Abstract
Objective:
Research on effects of pregnancy termination on women’s alcohol, tobacco, and other drug (ATOD) use suffers from methodological and conceptual problems. Improving on prior methodologies, this study examines changes in ATOD use over 5 years among women seeking terminations.
Method:
Data are from the Turnaway Study, a longitudinal study of 956 women seeking terminations at 30 U.S. facilities. Participants presented just below a facility’s gestational limit and received terminations (Near-Limits) or just beyond the limit and were denied terminations (Turnaways). Using mixed-effects logistic regression, we assessed differences in ATOD use over 5 years among Near-Limits and Turnaways.
Results:
There were no differences in ATOD use before pregnancy recognition; 1 week after termination seeking, Turnaways had lower odds than Near-Limits of any and heavy episodic alcohol use (p < .001), but not alcohol problem symptoms, tobacco use, or other drug use. Although both groups increased in any alcohol use over time, Turnaways increased more rapidly. Neither group increased any other ATOD measures over time. Turnaways’ lower odds of heavy episodic alcohol use at 1 week after termination seeking were maintained throughout the subsequent 5 years. There was no differential change in problem alcohol use or in tobacco or other drug use over time, yet fewer Turnaways than Near-Limits reported problem alcohol symptoms 6 months through 3.5 years.
Conclusions:
There is no indication that terminating a pregnancy led women to increase heavy episodic or problem alcohol use or to increase tobacco or other drug use. Women denied terminations had temporary or sustained reductions in all alcohol measures, but not tobacco or other drugs, suggesting that relationships between pregnancy/parenting and ATOD differ across substances.
Since the 1980s, physical and mental health effects of abortion have been central to advocacy for and against abortion rights worldwide (Center for Reproductive Rights, 2005; Wilmoth, 1992). In the United States, the mental health effects of abortion—including alcohol, tobacco, and other drug (ATOD) misuse—have remained a focal point of anti-abortion rights advocacy (Americans United for Life, 2016). Numerous studies and rigorous reviews about mental health effects have been published and generally conclude that there is no evidence that abortion causes women to develop mental health or ATOD use disorders (Charles et al., 2008; Koop, 1989; Major et al., 2009; Robinson et al., 2009). Some research has found higher levels of ATOD use and use disorders among women having abortions compared with women who give birth, have miscarriages, or who have not had a previous pregnancy (Coleman et al., 2002, 2005; Dingle et al., 2008; Fergusson et al., 2008; Major et al., 2009; Olsson et al., 2014; Pedersen, 2007; Steinberg & Finer, 2011). It is unclear, however, whether these higher levels are attributable to increases among women having abortions, decreases among women choosing to continue a pregnancy, or women with higher levels of ATOD use or use disorders being more likely to decide to terminate an unintended pregnancy.
Previous research about mental health effects of abortion has a number of methodological flaws. These include abortion under-reporting, not accounting for pre-pregnancy mental health or substance use, and using inappropriate comparison groups, such as women who have never been pregnant or who had a wanted pregnancy (Major et al., 2009; Steinberg & Finer, 2011). To address the major methodological concerns, in 1989 the U.S. Surgeon General recommended a prospective cohort study design that dealt with the problem of abortion under-reporting and compared women who had an abortion with women who carried to delivery or had a miscarriage (Koop, 1989). The U.S. Turnaway Study is a 5-year prospective cohort study that recruits women seeking abortion, some who receive abortions and some who are denied abortions and then carry to term, and thus conforms to those recommendations.
In addition to broader mental health (Biggs et al., 2015, 2016, 2017; Foster et al., 2015), the Turnaway Study includes assessment of ATOD use and alcohol misuse. We have published mid-study (2- to 2.5-year) findings for ATOD use (Roberts & Foster, 2015; Roberts et al., 2014, 2015, 2016). We found that women who had abortions had higher levels of any alcohol use, heavy episodic alcohol use, and tobacco use over 2 to 2.5 years than women denied abortions, but these differences were attributable to reductions among women denied (Roberts & Foster, 2015; Roberts et al., 2015), not increases among women receiving, abortions. We did not find differences in potential alcohol problem symptoms (eye-opener or blackout) or in drug use between groups (Roberts et al., 2014, 2015). We also did not find evidence that having abortions increased heavy episodic alcohol, problem alcohol, tobacco, or drug use or that differences in heavy episodic alcohol use between groups were explained by stress or negative emotions about the pregnancy (Roberts & Foster, 2015; Roberts et al., 2014, 2015, 2016). Together, these findings indicate that—over 2 to 2.5 years—women continuing unwanted pregnancies reduce/cease some, but not all, substance use, whereas women who have abortions tend to continue substance use patterns from before their abortions. Here, we extend previous work by examining whether these ATOD findings persist over the study’s entire 5-year period. Examining ATOD use over longer periods is important because some have argued that adverse mental health effects of having an abortion may emerge years later (Kelly, 2014).
Method
Data sources
Data come from the Turnaway Study, a 5-year prospective cohort study of 956 women seeking abortions across the United States. Study details have been published (Dobkin et al., 2014; Gould et al., 2012; Roberts et al., 2014; Upadhyay et al., 2014). The study received ethical approval from the University of California, San Francisco Institutional Review Board.
Between January 2008 and December 2010, we recruited participants from 30 abortion facilities throughout the United States. Eligible participants were English- and Spanish-speaking women age 15 or older, with no known fetal anomalies or demise, presenting at a facility within the gestational range of one of three study groups. The three groups included (a) Near-Limit-Abortions: presented for abortion within 2 weeks under a facility’s gestational limit for providing abortion and received abortions; (b) Turnaways: presented up to 3 weeks over a facility’s limit and were denied abortions; (c) First-Trimester Abortions: received abortions any time in the first trimester under the facility’s limit. Groups were recruited in a 2:1:1 ratio. We recruited twice the number of Near-Limits because we anticipated that fewer would meet criteria for Turnaways and we wanted an adequate sample. Turnaways versus Near-Limits was the main comparison; First-Trimesters were included because Near-Limits received abortions later than typical in the United States, where 90% of abortions occur in the first trimester (Pazol et al., 2013) and we wanted to examine whether Near-Limits’ experiences were typical.
We chose facilities with the latest gestational limit for providing abortions within 150 miles. Gestational limits vary according to state laws and provider factors (e.g., training, institutional limits, and staff preferences). Facilities had limits from 10 weeks through the end of the second trimester. Of facilities recruited, all but two agreed to participate. A facility with an identical gestational limit, the same catchment area, and similar patient volume replaced one that declined.
Data collection
Participants completed 11 semi-annual telephone interviews over 5 years. Participants were recruited and consented at the abortion-seeking visit. The baseline interview occurred 1 week after abortion seeking.
Participation
Of all eligible women approached, 1,132 (37.5%) consented to participate in the longitudinal study, and of these, 84.5% (n = 956) completed the baseline interview, a mean of 26 per site. There were no statistically significant differences in age or gestational age between those who consented and those who completed the baseline interview (Dobkin et al., 2014). Near-Limits and Turnaways (main study groups) did not differ in participation rates, although fewer women eligible for First-Trimesters participated (Dobkin et al., 2014). Of the 956, 452 were Near-Limits, 231 Turnaways, and 273 First-Trimesters. All participants from one facility—with a 10-week gestational limit and where more than 90% of Turnaways received an abortion elsewhere after being denied (n = 76)—were excluded from analyses. One First-Trimester and two Near-Limits later reported that they had not had the abortion and were excluded from analyses. The final sample comprised 413 Near-Limits, 210 Turnaways, and 254 First-Trimesters.
