Abstract
Pretomanid is a nitroimidazole antimicrobial active against drug-resistant Mycobacterium tuberculosis and approved in combination with bedaquiline and linezolid (BPaL) to treat multidrug-resistant (MDR) pulmonary tuberculosis (TB). However, the penetration of these antibiotics into the central nervous system (CNS), and the efficacy of the BPaL regimen for TB meningitis, are not well established. Importantly, there is a lack of efficacious treatments for TB meningitis due to MDR strains, resulting in high mortality. We have developed new methods to synthesize 18F-pretomanid (chemically identical to the antibiotic) and performed cross-species positron emission tomography (PET) imaging to noninvasively measure pretomanid concentration-time profiles. Dynamic PET in mouse and rabbit models of TB meningitis demonstrates excellent CNS penetration of pretomanid but cerebrospinal fluid (CSF) levels does not correlate with those in the brain parenchyma. The bactericidal activity of the BPaL regimen in the mouse model of TB meningitis is substantially inferior to the standard TB regimen, likely due to restricted penetration of bedaquiline and linezolid into the brain parenchyma. Finally, first-in-human dynamic 18F-pretomanid PET in six healthy volunteers demonstrates excellent CNS penetration of pretomanid, with significantly higher levels in the brain parenchyma than in CSF. These data have important implications for developing new antibiotic treatments for TB meningitis.
Subject terms: Central nervous system infections, Molecular medicine, Clinical microbiology, Tuberculosis
Pretomanid has been approved for use in cases of multi-drug resistant pulmonary tuberculosis, yet the penetration of this antibiotic into other target tissues is not well established. Authors provide insight on pretomanid pharmacokinetics in the central nervous system, using positron emission tomography in animal models, and human studies.
Introduction
Tuberculosis (TB) remains one of the leading killers from a single infectious agent1 and TB meningitis is the most devastating extrapulmonary form, especially in the young and immunocompromised2–4. Multidrug-resistant (MDR)-TB, caused by Mycobacterium tuberculosis resistant to first-line antibiotics (i.e., isoniazid and rifampin), is on the rise. TB meningitis due to MDR strains is associated with high mortality5–7, and drug-resistance is an independent predictor of death8. In a recent retrospective cohort study among 237 patients with TB meningitis, mortality was significantly higher among patients with drug-resistant (67%) than drug-susceptible disease (24%, P < 0.001)9. Moreover, mortality was significantly higher (adjusted hazards ratio of 7.2) in patients with drug-resistant TB meningitis after 90 days of initiation of treatment (P < 0.001). New drugs and more efficacious treatments against MDR-TB are therefore urgently needed to combat this public health threat. Pretomanid (formerly PA-824) is a small molecule belonging to the nitroimidazole class of antimicrobial agents, approved by the U.S. Food and Drug Administration (FDA) in 2019 for the treatment of pulmonary MDR-TB, in combination with bedaquiline and linezolid (BPaL - bedaquiline, pretomanid, linezolid)10. Pretomanid is active against both replicating and non-replicating M. tuberculosis, which contributes to its excellent bactericidal activity11–14.
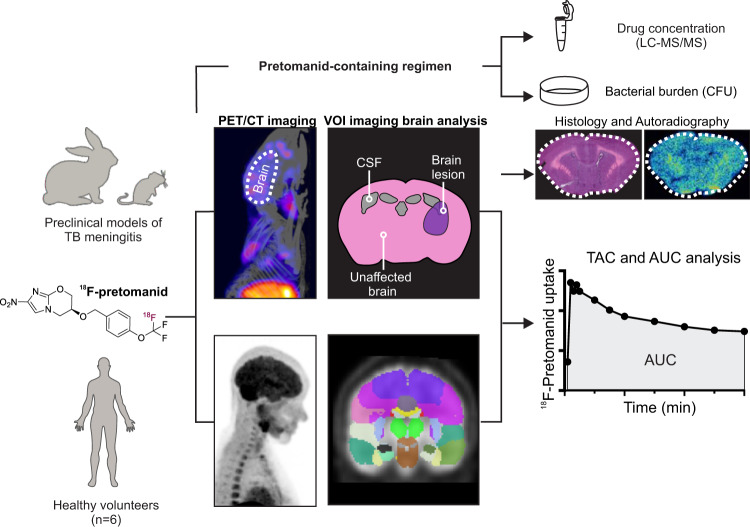
With few exceptions, current antibiotic dosing recommendations are based on plasma concentrations, without information on drug concentrations at the site of infection. Since inappropriate antibiotic levels in target tissues can lead to selection of resistant organisms, toxicity or organ injury, and ultimately treatment failure, a growing number of studies and the U.S. FDA increasingly support measuring antibiotic concentrations in infected tissues15. Therefore, we have developed positron emission tomography (PET)-based clinically-translatable technologies for noninvasive, simultaneous, and unbiased, multi-compartment in situ measurements of antibiotic concentration-time curves in animals and humans16–18. In this study, we report the development of 18F-pretomanid as a molecular imaging tool to noninvasively assess whole-body drug biodistribution (Fig. 1) utilizing detailed animal studies in mouse and rabbit models of TB meningitis17,19,20. In brief, infected animals undergo dynamic PET/computed tomography (CT) with 18F-pretomanid to obtain time-activity curves (TACs) and areas under the curve (AUCs) by quantifying the PET signal in volumes of interest (VOI). Post-mortem autoradiography and histology are also performed in all animal models. Given the unknown potential of pretomanid-containing regimens for TB meningitis, the bedaquiline (B), pretomanid (P) and linezolid (L) regimen is tested in a mouse model of TB meningitis20. Mass spectrometry and traditional microbiology techniques are employed to evaluate intraparenchymal drug levels and bactericidal efficacy (bacterial burden quantified with colony-forming units [CFU]) longitudinally. Radiosynthesis of 18F-pretomanid under current Good Manufacturing Practices (cGMP) facilitates translation into humans, and first-in-human dynamic 18F-pretomanid PET studies are performed in accordance with U.S. FDA guidelines.
Fig. 1. Schematic representation of the experimental design.
Mouse and rabbit models of TB meningitis were used for radiotracer validation, pharmacokinetic characterization and pretomanid-containing regimen testing. 18F-Pretomanid synthesis was optimized for clinical translation under cGMP and first-in-human PET imaging was performed. 18F-Pretomanid was administered intravenously. Following dynamic PET/CT imaging, several volumes of interest (VOI) were drawn to obtain PET-derived time-activity curves (TACs). TACs were used to calculate the area under the curve (AUC) and AUC tissue/plasma ratios.
