Abstract
Homologous recombination DNA-repair deficiency (HRD) is a common driver of genomic instability and confers a therapeutic vulnerability in cancer. The accurate detection of somatic allelic imbalances (AIs) has been limited by methods focused on BRCA1/2 mutations and using mixtures of cancer types. Using pan-cancer data, we revealed distinct patterns of AIs in high-grade serous ovarian cancer (HGSC). We used machine learning and statistics to generate improved criteria to identify HRD in HGSC (ovaHRDscar). ovaHRDscar significantly predicted clinical outcomes in three independent patient cohorts with higher precision than previous methods. Characterization of 98 spatiotemporally distinct metastatic samples revealed low intra-patient variation and indicated the primary tumor as the preferred site for clinical sampling in HGSC. Further, our approach improved the prediction of clinical outcomes in triple-negative breast cancer (tnbcHRDscar), validated in two independent patient cohorts. In conclusion, our tumor-specific, systematic approach has the potential to improve patient selection for HR-targeted therapies.
Subject terms: Ovarian cancer, Tumour biomarkers, Breast cancer
Introduction
As a part of the Fanconi Anemia (FA) pathway, homologous recombination (HR) is an evolutionarily conserved, tightly regulated mechanism for high-fidelity repair of DNA double-strand breaks (DSBs)1. Deficiency in homologous recombination (HRD) has profound consequences for replicating cells driving genomic instability and oncogenic transformation. In cancer, HRD results in a fundamental vulnerability, and tumors with HRD are markedly sensitive to DSB-inducing agents such as platinum-based chemotherapy and Poly-ADP Ribose Polymerase (PARP) inhibitors2.
High-grade serous ovarian cancer (HGSC), the most common and most lethal subtype of ovarian cancers3, is characterized by profound genomic instability. Around half of the HGSC cases harbor genomic alterations leading to HRD4, and these patients have been shown to benefit from treatment with PARP inhibitors5,6. The HRD test previously used in PARP inhibitor clinical trials (MyriadMyChoise®CDx)5,6 works by quantifying specific allelic imbalances (AIs): (1) Large scale transitions (LSTs)7, (2) Loss of heterozygosity (LOH)8 and (3) Telomeric allelic imbalances (TAIs)9. However, the decision criteria for these HRD-specific AIs (HRD-AIs) and the HRD status classification were originally designed using a mixture of breast and ovarian cancer samples7–10. Further, other algorithms for HRD detection have primarily focused on BRCA1/2 mutation prediction11,12. As the genomic drivers and mutational processes differ across the cancer types, the details of the genomic instability occurring due to HRD in HGSC remain unclear.
Herein, via pan-cancer analysis, we show that HGSC harbors unique patterns of AIs, which are also distinct from triple-negative breast cancers (TNBC). Using a systematic approach based on machine learning and statistics on The Cancer Genome Atlas ovarian cancer (OVA-TCGA) multi-omics dataset, we optimized the criteria for HRD-AIs on HGSC. We implemented these criteria as an open-source algorithm (ovaHRDscar) to reliably define HRD status beyond the prediction of BRCA1/2 mutations. We show that ovaHRDscar improves the prediction of clinical outcomes in three independent clinical datasets compared to previous algorithms. Further, we show that our approach improves the prediction of clinical outcomes also in TNBC (tnbcHRDscar). Thus, our machine learning-aided disease-specific approach (HRDscar) shows promise as a biomarker that can improve outcome prediction and patient selection for HR-targeted therapies in cancer.
Results
Systematic pan-cancer characterization reveals unique features of allelic imbalances in HGSC
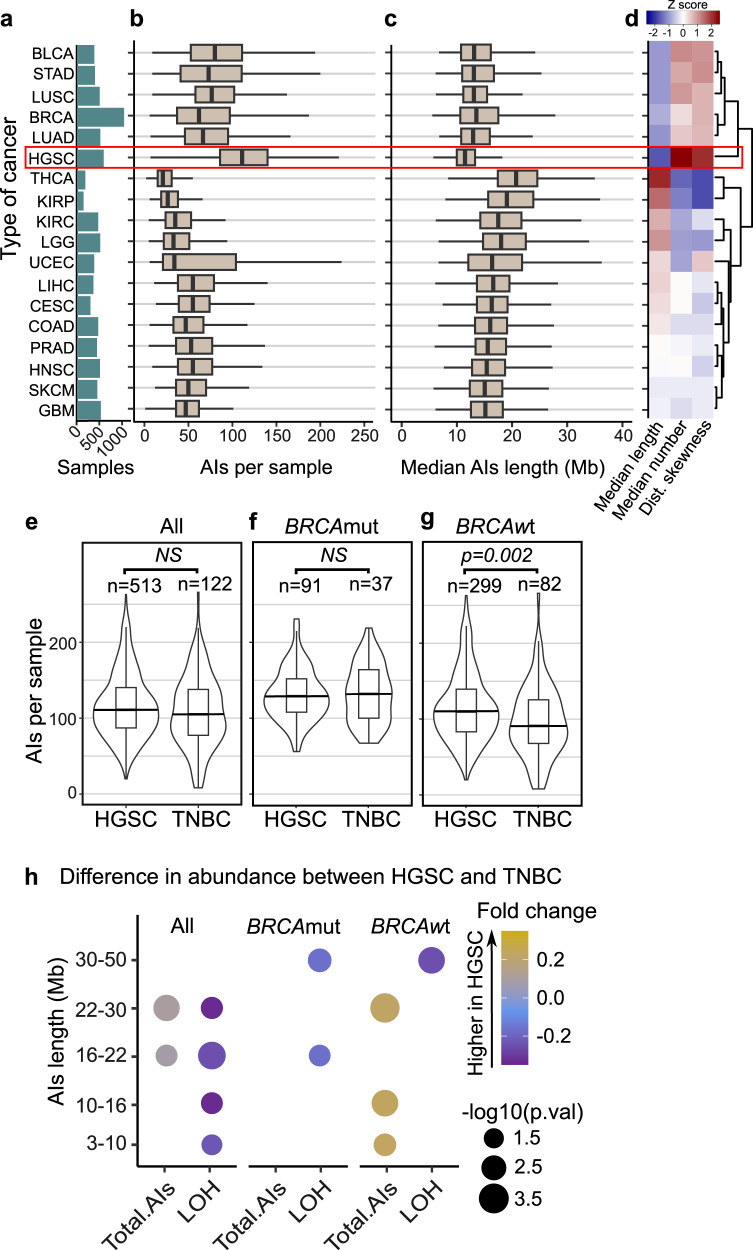
To elucidate the potential differences in the patterns of AIs across human cancers, we first characterized the quantity and the length distributions of AIs in the 18 most common cancer types from the TCGA (Fig. 1a). Interestingly, HGSC had the highest number of AIs (Fig. 1b) and the lowest median length (Fig. 1c). Concordantly, HGSC showed the highest levels of LOH events (Supplementary Fig. 1a) with one of the lowest median length (Supplementary Fig. 1b).
Fig. 1. Pan-cancer characterization of AIs reveals unique patterns in HGSC.
a Types of cancer with more than 200 samples in TCGA and their corresponding number of samples are shown in green bars; bladder urothelial carcinoma (BLCA), stomach adenocarcinoma (STAD), lung squamous cell carcinoma (LUSC), breast invasive carcinoma (BRCA), thyroid carcinoma (THCA), kidney renal papillary cell carcinoma (KIRP), kidney renal clear cell carcinoma (KIRC), brain Lower Grade Glioma (LGG), uterine Corpus endometrial carcinoma (UCEC), liver hepatocellular carcinoma (LIHC), cervical squamous cell carcinoma and endocervical adenocarcinoma (CESC), colon adenocarcinoma (COAD), prostate adenocarcinoma (PRAD), head and neck squamous cell carcinoma (HNSC), skin cutaneous melanoma (SKCM), glioblastoma multiforme (GBM). b Box plots representing the number of AIs longer than 3 Mb and smaller than 50 Mb per sample. HGSC showed the highest average levels of AIs. c Box plots showing the median length of AIs (longer than 3 Mb and smaller than 50 Mb) per sample. HGSC showed the lowest median length of AIs per sample. The black vertical lines represent the sample medians, the boxes extend from first to third quartile and whiskers indicate the values at 1.5 times the interquartile range, no outliers are shown. d Hierarchical clustering for the types of cancer using as variables the median length, the median number of AIs per sample, and the skewness of the distribution of AIs length. e Violin- and box plots (same notation as panels b,c) representing the number of AIs per sample. HGSC shows a similar number of AIs as compared to TNBC (two-sided U test). f Comparison of BRCAmut samples showing similar abundances of AIs in HGSC as compared to TNBC (two-sided U test). g The BRCAwt samples showing significantly higher number of AIs in HGSC than in TNBC (two-sided U test, p = 0.002). h Dot plot showing the difference in abundance for AIs of specific length between HGSC and TNBC. The dot sizes represent the p-values (two-sided U test) and dot colors represent the fold-change (ratio of HGSC/TNBC abundance of AIs minus one), only dots for corresponding significant differences are shown (p < 0.05).
