Abstract
Objective:
South Africa’s Western Cape Province has one of the highest rates of fetal alcohol spectrum disorder globally. Alcohol-serving venues are likely important sites to identify women at high risk of having a child with fetal alcohol spectrum disorder. The goal of this study was to examine the risk for alcohol-exposed pregnancies among women who drink in alcohol-serving venues.
Method:
Cross-sectional surveys were conducted with 200 women of reproductive age at seven drinking venues in a single Cape Town community. Surveys assessed sexual behavior, contraceptive use, and drinking behavior (both current and during previous pregnancies). Women were defined as being at risk for alcohol-exposed pregnancy if they were currently drinking, sexually active in the previous 60 days, and not consistently using modern contraceptives.
Results:
Almost all participants (95.5%) met criteria for hazardous drinking. In total, 20.3% of the 152 sexually active women were identified as at risk for alcohol-exposed pregnancy, and 2 women were currently pregnant and drinking. A majority of sexually active participants (79.6%) reported consistent use of a modern contraceptive. Most contraceptives (66.1%) were short-acting methods such as injectables. Of the 176 participants who reported previous pregnancies, 64.8% said they drank alcohol during a previous pregnancy and 51.1% met criteria for hazardous drinking during that pregnancy.
Conclusions:
Given the high rates of alcohol consumption during pregnancy, alcohol-serving venues should be targeted for fetal alcohol spectrum disorder prevention interventions. Efforts should be made to increase uptake of long-acting contraceptives among women who do not wish to get pregnant and to promote alcohol cessation among women with pregnancy intentions.
Fetal alcohol spectrum disorder (fasd) is a cluster of birth defects resulting from alcohol exposure in utero, which can cause lifelong developmental, cognitive, and behavioral impairments (Hoyme et al., 2016). Although FASD prevalence in the United States has been estimated at 2%–5% (May et al., 2009, 2014),observed FASD prevalence in the Western Cape of South Africa has been found to be as high as 18%–26% in recent studies, rates that are among the highest in the world (Adnams, 2017; May et al., 2016a, 2016b). Hazardous drinking in this location is typically characterized by episodic binge drinking (Choi et al., 2014). Longitudinal studies show that these patterns of hazardous drinking often continue into the pregnancy period because of a variety of social, contextual, and structural factors (Eaton, 2012; Watt et al., 2014, 2016).
Reducing the high burden of FASD and its consequences in South Africa requires a multimodal response. Whereas most FASD prevention efforts have focused on alcohol cessation among pregnant women, there remains an equally important need to prevent unintended pregnancies among hazardous drinkers, who are most at risk for an alcohol-exposed pregnancy (AEP; Rendall-Mkosi et al., 2013). Harmful effects of fetal alcohol exposure often occur early in the pregnancy, before the mother is aware that she is pregnant (May et al., 2013a). Therefore, by the time a mother attends prenatal clinic appointments and receives counseling, it may already be too late to prevent FASD for that pregnancy. In light of these findings, high-risk settings such as alcohol-serving venues are important sites to identify drinkers at risk for an AEP (Eaton et al., 2012).
This study aimed to understand the risk for AEPs among patrons of alcohol-serving venues in one community within the Cape Town, South Africa, metropolitan area. Results may inform novel interventions for community-based primary prevention of FASD in high-risk venues to reduce the harmful drinking that contributes to FASD early in pregnancies. The objectives were threefold: (a) to assess patterns of alcohol consumption, both current and in previous pregnancies; (b) to describe pregnancy intentions and contraceptive use among female drinkers; and (c) to characterize the risk for AEP in this sample.
Method
Overview and setting
The study was a cross-sectional survey of 200 women recruited from eight alcohol-serving venues in a single community in the Cape Town metropole. All procedures were approved by the ethical review boards of Duke University and Stellenbosch University.
