Abstract
We examined colonization patterns of Shiga toxin-producing Escherichia coli (STEC), concentrations of Shiga toxins (Stxs) and specific immunoglobulin A (lgA) against Stxs and STEC bacterial cell surface antigen in various portions of the gastrointestinal tract in an infant rabbit infection model. After inoculation of 3-day-old infant rabbits with STEC strain 89020087 at low doses (∼103 CFU/body), numbers of colonizing STEC bacteria and concentrations of Stxs in the intestine increased dramatically and the animals developed diarrhea within a couple of days after infection. Daily administration of Lactobacillus casei from the day of birth dramatically decreased the severity of diarrhea and lowered STEC colonization levels in the gastrointestinal tract 100-fold day 7 after infection. Both Stx1 and Stx2 concentrations in the intestines and histological damage to the intestinal mucus induced by STEC infection were decreased by the administration of L. casei. Examination of the concentrations of volatile fatty acids and pH of the intestinal contents revealed that the protective effect of L. casei administration against STEC infection was not due to fermented products such as lactic acid in the gastrointestinal tract. Administration of L. casei increased levels of lgAs against Stx1, Stx2, and formalin-killed STEC cells in the colon approximately two-, four-, and threefold, respectively, compared with those of the untreated controls by day 7 after infection. These results suggest that administration of L. casei strain Shirota enhances the local immune responses to STEC cells and Stxs and leads to elimination of STEC and thus decreases Stx concentrations in the intestines.
Shiga toxin-producing Escherichia coli (STEC) O157:H7 is characterized by production of two kinds of Shiga toxins (Stxs), Stx1 and Stx2, which cause hemorrhagic colitis followed, in some cases, by hemolytic-uremic syndrome and central nervous system complications (4, 25, 45, 51, 57). The mechanism of infection, however, remains unclear; thus, preventive and therapeutic measures have not been established.
A complex intestinal microflora provides protection against colonization by many pathogenic infectious agents (for reviews, see references 8 and 60). Increased susceptibility to STEC infection due to treatment of mice with antibiotics can be explained by disruption of the normal indigenous intestinal microflora (15, 27, 32, 59, 61). A hypothesis that foods fermented by lactobacilli help maintain a balance between lactobacilli and the indigenous intestinal flora, originally proposed by Metchnikoff (33) as early as 1908, has been supported by many investigators (3, 12, 41, 54), and probiotic Lactobacillus strains have been shown to protect against infection by pathogens such as Shigella sonnei (2, 35), Listeria monocytogenes (39, 52, 53), E. coli (40), Salmonella enterica serovar Typhimurium (13, 16) and rotavirus (20, 29).
In this study, by using newborn rabbits as an experimental infection model, the protective effects of oral administration of probiotic Lactobacillus casei strain Shirota (24) against STEC infection were investigated.
MATERIALS AND METHODS
Bacterial strain and growth conditions.
Clinically isolated STEC O157:H7 strain 89020087, which produces both Stx1 and Stx2, was used throughout. Cells were grown overnight in Casamino Acids-yeast extract (CA-YE) broth (11) at 37°C. L. casei strain Shirota is a stock culture of the Yakult Central Institute for Microbiological Research and was grown overnight anaerobically at 37°C in De Man-Rogosa-Sharpe (MRS) broth (Difco Laboratories, Detroit, Mich.) which had been purged of oxygen with nitrogen.
Animals.
Specific-pathogen-free Japanese White rabbits (pregnant for 24 days) were purchased from Kitayama Rabesu Co. Ltd., Ina, Japan. After parturition, neonatal rabbits 1 day old were isolated from their dams and housed in a clean isolator system with automatic control of temperature (25 ± 0.5°C), humidity (55% ± 5%), and light conditions (14 h of light and 10 h of darkness) and were kept individually in polypropylene cages (CLEA Japan, Inc., Tokyo, Japan) with stainless steel lids and sterilized paper bedding (CLEA). They were fed 20% pasteurized (65°C, 30 min) artificial milk for pet (PetAg, Inc., Hampshire, Ill.) intragastrically by a soft polyethylene catheter tube (Fuchigami Co., Kyoto, Japan) attached to a 5-ml syringe twice a day throughout the experiment (1, 34, 36).
Preparation of bacterial suspension and inoculation of infant rabbits.
After two passages in CA-YE broth, STEC was grown overnight in CA-YE broth at 37°C on a shaker for 18 h and the bacterial cells were washed once with saline by centrifugation. The precipitating bacterial cells were then suspended and diluted with saline to an optical density at 600nm (OD600) of 0.1 as determined with a spectrophotometer (U-2001; Hitachi Co. Ltd., Tokyo, Japan). This bacterial suspension was then diluted 104-fold with saline to make a suspension of ∼2 × 103 CFU/ml. An aliquot of 500 μl of the suspension was given orally to infant rabbits by using the catheter tube described above. For exact enumeration of an inoculum, this bacterial suspension was serially diluted with phosphate-buffered saline (PBS) and plated on Trypticase soybean agar plates (BBL Microbiology Systems, Cockeysville, Md.) and incubated overnight at 37°C.
Preparation of milk supplemented with L. casei.
After two passages in MRS broth at 37°C anaerobically, L. casei strain Shirota was grown in MRS broth overnight and the culture was centrifuged at 1,700 × g for 20 min (Kubota Co. Ltd., Tokyo, Japan). The bacterial pellet was resuspended in sterile artificial milk to a concentration of 108 CFU/ml. For exact enumeration of an inoculum, L. casei-supplemented milk was serially diluted with PBS, plated on lactitol-LBS-vancomycin (LLV) agar plates (66), and incubated aerobically for 48 h at 37°C. LLV agar contains the following (per liter): tryptic peptone (BBL), 10 g; yeast extract (Difco), 5 g; KH2PO4, 6 g; triammonium citrate, 2 g; sodium acetate · 3H2O, 25 g; MgSO4 · 7H2O, 0.58 g; MnSO4 · 2H2O, 0.12 g; FeSO4 · 7H2O, 0.034 g; Tween 80, 1 g; lactitol, 20 g; Bacto Agar (Difco), 15 g; vancomycin hydrochloride (Sigma Chemical Co., St. Louis, Mo.), 10 mg. The pH of the medium was adjusted to 6.1.
Experimental design.