We next performed hierarchical clustering using the median length and number of AIs per sample and the skewness of the length distribution of the AIs for each cancer type. This analysis shows two main clusters: the first cluster consisting of six cancer types (bladder urothelial carcinoma (BLCA), stomach adenocarcinoma (STAD), lung squamous cell carcinoma (LUSC), lung adenocarcinoma (LUAD), breast invasive carcinoma (BRCA), and HGSC) with a higher amount but a lower median length of AIs (upper cluster: Fig. 1d). The second cluster consisting of the remaining 12 cancer types (lower cluster: Fig. 1d). The same main clusters were observed when using only LOH events (Supplementary Figure 1c).
As TNBC and HGSC are enriched in BRCA1/2 genetic mutations (BRCAmut)13, both cancers were used to define the HRD-algorithm in the MyriadMyChoise®CDx assay by Telli et al.10. We next compared the differences in AIs between these two cancer types. We observed a significant difference in the abundance of AIs between HGSC and TNBC, specifically among the BRCA1/2-wild-type (BRCAwt) tumors (U test, p = 0.002, Fig. 1e–g). Interestingly, HGSC had lower levels of LOH events than TNBC (U test, p = 0.002, Supplementary Fig. 1d), also among the BRCAmut samples (U test, p = 0.049, Supplementary Fig. 1e) but not in the BRCAwt samples (Supplementary Fig. 1f). Overall, HGSC showed a higher number of AIs of different lengths, while TNBC had a higher number of LOH events (Fig. 1h). These results highlight the distinct characteristics of AI events in HGSC, especially among the BRCAwt tumors, compared to other cancer types.
Machine learning-aided detection of HRD-specific AIs improves the detection of HRD in HGSC
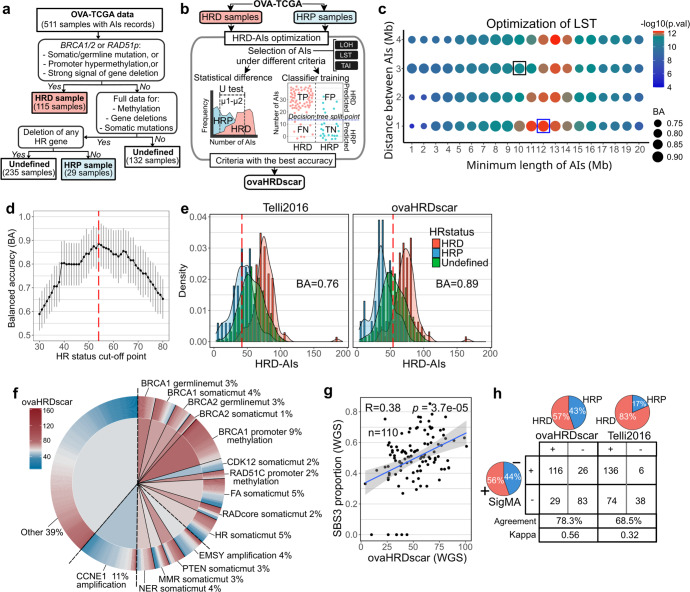
Although a wide range of molecular alterations is known to cause HRD, previous studies have focused on BRCA1/2 mutations to detect HRD-specific AIs (HRD-AIs), potentially failing to detect non-BRCA associated HRD alterations while losing specificity to classify the HR-proficient (HRP) samples accurately. To this end, we aimed to identify AIs overrepresented in samples carrying a wider range of genetic alterations (mutations, gene deletions, promoter hypermethylation) associated with HRD in HGSC (Fig. 2a). To generate accurate selection criteria for HRD-AIs, we utilized SNP-arrays data from HGSC samples from TCGA (OVA-TCGA) and its associated genomic and DNA methylation data. Using prior knowledge and multi-omics data, we annotated 115 HRD samples harboring a somatic or germline mutation, gene deletion, or promoter hypermethylation in the BRCA1/2 or RAD51 paralog genes, and 29 HRP samples that did not harbor any of the alterations used to select the HRD samples, nor deletions in any other HR-related gene (Fig. 2a). A detailed description of the genomic alterations in the samples is reported in Supplementary Table 1. Overall, the HRD samples had a higher number of all AIs than the HRP samples (U test, p = 0.0028, Supplementary Fig. 2a). Importantly, HRD samples had a notably higher proportion of AIs of a specific length that spanned from 1 Mb to 30 Mbs. In contrast, the HRP samples contained a higher proportion of AIs and LOH events smaller than 1 Mb (Supplementary Fig. 2b, c).
Fig. 2. Machine learning-aided detection of AIs associated with HRD shows improved accuracy and correlations with genomic features of HRD in HGSC.
a Selection criteria for annotating HRD, HRP and undefined HGSC samples in the OVA-TCGA. b A scheme of the approach used to generate accurate criteria for selecting HRD-AIs in HGSC samples. c For LST events, the size of dots represents the decision tree balanced accuracy (BA) of classifying HRD and HRP when selecting AIs of the corresponding criteria, the dot colors represent the statistical difference (U test, p-value) in abundance of AIs between HRD and HRP samples. The black box corresponds to the selection criteria proposed by Telli2016, the blue box correspond to the best BA and U test value. d Evaluation of ovaHRDscar cut-off to define HR-status. The black dots connected with a line correspond to the balanced accuracy (BA) of the classification of the annotated HRD and HRP samples using the given cut-off value, the 95% confidence intervals are shown in gray vertical lines, value of 54 (red dashed line) corresponds to the highest BA. e Density distribution of HRD-AIs according to Telli2016 and ovaHRDscar algorithms. The red dashed line represents the cut-off established to define the HR-status using Telli2016 (≥42) and using ovaHRDscar (≥54). The BA of classification of the annotated HRD and HRP is shown, density distribution colors correspond to the samples annotated as in the panel a. f Levels of ovaHRDscar in OVA-TCGA samples harboring different genetic or epigenetic alterations associated with HRD in HGSC4. The colors correspond to the ovaHRDscar; in the outer ring of the pie chart every line represents a sample and in the center of the pie chart the colors correspond to the average number of HRD-AIs per genetic or epigenetic alteration. For the somatic mutations (somaticmut) gene deletions were included. g Linear regression of the proportion of single base substitution signature 3 (SBS3) and the ovaHRDscar levels in PCAWG samples (Pearson r’ = 0.38). Blue line shows the regression line and the 95% confidence intervals are shown in gray. h The SBS3 status inferred using SigMA16 showing a higher agreement with ovaHRDscar (agreement = 78.3%, Cohen’s kappa = 0.56) than with the Telli2016 algorithm (agreement = 68.5%, Cohen’s kappa = 0.32). In the pie charts and table+ and - correspond to the number of HRD positive and HRD negative samples identified under each criterion, respectively. On the bottom is shown the number of samples and the level of agreement between the corresponding criteria.
We next applied statistics and machine learning14 to identify the specific length and selection criteria of LOH, LST, and TAI events overrepresented in the HRD samples (Fig. 2b). We then compared the accuracies of the herein optimized criteria for HRD to those used in Telli et al.10 (hereafter called Telli2016). Notably, for LSTs, our approach increased the accuracy of classification of the HRD/HRP samples from 86 to 90% when using the new criteria (Fig. 2c). For LOH events, the accuracy increased from 85 to 88% when using the new criteria (Supplementary Fig. 2d). We also assessed the HRD-classification accuracy of LSTs consisting of three consecutive AIs. However, this produced a lower accuracy (Supplementary Fig. 2e). The largest improvement in accuracy occurred after including all TAIs larger than 1 Mb, and the accuracy for HRD-specific TAI events increased from 67 to 78% when compared to the Telli2016 criteria (Supplementary Fig. 2f).
Via our systematic approach, we observed the following AIs to be most characteristic of HRD in HGSC: (1) LOH > 15 Mb and <50 Mb, (2) for LSTs AI > 12 Mb, with a distance between them <1 Mb, and (3) TAI > 1 Mb. The sum of these events is hereafter called the ovaHRDscar levels. Then, using bootstrapping subsampling of the pre-annotated HRD and HRP samples, we evaluated the optimal cut-off value for ovaHRDscar to define the final HR-status as HRD or HRP. The value with the highest balanced accuracy (BA) was 54 (Fig. 2d), meaning that values higher or equal than 54 correspond to HRD, with higher accuracy for HR-status classification (BA = 0.89, right panel Fig. 2e) as compared to the Telli2016 algorithm (BA = 0.76, left panel Fig. 2e). In addition, using a HRD/HRP cut-off value of 54 in the Telli2016 algorithm (hereafter Telli2016-54), the BA remained below that of ovaHRDscar (0.86 vs 0.89, Supplementary Fig. 2g).
ovaHRDscar levels correlate with genomic features of HRD and show concordance in WGS data
To investigate the relationships of ovaHRDscar with other known genomic features associated with HRD, we annotated the OVA-TCGA samples according to mutations, gene deletions, and promoter hypermethylation patterns previously reported to be associated with HRD4 (Fig. 2f). On average, samples with somatic mutations in BRCA1, BRCA2, PTEN, or somatic mutations or gene deletions in any gene belonging to the Fanconi Anemia (FA) or HR pathways showed high ovaHRDscar levels. Likewise, samples that contained hypermethylation in the promoter regions of BRCA1 or RAD51C genes or germline mutations in BRCA1 or BRCA2 had, on average, high ovaHRDscar levels. As expected, samples harboring an amplification in CCNE1 (Supplementary Fig. 2h) had significantly lower levels of ovaHRDscar. However, samples with EMSY amplification and CDK12 somatic mutation did not result in higher ovaHRDscar levels than CCNE1 amplified samples (Supplementary Fig. 2h).
