Abstract
Background
In primigravidas, childbirth, although physiological can be a frightening event. Two factors that accompany labor are anxiety and pain. This study aims to investigate the benefits of Iyengar yoga for anxiety and labor pain in primigravida women.
Material and methods
The study involved 59 female primigravida subjects, which were divided into 29 controls (without the provision of yoga exercises) and 30 people who received Iyengar yoga exercise. Anxiety and the degree of labor pain will be measured using the Hamilton Scale Rating for Anxiety (HSRA) and visual analog scale (VAS), respectively.
Results
Iyengar yoga significantly reduced VAS and HARS values compared to controls (p < 0.05).
Conclusion
It was concluded that Iyengar yoga in primigravida women was beneficial in reducing labor pain and anxiety. Thus, the Iyengar yoga technique can be a method for supporting the success and safety of labor.
Keywords: Pregnancy, Childbirth, Complementary medicine, VAS, HARS
Abbreviations: ACC, Anterior cingulate cortex; HRSA, Hamilton scale rating for anxiety; VAS, Visual analog scale
Graphical abstract
Highlights
-
•
A study on primigravida pregnancy.
-
•
Iyengar yoga for anxiety and labor pain.
-
•
Iyengar Yoga significantly reduced pain.
-
•
Iyengar Yoga significantly reduced anxiety.
1. Introduction
Primigravida is a woman who is pregnant for the first time or has been pregnant once. Physiological symptoms of pregnant women in seeking a general practitioner include nausea, vomiting, pelvic cavity pain, and back pain. These symptoms can appear simultaneously, even triggering anxiety in primigravida [1]. Anxiety during pregnancy triggers an increase in nausea and vomiting [2,3]. Epidemiologically, anxiety disorders occur in 15–50% of pregnant women and may have an impact on mothers and children born [4,5]. Anxiety disorders will determine the type of delivery chosen [6]. Previous studies have stated that anxiety tends to decrease in multigravida women [7].
In addition to anxiety, labor pain as a result of cervical dilatation and uterine contractions will gradually increased in intensity in the partum period [8]. Although physiologically valuable, the extreme degree of pain will trigger changes in cardiopulmonary function, neuroendocrine response, changes in acid-base blood, and uterine contractility. This pain can affect postpartum conditions and events [[9], [10], [11]]. Efforts to suppress labor pain have become one method of making labor safer. Some attempts include analgesics and epidural analgesia, but there are still side effects and are expensive [[12], [13], [14]].
Yoga is an ancient complementary technique that has become popular in the world. Yoga is practiced regularly for several purposes, such as to increase energy, increase immune function, improve health, and prevent disease [15]. The safety of yoga in the first trimester of pregnancy has been demonstrated in a previous study [16]. Yoga exercises are more effective than walking exercises or prenatal standard exercises because Yoga intervention decreases incidences of prenatal disorders, small gestational age, pain and stress [17]. Yoga is recommended for the management of pregnancy-related low back pain and pelvic pain [18,19]. However, its benefits are not yet known for labor pain.
Iyengar yoga is a type of Hatha yoga, originally developed by Iyengar. Iyengar yoga's focus is on strength, balance, breathing, and alignment of body postures [20]. This yoga technique provides the opportunity to use additional tools (such as chairs or wood) to help balance and stretch. This is easy to apply at all ages and fitness levels and is suitable for beginners [21]. Previous studies have shown that Iyengar yoga can reduce low back pain and pediatric pain [[22], [23], [24], [25]]. Iyengar yoga can also suppress depressive symptoms [26]. A study into the benefits of Iyengar yoga in suppressing pain and anxiety is still limited to the non-pregnant population or other diseases, none of which has been applied to primigravida women. Therefore, this study aims to investigate the benefits of Iyengar yoga for anxiety and pain in primigravida labor.
2. Material and methods
2.1. Subjects
This study was true experimental design with a post-test only control group. This study's patients were primigravida women in their third trimester who were separated into two study groups: the control group and the yoga group. The inclusion criteria for this study were age 20–35 years, primigravida, gestational age of 30 weeks, and with no prior yoga experience [27], and no analgesic treatment in labor. Exclusion criteria included women with multiple pregnancies, having medical limitations on exercise, using analgesics, and participating in other physical exercises. The setting of this study was private practice midwifery in Bantul Region, Special Region of Yogyakarta, Indonesia.
