Abstract
Background
Limited evidence exists on the impact of the Coronavirus Disease 2019 (COVID-19) pandemic on hospital efficiency worldwide. This study aimed to investigate the impact of the COVID-19 pandemic on public hospitals in Iran.
Methods
In this quasi-experimental study, monthly data on the average length of stay (ALoS), bed occupancy rate (BOR), bed turnover rate (BTR) and bed turnover interval (BTI) were collected for 58 months (36 months before and 22 months after the COVID-19 outbreak in Iran) from the health information systems of all 18 public hospitals affiliated with Kermanshah University of Medical Sciences in Kermanshah province, Iran. We used interrupted time series analysis and the Pabon Lasso model to investigate the impact of the COVID-19 pandemic on hospital efficiency.
Results
The monthly average ALoS, BOR, BTR and BTI before (after) the COVID-19 pandemic was 3.30 (3.48) days, 70.14% (49.37), 6.78 (4.81) patients per bed and 1.15 (2.88) days, respectively. The study indicated that a statistically significant decrease in ALoS of 0.29 and BOR of 25.09 in the first month following the COVID-19 pandemic. Compared with the before pandemic period, we observed a significant increase in the monthly trend of ALoS (coefficient = 0.021; p = 0.015), BOR (coefficient = 1.30; p = 0.002), and BTR (coefficient = 0.08, p = 0.012). We found a significant decrease in the monthly trend in BTI (coefficient = –0.11, p = 0.009) after the COVID-19 pandemic when compared with before the pandemic. Based on the Pabon Lasso model, before (after) the pandemic, 29.4% (29.4%) of the hospitals were located in zone 1 as an inefficient area, and 17.6% (35.3%) of hospitals were located in zone 3 as an efficient area.
Conclusion
The study demonstrated that the BOR and BTR decreased substantially after the outbreak of COVID-19. In contrast, the ALoS and BTI have significantly increased following the COVID-19 pandemic. We also found that hospitals’ performance in both periods was poor, and only 30% of hospitals were located in the efficient zone (zone three) based on the Pabon Lasso model. Further studies aimed at identifying the main factors affecting lower efficiency among hospitals in Iran are recommended.
Keywords: COVID-19 pandemic, Hospital efficiency, Pabon Lasso model, Interrupted time series analysis, Iran
INTRODUCTION
The Coronavirus Disease 2019 (COVID-19) was first diagnosed in Wuhan, China, in late December 2019, and it has spread with incredible speed throughout the world [1]. On 11 March, 2020, the World Health Organization (WHO) declared it as a pandemic, and it stated that this is the first pandemic caused by a coronavirus [2]. In Iran, the first death occurred by the COVID-19 was confirmed in Qom province on 19 February, 2020 and quickly spread to other provinces of Iran [3]. The COVID-19 pandemic has resulted in health and economic crises with a significant impact on the delivery of healthcare worldwide [4]. The pandemic has disrupted healthcare utilization [5,6], delayed initial diagnosis and treatment, increased demand for telehealth [7,8] and hospital services [9,10]. A significant reduction in the number of persons seeking medical care during the COVID-19 outbreak [11-15] suggests that the pandemic is impacting the behavior of entire populations in relation to willingness to receive care among non-COVID patients [16]. Hospitals have also reported unexplained reductions in admissions for severe medical illnesses [17]. In a systematic review study on the impact of COVID-19 pandemic on health care utilization, Moynihan et al. [18] showed showed a 30% decrease in health care utilization by 30%. The reduction in health care utilization was found to be higher among people with less severe illnesses.
Hospitals in all countries, regardless of development status, have undoubtedly been affected in a number of areas during the COVID-19 pandemic. Evaluating changes in hospital performance will enable us to better prepare for future crises and design cost-effective interventions for the optimal use of limited resources in the health sector. To date, only limited studies aim to assess the effect of COVID-19 pandemic on the efficiency of hospitals in other developing and developed countries [19,20]. To the best of our knowledge, the effect of the COVID-19 pandemic on Iran’s hospitals is not documented in the literature. In this study, we aimed to examine the impact of COVID-19 pandemic on the efficiency of hospitals affiliated with the Kermanshah University of Medical Sciences (KUMS) in the Kermanshah province in the west of Iran.
