Abstract
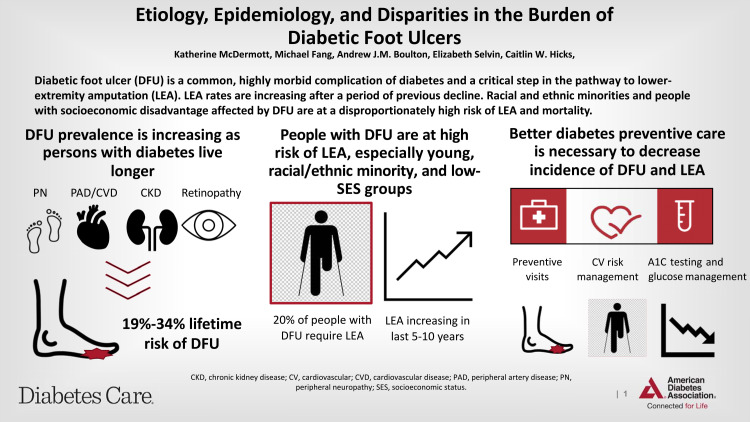
Diabetic foot ulcers (DFU) are a major source of preventable morbidity in adults with diabetes. Consequences of foot ulcers include decline in functional status, infection, hospitalization, lower-extremity amputation, and death. The lifetime risk of foot ulcer is 19% to 34%, and this number is rising with increased longevity and medical complexity of people with diabetes. Morbidity following incident ulceration is high, with recurrence rates of 65% at 3–5 years, lifetime lower-extremity amputation incidence of 20%, and 5-year mortality of 50–70%. New data suggest overall amputation incidence has increased by as much as 50% in some regions over the past several years after a long period of decline, especially in young and racial and ethnic minority populations. DFU are a common and highly morbid complication of diabetes. The pathway to ulceration, involving loss of sensation, ischemia, and minor trauma, is well established. Amputation and mortality after DFU represent late-stage complications and are strongly linked to poor diabetes management. Current efforts to improve care of patients with DFU have not resulted in consistently lower amputation rates, with evidence of widening disparities and implications for equity in diabetes care. Prevention and early detection of DFU through guideline-directed multidisciplinary care is critical to decrease the morbidity and disparities associated with DFU. This review describes the epidemiology, presentation, and sequelae of DFU, summarizes current evidence-based recommendations for screening and prevention, and highlights disparities in care and outcomes.
Graphical Abstract
Introduction
Diabetic foot ulcers (DFU) are a common, highly morbid consequence of longstanding and poorly managed diabetes. Of the estimated 537 million people worldwide who have diabetes (1), 19% to 34% will develop a DFU in their lifetime (2). Approximately 20% of people who develop a DFU will require lower-extremity amputation, either minor (below the ankle), major (above the ankle), or both (2), and 10% will die within 1 year of their first DFU diagnosis (3,4). The purpose of this review is to describe the presentation and epidemiology of DFU and its associated complications, including a discussion of disparities in DFU presentation and outcomes.
Presentation, Etiology, and Characterization of Diabetic Foot Ulcers
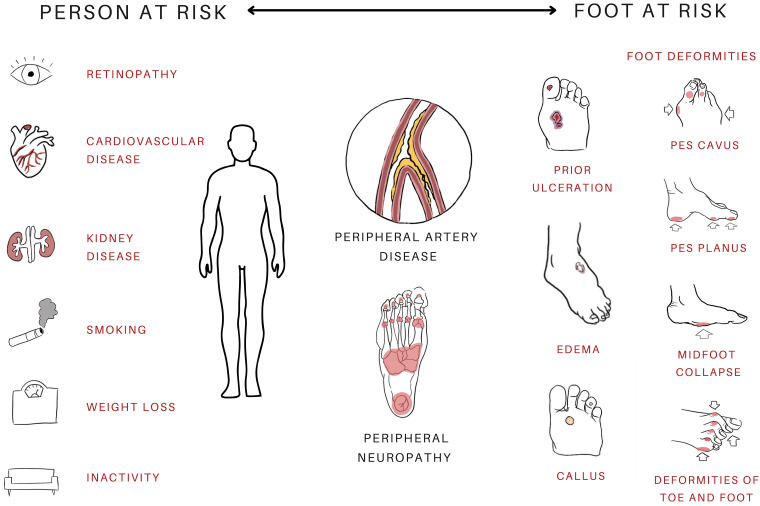
A DFU is defined as a break of the epidermis and at least part of the dermis in a person with diabetes. More superficial or closed lesions that do not penetrate to dermis (e.g., callous, blister, warmth, or erythema) are characterized as preulcerative but are at high risk of progression to ulcer (Fig. 1A) (5). Repetitive minor trauma causes ulcer formation in most cases (6), typically as a result of elevated pressure at plantar weightbearing sites, friction and shearing due to poorly fitting shoes or gait abnormalities, or an unrecognized injury sustained on an insensate foot (e.g., puncture wounds, burns, or ingrown toenails) (6). Structural deformities, such as Charcot neuroarthropathy, confer additional risk of DFU (2). Following a minor traumatic event, complex and multifactorial pathways ultimately lead to ulceration (Fig. 2) (6,7).
Figure 1.
Characteristic examples of preulcerative (A), neuropathic (B and C), neuroischemic (D–F), and ischemic (H–I) DFU.
Figure 2.
Person- and foot-specific factors interact to promote DFU risk and poor clinical outcomes.
The underlying etiology of DFU is classified into three types: purely neuropathic (35%), purely ischemic (15%), and mixed neuroischemic (50%) (8). These classifications are based on the presence or absence of peripheral neuropathy (PN) and associated sensory loss (neuropathic), peripheral artery disease (PAD) (ischemic), or both (neuroischemic) (8,9). Classic neuropathic ulcers present as painless, “punched out” round ulceration on the weightbearing surfaces of the foot with raised, macerated, or undermined margins and thick surrounding callous (Fig. 1B and C). Ischemic or neuroischemic ulcers are characteristically irregular lesions, often with a pale or necrotic base, sometimes presenting as gangrene (8), or round ulcerations at points of ischemia and friction, such as the dorsal surfaces of toe joints. Ischemic and neuroischemic ulcers are more likely than purely neuropathic ulcers to present as larger ulcers, midfoot ulcers, or hindfoot ulcers and to present with cellulitis, abscess, or osteomyelitis (Fig. 1D–I) (7). The prevalence of both PN and PAD increases with age, duration of diabetes, and higher HbA1c, and neuroischemic ulcers comprise an increasing proportion of DFU as the longevity of diabetes patients increases (7,10).
Peripheral Neuropathy
Diabetic PN is a heterogenous clinical entity but is broadly defined as any constellation of signs or symptoms of peripheral nerve dysfunction without another clear cause, presumed to be the result of both metabolic and vascular factors in the setting of chronic hyperglycemia (11). PN most often presents a symmetric polyneuropathy that is characterized by pain and paresthesia, or is asymptomatic in up to 50% of cases, along with sensory, motor, and autonomic deficits (11,12). Each of these deficits contributes to DFU occurrence.
Sensory neuropathy leads to loss of proprioception, pain, and temperature sensation (together called loss of protective sensation), which predisposes to unrecognized minor trauma and contributes to abnormal gait (8,12). Preulcerative lesions or minor wounds remain unnoticed and are repeatedly retraumatized, resulting in ulcer formation and, often, in delayed diagnosis of incident or recurrent ulcers. Motor neuropathy precipitates muscle wasting, which tends to preferentially affect extensors (8). The resulting flexor-extensor imbalance leads to foot deformities (equinus deformity, clawed toes), abnormal gait, and consequently abnormal pressure distribution that predisposes new pressure points to ulceration (Fig. 2). Autonomic neuropathy results in reduced sweating that causes dry, fragile skin prone to spontaneous cracking, reduced sympathetic nerve–induced vasoconstriction, and microvascular dysregulation of the skin that contributes to local edema and ultimately impaired healing (12).
The diagnosis of PN often requires dedicated sensory and monofilament testing, and even these can fail to diagnose mild neuropathy, especially when performed by untrained providers. The lifetime prevalence of PN in adults with diabetes is estimated to be at least 50% (12), and neuropathy of any kind confers an approximate sevenfold risk of DFU (12).
Peripheral Artery Disease
PAD is a narrowing or blockage of blood vessels in the extremities, usually the lower extremities, that results in decreased perfusion (13). Chronic limb-threatening ischemia is the clinical syndrome of end-stage PAD in which resting perfusion needs are unmet, and it manifests as rest pain and/or tissue loss (13). Diabetes is strongly associated with the development and acceleration of PAD (13,14) and leads to a unique PAD phenotype (8,15).
