Abstract
Background and Aims:
Tracking specific drugs contributing to drug overdose deaths is limited when relying on death certificate (DC) data alone. This study aimed to determine whether integrating DC data with medical examiner/coroner reports, including postmortem toxicology and death investigation findings, would enhance identification of (1) heroin and pharmaceutical morphine involvement in overdose deaths and (2) fentanyl source (illicitly manufactured versus pharmaceutical).
Design:
Retrospective analysis of heroin, pharmaceutical morphine, illicitly manufactured fentanyl (IMF) and pharmaceutical fentanyl involvement in fatal overdoses. DC and toxicology data were compared with enhanced definitions integrating overdose scene, witness and toxicology evidence.
Setting:
United States: 38 states and the District of Columbia, participating in Centers for Disease Control and Prevention (CDC)-funded opioid overdose death surveillance.
Cases:
Opioid overdose decedents from funded jurisdictions; deaths during 1 January 2018–31 December 2019.
Measurements:
Using medical examiner/coroner report data, deaths with 6-acetylmorphine and/or morphine detected by postmortem toxicology were defined as confirmed, probable or suspected heroin deaths, or probable pharmaceutical morphine deaths. Fentanyl was defined as probable or suspected IMF or probable pharmaceutical fentanyl.
Findings:
The enhanced definition defined 18 393 deaths as confirmed, probable, or suspected heroin deaths (including 2678 with morphine listed as cause of death on the DC) and 404 as probable pharmaceutical morphine deaths. Among deaths with fentanyl detected, 89.3% were defined as probable or suspected IMF and 1.0% as probable pharmaceutical fentanyl. Fentanyl source could not be determined for 9.7% of deaths.
Conclusions:
Integrating drug overdose scene, witness and toxicology findings can improve identification of specific drugs contributing to overdose deaths and enhance overdose intervention targeting.
Keywords: Fentanyl, heroin, morphine, opioids, overdose, toxicology
INTRODUCTION
In 2019, 70.6% of 70 630 drug overdose deaths in the United States involved opioids [1]; illicit opioids account for a substantial portion of opioid overdose deaths. Specifically, fentanyl [primarily illicitly manufactured fentanyl (IMF)] was the drug most frequently involved in overdose deaths in the United States in 2017 [2], and a 2019 multistate study estimated that more than two-thirds of opioid overdose deaths during January–June 2018 involved IMF [3]. While heroin overdose deaths slightly declined from 2017 to 2019, heroin was involved in 14 019 overdose deaths, or 28% of all opioid overdose deaths, in 2019 [1]. Tracking overdose deaths involving heroin and IMF is challenging, however, because US death certificate (DC) data, considered the gold standard for tracking drug overdose deaths, underestimate heroin involvement [4–8] and do not distinguish between IMF and pharmaceutical fentanyl [9].
Medical examiners can definitively identify drug overdose deaths on the DC as involving heroin when its primary metabolite, 6-acetylmorphine (6-AM), is detected by postmortem toxicology testing [10, 11]. Heroin itself is generally not tested for because it rapidly metabolizes (half-life = 2–6 minutes) to 6-AM; however, 6-AM is a metabolite unique to heroin, and is widely accepted as confirmation of heroin use [11]. Because 6-AM rapidly metabolizes (half-life = 6–25 minutes) to morphine, however, many overdose deaths involving heroin have morphine detected but not 6-AM [12]. Drug overdose death investigation guidelines indicate that ME/Cs can conclude heroin use when morphine but not 6-AM is detected by considering death scene evidence such as injection drug paraphernalia or heroin use history [11]. Heroin is much more prevalent in the illicit drug market than pharmaceutical morphine; therefore, evidence of injection drug paraphernalia is probably indicative of heroin use in the absence of pharmaceutical morphine use evidence [13]. ME/Cs may, however, be reluctant to indicate heroin involvement without detection of 6-AM because of legal consequences or stigma associated with heroin use [14]. In such scenarios, morphine may be listed as cause of death on the DC, reflecting postmortem toxicology findings without further interpretation (i.e. recognizing that morphine caused death without indicating whether it was detected because of pharmaceutical morphine use or because it metabolized from heroin).
Including only morphine on the DC when heroin may have been involved in a drug overdose death can result in three types of misclassifications when using DC data: (1) undercounting heroin deaths, (2) overcounting pharmaceutical morphine deaths and (3) overcounting prescription opioid deaths. The National Center for Health Statistics uses the International Classification of Diseases, 10th revision (ICD-10) system to classify DC cause of death information into six opioid subcategories [15]. When morphine is listed on the DC as a cause of death it is grouped into the natural and semi-synthetic opioids subcategory, which includes common prescription opioid pain relievers. This is problematic, because studies in the United States [4–6] and other countries [7, 8] found that death investigation evidence (e.g. drug paraphernalia, decedent’s drug use history) indicates that most deaths with morphine detected probably involved heroin instead of pharmaceutical morphine. Consequently, ICD-10 coding probably underestimates heroin deaths and overestimates pharmaceutical morphine deaths. Also, overdose deaths involving prescription opioids are probably overestimated because the ICD-10 natural and semi-synthetic opioids category is commonly used as a proxy for overdoses involving prescription opioids [16]. These three classification biases are potentially large: in 2017, 4800 drug overdose deaths, or approximately 10% of opioid overdose deaths, involved morphine [2].
