Summary
Goal:
The objective of this retrospective, observational study is to assess the mediating effect of medical complexity on the relationship between social vulnerability and four acute care resource use outcomes, specifically numbers of hospitalizations, emergency department (ED) visits, observation stays, and total visits. Such information may help management better anticipate the effects of interventions targeted to the socially vulnerable in their patient population and others.
Methods:
Electronic health record data from 147,496 adults served by 27 primary care practices in one large health system from 2015 to 2017 were used. Descriptive statistics were used to characterize patients and the primary care practices included in the study. Causal mediation analyses using a modified Baron and Kenny approach were performed.
Principal Findings:
Causal mediation analyses demonstrated that increased social vulnerability was associated with increased medical complexity (IRR=1.57), and increased number of hospitalizations (IRR=1.63), ED visits (IRR=2.14), observation stays (IRR=1.94), and total visits (IRR=2.04). Effects remained significant, though attenuated, after adjusting for medical complexity (mediator), demographics, and medications (hospitalizations IRR=1.44; ED visits IRR=2.02; observation stays IRR=1.74; and total visits IRR=1.86). Between 8% (ED visits) and 26% (hospitalizations) of variation in outcomes was explained by social vulnerability, given medical complexity.
Practical Applications:
These findings reinforce the need to modify interventions for medically complex adults to address social needs and, consequently, reduce use of costly health services. Health systems seeking to reduce the use of costly care can use these results to estimate savings in the treatment of patients with high social vulnerability—both before they get chronic conditions and afterwards as they seek care.
Introduction
Healthcare systems responsible for population health are increasingly challenged to reduce the effects of social vulnerability that contribute to adverse health outcomes among disadvantaged groups that may lead to avoidable resource use. System managers need to know the extent that social vulnerability matters in order to better target interventions. This paper describes a method to obtain more nuanced information about the effects of social vulnerability by illustrating different mechanisms by which it can affect health and cost of vulnerable subgroups in a population served by a large healthcare system. Causal mediation analysis can be a novel tool for managers to measure the potential effectiveness of interventions targeted at pathways through which social vulnerability affects acute care resource use.
It is widely documented that social vulnerability (Registry, 2018) influences healthcare outcomes, including acute care resource utilization (Hatef et al., 2020; Hu et al., 2019; Tsou, 2018). Social vulnerability is commonly assessed by level of education, income, employment status, living arrangements, and community characteristics (Flanagan et al., 2018; Spielman et al., 2020; Tsou, 2018). High-risk behaviors such as tobacco and substance abuse, obesity, and depression are more common among socially vulnerable individuals (Domènech-Abella et al., 2018; Seid et al., 2018; Tsuchiya et al., 2021). Prior studies have shown that socially vulnerable individuals are more likely to have limited health insurance, and thus reduced access to primary care, which leads to increased reliance on acute care services for healthcare, including the emergency department (ED) (Kim et al., 2017; Krieg et al., 2016). The presence of multiple chronic conditions and disease progression has also been linked to increased acute healthcare utilization and costs (Frølich et al., 2019; Okunrintemi et al., 2019; Rosella et al., 2018). Challenges in managing complex symptoms and therapies are major contributors to higher service use for people with multiple health problems (Bress et al., 2016; Skinner et al., 2016).
While relationships between social vulnerability or medical complexity and acute care resource use have been explored, limited research (Cho et al., 2008) focuses on examining the mediating effect of medical complexity on the relationship between social vulnerability and acute care resource use. It is hypothesized that a significant proportion of the observed gap in acute care resource use by social vulnerability status can be attributed to differences in medical complexity. Evidence that the relationship between social vulnerability and resource use is mediated by medical complexity will support the design of interventions to address the root causes of poor complexity management. Among those with complex conditions, targeted social solutions can enable more effective management of complex health problems.
Mediation analysis is used to identify causal pathways between an exposure and an outcome, through an intermediate variable posited to mediate the relationship between the two. Causal mediation analysis (Heckman & Pinto, 2015; Liu et al., 2016; Naimi et al., 2016; Nguyen et al., 2020; Zhang et al., 2016) is a method that dissects the total effect of an exposure into controlled direct and mediated effects. The controlled mediated effect is transmitted to the outcome by way of the mediator. This type of analysis is helpful in targeting modifiable characteristics, or potential areas for intervention, by determining the causal mechanisms between an exposure and the outcome of interest.
Methods
Design, Sample and Setting
This is a retrospective observational study of adult (≥18 years), non-pregnant patients who sought care from one of 27 primary care practices within a single urban academic health center.
Data
Patient characteristics
Electronic health record (EHR) data were requested for all patients from 2015 to 2017. Variables requested were based on a literature review of health and social factors influencing the care and outcomes of adult patients, with refinement by primary care clinical scholars and members of a Stakeholder Advisory Group. Baseline patient characteristic data from 2015 serve as the basis for this study; in situations where 2015 data are unavailable, 2016 or 2017 data were used.
Site characteristics
Primary care practice data from 2017 were obtained, including the number of: full-time employees, full-time advanced practice providers, actual visits, and active patients.
Health Resource Use
EHR data were used to capture number of hospitalizations, ED visits, and observation stays (i.e., outpatient observation status with health care monitoring, usually <48 hours) during 2017. An event was only counted once in the appropriate category—hospitalization, ED visit, or observation stay. Acute care resource data were limited to events that took place within the hospitals of the participating health system.
Predictor of Interest
Derived for each patient was a 2016 Social Vulnerability Index (SVI) (Registry, 2018), a metric used by the Center for Disease Control (CDC) to rank census tracts on 15 social factors that may weaken the ability of that tract’s population to respond to major health and social threats. These 15 factors are placed into four SVI themes (Socioeconomic Status, Household Composition & Disability, Minority Status & Language, and Housing & Transportation), and averaged to create an overall score for each census tract (Flanagan et al., 2011). The SVI overall and theme scores range from 0 to 1, with higher scores reflecting a more vulnerable community. For this analysis, a weighted SVI that corresponded to the zip code of the patient’s current address was derived with steps included as Supplemental Digital Content (see Supplemental Digital Content 1). Although SVI has only been validated as a predictive measure of damages and fatalities after a natural disaster (Bakkensen et al., 2017), this measure has also been used to examine its association with health outcomes, such as obesity (An, 2015) and hospice utilization (Abbas et al., 2020). To the best of our knowledge, no studies have utilized the CDC’s SVI as a measure of social vulnerability that may influence healthcare utilization.