Results
Radiosynthesis and characterization of 18F-pretomanid
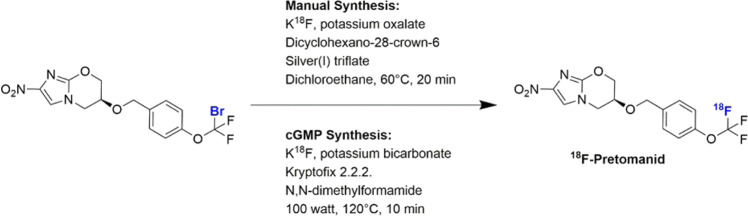
18F-Pretomanid was obtained through halogen exchange 18F-fluorination (Fig. 2) of an aryl-bromodifluoromethoxyl precursor, which was obtained from a five-step synthetic route (Figs. S1–2). The radiosynthetic approach employed a silver-catalyzed nucleophilic displacement, following an adapted protocol by Khotavivattana et al.21. We obtained a radiochemical yield (RCY) of 5 ± 2% (non-decay corrected [n.d.c.]), from starting 18F-fluoride to formulated 18F-pretomanid, and found that reducing the amount of precursor or changing the solvent had a detrimental effect on the RCY. High-performance liquid chromatography (HPLC) analysis on the isolated product revealed a radiochemical purity >98%. While this method allowed the radiosynthesis of 18F-pretomanid for animal studies, the use of dichloroethane precluded its clinical translation. Therefore, we tested alternative reaction solvents to translate the synthesis of 18F-pretomanid under cGMP conditions which unfortunately significantly reduced RCY. However, automated cGMP synthesis of 18F-pretomanid was successful under microwave irradiation at 100 watts for 10 min (reaching 120 °C) in dimethylformamide in the absence of silver salts, despite previous reports that catalyst-free thermal activation had been unsuccessful for the preparation of 18F-labeled aryl-OCF3 compounds. Under these conditions, 18F-pretomanid was obtained in 5.7 ± 0.3% n.d.c. yield and a specific activity of 68 ± 2 GBq/µmol. HPLC analysis showed ≥95% radiochemical purity and a single peak corresponding to the 19F-reference pretomanid in the UV chromatogram (Fig. S3).
Fig. 2. Synthesis of 18F-pretomanid.
18F-pretomanid was obtained through 18F-fluorination of an aryl-bromodifluoromethoxyl precursor. Manual synthesis was performed for preclinical imaging studies and optimized to comply with cGMP to allow clinical translation.
In vitro, unbound 18F-pretomanid remained stable (>90%) in mouse, rabbit, and human serum at 37 °C for three hours. Defluorination was not observed. Pretomanid is known to be highly protein bound (~86%) in human plasma22. When incubated with mouse, rabbit, and human serum at 37 °C, the protein binding level of 18F-pretomanid was 75–77% in healthy human, 78–80% in healthy rabbit, 80–83% in M. tuberculosis-infected rabbit, 75–80% in healthy mouse, and 74–78% in M. tuberculosis-infected mouse sera (Table S1). Overall, 18F-pretomanid had similar protein binding (74–83%) to unlabeled pretomanid, and no significant differences were found between species over time. 18F-Pretomanid experimental LogD7.4, which represents its distribution coefficient at physiological pH, was 1.9 ± 0.1, which is only a 0.4 Log decrease when compared to unlabeled pretomanid23. Thus, 18F-labeled and unlabeled pretomanid are expected to have similar tissue partitioning. Whole-body biodistribution of 18F-pretomanid was measured in mice with experimentally-induced pulmonary TB utilizing PET/CT and gamma counting (Fig. S4). Upon intravenous injection, 18F-pretomanid rapidly distributed to all major organs, which was also confirmed by post-mortem biodistribution quantification by gamma-counting (Fig. S4a, b). The activity in the bone was low and did not substantially increase over time which indicates that defluorination did not occur in vivo (Fig. S4c). Similar to the parent drug, 18F-pretomanid underwent both renal and hepatobiliary excretion (Fig. S4d). Low uptake was observed in muscle and high uptake was found in brown adipose tissue (BAT), which cleared within hours (Fig. S4e). Spatial distribution with ex vivo autoradiography in the mouse model of pulmonary TB showed reduced uptake of 18F-pretomanid in lung lesions compared to unaffected lung (Fig. S4f). The upper-body biodistribution of 18F-pretomanid was also measured in rabbits showing similar findings as in mice (Fig. S5).
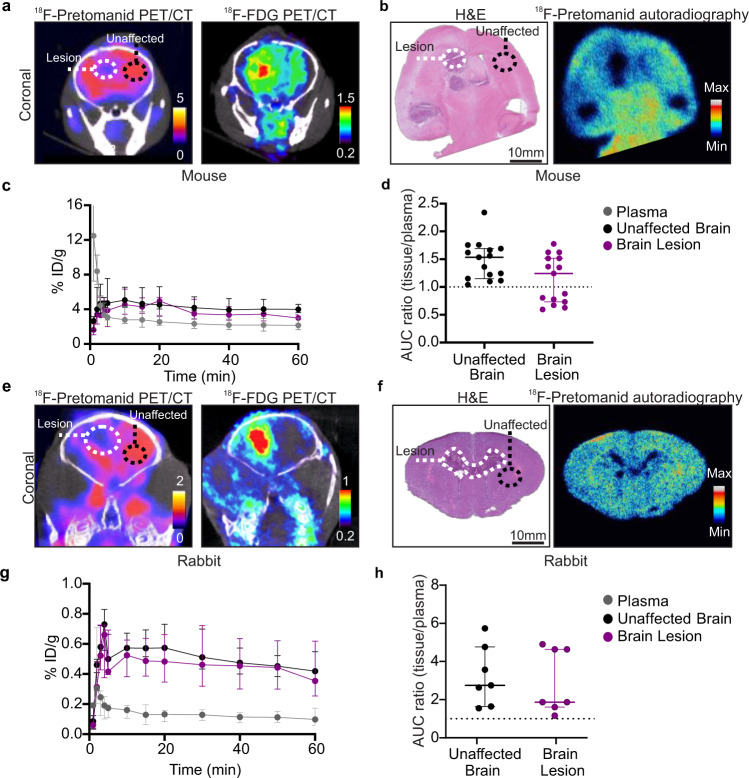
18F-Pretomanid has excellent central nervous system (CNS) penetration
Our initial studies characterizing the whole body biodistribution of 18F-pretomanid in mouse models of pulmonary TB revealed that the penetration into the brain parenchyma was high, with a median AUC ratio (brain/plasma) of 1.73 (IQR, 1.41–2.04), even in healthy brains. This prompted detailed investigation of 18F-pretomanid penetration into infected brains in two mammalian models of TB meningitis also showing excellent brain penetration of 18F-pretomanid [AUC ratios (brain/plasma) >1]. However, in vivo 3D PET/CT and 2D ex vivo autoradiography in the mouse model of TB meningitis showed reduced uptake of 18F-pretomanid with filling defects at the center of the brain lesion (visible in live animals with 18F-FDG PET/CT and ex vivo histopathology, respectively) (Fig. 3a, b). AUC ratio (brain/plasma) was 1.35 (median; IQR, 0.81–1.52) in brain lesions and 1.56 (median; IQR, 1.22–1.69) in unaffected brain regions (Fig. 3c, d). Similar findings were noted in a rabbit model of TB meningitis (Fig. 3e–h), with median AUC ratio (brain/plasma) of 1.87 (IQR, 1.66–4.63) into brain lesions and 2.75 (IQR, 1.64–5.73) into the unaffected brain.
