Abstract
Background
The surgical treatment for distal femur fractures has evolved over time, and it depends upon certain factors; open or closed fracture type, the pattern of fracture, presence of metaphyseal comminution, intra-articular extension, and the bone quality are some of the crucial ones. Both retrograde intramedullary nails (RIMN) and locking plates (LP) can be used for the fixation of these fractures. However, the optimal method among the two devices is still a topic of debate, the superiority of one over the other being unclear. Hence, this systematic review and meta-analysis was conceptualized to compare the outcomes of RIMN with distal femur LP.
Methods
The primary electronic search was conducted on Medline (PubMed), Scopus, Embase, Cinahl, and Cochrane Library databases for the published literature from the inception to 25th February 2022. The studies compared outcomes of RIMN versus LP fixation of the acute supracondylar or distal femur fracture (AO/OTA type-33A, B, and C) and reported at least one primary (mean fracture union time, complications, implant-related complications, and re-operation rate) or secondary outcome (duration of surgery, intra-operative blood loss, and knee range of motion), were included.
Results
Six randomized control trials, 2 prospective and 8 retrospective studies with 936 patients with 8 bilateral cases (467: RIMN; 477: LP) were included. Our analysis demonstrated no statistically significant difference in terms of mean fracture union time, overall complications, implant-related complications, re-operation rates, and duration of surgeries. Although a better knee range of motion was seen in the LP group, however, it also showed more nonunion and infection than the RIMN group.
Conclusion
The present review shows that there are significantly lesser nonunions and infections, in the RIMN group as compared to LP for distal femur fractures, although a better postoperative knee range of motion was seen in the latter. However, in terms of fracture union time, the overall rate of complications, re-operation rates, and duration of surgeries, there is no difference between the two surgical options.
Keywords: Distal femur fracture, Supracondylar femur fracture, Retrograde femoral nail, Distal femoral nail, Locking plate, Distal femoral locking plate
Highlights
-
•
Distal femur fractures account for 0.4% of all fractures, 3–6% of femur fractures. They result from low-energy trauma in elderly osteoporotic bones, and high energy trauma in younger individuals. Surgical treatment options have evolved over time however, the optimal method implant used for fixation is still a topic of debate.
-
•
The present meta-analysis was planned to compare the outcomes of RIMN to and LP for distal femur fracture fixation form currently available literature.
-
•
The present review shows that there are significantly lesser nonunion, and infections in RIMN compared toLP for distal femur fractures. However, a better knee range of motion was seen in the latter. In terms of fracture union time, overall rate of complications, re-operation, and duration of surgeries, no difference was seen.
1. Background
Low-energy trauma in elderly patients with osteoporotic bones and high-energy trauma in young adults causes distal femur fractures, which comprise of 0.4% of all fractures and 3–6% of femur fractures.1,2 Distal femur fracture treatment remains challenging, and they must be surgically treated to achieve an optimal outcome.1, 2, 3 Surgical treatment options have evolved over time, and the choices are dependent on factors like open or closed fracture types, the pattern of fractures, the presence of metaphyseal comminution, intra-articular extension, and bone quality.4
Earlier, open reduction and internal fixation with extramedullary implants were considered as the standard treatment for these fractures; and have a high incidence of postoperative complications in view of excessive intraoperative soft tissue stripping. Frequent secondary interventions like bone grafting were required to augment healing or attain fracture union.5 With the advent of LP, the ease of fracture fixation and the complications were minimized with excellent results, and currently, these are the most commonly used implants for periarticular distal femur fractures.4,6
Green et al.7 in 1988 introduced the RIMN for the fixation of distal femur fractures, with advantages like indirect reduction and internal fixation, which avoid soft tissue damage and disruption of blood supply and give excellent union rates in distal femur fractures.8,9 Being intramedullary, nails are load-sharing devices that remain close to the femoral axis, with better stress distribution than an eccentrically placed plate and screws construct; nailing also requires a short operative time, and there is less perioperative blood loss, and patients can be mobilized early.4,10
However, the optimal method among the two devices is still a topic of debate, with the superiority of one over the other being unclear in terms of advantages and disadvantages.11,12 In literature, there have been reviews, but with a limited number of studies, some of which also included results of dynamic condylar screws.13,14 Hence, this systematic review and meta-analysis was carried out to include as many eligible studies as possible and to compare the outcomes of RIMN with distal femur LP in terms of fracture union time, complications, duration of surgeries, intra-operative blood loss, and knee range of motion.
2. Methods
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines [15.]. A protocol of the systematic review was formulated and registered at the International Prospective Register of Systematic Reviews (PROSPERO) vide registration id: CRD42021258496.
3. Literature search
Three authors (RKR, PK, and AS) used a pre-formulated well-defined search strategy without initial limitation to the language and country of publication to conduct a primary search of the electronic databases of Medline (PubMed), Scopus, Embase, Cinahl, and Cochrane Library (an additional database was searched which was not mentioned in PROSPERO protocol registration) from the inception to 25th February 2022 [Table 1]. A manual search of the bibliography of the review articles and the included articles was done to find any potentially missed relevant articles. Additionally, we looked for other relevant studies in the electronic databases of a few pertinent peer-reviewed publications. Finally, a total of 1945 results were obtained.
Table 1.
Literature search strategy used for the study.
| Database | Period -from inception to 258h February 2022 with keywords | Results |
|---|---|---|
| MEDLINE (PubMed) | (((“distal"[All Fields] OR “distalization"[All Fields] OR “distalize"[All Fields] OR “distalized"[All Fields] OR “distalizer"[All Fields] OR “distalizers"[All Fields] OR “distalizes"[All Fields] OR “distalizing"[All Fields] OR “distally"[All Fields] OR “distals"[All Fields]) AND (“femoral fractures"[MeSH Terms] OR (“femoral"[All Fields] AND “fractures"[All Fields]) OR “femoral fractures"[All Fields] OR (“femur"[All Fields] AND “fracture"[All Fields]) OR “femur fracture"[All Fields])) OR (“supracondylar"[All Fields] AND (“femoral fractures"[MeSH Terms] OR (“femoral"[All Fields] AND “fractures"[All Fields]) OR “femoral fractures"[All Fields] OR (“femur"[All Fields] AND “fracture"[All Fields]) OR “femur fracture"[All Fields]))) AND ((“retrograde"[All Fields] OR “retrogradely"[All Fields]) AND (“fracture fixation, intramedullary"[MeSH Terms] OR (“fracture"[All Fields] AND “fixation"[All Fields] AND “intramedullary"[All Fields]) OR “intramedullary fracture fixation"[All Fields] OR “nailing"[All Fields] OR “nail s"[All Fields] OR “nailed"[All Fields] OR “nailings"[All Fields] OR “nails"[MeSH Terms] OR “nails"[All Fields])) AND ((“bone plates"[MeSH Terms] OR (“bone"[All Fields] AND “plates"[All Fields]) OR “bone plates"[All Fields] OR “plate"[All Fields] OR “plate s"[All Fields] OR “plated"[All Fields] OR “plates"[All Fields] OR “plating"[All Fields] OR “platings"[All Fields]) AND (“fixate"[All Fields] OR “fixated"[All Fields] OR “fixates"[All Fields] OR “fixating"[All Fields] OR “fixation"[All Fields] OR “fixational"[All Fields] OR “fixations"[All Fields] OR “fixator"[All Fields] OR “fixator s"[All Fields] OR “fixators"[All Fields])) | 130 |
| Embase | (('distal femur fracture' OR (supracondylar AND femur AND fracture)) AND ′locking plate fixation' OR ′locking compression plate') AND ′retrograde intramedullary nailing' OR ′retrograde nailing' | 290 |
| Scopus | (ALL(distal AND femur AND fracture) OR ALL (supracondylar AND femur AND fracture) AND ALL (locking AND plate AND fixation) OR ALL (locking AND compression AND plate AND fixation) AND ALL (retrograde AND nailing) OR ALL (retrograde AND intramedullary AND nailing)) | 753 |
| Cinahl | TX distal femur fracture OR TX supracondylar fracture femur AND TX locking plate fixation OR TX locking compression plate AND TX retrograde intramedullary nailing OR TX retrograde nailing | 432 |
| Cochrane Library | Cochrane Reviews matching distal femur fracture in All Text OR supracondylar femur fracture in All Text AND retrograde intramedullary nail in All Text OR retrograde nailing in All Text AND plate fixation in All Text - (Word variations have been searched) | 340 |
| Total | 1945 | |
4. PICO framework for the study
Participants: Adult humans with distal femur fractures.