The DC also does not systematically record the source of fentanyl (pharmaceutical or IMF) involved in overdose deaths. Postmortem toxicology testing results alone cannot indicate fentanyl source. While most fentanyl overdose deaths appear to involve IMF, some involve pharmaceutical fentanyl [17]. Identifying fentanyl source is important because different intervention approaches, such as tailoring prescribing practices or outreach for people at high risk for IMF exposure, may differ by fentanyl type.
Previous studies found that integrating ME/C report data, including full toxicology and investigative findings, with DC data may improve surveillance of heroin deaths [10–14]. Building from this work, the current analysis used data from CDC’s State Unintentional Drug Overdose Reporting System (SUDORS), which integrates data from ME/C reports and DCs, to implement enhanced definitions of overdose deaths involving heroin, pharmaceutical morphine, IMF and pharmaceutical fentanyl. The aims of this study were to generate and apply definitions using these integrated data to improve drug classification for overdose deaths, to determine whether previous findings were generalizable to a large number of states and to document the strength of the evidence supporting the enhanced definitions.
METHODS
Data source
CDC’s SUDORS program has funded state health departments and the District of Columbia to abstract DC and ME/C report data on unintentional and undetermined intent opioid overdose deaths since 2016. Jurisdictions submitted data twice yearly for 6-month increments of deaths (January–June and July-December) with a lag of 8–13 months after the date of death. For this report, 39 of 48 funded jurisdictions (38 states: Alaska, Arizona, California, Colorado, Connecticut, Delaware, Florida, Georgia, Illinois, Indiana, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Missouri, Montana, Nevada, New Hampshire, New Jersey, New Mexico, North Carolina, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Dakota, Tennessee, Utah, Vermont, Virginia, Washington, West Virginia, Wisconsin; and the District of Columbia) with complete data for at least one 6-month period during 1 January 2018–31 December 2019 were included. The nine remaining jurisdictions were not funded for the analysis period (five jurisdictions) or had not successfully submitted any data (four jurisdictions). Thirty-one jurisdictions reported all opioid overdose deaths within the jurisdiction, while seven states reported deaths within a subset of counties accounting for at least 75% of that state’s 2017 overdose deaths, per CDC reporting requirements.
Data were entered into a secure web-based platform [18] that captures DC information, overdose-specific contextual and circumstance data and data on all drugs and drug metabolites detected by postmortem toxicology, even those not ruled by a ME/C to have contributed to death.
Enhanced heroin/morphine definition
Opioid overdose deaths with: (1) postmortem toxicology results available, (2) 6-AM and/or morphine detected and (3) heroin and/or morphine listed as cause of death on the DC were defined as confirmed, probable or suspected heroin deaths, as probable pharmaceutical morphine deaths or as unknown morphine source deaths using full postmortem toxicology testing results and scene, witness and autopsy evidence of drug use, respectively. The definition was applied independently of ME/C cause of death classification (i.e. as heroin, morphine or both) to allow for comparison with the ME/C cause of death classification for each mutually exclusive defined category.
A hierarchical approach was used to define the categories (Figure 1). First, confirmed heroin deaths (category 1) were defined by detection of 6-AM [11], irrespective of other available evidence. Secondly, deaths with no 6-AM detected were defined as probable pharmaceutical morphine deaths (category 2) if there was evidence of pharmaceutical morphine use such as witness report or physical evidence at the overdose scene. Thirdly, in the absence of 6-AM detection and evidence of pharmaceutical morphine use, deaths were defined as probable heroin deaths (category 3) if: (1) heroin use history was documented (e.g. via witness report); (2) common heroin adulterants or impurities (quinine, procaine, xylazine, noscapine, papaverine, thebaine or acetylcodeine) [19] were detected by postmortem toxicology testing; or (3) there was evidence of injection drug use (e.g. needles/syringes at the scene, recent track-marks on the decedent). Injection drug use evidence was included because heroin is often injected [4]. Fourthly, deaths not meeting criteria for confirmed or probable heroin, or for probable pharmaceutical morphine, were defined as suspected heroin deaths (category 4) if there was scene (e.g. drug powders or illicit drug packaging) or toxicology (detection of cocaine, methamphetamine or illicit fentanyl analogs) evidence of illicit drug use, because heroin is often co-used with other illicit drugs [4]. Finally, deaths not captured in any category were defined as unknown morphine source deaths (category 5).
FIGURE 1.