The sample size was calculated based on the change in anxiety level from a prior study in which 29 postpartum women were randomly assigned to yoga or a control group and demonstrated significant reduction in anxiety level [28]. Considering dropout rate of 10%, each group had a minimum of 32 subjects.
2.2. Iyengar yoga
Iyengar exercise was adopted and modified from previous studies [29]. Modified Iyengar yoga exercises were given to pregnant women in exercise classes led by certified yoga instructors with pre-natal gentle Yoga qualification. The practice of yoga was done once a week; the duration of the exercise is 90 min each time. The total duration of training was twelve weeks (three months). Previous studies found yoga to be recommended for low-risk women during pregnancy [30]. Besides, regular and long-term Hatha yoga exercise (90 min per week, for 8 weeks) was able to reduce perceived stress [31]. The details of the yoga exercise are shown in Fig. 1 and Table 1.
Fig. 1.
The details step of Yoga exercise.
Table 1.
The goal and details about Modified Iyengar yoga exercise.
| Type of position | Goal | Details of exercise |
|---|---|---|
| CAT-COW POSE | This exercise has several goals, including reducing baby's pressure on the spine, optimizing baby's occiput posterior to occiput anterior, relaxing the spine, helping balance the pelvis, and strengthening the uterine support muscles and uterus. | Take a table pose position. Looking towards the front, open the chest and extend the back. Arch your back, look towards your stomach. Keep your hands in a straight position. Put the pelvis down, tighten the abdominal muscles. |
| CHILD-POSE | This step has several goals: relaxing the body, reducing pressure on the spine so that it is comfortable for the spine, and opening the pelvic cavity. | Take a table pose. Open your knees as wide as the mat and bring the backs of your feet together. Place the buttocks on the heels. On inspiration, raise both hands up and stretch the spine. When exhaling, fold the body forward and then head to the mattress or block. In the holding position, lengthen the spine by pulling the hands upwards while continuing to breathe. On inspiration, raise both hands up along with the body. When expiration lowers both hands. |
| ADHO-MUKA SVANASANA | This exercise has several goals, including helping breech babies to head position, stretching hamstrings, calves, heels, and hands, preventing twisting of the umbilical cord, and optimizing the baby from occiput posterior to occiput anterior. | Take a table pose position. On inspiration, look forward, open the chest and extend the back. On expiration, lift the pelvis up, extend the spine and align the ears with the arms. When holding, then keep breathing. When exhaling, return to the table pose. |
| SAVASANA | The goal of this study is to relax the body to boost the mood | Take a left side sleeping position. Straighten the left leg and slightly bend the right leg. Relax the body by regulating the breath. |
The subjects were assisted in adopting the sequence of poses and using selected breathing techniques. The exercise sequence included standing poses, front extension, inversion, backbend, and bends. Assistance can include props according to individual needs. Subjects start with a simplified version and progress to a more advanced version. Subjects were prohibited from taking sports classes or practicing yoga outside the classroom. We conducted interviews about pregnancy and exercises before and after yoga practice.
2.3. Measurement of the degree of pain
Measurement of the degree of pain was done using a visual analog scale [32].
2.4. Measuring the degree of anxiety
Degree of anxiety was measured using the Hamilton Scale Rating for Anxiety (HSRA) method [33,34]. Each of the 14 items was graded from 0 to 4, with 4 being the most severe. The overall score varies between 0 and 56. A score of 17 suggests mild anxiety, a score of 18–24 indicates mild to moderate anxiety, and a score of 25–30 indicates moderate to severe anxiety.
2.5. Ethics
This study was approved by the ethics committee of the Faculty of Health Sciences, Achmad Yani University, Yogyakarta, Indonesia (Number SKep/031/KEPK/IV/2019).
2.6. Statistical analysis
The pain and anxiety levels from each group were recorded and expressed as mean standard deviation. The t-student test was used to check if there were any significant differences in pain and anxiety levels between the control and yoga groups. All p values < 0.05 was considered to be statistically significant.
3. Results
The level of education, working status, and frequency of antenatal care are shown in Table 2.
Table 2.
The level of education, working status, and antenatal care in all subjects.
| Characteristics | Category | Group |
p value∗ | |
|---|---|---|---|---|
| Control group (n = 29) | Yoga group (n = 30) | |||
| Level of education | Senior high school | 3 (10.34%) | 5 (16.66%) | 0.2732 |
| Diploma/bachelor | 16 (55.17%) | 20 (66.68%) | ||
| Master | 10 (34.48%) | 5 (16.66%) | ||
| Working status | Non-working | 16 (55.18%) | 21 (70.00%) | 0.2390 |
| Working | 13 (44.82%) | 9 (30.00%) | ||
| Antenatal care | 5–10 | 14 (48.28%) | 17 (56.67%) | 0.5187 |
| >10 | 15 (51.72%) | 13 (43.33%) | ||
Note: ∗Chi-square test.
