Abstract
Aims
To examine whether the onset of the COVID-19 pandemic led to a change in demand for psychiatric treatment, interest in internet-based therapy, and differences in treatment requests by self-reported diagnoses (e.g., Posttraumatic Stress Disorder, Obsessive Compulsive Disorder, Generalized Anxiety Disorder, and Social Anxiety Disorder).
Methods
Using an interrupted time series design, we analyzed intake questionnaires of treatment-seeking patients (N = 1,954) at an anxiety treatment center between June 6, 2019 through September 13, 2021.
Results
The change in general treatment-seeking from before to immediately after the global pandemic declaration was not statistically significant. However, there was a steady increase in treatment seeking, with a more pronounced increase from 2020 into 2021. Interest in internet-based therapy increased significantly after the onset of COVID-19. The number of treatment-seeking individuals who self-reported “concerns or diagnoses” of PTSD increased significantly.
Conclusion
The study supports anecdotal reports from clinics across the country about unprecedented demand for services. It highlights that many patients experienced an immediate impact of the pandemic on their self-reported concerns about trauma and PTSD symptoms, which has important clinical implications. It also highlights a shifting openness to internet-based services during the pandemic.
Keywords: Anxiety treatment, PTSD treatment, Internet-based treatment
1. Introduction
The COVID-19 global pandemic has led to an increasing demand for mental health services via technology based treatments and a reduction in traditional access to mental health services as many providers were required to move from in-person treatment to completely remote treatment (Silver et al., 2021; Titov et al., 2020; Valdes et al., 2022). Overall, there was a significant increase in demand for access to technology-based services early in the pandemic. For example, a study assessing changes in demand for services between March 19 and April 15, 2020 (N = 1668) by Titov and colleagues (2020) found an 89% increase in website visits and a 90% increase in telephone calls to a digital mental health service providing telephone and online psychological assessments and online interventions.
This increase in demand is affirmed both by practitioners and insurance claims. According to the American Psychological Association's (APA, 2021) COVID-19 practitioner survey, psychologists self-reported a significant increase in individuals seeking treatment for anxiety, trauma, and stress-related disorders from 2019 to 2020 and again from 2020 to 2021. Valdes and colleagues (2022) examined health care utilization and Medicaid claims diagnoses (N = 1589,111) during the first year of the pandemic and found that new diagnoses of anxiety disorders significantly increased among adults. However, the focus of their study was limited to analyzing new cases of anxiety and depression, rather than new cases specific anxiety disorders.
While not a new technology, the COVID-19 pandemic required mental health providers to offer internet-based options for patients. Technology based treatments, both synchronous and asynchronous, offer an opportunity to respond to increased demand by expanding access to those in need of psychiatric care (Greenwood et al., 2022; Lindsay et al., 2014; Silver et al., 2021; Young and Badowski, 2017). Several studies supported the use of internet-based technologies to improve access to mental health services for individuals with posttraumatic stress disorder (PTSD; Acierno et al., 2017; Morland et al., 2017; Sloan et al., 2011), obsessive compulsive disorder (OCD; Aboujaoude, 2017; Pinciotti et al., 2022), generalized anxiety disorder (GAD; Durland et al., 2014), and social anxiety disorder (SAD; Graziano et al., 2021; Isautier et al., 2020; Kraus et al., 2021; Nauphal et al., 2021; Reay et al., 2020). The transition to technology-based treatments has led to improvements in access to treatment. For example, Silver and colleagues (2021) described the effect of the transition from in-person to telehealth appointments at an outpatient mental health clinic in the Northeast United States serving primarily Medicaid and low-income patients (N = 393). They found that there was a significant decrease in missed appointments upon switching to a telehealth model. However, they did not examine whether the onset of the pandemic led to sudden changes in treatment-seeking or differential rates of treatment-seeking by diagnosis.
Many of the studies published on changes in behavioral health treatment due to the onset of the COVID-19 pandemic examined the acute impacts of COVID-19 during the first 3–12 months of the pandemic (Silver et al., 2021; Titov et al., 2020; Valdes et al., 2022; Mahoney et al., 2021; Staples et al., 2021) rather than longer term impacts of the COVID-19 pandemic on treatment-seeking behaviors, which are not explored in the extant literature. Measuring both immediate and ongoing long-term effects of the pandemic on treatment seeking could help health systems understand both temporary and persisting changes in mental health services needs and preferences, as well as prepare for future global catastrophes. Furthermore, improving our understanding of treatment-seeking behaviors among individuals with self-reported symptoms of PTSD, GAD, and OCD in a naturalistic outpatient setting can provide important insight into how to best to prepare for treatment delivery during future catastrophes or pandemics.
We examined the effects of the COVID-19 global pandemic on the demand for psychiatric treatment and openness to internet-based treatments (defined as asynchronous or synchronous telemental health treatment options) at an anxiety specialty clinic using an interrupted time series analytical approach. We aimed to examine whether the onset of the COVID-19 pandemic was associated with a change in demand for psychiatric treatment, interest in internet-based therapy, and differences in treatment requests by self-reported diagnoses (e.g., PTSD, OCD, GAD, and SAD). We hypothesized that the onset of the pandemic would be associated with a significant increase in demand for psychiatric treatment, increased openness to internet-based therapy, and an increase in treatment requests across a variety of self-reported diagnoses.