To assess the concordance of ovaHRDscar between SNP array and whole genome sequencing (WGS) data, we next quantified the ovaHRDscar levels in HGSC samples from the Pan-Cancer Analysis of Whole Genomes project (PCAWG)15. The ovaHRDscar levels were highly concordant between WGS and SNP-arrays (Lin’s concordance correlation coefficient, ccc = 0.90; Supplementary Fig. 2i) in 41 OVA-TCGA samples that were also included in the PCAWG project, consistent with a previous report in breast cancer samples16. Next, we tested the correlation of ovaHRDscar with the single base substitution signature 3 (SBS3), which has been associated with HRD17. We found that the ovaHRDscar levels detected in WGS positively correlated with the proportion of SBS3 in WGS (Pearson, r’ = 0.38, p = 3.7e−05; Fig. 2g). The SBS3 proportions also correlated with the number of HRD-AIs using the Telli2016 algorithm in the PCAWG cohort (Supplementary Fig. 2j). We next compared the performance of ovaHRDscar to that of SBS3 inferred from whole exome sequencing (WES) data with a likelihood-based approach SigMA18, in 254 samples from the OVA-TCGA. The ovaHRDscar algorithm detected 57% of samples as HRD, and the SigMA tool classified 56% of samples as SBS3+; in contrast, the Telli2016 algorithm identified 83% of the samples as HRD (Fig. 2h). HRD detection with ovaHRDscar showed a higher agreement with SigMA (agreement 78.3% and Cohen’s kappa = 0.56) as compared to the Telli2016 algorithm (agreement 68.5% and Cohen’s kappa = 0.32; Fig. 2h) or to the Telli2016-54 (agreement 77.2% and Cohen’s kappa = 0.53; Supplementary Fig. 2k).
ovaHRDscar improves the prediction of PFS and OS compared to previous algorithms
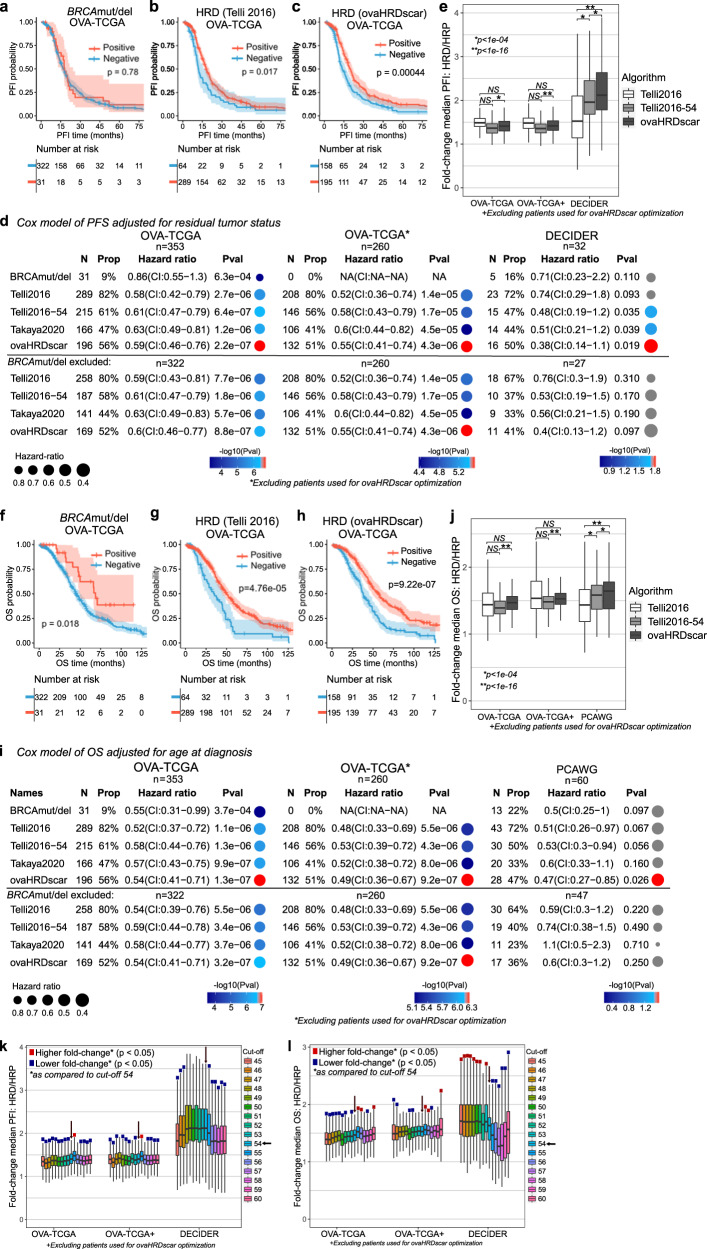
Next, we measured the association of HR-status classification by ovaHRDscar to progression-free survival (PFS, see methods) in advanced HGSC patients treated with platinum-based chemotherapy in the TCGA and an independent prospective validation dataset (DECIDER). We compared the performance of the ovaHRDscar to BRCA1/2 deficiency status to the Telli2016 algorithm. The Telli2016 algorithm uses a cut-off value of 63, as proposed by Takaya et al.19. As BRCA1/2 mutations can affect patient outcomes, we assessed the performances of ovaHRDscar in the TCGA dataset after excluding the samples used when defining ovaHRDscar, even though clinical outcomes were not utilized for designing the criteria of ovaHRDscar. BRCA1/2 mutation or deletion status (BRCAmut/del) was not significantly associated with PFS (Log-rank p = 0.72; Fig. 3a). For OVA-TCGA (Fig. 3a–c), we found that ovaHRDscar positivity was associated with prolonged PFS (Log-rank p = 4.4e−04; Fig. 3c). Consistently, ovaHRDscar positive patients had a longer PFS in the independent DECIDER validation cohort (Log-rank p = 0.001; Supplementary Fig. 3a–c), while the Telli2016 algorithm did not reach statistical significance in predicting PFS (Log-rank p = 0.11; Supplementary Fig. 3b).
Fig. 3. ovaHRDscar accurately predicts PFS and OS in HGSC patients.
a–c Kaplan–Meier plots of PFS in OVA-TCGA patients stratified with different criteria, in (a) patients were stratified according to the BRCAmut/del status with no significant difference in their PFS probability over time (Log-rank, p = 0.78); (b) patients were stratified according to the Telli2016 algorithm (Log-rank, p = 0.017); and (c) patients were stratified using the ovaHRDscar algorithm. HRD patients had a prolonged PFS as compared to the HRP (Log-rank, p = 4.4e−04). Blue and red shadow areas correspond to the 95% confidence intervals of probability. d Cox regression models for PFS adjusted for residual tumor after surgery according to the different HR classification criteria (BRCAmut/del, Telli2016, Telli2016-54, Takaya2020, ovaHRDscar). Three panels are shown: OVA-TCGA cohort in the left panel, OVA-TCGA cohort excluding the annotated HRD and HRP samples used for the detection of HRD-AIs in the middle panel, and the DECIDER prospective cohort (WGS) in the right panel. The number of patients (N) selected as HRD positive and their corresponding proportion (Prop), the hazard ratio for the Cox regression and the 95% confidence intervals (CI) and the p-value (Pval) of the regression are shown for each panel. The size of the dot represents the hazard ratio and color of the dot represents the p-value, gray dots represent non-statistical significant associations (p ≥ 0.05). e Fold-change of the difference in median PFS between HRD and HRP patients when stratified using ovaHRDscar, Telli2016 or Telli2016 using an HRD/HR cut-off value of 54 (Telli2016-54). Patients were bootstrapped 1000 times, and the median PFI fold-change was calculated for each iteration, the box plots represent the values obtained by each bootstrapping iteration. The black horizontal lines represent the sample medians, the boxes extend from first to third quartile and whiskers indicate the values at 1.5 times the interquartile range, no outliers are shown. The p-values were calculated using U test. f–h, Kaplan–Meier plots of OS for OVA-TCGA patients stratified using different criteria. i Cox regression models for OS according to the HR-status classification criteria. The PCAWG samples in the right panel, the left and center panels are the same as in (d). j Fold-change of the difference in median OS between HRD and HRP patients stratified using ovaHRDscar, Telli2016 or Telli2016-54 using the same approach as in (e). k–l Fold-changes of the difference in median PFS (k) & OS (l) between HRD and HRP patients stratified using different ovaHRDscar cut-off values. Patients were bootstrapped 1000 times and the resultant median fold-changes for each iteration are shown in box plots using the same approach as in (e). The statistical significance for the lower and higher fold-changes as compared to the cut-off of 54 were calculated independently using U test. The statistically significant differences show a colored square.