Intervention: Retrograde intramedullary nailing.
Control: Open reduction and internal fixation with locking plate.
Outcomes: Mean fracture union time, complications, duration of surgery, implant-related complication, re-operation rate, intra-operative blood loss, and knee range of motion.
5. Inclusion and exclusion criteria
Randomized control trials (RCTs) or non-randomized studies in the English language that compared outcomes of RIMN versus LP fixation of acute supracondylar or distal femur fractures (AO/OTA type-33A, B, and C), and reported at least one outcome interest of the review were included. Single cohort arm studies that have not compared the outcomes of RIMN versus LP for distal femur fracture fixation or those included patients aged <18 years, periprosthetic fractures, fracture non-union, pathological fracture, the study included the fixation of distal femur fracture other than RIMN and LP were excluded. Conference abstracts, book chapters, case reports, e-posters, review articles, cadaveric studies, biomechanical studies, and articles in languages other than English were also excluded.
6. Study selection
Based on the title of the article and abstracts, three authors (RKR, SA, and PK) independently screened the studies, and those found eligible for the study outcome were chosen. After the assessment of the full text of all selected studies, based on the inclusion and exclusion criteria, relevant studies were included in the current review. A disagreement among the authors was settled through mutual agreement.
7. Data extraction
Three authors (PK, RUH, and AS) extracted data from the studies and entered it into an excel spreadsheet with the names of the authors, the year the article was published, the level of evidence, the total number of patients, implants used, the number of patients in the individual group, pertinent demographic data, and the primary and secondary outcomes. This information was compiled in a table [Table-2] and outcome of intersts in Table 3 and 4. To eliminate any potential operator-dependent bias, all the writers of the current review studied and discussed each of the publications that were ultimately chosen. The current review included 16 studies that were relevant to the current systematic review and meta-analysis [Fig. 1].
Table 2.
Characteristics of included studies.
| Sl no. | Study | Study design | Level of evidence | Implant used | Number of patients/cases | Male/Female | Mean age in years (range/SD) | AO -Classification A1/A2/A3/B/C1/C2/C3 |
Open/closed fracture | Mean follow up (months) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Markmiller et al. 200419 | Prospective | III | RIMN | 16 (Overall total case = 39 (7 cases bilateral) | 14/2 | 43.7 (20–77) | A-11/C-8 one loss to follow up | High energy trauma-7 | Overall 12 |
| LP | 16 | 6/10 | 57.2 (17–83) | A-10/C-10 | High energy trauma-9 | |||||
| 2 | Thomson et al. 200820 | Retrospective | III | RIMN | 11 | 6/5 | 50.5 | Type-C | NR | Overall 80 |
| LP | 11 (one bilateral) = 12 cases | 7/4 | 49.9 | Type-C | NR | |||||
| 3 | Henderson et al. 201021 | Retrospective | III | RIMN | 12 | 4/8 | 63 (23–87) | A1-2, A2-2, A3-3 C1–1, C2-3, C3-1 | High energy-2 | 16.75 |
| LP | 12 | 3/9 | 65(25–96) | A1-2, A2-2, A3-3 C1–1, C2-3, C3-1 | High energy-3 | 14.25 | ||||
| 4 | Hierholzer et al. 201122 | Retrospective | III | RIMN | 59 | NR | Overall-54 (17–89) | A1:31, C:28 | High energy-31, Open-19 |
13 |
| LP | 56 | NR | A1:21, C:35 | High energy—37, Open-31 |
15 | |||||
| 5 | Gao et al. 201223 | Retrospective | III | RIMN | 17 | 13/4 | 50.6 ± 16.3 | A1/A2/A3-6/8/3 | High energy trauma-13 Multiple injury-5 |
26.29 ± 12.71 |
| LP | 19 | 12/7 | 54.7 ± 16.1 | A1/A2/A3-8/7/4- | High energy trauma-12, Multiple injury-3 | 23.37 ± 5.33 | ||||
| 6 | Demirtas et al. 201411 | Retrospective | III | RIMN | 13 | 11/2 | 31.1 | A1/A2/A3-4/5/4 | High energy-12, open-6 | 26.7 |
| LP | 15 | 13/2 | 36 | A1/A2/A3-3/5/7 | High energy-14, open-7 | 31.3 | ||||
| 7 | Chander et al. 201524 | Prospective | RIMN | 24 | NR | Overall 21-70 | A/C only | NR | Overall 12 | |
| LP | 30 | NR | A/C only | NR | ||||||
| 8 | Ciloglu et al. 201725 | RCT | I | RIMN | 23 | 16/7 | 37.2 ± 12.7 | A1/A2/A3-5/14/4 | High energy-15, Open-7 | 40 |
| LP | 24 | 18/6 | 42.6 ± 13 | A1/A2/A3/B1/C1-5/10/7/1/1 | High energy-17, Open-8 | 35 | ||||
| 9 | Gill et al. 201712 | RCT | I | RIMN | 20 | 13/7 | 36.0 ± 14.1 | A1/A2/A3-7/10/3 | high-energy-14, Open-5 | 27.8 ± 7 |
| LP | 22 | 16/6 | 38.7 ± 15.6 | A1/A2/A3-9/8/5 | high-energy-14, open-7 | 29.2 ± 92 | ||||
| 10 | Aggarwal et al. 20184 | RCT | I | RIMN | 20 | 15/5 | 39.6 | A3-6/C2-7/C3-2, rest unknown | high-energy-17, Open-7 | Overall 11.34 |
| LP | 20 | 16/4 | 37.4 | A3-4/C2-7/C3-5, rest unknown | high-energy-19, open-9 | |||||
| 11 | Rollo et al. 201926 | Retrospective | III | RIMN | 15 | 11/4 | 42.67 ± 18.32 | A/B/C-5/5/5 | high-energy-10 | Overall 16.24 ± 0.44 |
| LP | 15 | 11/4 | 42.84 ± 18.32 | A/B/C-5/5/5 | high-energy-10 | |||||
| 12 | Gupta et al. 202127 | RCT | I | RIMN | 20 | Overall 35/5 | Overall 47 (28–70) | NR | Overall High energy-35 | Overall 12 |
| LP | 20 | NR | ||||||||
| 13 | Ahmed et al. 202128 | RCT | I | RIMN | 80 | 56/24 | 33.9 ± 10.26 | NR | ||
| LP | 80 | 49/31 | 33.2 ± 48.61 | NR | ||||||
| 14 | Mahar et al. 202129 | RCT | I | RIMN | 50 | 30/20 | 20–60 | A1-32, A2-11 A3-7 | 31-high velocity | Minimum 6 |
| LP | 50 | 35/15 | 20–60 | A1-32, A2-11 A3-7 | 31-high velocity | Minimum 6. | ||||
| 15 | Meccariello et al. 202130 | Retrospective | III | RIMN | 30 | 22/8 | 42.67 ± 18.32 | A1-4, A2-4, A3-2 B1–4, B2-2, B3-4, C1-4, C2-4, C3-2 | RTA-16 | 17.32 ± 0.42 |
| LP | 30 | 20/10 | 42.84 ± 18.32 | A1-4, A2-5, A3-2 B1–5, B2-1, B3-5, C1-3, C2-4, C3-1 | RTA-19 | 16.45 ± 0.47 | ||||
| 16 | Vemulapalli et al. 202231 | Retrospective | III | RIMN | 50 | Overall 55/51 | 51 (21–86) | AO/OTA 33-C type | Overall 50-open, 56-closed | 11 |
| LP | 56 | 51 (21–86) | AO/OTA 33-C type | 12.7 |
RIMN-Retrograde intramedullary nail, LP-locking plate, NR-Not reported.
Table 3.