2. Methods
Participants were treatment-seeking patients (N = 1954) at a specialty anxiety-related disorder cognitive behavioral therapy clinic. The Institutional Review Board at the University of Pennsylvania approved all study methods. Data were collected for 119 weeks, beginning on June 6, 2019 (when we started collecting new patient questionnaires online) through September 13, 2021. Weeks 1–41 were pre-pandemic, and weeks 42–119 occurred post-announcement of COVID-19 as a global pandemic by the World Health Organization (WHO; Table 1 ). Between June 6, 2019 to September 13, 2021, there were a total of 1954 treatment seeking adults (mean age = 32.73, range = 18.01 - 82.63) who filled out a new patient questionnaire in the anxiety specialty treatment center. Only Individuals who completed the new patient questionnaire in full were included in this analysis. All patients who completed the full new patient questionnaire went on to receive a full intake and course of treatment.
Table 1.
Demographics.
| 2019 | 2020 | 2021 | Total | |
|---|---|---|---|---|
| Gender (N,%) | ||||
| Male | 189 (39.6) | 255 (33.8) | 266 (36.8) | 710 (36.3%) |
| Female | 283 (59.3) | 490 (65.0) | 432 (59.8) | 1205 (61.7%) |
|
Gender Non-Conforming / Genderqueer |
4 (0.8) | 5 (0.7) | 18 (2.5) | 27 (1.4) |
| Transgender | 1 (0.2) | 3 (0.4) | 5 (0.7) | 9 (0.5) |
| Something else | 0 (0) | 0 (0) | 1 (0.1) | 1 (0.1) |
| Prefer not to disclose | 0 (0) | 1 (0.1) | 1 (0.1) | 2 (0.1) |
| Age (mean, range) | 30.63 (18.1–72.2) | 33.20 (18.1–77.3) | 33.6(18.0–82.6) | 32.73 (18.0–82.6) |
Note: Data were collected for 119 weeks (June 6, 2019-September 13, 2021). The onset of the COVID-19 pandemic was defined as March 11, 2020, the date the WHO officially declared COVID-19 a global pandemic.
Using an interrupted time series (ITS) design, we examined whether the onset of the COVID-19 pandemic led to a change in treatment seeking in general, a change in interest in internet-based therapy and change in treatment-seeking by self-reported diagnoses (e.g., PTSD, OCD, GAD, and SAD). The onset of the COVID-19 pandemic was defined as March 11, 2020, the date the WHO officially declared COVID-19 a global pandemic.
We analyzed whether, at intake, treatment seeking individuals reported whether they were open to receiving internet-based therapy (“If available in the future, would you be interested in internet-based therapy services, yes or no?”). We also analyzed whether they reported having any of the following “concerns or diagnoses”: PTSD, OCD, GAD, and SAD. This question represents the primary reason individuals were seeking treatment. While we are not suggesting this equates to a valid or reliable diagnosis, we are interested in treatment seeking behaviors in naturalistic settings prior to actual diagnosis.
Interrupted Time series analysis is a statistical methodology commonly used in longitudinal research designs that involves single research units measured repeatedly at regular intervals over a large number of observations followed by a planned or unplanned intervention (in this case, the WHO global pandemic declaration), with additional observations following the intervention (Velicer, 2013).
The autoregressive integrated moving average (ARIMA) model tends to be the most prevalent methodology for time series analyses as it is able to effectively model the effects of dependency from the data series. That is, it can account for the relationship between observations over time (Velicer, 2013). An ARIMA model is comprised of three parameters, (p,d,q; for a more in-depth overview of the parameters, see Box, Jenkins, and Reinsel, 1994) the dependency in the data based on the data points prior to the intervention (p), the difference in nonseasonal observations (d), and the size of the moving average window (q).
While power is increased when the number of data points are equally distributed before and after the intervention, it is not always practical and therefore not a requirement of an ARIMA model given the quasi-experimental nature of this approach (Zhang et al., 2011). We began using the current version of the new patient questionnaire in July 2019 and 41 weeks later was the onset of the COVID-19 pandemic or our ARIMA "intervention." Because 41 weeks post “intervention” would only account for less than a year after the onset of COVID-19, the authors thought it was important to take into account the longer-term effects of the pandemic on self-reported symptoms as these analyses are missing from the extant literature. The ARIMA model was identified using SPSS limiting the data to the cases prior to the onset of COVID-19, which was then used to identify whether the announcement of COVID-19 pandemic was associated with a change in treatment-seeking in general, a preference for internet-based therapy, and a change in treatment seeking by self-reported diagnoses (PTSD, OCD, GAD, and SAD). SPSS determined the ARIMA model of being (0,0,0), demonstrating that there was no dependence between observations. Next, we determined that there were no outliers via inspection of residual Autocorrelation Function and Partial Autocorrelation Function plots. We then conducted the interrupted time series analysis and analyzed the output parameter estimates and calculated the effect size (R2). Percent change from prior to the pandemic to post-onset of pandemic was then calculated based on the ARIMA model time series parameter estimates (t) (i.e., not a comparison of the percent change in raw means).