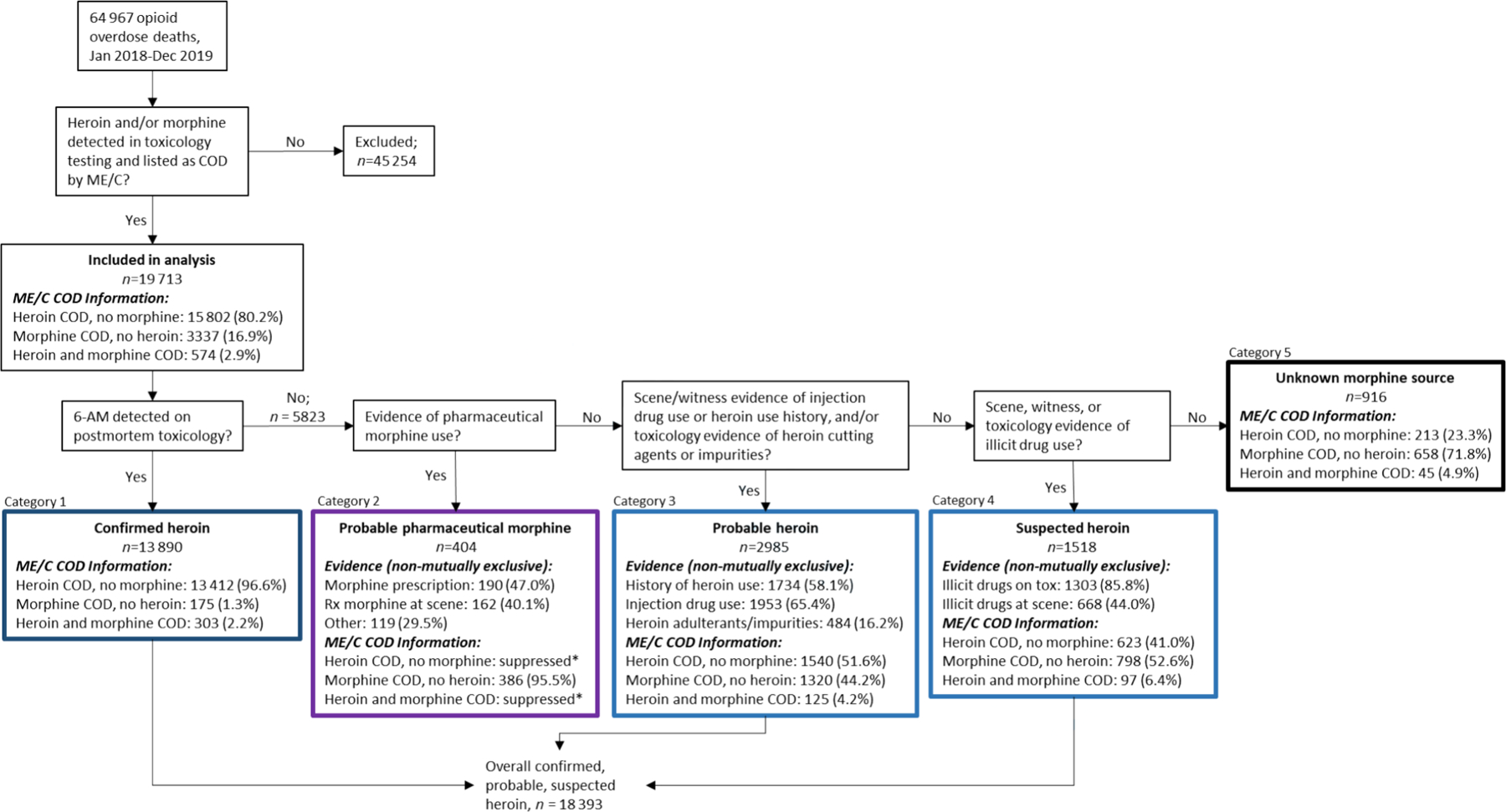
Flow-chart indicating how the enhanced heroin/morphine definition assigns deaths to each of the confirmed, probable and suspected heroin; probable pharmaceutical morphine; and unknown morphine source categories. COD = cause of death; ME/C = medical examiner/coroner; 6-AM = 6-acetylmorphine
Enhanced fentanyl source definition
Using postmortem toxicology testing results and scene, witness and autopsy evidence, source of fentanyl or norfentanyl detected or indicated as a cause of death was defined as probable IMF, suspected IMF, probable pharmaceutical fentanyl or unknown source fentanyl following a hierarchical approach (Figure 2). First, fentanyl was defined as probable IMF (category 1) if any fentanyl analog was detected, irrespective of other evidence, because nearly all fentanyl analogs are illicit [20] and are often mixed or co-used with IMF [3]; co-use of illicit fentanyl analogs with pharmaceutical fentanyl was considered unlikely. Fentanyl was also defined as probable IMF if any precursor used in IMF production was detected (e.g. 4-ANPP) [21].
FIGURE 2.