Animals were divided into two groups. One was fed sterilized artificial milk supplemented with L. casei strain Shirota at a concentration of 108 CFU/ml (total number, 18), and the other was fed only sterilized artificial milk (total number, 14). Feeding was carried out twice a day (10:00 am and 6:00 pm), from day 1 after birth until the morning of the day the animals turned 10 days old. Exactly the same amounts of the milk preparations were given to the animals of both groups. The amounts were as follows: 3.0 ml twice a day on days 1 and 2, 5 ml twice a day on days 3 and 4, and 7.0 ml twice a day on days 5 and 6 and once in the morning of day 7. When the animals became 3 days old, they were individually inoculated with 0.5 ml of STEC suspension with a sterile flexible polyethylene catheter tube. After infection, they were weighed daily and checked for diarrhea until day 7 after infection. Diarrhea was classified into the following severity groups: I, no diarrhea; II, slight diarrhea (mixed soft and hard stools); III, mild diarrhea (feces stuck to perineum and hind legs); IV, severe diarrhea (feces stuck to hind legs, wet tail, and prolapse of rectum).
On days 1, 4, and 7 after STEC inoculation, animals were sacrificed under anesthesia with an intraperitoneal injection of sodium pentobarbital (Dinabot Co., Ltd., Osaka, Japan) at a dose of 83 mg/kg of body weight. One experiment was carried out for analysis on day 1 (three infants per group). Three experiments were carried out for analysis on days 4 and 7 (11 infants in the control group and 15 infants in the L. casei-treated group). The gastrointestinal tract was dissected in an aseptic manner for determinations of viable STEC and L. casei counts, intestinal pH, and concentrations of volatile fatty acids (VFA); Stx assay; titration of specific lgA against Stx1, Stx2, and STEC intact cells, and histological examinations. All experimental procedures were carried out in accordance with the standards set forth in the Guide for the Care and Use of Laboratory Animals (37).
Bacteriological examination.
The removed gastrointestinal tracts were segmented into stomach, small intestine, cecum, and colon, and each section was weighed and homogenized in 5 ml of ice-cold saline. The suspension was centrifuged at 17,000 × g for 15 min (Microfuge R; Beckman Instruments Inc., Palo Alto, Calif.), and the pellet was washed once with PBS by centrifugation, resuspended in PBS, and diluted 10-fold serially with PBS for evaluation of bacterial CFU; 100-μl samples of the suspension were spread onto sorbitol MacConkey agar plates (Eiken Chem. Co. Ltd., Tokyo, Japan) and LLV agar plates for counting of STEC and L. casei strain Shirota colonies, respectively. Sorbitol MacConkey agar plates and LLV agar plates were incubated at 37°C overnight and for 48 h, respectively.
Gastrointestinal pH and concentrations of VFAs.
To examine pH values and concentrations of VFAs in the gastrointestinal contents of test animals, sections of gastrointestinal tracts were treated as described above. After homogenization, samples were centrifuged at 1,700 × g for 30 min and supernatants were filtered (pore size, 0.8 μm). The pH of filtrates was measured with a hand-held pH meter (B-212; Horiba Ltd., Kyoto, Japan). For VFA analysis, supernatants were mixed with 10% (vol/vol ratio, 9:1) trichloroacetic acid, incubated overnight at 4°C, and centrifuged at 20,000 × g for 10 min. After filtration (pore size, 0.22 μm), samples were analyzed by high-pressure liquid chromatography (TOA Electronics Ltd., Tokyo, Japan). The millimolar concentration of lactic acid in an undissociated form was calculated by the following formula: undissociated lactic acid = millimolar total lactic acid/(1 + 10pH−pKa).
Stx assay.
Concentrations of Stx1 and Stx2 in intestinal contents were assayed by a bead enzyme-linked immunosorbent assay (ELISA) method described previously (42, 67). Briefly, sections of gastrointestinal tracts were treated as described above. After homogenization, samples were centrifuged at 1,700 × g for 30 min and the supernatants were filtered (pore size, 0.8 μm). The filtrates were diluted twofold with PBS supplemented with 2% bovine serum albumin (BSA; Nakalai Tesque Inc., Kyoto, Japan) and 0.02% NaN3. Solid-phase beads coated with rabbit polyclonal lgG against purified Stx1 or Stx2 were added, and the mixtures were incubated at 37°C for 1 h. After being washed twice with PBS, the beads were incubated with goat anti-rabbit lgG-Fab′-horseradish peroxidase (HRP) conjugate diluted in PBS containing 2% BSA at 37°C for 1 h. After the beads had been washed twice with PBS, the enzymatic activity of the HRP bound to the beads was assayed by addition of 3, 3′, 5, 5′-tetramethylbenzidine as a substrate and the OD450 was measured with a spectrophotometer. Stx concentrations in intestinal contents were calculated relative to a standard curve of purified Stx1 or Stx2 and expressed as nanograms per gram of tissue.
lgA assay.
Samples were prepared as described above. Determination of lgA levels was performed as described by Keren et al. (22) and MacQueen et al. (31). Briefly, 96-well polystyrene microtiter plates (Maxisorp; Nalge Nunc International, Roskilde, Denmark) were coated with 100-μl portions of purified Stx1 or Stx2 at a concentration of 2.5 μg/ml in carbonate buffer (coating buffer), pH 9.6, or with a formalin-killed STEC whole-cell suspension diluted with coating buffer to an OD600 of 0.01. Purified Stx1 and Stx2 were prepared as described previously (38, 43, 65). Intact STEC cells were prepared as follows. STEC was cultured in CA-YE broth at 37°C for 18 h, washed twice with saline by centrifugation, suspended in saline containing 0.5% neutralized formalin, stored at room temperature for 3 days, and then washed three times with saline to remove free Stxs. Plates were incubated overnight at 4°C in a moist chamber to prevent evaporation. After incubation, wells were washed three times with PBS containing 0.02% Tween 20 (PBST) to remove the free Stx solution or STEC suspension. Wells were sequentially incubated with samples, 1/500 goat anti-rabbit lgA (Nordic Immunological Laboratories, Tilburg, The Netherlands) coupled to HRP, and finally a 2, 2′-azino+bis[3-ethylbenzthiazoline sulfonate (6)] (ABTS) substrate (Sigma). Wells were washed with PBST three times between incubations and reacted with PBST supplemented with 1% BSA at 37°C for 1 h before addition of the primary samples and before addition of the secondary antibody conjugate to inhibit nonspecific adherence. The OD405 of wells was measured in a microplate reader (Inter Med Immunomini NJ-2300; Nalge Nunc International), and results were expressed as OD405 units per gram of tissue. The background OD405 for this ELISA was 0.2/g of tissue.
Histopathological examinations.
Segments of the ileum, cecum, and distal colon were surgically removed, washed, and then fixed in 4% buffered formalin, blocked in paraffin, and sectioned. Sections were stained with hematoxylin and eosin, and examined under a microscope for pathological changes such as exfoliation, necrosis, edema, STEC cells attached to epithelial cells, and pseudoeosinophil infiltration. In addition, immunohistochemical staining of STEC cells was performed using goat anti-E. coli O157:H7 antibody (Kirkegaard & Perry Laboratories Inc., Gaithersburg, Md.), biotinylated rabbit anti-goat immunoglobulin, and 3, 3-diaminobenzidine in a chromogen solution (DAKO Japan, Kyoto, Japan).