Fig. 3. Brain penetration of 18F-pretomanid in mouse and rabbit models of TB meningitis.
a–d Mice, n = 8. a Coronal 18F-pretomanid and 18F-FDG PET/CT showing the brain lesion and unaffected brain. b Histopathology and 18F-pretomanid autoradiography of the same mouse brain showing brain lesions (white dotted line) and unaffected brain (black dotted line). c Time-activity curves (TACs) from 0 to 60 min for plasma, brain lesions and unaffected brain. d Area under the curve (AUC) ratios (tissue/plasma) in unaffected brain [n = 15 volume of interests (VOIs)] and brain lesion (n = 15 VOIs) (P = 0.055). Each dot represents a VOI. e–h Rabbits, n = 4. e Coronal 18F-pretomanid and 18F-FDG PET/CT in the same rabbit. f Histopathology and 18F-pretomanid autoradiography of the same rabbit brain showing brain lesions (white dotted line) and unaffected brain (black dotted line). g TAC from 0 to 60 min for plasma, unaffected brain, and brain lesions. h AUC ratio (tissue/plasma) comparing unaffected brain (n = 7 VOIs) and brain lesions (n = 7 VOIs). Each dot represents a VOI. PET studies are based on microdoses (ng-µg) administered intravenously. Data are represented as median ± IQR. Statistical comparisons were made using a two-tailed Mann–Whitney-Wilcoxon test. Source data are provided as a Source Data file.
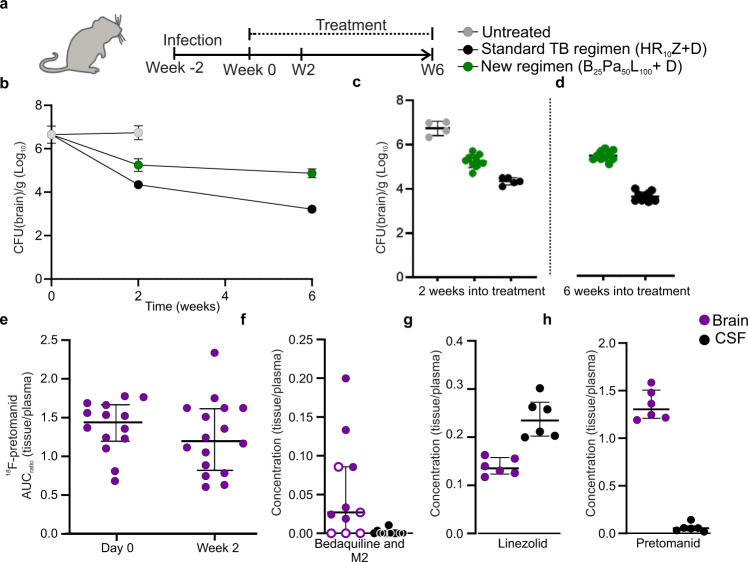
Assessment of the BPaL regimen in the mouse model of TB meningitis
We measured the efficacy of the pretomanid-containing BPaL regimen, currently the only U.S. FDA approved regimen for MDR-TB, in the mouse model of TB meningitis and compared it with the first-line, standard TB treatment (standard-dose rifampin, isoniazid, and pyrazinamide – HR10Z) (Fig. 4a). Adjuvant dexamethasone was administered with both regimens per current TB meningitis treatment guidelines2,24. While both regimens decreased the bacterial burden compared to untreated mice, the bactericidal activity of the BPaL regimen was substantially inferior to the standard TB regimen (P < 0.001) (Fig. 4b–d and Table S2).
Fig. 4. Evaluation of BPaL regimen in the mouse model of TB meningitis.
a After two weeks of infection incubation (week 0), mice were randomly allocated into treatment groups; standard TB regimen (rifampin [R], isoniazid [H] and pyrazinamide [Z]), and a new regimen (BPaL; bedaquiline [B], pretomanid [P] and linezolid [L]). Rifampin (10 mg/kg/day), isoniazid (10 mg/kg/day), pyrazinamide (150 mg/kg/day), pretomanid (50 mg/kg/day divided twice daily), bedaquiline (25 mg/kg/day), and linezolid (100 mg/kg/day divided twice daily) were administered via oral gavage. Mouse dosing was utilized to match the standard human equipotent dosing: rifampin (10 mg/kg/day), isoniazid (10 mg/kg/day), pyrazinamide (25 mg/kg/day), pretomanid (200 mg/day), bedaquiline (standard oral dosing), and linezolid (1200 mg/day). All regimens received adjunctive dexamethasone via intraperitoneal injection. Four mice remained untreated for two weeks. b Bacterial burden over the treatment duration and (c) after two (P = 0.001) and (d) six weeks (P < 0.001) of treatment (animal numbers at two weeks, n = 4/untreated, 5/standard TB regimen, and 10/BPaL; at six weeks n = 10/each group). e 18F-Pretomanid AUC ratios (brain/plasma) in mice with TB meningitis (P = 0.294). PET studies are based on microdoses (ng-µg) administered intravenously. Mass spectrometry-derived brain/plasma (purple dot) or CSF/plasma (black dot) concentration ratios for (f) bedaquiline [and M2 metabolite (open dot)] (P = 0.002), (g) linezolid (P = 0.002) and (h) pretomanid (P = 0.002) (n = 6/group) in mice with TB meningitis, following a single-dose and measured at Tmax. CFU data is represented as mean ± SD on a logarithmic scale. PET and mass spectrometry data are represented as median ± IQR. Statistical comparisons were made using two-tailed Mann–Whitney-Wilcoxon test or a two-way ANOVA followed by Bonferroni’s test. Source data are provided as a Source Data file.