Data reporting duration of surgery, fracture union time, blood loss, and knee range of motion.
| Sl no. | Study | Implant used | Duration of surgery in minutes | Mean fracture union time (weeks) | Blood loss (ml) | Knee ROM |
|---|---|---|---|---|---|---|
| 1 | Markmiller et al. 200419 | RIMN | NR | 14.6 | NR | 103 |
| LP | NR | 13.8 | NR | 110 | ||
| 2 | Thomson et al. 200820 | RIMN | NR | NR | NR | 1210 |
| LP | NR | NR | NR | 1020 | ||
| 3 | Henderson et al. 201021 | RIMN | NR | NR | NR | 2–970 |
| LP | NR | NR | NR | 0–990 | ||
| Hierholzer et al. 201122 | RIMN | NR | NR | NR | NR | |
| LP | NR | NR | NR | NR | ||
| 5 | Gao et al. 201224 | RIMN | 87.4 ± 13.2 | NR | 298 ± 65.2 | 103.5 ± 11.0 |
| LP | 79.7 ± 14.3 | NR | 200 ± 48.9 | 98.2 ± 21.5 | ||
| 6 | Demirtas et al. 201411 | RIMN | NR | 22.3 ± 10 | NR | NR |
| LP | NR | 25.7 ± 15 | NR | NR | ||
| 7 | Chander et al. 201524 | RIMN | NR | 18 | NR | NR |
| LP | NR | 14 | NR | NR | ||
| 8 | Ciloglu et al. 201725 | RIMN | NR | 25.3 ± 5.7 | NR | 102.6 ± 16.5 |
| LP | NR | 22.3 ± 9 | NR | 115.8 ± 18.3 | ||
| 9 | Gill et al. 201712 | RIMN | 102.3 ± 20.6 | 22.6 ± 13.1 | 323.0 ± 74.3 | 107.0 ± 9.9 |
| LP | 88.4 ± 17.6 | 26.5 ± 12.9 | 228.2 ± 45.8 | 112.0 ± 9.8 | ||
| 10 | Aggarwal et al. 20184 | RIMN | 105 | 14.6 | NR | Mean flexion 113.4 |
| LP | 110 | 16.2 | NR | Mean flexion 106.3 | ||
| 11 | Rollo et al. 201926 | RIMN | 52.8 ± 15.6 | 20.29 ± 2.24 | NR | NR |
| LP | 60.8 ± 20.4 | 20.43 ± 2.06 | NR | NR | ||
| 112 | Gupta 202127 | RIMN | NR | 15.2 ± 4.83 | NR | 109.5.2 ± 11.46 |
| LP | NR | 18.4 ± 1.23 | NR | 104.75 ± 8.19 | ||
| 13 | Ahmed et al. 202128 | RIMN | 83.29 ± 7.48 | NR | NR | NR |
| LP | 106.62 ± 7.69 | NR | NR | NR | ||
| 14 | Mahar et al. 202129 | RIMN | NR | 25.36 ± 6.32 | NR | NR |
| LP | NR | 24.16 ± 3.4 | NR | NR | ||
| 15 | Meccariello et al. 202130 | RIMN | 51.6 ± 17.6 | 20.64 ± 2.27 | NR | NR |
| LP | 62.7 ± 21.3 | 20.46 ± 2.01 | NR | NR | ||
| 16 | Vemulapalli et al. 202232 | RIMN | NR | 23.2 ± 13.6 | NR | NR |
| LP | NR | 26.4 ± 18.4 | NR | NR |
RIMN-Retrograde intramedullary nail, LP-locking plate, NR-Not reported.
Table 4.
Complications during the follow-up period.
| Sl no. | Study | Implant used | Non-union | Delayed union | Mal-union | Knee Stiffness | Knee pain | Re-operation | Implant related complications | Infection (superficial or deep) | Others | Overall complications |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Markmiller et al. 200420 | RIMN | 1 | NR | 2 | NR | 7 | 2 | NR | 1 | NR | 11 |
| LP | 2 | NR | 3 | NR | 6 | 2 | NR | 0 | NR | 11 | ||
| 2 | Thomson et al. 200821 | RIMN | 1 | NR | 0 | NR | NR | 1 | NR | 0 | NR | 1 |
| Plate | 4 | NR | 5 | NR | NR | 8 | NR | 3 | NR | 12 | ||
| 3 | Henderson et al. 201022 | RIMN | 1 | 0 | 1 | NR | NR | 4 | NR | 0 | NR | 2 |
| LP | 2 | 1 | 4 | NR | NR | 2 | NR | 0 | NR | 7 | ||
| Hierholzer et al. 201123 | RIMN | 5 | NR | NR | NR | NR | 42 | 36 | 1 | 1 | 43 | |
| LP | 6 | NR | NR | NR | NR | 18 | 4 | 5 | 3 | 18 | ||
| 5 | Gao et al. 201224 | RIMN | 1 | 0 | 2 | NR | 3 | 1 | 0 | 0 | NR | 6 |
| LP | 3 | 4 | 1 | NR | 1 | 4 | 2 | 1 | NR | 12 | ||
| 6 | Demirtas et al. 201412 | RIMN | 1 | 2 | 3 | 8 | 3 | NR | 0 | NR | NR | 17 |
| LP | 2 | 3 | 4 | 9 | 3 | NR | 1 | NR | NR | 22 | ||
| 7 | Chander et al. 201525 | RIMN | 1 | NR | NR | NR | NR | 8 | 1 | 0 | NR | 2 |
| LP | 1 | NR | NR | NR | NR | 3 | 4 | 2 | NR | 7 | ||
| 8 | Ciloglu et al. 201726 | RIMN | NR | 0 | 10 | 9 | 4 | 0 | NR | 0 | NR | 23 |
| LP | NR | 1 | 3 | 3 | 2 | 1 | NR | 0 | NR | 9 | ||
| 9 | Gill et al. 201713 | RIMN | 2 | 1 | 6 | NR | 1 | 1 | 0 | 3 | NR | 13 |
| LP | 2 | 5 | 3 | NR | 4 | 2 | 1 | 5 | NR | 20 | ||
| 10 | Aggarwal et al. 20186 | RIMN | 0 | 0 | 3 | 2 | NR | 0 | 0 | NR | 2 | 7 |
| LP | 0 | 1 | 2 | 5 | NR | 2 | 4 | NR | 3 | 15 | ||
| 11 | Rollo et al. 201927 | RIMN | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| LP | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | ||
| 12 | Gupta 202128 | RIMN | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| LP | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | ||
| 13 | Ahmed et al. 202129 | RIMN | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| LP | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | ||
| 14 | Mahar et al. 202130 | RIMN | 0 | 5 | NR | NR | NR | NR | NR | 0 | NR | 5 |
| LP | 0 | 2 | NR | NR | NR | NR | NR | 0 | NR | 2 | ||
| 15 | Meccariello et al. 202131 | RIMN | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| LP | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | ||
| 16 | Vemulapalli et al. 202232 | RIMN | 4 | NR | NR | NR | NR | 8 | NR | 1 | NR | 5 |
| LP | 11 | NR | NR | NR | NR | 18 | NR | 3 | NR | 14 |
RIMN-Retrograde intramedullary nail, LP-locking plate, NR-Not reported.
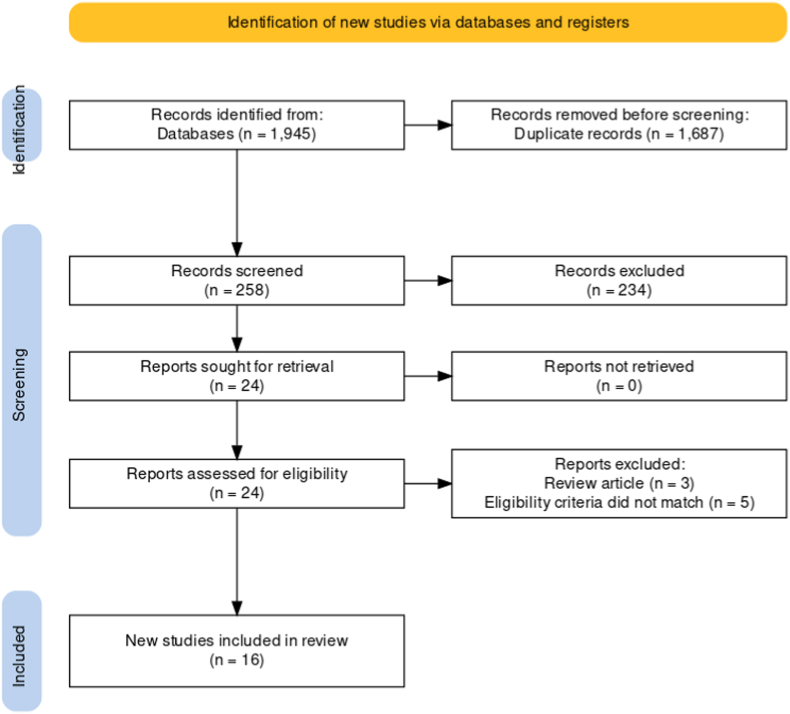
Fig. 1.
PRISMA flow diagram of study selection.
