Executive Summary
Around the world, populations are ageing at a faster pace than in the past and this demographic transition will have impacts on all aspects of societies. In May 2020, the UN General Assembly declared 2021–2030 the Decade of Healthy Ageing, highlighting the importance for policymakers across the world to focus policy on improving the lives of older people, both today and in the future. While rapid population ageing poses challenges, China’s rapid economic growth over the last forty years has created space for policy to assist older persons and families in their efforts to improve health and well-being at older ages. As China is home to 1/5 of the world’s older people, China is often held up as an example for other middle-income countries. This Commission Report aims to help readers to understand the process of healthy ageing in China as a means of drawing lessons from the China experience. In addition, with the purpose of informing the ongoing policy dialogue within China, the Commission Report highlights the policy challenges on the horizon and draws lessons from international experience.
The uniqueness of China’s ageing society
From a global perspective, China shares some of the economic and social challenges faced by other countries with rapidly ageing populations. China stands out, however, as it already has the world’s largest older population, and China’s ageing burdens will increase further as the ‘second baby boomers’ (those born between 1962 and 1975) start to enter retirement in 2022. In addition, China’s rapid demographic transition over the last four decades will lead to a dramatic decline in the number of living children for each older person in China and bring substantial challenges for both family-based care and social care. Compounding demographic changes, personnel planning in geriatric and rehabilitation medicine has not kept pace with the growth of the older age population, and there is a shortage of medical resources targeted at the ageing population. In Section 1, the report stresses the importance of achieving “healthy ageing” in light of socio-economic progress, urbanization and migration, and China’s demographic transition.
Health complexity and inequalities among China’s older population
China completed its epidemiological transition from infectious diseases to non-communicable diseases (NCDs) during the past three decades. As in many other ageing countries, the upward trend in the incidence of NCDs and the presence of multimorbidity pose special challenges for China’s healthcare sector. Even as some older Chinese continue to suffer from such communicable diseases as hepatitis, tuberculosis, and sexually transmitted diseases, chronic conditions, such as cognitive impairments, mental disorders, and frailty, are becoming much more prominent. These chronic conditions are complex to treat and manage and are associated with more functional disability and greater care needs. Along with the emergence of NCDs, substantial gaps in health are apparent by gender, rural versus urban residence, ethnicity, and socio-economic status. Investments in healthy ageing, from promoting education in health literacy to improving access to health care, are promising means of improving the well-being of older adults and reducing the gaps in health across socioeconomic groups in China. Even as China’s population ages, investments in healthy ageing offer a path for older Chinese to play meaningful and productive social roles in society, while limiting burdens on their families. The latest facts on health status and health inequities among China’s older adults are presented in Section 2 of the report.
Modifiable factors of healthy ageing: Evidence from China.
Current evidence on the determinants of health and functioning status of China’s older population is summarized in Section 3. In China, as elsewhere, health at older ages results from the cumulative effects of behaviours and events that occur across the life cycle. These include exposures to unhealthy environments and parental decisions influencing in-utero and childhood health, later health behaviours as teenagers and adults (including decisions on educational investments, smoking, drinking, and physical activity), and decisions over food consumption which influence diet and nutritional status. Many of these decisions and behaviors are influenced by health literacy and socio-economic conditions, but they may also be influenced by policy (Section 5). Finally, Section 3 highlights the health benefits of social connections and participating in leisure activities such as square dancing and promoting age-friendly environments in China.
Integrating medical and social care for Chinese older people.
Older people require access to high-quality health services that include prevention, promotion, curative, rehabilitative, palliative and end-of-life care. An update on China’s policy initiatives regarding healthcare and social care relevant to the ageing population is provided in Section 4. In addition to achieving universal health insurance coverage, China has invested heavily in public health promotion and the consolidation of the primary healthcare system. Further, as the role of the family in providing care for older people is eroded by dwindling family size and changing living arrangements, especially with the outmigration of adult children, China is taking steps to build up institutional and community care infrastructure as both a substitute for, and complement to, family care. Furthermore, long-term care insurance (LTCI) has been piloted in many cities as a financing mechanism. China’s experience with the LTCI pilots suggests that it will be difficult to sustain LTCI under the current pay-as-you-go framework, and that there will be a considerable public financial risk as the population ages. Although China’s government has placed the integration of health care with long-term care (LTC) at the forefront of its policy agenda, the progress for the integration has been slow.
Lessons learned from China and implications for the future.
An overview of the evidence presented earlier in the report is presented in Section 5, followed by policy recommendations for supporting healthy ageing in China. Policy recommendations outlined here can be generalized to other countries, especially low- and middle-income countries (LMICs). First, health promotion initiatives should focus on changing people’s behavior, especially smoking cessation, weight control, and health literacy education to reduce the incidence of NCDs and care burdens. Second, there is an urgent need to move away from disease-centred care to person-centred care and to increase the supply of health care workers, particularly in geriatric medicine, rehabilitation medicine, and hospice care. Third, innovative measures should be taken to remove obstacles to upgrading community and home environments and thus facilitate mobility and social engagement among older people.
There are several other policy areas that should be addressed, given China’s unique institutional environment. These include regional segmentation of health insurance systems and the regulatory environment for healthcare delivery. Specifically, the report suggests that policy in China should focus on: (1) national integration of the health insurance system to eliminate the current segmentation across regions and occupations; (2) capping regionally segmented LTCI initiatives, and striving for a national scheme that is independently funded; (3) switching government subsidies in the aged care sector from subsidising providers to subsidising consumers to facilitate market competition and to help existing care facilities to meet safety regulations; (4) strengthing the capacity to regulate medical service providers, especially in screening for fraud against the national medical insurance schemes and reforming the healthcare delivery sector by lowering barriers to entry and facilitating choice.
Older people are an important part of a family and an invaluable asset to society. Healthy ageing will not only enable older people to enjoy their later life to the fullest but has the potential to unleash the intellectual and vocational capacities of society as a whole. Recognizing that China’s older population will continue to grow, it is important to take their needs into account and prepare well in advance by creating an age-friendly environment for the ageing population. As China’s “second baby boomers” start to reach retirement age in 2022, it is imperative to take the window of opportunity afforded by China’s economic growth to make coordinated efforts across sectors to address the concerns of an ageing nation.
Section 1. Introduction
The Chinese population has aged and will continue to age rapidly for decades. In 2021, 14.2% of China’s population was 65 and older, implying that China doubled the share of its older adults aged 65 and over from 7% to 14% in 21 years. In contrast, high-income countries (HICs) took about half a century to double this share.1 By 2065, China will become the oldest country among the twenty most populous countries globally.2 China already has the world’s largest number of older people, and the number is growing. By 2050, there will be 395 million people aged 65 and older in China, equivalent to 1.2 times the current population of the United States (US). The oldest old, 80 and older, will reach 135 million and exceed the current population of Japan.2
As in the rest of the world, declining fertility and rising life expectancy have both contributed to population ageing in China. The total fertility rate was 6.1 in 1950–55; in 2020, it was 1.3. The total number of births reached a record low of 10.62 million in 2021, and net population growth was merely 0.48 million. Meanwhile, life expectancy at birth went from 44 years in 1950–1955; in 2021, it was 78.20 years.
A rapidly ageing population poses serious economic challenges. An ageing society can only be supported if the economy is growing successfully. A growing economy depends on a flourishing working-age population. When retirement age stays fixed, the number and proportion of the working-age population will decline, draining the economy of the productive labour force. With pay-as-you-go social security systems, which dominate almost all countries, rising retiree-to-worker ratios will either lead to a large and growing deficit in social pension programs or an increasing financial burden on the current working-age population. Health care financing will also be strained since older people tend to use health care services at disproportionally higher rates. Furthermore, older people, particularly those who are unhealthy, require more long-term care (LTC) than younger people, which adds to private and public financial and instrumental care burdens.