Mediator
The mediator examined is medical complexity defined by the number of CMS Hierarchical Condition Categories (HCCs) measured at the patient level (CMS, 2018). To increase reliability, the number of HCCs from primary care and specialist visits in 2015 and 2016 were averaged for each patient.
Outcomes
Acute care resource use outcomes included: number of hospitalizations (primary), emergency department (ED) visits, observation stays, and total number of hospitalizations, ED visits, and observations stays during 2017 (all secondary). To support causal inference, temporality is purposefully incorporated into this study by using patient characteristics measured in 2015 to predict outcomes observed in 2017.
Statistical Analyses
The objective of this study was to assess the mediating effect of medical complexity, as measured by the number of HCCs (count variable), on the relationship between social vulnerability (assessed on a continuum by overall SVI) and acute care resource use at the patient level (all count outcome variables). Preliminary analyses included generating descriptive statistics for patient demographic and health status characteristics, overall and by SVI group (SVI>0.5–1 vs. SVI 0–0.5). Comparisons by SVI group relied on two-sample t-tests and chi-square statistics for continuous and categorical characteristics, respectively. Cohen’s d and Cramer’s V effect sizes were generated to facilitate comparisons across SVI groups for clinically meaningful differences (medium or larger effect sizes) (Cohen, 1988).
For the current study, the methods of Baron and Kenny (Baron & Kenny, 1986) to conduct mediation analysis by multiple linear regression were generalized to negative binomial regression to properly accommodate the count mediator and outcome variables. Per these methods, three negative binomial models were generated for each acute care resource use outcome and adjusted for demographics, number of prescribed medications, and primary care site characteristics: (1) outcome regressed on SVI, (2) mediator (number of HCCs) regressed on SVI, and (3) outcome regressed on SVI when controlling for number of HCCs.
Using estimates from the negative binomial models, the incidence rate ratio (IRR) of the controlled direct and mediated effects were then computed by “controlling” the exposure (by fixing SVI to 0) or the mediator (by fixing number of HCCs to its expected value given that SVI is 0), and taking the ratio of expected counts under each model. In calculating each IRR, potential confounders were fixed to their observed means, as only the marginal effects of the exposure (SVI) and mediator (number of HCCs) were of interest. Additionally, the percentage of the total effect mediated was derived as the absolute value of log-IRR estimate for the controlled mediated effect divided by the sum of the absolute value of the log-IRR estimates for the controlled mediated and direct effects. As the percent mediated is a function of multiple parameters from both the mediator and outcome models, bootstrapping was used to obtain empirical 95% quantile-based confidence intervals.
Using Baron and Kenny’s guidelines (Baron & Kenny, 1986), the presence of mediation was inferred when: SVI was found to be a statistically significant predictor of the outcome, and of HCCs, after adjusting for potential measured confounders; and the proportion of the total effect accounted for by the controlled mediated effect was statistically significantly different from zero. Full mediation was demonstrated when the SVI estimate was no longer statistically significant after adjusting for HCCs; partial mediation was established when the SVI estimate remained statistically significant after adjusting for HCCs.
Because of the concern that suburban patients might use out-of-system hospitals, sensitivity analyses were performed using the eight urban sites located closest to the health system’s hospitals (N=62,232). Finally, recognizing that overall SVI is made up of four distinct themes, additional analyses were performed using the methods described above to examine which SVI themes were driving any significant findings. Statistical significance was taken at the 0.05 level. Descriptive analyses were conducted using SAS V9.4 (SAS Institute Inc., Cary, NC) and mediation analyses were performed via the ‘MASS’ package in R V3.6.
Results
Demographic and Health Status Characteristics
Descriptive statistics are provided in Table 1, overall and by SVI group. Specifically, EHR data from 147,496 patients with 803,939 visits (primary care and specialist) from 2017 who were affiliated with the 27 practices in urban (N=8) and suburban (N=19) settings were used in this analysis.
Table 1.
Demographic and Health Status Characteristics of Patients Served by 27 Primary Care Sites in a Large Urban Health System (N = 147,496 patients*)