3. Results
3.1. Demographics
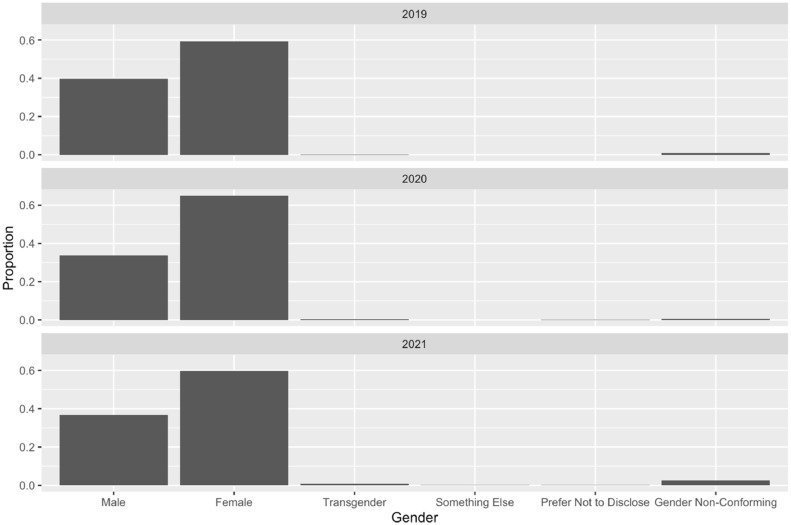
The sample consisted of 1205 women (61.7%), 710 men (36.3%), 9 transgender people (0.5%), 27 who identified as gender-non-conforming or genderqueer (1.4%), 2 individuals who preferred not to disclose (0.1%), and 1 individual who described themselves as “something else” (0.1%). Using Fisher's exact test, we found no significant difference in reported genders pre- or post-global declaration of the COVID-19 pandemic (p = 0.09). There was a significant difference in age from pre- (M = 30.68, SD = 11.09) to post-declaration [(M = 33.73, SD = 12.86); t(1952) = −5.13, p > 0.001]. The current version of the new patient questionnaire was implemented 41 weeks prior to the onset of COVID-19 declaration in July 2019. To account for longer-term changes after the onset of COVID-19, we examined 77 weeks after the global pandemic declaration. However, as mentioned previously, the ARIMA model does not require an equal sample before and after the intervention given the quasi-experimental nature of the ARIMA interrupted time-series analysis approach, and proportions per month were examined (Zhang et al., 2011).
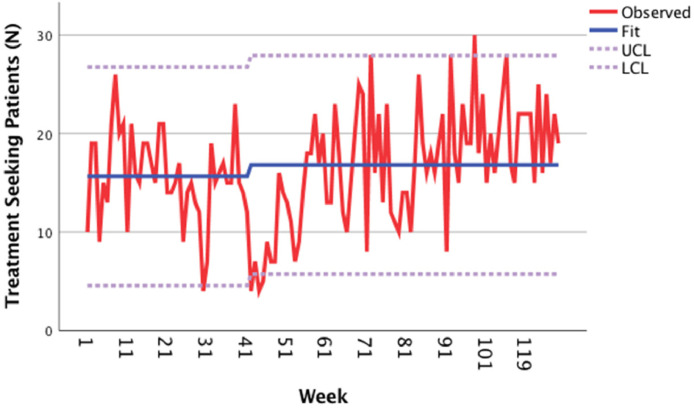
3.2. Interest in services in general
Overall, the change in general treatment-seeking from before to immediately after the global pandemic declaration was not statistically significant (p = 0.29, t = 1.08, R 2 = 0.01; Fig. 1 ). There was however a steady increase in treatment-seeking from 2020 into 2021 (monthly n2019 = 68.14; n2020 = 62.83 n2021 = 85.06). While on average we did not detect a significant change in treatment-seeking per month from 2019 to 2021, there was a greater increase in treatment-seeking by month in the second year of the pandemic (2021). Although we note a slight increase in treatment seeking per month from 2020 to 2021 (monthly n2019 = 40.43; n2020 = 40.83 n2021 = 50.82) among our patients who identified as women, this did not reach statistical significance or drive results.
Fig. 1.
Treatment seeking in general.
Note: UCL = upper confidence limit, LCL = lower confidence limit. Data were collected for 119 weeks (June 6, 2019-September 13, 2021). The onset of the COVID-19 pandemic was defined as March 11, 2020 (i.e. Week 41), the date the WHO officially declared COVID-19 a global pandemic.
(b) Treatment Seeking by Gender.