8. Outcome measure
The primary outcomes of interest were the mean fracture union time, complications (delayed union, non-union, malunion, knee stiffness, knee pain, infection, limb shortening >1.5 cm, and implant-related complications), and re-operation rate. The secondary outcomes were duration of surgery, intra-operative blood loss, knee range of motion, and functional outcome.
9. Statistical analysis
The qualitative data from individual studies were presented in tabular form for comparison purposes and included the baseline study characteristics as well as the primary and secondary study outcomes. If a specific outcome of interest was reported in two or more studies, a meta-analysis was performed. The effects measures for continuous variables were expressed with mean Difference or standard mean difference, and for dichotomous variables, it was expressed with odds ratio or relative risk. All of the findings were accompanied by 95% confidence intervals. Heterogeneity was evaluated by the use of the I2 test. Any cause of clinical heterogeneity was also investigated. If the heterogeneity was found low (I2 close to 0%) a fixed-effects model was used; otherwise, a random-effects model. Wherever possible, non-RCTs and RCTs were subjected to subgroup analysis. For the visual presentation of each outcome of interest, a forest plot was plotted and shown. All statistical analyses were carried out using Review Manager Software version 5.4. (RevMan 5.4.1).16
10. Risk of bias assessment
Assessment of the risk of bias was done by two independent observers (RKR and KR). MINORS tool17 was used for the assessment of the risk of bias in non-randomized comparative studies, and for RCTs, the Cochrane Collaboration's risk of bias tool18 was used. Any discrepancy was resolved by mutual agreement among the observers. The risk of bias and publication bias was assessed by Rev Man 5.4.1 software.16
11. Results
11.1. Search and screening
For each of the five searched databases, the results of the search strategy have been summarized in the table-1 using the PRISMA flowchart. Combining the results of all five databases yielded a total of 1945 results. 1687 articles were excluded after removing duplicates and articles not relevant to the current review. The remaining 258 studies were further reviewed. Following the screening through the titles and abstracts, 28 articles were identified, and the full text of all these articles was evaluated for eligibility. Finally, 16 articles4,11,12,19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31 were included in the current systematic review and meta-analysis [Fig. 1].
11.2. Characteristics of the included studies
8/16 included studies were prospective in design,4,12,19,24,25,27, 28, 29 with 6 being RCTs4,12,25,27, 28, 29 and the remaining 8 being retrospective.12,21, 22, 23, 24,27,31,32 The current study included 936 patients with 944 distal femur fractures. The RIMN was used in 467 fractures, while the LP was used in 477 fractures. The gender of the patients was reported in only 14/16 studies for the two groups treatment, with 472 males and 261 females. The patients' mean age ranged from 20 to 65 years, and the average follow-up period was 6–80 months.
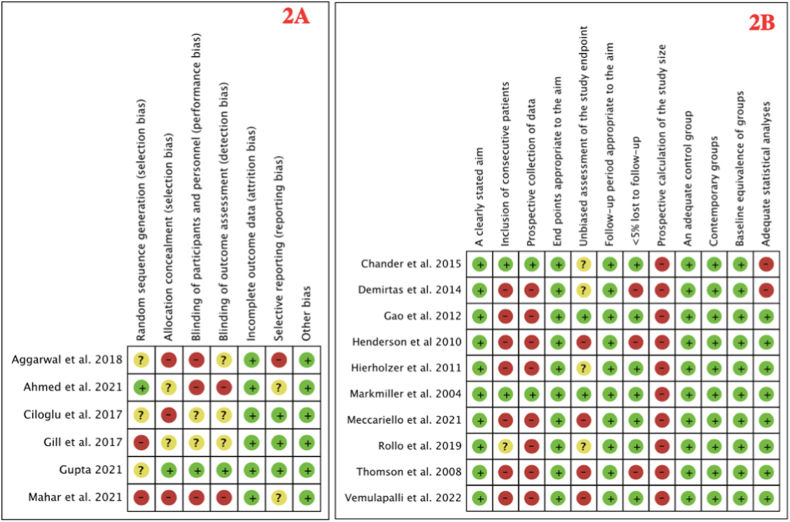
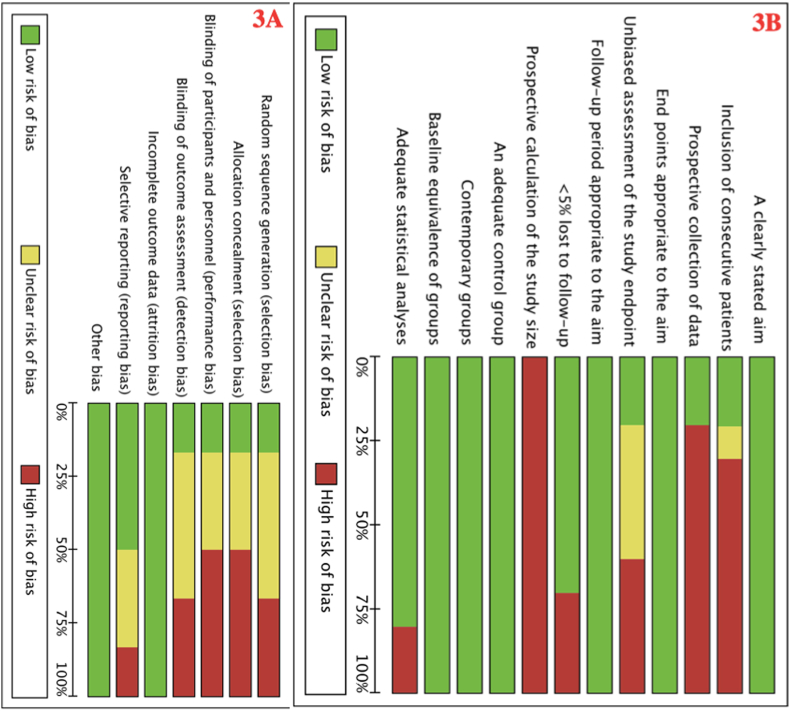
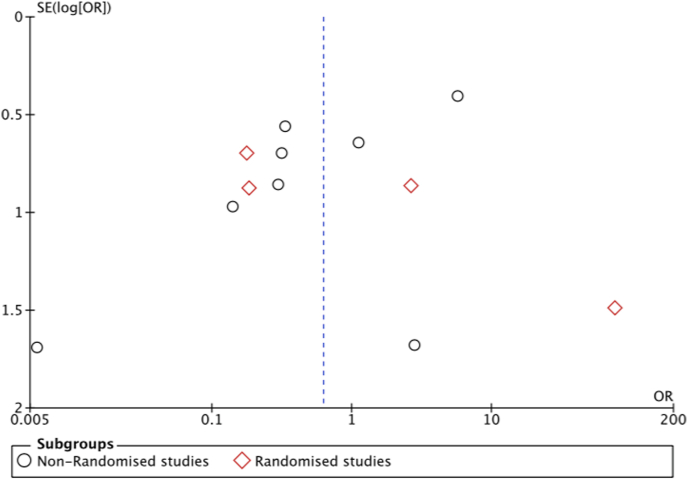
11.3. Assessment of risk of bias
There were ten non-randomized comparative studies11,19, 20, 21, 22, 23, 24,26,30,31 and six RCTs.4,12,25,27, 28, 29 For 7/10 non-randomized comparative studies, the MINORS tool Score was 16.19,22, 23, 24,26,30,31 The risk of bias summary and graph of all included articles is shown in Fig. 2, Fig. 3 respectively. For the assessment of publication bias, a funnel plot was used. The funnel plot revealed a skewed distribution, indicating possible publication bias (Fig. 4).
Fig. 2.
(a) Risk of bias summary for a non-nonrandomized, and (b) Randomized studies.
Fig. 3.
(a) Risk of bias graph for nonrandomized, and (b) Randomized studies.
Fig. 4.
Funnel plot showing a skewed distribution suggestive of possible publication bias.
11.4. Primary outcomes
-
1.