| Characteristic | Overall (N = 147,496) | Low SVI [0–0.5] (N = 96,702) | High SVI [>0.5–1.0] (N = 50,794) | p-value | Effect Size‡ | |||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Mean (SD) or Patient count | Median (Q1, Q3) or Percent | Mean (SD) or Patient count | Median (Q1, Q3) or Percent | Mean (SD) or Patient count | Median (Q1, Q3) or Percent | |||
| Age (years) | 52.80 (17.28) | 54 (39, 66) | 53.69 (17.08) | 55 (41, 66) | 51.11 (17.52) | 52 (37, 64) | <0.0001 | 0.15 |
| Female | 89,696 | 60.8% | 55,380 | 57.3% | 34,316 | 67.6% | <0.0001 | 0.10 |
| Non-White | 56,129 | 38.1% | 18,680 | 19.3% | 37,449 | 73.7% | <0.0001 | 0.53 |
| Non-English speaker | 3,417 | 2.3% | 2,168 | 2.2% | 1,249 | 2.5% | 0.0085 | 0.01 |
| Overall Social Vulnerability Index (SVI) | 0.41 (0.25) | 0.32 (0.19, 0.71) | 0.24 (0.11) | 0.23 (0.17, 0.32) | 0.72 (0.11) | 0.74 (0.66, 0.79) | - | - |
| 0.00–0.25 | 59,139 | 40.1% | 59,139 | 61.2% | 0 | 0 | - | - |
| >0.25–0.50 | 37,563 | 25.5% | 37,563 | 38.8% | 0 | 0 | ||
| >0.50–0.75 | 33,128 | 22.5% | 0 | 0 | 33,128 | 65.2% | ||
| >0.75–1.00 | 17,666 | 12.0% | 0 | 0 | 17,666 | 34.8% | ||
| SVI Theme 1: Socioeconomic Status | 0.40 (0.28) | 0.29 (0.17, 0.70) | 0.22 (0.13) | 0.19 (0.12, 0.29) | 0.75 (0.14) | 0.79 (0.70, 0.83) | - | - |
| 0.00–0.25 | 63,430 | 43.0% | 63,426 | 65.6% | 4 | <0.1% | - | - |
| >0.25–0.50 | 33,804 | 22.9% | 27,771 | 28.7% | 6,033 | 11.9% | ||
| >0.50–0.75 | 18,419 | 12.5% | 5,505 | 5.7% | 12,914 | 25.4% | ||
| >0.75–1.00 | 31,843 | 21.6% | 0 | 0 | 31,843 | 62.7% | ||
| SVI Theme 2: Household Composition & Disability | 0.39 (0.22) | 0.32 (0.21, 0.58) | 0.26 (0.13) | 0.25 (0.19, 0.32) | 0.63 (0.15) | 0.64 (0.49, 0.73) | - | - |
| 0.00–0.25 | 48,301 | 32.7% | 48,122 | 49.8% | 179 | 0.4% | - | - |
| >0.25–0.50 | 55,276 | 37.5% | 42,753 | 44.2% | 12,523 | 24.7% | ||
| >0.50–0.75 | 32,538 | 22.1% | 5,750 | 5.9% | 26,788 | 52.7% | ||
| >0.75–1.00 | 11,381 | 7.7% | 77 | 0.1% | 11,304 | 22.3% | ||
| SVI Theme 3: Minority Status & Language | 0.50 (0.18) | 0.49 (0.34, 0.67) | 0.41 (0.13) | 0.38 (0.32, 0.49) | 0.69 (0.10) | 0.68 (0.64, 0.74) | - | - |
| 0.00–0.25 | 8,994 | 6.1% | 8,780 | 9.1% | 214 | 0.4% | - | - |
| >0.25–0.50 | 65,908 | 44.7% | 65,278 | 67.5% | 630 | 1.2% | ||
| >0.50–0.75 | 61,356 | 41.6% | 21,404 | 22.1% | 39,952 | 78.7% | ||
| >0.75–1.00 | 11,238 | 7.6% | 1,240 | 1.3% | 9,998 | 19.7% | ||
| SVI Theme 4: Housing & Transportation | 0.45 (0.17) | 0.46 (0.35, 0.55) | 0.39 (0.16) | 0.37 (0.30, 0.47) | 0.57 (0.14) | 0.54 (0.46, 0.63) | - | - |
| 0.00–0.25 | 20,103 | 13.6% | 19,167 | 19.8% | 936 | 1.8% | - | - |
| >0.25–0.50 | 72,350 | 49.1% | 55,373 | 57.3% | 16,977 | 33.4% | ||
| >0.50–0.75 | 48,238 | 32.7% | 21,470 | 22.2% | 26,768 | 52.7% | ||
| >0.75–1.00 | 6,805 | 4.6% | 692 | 0.7% | 6,113 | 12.0% | ||
| Number of medications per patient | 3.38 (3.75) | 2 (1, 5) | 2.85 (3.15) | 2 (1, 4) | 4.39 (4.53) | 3 (1, 6) | <0.0001 | 0.42 |
| 0 | 28,135 | 19.1% | 20,704 | 21.4% | 7,431 | 14.6% | <0.0001 | 0.18 |
| 1 – 5 | 89,975 | 61.0% | 61,409 | 63.5% | 28,566 | 56.2% | ||
| 6 – 10 | 21,593 | 14.6% | 11,586 | 12.0% | 10,007 | 19.7% | ||
| 11 or more | 7,793 | 5.3% | 3,003 | 3.1% | 4,790 | 9.4% | ||
| Number of HCCs per patient | 0.75 (1.23) | 0 (0, 1) | 0.62 (1.08) | 0 (0, 1) | 0.99 (1.43) | 0 (0, 2) | <0.0001 | 0.30 |
| 0 | 87,904 | 59.6% | 61,549 | 63.6% | 26,355 | 51.9% | ||
| 1 | 32,568 | 22.1% | 20,907 | 21.6% | 11,661 | 23.0% | ||
| 2 | 14,476 | 9.8% | 8,240 | 8.5% | 6,236 | 12.3% | ||
| 3 | 6,537 | 4.4% | 3,275 | 3.4% | 3,262 | 6.4% | ||
| 4+ | 6,011 | 4.1% | 2,731 | 2.8% | 3,280 | 6.5% | ||
| Number of Primary Care visits per patient | 2.73 (2.19) | 2 (1, 4) | 2.65 (2.16) | 2 (1, 3) | 2.87 (2.25) | 2 (1, 4) | <0.0001 | 0.10 |
| Number of Specialist visits per patient | 2.72 (5.78) | 1 (0, 3) | 2.29 (5.18) | 0 (0, 3) | 3.55 (6.69) | 1 (0, 4) | ||
| Number of patients with at least one hospitalization | 7,822 | 5.3% | 3,991 | 4.1% | 3,831 | 7.5% | ||
| Number of hospitalizations per patient (n = 7,822) | 1.46 (1.08) | 1 (1, 2) | 1.40 (0.97) | 1 (1, 1) | 1.52 (1.19) | 1 (1, 2) | <0.0001 | 0.11 |
| 1 | 5,761 | 73.7% | 3,035 | 76.0% | 2,726 | 71.2% | <0.0001 | 0.06 |
| 2 | 1,292 | 16.5% | 616 | 15.4% | 676 | 17.6% | ||
| 3 | 421 | 5.4% | 190 | 4.8% | 231 | 6.0% | ||
| 4+ | 348 | 4.4% | 150 | 3.8% | 198 | 5.2% | ||
| Average length of hospital stay per patient (days) | 5.03 (5.82) | 4 (2, 6) | 4.82 (5.19) | 3 (2, 6) | 5.25 (6.41) | 4 (2, 6) | 0.0013 | 0.07 |
| Number of patients with at least one ED visit | 14,353 | 9.7% | 5,824 | 6.0% | 8,529 | 16.8% | <0.0001 | 0.17 |
| Number of ED visits per patient (n = 14,353) | 1.47 (1.70) | 1 (1, 2) | 1.34 (1.46) | 1 (1, 1) | 1.56 (1.84) | 1 (1, 2) | <0.0001 | 0.13 |
| 1 | 10,699 | 74.5% | 4,678 | 80.3% | 6,021 | 70.6% | <0.0001 | 0.12 |