Women in the study who had abortions were similar to women having abortions in the United States in general in terms of age, race, and parity (Finer & Zolna, 2011). Because of study design, fewer women having abortions had abortions in the first trimester than is typical in the United States (Pazol et al., 2013).
Measures
Outcomes included at each interview were past-month any alcohol use, heavy episodic alcohol use (more than five drinks at a time), potential alcohol problem symptom (eye-opener, blackout, or both), tobacco use, and drug use, all dichotomous. At the first interview, approximately 1 week after abortion seeking, women were asked about past-month use and use the month before pregnancy discovery; tobacco the month before pregnancy discovery was excluded. To better measure alcohol use, additional questions were added at the 4- and 5-year interviews: (a) TWEAK (tolerance, withdrawal, eye-opener, amnesia, and kut down), which identifies risky drinking patterns, typically among pregnant women (dichotomous: scores two or higher considered positive; Chang, 2001); and (b) volume (continuous: using indexing; Armor & Polich, 1982), based on past-month frequency, usual quantity, and number of 6+ occasions. To account for left skew in volume because of the preponderance of zeros and lower volumes, we restricted analyses to those who had consumed one or more drinks and used the natural log of (volume +1) as the outcome.
Main independent variables were study group, time (years), and Study Group × Time interactions. Study group is categorical: Near-Limits; Turnaway-Births (Turnaways who had a live birth, including 15 who placed their baby for adoption); Turnaway-No-Births (50 Turnaways who miscarried or received an abortion elsewhere); and First-Trimesters. We used Near-Limits as the reference so we could simultaneously compare experiences of Turnaway-Births and First-Trimesters with Near-Limits. Years was a continuous variable of years since recruitment. Study Group × Year interaction terms refer to group-specific use trajectories compared with Near-Limits, our reference group.
Covariates were measured at baseline. They included age in years (continuous), race (categorical: White, Black, Hispanic/Latina, multiracial/other), parity/recent birth (categorical: nulliparous [no previous live births]; past-year birth; one, no past-year birth; two or more, no past-year birth), marital status (categorical: single, married, separated/divorced); employed (dichotomous: employed part or full time vs. not), child abuse/neglect (dichotomous: physical abuse, neglect, and/or sexual abuse during childhood), and history of depression/anxiety (dichotomous: previous depression or anxiety diagnosis).
Retention
Of the 956 participants who completed the baseline interview, 58% were still in the study at 5 years. Of substance use variables, only any alcohol before pregnancy recognition was associated with loss to follow-up, with fewer who abstained in the study at 5 years. Although there were no differences in loss to follow-up by study group through the 10th interview, in the final 11th interview, Turnaway-Births (51%) were marginally less likely (p = .053) than Near-Limits (60%) to participate.
Analysis
Analyses were conducted using Stata Version 14.0 (Stata-Corp LP, College Station, TX). We used mixed-effects linear, logistic, and multinomial logistic regression to assess differences in baseline characteristics between Near-Limits and other groups, accounting for clustering within facilities.
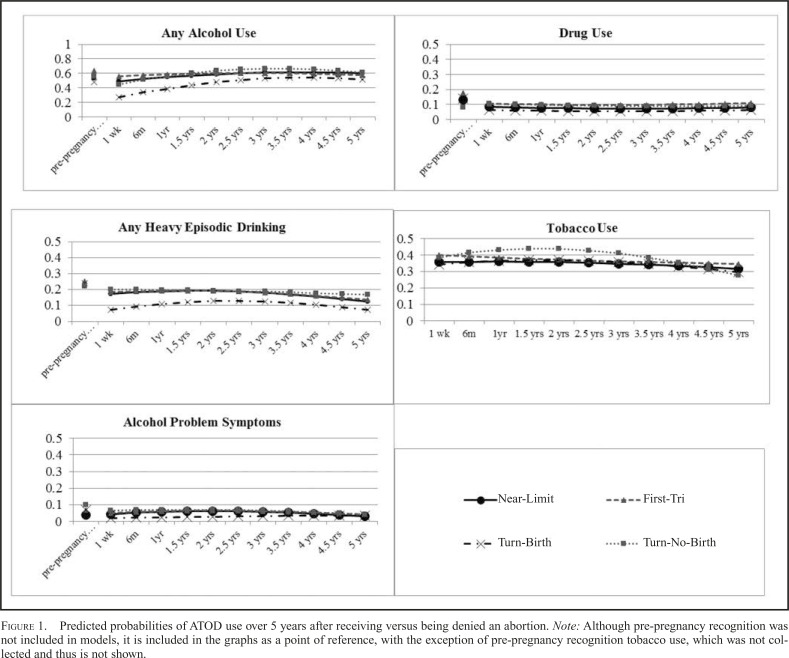
Longitudinal analyses using mixed-effects logistic regression then examined associations between study group and trajectories in ATOD use over 5 years. All available data from the 11 interviews were used. The maximum likelihood methods we used to fit the models provide consistent estimation of parameters of interest in settings where data are missing at random (Little & Rubin, 2002). Data about use the month before the first interview (rather than before pregnancy recognition) were the first time point. To account for clustering, random intercepts for facilities and individuals were used. When a significant (p < .05) likelihood ratio test indicated they improved model fit, random coefficients for individuals and quadratic terms for time were retained. To aid in model interpretation, we graphed population-average predicted probabilities based on model output. Graphs comparing outcomes are included as Figure 1. Using a series of post-estimation tests, we estimated study group differences at each 6-month study interval for each outcome and assessed whether trajectories changed over time or differed by study group.
Figure 1.
Predicted probabilities of ATOD use over 5 years after receiving versus being denied an abortion. Note: Although pre-pregnancy recognition was not included in models, it is included in the graphs as a point of reference, with the exception of pre-pregnancy recognition tobacco use, which was not collected and thus is not shown.
We included covariates we expected might influence ATOD use during and after pregnancy and baseline covariates that differed at p < .10 between Near-Limits and any other group. Gestational age, by study design, determined study group and thus was excluded from models.
To analyze volume and TWEAK outcomes (collected only at 4- and 5-year interviews), we used mixed-effects linear and logistic regressions to examine associations between study group and outcomes at each interview. We also assessed whether TWEAK findings were robust to our modeling decision by using a mixed-effects negative binomial regression; substantive findings did not differ.
Because there was some indication of differential loss to follow-up by the final (5-year) interview, we conducted a sensitivity analysis, removing the final two interviews and repeating all longitudinal analyses.