MATERIALS AND METHODS
1. Study setting
This was a quasi-experimental and descriptive-analytical study carried out in Kermanshah province, located in the western region of Iran. The province’s total population was estimated to be approximately two million in the year 2016. The province has 18 hospitals affiliated with KUMS that are responsible for the provision of most inpatient services.
2. Data and study population
All 18 hospitals affiliated with KUMS were used in the study. Using a self-constructed checklist, monthly data on the number of active beds, number of inpatients, occupied bed-days and active bed-days were collected from the health information system (HIS) of hospitals. Data were collected for a period of 58 months (36 months before and 22 months after the COVID-19 outbreak. Since the first confirmed case of the COVID-19 was reported on 19 February 2020 in Iran, we used data from 19 February, 2017 to 18 February, 2020 as pre-pandemic period and 19 February, 2020 to 21 December, 2021 as post-pandemic period.
As per previous studies [21,22], we used four indicators viz., average length of stay (ALoS), bed occupancy rate (BOR), bed turnover rate (BTR) and bed turnover interval (BTI) as measures of hospital efficiency. We used the collected data and the following formulas to calculate these efficiency indicators.
3. Data analysis
We used two models to examine the impact of the COVID-19 pandemic on hospital efficiency, including interrupted time series analysis (ITSA) and the Pabon Lasso model. We used the following segmented regression to estimate the effect of the COVID-19 outbreak on four hospital efficiency indicators included in the study [23,24]:
Yt = β0 + β1 * timet + β2 * COVID19t + β3 * timeafterCOVID19t + εt
Where Yt presents hospital efficiency indicator (e.g., ALoS) in the month t, timet is time trend variable that takes values between 1 (first observation) and 58 (last observation). The COVID19t is a binary variable for before (COVID19 = 0) and after (COVID19 = 1) the outbreak. The timeafterCOVID19t variable is assigned 0 for the period before the COVID-19 outbreak and coded between 1 and 22 for the period after the COVID-19 outbreak. In the model, β0 estimates the starting level of the outcome variable at time zero, β1 estimates the monthly change in the outcome variable before the COVID-19 outbreak (the pre-existing trend); β2 estimates the level change in the indicators immediately after the COVID-19 outbreak, and β3 estimates the monthly change in the outcome variable trend after COVID-19, compared with the pre-existing trend. The Newey-West approach was used to handle autocorrelation and possible heteroscedasticity [23,25] in the estimation. All data analysis related to ITSA model was performed using Stata statistical software, and 0.05 was considered a significant level (Ver-sion 16.0; Stata Corporation, College Station, TX, USA). Data on 18 hospitals was used in ITSA.
Pabon Lasso model was also used to determine the relative performance of the hospitals in terms of three efficiency indicators: ALoS, BOR and BTR [26]. In the Pabon Lasso model, interpretation of hospital performance is based on a chart that displays BOR on the Y-axis and BTR on the X-axis. Each hospital can be located in one zone out of four zones (Fig. 1). The definitions and interpretations of the four zones in the Pabon Lasso chart are given in Fig. 1. Since one of the hospitals was established after the outbreak of the COVID-19 pandemic, it was excluded from the Pabon Lasso analysis, and the data for 17 hospitals were included. Excel software was used to construct the Pabon Lasso graph.
Fig. 1.
Pabon Lasso graph illustrating the relative performance of hospitals.
RESULTS
The summary of the variables included in the study are reported in Table 1. The overall mean (standard deviation [SD]) of ALoS, BOR, BTR and BTI was 3.37 (0.25), 62.26 (13.00), 6.03 (1.14) and 1.81 (1.14), respectively, during the study period. The mean of ALOS before the COVID-19 pandemic was 3.30 (SD = 0.15), while it was 3.48 (0.33) for the period after the pandemic.
Table 1.