| 2 | 2,351 | 16.4% | 784 | 13.5% | 1,567 | 18.4% | ||
| 3 | 709 | 4.9% | 221 | 3.8% | 488 | 5.7% | ||
| 4+ | 594 | 4.1% | 141 | 2.4% | 453 | 5.3% | ||
| Number of patients with at least one observation stay | 2,851 | 1.9% | 1,168 | 1.2% | 1,683 | 3.3% | <0.0001 | 0.07 |
| Number of observation (OBS) stays per patient (n = 2,851) | 1.27 (0.70) | 1 (1, 1) | 1.19 (0.57) | 1 (1, 1) | 1.32 (0.77) | 1 (1, 1) | <0.0001 | 0.19 |
| 1 | 2,309 | 81.0% | 1,003 | 85.9% | 1,306 | 77.6% | <0.0001 | 0.10 |
| 2 | 397 | 13.9% | 124 | 10.6% | 273 | 16.2% | ||
| 3 | 99 | 3.5% | 29 | 2.5% | 70 | 4.2% | ||
| 4+ | 46 | 1.6% | 12 | 1.0% | 34 | 2.0% | ||
| Number of patients with at least one hospitalization, ED visits, or OBS stays | 20,938 | 14.2% | 9,378 | 9.7% | 11,560 | 22.8% | <0.0001 | 0.18 |
| Number of hospitalizations, ED visits, and OBS stays per patient (n = 20,938) | 1.73 (1.91) | 1 (1, 2) | 1.58 (1.62) | 1 (1, 2) | 1.85 (2.10) | 1 (1, 2) | <0.0001 | 0.14 |
| 1 | 13,762 | 65.7% | 6,616 | 70.5% | 7,146 | 61.8% | <0.0001 | 0.10 |
| 2 | 3,969 | 19.0% | 1,618 | 17.3% | 2,351 | 20.3% | ||
| 3 | 1,538 | 7.3% | 604 | 6.4% | 934 | 8.1% | ||
| 4+ | 1,669 | 8.0% | 540 | 5.8% | 1,129 | 9.8% | ||
This represents the total number of patients who had at least one encounter (PCP or specialist) or resource use episode (hospitalization, home healthcare visit, hospice visit, ED visit or observation stay) in 2017. Among these patients, 7,822 patients had at least one hospitalization.
Effect sizes are based on Cohen’s d (small: 0.20–0.49, medium: 0.50–0.80, large: >0.80) for continuous variables and Cramer’s V (small: 0.10–0.39, medium: 0.40–0.50, large: >0.50) for categorical variables. Note: Higher SVI scores indicate greater vulnerability of the community. HCCs = Hierarchical Condition Categories; Q1 = 25th percentile; Q3 = 75th percentile.
Patients were primarily female (61%), with a mean age of 53 years. Social vulnerability, as reflected in SVI overall scores, ranged from 12% living in a zip code with the highest vulnerability (>0.75–1.0) to 40% living in a zip code with the lowest vulnerability (0–0.25). The mean and median overall SVI score was 0.41 and 0.32, respectively. Thirty-eight percent of the patients were non-white, with 19% and 74% non-white among those with lower and higher social vulnerability, respectively. The median number of medications prescribed per patient was 2 overall, and 2 and 3 for those with lower and higher vulnerability, respectively. The mean and median number of HCCs per patient was 0.75 and 0, respectively, with the mean number of HCCs per patient among those with lower and higher social vulnerability equal to 0.6 and 1.0, respectively. Five percent of eligible patients (N=7,822) had at least one hospitalization, 10% had at least one ED visit, and 2% had an observation stay in 2017.
Site Characteristics
Characteristics of the 27 primary care sites are summarized in Table 2. Median number of active patients was 8,930 with a median number of 16,748 visits. The median number of full-time employees and advanced practice providers were 4 and 1.5, respectively.
Table 2.
Characteristics of 27 Primary Care Sites in a Large Urban Health System
| Characteristic (N = 27) | Mean (SD) | Median (Q1, Q3) | Range (Min, Max) |
|---|---|---|---|
| Number of Full-time Employees | 5.94 (4.81) | 4.01 (2.90, 7.09) | (1, 22) |
| Number of Full-time Advanced Practice Providers | 1.63 (1.44) | 1.50 (0.76, 2.00) | (0, 5.75) |
| FY17 Actual Visit Volume | 18,349.26 (10,007.88) | 16,748.00 (11,367.00, 22,103.00) | (5,496.00, 50,565.00) |
| Total Active Patients | 9,758.26 (5,625.28) | 8,930.00 (5,181.00, 12,921.00) | (2,537.00, 27,444.00) |
Note: FY17 = Fiscal Year 2017; SD = Standard Deviation; Q1 = 25th percentile; Q3 = 75th percentile; Min = Minimum; Max = Maximum.
Mediating Effects of Number of HCCs
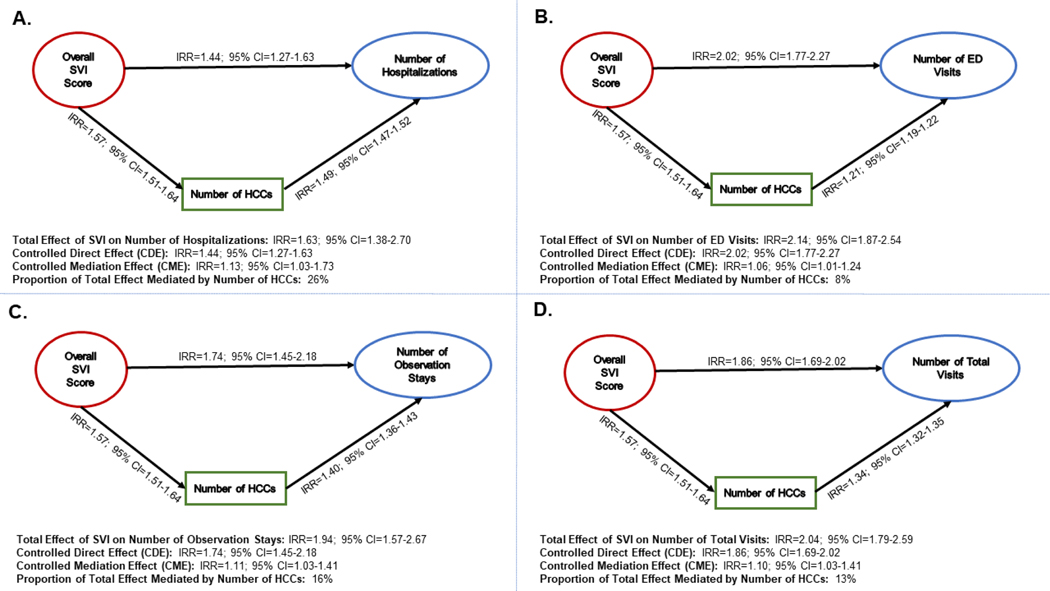
Table 3 provides a summary of the mediation analyses, with visualizations shown in Figure 1. When number of HCCs are not considered (total effect), the adjusted IRRs for SVI and the four acute care resource use outcomes range from 1.63 for hospitalizations to 2.14 for ED visits. When adjusting for number of HCCs as a potential mediator (the controlled direct effect), the adjusted IRRs for SVI were attenuated, but remained statistically significant, for all outcomes (ranging from 1.44 for hospitalizations to 2.02 for ED visits) and thus support partial mediation in all models. The percentage of the total effect of overall SVI on acute care resource use explained by the number of HCCs ranged from 8% to 26%. Specifically, 8% of the total SVI effect on number of ED visits can be explained by the number of HCCs, whereas 26% of the total SVI effect on number of hospitalizations can be explained by the number of HCCs.
