Abstract
Artificial intelligence (AI) is transforming the practice of medicine. Systems assessing chest radiographs, pathology slides, and early warning systems embedded in electronic health records (EHRs) are becoming ubiquitous in medical practice. Despite this, medical students have minimal exposure to the concepts necessary to utilize and evaluate AI systems, leaving them under prepared for future clinical practice. We must work quickly to bolster undergraduate medical education around AI to remedy this. In this commentary, we propose that medical educators treat AI as a critical component of medical practice that is introduced early and integrated with the other core components of medical school curricula. Equipping graduating medical students with this knowledge will ensure they have the skills to solve challenges arising at the confluence of AI and medicine.
Artificial intelligence (AI) is transforming the practice of medicine. Systems assessing chest radiographs, pathology slides, and early warning systems embedded in electronic health records (EHRs) are becoming ubiquitous in medical practice. Despite this, medical students have minimal exposure to the concepts necessary to utilize and evaluate AI systems, leaving them under prepared for future clinical practice. We must work quickly to bolster undergraduate medical education around AI to remedy this. In this commentary, we propose that medical educators treat AI as a critical component of medical practice that is introduced early and integrated with the other core components of medical school curricula. Equipping graduating medical students with this knowledge will ensure they have the skills to solve challenges arising at the confluence of AI and medicine.
Main text
The promise of artificial intelligence (AI) to aid the practice of medicine has long been a topic of discussion.1 What was once an abstract discussion of the future of medicine is now a clinical reality. Software employing AI is found throughout the clinical care continuum. The US Food and Drug Administration (FDA) has approved over 100 AI software devices.2 The purposes of these software devices range from measuring pulmonary nodules in chest CT scans to detecting different cell types in peripheral blood smears and screening for diabetic retinopathy using photos taken in primary-care settings. However, not all AI systems require FDA approval. Some of the most widely deployed AI systems are early warning systems that fall outside the FDA’s jurisdiction. AI systems for detecting in-hospital deterioration and sepsis are deployed at hundreds of US hospitals.3 The recent increased interest in medical AI is due to the availability of massive amounts of data, facilitated by widespread adoption of electronic health records (EHRs), and advances in AI techniques, driven by a combination of new hardware and computational methods.
Despite the accelerating use of AI in clinical practice, the pace of incorporating AI concepts into medical education has been slow and superficial.4 Only recently has it been proposed that AI concepts be included in medical education curricula.5,6 Most suggestions to date have framed training in AI as an added layer to current medical school curricula, hereafter referred to as undergraduate medical education (UME). Recommendations for incorporating AI into UME range widely, covering the gamut from teaching medical students how to code to EHR usage and the ethics surrounding the adoption of AI.7 However, proposals that treat AI as an additional curricular element or course struggle to gain traction in an overcrowded curriculum. In this commentary, we offer the collective perspective of a medical student, practicing physician, and medical educators. We propose that medical schools view AI as a fundamental component of medical practice and deeply integrate it throughout UME.8
We believe UME must quickly transition to address AI as a fundamental toolset, meaning that it contains many interrelated techniques that underpin the practice of medicine across specialties and care environments. However, the breadth of AI presents a challenge for medical educators seeking to provide a foundation in UME that can be built upon throughout one’s career. AI uses computational methods to process data, from identifying a pattern to generating a prediction or a recommendation. AI can be considered an umbrella term encapsulating many techniques, such as natural language processing and machine learning (ML). Practices from computer science, statistics, decision science, and operations research intersect with AI. These procedures are built upon a foundation of data processing dependent on two types of thinking: computational—being able to provide instructions to computers unambiguously—and statistical—being able to analyze the information derived from processes subject to randomness.
To add to the challenge, like the practice of medicine, the practice of AI is a combination of art and science, as AI systems are components of even larger and more complicated socio-technical systems. Therefore, in addition to technical knowledge, applying AI effectively in clinical practice demands careful consideration of the context, patient values and preferences, ethics, policy, and physician user experiences.
To assist the education community in setting priorities, we present the analytics hierarchy as an approach to stratifying AI methods in terms of complexity and relevance. This hierarchy permits framing of AI as a fundamental toolset of medical practice, which repositions it in medical education. Rather than being treated as an appendiceal element to UME, core concepts in AI should be taught early, built upon longitudinally, and integrated with other core skill sets of medicine. This approach focuses initial training on orientation to the socio-technical context and the core set of technical components that underly AI systems, before introducing educational programming based on specific models (e.g., training on a specific chest X-ray AI system). Empowering medical students with these first principles will enable them to assess and adapt to new AI systems as they are developed. This educational transition will prepare medical trainees to thrive in their future clinical environments, and it will enable clinicians to lead the application of AI to medicine.9,10
In this commentary, we explore what this transition will entail. We define the core concepts of AI as it pertains to medicine and discuss how AI can be presented as a critical skill in UME, akin to learning the fundamentals of anatomy and physiology. For example, medical students rely on their cardiac anatomy and physiology knowledge to identify a patient experiencing congestive heart failure (CHF). Furthermore, they use physical examination skills to identify an S3 (third heart sound) murmur, which may increase their suspicion for CHF. Soon, students may use their knowledge of AI to integrate risk estimates produced by AI systems embedded in the EHR and other points of care to diagnose and treat conditions like CHF.