Summary of variables included in the study
| Total period of the study (Mean ± SD) | Before the pandemic (Mean ± SD) | After the pandemic (Mean ± SD) | |
|---|---|---|---|
| ALoS (days) | 3.37 ± 0.25 | 3.30 ± 0.15 | 3.48 ± 0.33 |
| BOR (%) | 62.26 ± 13.00 | 70.14 ± 5.88 | 49.37 ± 11.00 |
| BTR | 6.03 ± 1.14 | 6.78 ± 0.54 | 4.81 ± 0.70 |
| BTI (days) | 1.81 ± 1.14 | 1.15 ± 0.28 | 2.88 ± 1.21 |
SD: standard deviation, ALoS: average length of stay, BOR: bed occupancy rate, BTR: bed turnover rate, BTI: bed turnover interval.
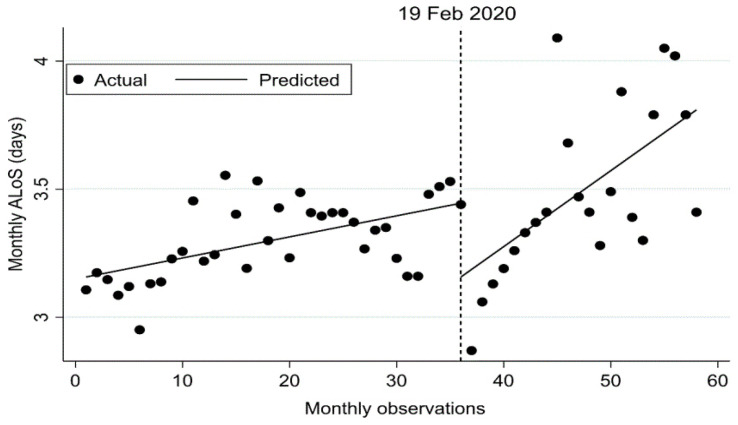
Our study indicated 3.15 days as the starting level of the ALoS (see Table 2). The ALoS statistically significantly increased by 0.0008 per month (p = 0.005) before the COVID-19 pandemic. We also found a statistically significant decrease in ALoS of 0.29 (p = 0.013) in the first month of the COVID-19 pandemic. Compared with the before the pandemic, we observed a significant increase in the monthly trend of ALoS at 0.021 (p = 0.015). The results for ALoS for the period before and after the COVID-19 pandemic have been illustrated in Fig. 2.
Table 2.
Estimated coefficients of segmented regression model for average length of stay (ALoS, days) before and after COVID-19 pandemic in Iran
| Variables | Coefficient | SE* | p-value | CI (95%) | |
|---|---|---|---|---|---|
|
| |||||
| Lower | Upper | ||||
| Intercept, β0 | 3.15 | 0.05 | < 0.001 | 3.05 | 3.25 |
| Pre-COVID-19 slope, β1 | 0.008 | 0.003 | 0.005 | 0.002 | –0.062 |
| Change in slope, β2 | –0.29 | 0.11 | 0.013 | –0.51 | –83.50 |
| Change in trend, β3 | 0.021 | 0.008 | 0.015 | 0.004 | 0.038 |
| Post-COVID-19 linear trend† | |||||
| Linear trend, βp1 | 0.029 | 0.008 | 0.0004 | 0.013 | 0.045 |
SE: standard error, CI: confidence interval.
*Newey-West standard errors.
†This obtained from the following time trend Equation: Ypt = βp0 + βp1 * timept + εt where Ypt is the value of ALoS at time t after the COVID-19 pandemic and timept is the time trend variable which takes values between 1 (first observation after the pandemic) and 22 (last observation after the pandemic).
Fig. 2.
Interrupted time series analysis with Newey–West standard errors and two lags for ALoS. Note: The date of the first confirmed case of COVID-19 in Iran (19 February, 2020) was used as the start of the pandemic period.
The results of BOR are shown in Table 3 and Fig. 3. As shown in Table 3, the starting level of the BOR was estimated at 75.95 (p = 0.001). The BOR was significantly decreasing by 0.33 (p = 0.002) per month prior to the pandemic outbreak. We observed that in the first month of the pandemic, BOR was significantly decreased by 25.09 (p = 0.001), followed by a significant increase in the monthly trend of BOR (compared to the before pandemic) of 1.30 (p = 0.002). After the COVID-19 pandemic, BOR significantly increased by 0.97 (p = 0.016) per month.
