures than other patients.
TABLE 3.
Multivariable Analysis of Financial Hardship in the Psychologic Response and Coping Behaviors Domains
DISCUSSION
Our study is the first to use nationally representative public survey data to characterize financial hardship in the psychologic response and coping behaviors domains in patients with HNC and to compare them to patients with other cancers. Important variables to consider in psychologic financial hardship and coping behavior measures in patients with HNC include female sex and Medicaid or no insurance. Interestingly, income and FPL were not associated with increased odds of psychologic financial hardship, but patients in the lower FPL brackets more often had coping behavior measures. Although patients with HNC had the same levels of psychologic financial hardship as patients with other cancers, they were more often in lower income/FPL brackets and more often expressed coping behavior measures compared with patients with other cancers.
We demonstrate that the factors associated with psychologic financial hardship differ from those associated with coping measures. This observation suggests that these two domains are unique entities, and psychologic financial hardship may not directly align with hardship related to the cost of medical care and the coping behaviors patients adopt as a result. Psychologic financial hardship appears independent of factors typically correlated with material financial concerns such as income. Our results support foundational work done by Altice et al2 that suggest that although there may be some overlap, these domains truly need to be considered separately when evaluating financial hardship among patients with cancer. Other work demonstrating that HNC-specific out-of-pocket expenses alone are not a predictive metric of psychologic financial hardship supports this assertion.17 Although there is a foundational body of work examining claims data, treatment costs, and medical expenditures in patients with HNC,9,10,12-14 the subjective implications of these financial consequences in the psychologic response domain are understudied and hence necessitate future research. Prior studies in survivors of other cancers have demonstrated that subjective indicators of financial burden such as perceived financial difficulty have a stronger impact on quality of life than direct health care costs.20
Patients with HNC more often experienced coping behavior measures because of financial hardship compared with patients with other cancers. This may be because of the combination of poorer baseline financial status compared with patients with other cancers and the way patients with HNC respond to their cancer-related expenses. Previous work investigating coping strategies for financial toxicity in patients with HNC demonstrated that 60% rely on a combination of savings and/or loans to offset expenses.18 Other potential coping strategies for patients with cancer include decreasing discretionary spending or working more hours; these coping strategies may be less accessible to patients with HNC who are disproportionally from lower socioeconomic classes7-9 and are often unable to continue working21 with approximately 33% of patients with HNC leaving the workforce entirely.11 The reliance on savings and loans may exacerbate this already vulnerable group's financial hardship compared with patients with other cancers. The higher report of financial hardship in the coping behaviors domain may also be because of elements inherent to HNC treatment that are less often found in other cancers, such as frequent needs for ancillary items that tend not to be insured (ie, dental implants, prostheses, other implants, and hearing aids), greater home care and home health needs, and greater transportation costs for adjuvant therapy.
Nevertheless, despite greater financial hardship in the coping behaviors domain, the psychologic financial hardship of patients with HNC remains similar to that experienced by patients with other cancers. This suggests that patients with HNC may under-report their psychologic response to financial hardship. Existing literature demonstrates that patients with HNC and patients in lower socioeconomic classes have a general tendency to under-report distress symptoms and need for psychosocial support.22 Clinicians should consider the potential under-reporting of psychologic financial hardship into consideration when screening patients with HNC for financial hardship using validated measures such as the COmprehensive Score for financial Toxicity (COST).15 Previous work has shown that average COST scores for patients with HNC are higher (less financial hardship),18 compared with those reported by patients across cancer types,23 although patients with HNC are more vulnerable and have higher total and relative out-of-pocket expenses compared with patients with other cancers.9 Prior qualitative work in the breast cancer literature report that more than half of the patients who expressed a desire to talk to their health care providers about the financial burden of their cancer treatment reported that they had not had a discussion about these issues.24 Thus, it is imperative that we develop interventions that improve clinician engagement and communication regarding the financial hardship of cancer treatment. While oncologists may focus on survival and quality-of-life outcomes, the impact of financial hardship cannot be ignored as the financial burdens of cancer treatment themselves can significantly affect quality-of-life and disease outcomes.3,5
Our study showed that patients with cancer who have Medicaid or no insurance more often reported financial hardship in both the psychologic response and coping behaviors domains. Uninsured patients were not included in the validation study on COST23 or in the two prior institutional studies at tertiary academic institutions that evaluated the COST scores for patients with HNC.4,18 Thus, COST may underestimate financial hardship in patients with HNC with limited or no insurance, and future validation studies in this safety net population are needed. Additionally, further work is needed to elucidate whether the increased financial hardship is due to the receipt of cancer care or the baseline financial status of patients with limited or no insurance.