Table 3 shows the characteristics of pregnancy outcome. There was no statistically significant variations in age between the two study groups (p > 0.05). All of the subjects had normal vaginal delivery. There were no postpartum complications for the mother and baby. Yoga did not result in a significant difference in weight of the baby when compared to the control group (p > 0.05).
Table 3.
The characteristics of age and pregnancy outcome.
| Control group (N = 29) | Yoga group (N = 30) | p value | |
|---|---|---|---|
| Age (years) | 27.827 ± 2.713 | 27.266 ± 2.377 | p > 0.05 |
| Vaginal delivery (%) | 29 (100%) | 30 (100%) | p > 0.05 |
| Postpartum complications | None | None | p > 0.05 |
| Baby weight (gram) | 3040.862 ± 138.667 | 3051.333 ± 100.609 | p > 0.05 |
xx
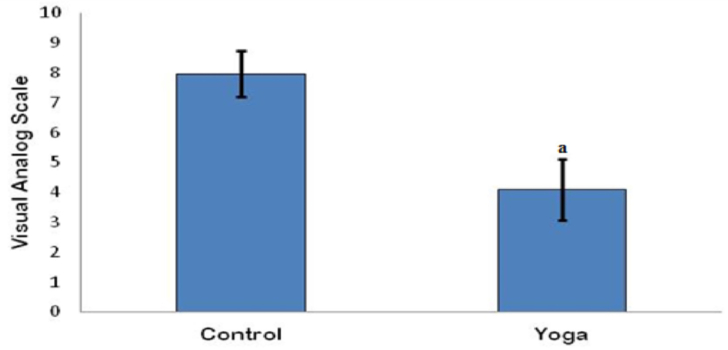
The visual analog score scores between the two study groups is shown in Fig. 2. The visual analog analog scores in the Yoga group was significantly lower than the control group (p < 0.05).
Fig. 2.
The visual analog scale in the control and Yoga group. Note: data presented as mean ± standard of deviation; a: p < 0.05 when compared to the control group.
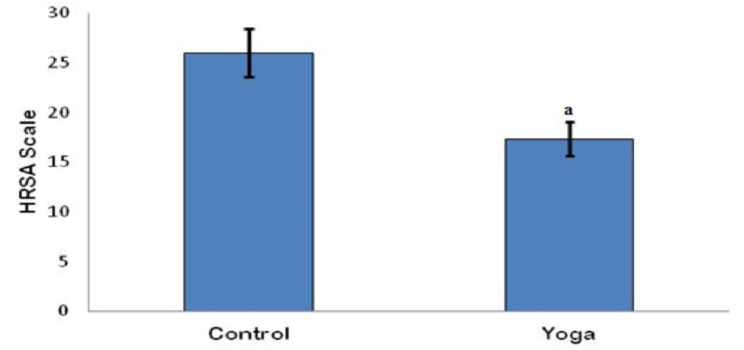
The HARS scores for the two study groups are shown in Fig. 3. The Yoga group's HARS score was significantly lower than that of the control group's (p < 0.05).
Fig. 3.
The visual analog scale in the control and Yoga group. Note: data presented as mean ± standard of deviation; a: p < 0.05 when compared to the control group.
4. Discussion
This study aimed to investigate the benefits of Modified Iyengar yoga in suppressing labor pain and anxiety. It involved 59 female primigravida subjects, divided into 29 controls (without training) and 30 people who received the Modified Iyengar yoga training. There was no age difference between the two groups. In addition, all subjects had normal vaginal delivery, normal baby weight, and no postpartum complications. Our finding is consistent with previous studies that found yoga was acceptable for young pregnant women [[35], [36], [37], [38]].