Study procedures
Study venues were selected via convenience sampling and were eligible if they served at least 100 unique patrons per week, with women making up at least a quarter of patrons. Of the eight venues, all were formal, licensed alcohol distributors. Four venues were primarily for in-house consumption and four were primarily for take-away consumption. The data collection team consisted of two female, university-trained researchers who shared the same cultural background (Cape Coloured) and language (Afrikaans) as the study community. Researchers approached female venue patrons of reproductive age (18–45 years) before they had begun drinking and invited them to complete a brief, researcher-administered survey. Oral consent was obtained before the survey, and no identifying information was collected. Surveys took approximately 15 minutes to complete.
Measures
Measures were adapted from previous research conducted in South Africa (Eaton et al., 2012; Pitpitan et al., 2013; Watt et al., 2012b) and were administered in Afrikaans.
Demographics.
Participants were asked to report their age, relationship status, education, employment status, in, and number of children.
Alcohol consumption.
The three-item Alcohol Use Disorders Identification Test–consumption (AUDIT-C), which has demonstrated validity in South Africa (Taylor et al., 2015), was used to assess frequency of alcohol consumption, number of drinks per occasion, and binge drinking, defined as six or more drinks in one sitting (Bush et al., 1998). The measure was administered twice: first asking about current drinking patterns (α = .85) and second, for women with previous pregnancies, asking about drinking during the pregnancy in which they drank the most (α = .91). For each reference point, the three items were summed (0–12). Hazardous drinking was defined as a score greater than 3, as long as all points were not attributable to drinking frequency (Bradley et al., 2003).
Pregnancy status and intentions.
Participants were asked questions about their current pregnancy status and whether they intended to become pregnant in the next year.
Sexual behavior.
Participants were asked questions regarding sexual activity in the past 60 days, including number of male partners, and number of vaginal sex acts.
Contraceptive use.
Participants reported whether they were currently using various contraceptives, including both short-acting methods (injectables, birth control pills) and long-acting methods (implants, intrauterine devices, sterilization). Follow-up questions asked about consistency and timing of use over the past 60 days. Subsequent analyses defined contraceptive coverage as consistent use of a chosen method for the past 60 days to be effective for preventing pregnancy. Women were asked about condom use, but reliance solely on condoms for contraception was not deemed sufficient contraceptive coverage because hazardous drinking is associated with condom accidents and inconsistent use (Chersich & Rees, 2010; Mantell et al., 2011).
Data analysis
Data were analyzed by calculating simple frequencies of scale responses, as well as chi-square analyses to assess potential differences in AEP risk based on AUDIT-C score, pregnancy intention, and parenthood status. First, we examined alcohol use patterns, both current and during a previous pregnancy. Second, we examined contraceptive use among sexually active participants (e.g., methods, consistency, and adherence for pregnancy and AEP coverage) and the relationship between contraceptive use and pregnancy intention. Third, we identified women currently drinking while pregnant and estimated risk for AEP during the previous 60 days.
Results
Description of the sample
Participants ranged in age from 18 to 43 (M = 29, SD = 7), and less than half (n = 81,41.1%) had completed secondary school. Most participants (n = 168, 84.0%) had at least one living child, with a mean of two children per participant (SD = 1). Nearly half (n = 99, 49.5%) were employed, with 48 (24.0%) reporting consistent, fixed employment. Median household income was 4,000 South African Rands per month, or approximately U.S. $300 (SD = 4,178). Most women (n = 147, 73.5%) reported being married or in a romantic relationship.