Mean fracture union time:
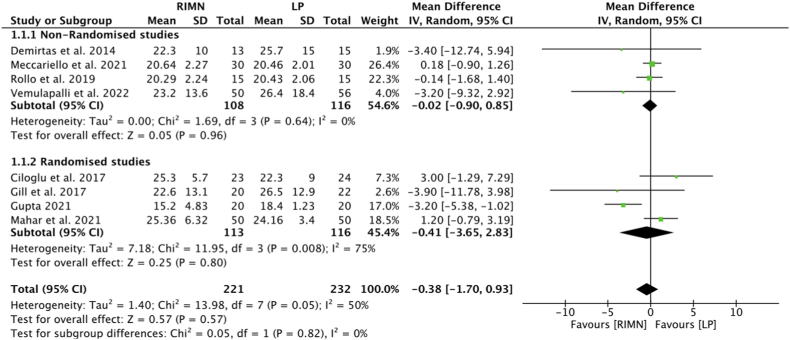
11/16 studies4,11,12,19,24, 25, 26, 27,29, 30, 31 reported mean fracture union time for two treatment groups individually. Overall the mean fracture union time ranged between 7.4 to 22 and 6.8–25.7 weeks for RIMN and LP groups respectively. However, only 8 studies, 4 non-RCTs11,26,30,31 and 4 RCTs12,25,27,29 were included in this analysis, as 3 studies4,19,24 have not reported the standard deviation. With a mean difference of −0.38 (95% CI -1.7, 0.93, p = 0.57; I2 = 50%), the meta-analysis did not find a difference in fracture union time between the two treatment groups. Similarly, no difference was observed between non-RCTs and RCTs with the effect of the estimate being −0.02 (95% CI -0.9, 0.85, I2 = 0%) and −0.41(95% CI-3.65, 2.83, I2 = 75%) respectively. The test for subgroup difference had p = 0.2 as shown in Fig. 5.
-
2.
Overall complications:
Fig. 5.
Forest plot comparing mean fracture union time.
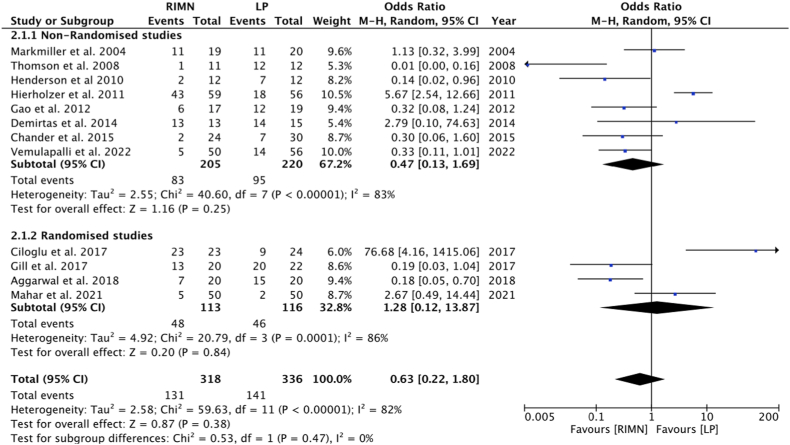
Complications were reported in 12/16 studies4,11,12,19, 20, 21, 22, 23, 24, 25,29,31 which included 8 non-RCTs11,19, 20, 21, 22, 23, 24,31 and 4 RCTs4,12,25,29 for the two treatment groups separately. The rates of overall complications were 42.9% and 44.9% for RIMN and LP groups respectively, which was higher for the LP group, with an odds ratio of 0.63 [95% CI 0.22, 1.80, p = 0.38; I2 = 82%], we did not find a statistically significant difference between the two. The effect of estimates for non-RCTs was 0.47 (95% CI 0.13,1.69, I2 = 83%), and for RCTs, it was 1.28 (95% CI 0.12,13.87, I2 = 86%). The test for subgroup difference had a value of p = 0.47, shown in Fig. 6.
Fig. 6.
Forest plot comparing overall complications.
We further analyzed some specific complications between the two treatment groups as well:
-
2.1.
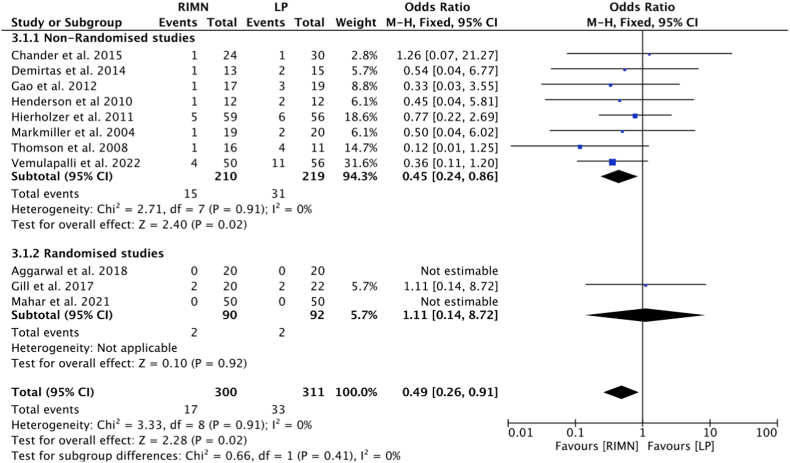
Nonunion: Comparative non-union rates were reported by 11/15 studies, with 8 non-RCTs11,19, 20, 21, 22, 23, 24,31 and 3 RCTs.4,12,29 The incidence was 5.8% and 10.7% for RIMN and LP groups respectively, with less events in RIMN group; analysis demonstrated a significantly lower nonunion rate in RIMN group with an odds ratio of 0.49 (95% CI 0.26, 0.91, p = 0.02; I2 = 0%). The effect of estimates for non-RCTs was 0.45 (95% CI 0.24, 0.86, I2 = 0%), which favored RIMN while for RCTs effect of the estimate was 1.11(95% CI 0.14, 8.72, I2 = 0%) with no statistical significance (the test for subgroup difference p = 0.41) shown in Fig. 7.
-
2.2.
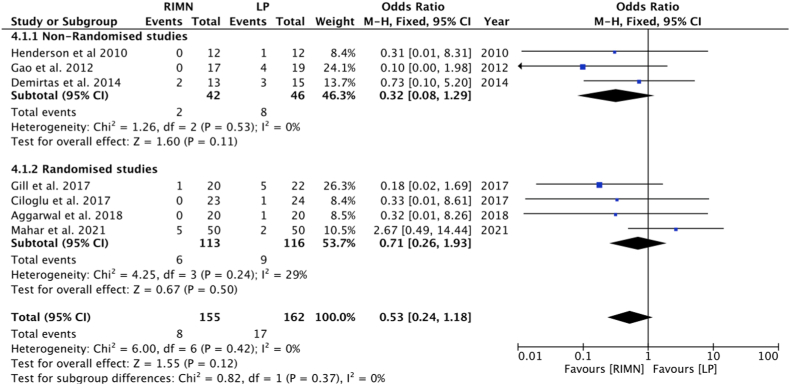
Delayed union: The delayed union was reported in 7/16 studies, 3 non-RCTs11,21,23 and 4 RCTs4,12,25,29 for two treatment groups individually. The incidence was 5.2% and 9.9% in RIMN and LP groups respectively. With an odds ratio of 0.53 (95% CI 0.24, 1.18, p = 0.42; I2 = 0%), we did not find a statistically significant difference between the two treatment groups. Similarly, there was no statistical difference between non-RCTs and RCTs with the effect of estimates of 0.32 (95% CI 0.08,1.29, I2 = 0%) and 0.71 (95% CI 0.26,1.93; I2 = 29%) (the test for subgroup difference p = 0.82) show in Fig. 8.
-
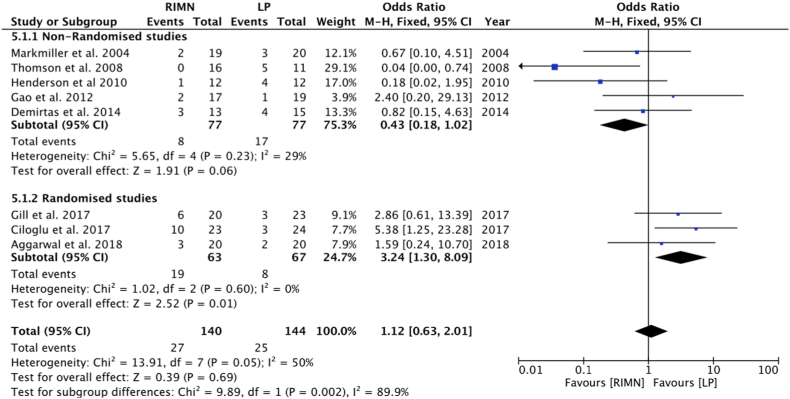
2.3.