This transition will require curricular modifications, reprioritizing resources, and analysis of the relationship of AI to existing curricular components of UME. While there is a need for AI educational programming across the medical education continuum, we will focus on opportunities to embed and integrate AI education into UME. Although we cannot predict the extent of AI’s future role in medical practice, we are confident that it will continue to grow in scope and importance in the near future. Therefore, it is imperative that the medical education system act now to introduce and integrate AI concepts into UME.
Employing an analytics hierachy
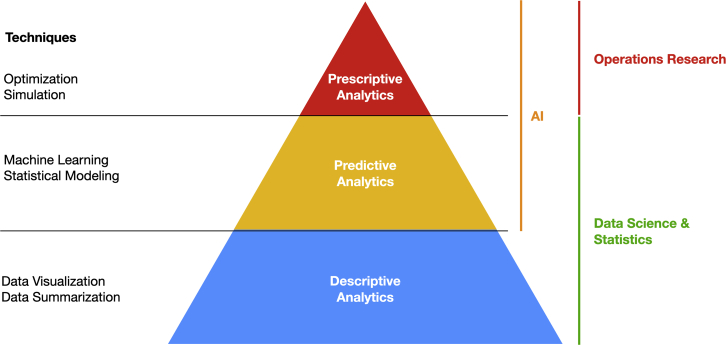
In Figure 1, we depict an example analytics hierarchy. This hierarchy has three tiers, each relating to a function of AI: descriptive analytics, predictive analytics, and prescriptive analytics.11
Figure 1.
An example analytics hierarchy
Adapted from “Descriptive, predictive and prescriptive: Three types of Business Analytics.” The University of Bath.
Descriptive analytics uncover patterns in data. One such line of inquiry might be to use EHR data to understand the relationship between a chemotherapeutic agent and the adverse side effect of nausea. Predictive analytics aim to create informed estimates of future outcomes given available data. An example might include determining which hospitalized patients could be at the highest risk of developing sepsis. Finally, prescriptive analytics attempt to generate recommendations based on known data. Generating resident schedules based on educational and staffing requirements is a task well suited for predictive analytics techniques. These examples are illustrations of analytics concepts; they are not specific UME educational objectives.
The analytics hierarchy is intentionally depicted as a series of stacking layers because understanding the techniques used in the lower layers is foundational knowledge for the higher layers. For a specific curricular example, assessing the effectiveness of an ML model for readmission prediction (a predictive analytics task) might be very difficult for a medical student who has never visualized data (a descriptive analytics task). Additionally, the lower layers contain techniques that are generalizable to other situations and contexts. For example, a conceptual understanding of descriptive analytics could strengthen one’s comprehension of descriptive statistics, a prerequisite for practice of evidence-based medicine (EBM). Relationships between the layers underscore that they are not genuinely distinct but share interrelated concepts and skills.
AI as a fundamental toolset for the practice of medicine
Integrating AI training following the above hierarchy ensures that curricular effort is devoted to essential AI concepts. The hierarchy provides a framework to systematically integrate AI concepts throughout UME across the foundational, clinical, and systems sciences essential to the practice of medicine.
This integrated approach does not entail radically altering or adding substantially to existing UME curriculum. However, it does require careful consideration of our traditional prioritization in UME of the acquisition of knowledge (memorization) over the retrieval, integration, and critical appraisal of information. An initial revamp is necessary to introduce the socio-technical context of AI in medicine; this can be followed by iterative educational changes to adapt to the rapidly evolving AI landscape. An analytics hierarchy ensures that students have a strong foundation early in their pre-clerkship education to build upon throughout the remainder of their training. By emphasizing AI as a fundamental toolset, much of the hierarchy can be introduced using minimally disruptive changes to UME. For example, many of the concepts of descriptive analytics mirror concepts in EBM; EBM curricula could be modified slightly to reinforce connections with descriptive analytics concepts.