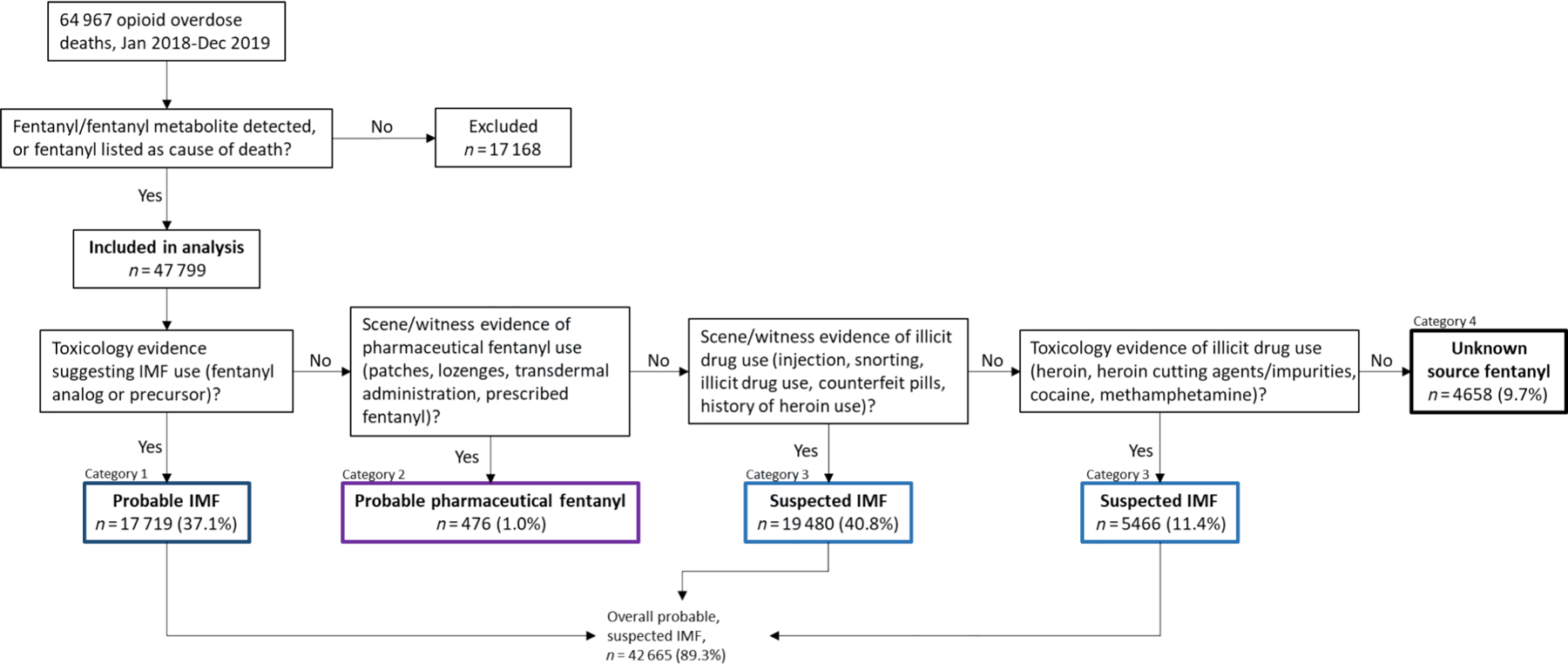
Flow-chart indicating how the enhanced fentanyl source definition assigns deaths to each of the probable and suspected illicitly manufactured fentanyl; probable pharmaceutical fentanyl; and unknown source fentanyl categories. IMF = illicitly manufactured fentanyl
Secondly, fentanyl detected in the absence of fentanyl analogs and precursors was defined as probable pharmaceutical fentanyl (category 2) when: (1) transdermal patches or packaging, or lozenges, were found at the scene or on the body; (2) there was witness report of using transdermal patches, lozenges or pharmaceutical fentanyl; or (3) there was evidence that the decedent was prescribed fentanyl (e.g. via witness report or prescription drug monitoring program data). Pharmaceutical fentanyl is sold in multiple forms such as transdermal patches and lozenges [17].
Thirdly, fentanyl not defined as probable IMF or probable pharmaceutical fentanyl was defined as suspected IMF (category 3) if evidence indicated illicit drug use, which is more suggestive of IMF use than pharmaceutical fentanyl use. Illicit drug use evidence included: (1) evidence the decedent injected or snorted drugs; (2) death scene documentation of drug powders or crystal, illicit drug packaging or counterfeit pills; (3) reported heroin use history; or (4) detection of 6-AM, common heroin adulterants or impurities, cocaine or methamphetamine. Fourthly, fentanyl not captured in any category was defined as unknown source fentanyl (category 4).
Analysis
The number of deaths that occurred during 1 January 2018 to 31 December 2019 in all 39 jurisdictions for each heroin/morphine and fentanyl source category was calculated. Each defined heroin/morphine category was compared to the ME/C cause of death classification on the DC (i.e. listing heroin, morphine or both).
RESULTS
Heroin/morphine
Among 64 967 opioid overdose deaths that occurred during 1 January 2018 to 31 December 2019, 19 713 deaths met inclusion criteria for the heroin/morphine definition (postmortem toxicology results available, 6-AM and/or morphine detected, and heroin and/or morphine listed as cause of death on the DC). Among those 19 713 deaths, the ME/C listed heroin but not morphine as cause of death for 80.2%, morphine but not heroin for 16.9% and both heroin and morphine in < 3% of deaths.