Malunion: malunion was reported in 8/16 studies including 5 non-RCTs11,19, 20, 21,23 and 3 RCTs.6,12,25 The incidence was 19.4% and 17.1% in RIMN and LP groups respectively. A meta-analysis demonstrated a statistically non-significant difference between the two groups of treatments with an odds ratio of 1.12 (95% CI 0.63, 2.01, p = 0.69; I2 = 50%). There was no significant difference between the two treatment groups among the non-RCTs, with an effect of estimates of 0.43 (95% CI 0.18,1.02; I2 = 29%). However, in RCTs, there was lesser malunion among the RIMN group, with an effect of the estimate of 3.24 (95% CI 1.3, 8.09; I2 = 0%). The test for subgroup difference showed p = 0.002, as shown in Fig. 9.
-
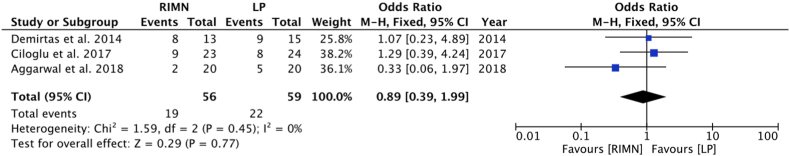
2.4.
Knee stiffness: Knee stiffness was reported by 3/16 studies4,11,12 for individual treatment groups. The incidence of stiffness was 33.9% and 28.8% in the 2 groups with no statistically significant difference and an odds ratio of 0.89 (95% CI 0.39, 1.99, p = 0.77; I2 = 0%) as shown in Fig. 10.
-
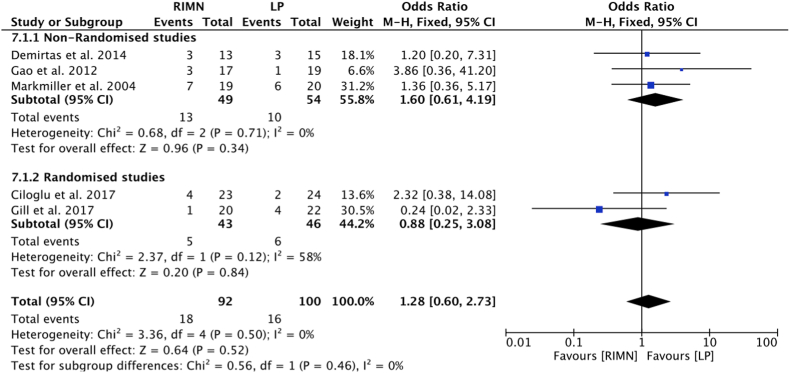
2.5.
Knee pain: Knee pain was reported in 5/16 studies, 3 non-RCTs11,19,23 and 2 RCTs12,25 for individual groups of treatment. The incidence of knee pain was 15.9% and 10.9% in RIMN and LP groups respectively. We did not find a statistically significant difference between the two groups of treatment with an odds ratio of 1.28 (95% CI 0.60, 2.73, p = 0.52; I2 = 0%). The effect of estimates for non-RCTs was 1.60 (95% CI 0.61,4.19; I2 = 0%) and for RCTs, it was 0.88 (95% CI 0.25, 3.08; I2 58%). The test for subgroup differences had a p-value of 0.46, as shown in Fig. 11.
-
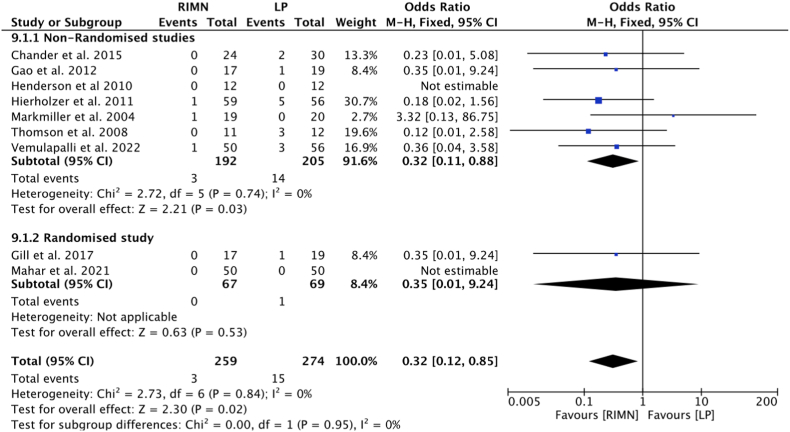
2.6.
Infection: Either superficial or deep infection was reported by 9/16 studies, 7 non-RCTs19, 20, 21, 22, 23, 24,31 and 2 RCTs,12,29 for the two treatment groups separately. The incidence of infection was 2.0% and 6.1% in RIMN and LP groups. A meta-analysis demonstrated a significantly lower rate of infection following RIMN compared to plating with an odds ratio of 0.32 (95% CI 0.12, 0.85; p = 0.02, I2 = 0%). The effect of estimate for non-RCTs 0.32 (95% CI 0.11, 0.88; I2 = 0%) favored the RIMN groups and for RCTs 0.32 (95% CI 0.01, 9.24) with no effect. The test for subgroup differences has a p-value of 0.95 shown in Fig. 12.
-
3.
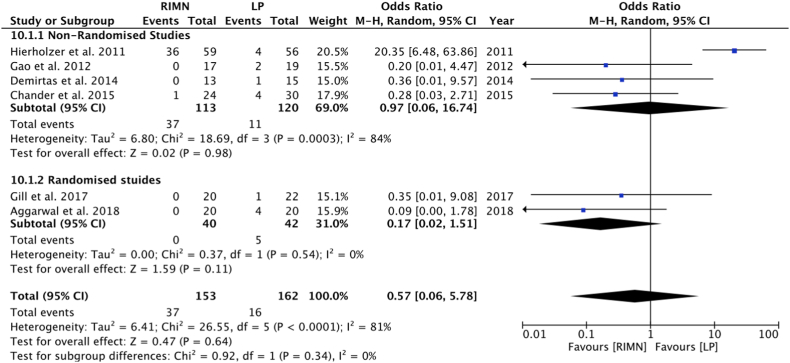
Implant-related complications: Implant-related complications were reported in 6/16 studies 4 non-RCTs11,22, 23, 24 and 2 RCTs4,12 individually for RIMN and LP groups. The incidence of implant-related complications was 26.8% in RIMN and 7.4% in LP fixation for the distal femur fractures. A meta-analysis demonstrated a statistically non-significant difference between the two treatment groups with an odds ratio of 0.57 (95% CI 0.06, 5.78 p < 0.0001; I2 = 81%). Similarly, no difference was found in subgroup analysis with the effect of estimates of 0.97 for non-RCTs (95% CI 0.06, 16.74; I2 = 84%) and 0.17 for RCTs (95% CI 0.02, 1.51; I2 = 0%). The test for subgroup difference had a p-value of 0.34, as shown in Fig. 13.
-
4.
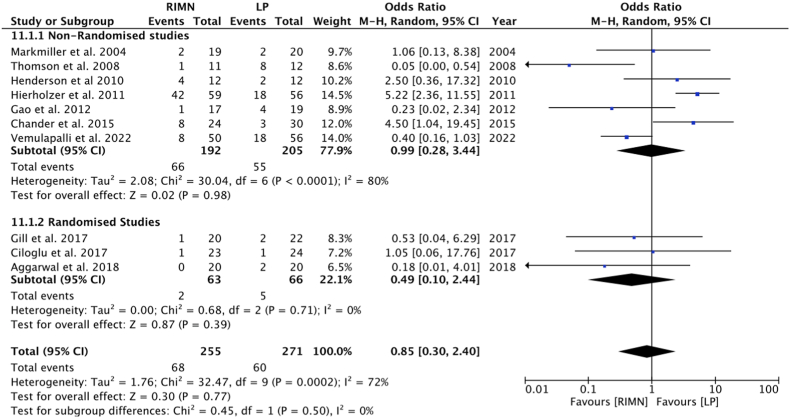
Re-operation rate: Re-operation due to implant related or any other postoperative complications were reported in 10/16 studies for two treatment groups separately with 7 non-RCTs19, 20, 21, 22, 23, 24,31 and 3 RCTs.4,12,25 The re-operation rate was 26.6% and 22.5% in RIMN and LP treatment groups respectively. The meta-analysis did not show a statistically significant difference between the two groups with an odds ratio of 0.85 (95% CI 0.30, 2.40, p = 0.77; I2 = 72%), and for subgroup analysis, the effect of estimate for non-RCTs was 0.99 (95% CI 0.28, 3.44; I2 80%) and for RCTs, it was 0.49 (95% CI 0.1, 2.44; I2 = 0%). The test for subgroup difference had a P value of 0.50, as shown in Fig. 14.