Residual tumor after primary debulking surgery has been shown to be a strong independent prognostic factor in HGSC20. We next used residual tumor status as a covariable in Cox proportional hazard models to assess the performance of HRD algorithms in predicting the PFS. We found that ovaHRDscar positivity was significantly associated with prolonged PFS in OVA-TCGA also when adjusting for residual tumor (Wald test p = 2.2e−07, Fig. 3d), similar to the Telli2016 (Wald test p = 2.7e−06), Telli2016-54 (Wald test p = 6.4e−07) and the Takaya algorithms (Wald test p = 1.2e−06). The same was true also after excluding the annotated HRD/HRP samples used in the optimization (middle panel, Fig. 3d) and when not adjusting for the residual tumor (Supplementary Fig. 3d). Importantly, ovaHRDscar significantly predicted PFS in the external DECIDER validation cohort (HR: 0.47 (CI:0.27-0.85), Wald test p = 0.026). To compare how well the three algorithms (ovaHRDscar, Telli2016, Telli2016-54) can predict the differential outcomes of patients, we next calculated the differences in PFS between the HRD and HRP using a bootstrapping approach. Consistently, we found that the difference in PFS was significantly greater using the ovaHRDscar than using the Telli2016 algorithm in the independent DECIDER validation cohort (Fig. 3e). Moreover, ovaHRDscar was superior to the Telli2016-54 algorithm in the OVA-TCGA (Fig. 3e). In further validation, we inspected the performance of the HRD-classification algorithms in an additional independent prospective cohort (TERVA) with tumor-only SNP array profiling (see methods). Importantly, ovaHRDscar positivity significantly predicted longer PFS using Log-rank test and Cox proportional hazard model in the TERVA external validation dataset (Supplementary Fig. 3e–g).
We next explored the association of ovaHRDscar with overall survival (OS) in HGSC patients in the OVA-TCGA cohort and in an independent AU-OVA cohort in PCAWG (Fig. 3f–h, Supplementary Fig. 3h–j). The clinical data in the prospective cohorts (DECIDER, TERVA) were not mature enough for OS evaluation. OvaHRDscar significantly predicted OS in the OVA-TCGA (Fig. 3h). In Cox regression analysis adjusted for age at diagnosis, ovaHRDscar significantly predicted OS, while the other algorithms did not reach statistical significance in the independent PCAWG validation dataset (Fig. 3i). These results were concordant also using a non-adjusted Cox regression analysis (Supplementary Fig. 3k). Importantly, the median OS in patients with HRD tumors as compared to HRP was significantly longer when using the ovaHRDscar than using the Telli2016 or the Telli2016-54 algorithms in the independent PCAWG cohort when using a bootstrapping approach (Fig. 3j). Additionally, we compared the performance of ovaHRDscar to the CHORD algorithm that uses structural variation and a random forest implementation to classify HR-status11. In the PCAWG cohort, ovaHRDscar significantly predicted OS using the Log-rank test (Supplementary Fig. 3l, m) and Cox proportional hazard models (Supplementary Fig. 3n), while the CHORD algorithm did not show statistical significance.
Finally, to further investigate the impact of the ovaHRDscar cut-off value in predicting PFS and OS, we plotted the differences of median PFS and OS in HRD vs HRP when using different cut-off values in two independent validation test sets (OVA-TCGA excluding samples used in the optimization and DECIDER) using bootstrapping (Fig. 3k, l). We observed that cut-off values lower than 54 led to significantly smaller differences (lower fold-changes) in PFS in the OVA-TCGA, and in the OVA-TCGA test set, while higher values led to smaller differences in the DECIDER cohort (Fig. 3k). Further, values lower than 54 lead to smaller differences in OS in the OVA-TCGA and OVA-TCGA test set, while higher values led to significantly smaller fold-change differences in the DECIDER cohort (Fig. 3l). Thus, the exploration of clinical outcomes in the multiple independent validation datasets supports HRD/HRP cut-off value of 54 as optimal for ovaHRDscar.
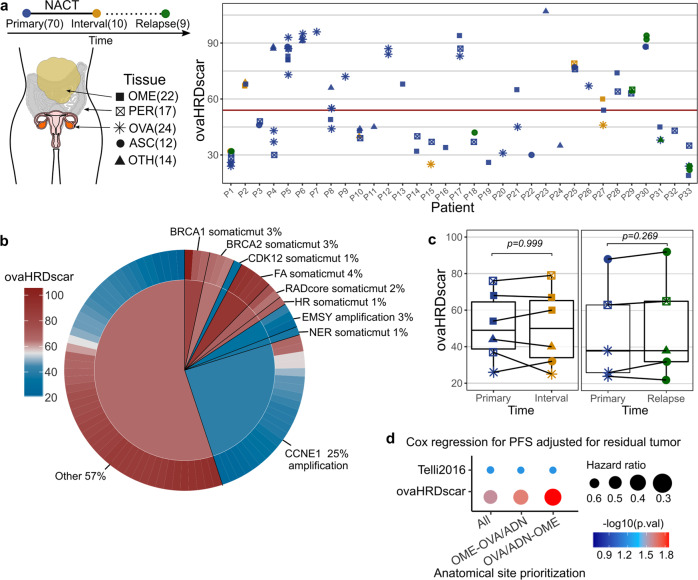
Low intra-patient variation of ovaHRDscar in spatiotemporal tumor profiling
HGSC is characterized by high inter-tumor heterogeneity, and we next explored whether the anatomical site or timing of sample retrieval affects HR-status classification in HGSC. For this, we investigated the concordance of the ovaHRDscar levels in the DECIDER prospective cohort, which included 89 tumor samples from 33 HGSC collected from different anatomical sites and different treatment phases (treatment-naive, after neoadjuvant chemotherapy, or at relapse) (Fig. 4a). Consistent with the TCGA dataset, ovaHRDscar levels corresponded with the known genomic predictors of HRD (Fig. 4b). Importantly, we found that the levels were similar in paired, anatomically matched samples obtained before and after neoadjuvant chemotherapy, and also in primary (treatment-naive) versus relapsed tumors (Fig. 4c). Samples collected from different anatomical sites showed intra-patient variation (Fig. 4a); however, it was lower than the observed inter-patient variation (U test p = 1.95e−38; Supplementary Fig. 4a). The intra-patient variability was not explained by differences in tumor purity (minimum 30%, see "Methods”) (Supplementary Fig". 4b, c). To determine the optimal anatomical sampling site, we next assessed HR-status per patient in treatment-naïve primary samples and compared ovaHRDscar calculated from different anatomical locations. Overall, the level of agreement for the HR-status classification ranged from 94 and 97% between the prioritization of different anatomical sites (Supplementary Fig. 4d). However, ovaHRDscar status calculated primarily from ovarian or adnexal tumors was the strongest predictor for PFS (Fig. 4d, Supplementary Fig. 4e). Consistently, prioritizing ovarian tumors accurately classified all tumors harboring CCNE1 amplification as HRP in the prospective DECIDER cohort (Supplementary Fig. 4d).
Fig. 4. Intra-patient spatiotemporal variation of ovaHRDscar levels in 98 prospective HGSC samples.
a Overview of the samples and their ovaHRDscar levels per patient in a prospective cohort (DECIDER). The tumor samples were collected at three different treatment phases and from different anatomical sites; the corresponding number of samples are displayed in parentheses. b Levels of ovaHRDscar in samples harboring different genetic or epigenetic alterations associated with HRD. The colors correspond to the ovaHRDscar levels, in the outer ring of the pie chart every bar represents a sample carrying the corresponding alteration, and average values for the genetic groups are displayed in the center of the pie chart. c ovaHRDscar values between paired samples for each patient (connected dots) did not change (Wilcoxon test) between the samples collected at different treatment phases. For the box plots, the black horizontal lines represent the sample medians, the boxes extend from first to third quartile and whiskers indicate the values at 1.5 times the interquartile range. d Comparison of anatomical site prioritizations using Cox regression models for PFS using the Telli2016 or the ovaHRDscar algorithms. The size of the dot represents the HR and color of the dot represents the p-value. The HR-status for each patient is shown assessed using three anatomical sample prioritization approaches: (1) average HRD-AIs per all samples (2) omentum, and OVA/ADN if omentum sample not available (OME-OVA/ADN) (3) OVA/ADN, and then omentum if OVA/ADN not available (OVA/ADN-OME). In the case of multiple samples per same site, the average was used.