Table 3.
Estimated coefficients of segmented regression model for bed occupancy rate (BOR, %) before and after COVID-19 pandemic in Iran
| Variables | Coefficient | SE* | p-value | CI (95%) | |
|---|---|---|---|---|---|
|
| |||||
| Lower | Upper | ||||
| Intercept, β0 | 75.95 | 1.87 | < 0.001 | 72.20 | 79.71 |
| Pre-COVID-19 slope, β1 | –0.33 | 0.10 | 0.002 | –0.53 | –0.12 |
| Change in slope, β2 | –25.09 | 4.90 | < 0.001 | –34.93 | –15.25 |
| Change in trend, β3 | 1.30 | 0.39 | 0.002 | 0.52 | 2.08 |
| Post-COVID-19 linear trend† | |||||
| Linear trend, βp1 | 0.97 | 0.37 | 0.016 | 0.226 | 1.729 |
SE: standard error, CI: confidence interval.
*Newey-West standard errors.
†This obtained from the following time trend Equation: Ypt = βp0 + βp1 * timept + εt where Ypt is the value of BOR at time t after the COVID-19 pandemic and timept is the time trend variable which takes values between 1 (first observation after the pandemic) and 22 (last observation after the pandemic).
Fig. 3.
Interrupted time series analysis with Newey–West standard errors and two lags for BOR. The date of the first confirmed case of COVID-19 in Iran (19 February, 2020) was used as the start of the pandemic period.
As reported in Table 4, the starting level of the BTR was estimated at 7.26. The BTR decreased by 0.03 (p = 0.001) per month before the COVID-19 pandemic. A statistically significant increase in BTR of 1.99 (p = 0.001) was observed in the first month of the pandemic. Compared with the period before the pandemic, we observed a significant increase in the monthly trend of BTR (coefficient = 0.08, p = 0.012). Segmented regression results also indicated that after the COVID-19 pandemic, the BTR increased monthly at the rate of 0.05 (p = 0.07). Fig. 4 provides a visual display of these results for the period before and after the COVID-19 pandemic.
Table 4.
Estimated coefficients of segmented regression model for bed turnover rate (BTR) before and after COVID-19 pandemic in Iran
| Variables | Coefficient | SE* | p-value | CI (95%) | |
|---|---|---|---|---|---|
|
| |||||
| Lower | Upper | ||||
| Intercept, β0 | 7.26 | 0.21 | < 0.001 | 6.83 | 7.69 |
| Pre-COVID-19 slope, β1 | –0.03 | 0.009 | < 0.001 | –2.74 | –1.25 |
| Change in slope, β2 | 1.99 | 0.37 | < 0.001 | –34.93 | –15.25 |
| Change in trend, β3 | 0.08 | 0.03 | 0.012 | 0.02 | 0.14 |
| Post-COVID-19 linear trend† | |||||
| Linear trend, βp1 | 0.05 | 0.03 | 0.07 | –0.006 | 0.11 |
SE: standard error, CI: confidence interval.
*Newey-West standard errors.
†This obtained from the following time trend Equation: Ypt = βp0 + βp1 * timept + εt where Ypt is the value of BTR at time t after the COVID-19 pandemic and timept is the time trend variable which takes values between 1 (first observation after the pandemic) and 22 (last observation after the pandemic).
Fig. 4.
Interrupted time series analysis with Newey–West standard errors and two lags for BTR. Note: The date of the first confirmed case of COVID-19 in Iran (19 February, 2020) was used as the start of the pandemic period.
Results also demonstrated that BTI was 1.00 at the starting month of the study period (see Table 5). There was no significant change in the BTI (p = 0.07) during the period before the COVID-19 pandemic. The estimated proportion of the BTI increased by 2.69 (p = 0.001) in the first month following the pandemic outbreak. We observed a significant decrease in the monthly trend of the BTI after the COVID-19 pandemic compared with the before the pandemic period (p = 0.009). Furthermore, the BTI decreased every month at the rate of 0.10 (p = 0.01) during the COVID-19 outbreak period. Fig. 5 provides a visual illustration of these results for the period before and after the pandemic.