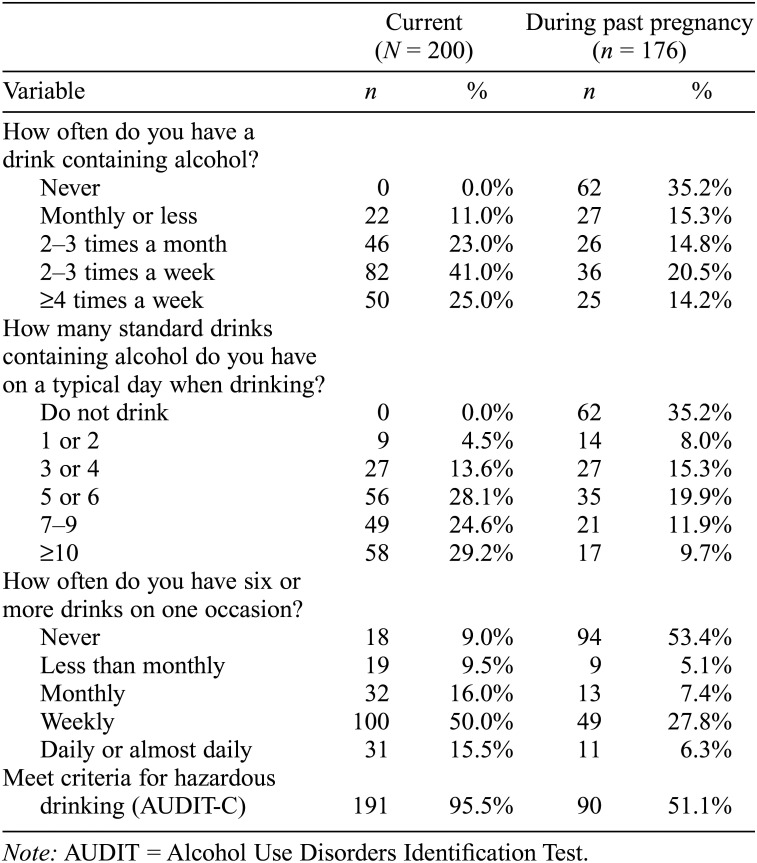
Drinking patterns
Almost all women (n = 191, 95.5%) met AUDIT-C criteria for current hazardous drinking (Table 1). Among a subset of 176 participants with previous pregnancies, 114 (64.8%) reported drinking alcohol while pregnant, with 90 (51.1%) meeting criteria for hazardous drinking and 82 (46.6%) reporting binge drinking during a previous pregnancy.
Table 1.
Drinking patterns of participants, current and during past pregnancy
| Current (N =200) |
During past pregnancy (n = 176) |
|||
| Variable | n | % | n | % |
| How often do you have a drink containing alcohol? | ||||
| Never | 0 | 0.0% | 62 | 35.2% |
| Monthly or less | 22 | 11.0% | 27 | 15.3% |
| 2–3 times a month | 46 | 23.0% | 26 | 14.8% |
| 2–3 times a week | 82 | 41.0% | 36 | 20.5% |
| ≥4 times a week | 50 | 25.0% | 25 | 14.2% |
| How many standard drinks containing alcohol do you have on a typical day when drinking? | ||||
| Do not drink | 0 | 0.0% | 62 | 35.2% |
| 1 or 2 | 9 | 4.5% | 14 | 8.0% |
| 3 or 4 | 27 | 13.6% | 27 | 15.3% |
| 5 or 6 | 56 | 28.1% | 35 | 19.9% |
| 7–9 | 49 | 24.6% | 21 | 11.9% |
| ≥10 | 58 | 29.2% | 17 | 9.7% |
| How often do you have six or more drinks on one occasion? | ||||
| Never | 18 | 9.0% | 94 | 53.4% |
| Less than monthly | 19 | 9.5% | 9 | 5.1% |
| Monthly | 32 | 16.0% | 13 | 7.4% |
| Weekly | 100 | 50.0% | 49 | 27.8% |
| Daily or almost daily | 31 | 15.5% | 11 | 6.3% |
| Meet criteria for hazardous | ||||
| drinking (AUDIT-C) | 191 | 95.5% | 90 | 51.1% |
Note: AUDIT = Alcohol Use Disorders Identification Test.