Table 3.
Mediation Model Effects* for Resource Use Outcomes: Primary and Sensitivity Analyses
| Dependent Variable (# of) | Predictor | Effect | Primary Analysis (N = 147,496) | Sensitivity Analysis** (N = 62,232) | ||
|---|---|---|---|---|---|---|
|
| ||||||
| IRR | 95% CI | IRR | 95% CI | |||
| HCCs | Overall SVI | Effect of Overall SVI on HCCs | 1.57 | (1.51, 1.64) | 1.35 | (1.28, 1.43) |
| Hospitalizations | Overall SVI | Direct effect of Overall SVI on hospitalizations | 1.44 | (1.27, 1.63) | 1.63 | (1.36, 1.95) |
| Effect of HCCs on hospitalizations | 1.49 | (1.47, 1.52) | 1.48 | (1.45, 1.51) | ||
| Effect of Overall SVI on hospitalizations mediated by HCCs | 1.13 | (1.03, 1.73) | 1.10 | (1.02, 1.59) | ||
| Total effect of Overall SVI on hospitalizations | 1.63 | (1.38, 2.70) | 1.79 | (1.47, 2.55) | ||
| Proportion of total effect mediated | 0.26 | (0.07, 0.63) | 0.16 | (0.04, 0.50) | ||
| ED Visits | Overall SVI | Direct effect of Overall SVI on ED visits | 2.02 | (1.77, 2.27) | 3.01 | (2.65, 3.55) |
| Effect of HCCs on ED visits | 1.21 | (1.19, 1.22) | 1.18 | (1.16, 1.20) | ||
| Effect of Overall SVI on ED visits mediated by HCCs | 1.06 | (1.01, 1.24) | 1.04 | (1.01, 1.18) | ||
| Total effect of Overall SVI on ED visits | 2.14 | (1.87, 2.54) | 3.13 | (2.69, 3.89) | ||
| Proportion of total effect mediated | 0.08 | (0.02, 0.26) | 0.03 | (0.01, 0.13) | ||
| Observation Stays | Overall SVI | Direct effect of Overall SVI on observation stays | 1.74 | (1.45, 2.18) | 2.63 | (1.98, 3.52) |
| Effect of HCCs on observation stays | 1.40 | (1.36, 1.43) | 1.38 | (1.34, 1.42) | ||
| Effect of Overall SVI on observation stays mediated by HCCs | 1.11 | (1.03, 1.41) | 1.08 | (1.02, 1.53) | ||
| Total effect of Overall SVI on observation stays | 1.94 | (1.57, 2.67) | 2.84 | (2.17, 4.44) | ||
| Proportion of total effect mediated | 0.16 | (0.05, 0.37) | 0.07 | (0.02, 0.29) | ||
| Total Visits | Overall SVI | Direct effect of Overall SVI on total visits | 1.86 | (1.69, 2.02) | 2.54 | (2.23, 2.82) |
| Effect of HCCs on total visits | 1.34 | (1.32, 1.35) | 1.30 | (1.29, 1.32) | ||
| Effect of Overall SVI on total visits mediated by HCCs | 1.10 | (1.03, 1.41) | 1.06 | (1.02, 1.31) | ||
| Total effect of Overall SVI on total visits | 2.04 | (1.79, 2.59) | 2.70 | (2.33, 3.54) | ||
| Proportion of total effect mediated | 0.13 | (0.04, 0.37) | 0.06 | (0.02, 0.22) | ||
Note: HCCs = Hierarchical Condition Categories based on yearly average from 2015–2016; SVI: Social Vulnerability Index; IRR: Incidence Rate Ratio; CI: Confidence Interval.
All models adjusted for demographic characteristics (age on a continuum, gender, race, language), number of prescribed medications, and primary care site characteristics (number of: full-time employees, full-time advanced practice providers, actual visits, active patients).
Sensitivity analyses were performed using only 8 sites located in communities where patients are more likely to use hospitals in the participating urban health system.
Figure 1.
Mediation model effects of number of Hierarchical Condition Categories (HCCs) on the relationship between overall Social Vulnerability Index (SVI) and resource use outcomes (A-D for hospitalizations, ED visits, observation stays, and total visits), Primary analyses
Similar mediation analyses and visualizations for the four SVI themes are provided as Supplemental Digital Content (see Table and Figures, Supplemental Digital Content 2-6, which include results for the effect of SVI themes on acute care resource use outcomes). Partial mediation was observed for three of the four SVI themes, where the percentage of the total effect of SVI themes on acute care resource use explained by the number of HCCs ranged from 2% to 22%. Specifically, 2% of the total SVI Housing & Transportation theme effect on number of ED visits can be explained by the number of HCCs, whereas 22% of the total SVI Socioeconomic Status theme effect on number of hospitalizations can be explained by number of HCCs. No mediation was observed for total SVI Household Composition & Disability theme effect on any of the four outcomes.
Discussion
The goal of this study was to examine medical complexity as a potential mediating pathway through which social vulnerability impacts costly healthcare resource use. Findings reveal that increased social vulnerability (assessed via the overall SVI score) demonstrates an increase in medical complexity (assessed via number of HCCs), while increased social vulnerability and medical complexity were independently associated with increased acute care resource use. The causal mediation analysis models showed that medical complexity partially mediates the effect of social vulnerability on acute care resource use with 26% of the overall effect of social vulnerability on number of hospitalizations mediated by medical complexity.