Table 5.
Estimated coefficients of segmented regression model for bed turnover interval (BTI, days) before and after COVID-19 pandemic in Iran
| Variables | Coefficient | SE* | p-value | CI (95%) | |
|---|---|---|---|---|---|
|
| |||||
| Lower | Upper | ||||
| Intercept, β0 | 1.00 | 0.10 | < 0.001 | 0.79 | 1.20 |
| Pre-COVID-19 slope, β1 | 0.008 | 0.004 | 0.074 | –0.0008 | 0.02 |
| Change in slope, β2 | 2.69 | 0.54 | < 0.001 | 1.59 | 3.78 |
| Change in trend, β3 | –0.11 | 0.04 | 0.009 | –0.20 | –0.03 |
| Post-COVID-19 linear trend† | |||||
| Linear trend, βp1 | –0.10 | 0.04 | 0.01 | –0.18 | –0.02 |
SE: standard error, CI: confidence interval.
*Newey-West standard errors.
†This obtained from the following time trend Equation: Ypt = βp0 + βp1 * timept + εt where Ypt is the value of BTR at time t after the COVID-19 pandemic and timept is the time trend variable which takes values between 1 (first observation after the pandemic) and 22 (last observation after the pandemic).
Fig. 5.
Interrupted time series analysis with Newey–West standard errors and two lags for BTI. Note: The date of the first confirmed case of COVID-19 in Iran (19 February, 2020) was used as the start of the pandemic period.
The results of the Pabon Lasso model on hospital efficiency are illustrated in Fig. 6. Hospitals were located in four performance zones. Panels A and B in Fig. 5 show the location of hospitals before and after the COVID-19 pandemic, respectively. The results for the period before the COVID-19 pandemic suggest that 29.4% (five) of hospitals were located in zone 1, 17.6% (three) of hospitals were located in zone 2, 17.6% (three) of hospitals were located in zone 3, and 23.5% (four) of hospitals were located in zone 4. One hospital was located exactly on the border between zones 1 and 2 and another was exactly on the border between zones 2 and 3. After the pandemic, 29.4% (five) of hospitals were in zone 1, 11.8% (two) of hospitals were in zone 2, 35.3% (six) of hospitals were in zone 3 and 29.4% (four) of hospitals were in zone 4. We also observed that one hospital was located exactly on the border between zones 3 and 4.
Fig. 6.
A Pabon Lasso graph for 17 hospitals affiliated with the Kermanshah University of Medical Sciences before and after the COVID-19 pandemic.
DISCUSSION
The COVID-19 pandemic has affected the performance and efficiency of hospitals and the extent to which people use health services [27]. In this study, we investigated the effect of COVID-19 outbreak on the efficiency of public hospitals in western part of Iran. As per previous studies [21,22,28], four indicators, including BOR, BTR, ALoS and BTI were used to assess the hospital performance.
Our study suggested increasing trends in ALoS before and after the COVID-19 pandemic. The rate of increase in ALoS was found to be higher after the outbreak compared to before the outbreak. The ALoS was significantly reduced in the first month following the outbreak of the disease. The significant decrease in the first month after the COVID-19 pandemic can be attributed to the fear of people getting the infection and trying to get an early discharge by both patients and providers. The increase in the ALoS in the months after the outbreak of COVID-19 can be explained by the fact that patients with mild diseases have delayed their hospitalization until after the end of the pandemic. The longer length of hospital stay of COVID-19 patients compared to patients with other diseases [29] might have contributed to the increase in the ALoS after the pandemic.
As a measure to evaluate the utilization of hospital beds, the BOR represents the efficiency in the use of hospital beds. Our results showed that BOR had a significantly decreasing trend in the months following the COVID-19 pandemic compared to before the pandemic. The reduction in BOR in the first month after the pandemic outbreak was about 30%. The Ministry of Health and Medical Education (MOHME) in Iran classifies the performance of hospitals into three groups based on the BOR: satisfactory performance (70% and above), somehow satisfactory performance (60-70%) and not satisfactory performance (less than 60%) [26]. The average BOR in the pre-pandemic period was about 70%, while the corresponding figure was around 50% after the COVID-19 pandemic. This indicates the under-utilization of health care resources in public hospitals in Kermanshah province during the COVID-19 pandemic as compared with the period before the pandemic. One of the main reasons for the decrease in the BOR in the hospitals during the pandemic is a decrease in the hospitalization rates for non-COVID disease [30-32]. Reduction in hospital admission was documented during the pandemic in some countries [30]. This reduction in hospital admission can be attributed to the factors such as rationing of the medical workforce and the fear people to seeking hospital care.