Results
Sample description
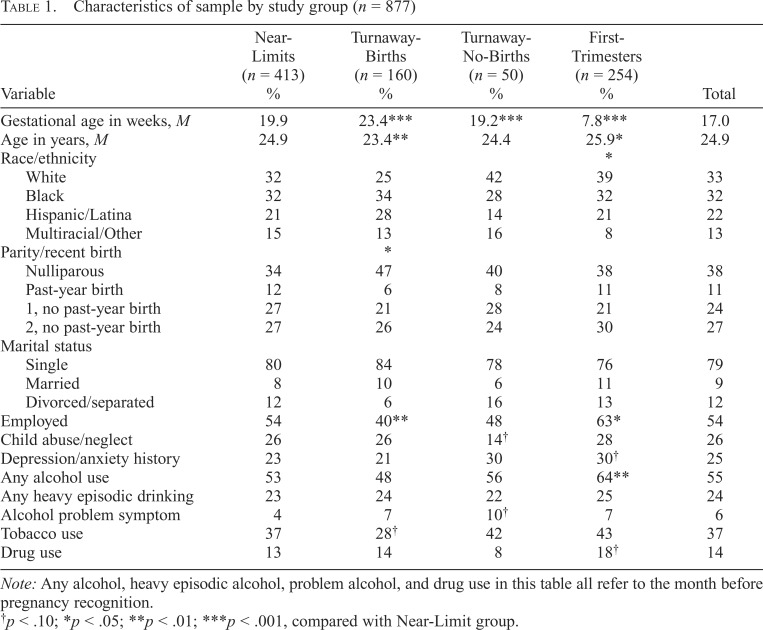
Participants were racially/ethnically diverse; about one third were White, one third Black, and 22% Hispanic/Latina (Table 1). On average, they were 25 years old and sought abortions at 17 weeks gestation. Almost two thirds had had a previous birth, with 11% having given birth in the previous year. Few (<10%) were currently married, and a little more than half were employed. About one fourth reported history of child abuse/neglect and about one fourth a history of depression/anxiety. More than half reported drinking any alcohol the month before pregnancy recognition, and about one fourth reported heavy episodic drinking, 6% an alcohol problem symptom, and 14% drug use. Almost 40% reported smoking the month before seeking abortion.
Table 1.
Characteristics of sample by study group (n = 877)
| Variable | Near-Limits (n = 413) % | Turnaway-Births (n = 160) % | Turnaway-No-Births (n = 50) % | First- Trimesters (n = 254) % | Total |
| Gestational age in weeks, M | 19.9 | 23.4*** | 19.2*** | 7.8*** | 17.0 |
| Age in years, M | 24.9 | 23.4** | 24.4 | 25.9* | 24.9 |
| Race/ethnicity | * | ||||
| White | 32 | 25 | 42 | 39 | 33 |
| Black | 32 | 34 | 28 | 32 | 32 |
| Hispanic/Latina | 21 | 28 | 14 | 21 | 22 |
| Multiracial/Other | 15 | 13 | 16 | 8 | 13 |
| Parity/recent birth | * | ||||
| Nulliparous | 34 | 47 | 40 | 38 | 38 |
| Past-year birth | 12 | 6 | 8 | 11 | 11 |
| 1, no past-year birth | 27 | 21 | 28 | 21 | 24 |
| 2, no past-year birth | 27 | 26 | 24 | 30 | 27 |
| Marital status | |||||
| Single | 80 | 84 | 78 | 76 | 79 |
| Married | 8 | 10 | 6 | 11 | 9 |
| Divorced/separated | 12 | 6 | 16 | 13 | 12 |
| Employed | 54 | 40** | 48 | 63* | 54 |
| Child abuse/neglect | 26 | 26 | 14† | 28 | 26 |
| Depression/anxiety history | 23 | 21 | 30 | 30† | 25 |
| Any alcohol use | 53 | 48 | 56 | 64** | 55 |
| Any heavy episodic drinking | 23 | 24 | 22 | 25 | 24 |
| Alcohol problem symptom | 4 | 7 | 10† | 7 | 6 |
| Tobacco use | 37 | 28† | 42 | 43 | 37 |
| Drug use | 13 | 14 | 8 | 18† | 14 |
Note: Any alcohol, heavy episodic alcohol, problem alcohol, and drug use in this table all refer to the month before pregnancy recognition.
p < .10;
p < .05;
p < .01;
p < .001, compared with Near-Limit group.
Baseline differences across study groups
There were few statistically significant differences at the p < .05 level at baseline. Turnaway-Births were younger and First-Trimesters older than Near-Limits. Fewer Turnaway-Births had a previous birth and fewer Turnaway-Births were employed than Near-Limits. First-Trimesters differed from Near-Limits in race/ethnicity. By study design, there were differences in gestational age between groups.
As reported previously (Roberts et al., 2014, 2015), there were no statistically significant differences in any alcohol use, heavy episodic drinking, problem symptoms, or drug use the month before pregnancy recognition between Turnaway-Births and Near-Limits, although more First-Trimesters than Near-Limits reported any alcohol use.
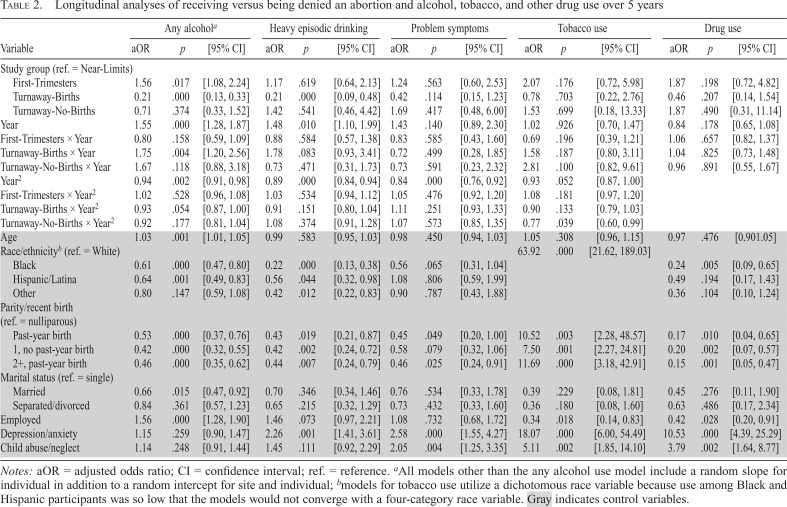
Longitudinal analyses of Turnaway-Births versus Near-Limits
One week after abortion seeking, Turnaway-Births had lower odds of any and heavy episodic alcohol use (reduction by Turnaway-Births) but not problem symptoms, tobacco use, or drug use compared with Near-Limits (Table 2 and Figure 1). Although both Turnaway-Births and Near-Limits increased any alcohol use over 5 years, Turnaway-Births increased more rapidly. The difference in any alcohol use between Turnaway-Births and Near-Limits 1 week post–termination seeking (Turnaway-Births still pregnant, Near-Limits not) was maintained throughout 5 years. Neither Turnaway-Births nor Near-Limits increased heavy episodic drinking, alcohol problem symptoms, tobacco use, or drug use over the 5 years (Table 2 and Figure 1). The difference in heavy episodic drinking between Turnaway-Births and Near-Limits at 1 week was maintained throughout the 5 years. There were no statistically significant differences in change over time in alcohol problem symptoms, tobacco use, or drug use over the 5 years between Turnaway-Births and Near-Limits (Table 2). Yet, fewer Turnaway-Births than Near-Limits reported problem symptoms from 6 months through 3.5 years, indicating a temporary reduction in problem symptoms among Turnaway-Births from before pregnancy recognition to 6 months through about 3 years postpartum (Table 2 and Figure 1).
Table 2.