Limitations of this study include its cross-sectional nature, which precludes the ability to determine directionality between the variables, and the use of self-reported public survey data. Insurance status was collected at the time of the survey, which may or may not reflect the patient's insurance at the time of cancer diagnosis. Since we lacked information on the timing of cancer diagnosis, it is possible that there are differences in financial hardship during the active treatment versus survivorship phases not captured in this study. Our analysis did not differentiate among the different subsites of HNC, disease stage, comorbidities, or treatments received. These factors may all affect levels of financial hardship.
In conclusion, patients with HNC are particularly vulnerable to financial hardship and have higher rates of coping measures than patients with other cancers; however, they report similar levels of psychologic financial hardship. Female, Medicaid, and uninsured patients are particularly vulnerable. Given concern for under-reporting of psychologic financial hardship, providers who care for patients with HNC should open a dialog regarding financial hardship with their patients and aim to practice value-based care. Furthermore, we should be actively developing prospective interventions to improve clinician engagement and effective communication strategies regarding financial hardship. Further studies are also needed to ensure that we have validated measures that adequately assess the needs of our most vulnerable uninsured patients.
ACKNOWLEDGMENT
M.M.C. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. M.M.C. is supported by the postdoctoral Ruth L. Kirschstein National Research Service Award (NIDCD; 5T32DC005356), and the funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. N.M.M. is supported by grant from the National Institutes of Health (NIH; 5 TL1 TR002242-05). L.A.D. reported receiving funding from the Agency for Healthcare Research and Quality (K08-HS-026030) during the conduct of the study. Z.S.Z.'s wife does legal work for Johnson & Johnson and Allergan through her law firm.
APPENDIX
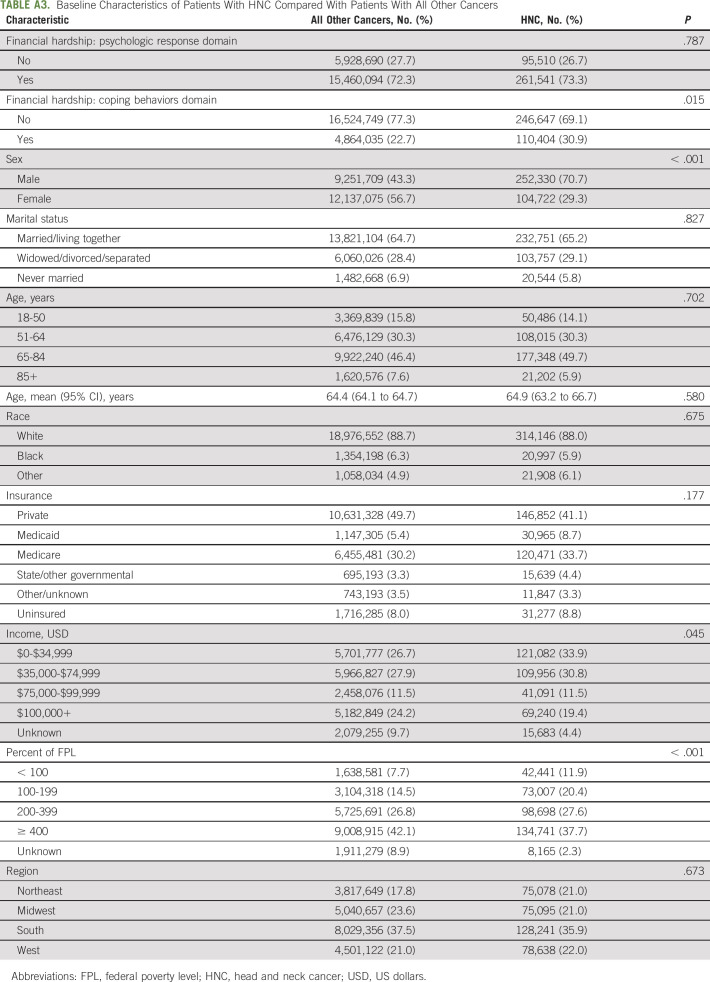
TABLE A1.