Our study also indicated that after the outbreak of the COVID-19 pandemic, the BTR decreased while the BTI increased. BTR measure the number of patients hospitalized per bed at a specific time (in this study, one month). BTI shows the average number of days that hospital beds are unoccupied between successive inpatients over a given period, such as month or year (in this study, month). The BTR and BTI can assess the productivity of hospital beds. The lower value of BTR and higher value of BTI in a hospital suggest that a hospital is less efficient. The results of BTR and BTI indicated a high level of inefficiency and poor performance of hospitals for beds utilization.
We also used the Pabon Lasso model to assess overall hospital efficiency before and after the COVID-19 pandemic. The Pabon Lasso model enabled us to simultaneously evaluate hospital efficiency using the three indicators of ALoS, BOR and BTR. Our study indicated that before (after) the COVID-19 pandemic, 29.4% (n = 5) of hospitals were in zone 1: an inefficient zone characterized by low BOR, high ALoS and low BTR. Hospitals in this zone experience under-utilization of hospitals beds. We also found that before the COVID-19 pandemic, 17.6% of hospitals were in zone 3 while 35.3% of hospitals were in this zone during the COVID-19 pandemic period. The zone 3 is the efficient zone that characterized by high BOR, high BTR and short ALoS. Hospitals in zone 3 have satisfactory performance with the small number of unoccupied beds [33].
The current study had some limitations that should be considered in interpreting the findings. Firstly, this study was conducted in one province, so the generalizability of the results is limited. Secondly, we only used public hospitals data to assess the impact of the COVID-19 pandemic on hospital efficiency. Since data on Social Security Organi-zation and private hospitals are not available to include in the analysis, the study results are not generalizable for these hospitals. Thirdly, we examined the impact of the COVID-19 pandemic on indicators of hospital efficiency three years before and approximately two years after (22 months) of the pandemic. Future studies are required to investigate the long-term impact of the COVID-19 pandemic on hospital performance.
CONCLUSION
This study aimed to investigate and compare the efficiency of public hospitals in Kermanshah province, the western part of Iran, using ITSA and the Pabon Lasso model before and after the COVID-19 pandemic in Iran. The study demonstrated that the BOR and BTR decreased substantially after the outbreak of COVID-19 disease compared with before the pandemic. In contrast, the ALoS and BTI have significantly increased following the COVID-19 pandemic. These findings suggest the inefficient use of public hospital beds in Iran. As less than a third of public hospitals were classified as efficient hospitals (zone three) based on the Pabon Lasso model before and after the outbreak of COVID-19, further studies aimed at identifying the main factors affecting inefficiency among public hospitals are needed.
ACKNOWLEDGEMENTS
This study received a grant from the Kermanshah University of Medical Sciences (Grant number: 4010052). The ethics committee of the Deputy of Research at Kermanshah University of Medical Sciences reviewed and approved the study protocol (IR.KUMS.REC.1400.856). The funder did not have any role in the design of the study, and in the collection, analysis, interpretation of data, and in the write-up of the manuscript.