Statistical examinations.
Statistical differences between the control group and the L. casei-treated group were evaluated with the cumulative chi-square test for the incidence of diarrhea and with Student's t test for other benchmarks. P < 0.05 was considered significant.
RESULTS
Clinical symptoms.
Most of the infected rabbits began to show diarrhea within 3 days. No animal in either group developed bloody diarrhea. By day 7 after infection, 77.3% of the rabbits in the control group suffered from severe diarrhea whereas only 16.0% of the rabbits in the L. casei-treated group showed severe diarrhea (Table 1). On the whole, the severity of diarrhea was less pronounced in the L. casei-treated group than in the control group. L. casei did not delay the onset of diarrhea. No clinical symptoms were observed in the group fed L. casei alone (data not shown).
TABLE 1.
Severity of diarrhea in rabbits infected with STEC O157:H7 strain 89020087 by day 7 after infection
| Diarrhea severity | No. of rabbits/total (%)a
|
|
|---|---|---|
| Control | L. casei treated | |
| None | 1/22 (4.5) | 6/25 (24.0) |
| Slight | 1/22 (4.5) | 11/25 (44.0) |
| Mild | 3/22 (13.6) | 4/25 (16.0) |
| Severe | 17/22 (77.3) | 4/25 (16.0) |
A significant difference was observed between the two groups (P < 0.0001) by cumulative chi-square analysis.
Colonization and distribution of STEC in the gastrointestinal tract.
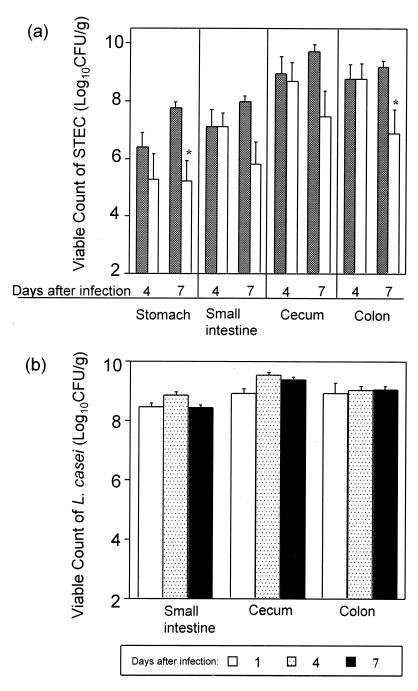
Viable STEC counts in the gastrointestinal tracts of mice in the control group increased dramatically to 107∼109 CFU/g of organ homogenate by day 7 after infection (Fig. 1a). Although STEC colonization levels in the L. casei-treated group were similar to those in the control group by day 4 after infection, they were approximately 100-fold lower than in the control group by day 7 after infection. Viable counts of L. casei in the gastrointestinal tract were sustained at higher than 108 CFU/g of organ throughout the experimental period (Fig. 1b).
FIG. 1.
Viable counts of STEC O157:H7 strain 89020087 (a) and L. casei (b) recovered from the gastrointestinal tract. Control rabbits (hatched columns) were fed artificial milk only, and L. casei-treated rabbits (white columns) were fed artificial milk supplemented with L. casei. A total of 103 CFU of STEC strain 89020087 was fed to the rabbits, and on day 1, 4, or 7 after infection, the rabbits were sacrificed and regions of the gastrointestinal tract were removed and homogenized. Viable counts of STEC (on days 4 and 7) and L. casei (on days 1, 4, and 7) in each homogenate were assayed as described in Materials and Methods. The bar at each point indicates the standard error of the geometric mean number of CFU per gram of tissue. Three rabbits from each group on day 1, 6 control and 7 L. casei-treated rabbits on day 4, and 11 control and 15 L. casei-treated rabbits on day 7 were tested. An asterisk indicates a significant difference (P < 0.05) from the value for the corresponding control group as calculated by Student's t test.
pH and lactic acid concentration in the gastrointestinal tract.
No differences in pH of the gastrointestinal contents on day 7 after infection was observed between the control and L. casei-treated groups (Table 2). In both groups, the pH of the stomach contents was approximately 5.1 and was higher than 6.5 in other parts of the intestine. Concentrations of lactic acid in the gastrointestinal tract were slightly higher in the L. casei-treated group than in the control group (Table 2). In both groups, concentrations of undissociated lactic acid in the gastrointestinal tract were less than 1.0 mM (data not shown).
TABLE 2.
pH and lactic acid concentration in gastrointestinal contents of rabbits on day 7 after infection
| Region | Mean pHa ± SD
|
Mean lactic acid concnb ± SD
|
||
|---|---|---|---|---|
| Control (11)c | L. casei treated (5) | Control (3) | L. casei treated (4) | |
| Stomach | 5.1 ± 0.1 | 5.1 ± 0.1 | 8.0 ± 1.8 | 10.5 ± 0.9 |
| Small intestine | 6.6 | 6.5 ± 0.1 | 10.7 ± 1.7 | 15.0 ± 1.3 |
| Cecum | 6.4 ± 0.1 | 6.4 ± 0.1 | 6.3 ± 1.5 | 9.5 ± 1.1 |
| Colon | 6.8 ± 0.1 | 6.5 ± 0.1 | 14.3 ± 2.4 | 18.5 ± 2.6 |
pH of gastrointestinal contents on day 7 after infection.
Concentration of lactic acid in gastrointestinal contents on day 7 after infection.
In parentheses is the number of rabbits tested.
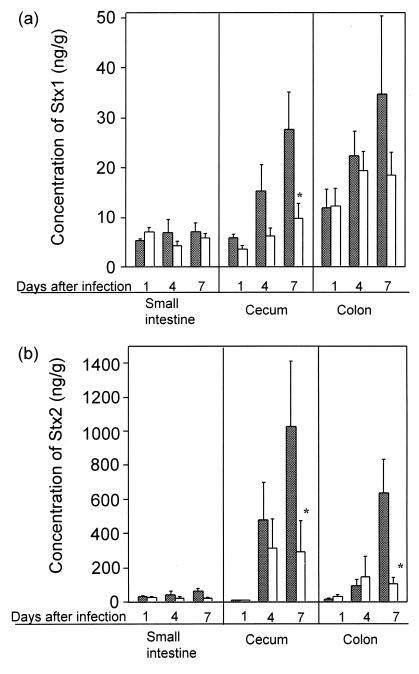
Stx concentrations in the intestinal contents.