Machine learning-aided detection of HRD-AIs improves the prediction of clinical outcomes in TNBC
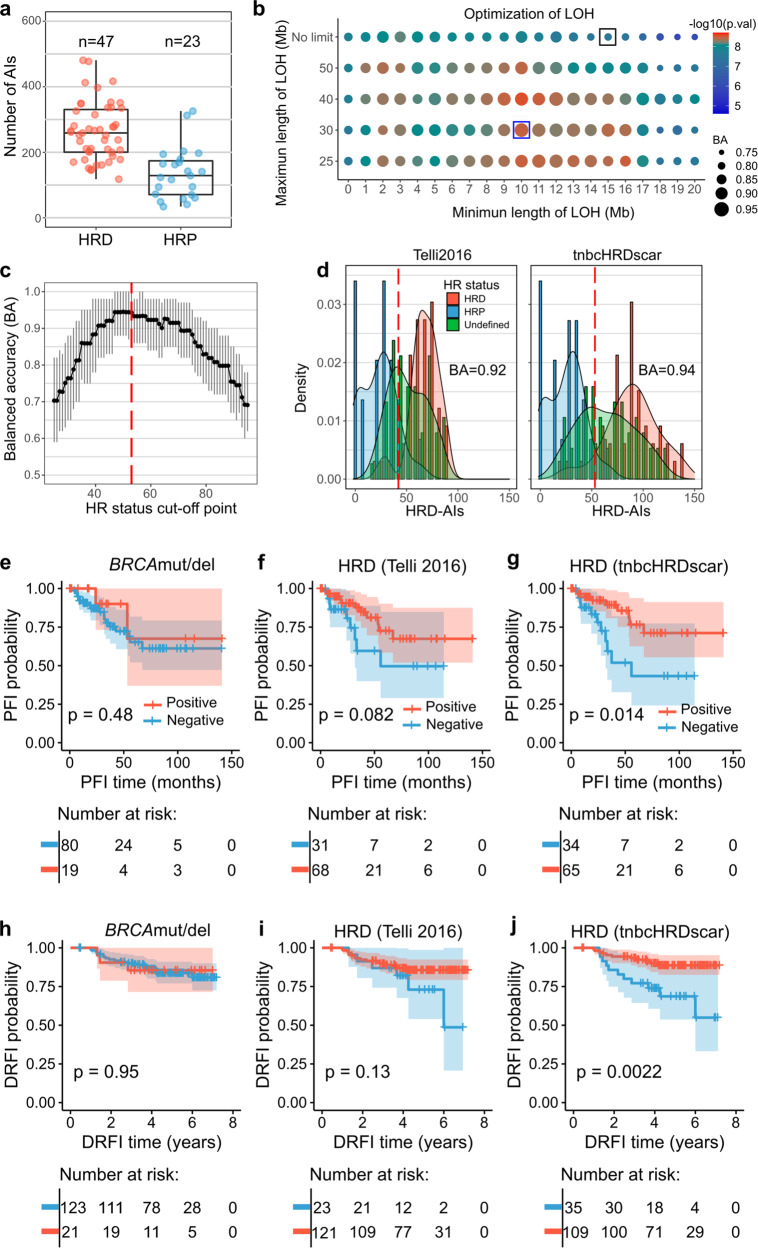
Finally, we tested whether our systematic detection of HRD-AIs could improve previous algorithms when predicting clinical outcomes in TNBC. For this, using multi-omics data in TCGA and the same classification approach (Fig. 2a), we annotated 47 TNBC as HRD and 23 as HRP (Fig. 5a). Detection of HRD-LOH increased the accuracy of classification of HR-status from 80% (Telli2016 algorithm) to 93% (Fig. 5b). Likewise for LSTs, the accuracy increased from 93 to 98% (Supplementary Fig. 5a) and for TAIs from 86 to 92% (Supplementary Fig. 5b). Similarly as for the HGSC, instead of selecting TAIs of a particular length, we selected TAIs longer than 1 Mb as this resulted in the largest increase in significance. The following HRD-AI criteria were observed as the most characteristic for TNBC: (1) LOH > 10 Mb and <30 Mb, (2) for LSTs AI > 5 Mb with a distance between them <2 Mb, and (3) TAI > 1 Mb. Then, using a subsampling approach, we identified that cut-off values for the sum of HRD-AIs (hereafter called tnbcHRDscar) from 47 to 53 produced the highest classification accuracy of the HRD and HRP samples (Fig. 5c), with the cut-off value of 53 as the closest value at the intersection of the HRP and HRP density distributions (Fig. 5d). Using the above criteria we observed that tnbcHRDscar increased the accuracy of classifying the HRD and HRP samples from 0.92 to 0.94 (Fig. 5d).
Fig. 5. Machine learning-aided detection of HRD-AI in TNBC improves the prediction of clinical outcomes.
a Number of AIs for TNBC in HRD and HRP samples in the TCGA. Corresponding box plots are shown, the black horizontal lines represent the sample medians, the boxes extend from first to third quartile and whiskers indicate the values at 1.5 times the interquartile range. b Detection of LOH events. The size of the dots represents the decision tree balanced accuracy (BA) of classifying HRD and HRP using LOHs of the corresponding length, and the dot colors represent the difference in abundance of LOH between HRD versus HRP samples (U test, p-value). Black box corresponds to the selection criteria utilized in the Telli2016 algorithm, and the blue box corresponds to the tnbcHRDscar BA and U test value. c Evaluation of the cut-off for tnbcHRDscar to define HR-status. The black dots connected with a line represent the balanced accuracy (BA) of the classification of the HRD and HRP samples using the given cut-off value, the 95% confidence intervals are shown in gray, the value of 53 (red dashed line) shows the highest BA. d Density distribution of HRD-AIs according to the Telli2016 and tnbcHRDscar algorithms. The red dashed line represents the cut-off established to define HR-status using Telli2016 (≥ 42) and tnbcHRDscar (≥53). The balanced accuracy (BA) for classifying the HR-status is shown for Telli2016 and ovaHRDscar algorithm. e–g Kaplan–Meier plots of PFS (Log-rank test) in TNBC patients in the TCGA stratified using: the BRCAmut/del status (e), the Telli2016 algorithm (f), the tnbcHRDscar (g). h–j Kaplan–Meier plots of distant relapse-free interval (DRFI, Log-rank test) of the TNBC patients in the validation dataset stratified using: the BRCAmut/del status (h), the Telli2016 algorithm (i), the tnbcHRDscar algorithm (j).
To test whether HR-status classification by tnbcHRDscar can predict clinical outcomes in TNBC, we next associated tnbcHRDscar with the PFS in the TCGA cohort and with the distant relapse-free interval (DRFI) in an independent TNBC SNP-array dataset21. Patients with the tnbcHRDscar-positive tumors had a significantly longer PFS than those with the tnbcHRDscar-negative tumors (Log-rank p = 0.014), while BRCAmut/del status or the Telli2016 algorithm did not significantly associate with PFS (Fig. 5e–g). Only tnbcHRDscar showed a statistically significant association with the DRFI (Log-rank p = 0.0022) in the independent validation dataset (Fig. 5h–j). Further, tnbcHRDscar classification in TCGA samples was also associated with OS (Log-rank p = 0.039), similarly to the Telli2016 algorithm (Log-rank p = 0.039; Supplementary Fig. 5c–e). We next applied Cox regression analysis to validate the association of tnbcHRDscar with PFS and OS. In the TCGA cohort, tnbcHRDscar significantly predicted PFS (HR: 0.34, p = 0.018, Supplementary Fig. 5f) but the Telli2016 algorithm did not, while both similarly predicted OS (Supplementary Fig. 5g). However, tnbcHRDscar but not the Telli2016 algorithm significantly predicted DRFI in the validation dataset (HR: 0.29, p = 0.004, Supplementary Fig. 5h). Additionally, we compared the performance of tnbcHRDscar with HRDetect12, an algorithm trained using WGS, to predict DRFI outcomes in the validation dataset. Interestingly, tnbcHRDscar improved the prediction of DRFI compared to the HRDetect (Supplementary Fig. 5h–j), regardless of the cut-off values selected for the HRDetect (Supplementary Fig. 5k).
Discussion
HRD tumors exhibit a distinct clinical phenotype with superior responses to platinum-based chemotherapy and sensitivity to PARP inhibitors. However, the accurate detection of HRD via somatic AIs has been confounded by the lack of systematic approaches and analyses performed in admixtures of tumor types with distinct genomic drivers. Herein, we established the HRDscar, a systematic approach for HRD detection to improve patient selection and clinical outcomes in cancer.
Several genomic approaches have been utilized to detect HRD, including (1) identification of single genetic mutations leading to predicted HRD22, (2) profiles of DNA-repair deficiency gene expression23,24, (3) specific mutational patterns accumulated due to HRD8,9,25 or (4) structural genomic imbalances7,26. These genomic features have been implemented alone or in combinations in the search for optimal HRD detection, which has profound therapeutic implications27. It is now becoming accepted that benefits from the HR-directed therapies such as PARP inhibitors extend beyond the identification of HRD via individual genetic mutations28. This is due to the fact that genes such as BRCA1/2 and RAD51 paralogs can be altered beyond mutations via, e.g., hypermethylation or gene deletions3,29, and not all genomic events leading to HRD have yet been defined30. Allelic imbalances are indicative of the genetic consequences of HRD and, although not dynamically reflective of tumors’ functional HRD status, have shown promise as a biomarker predictive of the magnitude of benefit from PARP inhibitors, especially in the front-line setting31,32. The HRD-algorithm used in ovarian cancer clinical trials (Telli2016) was, however, generated using breast cancer samples or a mixture of breast cancer and ovarian cancer samples using BRCA1/2 mutation as the sole determinant of HRD, and BRCAwt status as HRP8–10. Importantly, the European Society of Medical Oncology also indicated an urgent need to develop a more accurate HRD algorithm in HGSC to especially improve the identification of the HRP tumors28. Via a pan-cancer characterization of AIs, we discovered remarkable differences in the patterns of AIs of HGSC as compared to other cancer types, including TNBC, especially among the BRCAwt tumors. This prompted us to systematically identify the genomic footprints of HRD-AIs specific for HGSC using carefully annotated multi-omics data from TCGA and an iterative machine learning and statistical approach.
ovaHRDscar levels were concordant with tumor genetic alterations associated with HRD in the TCGA dataset and an external validation cohort (DECIDER). We found significantly lower levels of ovaHRDscar in tumors with CCNE1 amplification, which was also previously proposed to be mutually exclusive with HRD and associated with poor clinical outcomes33. In line with a previous report19, tumors with CDK12 mutation showed overall low levels of ovaHRDscar and thus could be considered HRP. In contrast, tumors with somatic mutations in PTEN, a gene associated with DNA repair34,35, showed high ovaHRDscar levels. However, the vulnerability of PTEN deficient cancers to PARP inhibitors remains to be verified in the clinical setting28,36. Further, ovaHRDscar showed a higher concordance with SBS3 than the Telli2016 algorithm. Most importantly, ovaHRDscar can be applied to detect HRD in HGSC samples using WGS or SNP-arrays, making it an attractive biomarker for the clinical setting.