Financial Hardship Survey Questions
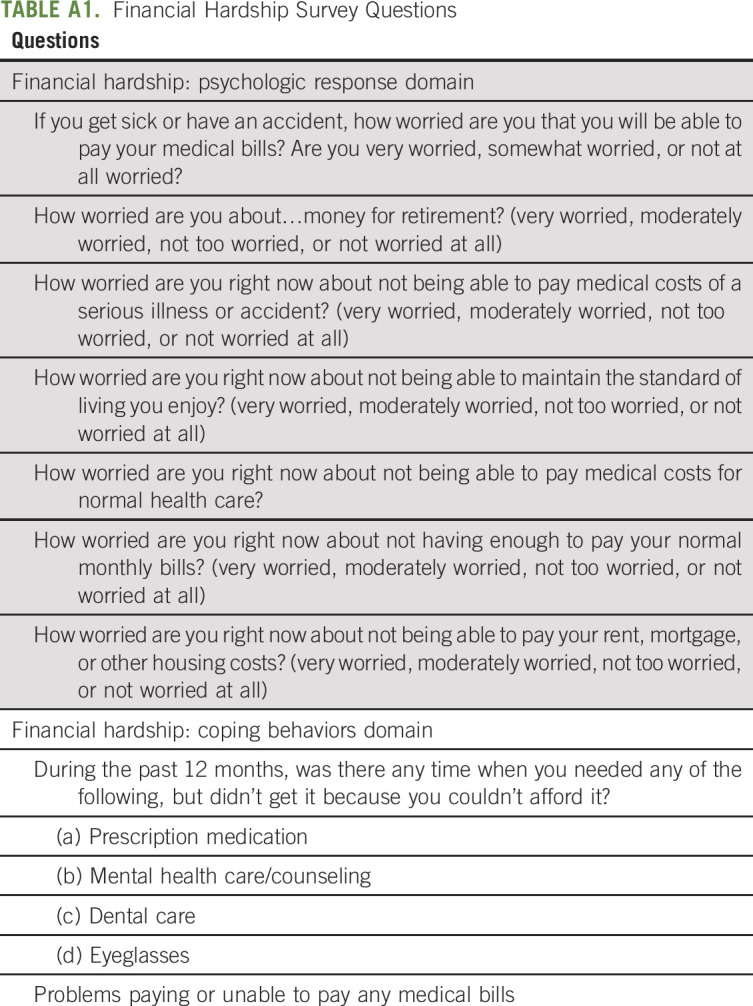
TABLE A2.
Descriptive Statistics for Financial Hardship Survey Questions by Domain
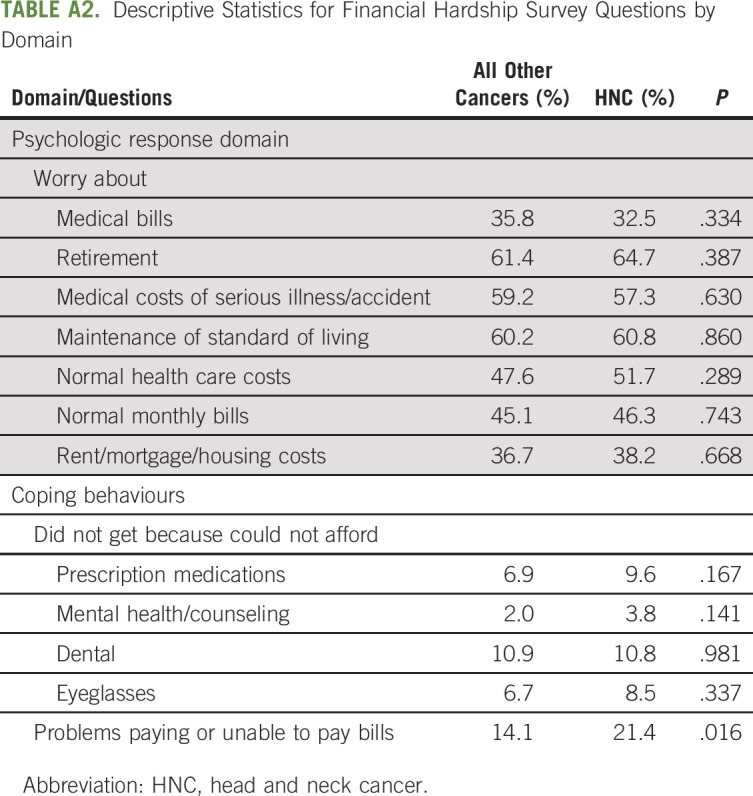
TABLE A3.