Medical educators can leverage the fact that AI plays a prominent role in the foundational, clinical, and systems sciences, underpinning the practice of medicine. Foundational science concepts can be horizontally integrated with core concepts in predictive analytics. For example, pre-clerkship sessions on chest X-ray interpretation might include an overview of how ML works and how a model could be designed to detect pulmonary nodules. This connection presents the opportunity to strengthen the student’s understanding of radiology and AI simultaneously. These connections can also occur vertically and longitudinally. For instance, clerkship training in reading electrocardiographs (ECGs) may include a discussion of the use of automated computer analysis of ECGs.12 Such deep longitudinal integration builds on current clinical practice to prepare medical students for a future of ubiquitous AI.
Using first principles as a scaffolding to build knowledge over subsequent learning opportunities is an important shift from the traditional emphasis on rote memorization toward application and continual self-directed learning over one’s career. We call on medical educators to carefully consider innovative educational methods that will allow students to develop the foundation necessary to become proficient users of AI in clinical practice. We recognize that this will entail effort on the part of educators, and it will require additional support of students. For example, not all matriculating students may have the requisite statistical background to evaluate an ML model. However, this is not dissimilar to other pre-medical concepts. For example, an incoming student with an advanced degree in neuroscience may have an advantage in neuroanatomy compared to another student with a bachelor’s degree in chemical engineering.
Medical educators will need to look to new partners. By collaborating with experts outside of traditional medical education (e.g., data scientists, engineers, and lawyers) and adapting resources that exist in the fields that traditionally teach AI concepts (e.g., computer science, statistics, and industrial engineering), medical educators may be able to build tailored content for UME.
A course for radiology residents has already demonstrated the value of introducing AI training.13 The course connected abstract concepts (such as clustering) to familiar concepts, like movie recommendations. Didactic materials initially focused on first principles that subsequently were used as a scaffold for additional content. First principles were accompanied by discussions about implementing these AI systems and related papers. Creation of this type of course requires both a deep understanding of learner mental models and the fundamentals of AI—still, it is the approach we feel is most likely to succeed.
Treating AI as an essential clinical tool fosters physician ownership of the AI systems used in clinical practice. The evolution of EHRs provides a cautionary tale; since physicians were not active in their design, the resulting EHRs did not satisfactorily meet the needs of patients or physicians. Medical students introduced to AI as a “tool of the trade” will be empowered to improve the AI systems they use daily, which is critical to address concerns about their equity and accuracy.
Providing an early foundation in AI for all students combined with the general trend in UME toward increased elective time,14 will position those students particularly interested in this field to pursue advanced training. Enabling students to address clinical and research problems that they are passionate about will develop a cadre of physicians with deep expertise in AI.
Conclusion
Effectively integrating AI into UME will present some challenges. However, we believe well-organized longitudinal AI curricula based upon an analytical hierarchy will equip all medical students with the knowledge needed to use these techniques competently. Further, we anticipate that framing AI as a toolset will inculcate the perspective that medical students have a significant stake in the application, design, and development of AI devices.
We suggest that AI-related medical education endeavors should anchor on an analytics hierarchy. This would help to organize AI concepts and ensure that students could build upon and connect concepts as they are presented. The hierarchy we presented consists of three levels: descriptive, predictive, and prescriptive analytics. Descriptive analytics help summarize and integrate information. Predictive analytics encapsulate tasks involving estimating unknown information given some known information. Prescriptive analytics provide decision-makers with estimates of what might be the best action to take given a specific scenario. Each of these levels are related to one another and build upon the concepts provided at lower levels.
While a one-size-fits-all approach will not work for all medical students or medical schools, we believe that expertise and resources can be pooled across institutions. Didactic and supplemental materials can be shared and even delivered virtually and asynchronously. Supporting resources for exercises requiring students to apply their developing knowledge, like de-identified datasets and software packages, will be critical and may also be shared. Additionally, students should play a key role in developing portions of this curriculum. Some students may come to medical school already equipped with AI expertise. These students can assist with development of content and provide peer-to-peer guidance.
Our perspective has limitations. Although our vision is tied to the literature and current medical education perspectives, we recognize the many challenges of delivering a high-quality medical education. We broadly define AI, but we suggest narrowly scoping AI training around an analytics hierarchy. There are many pressing issues in UME, however, focusing on the core concepts of AI facilitates integration into existing curricula. We have intentionally avoided discussion of specific AI courses curricular elements. Such a discussion requires a careful definition of competencies and curricular integration points, a conversation beyond this commentary’s scope. Finally, we are a small group, and others in the UME educational community might have different views. Nevertheless, we hope this work will prompt the larger educational community to define desired learning objectives and share best practices.