Longitudinal analyses of receiving versus being denied an abortion and alcohol, tobacco, and other drug use over 5 years
| Any alcohola |
Heavy episodic drinking |
Problem symptoms |
Tobacco use |
Drug use |
|||||||||||
| Variable | aOR | p | [95% CI] | aOR | p | [95% CI] | aOR | p | [95% CI] | aOR | p | [95% CI] | aOR | p | [95% CI] |
| Study group (ref. = Near-Limits) | |||||||||||||||
| First-Trimesters | 1.56 | .017 | [1.08, 2.24] | 1.17 | .619 | [0.64, 2.13] | 1.24 | .563 | [0.60, 2.53] | 2.07 | .176 | [0.72, 5.98] | 1.87 | .198 | [0.72, 4.82] |
| Turnaway-Births | 0.21 | .000 | [0.13, 0.33] | 0.21 | .000 | [0.09, 0.48] | 0.42 | .114 | [0.15, 1.23] | 0.78 | .703 | [0.22, 2.76] | 0.46 | .207 | [0.14, 1.54] |
| Turnaway-No-Births | 0.71 | .374 | [0.33, 1.52] | 1.42 | .541 | [0.46, 4.42] | 1.69 | .417 | [0.48, 6.00] | 1.53 | .699 | [0.18, 13.33] | 1.87 | .490 | [0.31, 11.14] |
| Year | 1.55 | .000 | [1.28, 1.87] | 1.48 | .010 | [1.10, 1.99] | 1.43 | .140 | [0.89, 2.30] | 1.02 | .926 | [0.70, 1.47] | 0.84 | .178 | [0.65, 1.08] |
| First-Trimesters × Year | 0.80 | .158 | [0.59, 1.09] | 0.88 | .584 | [0.57, 1.38] | 0.83 | .585 | [0.43, 1.60] | 0.69 | .196 | [0.39, 1.21] | 1.06 | .657 | [0.82, 1.37] |
| Turnaway-Births × Year | 1.75 | .004 | [1.20, 2.56] | 1.78 | .083 | [0.93, 3.41] | 0.72 | .499 | [0.28, 1.85] | 1.58 | .187 | [0.80, 3.11] | 1.04 | .825 | [0.73, 1.48] |
| Turnaway-No-Births × Year | 1.67 | .118 | [0.88, 3.18] | 0.73 | .471 | [0.31, 1.73] | 0.73 | .591 | [0.23, 2.32] | 2.81 | .100 | [0.82, 9.61] | 0.96 | .891 | [0.55, 1.67] |
| Year2 | 0.94 | .002 | [0.91, 0.98] | 0.89 | .000 | [0.84, 0.94] | 0.84 | .000 | [0.76, 0.92] | 0.93 | .052 | [0.87, 1.00] | |||
| First-Trimesters × Year2 | 1.02 | .528 | [0.96, 1.08] | 1.03 | .534 | [0.94, 1.12] | 1.05 | .476 | [0.92, 1.20] | 1.08 | .181 | [0.97, 1.20] | |||
| Turnaway-Births × Year2 | 0.93 | .054 | [0.87, 1.00] | 0.91 | .151 | [0.80, 1.04] | 1.11 | .251 | [0.93, 1.33] | 0.90 | .133 | [0.79, 1.03] | |||
| Turnaway-No-Births × Year2 | 0.92 | .177 | [0.81, 1.04] | 1.08 | .374 | [0.91, 1.28] | 1.07 | .573 | [0.85, 1.35] | 0.77 | .039 | [0.60, 0.99] | |||
| Age | 1.03 | .001 | [1.01, 1.05] | 0.99 | .583 | [0.95, 1.03] | 0.98 | .450 | [0.94, 1.03] | 1.05 | .308 | [0.96, 1.15] | 0.97 | .476 | [0.901.05] |
| Race/ethnicityb (ref. = White) | 63.92 | .000 | [21.62, 189.03] | ||||||||||||
| Black | 0.61 | .000 | [0.47, 0.80] | 0.22 | .000 | [0.13, 0.38] | 0.56 | .065 | [0.31, 1.04] | 0.24 | .005 | [0.09, 0.65] | |||
| Hispanic/Latina | 0.64 | .001 | [0.49, 0.83] | 0.56 | .044 | [0.32, 0.98] | 1.08 | .806 | [0.59, 1.99] | 0.49 | .194 | [0.17, 1.43] | |||
| Other | 0.80 | .147 | [0.59, 1.08] | 0.42 | .012 | [0.22, 0.83] | 0.90 | .787 | [0.43, 1.88] | 0.36 | .104 | [0.10, 1.24] | |||
| Parity/recent birth (ref. = nulliparous) | |||||||||||||||
| Past-year birth | 0.53 | .000 | [0.37, 0.76] | 0.43 | .019 | [0.21, 0.87] | 0.45 | .049 | [0.20, 1.00] | 10.52 | .003 | [2.28, 48.57] | 0.17 | .010 | [0.04, 0.65] |
| 1, no past-year birth | 0.42 | .000 | [0.32, 0.55] | 0.42 | .002 | [0.24, 0.72] | 0.58 | .079 | [0.32, 1.06] | 7.50 | .001 | [2.27, 24.81] | 0.20 | .002 | [0.07, 0.57] |
| 2+, past-year birth | 0.46 | .000 | [0.35, 0.62] | 0.44 | .007 | [0.24, 0.79] | 0.46 | .025 | [0.24, 0.91] | 11.69 | .000 | [3.18, 42.91] | 0.15 | .001 | [0.05, 0.47] |
| Marital status (ref. = single) | |||||||||||||||
| Married | 0.66 | .015 | [0.47, 0.92] | 0.70 | .346 | [0.34, 1.46] | 0.76 | .534 | [0.33, 1.78] | 0.39 | .229 | [0.08, 1.81] | 0.45 | .276 | [0.11, 1.90] |
| Separated/divorced | 0.84 | .361 | [0.57, 1.23] | 0.65 | .215 | [0.32, 1.29] | 0.73 | .432 | [0.33, 1.60] | 0.36 | .180 | [0.08, 1.60] | 0.63 | .486 | [0.17, 2.34] |
| Employed | 1.56 | .000 | [1.28, 1.90] | 1.46 | .073 | [0.97, 2.21] | 1.08 | .732 | [0.68, 1.72] | 0.34 | .018 | [0.14, 0.83] | 0.42 | .028 | [0.20, 0.91] |
| Depression/anxiety | 1.15 | .259 | [0.90, 1.47] | 2.26 | .001 | [1.41, 3.61] | 2.58 | .000 | [1.55, 4.27] | 18.07 | .000 | [6.00, 54.49] | 10.53 | .000 | [4.39, 25.29] |
| Child abuse/neglect | 1.14 | .248 | [0.91, 1.44] | 1.45 | .111 | [0.92, 2.29] | 2.05 | .004 | [1.25, 3.35] | 5.11 | .002 | [1.85, 14.10] | 3.79 | .002 | [1.64, 8.77] |
Notes: aOR = adjusted odds ratio; CI = confidence interval; ref. = reference.
All models other than the any alcohol use model include a random slope for individual in addition to a random intercept for site and individual;
models for tobacco use utilize a dichotomous race variable because use among Black and Hispanic participants was so low that the models would not converge with a four-category race variable. Gray indicates control variables.