Furthermore, while we did not have any a priori hypotheses about changes in treatment-seeking by gender identity from 2019 to 2021, as shown in Fig. 1b, we noted an increase in patients who identified as Gender Non-conforming/Genderqueer from 2019 to 2021 (monthly n2019 = 0.57; n2020 = 0.42 n2021 = 2.12) seeking treatment. There was a very slight increase in individuals reporting that they identify as Transgender (monthly n2019 = 0.14; n2020 = 0.25 n2021 = 0.60). The slight increases in both groups did not reach statistical significance (p > 0.05) however.
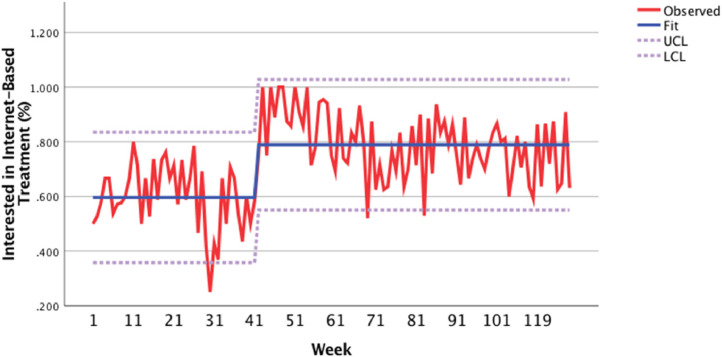
3.3. Interest in internet-based therapy
Following the announcement of COVID-19 as a global pandemic on March 11, 2020, interest in internet-based therapy increased significantly (p < 0.001; see Fig. 2 ). There was a 19.3% increase in interest in internet-based therapy after the announcement of the COVID-19 global pandemic (p = 0.00, t = 8.28, R 2 = 0.36), with a larger increase from 2020 into 2021 (monthly n2019 = 42.43; n2020 = 46.5; n2021 = 64.35).
Fig. 2.
Interest in internet-based treatment.
Note: Data were collected for 119 weeks (June 6, 2019-September 13, 2021). The onset of the COVID-19 pandemic was defined as March 11, 2020 (i.e. week 41), the date the WHO officially declared COVID-19 a global pandemic.
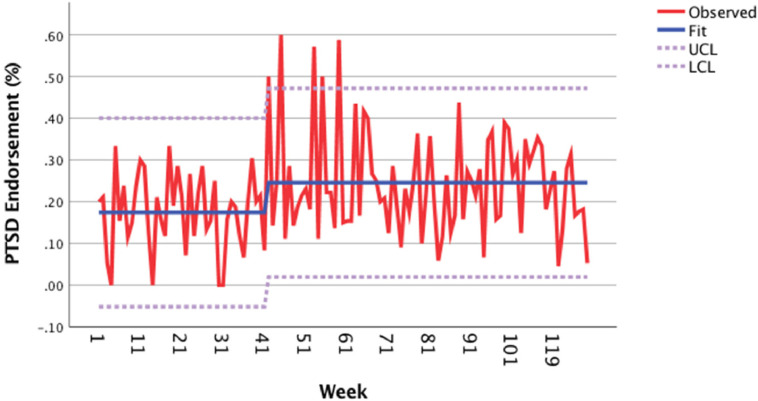
3.4. Self-reported principal diagnoses at time of treatment-seeking
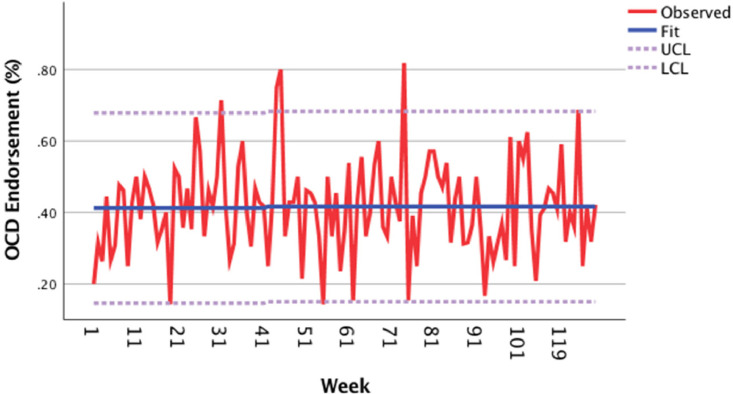
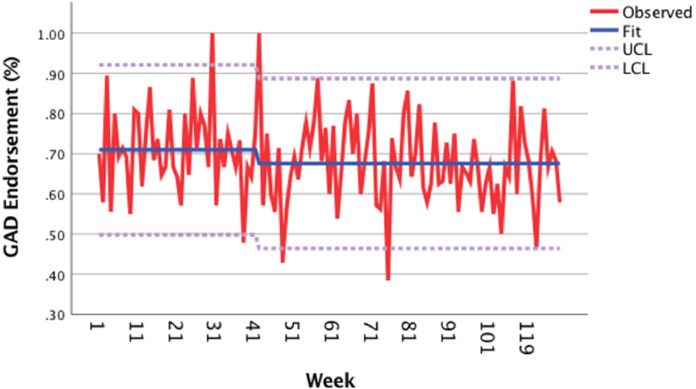
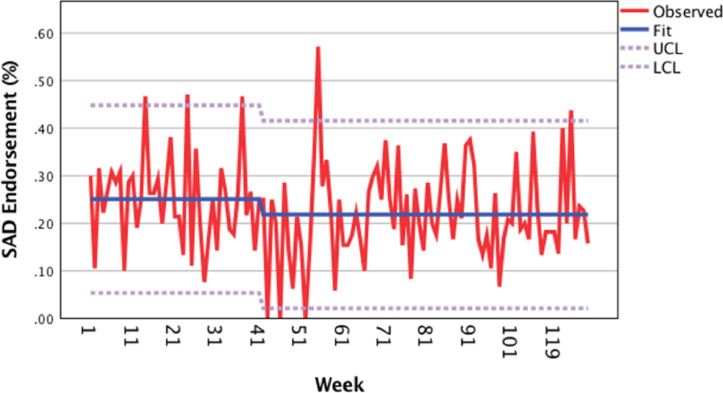
The number of treatment-seeking individuals who endorsed having “concerns or diagnoses” of PTSD (nPTSD 2019 = 12.57 monthly; nPTSD 2020 = 14.33 monthly; nPTSD Jan-Sept. 2021 = 20 monthly) increased significantly by 7.1% from before to after the global pandemic declaration (Fig. 3 a; p < 0.01, t = 3.24, R 2 = 0.10). In contrast, the change in the number of treatment-seeking individuals who endorsed having “concerns or diagnoses” of OCD (Fig. 3b; nOCD 2019 = 26.71 monthly; nOCD 2020 = 26.67 monthly; nOCD Jan-Sept. 2021 = 33.41 monthly; p = 0.87, t = 0.17, R 2 = 0.01), GAD (Fig. 3c; n GAD 2019 = 48.86 monthly; n GAD 2020 = 42.83 monthly; nGAD Jan-Sept. 2021 = 56.11 monthly; p = 0.1, t = −1.66, R 2 = 0.03), and SAD (Fig. 3d; nSAD 2019 = 17.57 monthly; nSAD 2020 = 14.25 monthly; nSAD Jan-Sept. 2021 = 19.17 monthly; p = 0.1, t = −1.68, R 2 = 0.01) was not statistically significant.
Fig. 3.
(a) PTSD endorsement, (b) OCD endorsement, (c) GAD endorsement, (d) Social anxiety disorder endorsement.
Note: Data were collected for 119 weeks (June 6, 2019-September 13, 2021). The onset of the COVID-19 pandemic was defined as March 11, 2020, the date the WHO officially declared COVID-19 a global pandemic.
4. Discussion