To the best of our knowledge, only one other study has examined the mediating role of health status on the relationship between social vulnerability and acute care resource use. Specifically, Cho et al. examined the mediating role of health status on the relationship between health literacy and healthcare utilization (Cho et al., 2008). Using path analysis, health literacy demonstrated significant direct effects on resource use outcomes (i.e., hospitalizations and ED visits) among 489 older adults (≥65 years); however, no significant mediation of health status was observed. Of note, Cho and colleagues used both self-reported health status (measured on a 5-point Likert scale) and healthcare utilization outcomes collected via face-to-face interviews. This current study extends that work by using a larger, broader sample (147,496 adults ≥18 years old), and also by capturing health status (assessed via number of HCCs) and four resource use outcomes (number of: hospitalizations, ED visits, observation stays, and total visits) using EHR data.
The impact of social vulnerability on heath care costs may be considered through two pathways, the controlled mediated effect (CME) and the controlled direct effect (CDE). To illustrate, consider the effect of social vulnerability on the number of hospitalizations during a particular time period. As shown in Figure 1A, the total effect of social vulnerability on hospitalizations is estimated to be 1.63; specifically, the number of hospitalizations increases by 5% for every 0.1-unit (computed as 1.630.1=1.05) increase in social vulnerability. The mediation analysis quantifies the degree to which hospitalizations resulting from social vulnerability are due to the medical complexities that also result from social vulnerability. This CME through medical complexity (IRR=1.13) demonstrates a 1% increase in the number of hospitalizations for every 0.1-unit increase in social vulnerability (computed as 1.130.1=1.01). Stated differently, the CME estimates how much social vulnerability affects hospitalizations if it only did so by increasing medical complexity. For example, a 0.1-unit increase in social vulnerability corresponded with a 1% increase in the number of hospitalizations by way of increases in medical complexity. If there was an innovative care management strategy that could be applied to a population with complex chronic conditions, with varying levels of social vulnerability, approximately 26% [computed as log(1.13)/log(1.63)] of the total effect of social vulnerability on hospitalizations could be impacted by the new intervention. Health systems could design services to address the root cause of the individual’s barriers to effective care management such as transportation for patients who miss provider appointments, or nurse-led models to engage high-risk patients in improving self-care via focus on individual patient goals (Hirschman et al., 2015).
The other pathway through which social vulnerability impacts resource use is through its CDE, which quantifies the magnitude of outcome change from differing levels of SVI, while holding the number of HCCs at a constant level (IRR=1.44). In this study, the CDE of social vulnerability on hospitalizations is quantified by an 4% increase in the number of hospitalizations for every 0.1-unit increase in overall SVI (computed as 1.440.1=1.04). This CDE relationship constitutes 75% [computed as log(1.44)/log(1.63)] of the total effect. This information can help predict the impact of a care management strategy to mitigate the effect of social vulnerability, and how and when those effects will be manifested. If a strategy can lead to more effective care of people already ill with chronic conditions by identifying the root causes of acute exacerbations, clinically meaningful reductions in hospitalizations could be achieved. For example, if a hospitalization is caused by symptom exacerbation due to the patient’s failure to take medications as prescribed, identifying and correcting the root cause is critical. Patients who suffer from clinical depression that interferes with complex self management are different from those who cannot afford to pay for the medications that they are willing to take. When supported by complementary strategies that aim to prevent vulnerability-related chronic conditions from arising in the first place (e.g., availability of healthy food resources in a neighborhood, smoking cessation programs), care management strategies will likely have a meaningful effect on hospitalizations.
These study findings should be interpreted within the context of acknowledged limitations. The first of these relates to reliance on data documented in the EHR, the limitations of which have been widely reported in the literature (Agniel et al., 2018; Casey et al., 2016; Leonard et al., 2017). For example, EHR data reflect information collected for billing purposes, not research. Additionally, analyses are restricted to available data and are notoriously incomplete, leaving the modeling vulnerable to bias from unmeasured confounding variables.
Individual-level data such as socioeconomic status or education level were not readily available; to address this limitation, a publicly available neighborhood-level measure such as the CDC’s SVI was used. The assignment of a neighborhood-level measure to an individual has been shown to be valid and performed as well or better than individual-level variables (Carmichael et al., 2019; Kind & Buckingham, 2018). Further, the CDC’s SVI has shown to be advantageous over more commonly used indices of social deprivation or vulnerability, such as the Area Deprivation Index (ADI), given the SVI’s four themes in addition to an overall score that can be used to identify specific aspects of social vulnerability that can be targeted via interventions (Carmichael et al., 2019; Kind & Buckingham, 2018).
Given the focus on medical complexity, note that information on health and chronic conditions was based on ICD-10 diagnoses at the encounter during the specific time frame examined, and may not necessarily represent existing chronic conditions. It is also important to note that the mediating role of medical complexity may be driven by the operationalization of medical complexity with number of HCCs. The use of a higher dimensional measure of medical complexity may provide a stronger path between social vulnerability and acute care resource use.
Additionally, data were limited to only reported hospitalizations within the participating academic health system. Some primary care sites in this system are situated closer to non-affiliated hospitals in which their patients likely seek emergent care; data from non-affiliated hospitals were not available. To mitigate this limitation, sensitivity analyses were conducted using only eight sites located in communities where patients were more likely to use hospitals within the participating systems. Similar to mediation results in the primary analysis, the sensitivity analysis showed that 16% of the total effect for hospitalizations is mediated by number of HCCs. Results from the sensitivity analysis are provided in Table 3 and Supplemental Digital Content 7. Additional limitations arising from the study data include the inability to generalize these results to non-urban health systems.
Finally, care must be taken when interpreting causal mediation model results. The modeling assumes no unmeasured confounders that may explain the associations are observed between social vulnerability and resource use outcomes. As mentioned above, this is also a limitation of using observational EHR data for research purposes. Additionally, reverse causality is a valid concern, where medical complexity may lead to social vulnerability, which in turn may increase resource use. In this study, we believe that reverse causality is less of a concern, given the temporal nature of the data modeled (patient-level covariates from 2015 and 2016 when possible, SVI representing zip code level metrics from 2016, and acute care resource use observed in 2017), coupled with the aggregate measure of social vulnerability at the zip code level (rather than individual level) being less likely to demonstrate a reverse relationship.