A dichotomous thresholding of a predictive HRD biomarker is needed for therapeutic decision-making. In the Telli2016 algorithm, the cut-off for the total number of events was derived from a mixture of breast and ovarian cancer samples10. More recently, Takaya et al. set out to improve the HRD test by adjusting the cut-off value in ovarian cancer19. However, only BRCAmut status was used for separating HRD from HRP samples and the same genomic features of HRD-AIs were used as in Telli et al. In ovaHRDscar, after the development of accurate definitions of both the criteria of HRD-AIs and the cut-off, we identified more samples as being HRP, and separated HRD from HRP with improved accuracy over previous algorithms. When testing the Telli2016 algorithm using the ovaHRDscar cut-off value of 54, the accuracy was still below that of ovaHRDscar, indicating that both the accurate identification of the HRD-AIs and the selection of the optimal cut-off are needed to improve HRD detection in HGSC. In agreement, in most survival analyses, especially in the independent validation cohorts, ovaHRDscar outperformed the previous algorithms in predicting clinical outcomes.
HRD tumors are known to have superior responses to platinum-based chemotherapy and prolonged overall survival37. Consistently, ovaHRDscar improved the prediction of PFS and OS for platinum-based chemotherapy in the OVA-TCGA, also after excluding patients used when defining the criteria for ovaHRDscar. ovaHRDscar significantly predicted PFS and OS also among only the BRCAwt tumors. Importantly, ovaHRDscar improved the prediction of clinical outcomes in two independent patient cohorts and in multivariable models after adjusting for clinical covariables, indicating that ovaHRDscar reliably captures the phenotypic clinical behavior of HRD in HGSC. Further, using a disease-specific, systematic approach in the classification of HR-status, we could improve the prediction of the clinical outcomes also in TNBC, and tnbcHRDscar significantly predicted disease-free survival in the TCGA and in an independent dataset. However, none of the clinical cohorts included patients treated prospectively with, e.g., PARP inhibitors; therefore, prospective validation in larger patient series is warranted.
Finally, as HGSC is characterized by a high intra-tumor heterogeneity, we aimed at assessing whether the anatomical site of tumor sampling or the exposure to chemotherapy affects HRD detection. Our analysis of 98 samples collected from different anatomical sites and treatment phases indicated that ovaHRDscar levels remain similar within each patient, including anatomically site-matched samples collected before and after neoadjuvant chemotherapy. ovaHRDscar can thus be reliably assessed during routine clinical practice and also after neoadjuvant chemotherapy, given that the tumor purity remains higher than 30%. Interestingly, ovaHRDscar levels were also similar between treatment-naive and relapsed tumors, reflecting the nature of HRD-AIs as a historical consequence rather than a dynamic read-out of functional HRD. Analysis of different anatomical sites revealed that the overall inter-patient variation was higher than the intra-patient variation. However, in four out of 21 (19%) patients with samples from multiple anatomical sites, the HRD category depended on the anatomical site of sampling. The survival analyses indicated that ovarian or adnexal sites, followed by omentum, could be the preferred sites for HRD testing, warranting future validation in larger cohorts.
In conclusion, ovaHRDscar shows promise as a precise, clinically feasible assay for both outcome prediction and selection of patients for HR-directed therapies. With the fully documented, publicly available algorithms and generation pipeline, ovaHRDscar can be applied to other tumor types and implemented clinically for optimal patient selection to improve outcomes for patients with cancer.
Methods
Dataset collection and classification
For pan-cancer samples, allele-specific copy-number segments were obtained from the Genomics Data Commons (GDC) portal (https://portal.gdc.cancer.gov/). The list of TNBC samples was adopted from Lehmann et al.38. For TNBC, samples were considered with BRCAmut if reported by Knijnenburg et al.39 to contain a gene deletion, gene mutation, or gene silencing of BRCA1 or BRCA2; while BRCAwt were considered those with no reported alterations.
For OVA-TCGA analysis, allele-specific copy-number segments, DNA methylation, gene-level copy-number profiles (including gene deletions), and clinical information data were obtained from the GDC data portal. Genes were considered with a “strong signal of deletion” if reported as such (labeled by −2) by Taylor et al.40. Gene promoter hypermethylation was considered when the probes up to 1500 bp downstream of the transcription start site had an average beta value ≥0.75. The catalog of mc3 somatic mutations was obtained from the PanCanAtlas-GDC data portal (https://gdc.cancer.gov/about-data/publications/pancanatlas). Somatic mutations were classified according to the recommendations of the American College of Medical Genetics and Genomics41 using the web-tool VarSome42. Only pathogenic somatic mutations were considered in the analysis. For germline mutations, we selected those labeled as pathogenic and prioritized by Huang et al. 201843. Genes were considered part of the HR pathway or other associated pathways according to the Kyoto Encyclopedia of Genes and Genomes database44. Complementary clinical information was obtained from the PanCanAtlas-GDC data portal. For PCAWG: allele-specific copy-number segments, mutational drivers, and clinical information were obtained from the International Cancer Genome Consortium data portal (https://dcc.icgc.org/pcawg).
Pan-cancer characterization of AIs
We used the allele-specific copy-number segments from the Genomics Data Commons. Segments that did not span a whole chromosome and with a total copy-number value different from two were selected as AIs. AIs shorter than 3 Mb and longer than 50 Mb were ignored. We quantified the number of AIs per sample and the median length of the AIs. The skewness of the distribution of the length AIs in different types of cancers was performed using the package DescTools.
Selection of criteria for HRD-AIs
First, we annotated the OVA-TCGA samples as HRD and HRP according to the following. For HRD samples, samples harboring somatic or germline mutations, promoter hypermethylation, or strong signal of deletion of the genes BRCA1, BRCA2, and RAD51 paralogs (Fig. 2a); for HRP sample annotation, we selected those with none of the HRD selection criteria, plus available data for methylation, gene deletion, somatic mutations and no deletion of any HR gene. The rest of the samples were annotated as “undefined” (Fig. 2a). The HRD and HRP annotation was used as “ground truth” in posterior accuracy assessment analysis. The HRP sample TCGA-13-1511 was annotated as “undefined” as an outlier in the number of total AIs. Then, for the annotated HRD/HRP samples, we quantified the HRD-AIs (LOH, LST, TAI) according to Marquard et al.45 under different criteria. For LOH, we used length criteria (minimum length: lmin, maximum length: lmax). Exhaustively for each pair of values, lmin and lmax, we quantified the number of LOH per sample. We selected the pair of values that produced the highest classification power (see below) according to the HRD and HRP annotations. The quantification of LST events, defined by the parameters s (minimum AI length) and m (maximum distance between the AI events that comprise an LST event), was optimized similarly. Finally, we quantified TAI events if they were larger than k, where the length k was evaluated following the same approach. The classification power was evaluated by combining two approaches: (1) differential abundance of selected AIs in the annotated HRD vs HRP using one-tailed Mann–Whitney U test; (2) classification performance by decision trees (R package ‘rpart’) taking the abundance of the selected AIs as split-point. For the decision trees approach, samples above the split-point were tentatively considered as HRD and below - HRP, then true positive rate (TPR) and true negative rate (TNR) was computed when compared against the ground truth annotations (Fig. 2b). For each type of HRD-AI, we selected the set of parameters ({lmin, lmax},{s,m}, k) with the highest product of U test p-value (p) and balance accuracy , the product was inferred with the formula: −1*log10(p)*BA. The selected set of parameters was incorporated in ovaHRDscar. The sum of HRD-AIs under the selected criteria was named the ovaHRDscar levels or values. A cut-off value to define the HR status (samples with values above the cut-off are considered HRD and below—HRP) for ovaHRDscar and tnbcHRDscar levels was determined by exploring different cut-off values. For each cut-off value, we resampled with replacement 29 of the annotated HRD and 29 of the HRP cases 10,000 times; for each pseudo replicate, we calculated the balanced accuracy by comparing the HR status using the cut-off value versus the ground truth annotations. Finally, we selected the cut-off value that produced the highest median balanced accuracy.