PAD in people with diabetes differentially affects the infrapopliteal arteries but also affects the iliac and femoral arteries at rates similar to those of adults without diabetes (15). PAD in people with diabetes is more likely to be diffuse and to present with long-segment arterial occlusions (rather than stenosis) compared with PAD in adults without diabetes (8,13) and is characterized by medial arterial calcification, as opposed to the intraluminal atherosclerosis typical of nondiabetic PAD (13,16).
PAD in adults with diabetes poses unique diagnostic challenges. Limited activity and PN may obscure symptoms of PAD (8,13). Additionally, medial calcification makes the standard ankle–brachial index unreliable due to noncompressible vessels, and toe pressures and/or toe cutaneous oxygenation are necessary adjuncts to evaluate PAD in these patients (8,13,16). PAD is likely underdiagnosed as a result, but lifetime prevalence of diagnosed PAD in diabetes is 20% to 50% (14). PAD is a contributing factor in 50% to 70% of DFU and is a significant risk factor for delayed wound healing, infection, amputation (here, and below where not specified, this includes both minor and major lower-extremity amputation), and mortality in both type 1 and type 2 diabetes (7,17,18,19).
Wound Classification and Staging
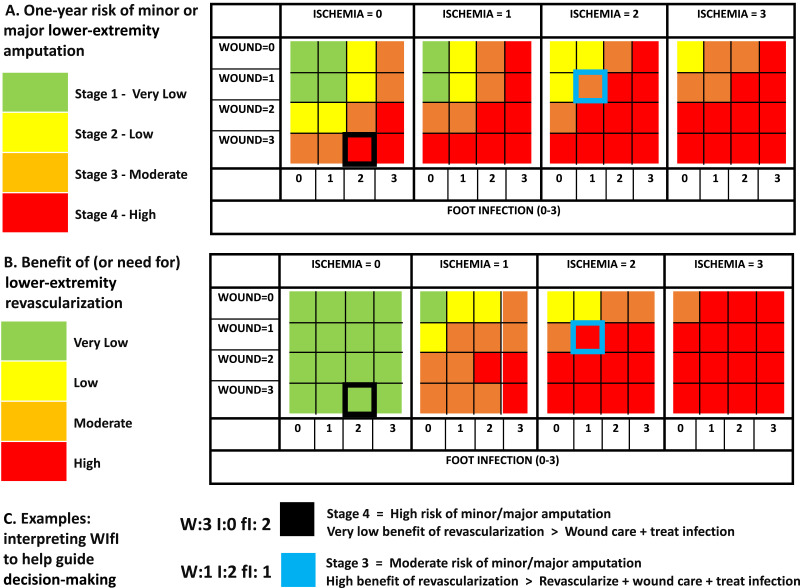
DFU comprise a wide spectrum of disease severity and acuity. Salient wound- and foot-specific factors considered in the evaluation of DFU are wound size and depth, presence and severity of infection, presence of PN or PAD, and ulcer location (20). Classification systems aim to standardize wound evaluation, communicate wound and patient characteristics between providers and across time, guide prognostication and clinical decision-making, and facilitate generalizable research on interventions and outcomes. There are several classification schemas frequently applied to DFU (Table 1), but no prevailing gold standard exists (20,21). Available resources, patient population, practice setting, and intended use generally determine which classification system is applied (20). One recently developed system widely used in multidisciplinary diabetic foot care settings is the Society Society for Vascular Surgery Wound, Ischemia, and foot Infection (WIfI) classification system (Table 1) (21), which, in addition to characterizing and risk stratifying DFU, was designed to guide clinical decision-making about the potential benefit of revascularization (Fig. 3). WIfI has been extensively validated and has prognostic utility for outcomes including wound healing rates and risk of amputation (21,22).
Table 1.
Description and summary of benefits and limitations for common existing diabetic foot and limb classification systems
| System | Components | Benefits | Limitations |
|---|---|---|---|
| Wagner (Meggit-Wagner) | Assigns ulcers one of six grades based on wound depth/extent and presence of infection, from pre- or postulcerative lesion without infection (0) to deep wound with whole-foot gangrene (5). | Simple First to be widely used, so allows for comparison with historic data High grade predicts LEA |
Variable interrater reliability Lacks inclusion of perfusion or PN/LOPS |
| University of Texas (UT) | Assigns ulcers a grade (0–3) based on depth and a stage (A–D) based on presence of infection (B), ischemia (C), or both (D). | Simple Unique in capturing pre- and postulcerative lesions High grade and stage predict LEA |
Only moderate interrater reliability Dichotomized ischemia lacks granularity Lacks inclusion of ulcer size or PN/LOPS |
| Society for Vascular Surgery Wound, Ischemia, and foot Infection (WIfI) |
Provides multilevel stratification of limb risk based on wound depth and size (W), ischemia (I), and presence and severity of foot infection (fI), each on a scale of 0–3 with detailed objective criteria for each category. Assigns a clinical stage that estimates risk of amputation from 1 (very low) to 4 (very high) based on the combination of these factors (stage 5: unsalvageable limb). | Very high interrater reliability Extensively validated Infection strata based on IWGDF Designed to provide clinical guidance about projected benefit of revascularization Predictive of LEA, time to healing, and functional status |
Relatively complex Requires expertise in perfusion measures Lacks inclusion of PN/LOPS |
| Perfusion, Extent/size, Depth/tissue loss, Infection, and Sensation (PEDIS) | Developed by the IWGDF to standardize prospective clinical research. Includes stratified categories for perfusion, extent/size, infection, and sensation, with grade provided for each category separately. | Extensively validated in diverse settings where data may be limited Unique in its inclusion of ulcer location High scores predictive of healing and LEA Has broad applications for use in population-based studies or resource-poor settings |
Dichotomized variables limit assessment of change over time or of the relative contribution of severe features (e.g., severe ischemia or infection) |
| Site, Ischemia, Neuropathy, Bacterial Infection, Area, and Depth (SINBAD) | Intended use for population-based audits. Assigns 1 (present) or 0 (absent) for location, ischemia, peripheral neuropathy, infection, area, and depth. | Extensively validated in diverse settings Unique in its inclusion of ulcer location High scores predictive of healing and LEA Has broad applications for use in population-based studies or resource-poor settings where data may be limited |
Dichotomized variables limit assessment of change over time or of the relative contribution of severe features (e.g., severe ischemia or infection) |
IWGDF, International Working Group on the Diabetic Foot, an international panel of experts including podiatrists, diabetologists, infectious disease specialists, and surgeons; LEA, lower-extremity amputation; LOPS, loss of protective sensation.
Figure 3.
Society for Vascular Surgery WIfI classification, amputation risk stratification, and benefit of revascularization. Adapted from Mills et al. (21).
Epidemiology of Diabetic Foot Ulcers
Incidence and Prevalence of DFU
Reported incidence of DFU varies widely depending on the study design, the population, and the era. In series since 2010, annual incidence generally ranges from 0.2% to 11% in diabetes-specific clinical settings (10,23–26) or from less than 0.1% to 8% in community- and population-based cohorts (10,17,27,28). Recent data on relative incidence in type 1 versus type 2 diabetes are conflicting (10,17), and differences in DFU risk between populations of type 1 and type 2 diabetes will be strongly determined by differences in age and duration of diabetes.
The International Diabetes Foundation estimates that 40 million to 60 million people globally are affected by DFU (1), a marked increase from 2015 estimates that ranged from 9 million to 26 million. Like incidence, prevalence estimates vary widely and are influenced by differences in definitions of DFU, the approach to surveillance, completeness of follow-up, and the definition of and approach to defining diabetes (denominator) (29). A recent meta-analysis found a 6.3% global prevalence of DFU among adults with diabetes (30), which equates to approximately 33 million people affected by DFU. While DFU has historically been reported at the highest rates in North America (30), modern cohort studies find rates upwards of 15% in populations of people with diabetes in Africa and South America. The global prevalence of DFU is reported to be lower in adults with type 1 compared with type 2 diabetes (30), which may reflect younger age and cumulative duration, differences in study design and data collection, and/or lack of representative cohorts of people with type 1 diabetes.
Patterns of DFU prevalence have remained stable despite fluctuations in incidence (4). Persistence of long healing times and one-year recurrence rates above 20% have not improved in the past 15–20 years despite advances in wound care and revascularization techniques (31). The lifetime risk of DFU has been frequently reported in the range of 12% to 25% (30), although a recent report by Armstrong et al. (2) suggests lifetime risk is higher (between 19% and 34%) as a result of increases in estimated life expectancy. There is a relative paucity of high-quality population-based studies of DFU incidence and prevalence. More community-based large-scale epidemiologic studies are needed to better characterize the frequency, clinical course, and risk factors for DFU, but clinical and demographic factors that have been strongly associated with DFU in the existing literature will be reviewed here.