Footnotes
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
References
- 1.Karimi SE, Ahmadi S, SoleimanvandiAzar N. Inequities as a social determinant of health: Responsibility in paying attention to the poor and vulnerable at risk of COVID-19. J Public Health Res. 2021;10(1):1904. doi: 10.4081/jphr.2021.1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio Medica. 2020;91(1):157–60. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salimi R, Gomar R, Heshmati B. The COVID-19 outbreak in Iran. J Glob Health. 2020;10(1):010365. doi: 10.7189/jogh.10.010365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bernacki K, Keister A, Sapiro N, Joo JS, Mattle L. Impact of COVID-19 on patient and healthcare professional attitudes, beliefs, and behaviors toward the healthcare system and on the dynamics of the healthcare pathway. BMC Health Serv Res. 2021;21(1):1–9. doi: 10.1186/s12913-021-07237-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang Y-N, Chen Y, Wang Y, Li F, Pender M, Wang N, Yan F, Ying XH, Tang SL, Fu CW. Reduction in healthcare services during the COVID-19 pandemic in China. BMJ Global Health. 2020;5(11):e003421. doi: 10.1136/bmjgh-2020-003421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yan H, Li X, Lu X, Zeng S, Yuan Y, Hu X, Zhu Y, Xiao Z. Changes in pediatric healthcare utilization in Hunan Province, China, during the COVID-19 pandemic: a multi-center cross-sectional study. Transl Pediatr. 2021;10(4):870–81. doi: 10.21037/tp-20-465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Madden N, Emeruwa UN, Friedman AM, Aubey JJ, Aziz A, Baptiste CD, Coletta JM, D'Alton ME, Fuchs KM, Goffman D, Gyamfi-Bannerman C, Kondragunta S, Krenitsky N, Miller RS, Nhan-Chang CL, et al. Telehealth uptake into prenatal care and provider attitudes during the COVID-19 pandemic in New York City: a quantitative and qualitative analysis. Am J Perinatol. 2020;37(10):1005–14. doi: 10.1055/s-0040-1712939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arora P, Mehta D, Ha J. Impact of telehealth on health care resource utilization during the COVID-19 pandemic. J Comp Eff Res. 2021;11(5):301–9. doi: 10.2217/cer-2021-0242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moore LD, Robbins G, Quinn J, Arbogast JW. The impact of COVID-19 pandemic on hand hygiene performance in hospitals. Am J Infect Control. 2021;49(1):30–3. doi: 10.1016/j.ajic.2020.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Melman G, Parlikad A, Cameron E. Balancing scarce hospital resources during the COVID-19 pandemic using discrete-event simulation. Health Care Manag Sci. 2021;24(2):356–74. doi: 10.1007/s10729-021-09548-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Angoulvant F, Ouldali N, Yang DD, Filser M, Gajdos V, Rybak A, Guedj R, Soussan-Banini V, Basmaci R, Lefevre-Utile A, Brun-Ney D, Beaujouan L, Skurnik D. Coronavirus Disease 2019 2019 pandemic: impact caused by school closure and national lockdown on pediatric visits and admissions for viral and nonviral infections—a time series analysis. Clin Infect Dis. 2021;72(2):319–22. doi: 10.1093/cid/ciaa710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang ZM, Wu MY, Lu JM, Li TZ, Shen P, Tang ML, Jin MJ, Lin HB, Shui LM, Chen K, Wang JB. Effect of COVID-19 on hospital visits in Ningbo, China: an interrupted time-series analysis. Int J Qual Health Care. 2021;33(2):mzab078. doi: 10.1093/intqhc/mzab078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M, Lam YM, Chan C, Tsang TC, Tsui M, Tse HF, Siu CW. Impact of coronavirus disease 2019 (COVID‐19) outbreak on outcome of myocardial infarction in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2021;97(2):E194–7. doi: 10.1002/ccd.28943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJJEhj. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41(19):1852–3. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, Gundlapalli AV. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mantica G, Riccardi N, Terrone C, Gratarola A. Non-COVID-19 visits to emergency departments during the pandemic: the impact of fear. Public Health. 2020;183:40–1. doi: 10.1016/j.puhe.2020.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP, Mancone M, Mercuro G, Muscoli S, Nodari S, Pedrinelli R, Sinagra G, Indolfi C. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41(22):2083–8. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, Jones M, Kitchener E, Fox M, Johansson M, Lang E, Duggan A, Scott I, Albarqouni L. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021;11(3):e045343. doi: 10.1136/bmjopen-2020-045343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kamel MA, Mousa ME-S. Measuring operational efficiency of isolation hospitals during COVID-19 pandemic using data envelopment analysis: a case of Egypt. Benchmarking An Int J. 2021;28:2178–201. doi: 10.1108/BIJ-09-2020-0481. [DOI] [Google Scholar]