In data from this naturalistic study, interest in internet-based services and services for PTSD increased from before to after the WHO official declaration of the COVID-19 global pandemic. These findings were consistent with hypotheses. Contrary to hypotheses, there was not a significant increase in treatment seeking at the point of the pandemic declaration. However, there was a general increase in treatment seeking over time, with a larger increase from 2020 to 2021. There was not a significant change in treatment-seeking for self-reported symptoms of OCD, GAD, or SAD. These findings suggest that the declaration of the pandemic marked a shift in technology-based offerings for mental health and a shift in treatment seeking for trauma-related distress.
There are several possible reasons why we observed a significant interest in internet-based therapy from before to after the global COVID-19 pandemic declaration. Most obviously, individuals were ordered to limit out-of-home activities, and telehealth options became widely available for the first time in history. A possible explanation for the increased interest could be increased comfort with video conferencing software, which proliferated in use across the workforce and entertainment industry, in addition to healthcare, at the time of the pandemic declaration. The ubiquity of video conference software may have resulted in increased comfort with technology compared to before the pandemic. Notably, 22.63% of individuals did not endorse interest in internet-based treatment after the point of the declaration. This may have been due to reluctance or resistance to the treatment modality (e.g., due to privacy concerns). Alternatively, this might suggest that increased interest in internet-based services may not have been purely based on logistical considerations. More research is needed to determine factors that may influence reluctance or acceptance of this modality in different contexts and among different clinical populations.
The significant increase in treatment seeking for PTSD and trauma-related distress from before to after the global COVID-19 pandemic mirrors a number of anecdotal reports in the media about the trauma of the pandemic. To be clear, we do not know whether individuals were reporting the pandemic as traumatic or if they had previous trauma for which symptoms were exacerbated. Furthermore, given that the data is self-reported, we do not know whether treatment seekers experienced a recent Criterion A trauma that would be necessary for a PTSD diagnosis or whether their Criterion A trauma was relevant to the pandemic. Some individuals seeking psychiatric treatment may have experienced the onset of the pandemic as traumatic (especially as it relates to grief and loss from the virus). Others may have experienced an exacerbation in pre-existing PTSD symptoms, especially with increased attention toward racial trauma (Carter, 2007; Carter et al., 2020; Comas-Díaz et al., 2019; Kirkinis et al., 2018) and other psychosocial stressors that might have increased baseline anxiety, including job or food insecurity (Fang et al., 2021). Regardless, the nature of the question posed to potential patients did not change from before to after the pandemic declaration, and yet patients reported a marked increase in interest in PTSD-related mental health care during this transition.