Risk Factors for DFU and Associated Morbidity
Both patient- and foot-specific factors contribute to the risk of DFU (Fig. 2) (22). The concept of the “at-risk foot,” which requires higher-intensity screening and surveillance for DFU, is an increasing focus of research and guideline-based care (16,32). Demographic, socioeconomic, and access-to-care factors are also strongly related to DFU and its complications (33–36). Studies including adults with both type 1 and type 2 diabetes suggest that risk factors for DFU are similar (17), and the factors described below apply to both type 1 and type 2 diabetes unless otherwise stated.
Age
The risk of DFU increases with age, which is closely related to longer duration of diabetes, the cumulative effects of hyperglycemia, and a higher prevalence of micro- and macrovascular complications (30,37,38). Young and middle-aged adults with DFU tend to present with more advanced ulcer stage and are more likely to have foot infection, hospitalization, and ulcer recurrence than older adults treated in similar settings (39,40). Higher HbA1c and higher rates of PN and smoking found in young adults with diabetes may account for some of these differences (39,40). Younger adults presenting with DFU tend to represent a phenotype of severe and/or poorly managed disease that warrants special attention to glycemic control and lifestyle modification in this population.
Sex/Gender
The incidence of DFU is approximately 1.5 times higher among men than women with diabetes (30,38,41). The incidences of minor and major amputation are also higher among men, with risk estimates for men ranging from 1.4 to 3.5 times higher in several large studies (3,42,43). Sex differences are likely explained by underlying risk factors, access to care, screening, and adherence to treatment. Compliance with therapeutic footwear is similar between men and women despite women’s more negative attitudes about these shoes (44), but women are more likely to perform recommended self-care and foot care (44). Men with diabetes have a higher prevalence of PN, PAD, and cardiovascular disease (45), which together account for a majority of observed sex differences in DFU risk (45).
Race, Ethnicity, Socioeconomic Status, and Geography
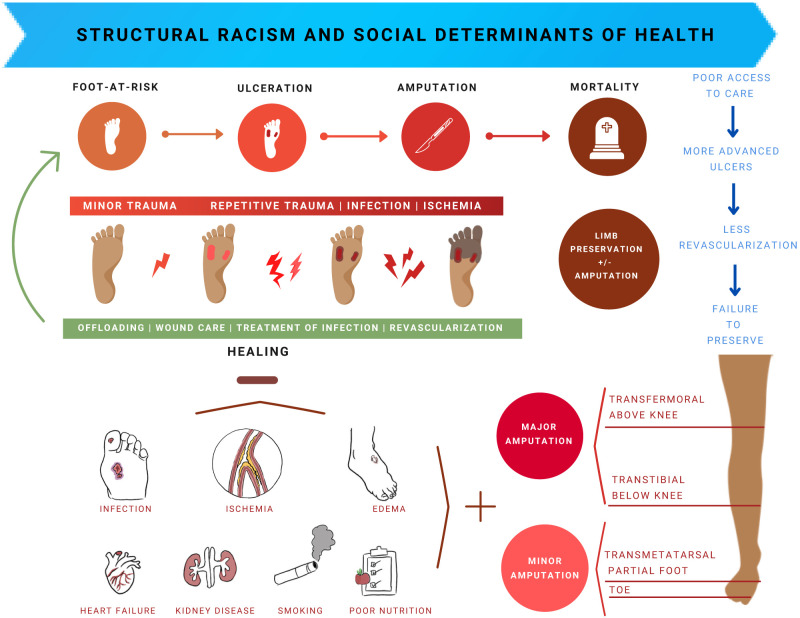
Black, Hispanic, and other non-White groups experience a much higher burden of diabetes than White adults, including a higher burden of DFU (35,46). Socioeconomic and geographic disparities overlap heavily with racial and ethnic disparities in DFU, and the independent effects of these factors are difficult to separate (47–50). Unequal access to care manifests in increased risk of incident DFU (51). Likelihood of advanced-stage ulcer at diagnosis and risk of hospitalization for DFU are higher among Black and Hispanic adults (26,36,49), individuals in the lowest-income categories (48), those with less comprehensive (or no) insurance (36,48), those with lower education levels (33), and those who live in socioeconomically deprived neighborhoods (36,48,51). Black and Hispanic adults presenting with infection and ischemia are less likely to undergo revascularization than White patients (52,53), and racial minorities and people without insurance are more likely to undergo early (within 1 year) minor or major amputation after incident DFU than White people or people with private insurance (49,54,55). These findings suggest that disparities in access to care and biases in practice patterns may each contribute to unequal outcomes (26,49,50,56,57).
High rates of lower-extremity amputation and mortality tend to cluster both within neighborhoods and by region (34,47,58,59), almost always corresponding to areas with a high density of economically deprived and racial and ethnic minority populations (47). This layering disadvantage is the consequence of racialized segregation, lack of economic opportunity, and unequal health care that characterize structural racism (60). Despite significant overlap, racial and ethnic differences in outcomes are not fully attenuated by controlling for socioeconomic or geographic factors (47,48,52). While risk for poor outcomes is compounded in people with more than one minority or disadvantaged group status (e.g., rural Black adults) (49), poor outcomes for minority groups persist despite socioeconomic advantage (e.g., high-income Black adults) (52). Some patterns, such as unequal revascularization rates in people with ischemic DFU, have been shown to widen among the highest-income Black and White adults (52). These findings reflect gaps in our ability to measure racial biases within the health system.
Geographic variation in lower-extremity outcomes is well established and is closely linked to socioeconomic status. In the U.S. and U.K., geographic variation accounts for a three- to fivefold difference in rates of incident lower-extremity amputation among adults with diabetes that can only partially be explained by clinical risk factors (34,59,57). Differential access to preventive and specialty care (59,61), financial constraints that delay presentation (62), and provider-specific practices in limb preservation (54) likely contribute to geographic disparities and to worse outcomes in minority and rural populations (49,61). Some health system-based measures, including managed care plans and Medicaid expansion, have demonstrated modest narrowing of disparities in DFU morbidity (26,63), although dedicated research on interventions to specifically address disparities is lacking.
Glycemic Management
The cumulative burden of hyperglycemia and its causal relationship with microvascular complications are well established (64). Chronically elevated HbA1c is an independent risk factor for DFU and for amputation and mortality following DFU (37). Maintaining a lower HbA1c delays the progression of microvascular complications of diabetes (65,66) and is associated with decreased risk of amputation in adults with type 1 and type 2 diabetes (65). Secondary analyses and extended follow-up of landmark trials show dose-response associations between HbA1c and risk of incident DFU and amputation (65). Early intensive glucose control may confer reduction in risk of DFU and amputation even during subsequent periods of elevated HbA1c (37), signaling a component of “metabolic memory.” These findings underscore the importance of aggressive up-front glucose management in patients with diabetes in decreasing the lifetime risk of DFU.
Overweight, Obesity, and Underweight
The association of obesity with incident DFU has not been consistently demonstrated, and obesity is not associated with incident or recurrent DFU, amputation, or mortality in several recent systematic reviews (30,38,41,67). In patients who develop DFU, underweight BMI has been linked to an increased risk of amputation and mortality in population- and hospital-based studies (17,41), likely reflecting higher rates of frailty and poor nutrition in the underweight population.
Smoking
Smoking is associated with an increased risk of PN in adults with diabetes and is an extremely strong risk factor for PAD (13). Several studies report strong associations of smoking with incident DFU (30), longer healing time, higher rates of nonhealing DFU (18), and a subsequent 1.5- to 2.5-fold increased risk of amputation (17,41,43). There are minimal data evaluating the impact of smoking cessation on PN progression or risk of lower-extremity amputation in people with DFU, but smoking cessation has been demonstrated to improve 5-year amputation-free survival by up to 20% in individuals with diabetes in PAD cohorts (68).
Cardiovascular Disease
Cardiovascular disease, including congestive heart failure, coronary artery disease, and stroke, affects up to 30% of people with diabetes globally and is the leading cause of death among people with DFU (64,69). Prospective cohorts demonstrate bidirectional associations between DFU and cardiovascular disease, with incident DFU associated with faster progression of cardiovascular disease (69), and even subclinical cardiovascular disease conferring increased risk of DFU (70). Cardiovascular disease is also associated with delayed healing and a higher risk of amputation and mortality (4,71). DFU and cardiovascular disease are both markers of diabetes severity and duration, and they act synergistically on physiologic (e.g., increased inflammatory markers, procoagulable state) and clinical (e.g., loss of functional status) factors that contribute to morbidity (72). Aggressive management of cardiovascular risk factors is a central goal of multidisciplinary diabetes care and has been shown to decrease risk of DFU occurrence and reduce mortality in people who develop DFU (73).