Iyengar yoga is a combination of the essential elements of yoga, namely the position (asana) and breath control (pranayama) accompanied by the use of stone tools (belts, wood, ropes, and blankets). This tool serves to maintain the position [39]. The pain in the first stage of labor is visceral and not localized. Pain is more strong and focused in the lower abdomen during the second stage of labor [40]. In this study, labor pain scores were significantly lower in the Modified Iyengar yoga group than controls (p < 0.05). This finding shows that the practice of modified Iyengar yoga can reduce labor pain in primigravida mothers. This study is consistent with previous findings that yoga can suppress labor pain [17,36]. In this study, the Yoga group's HARS score reduced much more than the control group's. This result indicates that anxiety in the group following Iyengar yoga is lower than control. This study extends previous findings that yoga can reduce anxiety throughout pregnancy by decreasing salivary cortisol levels [41]. Overall, we hypothesized that the mechanism of reducing pain and labor anxiety was caused by Iyengar yoga's capacity to increase pain tolerance, decrease unpleasant feelings, suppress of anxiety, and pain-related distress. These effects in the brain are based on decreased activation of the contralateral primary sensory, orbitofrontal, and thalamus (cortex) and increased activity of the ACC and anterior insula [42].
5. Conclusions
It was concluded that Iyengar Yoga in primigravida women was beneficial in suppressing labor pain and anxiety. Thus, the Iyengar Yoga technique can be a good method for supporting the success and safety of labor. In addition, the capacity to relieve pain through yoga practice can be a viable option in various therapeutic situations. Other applications necessitate a more in-depth investigation.
Funding source
This research received a novice lecturer grant from Ministry of Research, Technology and Higher Education of the Republic of Indonesia (Number T/140/E3/RA 00/2019).
Declaration of competing interest
No competing interest.
Acknowledgements
We thank the Research and Community Service Institute, University of Achmad Yani, Yogyakarta, Indonesia. We also acknowledged to Mr. Farid Abdullah as a laboratory assistant from the Department of Clinical Pathology, Faculty of Medicine, Gadjah Mada University, Yogyakarta for valuable technical assistance.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
References
- 1.Lutterodt M.C., Kahler P., Kragstrup J., Nicolaisdottir D.R., Siersma V., Ertmann R.K. Examining to what extent pregnancy-related physical symptoms worry women in the first trimester of pregnancy: a cross-sectional study in general practice. BJGP Open. 2019;12 doi: 10.3399/bjgpopen19X101674. pii: bjgpopen19X101674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodrigues P.B., Zambaldi C.F., Cantilino A., Sougey E.B. Special features of high-risk pregnancies as factors in development of mental distress: a review. Trends Psychiatry Psychother. 2016;38:136–140. doi: 10.1590/2237-6089-2015-0067. [DOI] [PubMed] [Google Scholar]
- 3.Kurki T., Hiilesmaa V., Raitasalo R., Mattila H., Ylikorkala O. Depression and anxiety in early pregnancy and risk for preeclampsia. Obstet. Gynecol. 2000;95:487–490. doi: 10.1016/s0029-7844(99)00602-x. [DOI] [PubMed] [Google Scholar]
- 4.Fairbrother N., Young A.H., Zhang A., Janseen P., Antony M.M. The prevalence and incidence of perinatal anxiety disorders among women experiencing a medically complicated pregnancy. Arch Women Ment Health. 2017;20(2):311–319. doi: 10.1007/s00737-016-0704-7. [DOI] [PubMed] [Google Scholar]
- 5.Ding X.X., Wu Y.L., Xu S.J., Zhu R.P., Jia X.M., Zhang S.F., Huang K., Zhu P., Hao J.H., Tao F.B. Maternal anxiety during pregnancy and adverse birth outcomes: a systematic review and meta-analysis of prospective cohort studies. J Affect Disord. 2014;159:103–110. doi: 10.1016/j.jad.2014.02.027. [DOI] [PubMed] [Google Scholar]
- 6.Tang S., Li X., Wu Z. Rising cesarean delivery rate in primiparous women in urban China: evidence from three nationwide household health surveys. Am J Obstet Gynecol. 2006;195(6):1527–1532. doi: 10.1016/j.ajog.2006.03.044. [DOI] [PubMed] [Google Scholar]