Using the enhanced definition, 13 890 deaths were defined as confirmed heroin deaths because 6-AM was detected (Figure 1, category 1). The ME/C listed heroin but not morphine as cause of death on the DC for 96.6% of these deaths and morphine for < 5% (2.2% with and 1.3% without heroin). Among 5823 deaths with no 6-AM detected, 404 (6.9%), 2985 (51.3%), 1518 (26.1%) and 916 (15.7%) deaths were defined as probable pharmaceutical morphine (category 2), probable heroin (category 3), suspected heroin (category 4) and unknown morphine source deaths (category 5), respectively. For most deaths (95.5%) defined as probable pharmaceutical morphine, the ME/C listed morphine but not heroin as cause of death on the DC; too few deaths had heroin listed as cause of death to report because of suppression rules. ME/C cause of death information was more evenly split between heroin and morphine for deaths defined as probable and suspected heroin deaths, with heroin but not morphine listed for 51.6 and 41.0% of deaths, respectively, and morphine but not heroin listed for 44.2 and 52.6% of deaths, respectively. Just 4.2 and 6.4% of deaths in the probable and suspected heroin categories had both heroin and morphine listed as cause of death on the DC. Nearly three-quarters (71.8%) of deaths in the unknown morphine source category had morphine but not heroin listed as cause of death. Overall, a combined 93.3% of deaths (n = 18 393) were defined as more likely heroin (confirmed, probable or suspected) compared to 2.0% (n = 404) defined as more likely pharmaceutical morphine; for 4.6% of deaths (n = 916), the source of morphine could not be determined (Figure 3).
FIGURE 3.
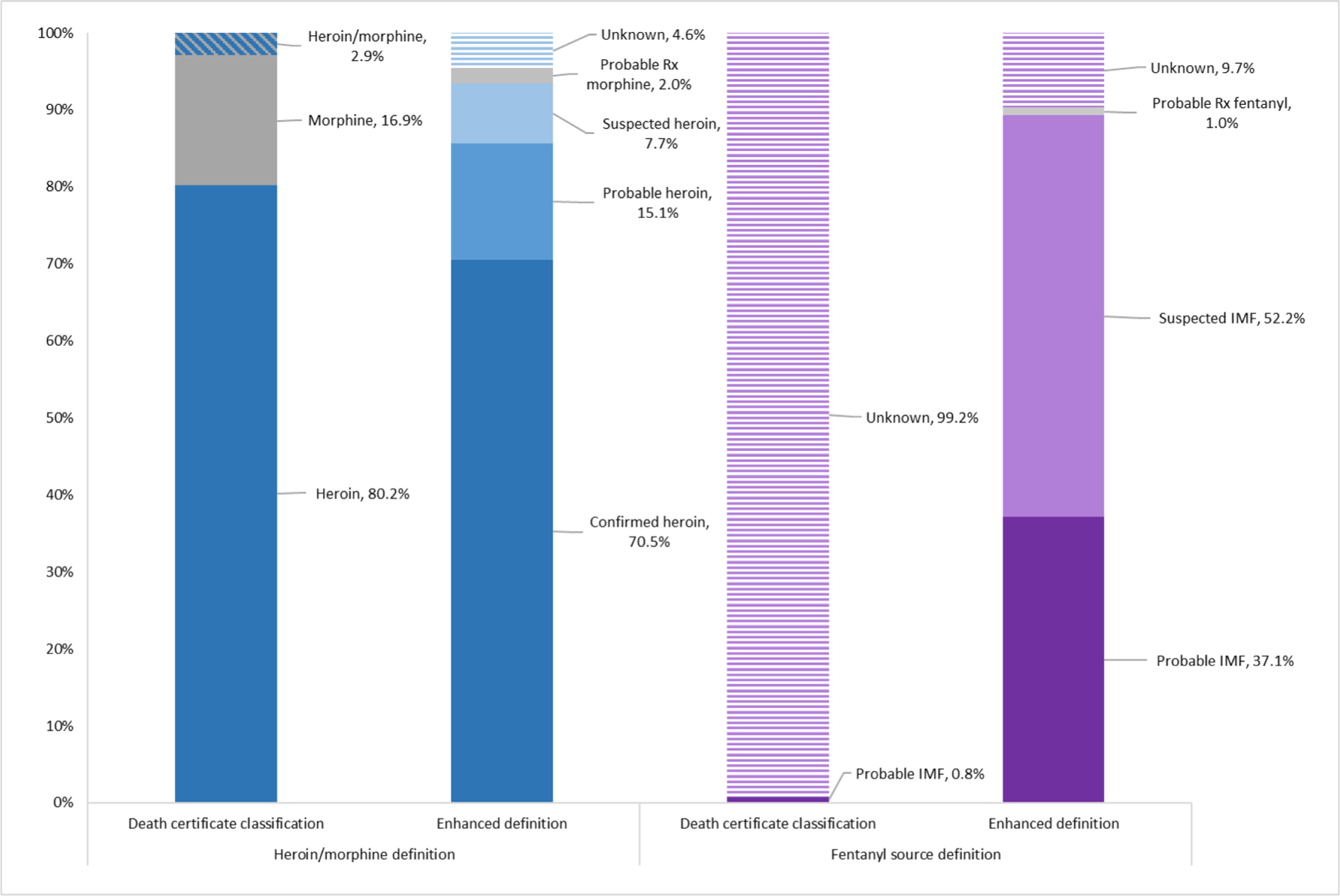
Defined involvement of heroin and pharmaceutical morphine and defined fentanyl source in drug overdose deaths compared to death certificate classifications. IMF = illicitly manufactured fentanyl; Rx = prescription (pharmaceutical)
Fentanyl source
Fentanyl or norfentanyl was detected or listed as cause of death in 47 799 (73.6%) of 64 967 opioid overdose deaths (Figure 2). Of these 47 799 deaths, fentanyl was defined as probable or suspected IMF (category 1, category 3), probable pharmaceutical fentanyl (category 2), and unknown fentanyl source (category 4) in 42 665 (89.3%), 476 (1.0%), and 4658 (9.7%) deaths, respectively (Figure 3). Among the 42 665 deaths where fentanyl was defined as more likely IMF, it was defined as probable IMF (category 1) in 17 719 deaths (41.5%) and suspected IMF (category 3) in 24 946 deaths (58.5%). Fentanyl was defined as suspected IMF because of scene or witness evidence (19 480 deaths), or toxicology evidence, in the absence of scene or witness evidence (5466 deaths).