Chronic Kidney Disease
Diabetes is a leading global cause of chronic kidney disease (CKD) and the most common cause of end-stage kidney disease (74). The prevalence of comorbid diabetes and CKD has risen markedly over the past two decades, driven primarily by increasing diabetes prevalence (74,75); an estimated 35–42% of patients with diabetes have some degree of renal impairment (46,74,75), and the prevalence of CKD among older adults with diabetes exceeds 50% (75). Black and Hispanic adults and low-income groups have much higher rates of CKD than White and middle- or high-income groups (75).
End-stage kidney disease and CKD are linked to higher risk of incident DFU, longer healing time, higher ulcer recurrence rates, and higher rates of lower-extremity amputation (76,77). These associations are strong enough to warrant inclusion of CKD in expert definitions of an at-risk foot even for people without prior DFU or structural deformity. For people with kidney disease, end-stage kidney disease on hemodialysis confers the greatest risk of DFU (77). Stage 4 CKD is associated with an almost 4-times-increased incidence of DFU and greater than 7-times-increased risk of amputation compared with GFR ≥60 mL/min/1.73 m2 (76); even mildly reduced kidney function (eGFR 30–60 mL/min/1.73 m2) is linked with higher risk of incident DFU and amputation (76). The high prevalence of CKD among racial and ethnic minorities and socioeconomically disadvantaged people contributes to the disproportionate burden of DFU morbidity in these populations.
Retinopathy
There is a strong association between the presence and severity of diabetic retinopathy and DFU. Diabetic retinopathy occurs at two- to fourfold higher rates among adults with DFU than in those without (78). Severe diabetic retinopathy (including proliferative retinopathy) is also more frequent among adults with DFU than those without, and chronic foot wounds lasting >3 months are associated with more rapid progression of retinopathy (79). Visual impairment secondary to retinopathy may worsen gait instability and increase risk of foot trauma in those with PN, which can precipitate DFU formation (78), although the causal mechanisms have not been definitively established. Both DFU and retinopathy are likely signs of advanced microvascular disease that may partially explain this association.
Morbidity and Mortality Related to DFU
Healing and Recurrence
Ulcer healing is defined as complete epithelialization of a previously ulcerated site (22). Time from diagnosis to wound healing and overall rates of healing differ widely based on ulcer etiology, size, presence of infection, and patient characteristics, with median healing times ranging from 3 months to more than 12 months (7,80). Ischemic ulcers, larger and deeper ulcers, plantar ulcers, and ulcers with infection are associated with poor or prolonged healing (7,18,81,82). In addition to wound- and patient-level risk factors described previously, nonambulatory status is associated with prolonged healing and lower amputation-free survival (7,18). There is currently no validated predictive model for DFU healing that includes both patient and wound factors.
The strongest clinical predictor of developing a DFU is a prior DFU or amputation (2). Recurrence is the occurrence of an ulcer, either at the site of a prior ulcer or at another site, after complete healing (5). Prospective cohort studies demonstrate 1- and 3- to 5-year recurrence rates from 25% to 44% and 50% to 65%, respectively (2,39,83). Contralateral lower-extremity amputation independently increases ulcer recurrence by two- to threefold and shortens the average interval to ulcer recurrence (84), presumably due to gait alterations. Other factors consistently associated with recurrence are similar to those for nonhealing, although PAD has not been shown to be a strong influence on DFU recurrence despite its effects on primary healing (84).
Infection
Diabetic foot infection affects approximately 60% of DFU and confers a substantial risk of morbidity (67,69,85). Infection is a primary driver of emergency department visits and hospitalization in patients with diabetes and with DFU specifically (86,87). Foot ulcer precedes the vast majority of diabetic foot infections, with higher risk of infection in recurrent wounds, long-standing wounds, and wounds that probe to bone, as well as among patients with recent history of prior non–foot infection (70,85,88). Relapsed or recalcitrant infection is common; even after debridement, up to 25% of adults with diabetic foot infection will have persistent infection after 10 to 20 days, and modern series show 10% to 45% of patients hospitalized for foot infection require readmission within 1 year (89,90). Among people who develop a diabetic foot infection, the majority will require operative intervention for debridement and 15% to 20% will require amputation for adequate source control or healing (69). In people with severe infection or osteomyelitis, the amputation rate rises to almost 90% (85).
Lower-Extremity Amputation
Diabetes is the leading risk factor for lower-extremity amputation in U.S. adults, with an estimated 150,000 diabetes-related major or minor amputations per year (46). Lifetime risk of any lower-extremity amputation among people with DFU is at least 19% (56). Overall diabetes-related amputations decreased steadily over the 1990s and 2000s despite rising diabetes prevalence. Over the same time, minor amputation made up an increasing proportion of these amputations, corresponding to higher rates of lower-extremity revascularization procedures; these trends are thought to represent improved efforts at limb preservation (91,92).
After a long period of decline in incidence, several recent studies demonstrate plateaued or increasing incidence of lower-extremity amputation, including major amputation (43), with some regions experiencing a nearly 50% uptick since 2014 (42,43,46,93). The overall resurgence in severe morbidity appears to disproportionately affect younger adults and Black and Hispanic groups (42,53,55,94), which is particularly concerning given the already wide inequities in care for racial and ethnic minorities. Even controlling for DFU incidence, Black and Hispanic adults have lower rates of attempted revascularization, higher rates of failed limb preservation, and higher risk of amputation than White adults (49,50,52,53). Amputation is a late-stage complication of poor long-term diabetes management, and it often reflects inadequate access to, delivery of, and uptake of diabetes care. The compounding effects of socioeconomic disadvantage, other social determinants of health, and structural racism on marked disparities in amputation rates by race, ethnicity, and socioeconomic status cannot be overstated (35,60).
Mortality
Survival in people with incident DFU is significantly worse compared with that of similar people with diabetes without foot complications (2,67). Although DFU is a marker of more severe microvascular disease and/or otherwise poor health status, both DFU and any lower-extremity amputation are independent predictors of mortality (Fig. 4) (67,69). A recent meta-analysis comprising almost 125,000 patients in 16 countries reported mortality rates of 13.1% at 1 year, 49.1% at 5 years, and 76.9% at 10 years following incident DFU, with cardiovascular disease and infection representing the leading causes of death (67). Mortality following diabetes-related amputation is even higher: the estimated five-year mortality is 54% to 79% following minor amputation (95,96) and 53% to 91.7% following major amputation, with notably higher mortality in older adults and those with CKD and PAD (19,97,98).
Figure 4.
Pathways to ulceration and lower-extremity amputation in DFU.
Economic Burden of DFU
Diabetes care in the U.S. accounts for an estimated $273 billion in direct and $90 billion in indirect costs annually (46). Foot complications represent a major source of costs among people with diabetes, leading to higher rates of hospital admission, emergency department visits, outpatient visits and home health care utilization, and excess annual expenditures of 50% to 200% above the baseline cost of diabetes-related care (86). Advanced-stage ulcers cost upwards of $50,000 per wound episode, and direct costs of major amputation are even higher (99). These numbers likely underestimate the true economic burden of DFU given out-of-pocket expenses, loss of productivity, and decreased employment associated with DFU (86).
Primary and Secondary Prevention of DFU
Guideline-Directed Screening and Management
Prevention and management of diabetic foot complications is a centerpiece of diabetes care. A discussion of best-practice diabetes care is beyond the scope of this review, but many DFU-associated metabolic and cardiovascular risk factors are modifiable in early stages and are addressed by clinical guidelines (16). Implementation of comprehensive guideline-directed care for patients with diabetes is improving, but rates of adherence to multiple quality indicators are only 50% to 68% in the U.S. and Europe (32). Achievement of clinical targets is lower, with blood pressure targets met in fewer than 30% of patients and HbA1c near or below 7.0% in fewer than 45% of patients (100). Black, Hispanic, Native American/American Indian, and indigenous peoples continue to be significantly less likely than non-Hispanic White groups to receive full guideline-directed care and to achieve guideline-recommended goals (32), almost certainly contributing to the increased risk of DFU in these populations.