Consistent with widespread media reports, there was a nearly 25% increase in monthly new patient contacts in 2021 (85.06 per month) compared to 2019 (68.14 per month). However, the timing of the global pandemic declaration was not associated with a significant increase in general treatment seeking, and monthly inquiries dipped from 2019 (68.14 per month) to 2020 (62.83 per month). There are a number of logistical explanations for this dip. In the first weeks of the pandemic, many clinics (including the one from which these data were extracted) temporarily ceased initial intake appointments. While this pause was not advertised on our website, it is possible that providers who typically referred patients to our clinic during that stretch delayed their referrals. It is also possible that for some individuals during the pandemic, there were delayed mental health effects that only emerged after the acute phase of the lockdowns expired. This is consistent with epidemiological studies that reported a worsening of mental health disorder prevalence in the second and third quarter of the pandemic, even beyond the prevalence in the immediate aftermath of the onset (Gan et al., 2020; Jia, 2021). Consistent with this possibility, while the onset of the global pandemic was associated with a significant increase in treatment seeking for PTSD, 2021 (20 monthly) had even higher monthly numbers of individuals seeking PTSD care than 2020 (14.3 monthly). Similar effects were observed for OCD, for which there was an increase in treatment seeking from 2020 (26.71 monthly) to 2021 (33.41 monthly). However, the change in OCD from before to after the onset of the pandemic was not statistically significant, suggesting that increased treatment seeking for OCD evolved over time rather than immediately after the pandemic declaration.
There was a notable increase in treatment seeking among patients who identified as Genderqueer/Gender non-conforming, particularly in the second year of the pandemic. Treatment seeking among Genderqueer/Gender non-conforming and Transgender individuals did not reach statistical significance, possibly due to low power given that our clinic is not an LBTQ+ specialty clinic. While examining the change in treatment-seeking among this population was not a primary aim of our study, it is still a notable change that merits discussion in light of several studies demonstrating the effect of the COVID-19 pandemic on the mental health of gender non-binary/non-conforming, genderqueer, and transgender individuals (Kidd et al., 2021; Krause, 2021; Salerno et al., 2020).
There are a number of important limitations of this study. First, the data reflect treatment seeking at a specialized anxiety disorder treatment center, which may not reflect trends in generalized practices or practices with other specialty areas. Second, patients indicated their reasons for treatment seeking using a self-reported checklist. Due to a number of logistical factors (insurance, need for immediate services, matching of patient preferences to therapists), not all patients who completed the new patient questionnaire received services at our center. Therefore, we cannot determine the accuracy of patients’ self-reported description of their chief concerns compared to a clinical interview. Another limitation was the fact that in the new patient questionnaire, in terms of demographic information, patients are only asked to report gender identity and age. At the time of the data collection, the new patient questionnaires did not ask about racial or ethnic identity, as a more in-depth demographic report is completed at the phone screen and formal intake. This information may be useful in understanding how generalizable our findings are. There are several methodological limitations that restrict the conclusions that can be drawn from this study. However, results still meaningfully contribute to the literature as they speak to how the onset of COVID-19 may have impacted self-reports of PTSD in a naturalistic setting. Lastly, the global pandemic was marked by waxing and waning surges of cases on different timeframes at different regions in the world. While it would have been interesting to explore multiple discrete time-periods, we made an a priori decision to focus this exploration on the declaration of the global pandemic due to the abrupt policy and social changes in many domains that occurred immediately after the declaration by the WHO. This was essential in our dataset as patients occasionally seek treatment for services from our center from across the nation and the world, where waves of case increases varied over time.
The study has a number of important findings for consideration. The study confirms anecdotal reports from clinics across the country unprecedented demand for services, often resulting in long waitlists. It highlights that a number of patients experienced an immediate impact of the pandemic on their self-reported concerns about trauma and PTSD symptoms. It also highlights a shifting openness to internet-based services during the pandemic. Prior to the pandemic, our clinic rarely offered telehealth; after the global declaration, telehealth became the modal treatment. Nevertheless, not all patients expressed interest in internet-based services even at the height of the pandemic. This reflects shifting interests in internet services but an ongoing need for availability of in-person options. In-person options could continue to be important for patients who live in homes without a private location for therapy or who wish to discuss sensitive subject matters that they do not want family/housemates overhearing.
In summary, our study demonstrated a robust increase in telehealth therapy from before to immediately after the global declaration of the COVID-19 pandemic. There was a slight increase in treatment seeking in general from 2019–2021 with a significant increase in treatment seeking for self-reported trauma and PTSD. Future research should continue to follow trends in treatment-seeking, especially for PTSD, as the pandemic continues. This will inform preparedness for mental health services to respond in the face of the changing COVID-19 pandemic and future catastrophes.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data are available upon request.