In the absence of coordinated investments in healthy ageing, the rate of demographic change in China implies that the economic and social challenges associated with population ageing could be greater for China. The old-age dependency ratio, defined as the ratio of people aged 65 and older to those aged 20–64, is expected to more than triple from 0.18 in 2019 to 0.55 in 2050.2 The social security system in China, which recently expanded to cover the rural population, is highly fragmented. People living in rural areas receive very little pension support and live well below the poverty line. China faces greater fiscal pressures to meet obligations for a viable social security program that provides economic security for older adults, and that burden is expected to rise rapidly. The Chinese family traditionally took care of their older parents and other relatives, but decreases in fertility over the last 40 years have put pressure on traditional arrangements, and in rural areas and small towns, family capacity to provide instrumental care is further eroded by the out-migration of working-age adults.
Can China solve the ageing problem by adopting radical pro-natalist policies to drive up birth rates and/or to increase immigration to supplement below-replacement fertility? For a country the size of China, the role of immigration will be minimal. The Chinese government officially terminated the one-child policy in 2015 and further permitted three children in 2020, coupled with a pledge to provide incentives for childbirth. However, many countries have tooled with pro-natalist policies in the past, and very few are effective. Even if fertility can rebound a little, it cannot stop the trend of population ageing, as continued advances in life expectancy will drive future ageing.
Even so, amid the doom and gloom of population ageing, the prospect of healthy ageing provides a reason for optimism. Healthier older adults will be physically able to delay retirement, converting an otherwise dependent population into a productive workforce that contributes to the economy. In so doing, they also delay taking social security, alleviating the adverse effects of the support ratio on the social pension system. In addition, improved health during old age can reduce the demand for healthcare services and lead to healthier older persons who can live independently for longer and require less care from family and society. Further, healthy older persons contribute to families and communities as providers of care and mentoring for children, which may facilitate an increased labor supply for working-age parents. As a result, policymakers in any country facing an ageing population would be wise to implement integrated policies to promote healthy ageing.
Under an ideal setting, healthy ageing would be reflected in a compression of morbidity, i.e., older adults living longer would live for more years in a healthy state and fewer years in an unhealthy one. There is evidence of morbidity compression in HICs, but limited evidence has been found in low- and middle-income countries (LMICs).3
Longevity does not guarantee good health in old age. People may live into old age against all odds but still bear the marks of past assaults on their bodies and minds. With the population ageing, China has shifted from a mortality pattern dominated by acute infectious diseases to chronic diseases. Thus, reducing mortality and improving the health of older adults will require a greater emphasis on controlling chronic diseases and the occurrence of multiple chronic conditions.
Healthy ageing, however, is more than just freedom from disease. According to the World Health Organization (WHO), healthy aging is more than just the absence of disease; it is the process of developing and maintaining the functional ability that enables well-being in older age.4 The Chinese Geriatric Association defines healthy ageing in five dimensions: free from major chronic diseases, without cognitive impairment, taking part in family and social activities, retaining functioning ability, and maintaining a healthy lifestyle.5 The key to healthy ageing is maintaining functional ability despite having chronic conditions. Subjective measures of well-being play an equally important role in healthy ageing. As such, the first goal of this report is to describe the health status, functional abilities, and subjective well-being (SWB) of older people in China (Section 2).
Understanding the determinants of health and functional status at older ages is essential to promoting healthy ageing. A better understanding of the health and functional status of older people in China will help the government develop well-designed interventions to improve older adults’ health and functional abilities. Thus, the second goal of this report is to present analyses about the determinants of health and functional status, with particular focus on those that may be modifiable (Section 3). This report takes a life-cycle perspective in understanding how interventions long before old age contribute to healthy ageing since health in old age reflects health-enhancing investments and negative perturbations to health over a lifetime.
Government has an important role to play in promoting healthy ageing. Even when health policies promulgated by China’s government do not explicitly target the health of older people, they have substantial impacts on health at older ages. One example is the expansion of health insurance coverage for the whole population. Other examples include establishing a national public health infrastructure, strengthening primary care, and implementing the clean air act. Some policies, such as integrating medical and social care, promote health services for older people. In addition to health care, social care for older people is also a necessary investment. Traditionally, Chinese families have taken care of their older members. However, caregiving may have adverse effects on family caregivers; some care needs, inevitably, may not be met under traditional family care. The Chinese government has implemented policies to enhance and support family care with social and institutional care. Although long-term care insurance (LTCI) provides funding for aged care, it can be expensive if improperly designed. We will review the progress in efforts in healthcare and social care in Section 4.
We summarise the evidence presented earlier in the report and provide the outlook and policy recommendations for healthy ageing in China. The policy recommendations target three main fields: enhancing an age-friendly environment and healthy behaviors, advancing useful innovations to current healthcare systems, and improving the LTC and insurance, which address the care needs of ageing populations in China (Section 5).
There are two concurrent cross-cutting themes throughout the report: inequity between urban and rural China and disparities between men and women. The disparities are generally evident in every section of the report. Older people’s health and functional status differ dramatically between urban and rural areas, as do health behaviors and the social and environmental factors that influence health. Further, while China’s government has made considerable efforts to improve access to high-quality health care for the rural population, substantial differences persist, and these are also manifest in differential access to LTC. There are also gender differences in health outcomes and health behaviors. Women tend to live longer than men, so their care needs are also more likely to be unmet since they have less access to high-quality care from within the family.
Beyond this introductory section, this report consists of four detailed sections. In Section 2, we describe the health and functioning status of older people in China, followed by Section 3, which discusses factors that can be modified to influence the health of older people. In Section 4, we overview the previous healthcare and social care policies that directly or indirectly promote healthy ageing. Finally, section 5 proposes the outlook and policy recommendations dedicated to health promotion for older people in China.
Section 2. Health status
2.1. Life expectancy and causes of death
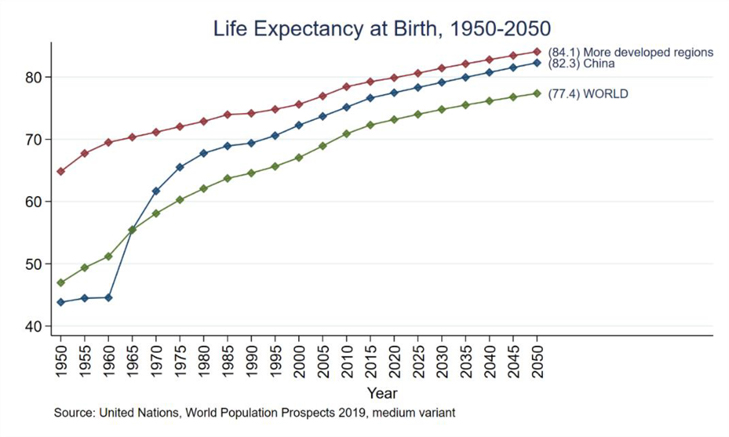
Life expectancy in China has increased significantly since the People’s Republic of China was founded (Figure 1). In the 1960s and 1970s, public health campaigns and universal basic medical care led to the greatest gains in life expectancy. Beginning in the early 1980s, China’s economic reforms reduced poverty and improved living standards considerably, altering disease patterns and closing the life expectancy gap with HICs.
Figure 1: Life expectancy at Birth, 1950–2050.