- 7.Korukcu O., Bulut O., Kukulu K. From experiences to expectations: A quantitative study on the fear of childbirth among multigravida women. Arch Physiatric Nurs. 2019;3(3):248–253. doi: 10.1016/j.apnu.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 8.Yuksel H., Cayir Y., Kosan Z., Tastan K. Effectiveness of breathing exercises during the second stage of labor on labor pain and duration: a randomized controlled trial. J Integr Med. 2017;15(6):456–461. doi: 10.1016/S2095-4964(17)60368-6. [DOI] [PubMed] [Google Scholar]
- 9.Brownridge P. The nature and consequences of childbirth pain. Eur J Obstet Gynecol Reprod Biol. 1995;59(Suppl):S9–S15. doi: 10.1016/0028-2243(95)02058-z. [DOI] [PubMed] [Google Scholar]
- 10.Sng B.L., Leong W.L., Zeng Y., Siddiqui F.J., Assam P.N., Lim Y., et al. Early versus late initiation of epidural analgesia for labour. Cochrane Database Syst Rev. 2014;10 doi: 10.1002/14651858.CD007238.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simkin P., Dickersin K. Oxford University Press; United Kingdom: 1996. A guide to effective care in pregnancy and childbirth. [Google Scholar]
- 12.Larsson C., Saltvedt S., Edman G., Wiklund I., Andolf E. Factors independently related to a negative birth experience in first-time mothers. Sex Reprod Healthc. 2011;2:83–89. doi: 10.1016/j.srhc.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 13.Thorp J.A., Breedlove G. Epidural analgesia in labor: an evaluation of risks and benefits. Birth (Berkeley) 1996;23:63–83. doi: 10.1111/j.1523-536x.1996.tb00833.x. [DOI] [PubMed] [Google Scholar]
- 14.Tulp M.J., Paech M.J. Analgesia for childbirth: modern insights into an age-old challenge and the quest for an ideal approach. Pain Manag. 2014;4:69–78. doi: 10.2217/pmt.13.63. [DOI] [PubMed] [Google Scholar]
- 15.Schmalzl L., Powers C., Henje Blom E. Neurophysiological and neurocognitive me-chanisms underlying the effects of yoga-based practices: towards a comprehensive theoretical framework. Front Hum Neurosci. 2015;9:235. doi: 10.3389/fnhum.2015.00235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Babbar S., Shyken J. Yoga in pregnancy. Clin Obstet Gynecol. 2016;59(3):600–612. doi: 10.1097/GRF.0000000000000210. [DOI] [PubMed] [Google Scholar]
- 17.Jiang Q., Wu Z., Zhou L., Dunlop J., Chen P. Effects of yoga intervention during pregnancy: a review for current status. Am J Perinatol. 2015;32(6):503–514. doi: 10.1055/s-0034-1396701. [DOI] [PubMed] [Google Scholar]
- 18.Kinser P.A., Pauli J., Jallo N., Shall M., Karst K., Hoekstra M., Starkweather A. Physical activity and yoga-based approaches for pregnancy-related low back and pelvic pain. J Obstet Gynecol Neonatal Nurs. 2017;46(3):334–336. doi: 10.1016/j.jogn.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 19.Martins R.F., Pinto e Silva J.L. Treatment of pregnancy-related lumbar and pelvic girdle pain by the yoga method: a randomized controlled study. J Altern Complement Med. 2014;20(1):24–31. doi: 10.1089/acm.2012.0715. [DOI] [PubMed] [Google Scholar]
- 20.Iyengar B.K.S. In: What is Yoga. Light on yoga. Iyengar B.K.S., editor. Schocken Books; New York: 1976. pp. 19–20. [Google Scholar]
- 21.Iyengar B.K.S. In: Technique and Effect of Pranayama. Light on yoga. Iyengar B.K.S., editor. Schocken Books; New York: 1976. pp. 441–442. [Google Scholar]
- 22.Nambi G.S., Inbasekaran D., Khuman R., Shanmugananth D.S., Jagannatahan K. Changes in pain intensity and health related quality of life with Iyengar yoga in nonspecific chronic low back pain: A randomized controlled study. Int J Yoga. 2014;7(1):48–53. doi: 10.4103/0973-6131.123481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Evans S., Sternlieb B., Zeltzer L., Tsao J.C.I. Iyengar yoga and the use of props for pediatric chronic pain: a case study. Altern Ther Helath Med. 2013;19(5):66–70. 23981408. [PMC free article] [PubMed] [Google Scholar]