Role of funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Gabriella E. Hamlett: Conceptualization, Methodology, Formal analysis, Writing – original draft, Writing – review & editing, Visualization. Jeremy Tyler: Writing – review & editing, Data curation. Keith Bredemeier: Conceptualization, Supervision, Writing – review & editing. Emily Ballentine: Writing – original draft, Writing – review & editing. Lily A. Brown: Conceptualization, Supervision, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
All authors have no conflicts of interest to disclose.
References
- Aboujaoude E. Three decades of telemedicine in obsessive-compulsive disorder: a review across platforms. J. Obsessive Compuls. Relat. Disord. 2017;14:65–70. doi: 10.1016/j.jocrd.2017.06.003. [DOI] [Google Scholar]
- Acierno R., Knapp R., Tuerk P., Gilmore A.K., Lejuez C., Ruggiero K., Muzzy W., Egede L., Hernandez-Tejada M.A., Foa E.B. A non-inferiority trial of prolonged exposure for posttraumatic stress disorder: in person versus home-based telehealth. Behav. Res. Ther. 2017;89:57. doi: 10.1016/j.brat.2016.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- APA. (2021). 2021 COVID-19 practitioner survey. https://www.apa.org/pubs/reports/practitioner/covid-19-2021.
- Carter R.T. Racism and psychological and emotional injury: recognizing and assessing race-based traumatic stress. Couns. Psychol. 2007;35(1):13–105. doi: 10.1177/0011000006292033. [DOI] [Google Scholar]
- Carter R.T., Kirkinis K., Johnson V.E. Relationships between trauma symptoms and race-based traumatic stress. Traumatology (Tallahass Fla) 2020;26(1):11–18. doi: 10.1037/trm0000217. [DOI] [Google Scholar]
- Comas-Díaz L., Hall G.N., Neville H.A. Racial trauma: theory, research, and healing: introduction to the special issue. Am. Psychol. 2019;74(1):1. doi: 10.1037/amp0000442. [DOI] [PubMed] [Google Scholar]
- Durland L., Interian A., Pretzer-Aboff I., Dobkin R.D. Vol. 105. 2014. Effect of telehealth-to-home interventions on quality of life for individuals with depressive and anxiety disorders. (Smart Homecare Technol. Telehealth). [DOI] [Google Scholar]
- Fang D., Thomsen M.R., Nayga R.M. The association between food insecurity and mental health during the COVID-19 pandemic. BMC Public Health. 2021;21(1):1–8. doi: 10.1186/s12889-021-10631-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan H., Zhang Y., Yuan M., Wu X.Y., Liu Z.R., Liu M., Wu J.B., Xu S.J., Gong L., Xu H.L., Tao F.B. Epidemiological analysis on 1,052 cases of COVID-19 in epidemic clusters. Zhonghua Liu Xing Bing Xue Za Zhi. 2020:1004–1008. doi: 10.3760/cma.j.cn112338-20200301-00223. [DOI] [PubMed] [Google Scholar]
- Graziano S., Boldrini F., Righelli D., Francesco M., Vincenzina L., Quittner A., Tabarini P. Psychological interventions during COVID pandemic: telehealth for individuals with cystic fibrosis and caregivers. Pediatr. Pulmonol. 2021;56(7):1976–1984. doi: 10.1002/ppul.25413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwood, H., Krzyzaniak, N., Peiris, R., Clark, J., Scott, A.M., Cardona, M., Griffith, R., & Glasziou, P. (2022). Telehealth versus face-to-face psychotherapy for less common mental health conditions: systematic review and meta-analysis of randomized controlled trials. https://mental.jmir.org/2022/3/e31780. [DOI] [PMC free article] [PubMed]
- Isautier J.M., Copp T., Ayre J., Cvejic E., Meyerowitz-Katz G., Batcup C., Bonner C., Dodd R., Nickel B., Pickles K., Cornell S., Dakin T., McCaffery K.J. People's experiences and satisfaction with telehealth during the COVID-19 pandemic in Australia: cross-sectional survey study. J. Med. Internet Res. 2020;22(12):e24531. doi: 10.2196/24531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia H. National and state trends in anxiety and depression severity scores among adults during the COVID-19 pandemic—United States. MMWR Morb. Mortal. Wkly. Rep. 2021;70:2020–2021. doi: 10.15585/mmwr.mm7040e3. [DOI] [PubMed] [Google Scholar]
- Kirkinis K., Pieterse A.L., Martin C., Agiliga A., Brownell A. Racism, racial discrimination, and trauma: a systematic review of the social science literature. Ethn. Health. 2018 doi: 10.1080/13557858.2018.1514453. [DOI] [PubMed] [Google Scholar]
- Kidd J.D., Jackman K.B., Barucco R., Dworkin J.D., Dolezal C., Navalta T.V., Bockting W.O. Understanding the impact of the COVID-19 pandemic on the mental health of transgender and gender nonbinary individuals engaged in a longitudinal cohort study. J. Homosex. 2021;68(4):592–611. doi: 10.1080/00918369.2020.1868185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause K.D. Implications of the COVID-19 pandemic on LGBTQ communities. J. Public Health Manag. Pract. 2021;27:S69–S71. doi: 10.1097/PHH.0000000000001273. [DOI] [PubMed] [Google Scholar]