Concentrations of both Stx1 and Stx2 in the cecum and colon in the control group increased at day 4 after infection, and further significant increases were observed at day 7. In contrast, Stx concentrations in the L. casei-treated group increased by day 4 after infection but showed no further increase thereafter (Fig. 2). Stx concentrations in the small intestine were quite low compared with those in the cecum and colon in both groups.
FIG. 2.
Changes in concentrations of Stx1 (a) and Stx2 (b) in the intestinal contents of control (hatched columns) and L. casei-treated (white columns) rabbits after STEC infection. A total of 103 CFU of STEC strain 89020087 was given orally to the rabbits. On day 1, 4, or 7 after infection, the rabbits were sacrificed and portions of the gastrointestinal tract were removed and homogenized. Concentrations of Stxs in each homogenate were assayed with a bead ELISA as described in Materials and Methods. Three rabbits from each group on day 1, 6 control and 7 L. casei-treated rabbits on day 4, and 11 control and 15 L. casei-treated rabbits on day 7 were tested. An asterisk indicates significant difference (P < 0.05) from the value for the corresponding control group as calculated by Student's t test.
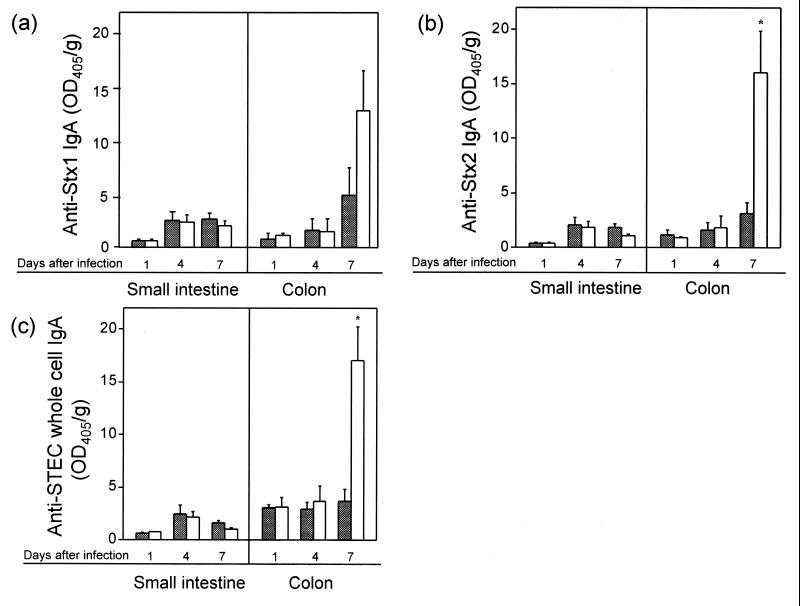
Specific IgA concentrations in the intestinal contents.
In the small intestine, concentrations of IgA against Stx and STEC cells remained low and no differences were observed between the control and L. casei-treated groups (Fig. 3). In the colon, in contrast, concentrations of IgAs against Stx1, Stx2, and intact STEC cells in the L. casei-treated group increased approximately two-, four-, and threefold, respectively, over those in the control group.
FIG. 3.
Changes in concentrations of IgAs against Stx1 (a), Stx2 (b), and STEC cells (c) in the intestinal contents of control (hatched columns) and L. casei-treated (white columns) rabbits. Concentrations of anti-Stx and anti-STEC bacterial cell surface antigen IgA in each homogenate were assayed as described in Materials and Methods. Three rabbits from both groups on day 1 after infection, 6 control and 7 L. casei-treated rabbits on day 4, and 8 control and 11 L. casei-treated rabbits on day 7 were examined. An asterisk indicates significant difference (P < 0.05) from the value for the corresponding control group as calculated by Student's t test.
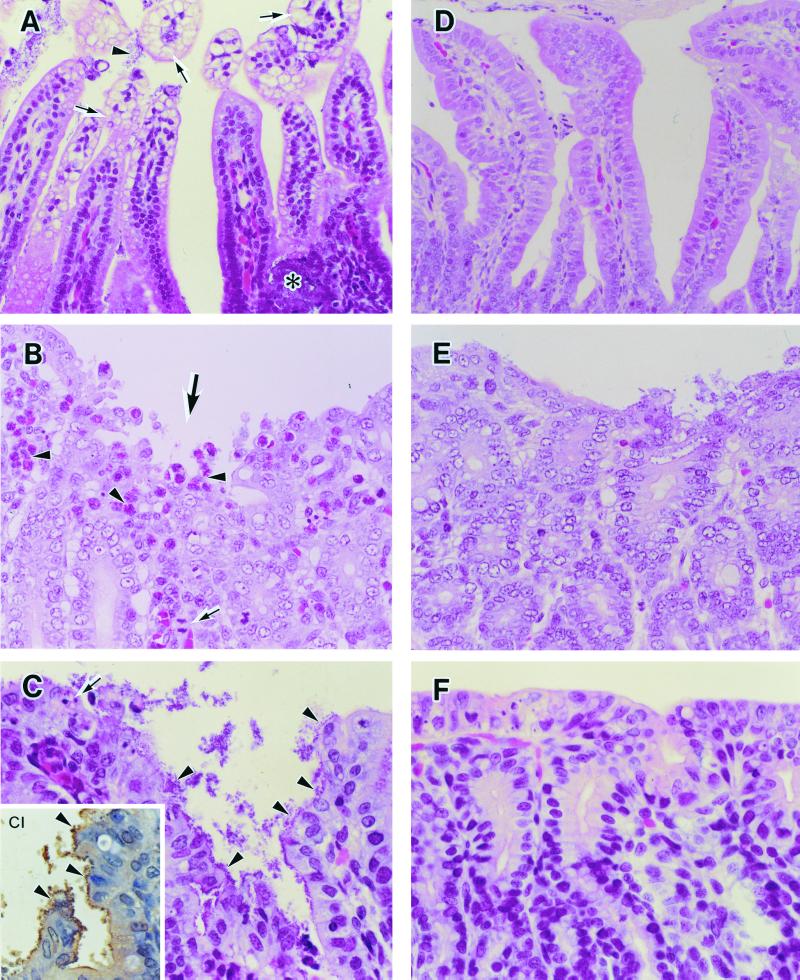
Histopathology.
In the control group, STEC infection led to vacuolation of epithelial cells (arrows) with attached STEC cells (arrowhead) on top of the villi and necrosis due to massive growth of STEC cells (asterisk) in the small intestine (Fig. 4A), exfoliation of epithelial cells (large arrows), pseudoeosinophil infiltration (arrowheads), and mitotic activity (small arrow) in the cecum (Fig. 4B), and exfoliation and necrosis (arrow) in the colon due to STEC cells attached to epithelial cells (arrowheads) (Fig. 4C). In contrast, no notable pathological changes except for low mitotic activity in the cecum and slight exfoliation of the epithelium in the colon were observed in the L. casei-treated group (Fig. 4D to F).