Foot Exams
Delayed ulcer presentation predicts poor prognosis (7,54,87). Frequent foot exams are fundamental to decreasing incidence and morbidity, and inadequate foot care is associated with higher rates of DFU, LEA, and mortality (101,102). Guidelines for frequency of screening for PN, PAD, and DFU or other preulcerative lesions in the adults with diabetes (Table 2) recommend at least an annual comprehensive foot exam for all patients with diabetes, including inspection, monofilament and tuning fork evaluation for loss of protective sensation, and pulse exam (1,16). Screening exams should be performed every 3–6 months for high-risk patients (16). The importance of multidisciplinary foot care for high-risk people deserves particular emphasis, especially the involvement of podiatry and vascular surgery (45).
Table 2.
Professional guidelines for screening and management of patients at risk for DFU
| Guidelines | Foot exams | PN | PAD | Footwear | Education |
|---|---|---|---|---|---|
| Society for Vascular Surgery 2016 | All: annual inspection by a provider trained in foot care Elevated risk: no specific recommendations, though consider referral to specialist or MDFC |
All: annual 10-g monofilament test with foot exam | All: screening ABI at the age of 50 years High risk (prior DFU or amputation, known CVD, nephropathy): annual LE vascular exam including ABI and TP ± TcPO2 |
Low risk: recommend against therapeutic footwear High risk (PN, foot deformity, previous amputation): custom footwear for high risk |
Patient education on preventive foot care |
| American Diabetes Association 2021 | All: comprehensive foot exam at least annually (inspection, 10-g monofilament testing + temp or pinprick or vibration, LE pulse exam) Any elevated risk (LOPS or prior ulceration or amputation): foot inspection at every visit High risk (active smoker, prior lower-extremity complications, LOPS, deformity, PAD): refer to foot care specialist |
All: screening for distal neuropathy with temp or pinprick and tuning fork (T2DM at diagnosis, T1DM 5 years after diagnosis) Annual monofilament testing |
All: annual vascular exam (lower extremity and foot pulses) Refer patients with claudication or absent pulses for ABI and vascular evaluation |
Therapeutic footwear for high risk (severe PN, PAD, foot deformity, preulcerative lesion, prior ulcer or amputation) | Patient education on preventive foot care |
| International Working Group on the Diabetic Foot 2019 | Very low risk: annual comprehensive foot exam Low risk (LOPS or PAD): exam every 6–12 months Moderate risk (any two of LOPS, PAD, foot deformity): exam every 3–6 months High risk (LOPS or PAD and history of ulcer or amputation or ESKD): exam every 1–3 months |
All: annual assessment for LOPS (10-g monofilament, tuning fork) If neither available assess sensation to light touch |
All: annual vascular exam (lower extremity and foot pulses) With active DFU: ABI or TBI and TP, TcPO2, refer for further imaging if ABI <0.5, TP <30 mmHg, or TcPO2 <25 mmHg |
Moderate risk or prior ulcer: properly fitting footwear that reduces plantar pressure Moderate risk with deformity or preulcer: consider custom-made footwear, insoles, orthoses Moderate risk with healed plantar ulcer: prescribe therapeutic footwear to reduce plantar pressure, emphasize consistent wear |
All: structured education on preventive practices and potential consequences of DFU Any level of risk: daily foot inspection by self or care partner Moderate or high risk: consider daily at-home foot temperature monitoring |
ABI, ankle-brachial index; CVD, cardiovascular disease; ESKD, end-stage kidney disease; LE, lower extremity; LOPS, loss of protective sensation; MDFC, multidisciplinary diabetic foot clinic; T1DM, type 1 diabetes; T2DM, type 2 diabetes; TBI, toe-brachial index; TcPO2, transcutaneous oximetry, (a measure of tissue oxygenation, where normal is >55 mmHg); temp, temperature; TP, toe pressure (usually systolic pressure).
Rates of annual foot exams by a provider in adults with diabetes vary widely (32). In the U.S., where annual foot exams are a quality metric tied to reimbursement, adherence has been stagnant despite improved achievement of other components of guideline-directed diabetes care (32). Certain racial and ethnic minority populations (e.g., Hispanic and Asian adults), people without insurance, and socioeconomically disadvantaged populations receive less overall guideline-directed care and are also less likely to report foot exam by a provider in the past year (32,35). The implementation of a hemodialysis center-based monthly foot screening in a U.S. study showed a 17% reduction in subsequent risk of amputation, demonstrating the significant potential effectiveness of screening in high-risk groups (103). Routine foot screening is critical and low rates of adherence to standards of care for preventing diabetic foot infections is a major concern.
Emerging Modalities for Self-Screening and Early Detection of DFU
Several promising technologies may aid in the early detection of preulcerative or ulcerative foot lesions. Telemedicine-assisted foot examinations have been shown in small studies to be as effective as in-person provider exams at detecting early lesions, with time and cost savings to patients that have promise to reduce existing barriers to care (62,104). Increased temperature is a well-validated preulcerative sign, and clinical trials of temperature-sensing mats (105) and socks (106) have been successful in identifying preulcer or DFU weeks earlier than a clinical exam. These passive surveillance technologies may be able to reduce incident DFU through alerts to offload pressure points temporarily or by prompting a thorough foot evaluation. Additional pressure-sensing modalities including insoles may help risk-stratify people with high plantar pressures, monitor for effective offloading before or during DFU episodes, and evaluate progress in gait retraining after DFU healing or amputation (107). Despite compelling evidence supporting their efficacy and cost effectiveness, these technologies have not been widely adopted.
Quality of Life and Functional Impact of DFU
The detrimental effect of DFU on overall health status and quality of life is well documented, and patient-reported outcomes are increasingly recognized as meaningful measures in diabetic foot care (108,109). People with DFU typically report poor quality of life, primarily in the domain of physical functioning. Persistent ulcers, major amputation, and limited ambulation are associated with worse quality of life for both patients and their caregivers (108,109). Healing, including after minor amputation, is associated with dramatic improvement in self-reported physical functioning, and people with healed DFU have overall self-reported quality of life near the norms for populations without diabetes (109).
Though qualitative studies consistently identify fear, anxiety, frustration, isolation, and sadness as common emotional responses to the diagnosis of DFU, few studies have demonstrated differences in psychosocial quality of life related to DFU (109). DFU-specific measures have been proposed to better assess the social and emotional consequences of active ulcers and should be considered when evaluating patient-reported outcomes.
Conclusions
DFU is a common complication of diabetes that has been aptly compared with cancer in terms of chronicity, recidivism, cost, and burden (97). Major clinical risk factors for DFU are PN, PAD, and foot deformities, but race, ethnicity, socioeconomic status, and geography are powerful mediators of risk for DFU and lower-extremity amputation. The consequences of first ulceration—poor quality of life, recurrence, major amputation, and death—are significant, but this morbidity is not reflected in the funding allocated for DFU-related research, which totals less than 0.2% of total federal spending on diabetes (97).
Complications of DFU can be attenuated by guideline-directed screening, early diagnosis, and aggressive medical management of diabetes and cardiovascular disease. Ineffective population-based screening, limited access to preventive care, and delays in access to diabetes, vascular, and podiatry specialist care contribute to late-stage ulcer presentation and, thus, to poor prognosis. Rising lower-extremity amputation rates among young and middle-aged adults with diabetes and persistent racial, ethnic, and socioeconomic disparities reflect these gaps in care.
Major efforts are needed to develop health system-wide improvements in DFU prevention and early diagnosis, especially in disadvantaged populations. Funding should be prioritized for high-quality population-based registries to track DFU incidence, prevalence, outcomes, and process measures. Initiatives to expand use of effective at-home screening modalities and allocate resources for more frequent provider foot exams in regions where major amputation rates are high have the potential to reduce DFU incidence and morbidity in the most at-risk populations. Dedicated research on racial and socioeconomic differences in timing of care, limb preservation, and amputation are necessary to identify and address factors perpetuating structural bias and disparate outcomes. Significantly more public and institutional funding for DFU research and care initiatives is warranted to correct the imbalance between current resource allocation and the enormous burden of DFU. Ultimately, a paradigm shift toward DFU prevention and health equity is required to produce meaningful reductions in DFU, major lower-extremity amputation, and mortality.
Article Information
Acknowledgments. We acknowledge the contributions of Caroline Wang (Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD) and Alana Keegan (Division of Vascular Surgery and Endovascular Therapy, Department of Surgery, Johns Hopkins University School of Medicine, Baltimore, MD) in creating and editing figures and tables.