- Kraus S., Jones P., Kailer N., Weinmann A., Chaparro-Banegas N., Roig-Tierno N. Digital transformation: an overview of the current state of the art of research. Sage Open. 2021 doi: 10.1177/21582440211047576. [DOI] [Google Scholar]
- Lindsay J.A., Kauth M.R., Hudson S., Martin L.A., Ramsey D.J., Daily L., Rader J. Implementation of video telehealth to improve access to evidence-based psychotherapy for posttraumatic stress disorder. Telemed. E-Health. 2014;21(6):467–472. doi: 10.1089/tmj.2014.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney A., Li I., Haskelberg H., Millard M., Newby J.M. The uptake and effectiveness of online cognitive behaviour therapy for symptoms of anxiety and depression during COVID-19. J. Affect. Disord. 2021;292:197–203. doi: 10.1016/j.jad.2021.05.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland L., Greene C., Rosen C., Kuhn E., Hoffman J., Sloan D. Telehealth and eHealth interventions for posttraumatic stress disorder. Curr Opin Psychol. 2017;14 doi: 10.1016/j.copsyc.2016.12.003. [DOI] [PubMed] [Google Scholar]
- Nauphal M., Swetlitz C., Smith L., Rosellini A. A Preliminary Examination of the Acceptability, Feasibility, and Effectiveness of a Telehealth Cognitive-Behavioral Therapy Group for Social Anxiety Disorder. Cogn Behav Pract. 2021;28(4):730–742. doi: 10.1016/j.cbpra.2021.04.011. [DOI] [Google Scholar]
- Pinciotti C., Bulkes N., Horvath G., Riemann B. Efficacy of intensive CBT telehealth for obsessive-compulsive disorder during the COVID-19 pandemic. J. Obsessive Compuls. Relat. Disord. 2022;32 doi: 10.1016/j.jocrd.2021.100705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reay R.E., Looi J.C., Keightley P. Telehealth mental health services during COVID-19: summary of evidence and clinical practice. Australas. Psychiatry. 2020;28(5):514–516. doi: 10.1177/1039856220943032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salerno J.P., Devadas J., Pease M., Nketia B., Fish J.N. Sexual and gender minority stress amid the COVID-19 pandemic: implications for LGBTQ young persons’ mental health and well-being. Public Health Rep. 2020;135(6):721–727. doi: 10.1177/0033354920954511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silver Z., Coger M., Barr S., Drill R. Psychotherapy at a public hospital in the time of COVID-19: telehealth and implications for practice. Couns. Psychol. Q. 2021;34(3–4):499–507. doi: 10.1080/09515070.2020.1777390. [DOI] [Google Scholar]
- Sloan D.M., Gallagher M.W., Feinstein B.A., Lee D.J., Pruneau G.M. Efficacy of telehealth treatments for posttraumatic stress-related symptoms: a meta-analysis. Cogn. Behav. Ther. 2011 doi: 10.1080/16506073.2010.550058. https://www.tandfonline.com/doi/abs/10.1080/16506073.2010.550058 [DOI] [PubMed] [Google Scholar]
- Staples L., Nielssen O., Kayrouz R., Cross S., Karin E., Ryan K., Dear B., Titov N. Rapid report 3: mental health symptoms, characteristics, and regional variation, for users of an Australian digital mental health service during the first 8 months of COVID-19. Internet Interv. 2021;24 doi: 10.1016/j.invent.2021.100378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N., Staples L., Kayrouz R., Cross S., Karin E., Ryan K., Dear B., Nielssen O. Rapid report_ Early demand, profiles and concerns of mental health users during the coronavirus (COVID-19) pandemic | Elsevier Enhanced Reader. Internet Interv. 2020;21 doi: 10.1016/j.invent.2020.100327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valdes E.G., Gorman J.M., Ren Y., Bowling M., Steiner L., Bethea J., Aamar R., Andel R., Reist C. Behavioral health diagnoses and health care use before and during the COVID-19 pandemic. Psychiatr. Serv. 2022 doi: 10.1176/appi.ps.202100133. [DOI] [PubMed] [Google Scholar]
- Young J.D., Badowski M.E. Telehealth: increasing access to high quality care by expanding the role of technology in correctional medicine. J. Clin. Med. 2017;6(2):20. doi: 10.3390/jcm6020020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang F., Wagner A.K., Ross-Degnan D. Simulation-based power calculation for designing interrupted time series analyses of health policy interventions. J. Clin. Epidemiol. 2011;64(11):1252–1261. doi: 10.1016/j.jclinepi.2011.02.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon request.