FIG. 4.
Histopathological examination of intestinal segments of infant rabbits infected with STEC O157:H7 strain 89020087 on day 7 after infection. Hematoxylin-and-eosin staining of the small intestine (A, D), cecum (B, E), and colon (C, F) from a control rabbit (A to C) and an L. casei-treated rabbit (D to F). (CI) Immunostaining of STEC O157 in a colon section from a control rabbit. Magnifications in both groups: small intestine ×260; cecum, ×390; colon, ×520. For details, see the text.
DISCUSSION
A number of experimental animal models have been proposed to study the pathogenicity of STEC (63), including gnotobiotic mice (17, 18, 64), streptomycin-treated mice (15, 27, 32, 61, 62), gnotobiotic piglets (14, 59), newborn chickens (5), and infant rabbits (26, 36, 44, 50). While mouse models have been used most frequently to date, most are not appropriate because high doses of inoculum, more than 107 CFU/body, are usually required for establishment of STEC infection, and often mice do not develop diarrhea even when they are inoculated with such high doses of STEC (21, 23). On the contrary, the rabbit model has the major advantages of the reproducibility of diarrhea and susceptibility to STEC infection and Stx toxicity (7, 26, 36, 44, 50, 55). In this study, we used the infant rabbit model with administration of a lower number of bacteria (∼103 CFU/body) than reported previously (36, 44, 50).
STEC infection in the infant rabbit model occurs reproducibly with an inoculum as small as 103 CFU/body (Table 1). Concentrations of Stxs in the gastrointestinal tract also increased in proportion to the time (days) after infection (Fig. 2). Both the number of colonizing bacteria and the concentration of Stxs were higher in the large intestine than in the small intestine. In particular, the concentration of Stx2 was significantly lower in the small intestine than in the cecum and the colon. Histological studies also showed that damage to the intestinal epithelium was more pronounced in the cecum and the colon than in the small intestine (Fig. 4). These findings are in agreement with the previously reported results that showed that the major colonization site of STEC in rabbit is the large intestine rather than the small intestine (36, 44, 50).
In rabbits administered L. casei strain Shirota, although levels of STEC colonization increased to levels similar to those of the control group by day 4 after infection, thereafter they remained unchanged or even decreased 100-fold by day 7 (Fig. 1). Concentrations of Stx1 and Stx2 were also lower in the L. casei-treated group, in parallel with decreased STEC colonization, compared with the controls (Fig. 2). Stx2 levels, in particular, were significantly lower in rabbits given L. casei in addition to STEC. The differences in diarrhea severity (Table 1) and mucosal damage in the intestines (Fig. 4) between the two groups was closely related to the differences in STEC colonization and Stx levels in the gastrointestinal tract.
Probiotics, including lactobacilli, are known to produce short-chain VFAs such as lactic acid (3, 12, 58). It has been reported that VFAs possess potent bactericidal activity and that the bactericidal activity of the organic acids depends mainly on their undissociated form (6, 10). Undissociated organic acids can permeate the cell membrane by diffusion and release protons in the cell. The influx of protons is thought to induce acidification of the cytoplasm and dissipate the membrane proton potential (ΔpH) (6, 9, 10). In a recent report, we demonstrated that L. casei strain Shirota exerts a bactericidal effect on STEC strains during coculture and that this effect is dependent on the lactic acid produced by L. casei during culture (M. Ogawa, K. Shimizu, K. Nomoto, R. Tanaka, T. Hamabata, S. Yamasaki, T. Takeda, and Y. Takeda, submitted for publication). In this study, there were no differences in the pH of the gastrointestinal contents between the control and L. casei-treated groups (Table 2). Concentrations of undissociated lactic acid in the gastrointestinal tract were less than 1.0 mM in both groups (data not shown). We previously showed that undissociated lactic acid at a concentration of more than 3.2 mM is required to inhibit the growth of STEC strain 89020087 (Ogawa et al., submitted). These results suggest that lactic acid produced by L. casei strain Shirota in the intestines may not contribute to its inhibitory effect on STEC in the gastrointestinal tract in infant rabbits.
It has been shown that probiotics, such as lactobacilli or bifidobacteria, can enhance specific and total IgA secretion when used as an oral adjuvant (19, 28, 30, 41, 49). Perdigon et al. reported that L. casei had a protective effect on intestinal infections with S. enterica serovar Typhimurium and E. coli by enhancing the secretion of specific IgA (47, 48). In this study, secretion of specific IgA antibodies against Stx1, Stx2, and STEC cells in the colon was enhanced locally by L. casei administration by 4 days after infection (Fig. 3). The most marked increase in the level of IgA was observed in the colon, where high levels of Stxs were detected. It has been reported that when antigens such as RDEC-1 (rabbit diarrheal E. coli) or Shiga toxin are used to inoculate rabbits by the oral route, mucosal IgA levels in the intestines increase within 7 days (22, 31, 56). The levels of IgA against Stxs and STEC cells in the colon in the L. casei-treated rabbits increased over the same period when STEC colonization and Stxs levels were reduced (days 4 to 7 after infection). It was also observed that levels of total IgA in the colon were increased by the administration of L. casei strain Shirota during STEC infection (data not shown). Paton et al. reported that antibody specific to STEC cells, especially lipopolysaccharide, inhibited the adherence of STEC to a human intestinal epithelial cell line (46). Therefore, a local increase in secretion of IgA, including specific IgA against Stxs and STEC bacterial cell surface antigen, by administration of L. casei strain Shirota may lead to the elimination of STEC and thus decrease the Stx concentration in the intestines.
In conclusion, the results obtained in this study suggest that preventive administration of probiotic lactobacilli to infants may lead to enhanced resistance to acute STEC infection due to acceleration of a specific humoral immune response to STEC, as well as Stxs.