Longitudinal analyses of First-Trimesters and Turnaway-No-Births versus Near-Limits
There were no statistically significant differences at 1 week or over 5 years between First-Trimesters and Near-Limits in heavy episodic drinking, alcohol problem symptoms, tobacco use, or drug use. Fewer Near-Limits than First-Trimesters reported any drinking at 1 week and 6 months, but this difference was not sustained (Table 2). There were no statistically significant differences at 1 week or over 5 years between Turnaway-No-Births and Near-Limits in any drinking, heavy episodic drinking, alcohol problem symptoms, tobacco use, or drug use.
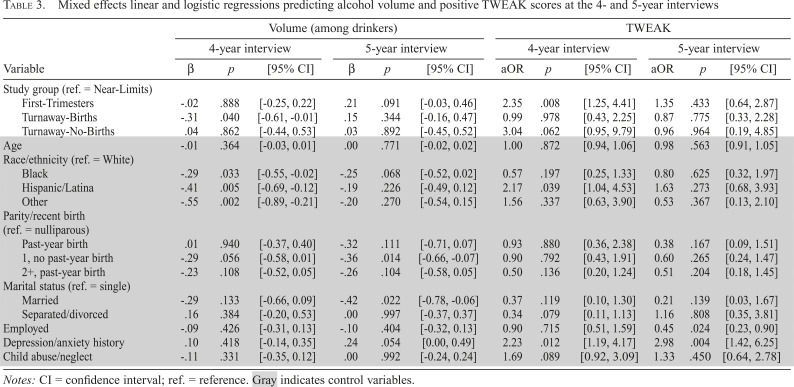
Alcohol volume and “risk” drinking at 4 and 5 years
Alcohol volume between Turnaway-Births and Near-Limits differed at the 4- but not 5-year interviews (Table 3); median volume for drinkers was six drinks/month among Turnaway-Births and nine among Near-Limits at 4 years and was six drinks/month among both groups at 5 years. There were also no statistically significant differences between Turnaway-Births and Near-Limits in odds of a positive TWEAK score at 4 or 5 years, with 9% having positive TWEAK scores at 4 and 8% at 5 years.
Table 3.
Mixed effects linear and logistic regressions predicting alcohol volume and positive TWEAK scores at the 4- and 5-year interviews
| Volume (among drinkers) |
TWEAK |
|||||||||||
| 4-year interview |
5-year interview |
4-year interview |
5-year interview |
|||||||||
| Variable | β | p | [95% CI] | β | p | [95% CI] | aOR | p | [95% CI] | aOR | p | [95% CI] |
| Study group (ref. = Near-Limits) | ||||||||||||
| First-Trimesters | -.02 | .888 | [-0.25, 0.22] | .21 | .091 | [-0.03, 0.46] | 2.35 | .008 | [1.25, 4.41] | 1.35 | .433 | [0.64, 2.87] |
| Turnaway-Births | -.31 | .040 | [-0.61, -0.01] | .15 | .344 | [-0.16, 0.47] | 0.99 | .978 | [0.43, 2.25] | 0.87 | .775 | [0.33, 2.28] |
| Turnaway-No-Births | .04 | .862 | [-0.44, 0.53] | .03 | .892 | [-0.45, 0.52] | 3.04 | .062 | [0.95, 9.79] | 0.96 | .964 | [0.19, 4.85] |
| Age | -.01 | .364 | [-0.03, 0.01] | .00 | .771 | [-0.02, 0.02] | 1.00 | .872 | [0.94, 1.06] | 0.98 | .563 | [0.91, 1.05] |
| Race/ethnicity (ref. = White) | ||||||||||||
| Black | -.29 | .033 | [-0.55, -0.02] | -.25 | .068 | [-0.52, 0.02] | 0.57 | .197 | [0.25, 1.33] | 0.80 | .625 | [0.32, 1.97] |
| Hispanic/Latina | -.41 | .005 | [-0.69, -0.12] | -.19 | .226 | [-0.49, 0.12] | 2.17 | .039 | [1.04, 4.53] | 1.63 | .273 | [0.68, 3.93] |
| Other | -.55 | .002 | [-0.89, -0.21] | -.20 | .270 | [-0.54, 0.15] | 1.56 | .337 | [0.63, 3.90] | 0.53 | .367 | [0.13, 2.10] |
| Parity/recent birth (ref. = nulliparous) | ||||||||||||
| Past-year birth | .01 | .940 | [-0.37, 0.40] | -.32 | .111 | [-0.71, 0.07] | 0.93 | .880 | [0.36, 2.38] | 0.38 | .167 | [0.09, 1.51] |
| 1, no past-year birth | -.29 | .056 | [-0.58, 0.01] | -.36 | .014 | [-0.66, -0.07] | 0.90 | .792 | [0.43, 1.91] | 0.60 | .265 | [0.24, 1.47] |
| 2+, past-year birth | -.23 | .108 | [-0.52, 0.05] | -.26 | .104 | [-0.58, 0.05] | 0.50 | .136 | [0.20, 1.24] | 0.51 | .204 | [0.18, 1.45] |
| Marital status (ref. = single) | ||||||||||||
| Married | -.29 | .133 | [-0.66, 0.09] | -.42 | .022 | [-0.78, -0.06] | 0.37 | .119 | [0.10, 1.30] | 0.21 | .139 | [0.03, 1.67] |
| Separated/divorced | .16 | .384 | [-0.20, 0.53] | .00 | .997 | [-0.37, 0.37] | 0.34 | .079 | [0.11, 1.13] | 1.16 | .808 | [0.35, 3.81] |
| Employed | -.09 | .426 | [-0.31, 0.13] | -.10 | .404 | [-0.32, 0.13] | 0.90 | .715 | [0.51, 1.59] | 0.45 | .024 | [0.23, 0.90] |
| Depression/anxiety history | .10 | .418 | [-0.14, 0.35] | .24 | .054 | [0.00, 0.49] | 2.23 | .012 | [1.19, 4.17] | 2.98 | .004 | [1.42, 6.25] |
| Child abuse/neglect | -.11 | .331 | [-0.35, 0.12] | .00 | .992 | [-0.24, 0.24] | 1.69 | .089 | [0.92, 3.09] | 1.33 | .450 | [0.64, 2.78] |
Notes: CI = confidence interval; ref. = reference. Gray indicates control variables.
Alcohol volume did not differ between First-Trimesters and Near-Limits or Turnaway-No-Births and Near-Limits at 4- or 5-year interviews (Table 3). First-Trimesters had higher odds than Near-Limits of a positive TWEAK score at 4, but not 5, years.
Sensitivity analysis
When we removed the last two interviews from longitudinal analyses, there were no substantive differences. In the any alcohol use, alcohol problem symptom, tobacco use, and drug use models, the effect sizes and statistical significance of study group and Group × Time interactions remained similar. In the heavy episodic drinking model, the quadratic terms for Turnaway-Births became statistically significant; however, this did not substantively change our findings.