Source: United Nations, World Population Prospects 2019, medium variant
Reducing infant mortality has largely contributed to an increase in life expectancy. In China, several national programs reduce maternal mortality and eliminate neonatal tetanus.6 Infectious diseases have also been controlled through medical innovations such as immunization and antibiotic therap.7 Based on the Global Burden of Disease (GBD) study, life expectancy in China improved from 1990 to 2013 due to reductions in diarrhea, lower respiratory infections, neonatal disorders, and cancer.8
During the 1990s and 2000s, China completed its epidemiological transition from infectious diseases to non-communicable diseases (NCDs). The age-standardised mortality rate decreased by 74.1% for communicable, maternal, neonatal, and nutritional diseases, higher than that for NCDs (35.7%).8 Between 1990 and 2017, communicable, maternal, neonatal, and nutritional diseases decreased by 1.2 million. Lower respiratory infections ranked first in 1999, but ranked 12th in 2017.9 However, deaths from NCDs rose from 5.9 million to 7.9 million. The most common NCDs, including stroke, ischemic heart disease, cancers, and chronic obstructive pulmonary diseases (COPD), have become the leading causes of death in China since the 1990s.9
2.2. Chronic conditions and Infectious Diseases
2.2.1. Chronic conditions
Cardiovascular and cerebrovascular diseases
China’s prevalence and mortality of Cardiovascular Disease (CVD) have increased substantially due to several reasons including high caloric diets and sedentary lifestyles. It was estimated that 230 million people suffered from CVD in 2007; by 2018, that number had increased to 290 million.10 CVD is China’s leading cause of death, accounting for over 40% of all deaths. As per the China Statistical Yearbook, CVD deaths accounted for 43.5% of mortality in urban areas and 45.9% in rural areas, with 265.11/100,000 deaths for heart disease and 126.41/100,000 deaths for cerebrovascular disease in urban areas and 161.18/100,000 deaths for heart disease and 158.15/100,000 deaths for cerebrovascular disease in rural areas.11
Stroke is also among the leading causes of death. According to the National Epidemiological Survey of Stroke in China (NESS-China), stroke prevalence in 2013 was 42.6% (men 47.1%, women 38.3%), 66.7% (men 75.1%, women 58.8%), and 59.7% (men 73.9%, women 48.1%) in those aged 60–69, 70–79, and 80 years old or older.12 First attacks have increased from 1,890 per million population (PMP) in 2002 to 3,790 in 2013, with an overall annual increase of 8.3%.13
Coronary heart disease (CHD) contributes to most cardiac deaths in China, and around half of CHD deaths are caused by acute myocardial infarction (AMI).10 From 2013 to 2017, cardiac mortality doubled in rural areas and exceeded that in urban.10 The mortality rate of CHD in 2017 was 1153 PMP in urban areas (1181 PMP compared to 1125 PMP for men and women) and 1220 PMP in rural areas (1257 PMP compared to 1183 PMP for men and women).11
Hypertension
Chinese hypertension prevalence has risen steadily since 1991. From 2012–2015, the China Hypertension Survey found that prevalence rates of hypertension were 44.6%, 55.7%, and 60.2% among people aged 55–64, 65–74, and ⩾75, respectively, and were higher among men (24.5% vs. 21.9% for women).14 Not surprisingly, hypertension is more prevalent among the older population. One study found a U-shaped association between SBP and all-cause mortality among respondents aged 80 or older. A study of oldest-old respondents found a U-shaped correlation between SBP and mortality. Among those with a SBP between 107 and 154 mm Hg, higher SBP (>154 mm Hg) was associated with CVD mortality, and lower SBP (<107 mm Hg) with non-CVD mortality. Older adults over the age of 80 may not benefit from current blood pressure guidelines.15
In rural areas, access to health care has been a major problem in diagnosing and treating hypertension. Improvements have been made in recent decades. Among hypertensive patients, hypertension awareness increased from 26.2% in 1991 to 46.9% by 2015. Treatment rates rose from 12.1% in 1991 to 40.7% in 2015.14 Rural improvements were even more impressive. Rural vs. urban awareness rates were 13.9% vs. 35.6% in 1991, narrowing to 44.7% vs. 50.9% in 2015. For treatment, the rural vs. urban rates were 5.4% vs. 17.1% in 1991, narrowing to 38.0% vs. 45.8% in 2015.14 Despite this progress, control rates remain low. Only 19.4% of urban and 13.1% of rural patients successfully controlled their blood pressure in 2015.14
Diabetes
Diabetes is increasingly prevalent in China, especially among older persons.16 Deaths from diabetes rose from 19th place in 1990 to 8th place in 2017.9According to a recent national survey, 27.8% of adults aged 70 and over had diabetes in 2018.17 Another national survey reported the weighted prevalence of diabetes in older adults aged 60–69 and 70 or older were 28.8% and 31.8%, respectively.18 In 2011–2012, the China Health and Retirement Longitudinal Study (CHARLS) reported 17.4% prevalence rate of diabetes (16.9% vs. 17.9% for men and women, 23.9% vs. 14.8% for urban and rural).16
Rural diabetes rates are rising faster than urban rates. In 1997, rural areas had lower diabetes and Impaired Glucose Tolerance (IGT) prevalence rates than urban areas (rural vs. urban diabetes rate: 1.7%–2.7% vs. 3.3%–4.6%; IGT: 3.1%–5.0%).19 Although rural residents still have a lower prevalence of diabetes (9.5% rural vs. 12.6% urban in 2013), rural residents have a relatively high prevalence of prediabetes (37.0% vs. 34.3%).20
According to CHARLS 2011 data, awareness of having diabetes was 40.7% (37.3% vs. 44.0% for men and women, 52.9% vs. 32.6% in urban and rural).16 However, diabetes awareness and treatment rates remain problems in China despite much stronger health campaigns since 2009.16 Treatment rates increased from 25.8% to 32.2%, and control rates among treated patients increased from 39.7% to 49.2% from 2010 to 2013.20 The management of diabetes in rural areas is much more challenging. Diabetes management in rural areas is more challenging. In 2013, the awareness, treatment, and control rates in rural areas were 29.1%, 25.2%, and 42.3%, significantly lower than in urban areas (43.1%, 38.4%, and 53.3%, respectively).20
Obesity and overweight
Overweight and obesity are associated with increased morbidity and CVD mortality.21 Rapid economic growth has led to changes in dietary and physical activity levels, leading to obesity and overweight in China.
Obesity prevalence rose from 3.1% in 2004 to 8.1% in 2018, according to the China Chronic Disease and Risk Factors Surveillance.22 Urban BMI and obesity prevalence has declined significantly since 2010, and moderately in rural men, but rural women’s prevalence has continued to rise. The CHARLS 2015 wave found that older women were more likely than men to be overweight/obese. The obesity prevalence among men (women) 60 and older was 3.0% (5.7%), and the central obesity prevalence was 8.0% (47.1%). People with non-agricultural hukou were more likely to be overweight (41.7% vs. 29.1%), obese (5.9% vs. 3.7%), and have central obesity (30.6% vs. 26.3%). The illiterate are more likely to be overweight, but less likely to be obese or have central obesity.