Pregnancy status and intentions
Two participants indicated that they were pregnant at the time of the survey, and five were unsure of their pregnancy status. Twenty-nine women (14.5%) indicated that they intended to become pregnant in the next year; 25 of these were sexually active.
Sexual behavior and contraceptive use
Most participants (n = 154, 77.0%) reported having had sex with a male partner in the past 60 days; of these, almost all (n = 147, 95.4%) reported a single sexual partner. Among the 152 nonpregnant, sexually active women, most (n = 121, 79.6%) reported that they were covered by at least one form of modern contraceptive throughout the past 60 days. The most common form of contraceptive was injectables (n = 77), followed by implants (n = 29), sterilization (n = 8), birth control pills (n = 6), and intrauterine devices (n = 4). Of 15 sexually active women who had used contraception within the past year but were no longer covered by any form, 14 (93.3%) had previously relied on short-acting methods (i.e., injectables or pills). In addition, 26 (16.9%) sexually active participants indicated that they had used a condom at some point in the past 60 days, and 9 (5.8%) had used a condom every time they had sex. Only 5 (3.3%) sexually active women reported dual coverage with condoms and a second form of contraception during every sexual encounter.
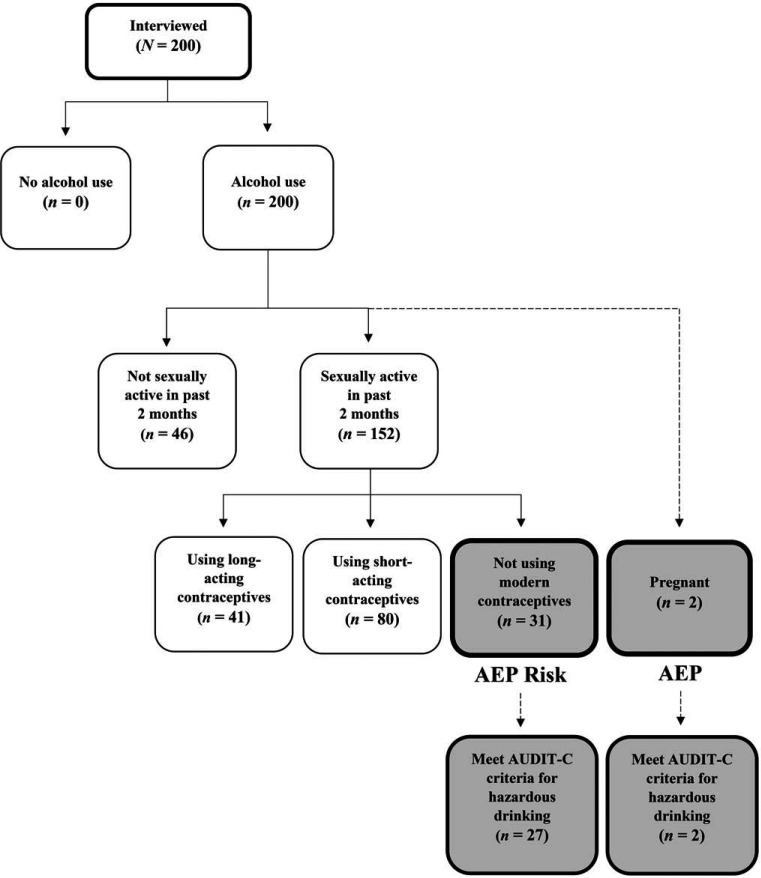
Risk for alcohol-exposed pregnancy
Figure 1 depicts the process of identifying risk for an AEP in this sample. All 200 participants reported regular alcohol consumption, and 154 were sexually active in the past 60 days, 2 of whom reported being pregnant. Both pregnant women were currently drinking at hazardous levels and were considered to have an AEP. Among the 152 sexually active, nonpregnant women, 121 (79.6%) were covered for pregnancy prevention by modern contraceptives throughout the previous 60 days. Thirty-one sexually active women (20.4%) reported inconsistent or no coverage with modern contraceptives during the past 60 days and therefore were at risk for AEP. Among these women, 21 (13.8%) reported that they did not intend to get pregnant and were thus vulnerable for an unintended pregnancy.