Discussion
Our study finds that having an abortion does not lead women to increase ATOD use, including problematic use. Similar to previously published analyses of data through 2 to 2.5 years (Roberts & Foster, 2015; Roberts et al., 2014, 2015), we found no increase in heavy episodic and potentially problematic alcohol use, in tobacco use, or in drug use through 5 years subsequent to having an abortion, although we did find an increase in any alcohol consumption. We note, however, that median volume among those reporting any drinking at 4 or 5 years was well below low-risk drinking guidelines (National Institute on Alcohol Abuse and Alcoholism [NIAAA], 2016). Consistent with other research using different comparison groups (Major et al., 2009; Steinberg & Finer, 2011), we found that women who had abortions had higher levels of any and heavy episodic alcohol use subsequent to abortion seeking than women denied abortions who continued their pregnancies. It appears that the differences are attributable to reductions in these alcohol consumption behaviors among women continuing pregnancies rather than increases among women having abortions.
Reductions in substance use among women denied abortion and continuing unwanted pregnancies differ across substances and alcohol use patterns, indicating that there is not a fixed relationship between pregnancy/parenting and substance use. The lack of a sustained pregnancy/parenting-related reduction in tobacco use among Turnaway-Births as compared with Near-Limits is consistent with previous literature that finds about two thirds who cease tobacco use during pregnancy resume postpartum (United States Department of Health and Human Services, 2001). The lack of a parenting-related reduction for drug use conflicts with some previous research that documents drug use reduction/cessation among pregnant/parenting women using marijuana and among adolescents (Bailey et al., 2008; Barnet et al., 1995; Gilchrist et al., 1996; Hayatbakhsh et al., 2011; Morrison et al., 1998; Spears et al., 2010; Substance Abuse and Mental Health Services Administration, 2009). The previous research may not apply to other drugs, to adults, or to women with unwanted pregnancies, who could possibly be less able to or less motivated to reduce drug use.
The fact that pregnant/parenting women reduce any and heavy episodic drinking compared with prior to pregnancy recognition and compared with women having abortions is consistent with published literature (Alvik et al., 2006; Major et al., 2009; Massey et al., 2011; Steinberg & Finer, 2011) and suggests that general population-targeted messages about harms of alcohol use during pregnancy are reaching this population. Based on our findings, it appears that women with problematic use may need support (e.g., individual counseling or formal treatment; Armstrong et al., 2009; Hser & Niv, 2006; Lester & Twomey, 2008) more than general population messages.
There are number of limitations. First, the ATOD measures are self-report and thus may be underreported, especially during pregnancy. Second, the first interview occurred about a week after abortion seeking. Women’s reports of their ATOD use in the previous month may have already been affected by whether they received or were denied an abortion. Because of stigma about alcohol and drug use during pregnancy, those denied abortion and continuing pregnancies may have been more likely to report lower levels of use than those who had an abortion. If this were the case, we would have expected to (but did not) see this across all substances and all substance use behaviors. Third, there are some limitations to our alcohol use measures because of limitations of the survey instruments. Our heavy episodic drinking measure was “more than five” rather than the more commonly used “five or more” or “four or more” drinks for women (NIAAA, 2004; Wechsler et al., 1995). Also, our longitudinal outcome measures were dichotomous. Thus, it was not possible to assess more subtle fluctuations in volume or in severity of alcohol-related problem symptoms over time. However, our assessment of volume and TWEAK scores at the 4- and 5-year interviews was generally consistent with the findings from the dichotomous measures.
Fourth, 37.5% of eligible participants consented. As previously noted, nonparticipation was unrelated to our primary exposure (receiving vs. being denied abortion), and sensitivity analyses for our 2- to 2.5-year analyses found no substantive differences when the sample was restricted to sites with higher participation (Roberts & Foster, 2015; Roberts et al., 2014, 2015). Lengthy prospective cohort studies that offer no direct benefit often have low participation rates (Ejiogu et al., 2011; Rothman et al., 2008), and participation rates in published investigations may suffer from reporting bias, in that prospective cohort studies with lower participation fail to report participation rates (Galea & Tracy, 2007). Although we cannot confirm this because studies with lower participation may be less likely to report participation rates, a 37.5% participation rate for a study asking women seeking a stigmatized health service to complete semiannual interviews over 5 years may be within the range of other large-scale prospective studies.
Fifth, more women who abstained from alcohol use before pregnancy recognition were lost to follow-up, and fewer Turnaways completed the final 5-year interview. The maximum likelihood methods we used to fit the regression models provide consistent estimation of parameters of interest in settings where data are missing at random (Little & Rubin, 2002), although we cannot confirm to what extent this is the case here. Sixth, most Near-Limits received abortions at later gestations than typical abortion patients, by study design (Pazol et al., 2013). Our findings show no notable differences in substance use subsequent to the abortion between Near-Limits and First-Trimesters, suggesting that our findings may be generalizable. Seventh, about 10% of Turnaway-Births placed their babies for adoption. Previous sensitivity analyses that restricted Turnaway-Births to those who did not place their baby for adoption did not find any substantive difference from models that included them (Roberts & Foster, 2015; Roberts et al., 2014, 2015).
This study also has strengths. Although numerous articles on abortion and subsequent ATOD use exist, the Turnaway Study is the first to use a study design recommended by Surgeon General Koop. This involves prospective measurement of substance use and addresses problems of abortion underreporting common to population-based surveys, where commonly half of abortions are not reported (Jones & Kost, 2007). Second, our study also includes a conceptually appropriate comparison group—women denied abortions just after the group receiving abortions—that is also appropriate in practice, as evidenced by the lack of differences in alcohol and other drug use before pregnancy recognition. Third, this study follows women for 5 years and thus, unlike our earlier analyses, would capture problems that emerged multiple years after the abortion, if such problems had emerged.
In conclusion, there is no indication that having an abortion led women to increase heavy episodic or problem ATOD use. Women denied abortions had temporary or sustained reductions in all alcohol use measures, but not tobacco or drugs, suggesting that relationships between pregnancy/parenting and ATOD differ across substances.
Acknowledgments
The authors thank Rana Barar and Sandy Stonesifer for study coordination and management; Mattie Boehler-Tatman, Janine Carpenter, Undine Darney, Ivette Gomez, Selena Phipps, Brenly Rowland, Claire Schreiber, and Danielle Sinkford for conducting interviews; Michaela Ferrari, Debbie Nguyen, Jasmine Powell, and Elisette Weiss for project support; and Jay Fraser and John Neuhaus for statistical and database assistance.
Footnotes
Components of this study were funded by the Wallace Alexander Gerbode Foundation, the William and Flora Hewlett Foundation, the David and Lucile Packard Foundation, the U.S. National Institute on Alcohol Abuse and Alcoholism/National Institutes of Health (Grant R21 AA021440), and an anonymous foundation.
References
- Alvik A., Heyerdahl S., Haldorsen T., Lindemann R. Alcohol use before and during pregnancy: A population-based study. Acta Obstetricia et Gynecologica Scandinavica . 2006;85:1292–1298. doi: 10.1080/00016340600589958. doi:10.1080/00016340600589958. [DOI] [PubMed] [Google Scholar]
- Americans United For Life. Summary of known health-risks of abortion: How abortion harms women and why concerns for women’s health must be part of abortion-related policies and media debate . 2016. Retrieved from http://www.realhealthcarerespectslife.com/summary-of-known-health-risks-of-abortion.