Chronic Kidney Disease
In 2016, chronic kidney disease (CKD) was the 16th most prevalent cause of Years of Life Lost (YLLs) in China, and it is anticipated to become the 5th most prevalent by 2040.23 According to a national survey in 2010, the prevalence of CKD was 10.8%. The prevalence was higher in rural areas (11.3% vs. 8.9% in urban areas) and among women (12.9% vs. 8.7% among men).24 Due to the rise in diabetes and hypertension, CKD has become more prevalent. According to a study using the National Hospital Quality Monitoring System database, diabetes-related CKD has overtaken glomerulonephritis as the most common cause of CKD.25 Diabetes-related CKD increased from 19.5% to 24.3% from 2010 to 2015, and hypertension-related CKD increased from 11.5% to 15.9%.25
Due to the disease’s silent nature, awareness of CKD was only 12.5% in 2010 despite its high prevalence rate.24 Previous studies suggest that screening for persistent albuminuria among high-risk populations could be a cost-effective strategy for early detection.26
Chronic Obstructive Pulmonary Disease
In 2017, chronic obstructive pulmonary disease (COPD) was China’s third leading cause of mortality.9,27 COPD incidence increased from 8.2% in 2004 to 13.6% in 2015 in China with industrialisation and air pollution.27,28 There was a higher prevalence among men than among women (19.0% vs. 8.1%). COPD prevalence was highest in southwest China (20.2%) and rural areas (14.9% vs. 12.2% in urban areas).27
At less than 3%, the awareness of COPD is extremely low.27 In COPD, only 5.9% of patients were tested by spirometry, a standard diagnostic test.27 Although the current diagnostic situation is still not optimal, there has been a significant increase in early-stage COPD diagnoses since 2004.27,28 The assessment of the Global Initiative for Chronic Obstructive Lung Disease stratification found that more COPD patients in stage I (mild disease) were diagnosed in 2015 while more patients in stage II (moderate disease) were diagnosed in 2004.27,28
Cancers
According to the Cancer Registration in China, although the crude cancer mortality rate rose from 74.2 per 100, 000 in 1973–75 to 170.1 per 100, 000 in 2015, age-standardised death rates declined from 94.4 per 100, 000 in 1990–92 to 77.9 per 100, 000 in 2015, indicating that much of the increase in the crude rate is associated with an ageing population.29 According to a multicenter study conducted in China, cancer is the leading cause of hospitalization among older inpatients, followed by hypertension, ischemic heart disease, diabetes, and cerebrovascular disease.30 China’s top five cancers in 2020 were lung cancer, stomach cancer, colorectum cancer, liver cancer, and breast cancer.31 For men, lung cancer was the most common type (n = 0.54 million), and to women, breast cancer was the most frequent type (n = 0.42 million).29,31 In 2013, cancer incidence was lower in rural than urban areas (182.4 vs. 189.9 per 100,000), but by 2015 it reversed (213.6 in rural vs. 191.5 in urban, per 100,000).32 Higher measured incidence may also be due to improvements in early detection and screening in rural areas.
The 5-year survival rate for all patients with cancer in 2012–15 was higher in urban areas (46·7%) than in rural areas (33·6%). The geographical disparities narrowed. As compared to 2003–05, rural cancer patients showed greater survival increases than urban cancer patients, with the survival gap declining from 17.7% in 2005–05 to 13.1% in 2012–15.33
Multimorbidity
Multimorbidity is more common among older adults as chronic disease becomes the dominant health concern. UK Academy of Medical Sciences defines multimorbidity as the coexistence of at least two chronic conditions, each of which must be an NCD, a mental health disorder, or an infectious disease with long duration.34 The neglect of multimorbidity and the treatment of each condition separately leads to excessive healthcare use, inappropriate polypharmacy, and conflicting treatments.35
It is interesting to note that multimorbidity prevalence is lower in LMICs than in HICs. There is a likely underdiagnosis of chronic diseases in these LMICs. China had the lowest multimorbidity prevalence among those aged 50–59 (including India, Ghana, Mexico, Russia, Poland, South Africa, Finland and Spain) according to a multi-country study. It is likely that this finding is due to nonrandom sampling in China, which results in a higher proportion of healthy participants.36
A CHARLS study with combined three waves (2011, 2013, and 2015) found a multimorbidity prevalence of 42.4% among participants 50 years and older, which was higher among urban residents (43.7% vs. 41.0% in rural areas) and women (45.6 vs. 39.6% among men). Relying on self-reports alone may lead to an undermeasurement of multimorbidity.37 Reliance on self-reports alone may well lead to under-measurement of multimorbidity, as suggested in a recent study. This study analyzed measured hypertension and blood biomarkers associated with a few chronic conditions, along with self-reported chronic conditions. According to the study, multimorbidity prevalence was 68.1% using objective measures, but only 47.7% using self-reported conditions alone.38
2.2.2. Infectious Diseases
The decline in intrinsic ability and immunity of older adults makes infectious diseases a significant threat to their health in China, despite NCDs becoming the leading cause of death. In China, despite the shift of resources to chronic diseases as a result of population ageing, infectious diseases are still a major threat to the health of older people. In addition to Corona virus disease 2019 (COVID-19), which affects older individuals disproportionately, many other diseases should require attention. In 2019, China reported 3,072,338 cases of infectious diseases of classes A and B.39 In contrast to Class A diseases, which include cholera and plague, Class B diseases include viral hepatitis, tuberculosis, syphilis, and HIV/AIDS, which are common and affect older people disproportionally.40
HIV/AIDS
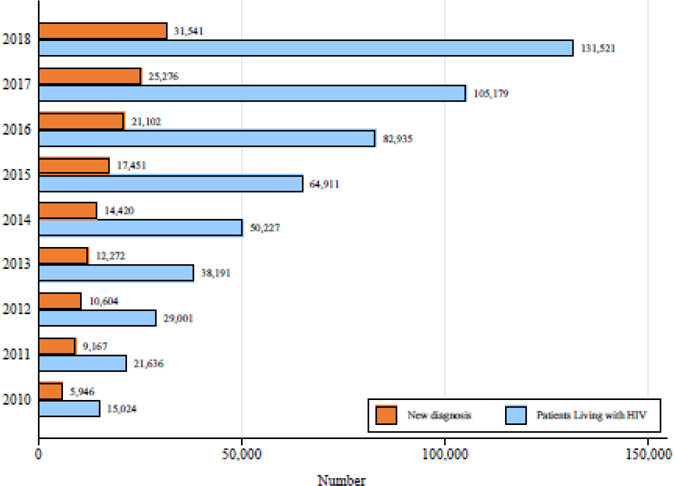
By global standards, China has a very low HIV/AIDS prevalence of under 0.1%, which should be borne in mind during this discussion. HIV transmission in China has shifted significantly from injection-drug-driven transmission to almost exclusively sexual transmission.41 Sexually active young people are frequently viewed as more responsible for HIV transmission. Over the past decade, however, HIV infection through heterosexual transmission has increased significantly among older individuals (≥60 years old), particularly older males, increased significantly over the past decade.41 The number of newly diagnosed HIV cases among older people increased from 5,946 in 2010 to 31,541 in 2018 (see Figure 2). The share of older heterosexual males among newly diagnosed HIV cases has increased from 7.4% in 2010 to 16.5% in 2018.42 China may have late diagnosis for some of these new cases among older people, but this is not the whole story. Researchers in Guangxi found that older males have a higher HIV infection risk than younger males, based on repeated HIV screenings of the population.43 An increase in infection among older males may be related to the rising popularity of erectile dysfunction medication (EDM) and less expensive illegally manufactured aphrodisiacs. Researchers have found that older Chinese men who engage in low-cost commercial sex and do not use condoms are more likely to contract HIV and other sexually transmitted infections when using EDM or aphrodisiacs.44 It is imperative to focus on prevention and testing interventions in this vulnerable group of older adults.
Figure 2. The number of HIV infections among older people (≥60) in China from 2010 to 2018.
Viral Hepatitis, Tuberculosis, and Syphilis
Virus hepatitis, tuberculosis, and syphilis affect older people disproportionally. In 2019, people aged 60 and older accounted for 18.1% of the total China’s population, but accounted for 24.9%, 22.5% and 34.5% of total viral hepatitis, viral hepatitis B, and viral hepatitis C cases, respectively.45 Similarly, tuberculosis and syphilis among those 60 and older accounted for 34.6% and 32.3% of total cases, respectively.45 The higher tuberculosis infection rates in older people may be due to their weakened immune systems, while the higher viral hepatitis C infection rates may be due to their more extensive use of blood infusions in medical treatments. As syphilis and HIV cases increase among older people, it indicates that older people are more sexually active than previously thought.