Funding. C.H. was supported by National Institutes of Health (NIH) National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grant K23 DK124515. L.S. was supported by NIH National Heart, Lung, and Blood Institute grant K24 HL152440. This work was also supported by NIH NIDDK grant R01 DK089174 to L.S.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. K.M. completed literature review and wrote the manuscript. M.F. and A.J.M.B. reviewed and edited the manuscript. E.S. and C.W.H. were involved in the conception of this work and reviewed and edited the manuscript. All authors approved of the final version of the manuscript. K.M. and C.W.H. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1. International Diabetes Federation . The Diabetic Foot. Brussels, Belgium, International Diabetes Federation, 2020. Accessed 1 August 2022. Available from https://www.idf.org/our-activities/care-prevention/diabetic-foot.html
- 2. Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med 2017;376:2367–2375 [DOI] [PubMed] [Google Scholar]
- 3. Hoffstad O, Mitra N, Walsh J, Margolis DJ. Diabetes, lower-extremity amputation, and death. Diabetes Care 2015;38:1852–1857 [DOI] [PubMed] [Google Scholar]
- 4. Meloni M, Izzo V, Giurato L, Lázaro-Martínez JL, Uccioli L. Prevalence, clinical aspects and outcomes in a large cohort of persons with diabetic foot disease: comparison between neuropathic and ischemic ulcers. J Clin Med 2020;9:1780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. van Netten JJ, Bus SA, Apelqvist J, et al.; International Working Group on the Diabetic Foot . Definitions and criteria for diabetic foot disease. Diabetes Metab Res Rev 2020;36(Suppl. 1):e3268. [DOI] [PubMed] [Google Scholar]
- 6. Boulton AJM. The pathway to foot ulceration in diabetes. Med Clin North Am 2013;97:775–790 [DOI] [PubMed] [Google Scholar]
- 7. Yotsu RR, Pham NM, Oe M, et al. Comparison of characteristics and healing course of diabetic foot ulcers by etiological classification: neuropathic, ischemic, and neuro-ischemic type. J Diabetes Complications 2014;28:528–535 [DOI] [PubMed] [Google Scholar]
- 8. Sidawy AN, Perler BA, Eds. Rutherford’s vascular surgery and endovascular therapy. 9th ed. Philadelphia, PA, Elsevier, 2019 [Google Scholar]
- 9. Armstrong DG, Cohen K, Courric S, Bharara M, Marston W. Diabetic foot ulcers and vascular insufficiency: our population has changed, but our methods have not. J Diabetes Sci Technol 2011;5:1591–1595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rasmussen A, Almdal T, Anker Nielsen A, et al. Decreasing incidence of foot ulcer among patients with type 1 and type 2 diabetes in the period 2001-2014. Diabetes Res Clin Pract 2017;130:221–228 [DOI] [PubMed] [Google Scholar]
- 11. Pop-Busui R, Boulton AJM, Feldman EL, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care 2017;40:136–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hicks CW, Selvin E. Epidemiology of peripheral neuropathy and lower extremity disease in diabetes. Curr Diab Rep 2019;19:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Conte MS, Bradbury AW, Kolh P, White JV, Dick F, Fitridge R, et al. Global vascular guidelines on the management of chronic limb-threatening ischemia. J Vasc Surg 2019;69:3S–125S.e40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Barnes JA, Eid MA, Creager MA, Goodney PP. Epidemiology and risk of amputation in patients with diabetes mellitus and peripheral artery disease. Arterioscler Thromb Vasc Biol 2020;40:1808–1817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jude EB, Oyibo SO, Chalmers N, Boulton AJM. Peripheral arterial disease in diabetic and nondiabetic patients: a comparison of severity and outcome. Diabetes Care 2001;24:1433–1437 [DOI] [PubMed] [Google Scholar]
- 16. Hingorani A, LaMuraglia GM, Henke P, et al. The management of diabetic foot: a clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. J Vasc Surg 2016;63(Suppl.):3S–21S [DOI] [PubMed] [Google Scholar]
- 17. Chamberlain RC, Fleetwood K, Wild SH, et al. Foot ulcer and risk of lower limb amputation or death in people with diabetes: a national population-based retrospective cohort study. Diabetes Care 2022;45:83–91 [DOI] [PubMed] [Google Scholar]
- 18. Zhang Y, Cramb S, McPhail SM, et al.; Diabetic Foot Working Group, Queensland Statewide Diabetes Clinical Network, Australia . Factors associated with healing of diabetes-related foot ulcers: observations from a large prospective real-world cohort. Diabetes Care 2021;44:e143–e145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Prompers L, Schaper N, Apelqvist J, et al. Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The EURODIALE Study. Diabetologia 2008;51:747–755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Game F. Classification of diabetic foot ulcers. Diabetes Metab Res Rev 2016;32(Suppl. 1):186–194 [DOI] [PubMed] [Google Scholar]
- 21. Mills JL Sr, Conte MS, Armstrong DG, et al.; Society for Vascular Surgery Lower Extremity Guidelines Committee . The Society for Vascular Surgery lower extremity threatened limb classification system: risk stratification based on wound, ischemia, and foot infection (WIfI). J Vasc Surg 2014;59:220–34.e1, 2 [DOI] [PubMed] [Google Scholar]
- 22. Monteiro-Soares M, Russell D, Boyko EJ, et al.; International Working Group on the Diabetic Foot (IWGDF) . Guidelines on the classification of diabetic foot ulcers (IWGDF 2019). Diabetes Metab Res Rev 2020;36(Suppl. 1):e3273. [DOI] [PubMed] [Google Scholar]
- 23. Paisey RB, Abbott A, Paisey CF, Walker D. Diabetic foot ulcer incidence and survival with improved diabetic foot services: an 18-year study. Diabet Med 2019;36:1424–1430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Crawford F, Nicolson DJ, Amanna AE, et al. Preventing foot ulceration in diabetes: systematic review and meta-analyses of RCT data. Diabetologia 2020;63:49–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chen D, Wang M, Shang X, et al. Development and validation of an incidence risk prediction model for early foot ulcer in diabetes based on a high evidence systematic review and meta-analysis. Diabetes Res Clin Pract 2021;180:109040. [DOI] [PubMed] [Google Scholar]
- 26. Tan TW, Calhoun EA, Knapp SM, et al. Rates of diabetes-related major amputations among racial and ethnic minority adults following Medicaid expansion under the Patient Protection and Affordable Care Act. JAMA Netw Open 2022;5:e223991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Røikjer J, Werkman NCC, Ejskjaer N, et al. Incidence, hospitalization and mortality and their changes over time in people with a first ever diabetic foot ulcer. Diabet Med 2022;39:e14725. [DOI] [PubMed] [Google Scholar]
- 28. Iwase M, Fujii H, Nakamura U, et al. Incidence of diabetic foot ulcer in Japanese patients with type 2 diabetes mellitus: the Fukuoka diabetes registry. Diabetes Res Clin Pract 2018;137:183–189 [DOI] [PubMed] [Google Scholar]
- 29. Margolis DJ, Jeffcoate W. Epidemiology of foot ulceration and amputation: can global variation be explained? Med Clin North Am 2013;97:791–805 [DOI] [PubMed] [Google Scholar]
- 30. Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Ann Med 2017;49:106–116 [DOI] [PubMed] [Google Scholar]
- 31. Fu XL, Ding H, Miao WW, Mao CX, Zhan MQ, Chen HL. Global recurrence rates in diabetic foot ulcers: a systematic review and meta-analysis. Diabetes Metab Res Rev 2019;35:e3160. [DOI] [PubMed] [Google Scholar]
- 32. Shin JI, Wang D, Fernandes G, et al. Trends in receipt of American Diabetes Association guideline-recommended care among U.S. adults with diabetes: NHANES 2005-2018. Diabetes Care 2021;44:1300–1308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tatulashvili S, Fagherazzi G, Dow C, Cohen R, Fosse S, Bihan H. Socioeconomic inequalities and type 2 diabetes complications: a systematic review. Diabetes Metab 2020;46:89–99 [DOI] [PubMed] [Google Scholar]
- 34. Zhang GQ, Canner JK, Kayssi A, Abularrage CJ, Hicks CW. Geographical socioeconomic disadvantage is associated with adverse outcomes following major amputation in diabetic patients. J Vasc Surg 2021;74:1317–1326.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Canedo JR, Miller ST, Schlundt D, Fadden MK, Sanderson M. Racial/ethnic disparities in diabetes quality of care: the role of healthcare access and socioeconomic status. J Racial Ethn Health Disparities 2018;5:7–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Blumberg SN, Warren SM. Disparities in initial presentation and treatment outcomes of diabetic foot ulcers in a public, private, and Veterans Administration hospital. J Diabetes 2014;6:68–75 [DOI] [PubMed] [Google Scholar]