- Armor D. J., Polich J. M. Measurement of alcohol consumption. In: Pattison E. M., Kaufman E., editors. Encyclopedic handbook of alcoholism (pp. 72–80) New York, NY: Gardner Press; 1982. [Google Scholar]
- Armstrong M. A., Kaskutas L. A., Witbrodt J., Taillac C. J., Hung Y. Y., Osejo V. M., Escobar G. J. Using drink size to talk about drinking during pregnancy: A randomized clinical trial of Early Start Plus. Social Work in Health Care . 2009;48:90–103. doi: 10.1080/00981380802451210. doi:10.1080/00981380802451210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey J. A., Hill K. G., Hawkins J. D., Catalano R. F., Abbott R. D. Men’s and women’s patterns of substance use around pregnancy. Birth . 2008;35:50–59. doi: 10.1111/j.1523-536X.2007.00211.x. doi:10.1111/j.1523-536X.2007.00211.x. [DOI] [PubMed] [Google Scholar]
- Barnet B., Duggan A. K., Wilson M. D., Joffe A. Association between postpartum substance use and depressive symptoms, stress, and social support in adolescent mothers. Pediatrics . 1995;96:659–666. [PubMed] [Google Scholar]
- Biggs M. A., Neuhaus J. M., Foster D. G. Mental health diagnoses 3 years after receiving or being denied an abortion in the United States. American Journal of Public Health . 2015;105:2557–2563. doi: 10.2105/AJPH.2015.302803. doi:10.2105/AJPH.2015.302803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biggs M. A., Rowland B., McCulloch C. E., Foster D. G. Does abortion increase women’s risk for post-traumatic stress? Findings from a prospective longitudinal cohort study. BMJ Open . 2016;6 doi: 10.1136/bmjopen-2015-009698. e009698. doi:10.1136/bmjopen-2015-009698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biggs M. A., Upadhyay U. D., McCulloch C. E., Foster D. G. Women’s mental health and well-being 5 years after receiving or being denied an abortion: A prospective, longitudinal cohort study. JAMA Psychiatry . 2017;74:169–178. doi: 10.1001/jamapsychiatry.2016.3478. doi:10.1001/jamapsychiatry.2016.3478. [DOI] [PubMed] [Google Scholar]
- Chang G. Alcohol-screening instruments for pregnant women . 2001. Retrieved from http://pubs.niaaa.nih.gov/publications/arh25-3/204-209.htm. [PMC free article] [PubMed]
- Charles V. E., Polis C. B., Sridhara S. K., Blum R. W. Abortion and long-term mental health outcomes: A systematic review of the evidence. Contraception . 2008;78:436–450. doi: 10.1016/j.contraception.2008.07.005. doi:10.1016/j.contraception.2008.07.005. [DOI] [PubMed] [Google Scholar]
- Coleman P. K., Reardon D. C., Cougle J. R. Substance use among pregnant women in the context of previous reproductive loss and desire for current pregnancy. British Journal of Health Psychology . 2005;10:255–268. doi: 10.1348/135910705X25499. doi:10.1348/135910705X25499. [DOI] [PubMed] [Google Scholar]
- Coleman P. K., Reardon D. C., Rue V. M., Cougle J. A history of induced abortion in relation to substance use during subsequent pregnancies carried to term. American Journal of Obstetrics and Gynecology . 2002;187:1673–1678. doi: 10.1067/mob.2002.127602. doi:10.1067/mob.2002.127602. [DOI] [PubMed] [Google Scholar]
- Center for Reproductive Rights. Safe abortion: A public health imperative . 2005 Retrieved from http://www.reproductiverights.org/sites/default/files/documents/pub_bp_tk_safe_abortion.pdf. [Google Scholar]
- Dingle K., Alati R., Clavarino A., Najman J. M., Williams G. M. Pregnancy loss and psychiatric disorders in young women: An Australian birth cohort study. British Journal of Health Psychology . 2008;193:455–460. doi: 10.1192/bjp.bp.108.055079. doi:10.1192/bjp.bp.108.055079. [DOI] [PubMed] [Google Scholar]
- Dobkin L. M., Gould H., Barar R. E., Ferrari M., Weiss E. I., Foster D. G. Implementing a prospective study of women seeking abortion in the United States: Understanding and overcoming barriers to recruitment. Women’s Health Issues . 2014;24:e115–e123. doi: 10.1016/j.whi.2013.10.004. doi:10.1016/j.whi.2013.10.004. [DOI] [PubMed] [Google Scholar]
- Ejiogu N., Norbeck J. H., Mason M. A., Cromwell B. C., Zonderman A. B., Evans M. K. Recruitment and retention strategies for minority or poor clinical research participants: Lessons from the Healthy Aging in Neighborhoods of Diversity Across the Life Span study. The Gerontologist, 51, Supplement 1 . 2011:S33–S45. doi: 10.1093/geront/gnr027. doi:10.1093/geront/gnr027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson D. M., Horwood L. J., Boden J. M. Abortion and mental health disorders: Evidence from a 30-year longitudinal study. British Journal of Psychiatry . 2008;193:444–451. doi: 10.1192/bjp.bp.108.056499. doi:10.1192/bjp.bp.108.056499. [DOI] [PubMed] [Google Scholar]
- Finer L. B., Zolna M. R. Unintended pregnancy in the United States: Incidence and disparities, 2006. Contraception . 2011;84:478–485. doi: 10.1016/j.contraception.2011.07.013. doi:10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster D. G., Steinberg J. R., Roberts S. C. M., Neuhaus J., Biggs M. A. A comparison of depression and anxiety symptom trajectories between women who had an abortion and women denied one. Psychological Medicine . 2015;45:2073–2082. doi: 10.1017/S0033291714003213. doi:10.1017/S0033291714003213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Tracy M. Participation rates in epidemiologic studies. Annals of Epidemiology . 2007;17:643–653. doi: 10.1016/j.annepidem.2007.03.013. doi:10.1016/j.annepidem.2007.03.013. [DOI] [PubMed] [Google Scholar]
- Gilchrist L. D., Hussey J. M., Gillmore M. R., Lohr M. J., Morrison D. M. Drug use among adolescent mothers: Prepregnancy to 18 months postpartum. Journal of Adolescent Health . 1996;19:337–344. doi: 10.1016/S1054-139X(96)00052-3. doi:10.1016/S1054-139X(96)00052-3. [DOI] [PubMed] [Google Scholar]
- Gould H., Perrucci A., Barar R., Sinkford D., Foster D. G. Patient education and emotional support practices in abortion care facilities in the United States. Women’s Health Issues . 2012;22:e359–e364. doi: 10.1016/j.whi.2012.04.003. doi:10.1016/j.whi.2012.04.003. [DOI] [PubMed] [Google Scholar]
- Hayatbakhsh M. R., Kingsbury A. M., Flenady V., Gilshenan K. S., Hutchinson D. M., Najman J. M. Illicit drug use before and during pregnancy at a tertiary maternity hospital 2000–2006. Drug and Alcohol Review . 2011;30:181–187. doi: 10.1111/j.1465-3362.2010.00214.x. doi:10.1111/j.1465-3362.2010.00214.x. [DOI] [PubMed] [Google Scholar]
- Hser Y. I., Niv N. Pregnant women in women-only and mixed-gender substance abuse treatment programs: A comparison of client characteristics and program services. Journal of Behavioral Health Services & Research . 2006;33:431–442. doi: 10.1007/s11414-006-9019-1. doi:10.1007/s11414-006-9019-1. [DOI] [PubMed] [Google Scholar]