COVID-19
Globally, COVID-19 has infected disproportionately older people, and clinical severity and case-fatality ratios are significantly higher among older adults than among youth.46 In China, the incidence of COVID-19 among people 60 years and older was two times higher than for people under 60 years of age. Case-fatality ratios were less than 1% for those under the age of 50, 3.1% for those between the ages of 50 and 59, 8.2% for those between the ages of 60 and 69, 18.5% for those between the ages of 70 and 79, and 32.1% for those over the age of 80.47 Meanwhile, older age was associated with a lack of willingness to accept COVID-19 vaccination.48
2.3. Mental Disorder and Cognition Impairment
2.3.1. Depression and Depressive symptoms
A mental disorder, also referred to as a mental illness or psychiatric disorder, is a pattern of behavior or mental experience that results in significant distress or functional impairment. Depression (major depressive disorder) is one common and serious mental disorder. Globally, depression is a major cause of death in old age. Institute for Health Metrics and Evaluation (IHME) estimates that loss of Disability-adjusted life year (DALYs) from major depression increased from 634 (ranked 20th) per 100,000 in 1990 to 675 (ranked 14th) per 100,000 in 2017, and 779 (ranked 20th) per 100,000 in 2017.49 According to the China Mental Health Survey (CMHS, 2012–15), lifetime depressive disorder prevalence was 7.3%, while 12-month depressive disorder prevalence was 3.8%.50 Chinese people aged 60 and older reported 3.0% major depressive disorder over the past 12 months.51
As different instruments (e.g., Center for Epidemiologic Studies Depression Scale [CES-D], Hamilton Depression Rating Scale [HAM-D], Patient Health Questionnaire [PHQ-9], and Geriatric Depression Scale [GDS]) are used in different studies, estimates of depressive symptoms among older Chinese vary greatly. Zhang et al. found that older Chinese had a pooled prevalence of depressive symptoms of 22.7% (95% CI: 19.4–26.4%).52 According to an updated meta-analysis, 19.9% of those 60 years and older in China reported depressive symptoms (95% CI: 13.9% - 28.6%) in 2011–2012.53 According to both meta-analyses, depressive symptoms are more prevalent in women (23.9%) than men (19.3%), and in rural (25.2%) than urban areas (20.6%). Furthermore, depressive symptoms decrease monotonically with education. There was no apparent age trend.
A ten-question version of the Center for Epidemiological Studies Depression (CESD-10) scale is used in the CHARLS data to measure depressive symptoms. Based on the 2018 CHARLS data, 42% of Chinese women and 29% of men showed elevated depressive symptoms. For both genders, rural residents have a higher prevalence (32% vs. 22% for men and 47% vs. 30% for women). Depressive symptoms grow monotonically with age among rural but not urban people. Illiterate adults suffer from 47.8% of depressive symptoms, while those with high school education and above have a prevalence of 20.9%.54 Depressive symptoms are associated with chronic pain in older adults. A CHARLS study found a positive correlation between pain severity and depressive symptoms.55
Anxiety disorders often accompany depression in older adults due to fears of falling, being unable to afford living expenses and medication, being victimized, being dependent, being alone, and being left alone.56 Older Chinese also experienced greater anxiety during the COVID-19 pandemic. The prevalence rates of anxiety symptoms among COVID-19 infected, healthy, and chronically ill individuals were 14%, 23%, and 85%, respectively, suggesting that we should pay particular attention to anxiety symptoms of older patients with chronic diseases during outbreaks.57
At its worst, depression can lead to suicide. Chinese suicide rates were among the lowest globally in 1999 with 5.29 per 100,000. Chinese older people, however, rank the third in the world.58 Chinese suicides show unique demographic patterns with age: the older group (aged 65 years and over) has the highest rate (44.3 to 200 suicides per 100,000), four to five times higher than the general population.58 Over the past three decades, suicides among older adults have decreased significantly. The national suicide rate of older adults significantly decreased from 76.6 in 1987 to 30.2 per 100000 in 2014: suicide rates among older adults decreased from 76.6 in 1987 to 30.2 in 2014.59
2.3.2. Dementia and Cognitive Impairment
The normal cognitive ageing process is associated with declines in cognitive abilities, which affecting decision making in late life’s daily living. It may be possible to achieve successful cognitive ageing by participating in certain activities, building cognitive reserves, and engaging in cognitive retraining. Some normal cognitive ageing may develop mild cognitive impairment and dementia over time.60
Dementia is a chronic disease primarily affecting older people that causes almost irreversible cognitive decline. Alzheimer’s disease (AD) and vascular dementia (VaD) are two of the most common causes of dementia. According to a multi-center survey of residents aged 65 or older conducted between 2008 and 2009 in China, dementia, AD, VaD, and Mild Cognitive Impairment (MCI) are prevalent to 5.14%, 3.21%, 1.50%, and 20.8%, respectively.61,62 In rural areas, dementia, MCI, and AD, but not VaD, were more prevalent than in urban areas, and differences in education may explain this.61,62 In 2013, there was a 5.56% prevalence of dementia among people aged 65 and above.51 Among people aged 60 and over recruited between 2015 and 2018, an age- and sex-adjusted prevalence of dementia was estimated at approximately 6.0%.63 China’s dementia surveys consistently show that it is highly prevalent.
MCI prevalence was found to be 12.7% (95% CI: 9.7% - 16.5%) in a meta-analysis of 22 community-based studies.64 According to another meta-analysis of 36 studies (total N = 114,592), community-dwelling adults aged 55 and older had a 14.5% prevalence of MCI (95% CI: 12.8% - 16.2%).65 MCI increased gradually between 2001 and 2015 (7.5% in 2001–2003, 12.1% in 2004–2006, 13.1% in 2007–2009, 16.9% in 2010–2012, and 19.5% in 2013–2015). There are considerable differences by geography. Shaanxi had the highest prevalence (20%–25%), followed by Inner Mongolia (15%) and Shanghai (10%). MCI prevalence increases with age and is highest among those over 90 (23.5%). There are significant differences in demographic characteristics; the prevalence is higher among women (16.0% vs. 12.6% in men), unmarried (16.4% vs. 13.1%), and rural residents (18.2% vs. 13.6%). Those with more education also have a lower prevalence of MCI: illiterate individuals had the highest prevalence (24.0%), followed by primary school students (20.1%), and higher education students (8.0%).63
2.4. Functioning independency and Disability
Although chronic illnesses can be debilitating, they do not necessarily cause one to lose independence when adequately treated and managed. Indeed, maintaining functionality despite having one or more chronic conditions is fundamental for healthy ageing.
2.4.1. Functioning independency
Functional independency is the ability to perform basic and instrumental activities of daily living. Activities of Daily Living (ADLs) measure the ability to carry on essential activities of functional living, and Instrumental Activities of Daily Living (IADLs) measure the ability to live independently in a community. Using the China Health and Nutrition Survey (CHNS), a longitudinal study with samples mostly in eastern provinces, IADL and ADL disability prevalence among those aged 60 and older declined from 1997 (38.9% and 13.2%) to 2006 (26.6% and 9.9%).66,67
CHARLS collected data regarding the functioning dependency in terms of ADLs and IADLs. ADLs include dressing, bathing, eating, using the toilet, getting in or out of bed, and continence; IADLs include cooking, shopping, making phone calls, managing money, doing housework, taking medications, and taking public transportation. According to a recent CHARLS study, those requiring help among the over 60 population, as indicated by ADLs, declined from 11.7% to 8.1% from 2011 to 2020. If determining care needs using both ADL and IADL items, the share requiring help declined from 24.5% to 17.8%.68 Disability prevalence has declined over the last few years due to improved educational attainment, age-friendly environments, and healthcare access. In 2011, the estimated number of people needing ADL/IADL help was 45.3 million and this number remained constant – the decline in the share of the population with disability and requiring help was offset by a larger population base and growth in older populations who were aged 60 years old and above.