- 24.Crow E.M., Jeannot E., Trewhela A. Effectiveness of Iyengar yoga in treating spinal (back and neck) pain: A systematic review. Int J Yoga. 2015;8(1):3–14. doi: 10.4103/0973-6131.146046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams K., Abildso C., Steinberg L., Doyle E., Epstein B., Smith D., Hobbs G., Gross R., Kelley G., Coope L. Evaluation of the effectiveness and efficacy of iyengar yoga therapy on chronic low back pain. Spine (Phila Pa 1976) 2009 September 1;34(19):2066–2076. doi: 10.1097/BRS.0b013e3181b315cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Streeter C.C., Gerbarg P.L., Whitfield T.H., Owen L., Johnston J., Silveri M.M., et al. Treatment of major depressive disorderwith iyengar yoga and coherent breathing:a randomized controlled dosing study. J Alternat Complement Med. 2017;23(3):201–207. doi: 10.1089/acm.2016.0140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bolanthakodi C., Raghunandan C., Saili A., Mondal S., Saxena P. Prenatal yoga: effects on alleviation of labor pain and birth outcomes. J Altern Complement Med. 2018;30 doi: 10.1089/acm.2018.0079. [DOI] [PubMed] [Google Scholar]
- 28.Buttner M.M., Brock R.L., O’Hara M.W., Stuart S. Efficacy of yoga for depressed postpartum women: A randomized controlled trial. Complement Ther Clin Pract. 2015;21(2):94–100. doi: 10.1016/j.ctcp.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 29.Iyengar B.K.S. Nikol; Hamburg, Germany: 2013. Licht auf Yoga: Das Grundlegende Lehrbuch des Hatha-Yoga. [Google Scholar]
- 30.Gavin N.R., Kogutt B.K., Fletcher W., Szymanski L.M. Fetal and maternal responses to yoga in the third trimester. J Matern-Fetal Neonatal Med. 2020;33(15):223–2627. doi: 10.1080/14767058.2018.1555815. [DOI] [PubMed] [Google Scholar]
- 31.Huang F.J., Chien D.K., Chung U.L. Effects of Hatha yoga on stress in middle-aged women. J Nurs Res. 2013;21(1):59–66. doi: 10.1097/jnr.0b013e3182829d6d. [DOI] [PubMed] [Google Scholar]
- 32.Hjermstad M.J., Fayers P.M., Haugen D.F., Caraceni A., Hank G.W., Loge J.H., et al. Studies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Managem. 2011;41(6):1073–1093. doi: 10.1016/j.jpainsymman.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 33.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;23:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 34.Hamilton M. Diagnosis and rating of anxiety. Br J Psychiatry Suppl. 1969;3:76–79. doi: 10.1002/acr.20561. [DOI] [Google Scholar]
- 35.Styles A., Loftus V., Nicolson S., Harms L. Prenatal yoga for young women a mixed methods study of acceptability and benefits. BMC Pregnancy Childbirth. 2019;19(1):449. doi: 10.1186/s12884-019-2564-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Corrigan L., Moran P., McGrath N., Eustace-Cook J., Daly D. The characteristics and effectiveness of pregnancy yoga interventions: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2022;22:250. doi: 10.1186/s12884-022-04474-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cramer H., Frawley J., Steel A., Hall H., Adams J., Broom A., Sibbritt D. Characteristics of women who practice yoga in different locations during pregnancy. BMJ Open. 2015;5(8) doi: 10.1136/bmjopen-2015-008641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lin I.H., Huang C.Y., Chou S.H., Shih C.L. Efficacy of prenatal yoga in the treatment of depression and anxiety during pregnancy: a systematic review and meta-analysis. Int J Environ Res Public Health. 2022 May 19;(9):5368. doi: 10.3390/ijerph19095368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jacobsen P.B., Muchnick S., Marcus S., Amheiser P., Reiersen P., Gonzales B., et al. Pilot study of Iyengar yoga for management of aromatase inhibitor-associated arthralgia in women with breast cancer. Psychooncology. 2015;24(11):1578–1580. doi: 10.1002/pon.3756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen P.J., Yang L., Chou C.C., Lie C.C., Chang Y.L., Liaw J.J. Effects of prenatal yoga on women’s stress and immune function across pregnancy: A randomized controlled trial. Complement Ther Med. 2017;31:109–117. doi: 10.1016/j.ctim.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 41.Kuczkowski K.M. Labor pain and its management with the combined spinal-epidural analgesia: what does an obstetrician need to know? Arch Gynecol Obstet. 2007;275(3):183–185. doi: 10.1007/s00404-006-0204-5. [DOI] [PubMed] [Google Scholar]
- 42.Rivest-Gadbois E., Boudrias M.H. What are the known effects of yoga on the brain in relation to motor performances, body awareness and pain? A narrative review. Complement Ther Med. 2019;44:129–142. doi: 10.1016/j.ctim.2019.03.021. [DOI] [PubMed] [Google Scholar]