Figure 1.
Risk for alcohol-exposed pregnancy (AEP). AUDIT-C = Alcohol Use Disorders Identification Test-consumption.
Women were more likely to be at risk for AEP if they did not have children (44.4% vs. 17.2%), χ2 = 7.274, p = .007, or had an intention to get pregnant in the next year (40.0% vs. 16.5%), χ2 = 7.084, p = .008. In addition, women at risk for AEP had lower AUDIT-C scores compared with women not at risk for AEP (M = 6.758 vs. M = 8.438), t(150) = 3.046,p = .003, indicating that at-risk women may be aware that they could become pregnant and were intentionally reducing their consumption but, nevertheless, were still drinking at hazardous levels.
Discussion
The data presented in this study highlight the risk for AEPs among women who frequent alcohol-serving venues in a Cape Town community, and underscore the importance of alcohol-serving venues as spaces to identify and reach women for primary prevention of FASD. More than 2 in 10 sexually active women recruited from drinking venues were at risk for AEP, and almost all were drinking at hazardous levels. Further, short-acting contraceptives were by far the most commonly used, increasing the likelihood of unintended pregnancy because of lapses in coverage (Baumgartner et al., 2007). The high rates of reported drinking during previous pregnancies, including binge drinking, further underscore the magnitude of AEP risk and its consequences, including FASD. Reducing FASD incidence in the Western Cape requires evidence-based prevention efforts, targeting women in sites where there is high risk for AEP.
Use of modern contraceptives in this sample was high overall, but a substantial number of sexually active women who did not intend to get pregnant remained without coverage. Women who intended to become pregnant were less likely to be covered by modern contraceptives and were drinking at lower, but still hazardous, levels, putting them at risk for FASD and other consequences (Hoyme et al., 2016). Injectable contraceptives were the most common form of contraception, likely because they are freely available at community health centers and can be used without partner consent (Morroni et al., 2006; South African Medical Research Council, 2007). However, research in South Africa suggests that women face challenges adhering to injection schedules, increasing risk of unintended pregnancies (Baumgartner et al., 2007). In addition, because women using injectables may cease contraceptive coverage at any time by not returning for an injection, there is no natural opportunity to counsel them on health behaviors before conception.
Considering that women have different family-planning needs, interventions should be tailored to increase access to appropriate contraceptive technologies, depending on women’s pregnancy intentions. In particular, it would be beneficial to transition women wishing to prevent pregnancy to long-acting forms of contraception (e.g., implants or intrauterine devices) and to integrate FASD prevention messages into family-planning appointments. At the same time, broad public health interventions should be promoted to prevent alcohol consumption among women who are pregnant or trying to conceive. Such interventions should include targeted and high-visibility campaigns on the risks of AEPs, and restrictions in alcohol advertising, a strategy that has been met with resistance by the alcohol industry (Parry et al., 2014).
Although previous interventions have targeted South African women at risk for AEP in clinical settings (Rendall- Mkosi et al., 2013) or case management thereafter (de Vries et al., 2015; May et al., 2013b), the data presented here suggest that it is also important to target women in alcohol-serving venues, where women of reproductive age who are drinking at high levels may be readily identified. Our history of research in this setting suggests that community-based interventions with women identified in alcohol-serving venues can be a feasible and effective strategy for reaching women at risk for AEP (Watt et al., 2014, 2016). In a longitudinal cohort study following 560 female patrons from alcohol-serving venues, 12% became pregnant in the course of a year, and alcohol consumption typically continued during the pregnancy period (Choi et al., 2014). Although alcohol-serving venues can be sites of risk behavior, they also have the potential to serve as a source of support and pro-social norms, making them unique sites for behavioral interventions (Dresser et al., 2011; Watt et al., 2012a). Our data suggest that venue-based interventions should promote women’s uptake of appropriate contraceptives, increase self-efficacy to plan for pregnancy, facilitate behavior change, and address community norms around drinking during pregnancy. Interventions that focus on women’s goals of family formation and parenting may be particularly effective, given that a majority of women had at least one child and women without children were more likely to be at risk for AEP.