In previous studies18,25, we have reported that the AUC ratios (brain/plasma) of 76Br-bedaquiline and 18F-linezolid (both chemically identical to the parent drugs) into uninfected brain tissues were 0.15 and 0.34 respectively (Fig. S6). However, our current study demonstrated that 18F-pretomanid AUC ratios (brain/plasma) were high (>1.5) at the start of treatment (and remained high (>1) after two weeks of treatment (Fig. 4e). Brain parenchymal and CSF drug and metabolite levels were also measured by mass spectrometry, which demonstrated discordant penetration into the brain parenchyma and CSF compartments (P = 0.002, Fig. 4f–h and Table S3). While linezolid levels were higher in the CSF compared to the brain parenchyma, both pretomanid and bedaquiline levels were higher in the brain parenchyma compared to the CSF. Bedaquiline rapidly undergoes N-demethylation in vivo to form a metabolite (M2), which is also active against M. tuberculosis. We found that M2 levels (albeit still low) were higher in the brain parenchyma than the parent drug (Table S3).
It has been hypothesized that outcomes in TB meningitis are also associated with changes in intracerebral inflammation2,5. Therefore, we also assessed levels for select inflammatory cytokines in brain lysates, which did not show significant differences between the two regimens (Fig. S7).
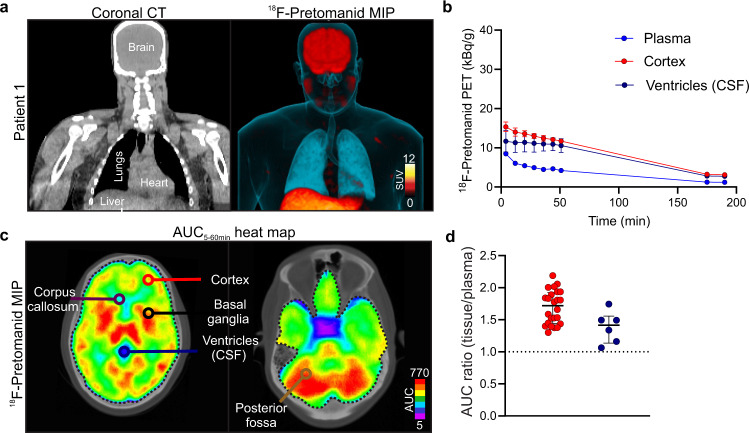
First-in-human 18F-pretomanid PET studies
Six healthy volunteers (three male and three female), with an age range of 20–53 years were recruited in an ongoing first-in-human 18F-pretomanid PET study at the Johns Hopkins Hospital (Table S4). While this study was not designed to assess safety the procedures were safe, no adverse or clinically detectable pharmacological effects were noted and no anatomic abnormalities were detected in any subject. Similar to the animal studies, after intravenous administration, 18F-pretomanid rapidly distributed to all major organs, and underwent both renal and hepatobiliary excretion. Importantly, 18F-pretomanid demonstrated excellent penetration into the brain parenchyma and the CSF, with an AUC (tissue/plasma) ratio >1 (Fig. 5 and Fig. S8). Additionally, and similar to the findings in the animal models, 18F-pretomanid exposures were compartmentalized with significantly lower penetration noted in the CSF (ventricles), compared to the brain parenchyma (Fig. 5; P = 0.018).
Fig. 5. First-in-human 18F-pretomanid PET.
a Coronal CT and 18F-pretomanid PET maximum-intensity projection (MIP) images. b Representative time-activity curves (TACs) from subject 1 in brain parenchyma and CSF (ventricles) using automated segmentation. A total of 45 volume of interests (VOIs) were analyzed from six subjects. Remaining TACs are shown in Fig. S8. c Transverse 18F-pretomanid PET AUC heat maps demonstrating spatially compartmentalized distribution. d AUC4-55min (tissue/plasma) ratios from the cortex and CSF (ventricles) (P = 0.018). PET studies are based on microdoses (ng-µg) administered intravenously from six human subjects. SUV, standard uptake values. Data are represented as median ± IQR. Statistical comparisons were performed using 2-way ANOVA followed by Bonferroni’s multiple-comparison test. Source data are provided as a Source Data file.
Discussion
While optimal drug dosing can shorten current treatment regimens, suboptimal dosing is a major factor promoting antibiotic resistance, which the World Health Organization declared as one of the top ten threats to human health26. Notably, TB meningitis due to MDR strains lacks highly efficacious treatments and is associated with 40% to 100% mortality with current regimens5–7,9. Therefore, there is an urgent need to optimize antibiotic treatments for TB meningitis, especially for those caused by MDR strains.
Pretomanid has been studied for pulmonary TB, and exhibits time-dependent bactericidal activity in the lungs22. However, there is limited data on its penetration into privileged sites such as the CNS2. Additionally, TB treatments can be particularly challenging because of the simultaneous co-existence of heterogeneous lesions with a complex microenvironment in the same host16,17,20,27. For instance, the blood-brain barrier (BBB) limits the access of several antimicrobials into the CNS2,20. Although mass spectrometry studies have demonstrated good CNS penetration of pretomanid in uninfected, healthy rats28, these data provide measures only at a single time point and do not provide detailed spatiotemporal concentration-time measures in infected tissues. In addition to the unique microenvironments at the infection site, the physicochemical properties of specific drugs affect pharmacokinetic (PK) parameters such as drug penetration and clearance29. Our studies demonstrate that pretomanid has excellent penetration into the brain, including infected brain tissues [(brain/plasma) ≥1] in both mice and rabbits. While prior studies have shown that rifampin penetration into the brain decreases dramatically as early as two weeks after initiation of TB treatments17,20, we show that CNS penetration of pretomanid remains high [AUC (tissue/plasma) ratio >1] even after initiation of treatment with dexamethasone-containing regimens, which decreases BBB permeability.
Given the high brain penetration of 18F-pretomanid, we measured the efficacy of the BPaL regimen, currently, the only U.S. FDA approved regimen for MDR-TB, in the mouse model of TB meningitis and compared it with the first-line, standard TB treatment (HR10Z). Adjuvant dexamethasone was administered with both regimens per current TB meningitis treatment guidelines. While the BPaL regimen decreased the bacterial burden in the brain (compared to untreated mice), surprisingly and contrary to what is noted for pulmonary TB30, the bactericidal activity of the BPaL regimen was substantially inferior to the standard TB regimen, even six weeks after treatment initiation.