REFERENCES
- 1.Akuzawa M, Matsunuma N, Suzuki Y. Hand-rearing of rabbits using rabbit milk and commercial milk powder, Teo Milk. Jikken Dobutsu. 1978;27:427–429. doi: 10.1538/expanim1978.27.4_427. [DOI] [PubMed] [Google Scholar]
- 2.Apella M C, Gonzalez S N, Nader de Macias M E, Romero N, Oliver G. In vitro studies on the growth of Shigella sonnei by Lactobacillus casei and Lact. acidophilus. J Appl Bacteriol. 1992;73:480–483. doi: 10.1111/j.1365-2672.1992.tb05008.x. [DOI] [PubMed] [Google Scholar]
- 3.Beck C, Necheles H. Beneficial effects of administration of Lactobacillus acidophilus in diarrhoeal and other intestinal disorders. Am J Gastroenterol. 1961;35:522–530. [PubMed] [Google Scholar]
- 4.Bell B P, Goldoft M, Griffin P M, Davis M A, Gordon D C, Tarr P I, Bartleson C A, Lewis J H, Barrett T J, Wells J G, Baron R, Kobayashi J. A multistate outbreak of Escherichia coli O157:H7-associated bloody diarrhea and hemolytic uremic syndrome from hamburgers. JAMA. 1994;272:1349–1353. [PubMed] [Google Scholar]
- 5.Berry J T, Doyle M P, Schoeni J L. Colonization of chicken cecae by Escherichia coli associated with hemorrhaghic colitis. Infect Immun. 1985;49:310–315. doi: 10.1128/aem.49.2.310-315.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brocklehurst T F, Lund B M. The influence of pH, temperature and organic acids on the initiation of growth of Yersinia enterocolitica. J Appl Bacteriol. 1990;69:390–397. doi: 10.1111/j.1365-2672.1990.tb01529.x. [DOI] [PubMed] [Google Scholar]
- 7.Cavanagh J B, Howard J G, Whitby J L. The neurotoxin of Shigella shigae: a comparative study of the effects produced in various laboratory animals. Br J Exp Pathol. 1956;37:272–278. [PMC free article] [PubMed] [Google Scholar]
- 8.Clasener H A L, Vollaard E J, van Saene H K F. Long-term prophylaxis of infection by selective decontamination in leukopenia and in mechanical ventilation. Rev Infect Dis. 1987;9:295–328. doi: 10.1093/clinids/9.2.295. [DOI] [PubMed] [Google Scholar]
- 9.Cramer J A, Prestegard J H. NMR studies of pH-induced transport of carboxylic acids across phospholipid vesicle membranes. Biochem Biophys Res Commun. 1977;75:295–301. doi: 10.1016/0006-291x(77)91042-7. [DOI] [PubMed] [Google Scholar]
- 10.Eklund T. The antimicrobial effect of dissociated and undissociated sorbic acid at different pH levels. J Appl Bacteriol. 1983;54:383–389. doi: 10.1111/j.1365-2672.1983.tb02632.x. [DOI] [PubMed] [Google Scholar]
- 11.Evans D J, Evans D G, Gorbach S L. Production of vascular permeability factor by enterotoxigenic Escherichia coli isolated from man. Infect Immun. 1973;8:725–730. doi: 10.1128/iai.8.5.725-730.1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feresu S, Nyati H. Fate of pathogenic and non-pathogenic Escherichia coli strains in two fermented milk products. J Appl Bacteriol. 1990;69:814–821. doi: 10.1111/j.1365-2672.1990.tb01578.x. [DOI] [PubMed] [Google Scholar]
- 13.Fichera G A, Pappalardo C, Furneri P M, Gismondo M R, Nicoletti G. Evaluation of antiinfective activity of an association Bifidobacterium/Lactobacillus in mouse intestine. G Batteriol Virol Immunol. 1987;80:189–205. [PubMed] [Google Scholar]
- 14.Francis D H, Moxley R A, Andraos C Y. Edema disease-like brain lesions in gnotobiotic piglets infected with Escherichia coli serotype O157:H7. Infect Immun. 1989;57:1339–1342. doi: 10.1128/iai.57.4.1339-1342.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fujii J, Kita T, Yoshida S I, Takeda T, Kobayashi H, Tanaka N, Ohsato K, Mizuguchi Y. Direct evidence of neuron impairment by oral infection with verotoxin-producing Escherichia coli O157:H− in mitomycin-treated mice. Infect Immun. 1994;62:3447–3453. doi: 10.1128/iai.62.8.3447-3453.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hudault S, Lievin V, Bernet-Camard M F, Servin A L. Antagonistic activity exerted in vitro and in vivo by Lactobacillus casei (strain GG) against Salmonella typhimurium C5 infection. Appl Environ Microbiol. 1997;63:513–518. doi: 10.1128/aem.63.2.513-518.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Isogai E, Isogai H, Takeshi K, Nishikawa T. Protective effect of Japanese green tea extract on gnotobiotic mice infected with an Escherichia coli O157:H7 strain. Microbiol Immunol. 1998;42:125–128. doi: 10.1111/j.1348-0421.1998.tb02260.x. [DOI] [PubMed] [Google Scholar]
- 18.Isogai E, Isogai H, Kimura K, Hayashi S, Kubota T, Fujii N, Takeshi K. Role of tumor necrosis factor alpha in gnotobiotic mice infected with an Escherichia coli O157:H7 strain. Infect Immun. 1998;66:197–202. doi: 10.1128/iai.66.1.197-202.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaila M, Isolauri E, Soppi E, Virtanen E, Laine S, Arvilommi H. Enhancement of the circulating antibody secreting cell response in human diarrhea by a human Lactobacillus strain. Pediatr Res. 1992;32:141–144. doi: 10.1203/00006450-199208000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Kaila M, Isolauri E, Saxelin M, Arvilommi H, Vesikari T. Viable versus inactivated Lactobacillus strain GG in acute rotavirus diarrhoea. Arch Dis Child. 1995;72:51–53. doi: 10.1136/adc.72.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karpman D, Connell H, Svensson M, Scheutz F, Alm P, Svanborg C. The role of lipopolysaccharide and Shiga-like toxin in a mouse model of Escherichia coli O157:H7 infection. J Infect Dis. 1997;175:611–620. doi: 10.1093/infdis/175.3.611. [DOI] [PubMed] [Google Scholar]
- 22.Keren D F, Brown J E, McDonald R A, Wassef J S. Secretory immunoglobulin A response to Shiga toxin in rabbits: kinetics of the initial mucosal immune response and inhibition of toxicity in vitro and in vivo. Infect Immun. 1989;57:1885–1889. doi: 10.1128/iai.57.7.1885-1889.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kurioka T, Yunou Y, Kita E. Enhancement of susceptibility to Shiga toxin-producing Escherichia coli O157:H7 by protein calorie malnutrition in mice. Infect Immun. 1998;66:1726–1734. doi: 10.1128/iai.66.4.1726-1734.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee Y K, Nomoto K, Salminen S, Gorbach S L. Role of probiotics in health and diseases. In: Lee Y K, Nomoto K, Salminen S, Gorbach S L, editors. Handbook of probiotics. New York, N.Y: John Wiley & Sons, Inc.; 1999. pp. 67–146. [Google Scholar]