The strength of this study is that it included women from a high-risk, naturalistic setting who may not be captured through research in clinical settings. The study is limited by a convenience sample and administration of surveys in a social environment, which may have increased social desirability bias. Because of this purposive venue-based sampling, the results likely represent women at high risk for AEP in the community and should not be generalized to the public at large. Contraceptive use, including adherence to contraceptive methods, was assessed by self-report. Future research should include triangulation of self-reports with clinical data and timeline followback techniques to more objectively capture sexual behavior and contraceptive coverage.
Although typical FASD prevention interventions focus on screening pregnant women for alcohol use and counseling for alcohol cessation, pregnancy planning and prevention among women who drink alcohol is equally important. A dual approach addressing both pregnancy and drinking could be modeled after existing prevention programs (Masis & May, 1991; Rendall-Mkosi et al., 2013). Future research should address contextual barriers that influence access and effective use of contraceptives, particularly among such at-risk populations as patrons of alcohol-serving venues.
Acknowledgments
The authors are grateful to the efforts of Desiree Pieterse and Mariana Bolumole, who collected the data, and to the participants who contributed time and energy to this study.
Footnotes
This study was funded by a grant from the Duke Global Health Institute, through the Maternal, Adolescent and Child Health Working Group. We acknowledge support received from the Duke Center for AIDS Research (P30 AI064518) and the UCLA HIV/AIDS, Substance Abuse and Trauma Training Program (R25 DA035692).
References
- Adnams C. M. Fetal alcohol spectrum disorder in Africa. Current Opinion in Psychiatry . 2017;30:108–112. doi: 10.1097/YCO.0000000000000315. doi:10.1097/YC0.0000000000000315. [DOI] [PubMed] [Google Scholar]
- Baumgartner J. N., Morroni C., Mlobeli R. D., Otterness C., Myer L., Janowitz B., Buga G. Timeliness of contraceptive reinjections in South Africa and its relation to unintentional discontinuation. International Family Planning Perspectives . 2007;33:66–74. doi: 10.1363/3306607. doi:10.1363/3306607. [DOI] [PubMed] [Google Scholar]
- Bradley K. A., Bush K. R., Epler A. J., Dobie D. J., Davis T. M., Sporleder J. L., Kivlahan D. R. Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT): Validation in a female Veterans Affairs patient population. Archives of Internal Medicine . 2003;163:821–829. doi: 10.1001/archinte.163.7.821. doi:10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- Bush K., Kivlahan D. R., McDonell M. B., Fihn S. D., Bradley K. A. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Archives of Internal Medicine . 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. doi:10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Chersich M. F., Rees H. V. Causal links between binge drinking patterns, unsafe sex and HIV in South Africa: It’s time to intervene. International Journal of STD & AIDS . 2010;21:2–7. doi: 10.1258/ijsa.2000.009432. doi:10.1258/ijsa.2000.009432. [DOI] [PubMed] [Google Scholar]