Despite these limitations and pending validation from additional research, findings suggest that medical complexity may be added to the list of previously established mediators linking social vulnerability to resource use, including behavioral and lifestyle factors, social and environmental exposures, and healthcare access and quality.
Deepening our knowledge of the underlying pathways between social vulnerability and acute care resource use, the mediating role of medical complexity may have important implications for care management interventions focused on reducing health disparities, as medical complexity may be more easily modified than social vulnerability. Additionally, policies that expand health coverage for managing populations with complex conditions or that address modifiable social challenges such as increased access to transportation may effectively advance health equity.
Future research should include additional sources of data to confirm resource use outcomes, comparing performance of the SVI with other publicly available indices, along with an examination of moderators that may include specific patient subpopulations, potentially strengthening the mediating role of medical complexity in various demographic and health domains. Lastly, this study should be expanded by future work to include an examination of multiple mediators (behavioral and lifestyle factors, social and environmental exposures, healthcare access and quality) linking social vulnerability to resource use and placing medical complexity with the broader context of previously established mediators.
Conclusion
If confirmed in future studies, these findings provide insight into the underlying mechanisms by which social vulnerability contributes to resource use, and also suggests that medically complex socially vulnerable individuals may serve as a target of novel policies and clinical interventions to reduce health disparities. Additionally, these results could contribute valuable information on the effectiveness of interventions targeted at socially vulnerable patients to health system managers weighing the costs and benefits of such interventions. Thus, a thorough investigation and deep understanding of medical complexity (i.e., using large datasets from multiple sources, advanced data science methods combined with sophisticated statistical models) as a mediator of the relationship between social vulnerability and acute care resource use will be critical to contextualize, tailor and optimize public health efforts targeted at reducing health inequalities. Given the limited research in this area, future studies might consider potential moderators of these pathways, multidimensional measures of medical complexity, and refined acute care resource use outcomes.
Supplementary Material
ACKNOWLEDGEMENTS
The authors acknowledge Kevin L. McKee, PhD for his contributions generating and interpreting the causal mediation analyses in R.
Research reported in this publication was supported in part by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR003015. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Support was also provided by the NewCourtland Center for Transitions and Health at the University of Pennsylvania School of Nursing and the Perelman School of Medicine Center for Therapeutic Effectiveness Research.
Footnotes
CONFLICTS OF INTEREST AND SOURCE OF FUNDING The authors have no conflicts of interest to declare.
References
- Abbas A, Madison Hyer J, & Pawlik TM (2020). Race/Ethnicity and County-Level Social Vulnerability Impact Hospice Utilization Among Patients Undergoing Cancer Surgery. Annals of Surgical Oncology. 10.1245/s10434-020-09227-6 [DOI] [PubMed]
- Agniel D, Kohane IS, & Weber GM (2018). Biases in electronic health record data due to processes within the healthcare system: retrospective observational study. BMJ, 361, k1479. 10.1136/bmj.k1479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- An R, Xiang X. (2015). Social vulnerability and obesity among U.S. Adults. Int J Health Sci, 3, 7–21. [Google Scholar]
- Bakkensen LA, Fox-Lent C, Read LK, & Linkov I. (2017). Validating Resilience and Vulnerability Indices in the Context of Natural Disasters. Risk Anal, 37(5), 982–1004. 10.1111/risa.12677 [DOI] [PubMed] [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol, 51(6), 1173–1182. 10.1037//0022-3514.51.6.1173 [DOI] [PubMed] [Google Scholar]
- Bress AP, King JB, Brixner D, Kielhorn A, Patel HK, Maya J, Lee VC, Biskupiak J, & Munger M. (2016). Pharmacotherapy Treatment Patterns, Outcomes, and Health Resource Utilization Among Patients with Heart Failure with Reduced Ejection Fraction at a U.S. Academic Medical Center [ 10.1002/phar.1701]. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy, 36(2), 174–186. 10.1002/phar.1701 [DOI] [PubMed] [Google Scholar]
- Carmichael H, Moore A, Steward L, & Velopulos CG (2019). Using the Social Vulnerability Index to Examine Local Disparities in Emergent and Elective Cholecystectomy. Journal of Surgical Research, 243, 160–164. 10.1016/j.jss.2019.05.022 [DOI] [PubMed] [Google Scholar]
- Casey JA, Schwartz BS, Stewart WF, & Adler NE (2016). Using Electronic Health Records for Population Health Research: A Review of Methods and Applications. Annual review of public health, 37, 61–81. 10.1146/annurev-publhealth-032315-021353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho YI, Lee SY, Arozullah AM, & Crittenden KS (2008). Effects of health literacy on health status and health service utilization amongst the elderly. Soc Sci Med, 66(8), 1809–1816. 10.1016/j.socscimed.2008.01.003 [DOI] [PubMed] [Google Scholar]
- CMS. (2018). Medicare Advantage Rates & Statistics. Retrieved April 10 from https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Risk-Adjustors
- Cohen J. (1988). Statistical Power Analysis for the Behavioral Sciences (2nd Edition ed.). Routledge. [Google Scholar]
- Domènech-Abella J, Mundó J, Leonardi M, Chatterji S, Tobiasz-Adamczyk B, Koskinen S, Ayuso-Mateos JL, & Haro JM (2018). The association between socioeconomic status and depression among older adults in Finland, Poland and Spain: A comparative cross-sectional study of distinct measures and pathways. Journal of Affective Disorders, 241, 311–318. 10.1016/j.jad.2018.08.077 [DOI] [PubMed] [Google Scholar]
- Flanagan BE, Gregory EW, & Hallisey EJ (2011). A Social Vulnerability Index for Disaster Management. Journal of Homeland Security and Emergency Management, 8(1), 0000102202154773551792. 10.2202/1547-7355.1792 [DOI] [Google Scholar]