Baseline Characteristics of Patients With HNC Compared With Patients With All Other Cancers
Michelle L. Mierzwa
Research Funding: Debiopharm Group
Zachary S. Zumsteg
Consulting or Advisory Role: EMD Serono, Scripps Proton Therapy Center
Other Relationship: King and Spalding LLP
Mark E.P. Prince
Patents, Royalties, Other Intellectual Property: Receive royalties for several head and neck cancer cell lines managed by EMD Millipore Corp, US Patent US 7,723,112 B2. Compositions and Methods for Diagnosing and Treating Cancer Patents licensed to OncoMed. This is a method for sorting cancer cells to isolate cancer stem cells
Lesly A. Dossett
Research Funding: AHRQ
Michelle M. Chen
Research Funding: NIH
No other potential conflicts of interest were reported.
SUPPORT
N.M.M. is supported by grant from the National Institutes of Health (NIH; 5 TL1 TR002242-05). M.M.C. is supported by the postdoctoral Ruth L. Kirschstein National Research Service Award (NIDCD; 5T32DC005356). L.A.D. reported receiving funding from the Agency for Healthcare Research and Quality (K08-HS-026030) during the conduct of the study.
AUTHOR CONTRIBUTIONS
Conception and design: Nicole M. Mott, Michelle L. Mierzwa, Lesly A. Dossett, Michelle M. Chen
Administrative support: Michelle M. Chen
Collection and assembly of data: Nicole M. Mott, Michelle M. Chen
Data analysis and interpretation: Nicole M. Mott, Keith A. Casper, Jennifer L. Shah, Jon Mallen-St. Clair, Allen S. Ho, Zachary S. Zumsteg, Mark E.P. Prince, Michelle M. Chen
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Financial Hardship in Patients With Head and Neck Cancer
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Michelle L. Mierzwa
Research Funding: Debiopharm Group
Zachary S. Zumsteg
Consulting or Advisory Role: EMD Serono, Scripps Proton Therapy Center
Other Relationship: King and Spalding LLP
Mark E.P. Prince
Patents, Royalties, Other Intellectual Property: Receive royalties for several head and neck cancer cell lines managed by EMD Millipore Corp, US Patent US 7,723,112 B2. Compositions and Methods for Diagnosing and Treating Cancer Patents licensed to OncoMed. This is a method for sorting cancer cells to isolate cancer stem cells
Lesly A. Dossett
Research Funding: AHRQ
Michelle M. Chen
Research Funding: NIH
No other potential conflicts of interest were reported.