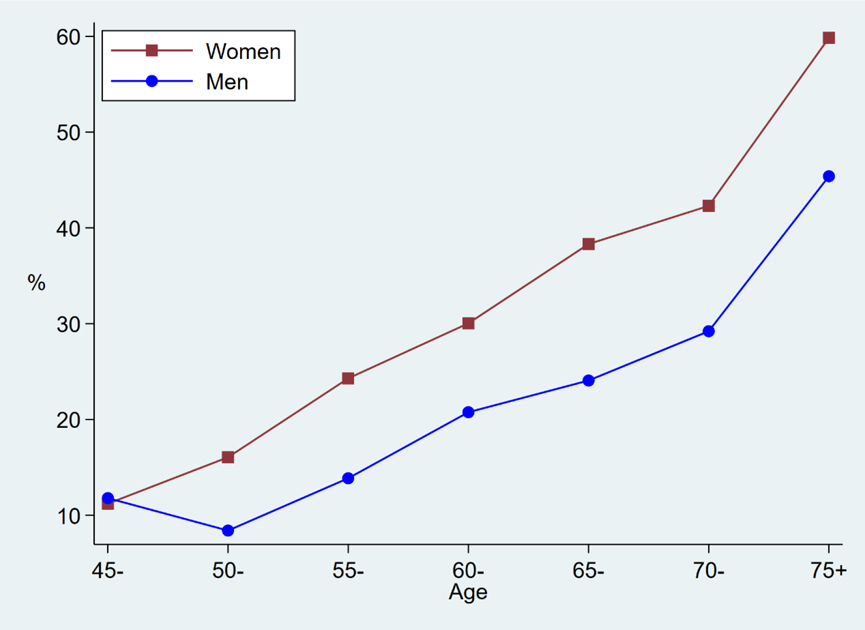
The ADL/IADL disability prevalence increases sharply with age (Figure 3). The prevalence of disability is higher among agricultural than non-agricultural hukou holders. An education gradient is evident: disability prevalence in 2020 is 49.2% among illiterate older adults, and 13.0% among those with high school degrees or more.
Figure 3: Disability rates by age and gender from CHARLS 2020 data.
2.4.2. Frailty and Sarcopenia
Frailty, another major risk factor for functional dependency, is a clinical syndrome characterised by the decline in the physiological capacity of multiple organ systems, resulting in increased susceptibility to stressors.69 Worldwide, there are two main frailty assessment methods, based on different conceptual models. Fried frailty phenotypes (FFPs) underlie phenotypic models. It suggests frailty is a syndrome characterized by physiological and metabolic changes. FFP determines frailty by three or more characteristics: weakness, slow gait speed, low physical activity, exhaustion, and unintentional weight loss. A second method is the frailty index (FI), which takes into account signs, symptoms, and diseases to analyze frailty. FI indicates how many potentially unhealthy measurement indicators there are in their physical, social, cognitive, and psychological measurements.70 The number of indicators and cut-off value of FI may vary depending on the research purpose. As an example, Li et al. constructed an FI consisting of 28 indicators based on CKB,71 while Gu et al. built an FI with 38 indicators based on Chinese Longitudinal Healthy Longevity Survey (CLHLS).72 Frailty prevalence varies due to differences in measures. Chinese older adults aged 65 years in 14 studies showed 8% and 12% frailty prevalence, respectively, in the FFP and FI.73 In a CHARLS study, the prevalence of frailty among 5330 older people aged ≥60 years was 9.6% for the FI in 2011.74 CHARLS also found an incidence of 60.6/1000 person-years of frailty among 4939 community older adults aged 60 and over over an average follow-up period of 2.1 years.75
Sarcopenia and frailty are linked, but distinct, correlates of musculoskeletal aging. Sarcopenia has received considerable attention around the world as an age-related disease. Sarcopenia is defined by the Asian Working Group for Sarcopenia (AWGS) 2014 consensus as “aging-related loss of muscle mass, weak muscles, and/or low physical performance.”76 In the AWGS 2019, the diagnosis and treatment of sarcopenia were updated. AWGS 2019 provides two assessment/diagnostic criteria for community and clinical settings. The AWGS 2019 introduced the concept of “possible sarcopenia”, defined as low muscle strength or physical performance in the community. 77
There was a 12.9% prevalence of sarcopenia in men and 11.2% in women in a meta-analysis of 24,879 community-dwelling Chinese older adults aged 65 years, based on AWGS 2014 criteria.78 A recent CHARLS study found a prevalence of 38.5%, 18.6%, and 8.0% of possible sarcopenia, sarcopenia, and severe sarcopenia, respectively.79
2.4.3. Falls and Fractures
Older Chinese are at risk of fall-related injuries, a major cause of disability. In China, the number of DALYs caused by falls increased from 27th in 1990 to 17th in 2017.9 Based on GBD data, the estimated incidence rate of falls among people aged 60 years and older was 3799.4 per 100 000.80 The WHO Global Ageing and Adult Health (SAGE) project in China reported that the incidence of fall-related injuries in the past year was 3.2% among adults 50 and older in 2010.81
In China, falls are the leading cause of injury-related mortality and traumatic bone fractures among older people.82 Over the past two years, a CHARLS study reported that 15.9% of men and 24.5% of women 60 and older experienced falls in 2015; among them 8.7% of men and women suffered serious falls. In comparison to older people with non-agricultural hukou, older people with agricultural hukou suffered more falls (21.3% vs. 18.1%) and fall-related injuries (9.1% vs. 7.6%). The illiterate experience more falls and serious falls than those with at least a high school diploma (24.0% compared to 11.4% for falls and 11.4% compared to 8.7% for serious falls in 2018).
Fractures are also a public health concern because they cause considerable morbidity, excess mortality, great risk of disability, and high societal healthcare costs. According to prospective studies in China, post-fall injuries occur in 60–70% of falls. A systematic review and meta-analysis found 54.95 injuries per 1,000 in mainland China. Of all falls, 10% are major injuries, and 6–8% are fractures.80 Of all fall-related injuries, 10% are major injuries, and fall-related fractures accounted for 6–8% of all injuries. Fall-related hip fractures are often the most serious and costly consequences of a fall. For females, hip fracture incidence rates were 180.72 (95% CI 137.16, 224.28) in 2012 and 177.13 (95% CI 139.93, 214.33) in 2016, and for males, the incidence was 121.86 (95% CI 97.30, 146.42) in 2012 and 99.15 (95% CI 81.31, 116.99) in 2016.83 There is a high prevalence of osteoporosis and fractures in China; 5.0% of men and 20.6% of women over 40 have osteoporosis, and 10.5% of men and 9.7% of women have vertebral fractures.84 China National Fracture Study (CNFS) showed that slips, trips, and falls (57.7%) caused the most fractures in older women and men, followed by traffic accidents (20.4%).85
Falls and fractures can be prevented. Exercise, nutrition, and home safety modifications can reduce falls.86 China has taken concrete measures to prevent falls by hardening rural roads, installing more streetlights, and building handicap access. Additionally, there are programs to provide handrails, anti-slip floors, and remove door sills for low-income families. (more in Section 6, Home Environment and Housing Policy). In 2021, the National Health Commission (NHC) issued 15 guidelines regarding fall risks, modifiable factors, prevention, education, and care for older people who fell.
2.4.4. Self-Reported Pain
Pain is associated with a greater risk of functional decline. Early-life adversity (ELA) such as parental neglect, physical abuse, and social stress can predispose adults to chronic pain.87
The 4th wave of the CHNS in 2008, which measured pain from one of the EuroQol five dimensions (EQ-5D) items: pain/discomfort in the interviewed day, showed that 18.3% of the over 60 population reported self-reported pain.88 According to CHARLS 2018, 67.8% and 53.2% of women and men over 60, reported experiencing pain. Pain is more common in agricultural hukou holders than in non-agricultural hukou holders (63.1% vs. 54.8%). There is a sharp education gradient here, with 48.5% of those with at least a high school education reporting pain, while 67.1% report pain among the illiterate.