- 20.Pecoraro F, Luzi D, Clemente F. The efficiency in the ordinary hospital bed management: A comparative analysis in four European countries before the COVID-19 outbreak. PLoS One. 2021;16(3):e0248867. doi: 10.1371/journal.pone.0248867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rezaei S, Hajizadeh M, Nouri B, Ahmadi S, Rezaeian S, Salimi Y, Karyani AK. Iranian hospital efficiency: a systematic review and meta-analysis. Int J Health Care Qual Assur. 2019;32(2):385–97. doi: 10.1108/IJHCQA-03-2018-0067. [DOI] [PubMed] [Google Scholar]
- 22.Amini S, Karami Matin B, Didehdar M, Alimohammadi A, Salimi Y, Amiresmaili M, Kazemi-Karyani A. Efficiency of Iranian hospitals before and after health sector evolution plan: a systematic review and meta-analysis study. Front Public Health. 2021;9:727669. doi: 10.3389/fpubh.2021.727669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wagner AK, Soumerai SB, Zhang F, Ross‐Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 24.Rashidian A, Joudaki H, Khodayari-Moez E, Omranikhoo H, Geraili B, Arab M. The impact of rural health system reform on hospitalization rates in the Islamic Republic of Iran: an interrupted time series. Bull World Health Organ. 2013;91:942–9. doi: 10.2471/BLT.12.111708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Linden A. Conducting interrupted time-series analysis for single-and multiple-group comparisons. Stata Journal. 2015;15(2):480–500. doi: 10.1177/1536867X1501500208. [DOI] [Google Scholar]
- 26.Rezaei S, Hajizadeh M, Bazyar M, Karyani AK, Jahani B, Matin BK. The impact of health sector evolution plan on the performance of hospitals in Iran: evidence from the Pabon Lasso model. Int J Health Gov. 2018;23(2):111–9. doi: 10.1108/IJHG-09-2017-0046. [DOI] [Google Scholar]
- 27.Howarth A, Munro M, Theodorou A, Mills PR. Trends in healthcare utilisation during COVID-19: a longitudinal study from the UK. BMJ Open. 2021;11(7):e048151. doi: 10.1136/bmjopen-2020-048151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ajlouni MM, Zyoud A, Jaber B, Shaheen H, Al-Natour M, Anshasi RJ. The relative efficiency of Jordanian public hospitals using data envelopment analysis and Pabon Lasso diagram. Glob J Bus Res. 2013;7(2):59–72. [Google Scholar]
- 29.Rees EM, Nightingale ES, Jafari Y, Waterlow NR, Clifford S, B Pearson CA, Group CW, Jombart T, Procter SR, Knight GM. COVID-19 length of hospital stay: a systematic review and data synthesis. BMC Med. 2020;18(1):270. doi: 10.1186/s12916-020-01726-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kalanj K, Marshall R, Karol K, Tiljak MK, Orešković S. The Impact of COVID-19 on Hospital Admissions in Croatia. Front Public Health. 2021;9:720948. doi: 10.3389/fpubh.2021.720948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oseran AS, Nash D, Kim C, Moisuk S, Lai PY, Pyhtila J, Sequist TD, Wasfy JH. Changes in hospital admissions for urgent conditions during COVID-19 pandemic. Am J Manag Care. 2020;26(8):327–8. doi: 10.37765/ajmc.2020.43837. [DOI] [PubMed] [Google Scholar]
- 32.Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The impact of the COVID-19 pandemic on hospital admissions in the United States: study examines trends in US hospital admissions during the COVID-19 pandemic. Health Aff. 2020;39(11):2010–7. doi: 10.1377/hlthaff.2020.00980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aloh HE, Onwujekwe OE, Aloh OG, Nweke CJ. Is bed turnover rate a good metric for hospital scale efficiency? A measure of resource utilization rate for hospitals in Southeast Nigeria. Cost Eff Resour Alloc. 2020;18(1):1–8. doi: 10.1186/s12962-020-00216-w. [DOI] [PMC free article] [PubMed] [Google Scholar]