To understand the lower than expected efficacy of the BPaL regimen, we measured the penetration of each antibiotic into the CNS as single time-point post-mortem levels using mass spectrometry and measured pretomanid AUC in live animals using PET. As noted, pretomanid has excellent penetration into the CNS. However, in previous studies utilizing 18F-linezolid and 76Br-bedaquiline (both chemically identical to the parent drugs)18,25 we have demonstrated that linezolid levels were lower than anticipated based on other published literature31, and bedaquiline levels were substantially lower, but in line with the low CNS levels noted in published studies32,33. Importantly, we also demonstrate discordant antibiotic concentrations in the brain parenchyma and CSF compartments, which are likely influenced by drug properties. For example, linezolid, an oxazolidinone with low protein-binding that was found to be beneficial in retrospective studies for the treatment of TB meningitis34, had substantially higher CSF concentration, but lower levels were achieved in the brain tissues. Conversely, both bedaquiline (and M2 metabolite) as well as pretomanid, which are lipophilic and with higher protein-binding, showed higher concentration in the brain tissue compared with the CSF. This is consistent with differential partitioning of drugs into the protein and lipid rich brain parenchyma versus CSF which is hydrophilic and low in protein. We have noted similar discordance between the CSF and the brain tissue compartments for rifampin and delamanid (also a nitroimidazole, with physiolochemical properties similar to pretomanid) levels17,20,35, and markers of inflammation20. The current studies extend this concept demonstrating that drug properties also influence discordant penetration into the CNS.
The ability to perform cross-species and translational clinical studies with 18F-pretomanid PET is a major advantage of this technology. Therefore, we developed a cGMP-compliant radiosynthesis scheme for 18F-pretomanid to facilitate clinical translation and perform first-in-human imaging studies. First-in-human, dynamic 18F-pretomanid PET in healthy controls confirmed the excellent but heterogenous brain penetration visualized in our mammalian models of TB meningitis, validating 18F-pretomanid PET as a powerful translational tool in drug development and treatment optimization. Additionally, the 18F-pretomanid PET signal in the CSF (brain ventricles), was significantly lower than in other regions of the brain parenchyma. These results confirm compartmentalized and discordant antibiotic penetration into the CNS and highlight the importance of using animal models and imaging technology in humans that can measure antibiotic exposures in the brain parenchyma as well as the CSF.
Our studies have some limitations which we aimed to overcome. Since even minor modifications in the chemical structure of antimicrobials can lead to drastic changes in the physicochemical properties and biological activity of small molecule drugs, we developed a radiosynthetic approach using radiofluorination chemistry that retains the chemical identity of pretomanid. Additionally, the PET studies administered microdoses (ng-µg) of 18F-pretomanid per subject for the PET studies and current evidence suggests that microdosing is a reliable predictor of the drug biodistribution at therapeutic doses36,37. Another limitation of the study is that mass spectrometry drug levels were measured at Tmax (time to reach maximum concentration) and represent a single time point, and not time-concentration curves (AUC) as measured by PET. This difference in measurement could explain why the brain/plasma ratios were found to be higher by mass spectrometry compared to PET-derived AUC ratios. Moreover, since 18F-pretomanid is administered intravenously, the time of injection corresponds to plasma Tmax, and brain uptake reaches Cmax (maximum concentration) within the first 15 min. Therefore, the first 60 min represent the maximum concentration of 18F-pretomanid to reach the brain. While rabbit studies utilized both males and females, only female mice were used, and future studies with both males and females would be required to investigate how gender may affect pretomanid PK. Finally, while the reduced penetration of linezolid and bedaquiline into the brain parenchyma are a likely cause of the reduced efficacy of the BPaL regimen compared to standard TB therapy (HR10Z), other factors may be considered, and further research is needed. For example, it is possible that bacteria in this model are more susceptible to HR10Z due to the effect of isoniazid against fast-replicating bacteria. Furthermore, a dose-escalating study would be useful to assess if increased doses of linezolid and/or bedaquiline might improve outcomes, as we previously observed with high-dose rifampin. In this case however, safety concerns regarding higher doses of linezolid and bedaquiline could be limiting, and analogs could be tested instead.
Here we show the value added by imaging technologies for the characterization of novel drugs and treatment optimization. The use of radiolabeled antimicrobials, combined with conventional microbiology techniques and novel animal models, offers unmatched potential to noninvasively assess PK profiles in infected tissues, characterized by complex, heterogeneous lesions existing simultaneously in the same host27. Importantly, our studies demonstrate that pretomanid has excellent penetration into the CNS, confirmed in first-in-human 18F-pretomanid studies, suggesting that novel pretomanid-based regimens in combination with other antibiotics active against MDR strains and with excellent brain penetration should be considered for the treatment of MDR-TB meningitis. Finally, our studies reaffirm the compartmentalized and discordant antibiotic penetration into the CNS, which are related to the physiochemical properties of the antibiotic. Overall, this is an important finding as CSF studies are commonly utilized in many clinical trials, but CSF may not be an adequate surrogate of disease or drug levels in the brain tissues.
Methods
Study design
The overall goal of this study was to develop radiolabeled-pretomanid for dynamic, concentration-time profiles using PET to characterize pretomanid brain PK (in animal and human studies) and assess the efficacy of a pretomanid-containing regimen for TB meningitis. We performed cross-species analyses for preclinical validation of 18F-pretomanid as a molecular imaging tool to noninvasively assess whole-body drug penetration and then optimized the radiosynthesis of 18F-pretomanid under cGMP to facilitate the execution of first-in-human studies. Dynamic 18F-pretomanid PET/CT was used to obtain TACs and AUCs by quantifying the PET signal in VOIs in animal models and human studies. In animal models, post-mortem autoradiography/histology and mass spectrometry were also performed to characterize pretomanid’s heterogenous brain penetration, both spatially and temporally. Given the unknown potential of pretomanid-containing regimens for TB meningitis, BPaL, the only FDA approved pretomanid-containing regimen, was tested in the mouse model of TB meningitis to evaluate intraparenchymal drug levels and bactericidal activity longitudinally. All protocols were approved by the Johns Hopkins University Biosafety, Radiation Safety, Animal Care and Use (RB19M417, MO19M382) and Institutional Review Board Committees (IRB00303845). 18F-Pretomanid was used according to the FDA Radioactive Drug Research Committee guidelines for investigational drugs.
Radiosynthesis of 18F-pretomanid
Radiosynthesis of 18F-pretomanid was first developed as a manual synthesis using silver-catalyzed nucleophilic displacement for preclinical animal studies. For clinical translation, the radiosynthesis was adapted to an automated cGMP synthesis of 18F-pretomanid under microwave irradiation in dimethylformamide in the absence of silver salts. Details of the synthesis of 18F-pretomanid, including the radiolabeling precursor and intermediates and in vitro characterization of 18F-pretomanid, is available in supplementary materials.
Animal studies
Mouse model of pulmonary TB
Four to six-week-old female C3HeB/FeJ mice (Jackson Laboratory) were aerosol-infected with frozen stocks of M. tuberculosis (H37Rv), using the Middlebrook Inhalation Exposure System (Glas-Col)38.