- Flanagan BE, Hallisey EJ, Adams E, & Lavery A. (2018). Measuring Community Vulnerability to Natural and Anthropogenic Hazards: The Centers for Disease Control and Prevention’s Social Vulnerability Index. Journal of environmental health, 80(10), 34–36. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7179070/ [PMC free article] [PubMed] [Google Scholar]
- Frølich A, Ghith N, & Schiøtz M. (2019). Multimorbidity, healthcare utilization and socioeconomic status: A register-based study in Denmark. PloS one, 14(8), e0214183-e0214183. 10.1371/journal.pone.0214183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatef E, Ma X, Rouhizadeh M, Singh G, Weiner JP, & Kharrazi H. (2020). Assessing the Impact of Social Needs and Social Determinants of Health on Health Care Utilization: Using Patient- and Community-Level Data. Population Health Management. 10.1089/pop.2020.0043 [DOI] [PMC free article] [PubMed]
- Heckman JJ, & Pinto R. (2015). Econometric Mediation Analyses: Identifying the Sources of Treatment Effects from Experimentally Estimated Production Technologies with Unmeasured and Mismeasured Inputs. Econometric Reviews, 34(1–2), 6–31. 10.1080/07474938.2014.944466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschman KB, Shaid E, McCauley K, Pauly MV, & Naylor MD (2015). Continuity of Care: The Transitional Care Model. Online J Issues Nurs, 20(3), 1. [PubMed] [Google Scholar]
- Hu Y, Leinonen T, van Hedel K, Myrskylä M, & Martikainen P. (2019). The relationship between living arrangements and higher use of hospital care at middle and older ages: to what extent do observed and unobserved individual characteristics explain this association? BMC Public Health, 19(1), 1011-1011. 10.1186/s12889-019-7296-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim TJ, Vonneilich N, Lüdecke D, & von dem Knesebeck O. (2017). Income, financial barriers to health care and public health expenditure: A multilevel analysis of 28 countries. Social Science & Medicine, 176, 158–165. 10.1016/j.socscimed.2017.01.044 [DOI] [PubMed] [Google Scholar]
- Kind AJH, & Buckingham WR (2018). Making Neighborhood-Disadvantage Metrics Accessible — The Neighborhood Atlas. New England Journal of Medicine, 378(26), 2456–2458. 10.1056/NEJMp1802313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieg C, Hudon C, Chouinard M-C, & Dufour I. (2016). Individual predictors of frequent emergency department use: a scoping review. BMC Health Services Research, 16(1), 594. 10.1186/s12913-016-1852-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard CE, Brensinger CM, Nam YH, Bilker WB, Barosso GM, Mangaali MJ, & Hennessy S. (2017). The quality of Medicaid and Medicare data obtained from CMS and its contractors: implications for pharmacoepidemiology. BMC Health Services Research, 17(1), 304-304. 10.1186/s12913-017-2247-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S, Ulbricht CM, & Chrysanthopoulou SA (2016). Implementation and reporting of causal mediation analysis in 2015: a systematic review in epidemiological studies. BMC Res Notes 9, 354. 10.1186/s13104-016-2163-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naimi AI, Schnitzer ME, & Moodie EE (2016). Mediation Analysis for Health Disparities Research. Am J Epidemiol, 184(4), 315–324. 10.1093/aje/kwv329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen TQ, Schmid I, & Stuart EA (2020). Clarifying causal mediation analysis for the applied researcher: Defining effects based on what we want to learn. Psychological Methods, No Pagination Specified-No Pagination Specified. 10.1037/met0000299 [DOI] [PMC free article] [PubMed]
- Okunrintemi V, Valero-Elizondo J, Michos ED, Salami JA, Ogunmoroti O, Osondu C, Tibuakuu M, Benson E-M, Pawlik TM, Blaha MJ, & Nasir K. (2019). Association of Depression Risk with Patient Experience, Healthcare Expenditure, and Health Resource Utilization Among Adults with Atherosclerotic Cardiovascular Disease. Journal of General Internal Medicine, 34(11), 2427–2434. 10.1007/s11606-019-05325-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- OPD&R. (2020). HUD USPS ZIP Code Crosswalk Files. Retrieved September 11, 2020 from https://www.huduser.gov/portal/datasets/usps_crosswalk.html#codebook
- Registry, A. f. T. S. a. D. (2018). CDC’s Social Vulnerability Index (SVI). Retrieved April 30 from https://svi.cdc.gov
- Rosella LC, Kornas K, Yao Z, Manuel DG, Bornbaum C, Fransoo R, & Stukel T. (2018). Predicting High Health Care Resource Utilization in a Single-payer Public Health Care System: Development and Validation of the High Resource User Population Risk Tool. Medical care, 56(10), e61–e69. 10.1097/MLR.0000000000000837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seid AK, Bloomfield K, & Hesse M. (2018). The relationship between socioeconomic status and risky drinking in Denmark: a cross-sectional general population study. BMC Public Health, 18, 743. 10.1186/s12889-018-5481-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner HG, Coffey R, Jones J, Heslin KC, & Moy E. (2016). The effects of multiple chronic conditions on hospitalization costs and utilization for ambulatory care sensitive conditions in the United States: a nationally representative cross-sectional study. BMC Health Services Research, 16(1), 77. 10.1186/s12913-016-1304-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielman SE, Tuccillo J, Folch DC, Schweikert A, Davies R, Wood N, & Tate E. (2020). Evaluating social vulnerability indicators: criteria and their application to the Social Vulnerability Index. Natural Hazards, 100(1), 417–436. 10.1007/s11069-019-03820-z [DOI] [Google Scholar]
- Tsou M-T (2018). Healthcare Service Utilization and Associated Factors in Community-Dwelling Elderly in Northern Taiwan: One Medical Center’s Experience. International Journal of Gerontology, 12(2), 144–149. 10.1016/j.ijge.2018.02.015 [DOI] [Google Scholar]
- Tsuchiya C, Furusawa T, Tagini S, & Nakazawa M. (2021). Socioeconomic and Behavioral Factors Associated with Obesity Across Sex and Age in Honiara, Solomon Islands. Hawai’i journal of health & social welfare, 80(2), 24–32. https://pubmed.ncbi.nlm.nih.gov/33575662 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7871455/ [PMC free article] [PubMed] [Google Scholar]
- Wilson R, & Din A. (2018). Understanding and Enhancing the U.S. Department of Housing and Urban Development’s ZIP Code Crosswalk Files. Cityscape, 20(2), 277–294. https://www.jstor.org/stable/26472179 [Google Scholar]
- Zhang Z, Zheng C, & Kim C. (2016). Causal mediation analysis in the context of clinical research. Ann Transl Med, 4(21), 425. 10.21037/atm.2016.11.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.