DISCUSSION
This report demonstrates that integrating DC data with comprehensive ME/C data, including full toxicology results, can strengthen drug overdose death surveillance throughout a large number of US states by: (1) improving classification of deaths as more likely involving heroin or pharmaceutical morphine; and (2) providing information about the probable source of fentanyl as illicitly manufactured or pharmaceutical. DC data reflect ME/C cause of death determination, considered the gold standard for drug overdose death surveillance in the United States given the national coverage and consistency over time; however, these data may lack specificity about the source of the drug(s) involved in overdoses if the ME/C listed toxicological findings without further interpretation. For example, listing ‘morphine overdose’ as cause of death does not necessarily mean that the ME/C thought the decedent had used pharmaceutical morphine, but that morphine in the body (from using pharmaceutical morphine or heroin) had caused death. Integrating ME/C and full toxicology data can provide this additional context and improve drug classification, which can enhance tailoring, prioritization and evaluation of interventions at local and national levels to more effectively address threats from illicit and prescription drugs.
Distinguishing between overdose deaths involving pharmaceutical morphine and heroin is critical, because some interventions vary depending on involvement of prescription or illicit opioids. For example, prescription opioid overdose prevention might focus upon improving prescribing practices, while illicit opioid overdose prevention might focus upon building awareness of the illicit drug supply or linking people to treatment from public safety settings such as pre-arrest diversion programs or drug courts [22]. Limitations and variations in the strength of the evidence in ME/C reports can be recognized by using confirmed, probable and suspected categories. More than two-thirds of deaths in the heroin/morphine analysis (70.5%) were defined as confirmed heroin because 6-AM was detected and nearly one-fifth (17.2%) were defined as probable heroin or probable pharmaceutical morphine because scene, witness or toxicology evidence strongly indicated heroin or pharmaceutical morphine involvement. Only 7.7% were defined as suspected heroin using weaker evidence of other illicit drug use. The suspected category should be used cautiously, because co-use of other illicit drugs is not exclusive to heroin; however, this category is limited to deaths without evidence of pharmaceutical morphine use, strengthening its validity. More conservative analyses could shift the 1518 suspected heroin deaths to unknown morphine source.
Integrating ME/C and full toxicology data into national drug overdose surveillance can also help to address substantial misclassifications of pharmaceutical morphine and heroin deaths resulting from using DC data. The enhanced definition aligned closely with ME/C cause of death classifications in the confirmed heroin category, in which the ME/C listed heroin but not morphine for 96.6% of deaths, and in the probable pharmaceutical morphine category, in which the ME/C listed morphine but not heroin for 95.5% of deaths. The largest differences between the enhanced definition and ME/C cause of death classifications were apparent in the probable and suspected heroin categories. For these categories, morphine (but not 6-AM) was detected and listed as cause of death for approximately half of deaths; however, we found some indication that morphine was more likely to have metabolized from heroin than to reflect pharmaceutical morphine use. Using these categories would redefine as heroin overdose deaths (and therefore as illicit opioid overdose deaths) 2678 deaths that would have been coded as morphine overdose deaths (and therefore as prescription opioid overdose deaths) with DC data. The categorization of most deaths as heroin rather than pharmaceutical morphine is consistent with previous reports [4–6], and the enhanced definition aligns with other definitions that incorporate similar evidence into classifying heroin and morphine [4, 6,12, 23].
The focus of public health surveillance on populations, compared with ME/C focus on determining the cause(s) of individual deaths, probably contributes to differences between the enhanced definition and the ME/C cause of death classifications. When determining cause of death, ME/Cs require high standards of evidence because misclassifying a death may have legal and emotional consequences for family and friends of the decedent, especially because heroin use is stigmatized [14]. In contrast, because public health surveillance tracks population trends, misclassifying individual deaths has limited public health implications but systematic error can bias analyses and potentially misinform interventions; therefore, surveillance can use the preponderance of evidence to classify deaths. These different goals might contribute to more conservative use of death investigation evidence by ME/Cs in determining heroin involvement in deaths when 6-AM is not detected, and might lead to more often listing toxicology findings (i.e. morphine) on the DC without further interpretation. The finding that heroin was listed on the DC for approximately half of probable and suspected heroin deaths, however, suggests that many ME/Cs do use investigative findings when considering heroin involvement. Further examination of how ME/Cs interpret different types of evidence is needed.