REFERENCES
- 1.Carrera PM, Kantarjian HM, Blinder VS: The financial burden and distress of patients with cancer: Understanding and stepping-up action on the financial toxicity of cancer treatment. CA Cancer J Clin 68:153-165, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Altice CK, Banegas MP, Tucker-Seeley RD, et al. : Financial hardships experienced by cancer survivors: A systematic review. J Natl Cancer Inst 109:djw205, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lentz R, Benson AB, Kircher S: Financial toxicity in cancer care: Prevalence, causes, consequences, and reduction strategies. J Surg Oncol 120:85-92, 2019 [DOI] [PubMed] [Google Scholar]
- 4.Beeler WH, Bellile EL, Casper KA, et al. : Patient-reported financial toxicity and adverse medical consequences in head and neck cancer. Oral Oncol 101:104521, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chino F, Peppercorn J, Taylor DH, et al. : Self-reported financial burden and satisfaction with care among patients with cancer. Oncologist 19:414-420, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ma SJ, Iovoli AJ, Attwood K, et al. : Association of significant financial burden with survival for head and neck cancer patients treated with radiation therapy. Oral Oncol 115:105196, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson S, McDonald JT, Corsten MJ: Socioeconomic factors in head and neck cancer. J Otolaryngol Head Neck Surg 37:597-601, 2008 [PubMed] [Google Scholar]
- 8.Hwang E, Johnson-Obaseki S, McDonald JT, et al. : Incidence of head and neck cancer and socioeconomic status in Canada from 1992 to 2007. Oral Oncol 49:1072-1076, 2013 [DOI] [PubMed] [Google Scholar]
- 9.Massa ST, Osazuwa-Peters N, Adjei Boakye E, et al. : Comparison of the financial burden of survivors of head and neck cancer with other cancer survivors. JAMA Otolaryngol Head Neck Surg 145:239-249, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jacobson JJ, Epstein JB, Eichmiller FC, et al. : The cost burden of oral, oral pharyngeal, and salivary gland cancers in three groups: Commercial insurance, Medicare, and Medicaid. Head Neck Oncol 4:15, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Giuliani M, Papadakos J, Broadhurst M, et al. : The prevalence and determinants of return to work in head and neck cancer survivors. Support Care Cancer 27:539-546, 2019 [DOI] [PubMed] [Google Scholar]
- 12.Wissinger E, Griebsch I, Lungershausen J, et al. : The economic burden of head and neck cancer: A systematic literature review. Pharmacoeconomics 32:865-882, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coughlan D, Yeh ST, O'Neill C, et al. : Evaluating direct medical expenditures estimation methods of adults using the medical expenditure panel survey: An example focusing on head and neck cancer. Value Health 17:90-97, 2014 [DOI] [PubMed] [Google Scholar]
- 14.Dwojak SM, Bhattacharyya N: Incremental and comparative health care expenditures for head and neck cancer in the United States. Laryngoscope 124:2305-2308, 2014 [DOI] [PubMed] [Google Scholar]
- 15.de Souza JA, Kung S, O'Connor J, et al. : Determinants of patient-centered financial stress in patients with locally advanced head and neck cancer. J Oncol Pract 13:e310-e318, 2017 [DOI] [PubMed] [Google Scholar]
- 16.Balfe M, Butow P, O'Sullivan E, et al. : The financial impact of head and neck cancer caregiving: A qualitative study. Psychooncology 25:1441-1447, 2016 [DOI] [PubMed] [Google Scholar]
- 17.Baddour K, Fadel M, Zhao M, et al. : The cost of cure: Examining objective and subjective financial toxicity in head and neck cancer survivors. Head Neck 43:3062-3075, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mady LJ, Lyu L, Owoc MS, et al. : Understanding financial toxicity in head and neck cancer survivors. Oral Oncol 95:187-193, 2019 [DOI] [PubMed] [Google Scholar]
- 19.National Center for Health Care Statistics : NHIS—About the National Health Interview Survey. Centers for Disease Control and Prevention, September 16 AA, 2020. https://www.cdc.gov/nchs/nhis/about_nhis.htm [Google Scholar]
- 20.Chen JE, Lou VW, Jian H, et al. : Objective and subjective financial burden and its associations with health-related quality of life among lung cancer patients. Support Care Cancer 26:1265-1272, 2018 [DOI] [PubMed] [Google Scholar]
- 21.Taylor JC, Terrell JE, Ronis DL, et al. : Disability in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg 130:764-769, 2004 [DOI] [PubMed] [Google Scholar]
- 22.Söllner W, DeVries A, Steixner E, et al. : How successful are oncologists in identifying patient distress, perceived social support, and need for psychosocial counselling? Br J Cancer 84:179-185, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.de Souza JA, Yap BJ, Wroblewski K, et al. : Measuring financial toxicity as a clinically relevant patient-reported outcome: The validation of the COmprehensive Score for financial Toxicity (COST). Cancer 123:476-484, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jagsi R, Ward KC, Abrahamse PH, et al. : Unmet need for clinician engagement regarding financial toxicity after diagnosis of breast cancer. Cancer 124:3668-3676, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]