- Choi K. W., Abler L. A., Watt M. H., Eaton L. A., Kalichman S. C., Skinner D., Sikkema K. J. Drinking before and after pregnancy recognition among South African women: The moderating role of traumatic experiences. BMC Pregnancy and Childbirth . 2014;14:97. doi: 10.1186/1471-2393-14-97. doi:10.1186/1471-2393-14-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Vries M. M., Joubert B., Cloete M., Roux S., Baca B. A., Hasken J. M., May P. A. Indicated prevention of fetal alcohol spectrum disorders in South Africa: Effectiveness of Case Management. International Journal of Environmental Research and Public Health . 2015;13:76. doi: 10.3390/ijerph13010076. doi:10.3390/ijerph13010076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dresser J., Starling R., Woodall W. G., Stanghetta P., May P. A. Field trial of alcohol-server training for prevention of fetal alcohol syndrome. Journal of Studies on Alcohol and Drugs . 2011;72:490–496. doi: 10.15288/jsad.2011.72.490. doi:10.15288/jsad.2011.72.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton L. A., Kalichman S. C., Sikkema K. J., Skinner D., Watt M. H., Pieterse D., Pitpitan E. V. Pregnancy, alcohol intake, and intimate partner violence among men and women attending drinking establishments in a Cape Town, South Africa township. Journal of Community Health . 2012;37:208–216. doi: 10.1007/s10900-011-9438-7. doi:10.1007/s10900-011-9438-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyme H. E., Kalberg W. O., Elliott A. J., Blankenship J., Buckley A., Marais A.-S., May P. A. Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders. Pediatrics . 2016;138(2):e20154256. doi: 10.1542/peds.2015-4256. doi:10.1542/peds.2015-4256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantell J. E., Smit J. A., Beksinska M., Scorgie F., Milford C., Balch B., Stein Z. A. Everywhere you go, everyone is saying condom, condom. But are they being used consistently? Reflections of South African male students about male and female condom use. Health Education Research . 2011;26:859–871. doi: 10.1093/her/cyr041. doi:10.1093/her/cyr041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masis K. B., May P. A. A comprehensive local program for the prevention of fetal alcohol syndrome. Public Health Reports . 1991;106:484–489. [PMC free article] [PubMed] [Google Scholar]
- May P. A., Baete A., Russo J., Elliott A. J., Blankenship J., Kalberg W. O., Hoyme H. E. Prevalence and characteristics of fetal alcohol spectrum disorders. Pediatrics . 2014;134:855–866. doi: 10.1542/peds.2013-3319. doi:10.1542/peds.2013-3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May P. A., Blankenship J., Marais A.-S., Gossage J. P., Kalberg W. O., Joubert B., Seedat S. Maternal alcohol consumption producing fetal alcohol spectrum disorders (FASD): Quantity, frequency, and timing of drinking. Drug and Alcohol Dependence . 2013a;133:502–512. doi: 10.1016/j.drugalcdep.2013.07.013. doi:10.1016/j.drugalcdep.2013.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May P. A., de Vries M. M., Marais A.-S., Kalberg W. O., Adnams C. M., Hasken J. M., Hoyme H. E. The continuum of fetal alcohol spectrum disorders in four rural communities in South Africa: Prevalence and characteristics. Drug and Alcohol Dependence . 2016a;159:207–218. doi: 10.1016/j.drugalcdep.2015.12.023. doi:10.1016/j.drugalcdep.2015.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May P. A., Gossage J. P., Kalberg W. O., Robinson L. K., Buckley D., Manning M., Hoyme H. E. Prevalence and epidemiologic characteristics of FASD from various research methods with an emphasis on recent in-school studies. Developmental Disabilities Research Reviews . 2009;15:176–192. doi: 10.1002/ddrr.68. doi:10.1002/ddrr.68. [DOI] [PubMed] [Google Scholar]