Monitoring fentanyl involvement in overdose deaths is essential because it: (1) has emerged as the drug most commonly involved in overdose deaths [2], (2) is increasingly used in combination with other opioids and stimulants [3, 24] and (3) has infiltrated drug markets across the United States after initially being most predominant east of the Mississippi River [1, 25, 26]. Pharmaceutical fentanyl and IMF differ in potency, dose, purity, consistency and patterns of co-use with other drugs [3, 27]. Defining fentanyl source as pharmaceutical or illicit can therefore help to inform tailored interventions. With the enhanced fentanyl source definition, we defined 87.4% of fentanyl as probable or suspected IMF. Approximately four in 10 deaths were defined as probable IMF based on fentanyl analog or precursor detection, representing the strongest evidence of IMF use and reflecting the overlap of fentanyl products in the illicit market. Nearly half of probable/suspected IMF deaths were defined as suspected IMF using scene or witness evidence of illicit drug use, demonstrating the importance of collecting overdose-specific circumstance data for identifying fentanyl source. The remainder were defined as suspected IMF because other illicit drugs were detected by toxicology testing, further emphasizing the importance of collecting information on all drugs detected and highlighting the contributions of illicit drugs to overdose deaths, especially in combination [3, 28]. These results support evidence from other sources indicating that most fentanyl overdose deaths involve IMF [27].
This analysis was subject to several limitations. First, data availability and quality issues might have contributed to enhanced definition misclassifications. Systematic quality-checking procedures in SUDORS, however, help to limit data quality issues. Secondly, SUDORS does not collect quantified toxicology results; therefore, the definition could not incorporate information such as the ratio of morphine to codeine, which has been used to indicate probable use of heroin versus morphine [12, 23]. Thirdly, defined heroin and morphine categories were mutually exclusive for simplicity and because heroin and pharmaceutical morphine co-use was found to be rare in sensitivity analyses. Specifically, sensitivity analyses found minimal overlap of category-specific information (e.g. < 1% of confirmed heroin deaths had evidence of pharmaceutical morphine use) and limited listing of both heroin and morphine as cause of death on the DC (< 3% of analyzed deaths). Fourthly, SUDORS does not collect information about postmortem toxicology testing scope, and therefore we could not determine the impact on the definitions of differences in testing (e.g. whether certain fentanyl analogs were being tested for). Finally, using available evidence, 4.6 and 9.7% of deaths to which the heroin/morphine and fentanyl definitions were applied, respectively, were defined as unknown. This limits dichotomous classification of prescription versus illicit opioids; however, the unknown categories could be included with heroin or pharmaceutical morphine, or as IMF or pharmaceutical fentanyl, depending on local epidemiology and other considerations, and future work can explore missing data imputation. Further, the < 10% unknown fentanyl source represents a vast improvement over death certificate data, in which there was no classification of fentanyl source on the death certificate for nearly 100% of deaths with fentanyl detected (Figure 3).
Detailed scene, witness and toxicology evidence for unintentional and undetermined intent opioid overdose deaths from 38 states and the District of Columbia participating in SUDORS was used to define heroin and pharmaceutical morphine overdose deaths, and to define fentanyl as IMF or pharmaceutical fentanyl. This type of detailed evidence was not available among multiple jurisdictions previously, and it builds upon what can be learned about specific drugs contributing to drug overdose deaths strictly using DC information. As a result, we can more provide more specification about contributions of prescription and illicit opioids to overdose deaths, with important implications for tailored overdose prevention and response efforts.
ACKNOWLEDGEMENTS
This study was supported by jurisdictions participating in CDC’s Overdose Data to Action (OD2A) program and providing data in the State Unintentional Drug Overdose Reporting System (SUDORS), including state and jurisdictional health departments, vital registrar offices and coroner and medical examiner offices; the CDC OD2A team, Division of Overdose Prevention, National Center for Injury Prevention and Control, CDC.
Funding information
National Center for Injury Prevention and Control
Footnotes
DECLARATION OF INTERESTS
None.