- Jones R. K., Kost K. Underreporting of induced and spontaneous abortion in the United States: An analysis of the 2002 National Survey of Family Growth. Studies in Family Planning . 2007;38:187–197. doi: 10.1111/j.1728-4465.2007.00130.x. doi:10.1111/j.1728-4465.2007.00130.x. [DOI] [PubMed] [Google Scholar]
- Kelly K. The spread of post abortion syndrome as social diagnosis. Social Science & Medicine . 2014;102:18–25. doi: 10.1016/j.socscimed.2013.11.030. doi:10.1016/j.socscimed.2013.11.030. [DOI] [PubMed] [Google Scholar]
- Koop C. E. Post abortion syndrome: Myth or reality? Health Matrix . 1989;7:42–44. [PubMed] [Google Scholar]
- Lester B. M., Twomey J. E. Treatment of substance abuse during pregnancy. Women’s Health . 2008;4:67–77. doi: 10.2217/17455057.4.1.67. doi:10.2217/17455057.4.1.67. [DOI] [PubMed] [Google Scholar]
- Little R. J. A., Rubin D. B. Statistical analysis with missing data . 2nd ed. Hoboken, NJ: John Wiley & Sons; 2002. [Google Scholar]
- Major B., Appelbaum M., Beckman L., Dutton M. A., Russo N. F., West C. Abortion and mental health: Evaluating the evidence. American Psychologist . 2009;64:863–890. doi: 10.1037/a0017497. doi:10.1037/a0017497. [DOI] [PubMed] [Google Scholar]
- Massey S. H., Lieberman D. Z., Reiss D., Leve L. D., Shaw D. S., Neiderhiser J. M. Association of clinical characteristics and cessation of tobacco, alcohol, and illicit drug use during pregnancy. American Journal on Addictions . 2011;20:143–150. doi: 10.1111/j.1521-0391.2010.00110.x. doi:10.1111/j.1521-0391.2010.00110.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison D. M., Spencer M. S., Gillmore M. R. Beliefs about substance use among pregnant and parenting adolescents. Journal of Research on Adolescence . 1998;8:69–95. doi: 10.1207/s15327795jra0801_4. doi:10.1207/s15327795jra0801_4. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. NIAAA council approves definition of binge drinking. NIAAA Newsletter . 2004 Retrieved from https://pubs.niaaa.nih.gov/publications/Newsletter/winter2004/Newsletter_Number3.pdf. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Rethinking drinking: Alcohol & your health . 2016 Retrieved from https://www.rethinkingdrinking.niaaa.nih.gov. [Google Scholar]
- Olsson C. A., Horwill E., Moore E., Eisenberg M. E., Venn A., O’Loughlin C., Patton G. C. Social and emotional adjustment following early pregnancy in young Australian women: A comparison of those who terminate, miscarry, or complete pregnancy. Journal of Adolescent Health . 2014;54:698–703. doi: 10.1016/j.jadohealth.2013.10.203. doi:10.1016/j.jadohealth.2013.10.203. [DOI] [PubMed] [Google Scholar]
- Pazol K., Creanga A. A., Burley K. D., Hayes B., Jamieson D. J. the Centers for Disease Control and Prevention (CDC) Abortion surveillance – United States, 2010. MMWR Surveillance Summaries, 62, No. SS-8 . 2013, November 29:1–44. Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/ss6208a1.htm. [PubMed] [Google Scholar]
- Pedersen W. Childbirth, abortion and subsequent substance use in young women: A population-based longitudinal study. Addiction . 2007;102:1971–1978. doi: 10.1111/j.1360-0443.2007.02040.x. doi:10.1111/j.1360-0443.2007.02040.x. [DOI] [PubMed] [Google Scholar]
- Roberts S. C. M., Delucchi K., Wilsnack S. C., Foster D. G. Receiving versus being denied a pregnancy termination and subsequent alcohol use: A longitudinal study. Alcohol and Alcoholism . 2015;50:477–484. doi: 10.1093/alcalc/agv021. doi:10.1093/alcalc/agv021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts S. C. M., Foster D. G. Receiving versus being denied an abortion and subsequent tobacco use. Maternal and Child Health Journal . 2015;19:438–446. doi: 10.1007/s10995-014-1515-y. doi:10.1007/s10995-014-1515-y. [DOI] [PubMed] [Google Scholar]
- Roberts S. C. M., Rocca C. H., Foster D. G. Receiving versus being denied an abortion and subsequent drug use. Drug and Alcohol Dependence . 2014;134:63–70. doi: 10.1016/j.drugalcdep.2013.09.013. doi:10.1016/j.drugalcdep.2013.09.013. [DOI] [PubMed] [Google Scholar]
- Roberts S. C. M., Subbaraman M. S., Delucchi K. L., Wilsnack S. C., Foster D. G. Moderators and mediators of the relationship between receiving versus being denied a pregnancy termination and subsequent binge drinking. Drug and Alcohol Dependence . 2016;159:117–124. doi: 10.1016/j.drugalcdep.2015.11.033. doi:10.1016/j.drugalcdep.2015.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson G. E., Stotland N. L., Russo N. F., Lang J. A., Occhiogrosso M. Is there an abortion trauma syndrome? Critiquing the evidence. Harvard Review of Psychiatry . 2009;17:268–290. doi: 10.1080/10673220903149119. doi:10.1080/10673220903149119. [DOI] [PubMed] [Google Scholar]
- Rothman K., Greenland S., Lash T. L. Modern epidemiology . Philadelphia, PA: Lippincott, Williams, & Wilkins; 2008. [Google Scholar]
- Spears G. V., Stein J. A., Koniak-Griffin D. Latent growth trajectories of substance use among pregnant and parenting adolescents. Psychology of Addictive Behaviors . 2010;24:322–332. doi: 10.1037/a0018518. doi:10.1037/a0018518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg J. R., Finer L. B. Examining the association of abortion history and current mental health: A reanalysis of the National Comorbidity Survey using a common-risk-factors model. Social Science & Medicine . 2011;72:72–82. doi: 10.1016/j.socscimed.2010.10.006. doi:10.1016/j.socscimed.2010.10.006. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Administration Services Administration. Substance use among women during pregnancy and following childbirth. The NSDUH Report . 2009 Retrieved from https://roar.nevadaprc.org/system/documents/2924/original/NPRC.1362.May21_2009.pdf?1425586367 p.13. [Google Scholar]
- Upadhyay U. D., Weitz T. A., Jones R. K., Barar R. E., Foster D. G. Denial of abortion because of provider gestational age limits in the United States. American Journal of Public Health . 2014;104:1687–1694. doi: 10.2105/AJPH.2013.301378. doi:10.2105/AJPH.2013.301378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. Women and smoking: A Report of the Surgeon General . Atlanta, GA: Office on Smoking and Health; 2001. [Google Scholar]
- Wechsler H., Dowdall G. W., Davenport A., Rimm E. B. A gender-specific measure of binge drinking among college students. American Journal of Public Health . 1995;85:982–985. doi: 10.2105/ajph.85.7.982. doi:10.2105/AJPH.85.7.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilmoth G. H. Abortion, public health policy, and informed consent legislation. Journal of Social Issues . 1992;48:1–17. doi: 10.1111/j.1540-4560.1992.tb00895.x. doi:10.1111/j.1540-4560.1992.tb00895.x. [DOI] [PubMed] [Google Scholar]