- 25.Levin M. Escherichia coli that cause diarrhea: enterotoxigenic, enteropathogenic, enteroinvasive, enterohemorrhagic, and enteroadherent. J Infect Dis. 1987;155:377–389. doi: 10.1093/infdis/155.3.377. [DOI] [PubMed] [Google Scholar]
- 26.Li Z, Bell C, Buret A, Robins-Browne R, Stiel D, O'Loughlin E, Rademaker C M, Martinez L, Perea E J, Jansze M, Fluit A C, Glerum J H, Verhoef J. The effect of enterohemorrhagic Escherichia coli O157:H7 on intestinal structure and solute transport in rabbits. Gastroenterology. 1993;104:467–474. doi: 10.1016/0016-5085(93)90415-9. [DOI] [PubMed] [Google Scholar]
- 27.Lindgren S W, Melton A R, O'Brien A D. Virulence of enterohemorrhagic Escherichia coli O91:H21 clinical isolates in an orally infected mouse model. Infect Immun. 1993;61:3832–3842. doi: 10.1128/iai.61.9.3832-3842.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Link-Amster H, Rochat F, Saudan K Y, Mignot O, Aeschlimann J M. Modulation of a specific humoral immune response and changes in intestinal flora mediated through fermented milk intake. FEMS Immunol Med Microbiol. 1994;10:55–63. doi: 10.1111/j.1574-695X.1994.tb00011.x. [DOI] [PubMed] [Google Scholar]
- 29.Majamaa H, Isolauri E, Saxelin M, Vesikari T. Lactic acid bacteria in the treatment of acute rotavirus gastroenteritis. J Pediatr Gastroenterol Nutr. 1995;20:333–338. doi: 10.1097/00005176-199504000-00012. [DOI] [PubMed] [Google Scholar]
- 30.Malin M, Suomalainen H, Saxelin M, Isolauri E. Promotion of IgA immune response in patients with Crohn's disease by oral bacteriotherapy with Lactobacillus GG. Ann Nutr Metab. 1996;40:137–145. doi: 10.1159/000177907. [DOI] [PubMed] [Google Scholar]
- 31.McQueen C E, Boedeker E C, Le M, Hamada Y, Brown W R. Mucosal immune response to RDEC-1 infection: study of lamina propria antibody-producing cells and biliary antibody. Infect Immun. 1992;60:206–212. doi: 10.1128/iai.60.1.206-212.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Melton-Celsa A R, Darnell S C, O'Brien A D. Activation of Shiga-like toxins by mouse and human intestinal mucus correlates with virulence of enterohemorrhagic Escherichia coli O91:H21 isolates in orally infected, streptomycin-treated mice. Infect Immun. 1996;64:1569–1576. doi: 10.1128/iai.64.5.1569-1576.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Metchnikoff E. The prolongation of life. New York, N.Y: G. P. Putnam's Sons; 1908. [Google Scholar]
- 34.Myers L L, Shoop D S, Collins J E, Bradbury W C. Diarrheal disease caused by enterotoxigenic Bacteroides fragilis in infant rabbits. J Clin Microbiol. 1989;27:2025–2030. doi: 10.1128/jcm.27.9.2025-2030.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nader de Macias M E, Apella M C, Romero N C, Gonzalez S N, Oliver G. Inhibition of Shigella sonnei by Lactobacillus casei and Lact. acidophilus. J Appl Bacteriol. 1992;73:407–411. doi: 10.1111/j.1365-2672.1992.tb04996.x. [DOI] [PubMed] [Google Scholar]
- 36.Nakazawa M, Itoh K. Experimental infection of infant rabbits with verocytotoxin-producing Escherichia coli of bovine origin. Jap J Infect Dis. 1995;69:772–776. doi: 10.11150/kansenshogakuzasshi1970.69.772. [DOI] [PubMed] [Google Scholar]
- 37.National Institutes of Health. Guide for the care and use of laboratory animals. National Institutes of Health publication no. 85-23. Bethesda, Md: National Institutes of Health; 1985. [Google Scholar]
- 38.Noda M, Yutsudo T, Nakabayashi N, Hirayama T, Takeda Y. Purification and some properties of Shiga-like toxin from Escherichia coli O157:H7 that is immunologically identical to Shiga toxin. Microb Pathog. 1987;2:339–349. doi: 10.1016/0882-4010(87)90076-3. [DOI] [PubMed] [Google Scholar]
- 39.Nomoto K, Miake S, Hashimoto S, Yokokura T, Mutai M, Yoshikai Y. Augmentation of host resistance to Listeria monocytogenes infection by Lactobacillus casei. J Clin Lab Immunol. 1985;17:91–97. [PubMed] [Google Scholar]
- 40.Nomoto K, Yokokura T, Mitsuyama M, Yoshikai Y. Prevention of indigenous infection of mice with Escherichia coli by nonspecific immunostimulation. Antimicrob Agents Chemother. 1992;36:361–367. doi: 10.1128/aac.36.2.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Norton P M, Brown H W, Le Page R W. Mucosal and systemic responses following enteric exposure to lactic acid bacteria. Adv Exp Med Biol. 1995;371b:1559–1562. [PubMed] [Google Scholar]
- 42.Oku Y, Uesaka Y, Hirayama T, Takeda Y. Development of a highly sensitive bead-ELISA to detect bacterial protein toxins. Microbiol Immunol. 1988;32:807–816. doi: 10.1111/j.1348-0421.1988.tb01442.x. [DOI] [PubMed] [Google Scholar]
- 43.Oku Y, Yutsudo T, Hirayama T, O'Brien A D, Takeda Y. Purification and some properties of a Vero toxin from a human strain of Escherichia coli that is immunologically related to Shiga-like toxin II (VT2) Microb Pathog. 1989;6:113–122. doi: 10.1016/0882-4010(89)90014-4. [DOI] [PubMed] [Google Scholar]
- 44.Pai C H, Kelly J K, Meyers G L. Experimental infection of infant rabbits with verotoxin-producing Escherichia coli. Infect Immun. 1986;51:16–23. doi: 10.1128/iai.51.1.16-23.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Paton A W, Ratcliff R M, Doyle R M, Seymour-Murray J, Davos D, Lanser J A, Paton J C. Molecular microbiological investigation of an outbreak of hemolytic-uremic syndrome caused by dry fermented sausage contaminated with Shiga-like toxin-producing Escherichia coli. J Clin Microbiol. 1996;34:1622–1627. doi: 10.1128/jcm.34.7.1622-1627.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paton A W, Voss E, Manning P A, Paton J C. Antibodies to lipopolysaccharide block adherence of Shiga toxin-producing Escherichia coli to human intestinal epithelial (Henle 407) cells. Microb Pathog. 1998;24:57–63. doi: 10.1006/mpat.1997.0172. [DOI] [PubMed] [Google Scholar]