Quantification of HRD-AIs
The quantification of HRD-AIs by the Telli2016 algorithm, the Takaya2020, the ovaHRDscar, and the tnbcHRDScar was performed using an in-house R-package (see code availability) adapted from the package scarHRD46. This package allows for the quantification of LOH, LSTs and TAIs under different selection criteria. Allelic imbalances smaller than 50 bp were smoothed, as previously suggested by Popova et al.7. The selection criteria of HRD-AIs for Telli2016: LOH lmin = 15 Mb, lmax = 50 Mb; LSTs s = 12 Mb, m = 1 Mb, TAI k = 1 Mb, samples with HRD-AIs ≥ 42 were considered HRD otherwise—HRP. For the Takaya2020 algorithm, the same HRD-AIs selection criteria as for Telli2016 were used: samples with HRD-AIs ≥ 63 were considered HRD, and otherwise—HRP. For ovaHRDscar, the HRD-AIs selection criteria are LOH lmin = 15 Mb, lmax = 50 Mb; LSTs s = 12 Mb, m = 1 Mb, TAI k = 1 Mb; samples with HRD-AIs ≥54 were considered HRD, and otherwise—HRP.
Survival analysis
Survival plots, Log-rank and Cox regression models were performed in R using the packages “survminer” and “survival”. For OVA-TCGA, only patients disease treated with cisplatin or carboplatin were selected. For PCAWG, data from all patients were used (no treatment information available). Only data from primary samples (treatment-naive) were used. The BRCAmut/del status includes pathogenic somatic mutations, germline mutations, and “strong signal of deletion” in the genes BRCA1 or BRCA2. Residual tumor after surgery was categorized as present or absent. For the indicated Cox regressions, residual tumor status or patient age at diagnosis was used as a covariable. Progression-free survival (PFS) and overall survival (OS) were defined as in Liu et al.47. The CHORD signature HR-status classification for PCAWG samples was adopted from Nguyen et al. 202011. In the TNBC cohort from TCGA, only patients with advanced Stage III-IV were selected. For survival analysis using HRDetect stratification, positive status was labeled for patients with an HRDetect value ≥ 0.7, and HRDetect negative for those with a value ≤ 0.2, patients with intermediate values were ignored. The mean differences of PFS and OS between HRD and HRP patients according to different criteria were calculated by bootstrapping the patients 1000 times; for each bootstrapping replicate was calculated the fold-change of median PFS or OS as median survival (PFS or OS) time in HRD patients divided by median survival (PFS or OS) time in HRP patients.
Prospective DECIDER and TERVA data analysis
The tumor samples were prospectively collected in the DECIDER (http://www.project-DECIDER.eu) and TERVA (https://www.healthcampusturku.fi/innovation-new/terva-project/) projects. The Ethics Committee of the Hospital District of Southwest Finland approved both studies (Dnro: 145 /1801/2015). All patients gave their written informed consent to take part in the study. For DECIDER, paired fresh tumor and normal blood samples were sequenced using Illumina-HiSeq X Ten WGS. Raw reads were trimmed and filtered with Trimmomatic48, followed by duplicate marking with Picard Tools (https://broadinstitute.github.io/picard/). Alignment to the human genome GRCh38 was done using the Burrows-Wheeler aligner BWA-MEM49. Mutations were detected using GATK4-Mutect2 approach50. GATK4-Mutect2 was used for the detection of allele-specific copy numbers; regions listed in the ENCODE blacklist51 were omitted. Tumor purity was estimated using two approaches: (1) Based on somatic copy-number profiles using the software ASCAT v2.5.251 (2) Based on variant allele frequency of the truncal mutation in gene TP53 (TP53-VAF), purity was estimated using the formula: 2/((CN/TP53-VAF) - (CN - 2)), where CN corresponds to the absolute copy-number value estimated by ASCAT in the corresponding truncal mutation locus. Subsequently, the higher purity value was selected. For the TERVA samples tumor-only profiling, tumor samples were genotyped using the Infinium™ Global Screening Array-24 v2.0. B allele frequency and LogR ratios per sample probe were calculated using Illumina-GenomeStudio. ASCAT software was used for the detection of allele-specific copy numbers, ascat.predictGermlineGenotypes module was performed, adjusting parameters according to a panel of 200 normal germline blood samples. Intra- and inter-patient variability of ovaHRDscar values in the DECIDER cohort was determined by calculating the absolute value of the pairwise ovaHRDscar difference between all pair combinations of samples52. Patient P19 was omitted from survival analysis because she received PARP inhibitors as maintenance after the first-line therapy.
Statistics
The statistics analysis was performed in R. Difference in abundances was calculated using one-sided Mann–Whitney U test unless stated it was two-sided. Paired difference in abundances was calculated using two-sided Wilcoxon test. Agreement was calculated using the Cohen kappa test. Concordance was measured using Lin’s concordance correlation coefficient. Level of correlations was assessed using Pearson correlations. P-value less than 0.05 was considered statistically significant.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Supplementary information
Acknowledgements
This study was funded by the Sigrid Jusélius Foundation (A.F., L.K.), Cancer Society of Finland (A.F., J.C., L.K.), Academy of Finland (grant number 339805, 322979, 350396 to A.F., grant numbers 314394 and 322178 to L.K., grant number 314398 to SaHi), Paolo Foundation (A.F.), The Finnish Medical Foundation (A.F.), Finnish Cultural Foundation (A.F.), Instrumentarium Foundation (A.F., J.C.), University of Helsinki (A.F.), AstraZeneca (to SaHi), the European Union’s Horizon 2020 research and innovation program under grant agreement No 667403 for HERCULES (SHa, J.H., SaHi) and No 965193 for DECIDER (SHa, J.H., SaHi). We also wish to thank FIMM Genomics core facility, The FINNPEC for the statistical reference data, Johan Staaf for assistance in TNBC data access, and the IT Center for Science (CSC) for computational resources.
Author contributions
A.F. and F.P. conceived and designed the study with contributions from L.K., J.O., P.A.K. and S.H. F.P., J.O., J.C., D.C.G., Y.L. and K.L. analyzed the data. F.P. performed the statistical analysis. A.C., M.T., S.K., J.H., U.H., J.S.T. and H.L. performed experiments and provided materials. All authors wrote and approved the manuscript.
Data availability
Somatic whole genome sequencing data for the DECIDER and TERVA cohort are available through the European Genome-Phenome Archive under the study accession number EGAS00001006775.
Code availability
The code used for the data analysis is available on Github (https://github.com/farkkilab/pubs/tree/master/Perez_et_al_2022). The ovaHRDscar algorithm implementation is available as an R package on Github (https://github.com/farkkilab/ovaHRDscar).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41698-022-00339-8.
References
- 1.Ceccaldi R, Rondinelli B, D’Andrea AD. Repair pathway choices and consequences at the double-strand break. Trends Cell Biol. 2016;26:52–64. doi: 10.1016/j.tcb.2015.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lord CJ, Ashworth A. PARP inhibitors: Synthetic lethality in the clinic. Science. 2017;355:1152–1158. doi: 10.1126/science.aam7344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Torre LA, et al. Ovarian cancer statistics, 2018. CA Cancer J. Clin. 2018;68:284–296. doi: 10.3322/caac.21456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Konstantinopoulos PA, Ceccaldi R, Shapiro GI, D’Andrea AD. Homologous recombination deficiency: exploiting the fundamental vulnerability of ovarian cancer. Cancer Discov. 2015;5:1137–1154. doi: 10.1158/2159-8290.CD-15-0714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ray-Coquard I, et al. Olaparib plus Bevacizumab as first-line maintenance in ovarian cancer. N. Engl. J. Med. 2019;381:2416–2428. doi: 10.1056/NEJMoa1911361. [DOI] [PubMed] [Google Scholar]
- 6.Gonzalez-Martin A, et al. Niraparib in patients with newly diagnosed advanced ovarian cancer. N. Engl. J. Med. 2019;381:2391–2402. doi: 10.1056/NEJMoa1910962. [DOI] [PubMed] [Google Scholar]
- 7.Popova T, et al. Ploidy and large-scale genomic instability consistently identify basal-like breast carcinomas with BRCA1/2 inactivation. Cancer Res. 2012;72:5454–5462. doi: 10.1158/0008-5472.CAN-12-1470. [DOI] [PubMed] [Google Scholar]
- 8.Abkevich V, et al. Patterns of genomic loss of heterozygosity predict homologous recombination repair defects in epithelial ovarian cancer. Br. J. Cancer. 2012;107:1776–1782. doi: 10.1038/bjc.2012.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Birkbak NJ, et al. Telomeric allelic imbalance indicates defective DNA repair and sensitivity to DNA-damaging agents. Cancer Discov. 2012;2:366–375. doi: 10.1158/2159-8290.CD-11-0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Telli ML, et al. Homologous recombination deficiency (HRD) score predicts response to platinum-containing neoadjuvant chemotherapy in patients with triple-negative breast cancer. Clin. Cancer Res. 2016;22:3764–3773. doi: 10.1158/1078-0432.CCR-15-2477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nguyen L, Martens JWM, Van Hoeck A, Cuppen E. Pan-cancer landscape of homologous recombination deficiency. Nat. Commun. 2020;11:5584. doi: 10.1038/s41467-020-19406-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davies H, et al. HRDetect is a predictor of BRCA1 and BRCA2 deficiency based on mutational signatures. Nat. Med. 2017;23:517–525. doi: 10.1038/nm.4292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stefansson OA, et al. Genomic profiling of breast tumours in relation to BRCA abnormalities and phenotypes. Breast Cancer Res. 2009;11:R47. doi: 10.1186/bcr2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Breiman, L. Classification and Regression Trees (Wadsworth International Group, 1984).