Mouse model of TB meningitis
Female C3HeB/FeJ mice (7–8 weeks old, Jackson laboratories) were infected intraventricularly (titrated frozen stocks with ~6.5 log10 CFU of M. tuberculosis H37Rv) via a burr hole using a Hamilton syringe (Hamilton, 88,000) and stereotaxic instrument (David KOPF instrument, model 900, coordinates 0.6 mm dorsal to bregma, 1.2 mm lateral to middle line and 2 mm ventral)20. The infection was allowed to incubate for 14 days.
Rabbit model of TB meningitis
Male and female New Zealand White rabbits (5–7 day old, Robinson Services Inc.) were infected intraventricularly (titrated frozen stock with ~6.5 log10 of M. tuberculosis H37Rv) via the bregma using a 30-gauge insulin syringe. Prior to infection, rabbits were sedated with dexmedetomidine hydrochloride (0.2 µg/g; Zoetis, Florham Park, NJ) and topical anesthesia (lidocaine 4%; Ferndale IP Inc., Ferndale, MI) was applied to the bregma17,19,20. The infection was allowed to incubate for at least 14 days before imaging was performed.
Ethical approval
All the animal experiments in this study were approved by the Johns Hopkins University Animal Care and Use Committee.
Ex vivo biodistribution
Anesthetized mice (n = 4 per time point) were injected with 18F-pretomanid (2.6 ± 1.9 MBq) via the tail vein and sacrificed 1, 2, and 4 h post-injection. Organs and tissues of interest were harvested, weighed, and the radioactivity gamma-counted. Data are represented as percent injected dose per weight of tissue (%ID/g).
Autoradiography
Following intravenous injection of 18F-pretomanid, animals were sacrificed, perfused with saline, and brains collected. Tissues were embedded in OCT and 20 µm sections placed on slides. The radioactive slides were placed inside an exposure cassette (GE, code no. 29175523) and exposed for 2–5 half-lives before being developed by phosphor storage imaging (GE Typhoon). Following radioactive decay, the tissues used for autoradiography were fixed in formalin and underwent hematoxylin and eosin staining.
Antimicrobial treatments and efficacy
Drug stocks were prepared and administered five days a week as previously described30,39. Rifampin (10 mg/kg/day), isoniazid (10 mg/kg/day), pyrazinamide (150 mg/kg/day), pretomanid (50 mg/kg/day divided twice daily), bedaquiline (25 mg/kg/day), and linezolid (100 mg/kg/day divided twice daily) were prepared for oral administration via gavage and dexamethasone was prepared for intraperitoneal injection and stored at 4 °C. Mouse dosing was utilized to match the standard human equipotent dosing: rifampin (10 mg/kg/day), isoniazid (10 mg/kg/day), pyrazinamide (25 mg/kg/day), pretomanid (200 mg/day)40, bedaquiline (standard oral dosing)41, and linezolid (1200 mg/day)42. Treatment efficacy was determined by whole brain bacterial burden (CFU) at 2 and 6 weeks after initiation of treatment using 7H11 plates supplemented with activated charcoal.
Imaging
M. tuberculosis-infected mice and rabbits were imaged inside transparent and sealed biocontainment containers, compliant with biosafety level (BSL)-3 containment and capable of delivering O2-anesthetic mixture to sustain live animals during imaging as previously described43. PET acquisition and subsequent CT were performed using the nanoScan PET/CT (Mediso, Arlington, VA) and images automatically co-registered. 18F-Pretomanid PET/CT: Mice were injected with 18F-pretomanid (pulmonary TB, 3.77 ± 1.78 MBq; TB meningitis, 3.88 ± 1.44 MBq) via the tail vein. Anesthetized rabbits were injected with 18F-pretomanid (4.65 ± 0.75 MBq) through the ear vein. The injection time coincided with the start of the dynamic PET acquisition. 18F-FDG PET/CT: Animals were imaged as previously described20.
Mass spectrometry
Terminal samples (blood, brain and CSF) were collected at the appropriate plasma Tmax for each antimicrobial44–46. Blood was collected in EDTA tubes (BD Microtainer, Fisher Scientific) for plasma separation. Bedaquiline, bedaquiline M2 metabolite, pretomanid and linezolid in plasma, CSF and brain tissues from M. tuberculosis-infected mice were quantified using validated ultra-high-performance liquid chromatography (UPLC) and tandem mass spectrometry (LC–MS/MS) at the Infectious Diseases Pharmacokinetics Laboratory of the University of Florida. Calibration standard curves ranges were bedaquiline (and M2 metabolite) 2.00 to 0.01 µg/mL, pretomanid 30.00 to 0.01 µg/mL, and linezolid 30.00 to 0.03 µg/mL.
Cytokine analysis
Samples for cytokine analysis were collected from supernatants after centrifuged brain homogenization and stored at −80 °C until analysis. IL-1α, vascular endothelial growth factor A (VEGFA) and matrix metalloproteinase-8 (MMP-8) were analyzed on Luminex Multiplex assays by the Oncology Human Immunology Core of Johns Hopkins University.
Human studies
18F-Pretomanid was synthesized as a sterile solution with high specific activity (40.27 ± 12.82 GBq/µmol) and high radiochemical purity (>95%) using cGMP by the Johns Hopkins PET Radiotracer Center. Written informed consent was obtained from all healthy volunteers and deidentified images were analyzed. All subjects had a physical exam by a trained physician and screening laboratory tests before imaging to confirm eligibility. Each subject received an intravenous bolus of 359.52 ± 2.79 MBq of 18F-pretomanid followed by dynamic PET utilizing a multi-bed protocol immediately after tracer injection (0–60 min) and 180 min after tracer injection (180–210 min) using Siemens Biograph mCT 128-slice scanner. All subjects were assessed for adverse events immediately after the completion of the imaging studies and via a follow up telephone interview at 20–25 days after the imaging studies. A trained radiologist also evaluated the CT images for all subjects to assess for any anatomic abnormalities.
Image analysis
PET/CT images were analyzed using VivoQuant 2020 (Invicro) or PMOD (3.402) for animal and human studies, respectively. In humans, the brain segmentation tool (Hammers N30R83) was used to draw VOIs and OsiriX MD 11.0 DICOM Viewer (Pixmeo SARL) was used to create 3D MIP images. Data for blood were obtained by placing a VOI in the left heart ventricle and then correcting to plasma using individual subject hematocrit values or standard hematocrit47 and red blood cell partition coefficient of pretomanid48 (Table S5). PET data were adjusted for mass using the density of each organ obtained from the CT (Hounsfield units). Data are expressed as %ID/g or standard uptake values (SUV) in animal or human studies, respectively. Heatmap overlays were created using RStudio.