- 47.Perdigon G, Nader de Macias M E, Alvarez S, Oliver G, Pesce de Ruiz Holgado A A. Prevention of gastrointestinal infection using immunobiological methods with milk fermented with Lactobacillus casei and Lactobacillus acidophilus. J Dairy Res. 1990;57:255–264. doi: 10.1017/s002202990002687x. [DOI] [PubMed] [Google Scholar]
- 48.Perdigon G, Alvarez S, Pesce de Ruiz Holgado A. Immunoadjuvant activity of oral Lactobacillus casei: influence of dose on the secretory immune response and protective capacity in intestinal infections. J Dairy Res. 1991;58:485–496. doi: 10.1017/s0022029900030090. [DOI] [PubMed] [Google Scholar]
- 49.Perdigon G, Alvarez S, Rachid M, Aguero G, Gobbato N. Immune system stimulation by probiotics. J Dairy Sci. 1995;78:1597–1606. doi: 10.3168/jds.S0022-0302(95)76784-4. [DOI] [PubMed] [Google Scholar]
- 50.Potter M E, Kaufmann A F, Thomason B M, Blake P A, Farmer J J., III Diarrhea due to Escherichia coli O157:H7 in the infant rabbit. J Infect Dis. 1985;152:1341–1343. doi: 10.1093/infdis/152.6.1341. [DOI] [PubMed] [Google Scholar]
- 51.Rowe P C, Orrbine E, Lior H, Wells G A, Yertisir E, Clulow M, McLaine P N. Risk of hemolytic uremic syndrome after sporadic Escherichia coli 0157:H7 infection: results of a Canadian collaborative study. Investigators of the Canadian Pediatric Kidney Disease Research Center. J Pediatr. 1998;132:777–782. doi: 10.1016/s0022-3476(98)70303-8. [DOI] [PubMed] [Google Scholar]
- 52.Sato K. Enhancement of host resistance against Listeria infection by Lactobacillus casei: role of macrophages. Infect Immun. 1984;44:445–451. doi: 10.1128/iai.44.2.445-451.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sato K, Saito H, Tomioka H. Enhancement of host resistance against Listeria infection by Lactobacillus casei: activation of liver macrophages and peritoneal macrophages by Lactobacillus casei. Microbiol Immunol. 1988;32:689–698. doi: 10.1111/j.1348-0421.1988.tb01430.x. [DOI] [PubMed] [Google Scholar]
- 54.Shornikova A V, Casas I A, Isolauri E, Mykkanen H, Vesikari T. Lactobacillus reuteri as a therapeutic agent in acute diarrhea in young children. J Pediatr Gastroenterol Nutr. 1997;24:399–404. doi: 10.1097/00005176-199704000-00008. [DOI] [PubMed] [Google Scholar]
- 55.Sjogren R, Neill R, Rachmilewitz D, Fritz D, Newland J, Sharpnack D, Colleton C, Fondacaro J, Gemski P, Boedeker E. Role of Shiga-like toxin I in bacterial enteritis: Comparison between isogenic Escherichia coli strains induced in rabbits. Gastroenterology. 1994;106:306–317. doi: 10.1016/0016-5085(94)90587-8. [DOI] [PubMed] [Google Scholar]
- 56.Smith J W, Hand W L, Sanford J P. Synthesis and secretion of local immunoglobulin by the intestinal tract of newborn rabbits. J Infect Dis. 1971;124:494–498. doi: 10.1093/infdis/124.5.494. [DOI] [PubMed] [Google Scholar]
- 57.Tarr P I. Escherichia coli O157:H7: clinical, diagnostic, and epidemiological aspects of human infection. Clin Infect Dis. 1995;20:1–8. doi: 10.1093/clinids/20.1.1. [DOI] [PubMed] [Google Scholar]
- 58.Trammer J. Inhibitory effect of Lactobacillus acidophilus. Nature. 1966;211:204–205. doi: 10.1038/211204a0. [DOI] [PubMed] [Google Scholar]
- 59.Tzipori S, Wachsmuth I K, Chapman C, Birden R, Brittingham J, Jackson C, Hogg J. The pathogenesis of hemorrhagic colitis caused by Escherichia coli O157:H7 in gnotobiotic piglets. J Infect Dis. 1986;154:712–716. doi: 10.1093/infdis/154.4.712. [DOI] [PubMed] [Google Scholar]
- 60.Vollaard E J, Clasener H A. Colonization resistance. Antimicrob Agents Chemother. 1994;38:409–414. doi: 10.1128/aac.38.3.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wadolkowski E A, Burris J A, O'Brien A D. Mouse model for colonization and disease caused by enterohemorrhagic Escherichia coli O157:H7. Infect Immun. 1990;58:2438–2445. doi: 10.1128/iai.58.8.2438-2445.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wadolkowski E A, Sung L M, Burris J A, Samuel J E, O'Brien A D. Acute renal tubular necrosis and death of mice orally infected with Escherichia coli strains that produce Shiga-like toxin type II. Infect Immun. 1990;58:3959–3965. doi: 10.1128/iai.58.12.3959-3965.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Whipp S C, Rasmussen M A, Cray W C., Jr Animals as a source of Escherichia coli pathogenic for human beings. J Am Vet Med Assoc. 1994;204:1168–1175. [PubMed] [Google Scholar]
- 64.Xin-He L, Xu J-G, Liu B-Y. Experimental infection of specific-pathogen-free mice with enterohemorrhagic Escherichia coli O157:H7. Microbiol Immunol. 1991;35:515–524. doi: 10.1111/j.1348-0421.1991.tb01582.x. [DOI] [PubMed] [Google Scholar]
- 65.Yamasaki S, Lin Z, Shirai H, Terai A, Oku Y, Ito H, Ohmura M, Karasawa T, Tsukamoto T, Kurazono H, Takeda Y. Typing of verotoxins by DNA colony hybridization with poly- and oligonucleotide probes, a bead-enzyme-linked immunosorbent assay, and polymerase chain reaction. Microbiol Immunol. 1996;40:345–352. doi: 10.1111/j.1348-0421.1996.tb01078.x. [DOI] [PubMed] [Google Scholar]
- 66.Yuki N, Watanabe K, Mike A, Tagami Y, Tanaka R, Ohwaki M, Morotomi M. Survival of a probiotic, Lactobacillus casei strain Shirota, in the gastrointestinal tract: selective isolation from feces and identification using monoclonal antibodies. Int J Food Microbiol. 1999;48:51–57. doi: 10.1016/s0168-1605(99)00029-x. [DOI] [PubMed] [Google Scholar]
- 67.Yutsudo T, Nakabayashi N, Hirayama T, Takeda Y. Purification and some properties of a Vero toxin from Escherichia coli O157:H7 that is immunologically unrelated to Shiga toxin. Microb Pathog. 1987;3:21–30. doi: 10.1016/0882-4010(87)90034-9. [DOI] [PubMed] [Google Scholar]