2.4.5. Self-Reported Sensory Function
In 2017, sensory organ disease affecting vision and hearing was the third leading cause of years lived with disability (YLDs).9 In 2018, 27.6% of men and 36.3% of women aged 60 and over reported poor eyesight, while 18.2% of older men and 18.8% of older women reported poor hearing, according to CHARLS. Agricultural hukou holders had a higher rate of impaired sensory function (35.6% vs. 23.8% for impaired vision and 20.8% vs. 13.3% for impaired hearing) than non-agricultural hukou holders. Sensory function is also associated with education. Illiterates are more likely than high school graduates to have poor sensory function (42.1% vs. 20.1% have poor vision, 24.3% vs. 11.7% have poor hearing in 2018).
Using sensory aids contributes to the difference in sensory function between agricultural and non-agricultural hukou. Only 13.8% of older people wore glasses, and only 1.0% wore hearing aids. People with agricultural hukou are less likely to wear glasses and hearing aids (9.1% vs. 24.5% for glasses and 0.96% vs. 1.04% for hearing aids in 2018). In 2018, high school graduates are more likely to wear glasses and hearing aids than illiterates (30.9% vs. 6.3% for glasses, 1.0% vs. 0.8% for hearing aids).
2.4.6. Dental Health
Despite eating being vital for physical health, Chinese oral health is poor. Only 23% of older adults brush their teeth twice a day; only 5% use fluoridated toothpaste, and only 6% have had a dental checkup in the last two years.89 Tooth loss is the most important indicator of poor oral health, with edentulism being the extreme case.
According to the CHARLS 2018 wave, 26.0% of people aged 60 and older had edentulism. Women are more likely than men to be edentulous (28.2% vs. 23.7%). In agricultural hukou, 28.8% of those were edentulous versus 19.4% in non-agricultural hukou. Older people rarely see dentists; only 19.1% did in 2015. No obvious gender difference exists in seeking dental care. In 2015, agricultural hukous were much less likely to have dental care than non-agricultural hukous (15.4% vs. 26.1%). High school graduates are less likely to be edentulous and more likely to receive dental care than the illiterate (14.2% vs. 34.5% for edentulous in 2018, 29.3% vs. 14.2% for dental care in 2015).
2.5. Subjective Wellbeing and related conditions
2.5.1. Subjective Wellbeing
An evaluation of subjective well-being (SWB) allows us to sketch a more comprehensive picture of the health status of older individuals.90 Across the world, the age pattern of SWB reports has attracted substantial attention. Typically, a review paper observed a U-shaped age pattern regarding the SWB in 145 countries, the pattern was also found in China.91
A rapid expansion in education across birth cohorts also implies a strong negative correlation between education and age. Since both factors—economic resources and education—improve SWB but decline with age in China, the age profile tends to show an even sharper increase in SWB at older ages: positive cohort effects, in terms of more education and economic resources, tend to reduce the growth rate in SWB among older ages in China. Without those positive cohort effects, SWB would increase at an even more rapid flow at older groups.
A study investigated the relationship between social networks and SWB in China.92 Overall, their analysis indicates that maintaining good social networks in China is associated with better SWB. Concerning kinship relationships, they find the probability of being very happy is 13.8 percentage points higher for married people, while the likelihood of being very satisfied with life is 10.3 percentage points higher. Families with more visits to family and friends during the Spring Festival have a higher sense of well-being and satisfaction with life, and the more frequent such contacts, the higher the life satisfaction they could observe. One notably particular but also interesting finding is on gift-giving/receiving behaviour, the four groups of participants have ranked in terms of happiness and life satisfaction, with the both-giver-and-receiver group first, followed by the only giver second, the only receiver, and the neither group taken the last.
In these associations between SWB and social networks, it is essential to remember that both may be associated with both observable and unobservable dimensions of access to economic resources and vulnerability. While the nature of this association between SWB and economic factors such as wealth, inequality and economic growth and fluctuations, are constant and contested themes in the literature.93
Just as education and economic resources matter for individual happiness and life satisfaction, so are gender and residence. Adult men in China are less satisfied with their lives than women, and adults in urban places are less satisfied with their lives.92 Older women are happier than older men, and those living in cities are happier than those living in villages, although those living in townships do not differ much from those in rural areas.94
2.5.2. Skin conditions, urinary incontinence, and lack of sexual activities
In older individuals, skin and subcutaneous diseases (skin conditions), urinary incontinence and lack of sexual activities are among the most prevalent conditions that do not necessarily cause great physical pains or premature deaths, but can adversely affect the quality of life and SWB.
Skin conditions
Skin conditions are more common among older people because their skin is less oily, less elastic and thinner.95 Eczema, psoriasis, and pruritus are the most common skin conditions among older people. When left untreated, patients scratch the skin, which can worsen the condition. Skin diseases can affect older patients’ physical health, causing pain, sleep disturbance and itching.96
Age-related skin conditions can be easily prevented with emollients and soap substitutes. Because these conditions are not life-threatening, older Chinese tend to view them as nuisances and rarely seek treatment. Epidemiological and prevention studies of skin diseases in older people are rare. One study indicated that skin diseases significantly affect the YLDs. In 2017, there were 7.05 million YLDs due to skin disease, compared to 6.16 million in 1990 as a result of population growth and ageing.97
Studies have revealed that older adults with skin disorders have higher rates of depression, anxiety, inferiority, shame, social barriers, even suicidal tendencies and other negative psychological states.98 It is important to take good care of the mental health of older people with skin diseases, helping them overcome their anxiety and face the disease positively, as this is conducive to the realization of healthy ageing.
Urinary incontinence
Urinary incontinence is defined as the involuntary loss of urine. Older women are more likely to experience urinary incontinence due to weak bladder and pelvic floor muscles. In a literature review conducted between 2013 and 2019, 16.9–61.6% of Chinese older women reported urinary incontinence.99 Women predominate (56.3% of females and 35.0% of males) among Chinese rural residents aged 65 years and older.100 Since patients and caregivers lack a proper understanding of urinary incontinence, the actual prevalence rate may be higher than reported.101
Older people may reduce going out due to frequent bathroom needs. In addition, being embarassed by leaking urine leads to a shrinking away from social contacts. Consequently, the person experiences urinary incontinence and social isolation, leading to a higher risk of self-neglect and death. Urinary incontinence can be prevented or alleviated by pelvic floor muscle training. China has not yet popularized such training. Using adult diapers can prevent embarrassing leaks, but many older Chinese are ashamed of the practice.
Sexual activities
Sexual activities are generally associated with better mental health, self-esteem, marital quality, and SWB.102 Older people experience the same. However, in certain countries like China and India, it is taboo for older people to express their sexual expectations and desires.103,104
Currently, very little scientific literature exists on sexuality in later life, especially in China.105 A Chinese females are usually reluctant to discuss sexual issues because of a long history of conservatism and a lack of sex education.106 In a study conducted in Central China, approximately one-third of older adults consider sex abnormal or unhealthy in later life.107 The percentage of older women who engaged in sexual activity in perimenopause and postmenopause, respectively, more than once a week was only 18.4% and 2.8%, respectively.104 It has been found in several studies that older Chinese have relatively low levels of sexual interest and types of sexual activity.102,104,106
The lack of partners and limited social activities also prevent most older people from having access to the sexual experiences they need. It is important for older adults and their families, as well as medical practitioners, to realize that many older people are still interested in sex and are sexually active. Health education should consider sexual conditions, and physicians should be instructed to ask their older patients about their sexual concerns.