Statistical analysis
Data were analyzed using Prism 8 version 8.1.0 (GraphPad). AUCs were calculated using the linear trapezoidal rule. Comparisons were made using a two-tailed, Mann–Whitney-Wilcoxon test or ANOVA followed by Bonferroni’s multiple-comparison test. P values ≤ 0.05 were considered statistically significant.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Acknowledgements
The authors would like to thank Eric Nuermberger (Johns Hopkins Hospitals) for assistance with antibiotic dosing, Mariah Klunk for assistance with PET/CT imaging, and Axia Chemicals Ltd. for developing the precursor for 18F-pretomanid. We also want to thank all the study subjects as well as Amanda Henderson, Ergi Spiro and Jeff Leal (Johns Hopkins Hospitals) for help with recruiting the human subjects and curating the human imaging data respectively. Funding: This work was funded by the US National Institutes of Health R01-AI145435-A1 (S.K.J.), R01-AI153349 (S.K.J.), R01-HL131829 (S.K.J.), R21- AI149760 (S.K.J.), and K08-AI139371 (E.W.T.).
Source data
Author contributions
F.M., C.A.R.-B. and S.K.J. conceptualized and designed the studies. F.M. and P.D.J. performed the manual radiosyntheses. D.P.H. and R.F.D. developed the cGMP synthesis. F.M., C.A.R.-B., P.D.J., M.B. and K.F. performed the mouse studies. X.C. performed the cytokine analysis. F.M., C.E., J.K. and E.W.T. performed the rabbit studies. E.W.T. supervised the rabbit studies. A.A.O. and S.K.J. wrote the protocol for the human studies. A.A.O., C.A.R.-B., E.W.T. and M.K.B. recruited and consented the human subjects and analyzed the human imaging data. C.A.P. performed mass spectrometry analysis. S.K.J. provided funding and supervised the project. F.M., C.A.R.-B., E.W.T. and S.K.J. wrote the manuscript with substantial input from all co-authors.
Peer review
Peer review information
Nature Communications thanks the other anonymous reviewer(s) for their contribution to the peer review of this work. Peer review reports are available.
Data availability
All data are available in the main text or the supplementary materials. Source data are provided with this paper.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Filipa Mota, Camilo A. Ruiz-Bedoya, Elizabeth W. Tucker, Daniel P. Holt.
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-022-35730-3.
References
- 1.WHO. Global tuberculosis report. Geneva: World Health Organization (2022).
- 2.Jain SK, et al. Tuberculous meningitis: a roadmap for advancing basic and translational research. Nat. Immunol. 2018;19:521–525. doi: 10.1038/s41590-018-0119-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilkinson RJ, et al. Tuberculous meningitis. Nat. Rev. Neurol. 2017;13:581–598. doi: 10.1038/nrneurol.2017.120. [DOI] [PubMed] [Google Scholar]
- 4.Chiang SS, et al. Treatment outcomes of childhood tuberculous meningitis: a systematic review and meta-analysis. Lancet Infect. Dis. 2014;14:947–957. doi: 10.1016/S1473-3099(14)70852-7. [DOI] [PubMed] [Google Scholar]
- 5.Thwaites GE, et al. Effect of antituberculosis drug resistance on response to treatment and outcome in adults with tuberculous meningitis. J. Infect. Dis. 2005;192:79–88. doi: 10.1086/430616. [DOI] [PubMed] [Google Scholar]
- 6.Senbayrak S, et al. Antituberculosis drug resistance patterns in adults with tuberculous meningitis: results of haydarpasa-iv study. Ann. Clin. Microbiol Antimicrob. 2015;14:47. doi: 10.1186/s12941-015-0107-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vinnard C, et al. Long-term mortality of patients with tuberculous meningitis in New York City: a cohort study. Clin. Infect. Dis. 2017;64:401–407. doi: 10.1093/cid/ciw763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heemskerk AD, et al. Clinical outcomes of patients with drug-resistant tuberculous meningitis treated with an intensified antituberculosis regimen. Clin. Infect. Dis. 2017;65:20–28. doi: 10.1093/cid/cix230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Evans EE, et al. Long term outcomes of patients with tuberculous meningitis: the impact of drug resistance. PLoS One. 2022;17:e0270201. doi: 10.1371/journal.pone.0270201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Keam SJ. Pretomanid: first approval. Drugs. 2019;79:1797–1803. doi: 10.1007/s40265-019-01207-9. [DOI] [PubMed] [Google Scholar]
- 11.Stover CK, et al. A small-molecule nitroimidazopyran drug candidate for the treatment of tuberculosis. Nature. 2000;405:962–966. doi: 10.1038/35016103. [DOI] [PubMed] [Google Scholar]
- 12.Singh R, et al. PA-824 kills nonreplicating Mycobacterium tuberculosis by intracellular NO release. Science. 2008;322:1392–1395. doi: 10.1126/science.1164571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dogra M, et al. Comparative bioactivation of the novel anti-tuberculosis agent PA-824 in mycobacteria and a subcellular fraction of human liver. Br. J. Pharm. 2011;162:226–236. doi: 10.1111/j.1476-5381.2010.01040.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lenaerts AJ, et al. Preclinical testing of the nitroimidazopyran PA-824 for activity against mycobacterium tuberculosis in a series of in vitro and in vivo models. Antimicrob. Agents Chemother. 2005;49:2294–2301. doi: 10.1128/AAC.49.6.2294-2301.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muller M, dela Pena A, Derendorf H. Issues in pharmacokinetics and pharmacodynamics of anti-infective agents: distribution in tissue. Antimicrob. Agents Chemother. 2004;48:1441–1453. doi: 10.1128/AAC.48.5.1441-1453.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ordonez AA, et al. Dynamic imaging in patients with tuberculosis reveals heterogeneous drug exposures in pulmonary lesions. Nat. Med. 2020;26:529–534. doi: 10.1038/s41591-020-0770-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tucker EW, et al. Noninvasive (11)C-rifampin positron emission tomography reveals drug biodistribution in tuberculous meningitis. Sci. Transl. Med. 2018;10:eaau0965. doi: 10.1126/scitranslmed.aau0965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mota F, et al. Radiosynthesis and biodistribution of (18)F-Linezolid in mycobacterium tuberculosis-infected mice using positron emission tomography. ACS Infect. Dis. 2020;6:916–921. doi: 10.1021/acsinfecdis.9b00473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tucker EW, et al. Microglia activation in a pediatric rabbit model of tuberculous meningitis. Dis. Model Mech. 2016;9:1497–1506. doi: 10.1242/dmm.027326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ruiz-Bedoya, C. A. et al. High-dose rifampin improves bactericidal activity without increased intracerebral inflammation in animal models of tuberculous meningitis. J. Clin. Invest.132, 1–11 (2022). [DOI] [PMC free article] [PubMed]
- 21.Khotavivattana T, et al. 18F‐Labeling of Aryl‐SCF3,‐OCF3 and‐OCHF2 with [18F] Fluoride. Angew. Chem. 2015;127:10129–10133. doi: 10.1002/ange.201504665. [DOI] [PubMed] [Google Scholar]
- 22.Ahmad Z, et al. PA-824 exhibits time-dependent activity in a murine model of tuberculosis. Antimicrob. Agents Chemother. 2011;55:239–245. doi: 10.1128/AAC.00849-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.European Medicines Agency. Pretomanid FGK, Assessment report. European Medicines Agency (2020).