- 37. Boyko EJ, Zelnick LR, Braffett BH, et al. Risk of foot ulcer and lower-extremity amputation among participants in the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study. Diabetes Care 2022;45:357–364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Rossboth S, Lechleitner M, Oberaigner W. Risk factors for diabetic foot complications in type 2 diabetes-A systematic review. Endocrinol Diabetes Metab 2020;4:e00175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hicks CW, Canner JK, Mathioudakis N, Lippincott C, Sherman RL, Abularrage CJ. Incidence and risk factors associated with ulcer recurrence among patients with diabetic foot ulcers treated in a multidisciplinary setting. J Surg Res 2020;246:243–250 [DOI] [PubMed] [Google Scholar]
- 40. Tong T, Yang C, Tian W, et al. Phenotypes and outcomes in middle-aged patients with diabetic foot ulcers: a retrospective cohort study. J Foot Ankle Res 2020;13:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lin C, Liu J, Sun H. Risk factors for lower extremity amputation in patients with diabetic foot ulcers: a meta-analysis. PLoS One 2020;15:e0239236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Geiss LS, Li Y, Hora I, Albright A, Rolka D, Gregg EW. Resurgence of diabetes-related nontraumatic lower-extremity amputation in the young and middle-aged adult U.S. population. Diabetes Care 2019;42:50–54 [DOI] [PubMed] [Google Scholar]
- 43. Harding JL, Andes LJ, Rolka DB, et al. National and state-level trends in nontraumatic lower-extremity amputation among U.S. Medicare beneficiaries with diabetes, 2000-2017. Diabetes Care 2020;43:2453–2459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Jarl G, Alnemo J, Tranberg R, Lundqvist LO. Gender differences in attitudes and attributes of people using therapeutic shoes for diabetic foot complications. J Foot Ankle Res 2019;12:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Sorber R, Abularrage CJ. Diabetic foot ulcers: epidemiology and the role of multidisciplinary care teams. Semin Vasc Surg 2021;34:47–53 [DOI] [PubMed] [Google Scholar]
- 46. Centers for Disease Control and Prevention . National Diabetes Statistics Report. Atlanta, GA, Centers for Disease Control and Prevention, 2022. Accessed 6 June 2022. Available from https://www.cdc.gov/diabetes/data/statistics-report/index.html
- 47. Fanaroff AC, Yang L, Nathan AS, et al. Geographic and socioeconomic disparities in major lower extremity amputation rates in metropolitan areas. J Am Heart Assoc 2021;10:e021456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Eslami MH, Zayaruzny M, Fitzgerald GA. The adverse effects of race, insurance status, and low income on the rate of amputation in patients presenting with lower extremity ischemia. J Vasc Surg 2007;45:55–59 [DOI] [PubMed] [Google Scholar]
- 49. Brennan MB, Powell WR, Kaiksow F, et al. Association of race, ethnicity, and rurality with major leg amputation or death among Medicare beneficiaries hospitalized with diabetic foot ulcers. JAMA Netw Open 2022;5:e228399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Mizelle RM Jr. Diabetes, race, and amputations. Lancet 2021;397:1256–1257 [DOI] [PubMed] [Google Scholar]
- 51. Riley J, Antza C, Kempegowda P, et al. Social deprivation and incident diabetes-related foot disease in patients with type 2 diabetes: a population-based cohort study. Diabetes Care 2021;44:731–739 [DOI] [PubMed] [Google Scholar]
- 52. Durazzo TS, Frencher S, Gusberg R. Influence of race on the management of lower extremity ischemia: revascularization vs amputation. JAMA Surg 2013;148:617–623 [DOI] [PubMed] [Google Scholar]
- 53. Garcia M, Hernandez B, Ellington TG, et al. A lack of decline in major nontraumatic amputations in Texas: contemporary trends, risk factor associations, and impact of revascularization. Diabetes Care 2019;42:1061–1066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Fan KL, DeLia D, Black CK, et al. Who, what, where: demographics, severity of presentation, and location of treatment drive delivery of diabetic limb reconstructive services within the National Inpatient Sample. Plast Reconstr Surg 2020;145:1516–1527 [DOI] [PubMed] [Google Scholar]
- 55. Miller TA, Campbell JH, Bloom N, Wurdeman SR. Racial disparities in health care with timing to amputation following diabetic foot ulcer. Diabetes Care 2022;45:2336–2341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Rodrigues BT, Vangaveti VN, Urkude R, Biros E, Malabu UH. Prevalence and risk factors of lower limb amputations in patients with diabetic foot ulcers: a systematic review and meta-analysis. Diabetes Metab Syndr 2022;16:102397. [DOI] [PubMed] [Google Scholar]
- 57. Newhall K, Spangler E, Dzebisashvili N, Goodman DC, Goodney P. Amputation rates for patients with diabetes and peripheral arterial disease: the effects of race and region. Ann Vasc Surg 2016;30:292–298.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Hurst JE, Barn R, Gibson L, et al. Geospatial mapping and data linkage uncovers variability in outcomes of foot disease according to multiple deprivation: a population cohort study of people with diabetes. Diabetologia 2020;63:659–667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Margolis DJ, Hoffstad O, Nafash J, et al. Location, location, location: geographic clustering of lower-extremity amputation among Medicare beneficiaries with diabetes. Diabetes Care 2011;34:2363–2367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Bailey ZD, Feldman JM, Bassett MT. How structural racism works—racist policies as a root cause of U.S. racial health inequities. N Engl J Med 2021;384:768–773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Sutherland BL, Pecanac K, Bartels CM, Brennan MB. Expect delays: poor connections between rural and urban health systems challenge multidisciplinary care for rural Americans with diabetic foot ulcers. J Foot Ankle Res 2020;13:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Tan TW, Crocker RM, Palmer KNB, Gomez C, Armstrong DG, Marrero DG. A qualitative study of barriers to care-seeking for diabetic foot ulceration across multiple levels of the healthcare system. J Foot Ankle Res 2022;15:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. McEwen LN, Ylitalo KR, Herman WH, Wrobel JS. Prevalence and risk factors for diabetes-related foot complications in Translating Research Into Action for Diabetes (TRIAD). J Diabetes Complications 2013;27:588–592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Skyler JS, Bergenstal R, Bonow RO, et al.; American Diabetes Association; American College of Cardiology Foundation; American Heart Association . Intensive glycemic control and the prevention of cardiovascular events: implications of the ACCORD, ADVANCE, and VA diabetes trials: a position statement of the American Diabetes Association and a scientific statement of the American College of Cardiology Foundation and the American Heart Association. Circulation 2009;119:351–357 [DOI] [PubMed] [Google Scholar]
- 65. Goldman MP, Clark CJ, Craven TE, et al. Effect of intensive glycemic control on risk of lower extremity amputation. J Am Coll Surg 2018;227:596–604 [DOI] [PubMed] [Google Scholar]
- 66. Patel A, MacMahon S, Chalmers J, et al.; ADVANCE Collaborative Group . Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560–2572 [DOI] [PubMed] [Google Scholar]
- 67. Chen L, Sun S, Gao Y, Ran X. Global mortality of diabetic foot ulcer: a systematic review and meta-analysis of observational studies. Diabetes Obes Metab. 20 August 2022 [Epub ahead of print]. DOI: 10.1111/dom.14840 [DOI] [PubMed] [Google Scholar]
- 68. Armstrong EJ, Wu J, Singh GD, et al. Smoking cessation is associated with decreased mortality and improved amputation-free survival among patients with symptomatic peripheral artery disease. J Vasc Surg 2014;60:1565–1571 [DOI] [PubMed] [Google Scholar]
- 69. Fang M, Hu J, Matsushita K, Selvin E, Hicks CW. 126-OR: Long-term consequences of diabetic foot infection: the Atherosclerosis Risk in Communities (ARIC) Study. Diabetes 2022;71(Suppl. 1):126-OR [Google Scholar]
- 70. Fang M, Hu J, Matsushita K, Selvin E, Hicks CW. Abstract MP10: Risk factors for diabetic foot infection: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation 2022;145:AMP10 [Google Scholar]
- 71. Bruun C, Siersma V, Guassora AD, Holstein P, de Fine Olivarius N. Amputations and foot ulcers in patients newly diagnosed with type 2 diabetes mellitus and observed for 19 years. The role of age, gender and co-morbidity. Diabet Med 2013;30:964–972 [DOI] [PubMed] [Google Scholar]
- 72. Dietrich I, Braga GA, de Melo FG, da Costa Silva Silva ACC. The diabetic foot as a proxy for cardiovascular events and mortality review. Curr Atheroscler Rep 2017;19:44. [DOI] [PubMed] [Google Scholar]