DISCLAIMER
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths—United States, 2013–2019. Morb Mort Wkly Rep 2021;70:202–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hedegaard H, Bastian BA, Trinidad JP, Spencer MR, Warner M. Regional differences in the drugs most frequently involved in drug overdose deaths: United States, 2017. Natl Vital Stat Rep 2019;68:1–16. [PubMed] [Google Scholar]
- 3.Gladden RM, O’Donnell J. Mattson CL, Seth P. Changes in opioid-involved overdose deaths by opioid type and presence of benzodiazepines, cocaine, and methamphetamine—25 states, July–December 2017 to January–June 2018. Morb Mort Wkly Rep 2019;68:737–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hurstak E, Rowe C, Turner C, Behar E, Cabugao R, Lemos NP, et al. Using medical examiner case narratives to improve opioid overdose surveillance. Int J Drug Policy 2018;54:35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mertz KJ, Janssen JK, Williams KE. Underrepresentation of heroin involvement in unintentional drug overdose deaths in Allegheny County, PA. J Forens Sci 2014;59:1583–5. [DOI] [PubMed] [Google Scholar]
- 6.Horon IL, Singal P, Fowler DR, Sharfstein JM. Standard death certificates versus enhanced surveillance to identify heroin overdose-related deaths. Am J Public Health 2018;108:777–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stam NC, Gerostamoulos D, Pilgrim JL, Smith K, Moran L, Parsons S, et al. An analysis of issues in the classification and reporting of heroin-related deaths. Addiction 2019;114:504–12. [DOI] [PubMed] [Google Scholar]
- 8.Roxburgh A, Pilgrim JL, Hall WD, Burns L, Degenhardt L. Accurate identification of opioid overdose deaths using coronial data. Forens Sci Int 2018;287:40–6. [DOI] [PubMed] [Google Scholar]
- 9.Seth P, Rudd RA, Noonan RK, Haegerich TM. Quantifying the epidemic of prescription opioid overdose deaths. Am J Public Health 2018;108:500–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldberger BA, Darwin WD, Grant TM, Allen AC, Caplan YH, Cone EJ. Measurement of heroin and its metabolites by isotope-dilution electron-impact mass spectrometry. Clin Chem 1993;39:670–5. [PubMed] [Google Scholar]
- 11.Davis GG, Cadwallader AB, Fligner CL, Gilson TP, Hall ER, Harshbarger KE, et al. Position paper: Recommendations for the investigation, diagnosis, and certification of deaths related to opioid and other drugs. Am J Forens Med Pathol 2020;41:152–9. [DOI] [PubMed] [Google Scholar]
- 12.Ellis AD, McGwin G, Davis GG, Dye DW. Identifying cases of heroin toxicity where 6-acetylmorphine (6-AM) is not detected by toxicological analyses. Forens Sci Med Pathol 2016;12:243–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.US Drug Enforcement Administration, Diversion Control Division. National Forensic Laboratory Information System: NFLIS-Drug 2019 Annual Report Springfield, VA: US Drug Enforcement Administration; 2020. [Google Scholar]
- 14.Goodyear K, Chavanne D. Stigma and policy preference toward individuals who transition from prescription opioids to heroin. Addict Behav 2021:115:106784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Center for Health Statistics. In: National Center for Health Statistics, editorA reference guide for completing the death certificate for drug toxicity deaths Hyattsville, MD; 2019. [Google Scholar]
- 16.Glerum PJ, Maliepaard M, de Valk V, Scholl JHG, van Hunsel F, van Puijenbroek EP, et al. Quantification of adverse drug reactions related to drug switches in the Netherlands. Clin Transl Sci 2020;13:599–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kuczynska K, Grzonkowski P, Kacprzak L, Zawilska JB. Abuse of fentanyl: an emerging problem to face. Forens Sci Int 2018;289:207–14. [DOI] [PubMed] [Google Scholar]
- 18.Blair JM, Fowler KA, Jack SP, Crosby AE. The National Violent Death Reporting System: overview and future directions. Inj Prev 2016;22: i6–i11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fiorentin TR, Krotulski AJ, Martin DM, Browne T, Triplett J, Conti T, et al. Detection of cutting agents in drug-positive seized exhibits within the United States. J Forens Sci 2019;64:888–96. [DOI] [PubMed] [Google Scholar]
- 20.Lovrecic B, Lovrecic M, Gabrovec B, Carli M, Pacini M, Maremmani AGI, et al. Non-medical use of novel synthetic opioids: a new challenge to public health. Int J Environ Res Public Health 2019;16:177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.US Drug Enforcement Administration (DEA), Strategic Intelligence Section. 2018 National Drug Threat Assessment Arlington, VA: US DEA; 2018. [Google Scholar]
- 22.Baldwin GT, Seth P, Noonan RK. Continued increases in overdose deaths related to synthetic opioids: Implications for clinical practice. JAMA 2021;325:1151–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stam NC, Gerostamoulos D, Dietze PM, Parsons S, Smith K, Lloyd B, et al. The attribution of a death to heroin: a model to help improve the consistent and transparent classification and reporting of heroin-related deaths. Forens Sci Int 2017;281:18–28. [DOI] [PubMed] [Google Scholar]
- 24.Kariisa M, Scholl L, Wilson N, Seth P, Hoots B. Drug overdose deaths involving cocaine and psychostimulants with abuse potential—United States, 2003–2017. Morb Mort Wkly Rep 2019;68:388–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.US Drug Enforcement Agency (DEA), Strategic Intelligence Section. National Drug Threat Assessment Arlington, VA: US DEA;2019. [Google Scholar]
- 26.Shover CL, Falasinnu TO, Dwyer CL, Santos NB, Cunningham NJ, Freedman RB, et al. Steep increases in fentanyl-related mortality west of the Mississippi River: recent evidence from county and state surveillance. Drug Alcohol Depend 2020;216:108314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Suzuki J, El-Haddad S. A review: fentanyl and non-pharmaceutical fentanyls. Drug Alcohol Depend 2017;171:107–16. [DOI] [PubMed] [Google Scholar]
- 28.O’Donnell J, Gladden RM, Mattson CL, Hunter CT, Davis NL. Vital signs: characteristics of drug overdose deaths involving opioids and stimulants—24 states and the District of Columbia, January–June 2019. Morb Mort Wkly Rep 2020;69:1189–97. [DOI] [PMC free article] [PubMed] [Google Scholar]