- 24.Thwaites GE, et al. Dexamethasone for the treatment of tuberculous meningitis in adolescents and adults. N. Engl. J. Med. 2004;351:1741–1751. doi: 10.1056/NEJMoa040573. [DOI] [PubMed] [Google Scholar]
- 25.Ordonez AA, et al. Radiosynthesis and PET bioimaging of (76)Br-bedaquiline in a murine model of tuberculosis. ACS Infect. Dis. 2019;5:1996–2002. doi: 10.1021/acsinfecdis.9b00207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.WHO. Ten threats to global health. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (2019).
- 27.Ordonez, A. A. et al. Visualizing the dynamics of tuberculosis pathology using molecular imaging. J. Clin. Invest.131, 1–11 (2021). [DOI] [PMC free article] [PubMed]
- 28.Bratkowska D, et al. Determination of the antitubercular drug PA-824 in rat plasma, lung and brain tissues by liquid chromatography tandem mass spectrometry: application to a pharmacokinetic study. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2015;988:187–194. doi: 10.1016/j.jchromb.2015.02.041. [DOI] [PubMed] [Google Scholar]
- 29.Bjarnsholt T, et al. The importance of understanding the infectious microenvironment. Lancet Infect. Dis. 2022;22:e88–e92. doi: 10.1016/S1473-3099(21)00122-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xu, J. et al. Contribution of pretomanid to novel regimens containing bedaquiline with either linezolid or moxifloxacin and pyrazinamide in murine models of tuberculosis. Antimicrob. Agents Chemother.63, 1–14 (2019). [DOI] [PMC free article] [PubMed]
- 31.Beer R, et al. Pharmacokinetics of intravenous linezolid in cerebrospinal fluid and plasma in neurointensive care patients with staphylococcal ventriculitis associated with external ventricular drains. Antimicrob. Agents Chemother. 2007;51:379–382. doi: 10.1128/AAC.00515-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Akkerman OW, et al. Pharmacokinetics of bedaquiline in cerebrospinal fluid and serum in multidrug-resistant tuberculous meningitis. Clin. Infect. Dis. 2016;62:523–524. doi: 10.1093/cid/civ921. [DOI] [PubMed] [Google Scholar]
- 33.Upton CM, et al. Pharmacokinetics of bedaquiline in cerebrospinal fluid (CSF) in patients with pulmonary tuberculosis (TB) J. Antimicrob. Chemother. 2022;77:1720–1724. doi: 10.1093/jac/dkac067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sun F, et al. Linezolid manifests a rapid and dramatic therapeutic effect for patients with life-threatening tuberculous meningitis. Antimicrob. Agents Chemother. 2014;58:6297–6301. doi: 10.1128/AAC.02784-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tucker, E. W. et al. Delamanid central nervous system pharmacokinetics in tuberculous meningitis in rabbits and humans. Antimicrob. Agents Chemother.63, 1–11 (2019). [DOI] [PMC free article] [PubMed]
- 36.Lappin G, Noveck R, Burt T. Microdosing and drug development: past, present and future. Expert Opin. Drug Metab. Toxicol. 2013;9:817–834. doi: 10.1517/17425255.2013.786042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burt T, et al. Phase 0/microdosing approaches: time for mainstream application in drug development? Nat. Rev. Drug Disco. 2020;19:801–818. doi: 10.1038/s41573-020-0080-x. [DOI] [PubMed] [Google Scholar]
- 38.Weinstein EA, et al. Noninvasive determination of 2-[18F]-fluoroisonicotinic acid hydrazide pharmacokinetics by positron emission tomography in Mycobacterium tuberculosis-infected mice. Antimicrob. Agents Chemother. 2012;56:6284–6290. doi: 10.1128/AAC.01644-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosenthal IM, et al. Dose-ranging comparison of rifampin and rifapentine in two pathologically distinct murine models of tuberculosis. Antimicrob. Agents Chemother. 2012;56:4331–4340. doi: 10.1128/AAC.00912-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bigelow, K. M., Tasneen, R., Chang, Y. S., Dooley, K. E. & Nuermberger, E. L. Preserved efficacy and reduced toxicity with intermittent linezolid dosing in combination with bedaquiline and pretomanid in a murine tuberculosis model. Antimicrob. Agents Chemother.64, 1–13 (2020). [DOI] [PMC free article] [PubMed]
- 41.Andries K, et al. A diarylquinoline drug active on the ATP synthase of Mycobacterium tuberculosis. Science. 2005;307:223–227. doi: 10.1126/science.1106753. [DOI] [PubMed] [Google Scholar]
- 42.Tasneen R, et al. Contribution of oxazolidinones to the efficacy of novel regimens containing bedaquiline and pretomanid in a mouse model of tuberculosis. Antimicrob. Agents Chemother. 2016;60:270–277. doi: 10.1128/AAC.01691-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ordonez AA, et al. Radioiodinated DPA-713 imaging correlates with bactericidal activity of tuberculosis treatments in mice. Antimicrob. Agents Chemother. 2015;59:642–649. doi: 10.1128/AAC.04180-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Irwin SM, et al. Bedaquiline and pyrazinamide treatment responses are affected by pulmonary lesion heterogeneity in mycobacterium tuberculosis infected C3HeB/FeJ Mice. ACS Infect. Dis. 2016;2:251–267. doi: 10.1021/acsinfecdis.5b00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nuermberger E, et al. Combination chemotherapy with the nitroimidazopyran PA-824 and first-line drugs in a murine model of tuberculosis. Antimicrob. Agents Chemother. 2006;50:2621–2625. doi: 10.1128/AAC.00451-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bigelow KM, et al. Pharmacodynamic correlates of linezolid activity and toxicity in murine models of tuberculosis. J. Infect. Dis. 2021;223:1855–1864. doi: 10.1093/infdis/jiaa016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.O’Connell KE, et al. Practical murine hematopathology: a comparative review and implications for research. Comp. Med. 2015;65:96–113. [PMC free article] [PubMed] [Google Scholar]
- 48.Stancil SL, Mirzayev F, Abdel-Rahman SM. Profiling pretomanid as a therapeutic option for TB infection: evidence to date. Drug Des. Dev. Ther. 2021;15:2815–2830. doi: 10.2147/DDDT.S281639. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are available in the main text or the supplementary materials. Source data are provided with this paper.