- May P. A., Marais A.-S., de Vries M. M., Kalberg W. O., Buckley D., Hasken J. M., Hoyme H. E. The continuum of fetal alcohol spectrum disorders in a community in South Africa: Prevalence and characteristics in a fifth sample. Drug and Alcohol Dependence . 2016b;168:274–286. doi: 10.1016/j.drugalcdep.2016.09.025. doi:10.1016/j.drugalcdep.2016.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May P. A., Marais A.-S., Gossage J. P., Barnard R., Joubert B., Cloete M., Blankenship J. Case management reduces drinking during pregnancy among high-risk women. International Journal of Alcohol and Drug Research . 2013b;2:61–70. doi: 10.7895/ijadr.v2i3.79. doi:10.7895/ijadr.v2i3.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morroni C., Myer L., Moss M., Hoffman M. Preferences between injectable contraceptive methods among South African women. Contraception . 2006;73:598–601. doi: 10.1016/j.contraception.2006.01.005. doi:10.1016/j.contraception.2006.01.005. [DOI] [PubMed] [Google Scholar]
- Parry C., London L., Myers B. Delays in South Africa’s plans to ban alcohol advertising. The Lancet . 2014;383:1972. doi: 10.1016/S0140-6736(14)60954-5. doi:10.1016/S0140-6736(14)60954-5. [DOI] [PubMed] [Google Scholar]
- Pitpitan E. V, Kalichman S. C., Eaton L. A., Cain D., Sikkema K. J., Skinner D., Pieterse D. Gender-based violence, alcohol use, and sexual risk among female patrons of drinking venues in Cape Town, South Africa. Journal of Behavioral Medicine . 2013;36:295–304. doi: 10.1007/s10865-012-9423-3. doi:10.1007/s10865-012-9423-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendall-Mkosi K., Morojele N., London L., Moodley S., Singh C., Girdler-Brown B. A randomized controlled trial of motivational interviewing to prevent risk for an alcohol-exposed pregnancy in the Western Cape, South Africa. Addiction . 2013;108:725–732. doi: 10.1111/add.12081. doi:10.1111/add.12081. [DOI] [PubMed] [Google Scholar]
- South African Medical Research Council 2007South Africa demographic and health survey 2003. Pretoria, South Africa: Department of Health; Retrieved from http://www.mrc.ac.za/bod/sadhs.htm [Google Scholar]
- Taylor M., Kauchali S., Chhagan M., Craib M., Mellins C., Davidson L.2015The AUDIT-C: A better screen than the AUDIT to identify primary child carers at risk of alcohol abuse in the Asenze Study, Kwazulu-Natal, South Africa International Journal of Epidemiology, 44, Supplement 1i136–i137.doi:10.1093/ije/dyv096.143 [Google Scholar]
- Watt M. H., Aunon F. M., Skinner D., Sikkema K. J., Macfarlane J. C., Pieterse D., Kalichman S. C. Alcohol-serving venues in South Africa as sites of risk and potential protection for violence against women. Substance Use & Misuse . 2012a;47:1271–1280. doi: 10.3109/10826084.2012.695419. doi:10.3109/10826084.2012.695419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt M. H., Eaton L. A., Choi K. W., Velloza J., Kalichman S. C., Skinner D., Sikkema K. J. It’s better for me to drink, at least the stress is going away: Perspectives on alcohol use during pregnancy among South African women attending drinking establishments. Social Science & Medicine . 2014;116:119–125. doi: 10.1016/j.socscimed.2014.06.048. doi:10.1016/j.socscimed.2014.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt M. H., Eaton L. A., Dennis A. C., Choi K. W., Kalichman S. C., Skinner D., Sikkema K. J. Alcohol use during pregnancy in a South African community: Reconciling knowledge, norms, and personal experience. Maternal and Child Health Journal . 2016;20:48–55. doi: 10.1007/s10995-015-1800-4. doi:10.1007/s10995-015-1800-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt M. H., Ranby K. W., Meade C. S., Sikkema K. J., MacFarlane J. C., Skinner D., Kalichman S. C. Posttraumatic stress disorder symptoms mediate the relationship between traumatic experiences and drinking behavior among women attending alcohol-serving venues in a South African township. Journal of Studies on Alcohol and Drugs . 2012b;73:549–558. doi: 10.15288/jsad.2012.73.549. doi:10.15288/jsad.2012.73.549. [DOI] [PMC free article] [PubMed] [Google Scholar]