We believe the time to integrate AI education into UME is now so that physicians have an opportunity to shape an emerging technology. We must do so by treating AI as a fundamental toolset of medical practice, understanding that its core concepts will touch all parts of medicine. Medical curricula should longitudinally integrate AI into the foundational, clinical, and system sciences students learn throughout their UME journey. This approach will prepare medical trainees to thrive in their future practice environments and will enable the medical profession to guide the development and incorporation of AI to the benefit of patients and populations.
Acknowledgments
The opinions expressed in this article are those of the authors and do not necessarily reflect official AMA policy. E.Ö. was supported by grant T32GM007863 from the National Institutes of Health.
Author contributions
Conceptualization: E.Ö. and C.A.J.; writing – original draft: E.Ö.; writing – reviewing and editing: E.Ö., C.A.J., K.D.L., and J.O.W.
Declaration of interests
E.Ö. reports having a patent pending for the University of Michigan for an AI-based approach for the dynamic prediction of health states for patients with occupational injuries.
Inclusion and diversity
One or more of the authors of this paper self-identifies as an underrepresented ethnic minority in their field of research or within their geographical location. We support inclusive, diverse, and equitable conduct of research.
References
- 1.Kulikowski C.A. Beginnings of artificial intelligence in medicine (AIM): computational Artifice assisting Scientific inquiry and clinical art – with Reflections on present AIM challenges. Yearbook of Medical Informatics. 2019-08-01 2019;28:249–256. doi: 10.1055/s-0039-1677895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu E., Wu K., Daneshjou R., Ouyang D., Ho D.E., Zou J. How medical AI devices are evaluated: limitations and recommendations from an analysis of FDA approvals. Nat. Med. 2021-04-01 2021;27:582–584. doi: 10.1038/s41591-021-01312-x. [DOI] [PubMed] [Google Scholar]
- 3.Wong A., Otles E., Donnelly J.P., Krumm A., McCullough J., DeTroyer-Cooley O., Pestrue J., Phillips M., Konye J., Penoza C., et al. External Validation of a widely implemented Proprietary sepsis prediction model in hospitalized patients. JAMA Intern. Med. 2021-06;181:1065–1070. doi: 10.1001/jamainternmed.2021.2626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sapci A.H., Sapci H.A. Artificial intelligence education and tools for medical and health Informatics students: Systematic Review. JMIR Medical Education. 2020-06-30 2020;6 doi: 10.2196/19285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.James C.A., Wheelock K.M., Woolliscroft J.O. Machine learning: the Next Paradigm shift in medical education. Acad. Med. 2021;96:954–957. doi: 10.1097/acm.0000000000003943. [DOI] [PubMed] [Google Scholar]
- 6.Lomis K., Jeffries P., Palatta A., Sage M., Sheikh J., Sheperis C., Whelan A. Artificial intelligence for health professions educators. NAM Perspect. 2021;2021 doi: 10.31478/202109a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee J., Wu A.S., Li D., Kulasegaram K.M. Artificial intelligence in undergraduate medical education: a scoping Review. Acad. Med. 2021;96:S62–S70. doi: 10.1097/acm.0000000000004291. [DOI] [PubMed] [Google Scholar]
- 8.Wartman S.A. Medicine, machines, and medical education. Acad. Med. 2021;96:947–950. doi: 10.1097/acm.0000000000004113. [DOI] [PubMed] [Google Scholar]
- 9.Masters K. Artificial intelligence in medical education. Med. Teach. 2019-09-02 2019;41:976–980. doi: 10.1080/0142159x.2019.1595557. [DOI] [PubMed] [Google Scholar]
- 10.Ooi S.K.G., Makmur A., Soon Y., Fook-Chong S., Liew C., Sia D., Ting Y., Lim C. Attitudes toward artificial intelligence in radiology with learner needs assessment within radiology residency programmes: a national multi-programme survey. Singapore Med J. Mar. 2021;62:126–134. doi: 10.11622/smedj.2019141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Descriptive, Predictive and Prescriptive: Three Types of Business Analytics. The University of Bath. 2022.
- 12.Estes N.M. Computerized interpretation of ECGs. Circulation: Arrhythmia and Electrophysiology. 2013-02-01 2013;6:2–4. doi: 10.1161/circep.111.000097. [DOI] [PubMed] [Google Scholar]
- 13.Lindqwister A.L., Hassanpour S., Lewis P.J., Sin J.M. AI-RADS: an artificial intelligence curriculum for residents. Acad. Radiol. 2021-12-01 2021;28:1810–1816. doi: 10.1016/j.acra.2020.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ngo B., Nguyen D., vanSonnenberg E. Artificial intelligence: has its time come for inclusion in medical school education? Maybe… Maybe not. MedEdPublish. 2021:10. doi: 10.15694/mep.2021.000131.2. [DOI] [PMC free article] [PubMed] [Google Scholar]