- 15.Consortium, I. T. P.-C. A. o. W. G. Pan-cancer analysis of whole genomes. Nature. 2020;578:82–93. doi: 10.1038/s41586-020-1969-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Luca XM, et al. Using whole-genome sequencing data to derive the homologous recombination deficiency scores. NPJ Breast Cancer. 2020;6:33. doi: 10.1038/s41523-020-0172-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alexandrov LB, et al. The repertoire of mutational signatures in human cancer. Nature. 2020;578:94–101. doi: 10.1038/s41586-020-1943-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gulhan DC, Lee JJ, Melloni GEM, Cortes-Ciriano I, Park PJ. Detecting the mutational signature of homologous recombination deficiency in clinical samples. Nat. Genet. 2019;51:912–919. doi: 10.1038/s41588-019-0390-2. [DOI] [PubMed] [Google Scholar]
- 19.Takaya H, Nakai H, Takamatsu S, Mandai M, Matsumura N. Homologous recombination deficiency status-based classification of high-grade serous ovarian carcinoma. Sci. Rep. 2020;10:2757. doi: 10.1038/s41598-020-59671-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Polterauer S, et al. Prognostic value of residual tumor size in patients with epithelial ovarian cancer FIGO stages IIA-IV: analysis of the OVCAD data. Int J. Gynecol. Cancer. 2012;22:380–385. doi: 10.1097/IGC.0b013e31823de6ae. [DOI] [PubMed] [Google Scholar]
- 21.Staaf J, et al. Whole-genome sequencing of triple-negative breast cancers in a population-based clinical study. Nat. Med. 2019;25:1526–1533. doi: 10.1038/s41591-019-0582-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wagle N, et al. High-throughput detection of actionable genomic alterations in clinical tumor samples by targeted, massively parallel sequencing. Cancer Discov. 2012;2:82–93. doi: 10.1158/2159-8290.CD-11-0184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kang J, D’Andrea AD, Kozono D. A DNA repair pathway-focused score for prediction of outcomes in ovarian cancer treated with platinum-based chemotherapy. J. Natl Cancer Inst. 2012;104:670–681. doi: 10.1093/jnci/djs177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Konstantinopoulos PA, et al. Gene expression profile of BRCAness that correlates with responsiveness to chemotherapy and with outcome in patients with epithelial ovarian cancer. J. Clin. Oncol. 2010;28:3555–3561. doi: 10.1200/JCO.2009.27.5719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang YK, et al. Genomic consequences of aberrant DNA repair mechanisms stratify ovarian cancer histotypes. Nat. Genet. 2017;49:856–865. doi: 10.1038/ng.3849. [DOI] [PubMed] [Google Scholar]
- 26.Polak P, et al. A mutational signature reveals alterations underlying deficient homologous recombination repair in breast cancer. Nat. Genet. 2017;49:1476–1486. doi: 10.1038/ng.3934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Swisher EM, et al. Rucaparib in relapsed, platinum-sensitive high-grade ovarian carcinoma (ARIEL2 Part 1): an international, multicentre, open-label, phase 2 trial. Lancet Oncol. 2017;18:75–87. doi: 10.1016/S1470-2045(16)30559-9. [DOI] [PubMed] [Google Scholar]
- 28.Miller RE, et al. ESMO recommendations on predictive biomarker testing for homologous recombination deficiency and PARP inhibitor benefit in ovarian cancer. Ann. Oncol. 2020;31:1606–1622. doi: 10.1016/j.annonc.2020.08.2102. [DOI] [PubMed] [Google Scholar]
- 29.Golmard L, et al. Contribution of germline deleterious variants in the RAD51 paralogs to breast and ovarian cancers. Eur. J. Hum. Genet. 2017;25:1345–1353. doi: 10.1038/s41431-017-0021-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Radhakrishnan SK, Jette N, Lees-Miller SP. Non-homologous end joining: emerging themes and unanswered questions. DNA Repair (Amst.) 2014;17:2–8. doi: 10.1016/j.dnarep.2014.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ray-Coquard I, et al. Olaparib plus bevacizumab as first-line maintenance in ovarian cancer. N. Engl. J. Med. 2019;381:2416–2428. doi: 10.1056/NEJMoa1911361. [DOI] [PubMed] [Google Scholar]
- 32.Gonzalez-Martin A, et al. Niraparib in patients with newly diagnosed advanced ovarian cancer. N. Engl. J. Med. 2019;381:2391–2402. doi: 10.1056/NEJMoa1910962. [DOI] [PubMed] [Google Scholar]
- 33.Etemadmoghadam D, et al. Synthetic lethality between CCNE1 amplification and loss of BRCA1. Proc. Natl Acad. Sci. USA. 2013;110:19489–19494. doi: 10.1073/pnas.1314302110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Saal LH, et al. Recurrent gross mutations of the PTEN tumor suppressor gene in breast cancers with deficient DSB repair. Nat. Genet. 2008;40:102–107. doi: 10.1038/ng.2007.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bassi C, et al. Nuclear PTEN controls DNA repair and sensitivity to genotoxic stress. Science. 2013;341:395–399. doi: 10.1126/science.1236188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bian X, et al. PTEN deficiency sensitizes endometrioid endometrial cancer to compound PARP-PI3K inhibition but not PARP inhibition as monotherapy. Oncogene. 2018;37:341–351. doi: 10.1038/onc.2017.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Norquist BM, et al. Mutations in homologous recombination genes and outcomes in ovarian carcinoma patients in GOG 218: An NRG oncology/gynecologic oncology group study. Clin. Cancer Res. 2018;24:777–783. doi: 10.1158/1078-0432.CCR-17-1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lehmann BD, et al. Refinement of triple-negative breast cancer molecular subtypes: implications for neoadjuvant chemotherapy selection. PLoS ONE. 2016;11:e0157368. doi: 10.1371/journal.pone.0157368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Knijnenburg TA, et al. Genomic and molecular landscape of DNA damage repair deficiency across the cancer genome atlas. Cell Rep. 2018;23:239–254.e236. doi: 10.1016/j.celrep.2018.03.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Taylor AM, et al. Genomic and functional approaches to understanding cancer aneuploidy. Cancer Cell. 2018;33:676–689.e673. doi: 10.1016/j.ccell.2018.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Richards S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–424. doi: 10.1038/gim.2015.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kopanos C, et al. VarSome: the human genomic variant search engine. Bioinformatics. 2019;35:1978–1980. doi: 10.1093/bioinformatics/bty897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huang KL, et al. Pathogenic germline variants in 10,389 adult cancers. Cell. 2018;173:355–370.e314. doi: 10.1016/j.cell.2018.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kanehisa M, Goto S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28:27–30. doi: 10.1093/nar/28.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Marquard AM, et al. Pan-cancer analysis of genomic scar signatures associated with homologous recombination deficiency suggests novel indications for existing cancer drugs. Biomark. Res. 2015;3:9. doi: 10.1186/s40364-015-0033-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sztupinszki Z, et al. Migrating the SNP array-based homologous recombination deficiency measures to next generation sequencing data of breast cancer. NPJ Breast Cancer. 2018;4:16. doi: 10.1038/s41523-018-0066-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu J, et al. An integrated TCGA pan-cancer clinical data resource to drive high-quality survival outcome analytics. Cell. 2018;173:400–416.e411. doi: 10.1016/j.cell.2018.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bolger AM, Lohse M, Usadel B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics. 2014;30:2114–2120. doi: 10.1093/bioinformatics/btu170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li H, Durbin R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics. 2009;25:1754–1760. doi: 10.1093/bioinformatics/btp324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cibulskis K, et al. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat. Biotechnol. 2013;31:213–219. doi: 10.1038/nbt.2514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Amemiya HM, Kundaje A, Boyle AP. The ENCODE blacklist: identification of problematic regions of the genome. Sci. Rep. 2019;9:9354. doi: 10.1038/s41598-019-45839-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Van Loo P, et al. Allele-specific copy number analysis of tumors. Proc. Natl Acad. Sci. USA. 2010;107:16910–16915. doi: 10.1073/pnas.1009843107. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Somatic whole genome sequencing data for the DECIDER and TERVA cohort are available through the European Genome-Phenome Archive under the study accession number EGAS00001006775.
The code used for the data analysis is available on Github (https://github.com/farkkilab/pubs/tree/master/Perez_et_al_2022). The ovaHRDscar algorithm implementation is available as an R package on Github (https://github.com/farkkilab/ovaHRDscar).