Fig. 7.
Forest plot comparing nonunion.
Fig. 8.
Forest plot comparing delayed union.
Fig. 9.
Forest plot comparing malunion.
Fig. 10.
Forest plot comparing knee stiffness.
Fig. 11.
Forest plot comparing knee pain.
Fig. 12.
Forest plot comparing infection.
Fig. 13.
Forest plot comparing implant-related complication.
Fig. 14.
Forest plot comparing the re-operation rate.
11.5. Secondary outcomes
-
1.
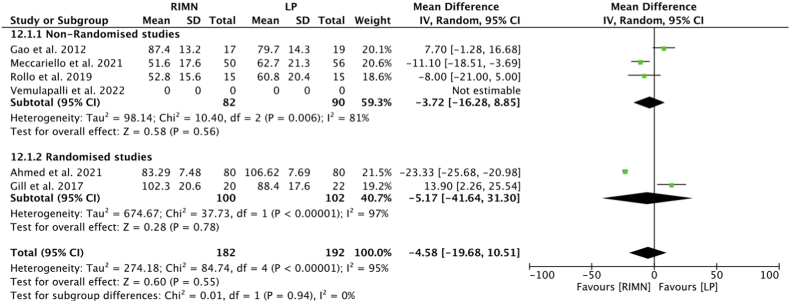
Duration of surgery: 6/16 studies 3 non-RCTs23,26,31 and 3 RCTs4,12,28 studies reported the duration of surgery for individual groups. The mean duration of surgery for RIMN was 51.6–105 min and that for the LP group was 60.8–110 min, which was more for LP group than RIMN group. For statistical analysis, we included only 5 studies and one study did not report the standard deviation. No statistically significant difference was found between the two groups with a mean difference of −4.58 (95% CI -19.68,10.51, p = 0.55; I2 = 95%). The effect of the estimate for non-RCTs was −3.72 (95% CI -16.28, 8.85, I2 81%) and for RCTs was −5.17 (95% CI -41.64, 31.3; I2 = 97%). The test for subgroup difference had a p-value of 0.94 shown in Fig. 15.
-
2.
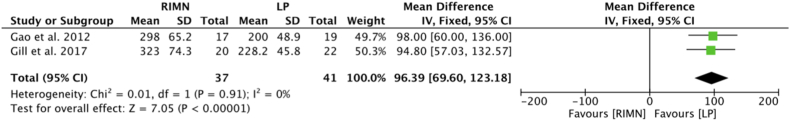
Intra-operative blood loss: Intra-operative blood loss was reported in only 2/16 included studies12,23 for individual groups. Mean blood loss was 323.0-248.13 ml and 200–434.38 ml for RIMN and LP respectively. A statistically significant difference was found between the two treatment groups with a mean difference of 96.39 (95% CI 69.6,123.18, p < 0.00001; I2 = 0%) which favors LP group with a lesser amount of blood loss compared to the RIMN group shown in Fig. 16.
-
3.
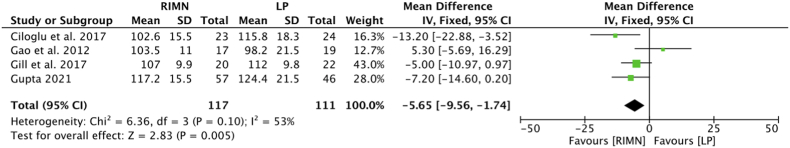
Knee Range of motion: The knee range of motion was reported in 8/16 studies4,12,19, 20, 21,23,25,27 individually for two groups however, the mean with a standard difference was given only for 4 studies13,24,26,28 which were statistically analyzed. Statistically, a significant difference was found between the two treatment groups, which favored the LP group with a mean difference of −5.65 (95% CI -9.56, −1.74, p = 0.005; I2 = 53%) Fig. 17.
Fig. 15.
Forest plot comparing the duration of surgery.
Fig. 16.
Forest plot comparing intra-operative blood loss.
Fig. 17.
Forest plot comparing knee range of motion.
12. Discussion
The RIMN has the advantage of less soft tissue and vascular disruption as compared to LP; these nails are also considered biomechanically superior, being closer to the femoral mechanical axis and acting as load-sharing devices.8,9 But, how much of the theoretical advantages work clinically was the study question we strived to answer in the present review.
With the above-mentioned features, theoretically, nailing should be associated with better wound healing, fewer infections, faster surgeries, and lesser blood loss in comparison to plating, which requires open reduction with surgical dissection of the soft tissues and impact on vascularity. However, when we compared these variables in the present review, the results were different. There was no difference between the two surgeries in terms of surgical duration; however, these results may have been skewed as certain nailing cases would have needed open reduction when intraoperative attempts for closed/indirect reduction went unsuccessful. The intra-operative blood loss was significantly lesser in LP group compared to RIMN fixation; this may be attributed to the sequential intramedullary reaming to insert a snugly fitting nail, leading to more amount of bleeding. However, this finding needs to be taken with caution as there were only 2 studies that could be meta-analyzed for this outcome.
The overall rates of complications were also not different between the 2 groups; however, looking at the specific complication of superficial/deep infection, rates were significantly higher in the plating group. Implant-related complications, malunions, and re-operation rates were also similar in both groups; however, subgroup analysis of the RCTs showed lesser malunions in the LP group. This could have been because of the better quality of reduction in these cases owing to the opening of the fracture site and directly reducing it, than indirect methods in the nailing group.
Another important variable that did favor nailing over plating in distal femur fractures was non-unions which were more in plating cases. The postoperative range of motion was better in the locked plate group. The latter could have been because of the initiation of ROM exercises early in such cases for better healing and lesser stiffness. Also, retrograde nails need to get access through the knee joint, which may cause issues with subsequent articular mobility.
Overall, both the implant choices have shown good outcomes, but the choice in specific case scenarios also depends on certain patient-related factors; pre-injury knee ROM status is an important consideration with certain degrees of flexion essentially needed for RIMN. Also, if an intra-articular extension of the distal femoral fracture is present, nailing becomes technically difficult, and direct reduction of the intra-articular fragments by opening the fracture site is essential. In such scenarios, plating becomes a better option. On the other hand, if there is an associated neck femur fracture with the distal femur fracture, RIMN with DHS/CCS for the proximal femur is a viable option.32 Also, when there is an ipsilateral shaft of tibia fracture co-existing, the same entry point can be used to nail both fractures.33
The strength of the current study is the fact that we have analyzed a large number of studies as compared to previous reviews. But there are also certain limitations like inclusion of both prospective and retrospective studies; out of 16 studies, only 6 are RCTs, while the remaining 9 are observational studies. In addition to this most of the included studies have less number of patients. However, the total number of studies and number of patients analyzed is much more than any previous work, and we have also done a sub-group analysis of the variables based on the type of studies.
There is still a need for more prospective randomized control trials with a larger number of patients for robust evidence and further substantiate the findings of this review.
13. Conclusion
The present review shows a significantly lesser nonunion, and infection, in the RIMN group for distal femur fractures. However, we did not find a significant difference in the two treatment groups in terms of fracture union time, overall complications, reoperation rates, and duration of surgery. But a better postoperative knee range of motion was seen in the LP group. Both the options of fixation appear to be feasible options, and specific indications should be considered for making the final choice.
Ethical approval
Not Applicable
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Availability of data and materials
No repositories were used for data.
Informed consent
Does not need for as this is a review article.
Institutional ethical committee approval
Does not need for as this is a review article.
Funding statement
We did not receive any kind of funding from any source.
Authors statement
Rajesh Kumar Rajnish and Amit Srivastava: conceptualization and designing of the study, Prasoon Kumar, Rehan Ul Haq, and Kuldeep Rathor: acquisition of data, or analysis of data and its interpretation, Sameer Aggarwal and Rajesh Kumar Rajnish: drafting and critically revising the article, and Sameer Aggarwal: approval of the final version of the manuscript to be submitted.
Declaration of competing interest
The authors declare no competing interests.
Acknowledgment
None.
Contributor Information
Sameer Aggarwal, Email: drsameer35@yahoo.co.in.
Rajesh Kumar Rajnish, Email: duktiraj@gmail.com.
Prasoon Kumar, Email: drprasoonksingh@gmail.com.
Amit Srivastava, Email: amitsrvstv00@gmail.com.