- 73. Williams DT, Powell-Chandler A, Qureshi Q, Zaidi A, Whitaker CJ. Improved limb salvage for patients with vascular disease and tissue loss associated with new model of provision targeted at the diabetic foot. Diabetes Res Clin Pract 2018;135:50–57 [DOI] [PubMed] [Google Scholar]
- 74. United States Renal Data System . USRDS annual data report: epidemiology of kidney disease in the United States. Bethesda, MD, United States Renal Data System, 2020. Accessed 10 August 2022. Available from https://adr.usrds.org/2020
- 75. Kibria GMA, Crispen R. Prevalence and trends of chronic kidney disease and its risk factors among US adults: an analysis of NHANES 2003–18. Prev Med Rep 2020;20:101193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Margolis DJ, Hofstad O, Feldman HI. Association between renal failure and foot ulcer or lower-extremity amputation in patients with diabetes. Diabetes Care 2008;31:1331–1336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Ndip A, Lavery LA, Boulton AJM. Diabetic foot disease in people with advanced nephropathy and those on renal dialysis. Curr Diab Rep 2010;10:283–290 [DOI] [PubMed] [Google Scholar]
- 78. Serban D, Papanas N, Dascalu AM, et al. Diabetic retinopathy in patients with diabetic foot ulcer: a systematic review. Int J Low Extrem Wounds 2021;20:98–103 [DOI] [PubMed] [Google Scholar]
- 79. Sellman A, Katzman P, Andreasson S, Löndahl M. Presence of chronic diabetic foot ulcers is associated with more frequent and more advanced retinopathy. Diabet Med 2018;35:1364–1370 [DOI] [PubMed] [Google Scholar]
- 80. Zhang Y, Cramb S, McPhail SM, et al.; Diabetic Foot Working Group, Queensland Statewide Diabetes Clinical Network, Australia . Multiple factors predict longer and shorter time-to-ulcer-free in people with diabetes-related foot ulcers: survival analyses of a large prospective cohort followed-up for 24-months. Diabetes Res Clin Pract 2022;185:109239. [DOI] [PubMed] [Google Scholar]
- 81. Ghanassia E, Villon L, Thuan dit Dieudonné JF, Boegner C, Avignon A, Sultan A. Long-term outcome and disability of diabetic patients hospitalized for diabetic foot ulcers. Diabetes Care 2008;31:1288–1292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Hicks CW, Canner JK, Mathioudakis N, et al. The Society for Vascular Surgery Wound, Ischemia, and foot Infection (WIfI) classification independently predicts wound healing in diabetic foot ulcers. J Vasc Surg 2018;68:1096–1103 [DOI] [PubMed] [Google Scholar]
- 83. Petersen BJ, Rothenberg GM, Lakhani PJ, et al. Ulcer metastasis? Anatomical locations of recurrence for patients in diabetic foot remission. J Foot Ankle Res 2020;13:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Huang ZH, Li SQ, Kou Y, Huang L, Yu T, Hu A. Risk factors for the recurrence of diabetic foot ulcers among diabetic patients: a meta-analysis. Int Wound J 2019;16:1373–1382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Lavery LA, Ryan EC, Ahn J, et al. The infected diabetic foot: re-evaluating the Infectious Diseases Society of America diabetic foot infection classification. Clin Infect Dis 2020;70:1573–1579 [DOI] [PubMed] [Google Scholar]
- 86. Rice JB, Desai U, Cummings AKG, Birnbaum HG, Skornicki M, Parsons NB. Burden of diabetic foot ulcers for Medicare and private insurers. Diabetes Care 2014;37:651–658 [DOI] [PubMed] [Google Scholar]
- 87. Fang M, Ishigami J, Echouffo-Tcheugui JB, Lutsey PL, Pankow JS, Selvin E. Diabetes and the risk of hospitalisation for infection: the Atherosclerosis Risk in Communities (ARIC) study. Diabetologia 2021;64:2458–2465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Tan TW, Shih CD, Concha-Moore KC, et al. Disparities in outcomes of patients admitted with diabetic foot infections. PLoS One 2019;14:e0211481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Delcourt C, Orioli L, Maiter D, et al. IDF21-0337 diabetic foot infection and its recurrence: a retrospective study from an academic center in Belgium. Diabetes Res Clin Pract 2022;186:109435 [Google Scholar]
- 90. Hicks CW, Selvarajah S, Mathioudakis N, et al. Burden of infected diabetic foot ulcers on hospital admissions and costs. Ann Vasc Surg 2016;33:149–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Meloni M, Morosetti D, Giurato L, et al. Foot revascularization avoids major amputation in persons with diabetes and ischaemic foot ulcers. J Clin Med 2021;10:3977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Hicks CW, Selvarajah S, Mathioudakis N, et al. Trends and determinants of costs associated with the inpatient care of diabetic foot ulcers. J Vasc Surg 2014;60:1247–1254.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Chatha KK, Walsh B, La Fontaine J, Bowen ME, Meneghini L. Lower-extremity amputation trends among people with diabetes in a large urban environment. Diabetes Care 2021;44:e91–e92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Gasoyan H, Hussain SR, Wright WG, Sarwer DB. Disparities in diabetes-related lower extremity amputations in the United States: a systematic review. Health Aff (Millwood) 2022;41:985–993 [DOI] [PubMed] [Google Scholar]
- 95. Harris RC 3rd, Fang W. Transmetatarsal amputation outcomes when utilized to address foot gangrene and infection: a retrospective chart review. J Foot Ankle Surg 2021;60:269–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Yammine K, Hayek F, Assi C. A meta-analysis of mortality after minor amputation among patients with diabetes and/or peripheral vascular disease. J Vasc Surg 2020;72:2197–2207 [DOI] [PubMed] [Google Scholar]
- 97. Armstrong DG, Swerdlow MA, Armstrong AA, Conte MS, Padula WV, Bus SA. Five year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J Foot Ankle Res 2020;13:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Vuorlaakso M, Kiiski J, Salonen T, Karppelin M, Helminen M, Kaartinen I. Major amputation profoundly increases mortality in patients with diabetic foot infection. Front Surg 2021;8:655902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Hicks CW, Canner JK, Karagozlu H, et al. The Society for Vascular Surgery Wound, Ischemia, and foot Infection (WIfI) classification system correlates with cost of care for diabetic foot ulcers treated in a multidisciplinary setting. J Vasc Surg 2018;67:1455–1462 [DOI] [PubMed] [Google Scholar]
- 100. Fang M, Wang D, Coresh J, Selvin E. Trends in diabetes treatment and control in U.S. adults, 1999-2018. N Engl J Med 2021;384:2219–2228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Paisey RB, Abbott A, Levenson R, et al.; South-West Cardiovascular Strategic Clinical Network peer diabetic foot service review team . Diabetes-related major lower limb amputation incidence is strongly related to diabetic foot service provision and improves with enhancement of services: peer review of the South-West of England. Diabet Med 2018;35:53–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Wang Z, Hazlehurst J, Subramanian A, et al. Diabetic foot risk classification at the time of type 2 diabetes diagnosis and subsequent risk of mortality: a population-based cohort study. Front Endocrinol (Lausanne) 2022;13:888924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Marn Pernat A, Peršič V, Usvyat L, et al. Implementation of routine foot check in patients with diabetes on hemodialysis: associations with outcomes. BMJ Open Diabetes Res Care 2016;4:e000158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Yammine K, Estephan M. Telemedicine and diabetic foot ulcer outcomes. A meta-analysis of controlled trials. Foot 2022;50:101872. [DOI] [PubMed] [Google Scholar]
- 105. Banks JL, Petersen BJ, Rothenberg GM, Jong AS, Page JC. Use of a remote temperature monitoring mat for the early identification of foot ulcers. Wounds 2020;32:44–49 [PubMed] [Google Scholar]
- 106. Scholten HJ, Shih CD, Ma R, Malhotra K, Reyzelman AM. Utilization of a smart sock for the remote monitoring of patients with peripheral neuropathy: cross-sectional study of a real-world registry. JMIR Form Res 2022;6:e32934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Najafi B, Mishra R. Harnessing digital health technologies to remotely manage diabetic foot syndrome: a narrative review. Medicina (Kaunas) 2021;57:377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Vileikyte L, Pouwer F, Gonzalez JS. Psychosocial research in the diabetic foot: are we making progress? Diabetes Metab Res Rev 2020;36(Suppl. 1):e3257. [DOI] [PubMed] [Google Scholar]
- 109. Khunkaew S, Fernandez R, Sim J. Health-related quality of life among adults living with diabetic foot ulcers: a meta-analysis. Qual Life Res 2019;28:1413–1427 [DOI] [PubMed] [Google Scholar]