Kuldeep Rathor, Email: kuldeeprathor21@gmail.com.
Rehan Ul Haq, Email: docrehan1975@gmail.com.
References
- 1.Court-Brown C.M., Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 2.Gwathmey F.W., Jr., Jones-Quaidoo S.M., Kahler D., Hurwitz S., Cui Q. Distal femoral fractures: current concepts. J Am Acad Orthop Surg. 2010;18(10):597–607. doi: 10.5435/00124635-201010000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Zlowodzki M., Bhandari M., Marek D.J., Cole P.A., Kregor P.J. Operative treatment of acute distal femur fractures: systematic review of two comparative studies and 45 case series (1989-2005) J Orthop Trauma. 2006;20:366–371. doi: 10.1097/00005131-200605000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Walcher F., Frank J., Marzi I. Retrogradenailing of distal femoral fracture–clear andpotential indications. Eur J Trauma. 2000;26(4):155–168. [Google Scholar]
- 5.Wenger D., Andersson S. Low risk of nonunion with lateral locked plating of distal femoral fractures-A retrospective study of 191 consecutive patients. Injury. 2019;50(2):448–452. doi: 10.1016/j.injury.2018.10.039. [DOI] [PubMed] [Google Scholar]
- 6.Agarwal S., Udapudi S., Gupta S. To assess functional outcome for intra-articular and extra-articular distal femur fracture in patients using retrograde nailing or locked compression plating. J Clin Diagn Res. 2018;12(3):RC21RC24. [Google Scholar]
- 7.Green S.A. Distal intramedullary fixation of supracondylar fractures of the femur. Tech Orthop. 1988;3:71–76. [Google Scholar]
- 8.Smith W.R., Ziran B.H., Anglen J.O., Stahel P.F. Locking plates: tips and tricks. J Bone Joint Surg Am. 2007;89(10):2298–2307. doi: 10.2106/00004623-200710000-00028. [DOI] [PubMed] [Google Scholar]
- 9.Ricci W.M., Loftus T., Cox C., Borrelli J. Locked plates combined with minimally invasive insertion technique for the treatment of periprosthetic supracondylar femur fractures above a total knee arthroplasty. J Orthop Trauma. 2006;20(3):190–196. doi: 10.1097/00005131-200603000-00005. [DOI] [PubMed] [Google Scholar]
- 10.El-Kawy S., Ansara S., Moftah A., et al. Retrograde femoral nailing in elderly patients with supracondylar fracture femur; is it the answer for a clinical problem? Int Orthop. 2007;31(1):83. doi: 10.1007/s00264-006-0137-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Demirtş A., Azboy I., Özkul E., Gem M., Alemdar C. Comparison of retrograde intramedullary nailing and bridge plating in the treatment of extra-articular fractures of the distal femur. Acta Orthop Traumatol Turcica. 2014;48(5):521–526. doi: 10.3944/AOTT.2014.14.0004. [DOI] [PubMed] [Google Scholar]
- 12.Gill S Mittal A., Raj M., Singh P., Singh J., Kumar S. Extra articular supracondylar femur fractures managed with locked distal femoral plate or supracondylar nailing: a comparative outcome study. J Clin Diagn Res. 2017;11(5):RC19–RC23. doi: 10.7860/JCDR/2017/25062.9936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WangA ZongS., SuL LiangW., CaoX ZhengQ., et al. Meta-analysis of postoperative complications in distal femoral fractures: retrograde intramedullary nailing versus plating. Int J Clin Exp Med. 2016;10:18900–18911. [Google Scholar]
- 14.Neradi D., Sodavarapu P., Jindal K., Kumar D., Kumar V., Goni V. Locked plating versus retrograde intramedullary nailing for distal femur fractures: a systematic review and meta-analysis. The Archives of Bone and Joint Surgery. 2022;10(2):141–152. doi: 10.22038/abjs.2021.53515.2656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Review Manager (RevMan) [Computer program]. Version 5.4.1, The Cochrane Collaboration, 2020.
- 17.Slim K., Nini E., Forestier D., Kwiatkowski F., Panis Y., Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 18.Higgins J.P.T., Altman D.G., Gotzsche P.C., et al. Cochrane bias methods group Cochrane statistical methods group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Markmiller M., Konrad G., Südkamp N. Femur-LISS and distal femoral nail for fixation of distal femoral fractures: are there differences in outcome and complications? Clin Orthop Relat Res. 2004;426:252–257. doi: 10.1097/01.blo.0000141935.86481.ba. [DOI] [PubMed] [Google Scholar]
- 20.Thomson A.B., Driver R., Kregor P.J., Obremskey W.T. Long-term functional outcomes after intra-articular distal femur fractures: ORIF versus retrograde intramedullary nailing. Orthopedics. 2008;31(8):748–750. doi: 10.3928/01477447-20080801-33. [DOI] [PubMed] [Google Scholar]
- 21.Henderson C.E., Lujan T., Bottlang M., Fitzpatrick D.C., Madey S.M., Marsh J.L. Stabilization of distal femur fractures with intramedullary nails and locking plates: differences in callus formation. Iowa Orthop J. 2010;30:61–68. [PMC free article] [PubMed] [Google Scholar]
- 22.Hierholzer C., Cv Rüden, P tzel T., Woltmann A., Bühren V. Outcome analysis of retrograde nailing and less invasive stabilization system in distal femoral fractures: a retrospective analysis. Indian J Orthop. 2011;45:243–250. doi: 10.4103/0019-5413.80043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gao K., Gao W., Huang J., et al. Retrograde nailing versus locked plating of extra-articular distal femoral fractures: comparison of 36 cases. Med Princ Pract. 2013;22(2):161–166. doi: 10.1159/000342664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chander A., Ganesan G.R., Jayabalan V. Is distal femur locking plate a superior implant in distal femur fracture? Open J Orthoped. 2015;5:258–263. [Google Scholar]
- 25.Çiloglu O., Dursun M., Kalkan T., Çıçek H., Seyfettinoglu F., Ogur H. Comparison of retrograde intramedullary nailing and percutaneous plate osteosynthesis methods in distal femur fractures. Cukurova Med J. 2017;42(3):490–498. [Google Scholar]
- 26.Rollo G., Bisaccia M., Rinonapoli G., et al. Radiographic, bone densitometry and clinic outcomes assessments in femoral shaft fractures fixed by plating or locking retrograde nail. Med Arch. 2019;73(3):195–200. doi: 10.5455/medarh.2019.73.195-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gupta M.K., Bhargava R., Garg S. Comparative study between distal femoral locking plate and retrograde femoral nail in surgical management of supracondylar fracture of femur. Int J Sci Stud. 2021;8(12):60–63. [Google Scholar]
- 28.Ahmed U., Ahmad U., Zaheer M., Sadaqat A., Khalid Z. Comparison of outcome with retrograde nailing versus locked compressive plating in the treatment of extra articular supracondylar femur fractures. Pak J Med Health Sci. 2021;15(12):3410–3412. [Google Scholar]
- 29.Mahar S.A., Aziz S., Ahmed S., Kumar J., Ali S. Outcome of extra-articular fractures of distal femur: less invasive stabilization on system (LISS) plating versus closed retrograde intramedullary interlocking nail Pakistan. J Med Health Sci. 2021;15(5):1144–1147. [Google Scholar]
- 30.Meccariello L., Bisaccia M., Ronga M., et al. Locking retrograde nail, non-locking retrograde nail and plate fixation in the treatment of distal third femoral shaft fractures: radiographic, bone densitometry and clinical outcomes. J Orthop Traumatol. 2021;22(1):33. doi: 10.1186/s10195-021-00593-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chandra Vemulapalli K., Pechero G.R., Warner S.J., et al. Is retrograde nailing superior to lateral locked plating for complete articular distal femur fractures? Injury. 2022;53(2):640–644. doi: 10.1016/j.injury.2021.11.037. [DOI] [PubMed] [Google Scholar]
- 32.Ostrum R.F., Tornetta P., 3rd, Watson J.T., Christiano A., Vafek E. Ipsilateral proximal femur and shaft fractures treated with hip screws and a reamed retrograde intramedullary nail. Clin Orthop Relat Res. 2014 Sep;472(9):2751–2758. doi: 10.1007/s11999-013-3271-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vallier H.A., Manzano G.W. Management of the floating knee: ipsilateral fractures of the femur and tibia. J Am Acad Orthop Surg. 2020;28(2):e47–e54. doi: 10.5435/JAAOS-D-18-00740. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No repositories were used for data.