Section 3. Determinants of health status of Chinese older people
Understanding health and functional status determinants are essential to prioritizing interventions in policymaking. In China, as elsewhere, health at older age result from the cumulative effects of behaviours and eventsthroughout their lifespan. These include exposure to parental decisions influencing in-utero and childhood health, health behaviours in adulthood (including smoking, drinking, and physical activity), and diet and nutritional status, many of which are heavily affected by socio-economic conditions. Less directly, the unobserved dimensions like socioeconomic position (SEP) may have additional influence on physical and emotional well-being, associated with the interaction within the family and community. Finally, environmental hazards are an unavoidable challenge for health. This section summarizes current evidence on these potential influences on the health status of older people in China.
3.1. In Utero and Childhood Health
Growing evidence suggests that ageing begins early in life, during which family and community environments play ireeplaceable roles. Childhood, and even as early as in utero circumstances, may be influential factors in hralthy ageing.108–110 Studies demonstrating the negative impacts of adverse early life circumstances and perturbations on well-being in old-age have exploited both retrospective information and the exposure to the severe nutritional events during China’s Great Famine.
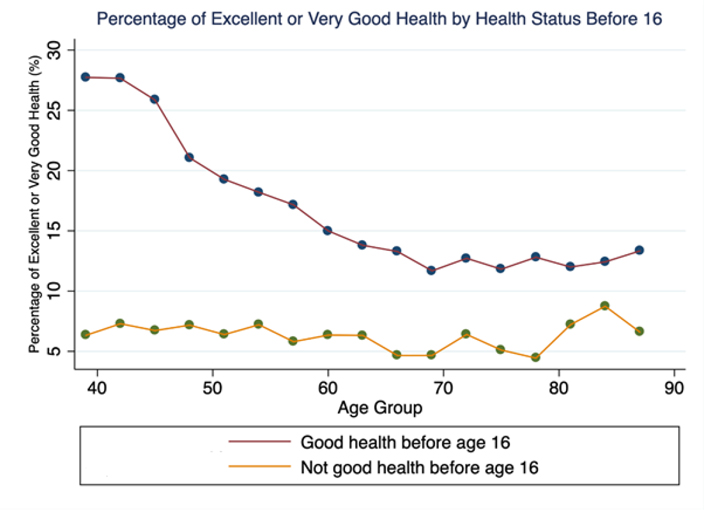
Back the data from the CHARLS survey, for example, respondents self-reported their child health status before age 16, while the comparsion with the current health status is shown in Figure 4. Childhood advantage in good health evidently persists over time, which that consistently higher than for those in poor childhood health and without improvement.
Figure 4: Self-rated Health among Middle-Aged and Older Adults by Child Health.
Source: CHARLS National Sample (2011, 2013, 2015)
Notes: In this figure, each respondent in the longitudinal survey is only counted once. In cases when a respondent participated in multiple waves of survey, information on the earliest wave of participation is used in plotting the figure.
Health outcomes may be impacted even more by adverse events during the first two trimesters of pregnancy. 108 For example, the Great Famine of 1959–61, to which most Chinese over 60-year-olds today were exposed at some point in their early lives, has been linked to several diseases in late life. The famine, coupled with a ‘rich’ nutrient environment later in life, may add to health risks in old age, especially for those with high incomes.109 Malnourished people may have developed a “thrifty genotype” to cope with adversity during the 1959–1961 famine. Undernutrition, however, was followed by rapid economic development since 1978, leading to nutritional abundance and a higher risk of obesity, type 2 diabetes, and CHD.110
In recent studies, comprehensive domains of risk factors have been assembled to understand how child factors may coalesce and show up in health disparities later in life. This will further promote the efficient allocation of resources in a way that mitigates health disparities. Research, for instance, has shown that in China, low educational attainment is among the most relevant risk for late-life frailty, followed by poor childhood health, poor neighbourhood quality, and low paternal education.111
3.2. Health Behaviours
With the population agieng in China, the health issues of older people have gained greater attention from all sectors. Considering the impact of unhealthy lifestyles on ageings’ health from multiple perspectives, including smoking, alcohol consumption, sedentary lifestyles, and diet, is essential to promoting “healthy ageing”.
3.2.1. Smoking
The harms of tobacco exposure are to nearly all organs of the body and all ages of society, and smoking is one of the leading causes of death for men in China. During the 2010s, it is estimated that smoking caused 20% of all adult male deaths in China,112 with 33.6% of male deaths attributable to smoking in 2019.113
Smoking prevalence has declined in China, as it has in many other countries, but the increase in the population has not resulted in a decrease in the total number of smokers.113,114 Between 1980 and 2012, the prevalence of daily tobacco consumption decreased by 8.1% (53.2% to 45.1%), while the number of smokers increased by about 100 million (182 million to 282 million).113,114 In the absence of widespread cessation, China’s tobacco-related deaths are projected to increase from about 1 million in 2010 to 2 million in 2030 and 3 million in 2050.113
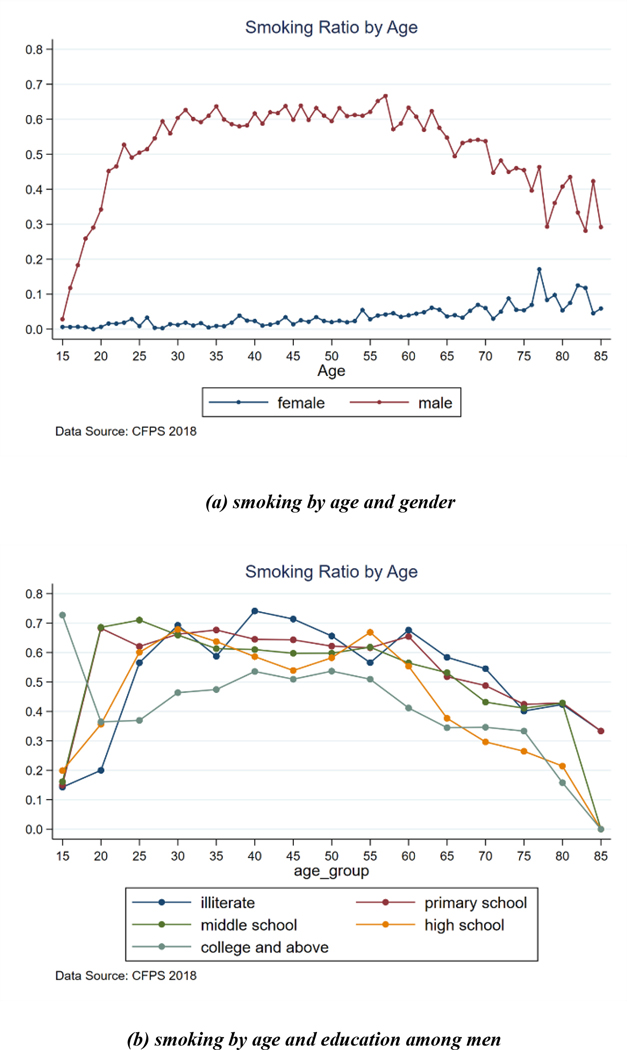
China has one of the highest smoking levels worldwide, especially among men. According to GBD 2019 Tobacco Collaborators, 49.7% of men and 3.5% of women older over age ten in China smoke, and the former is 17 percent higher than the global picture.113 According to the 2018 wave of Chinese Family Panel Studies (CFPS) data, smoking increases drastically at school-leaving ages115, while some cessation occurs after age 55. The difference in smoking for higher education obtained versus other education levels is significant (Figure 5), and the similar situation exists for older men in agricultural hukou versus non-agricultural hukou (49.6% vs. 39.5%), regarding the 2018 CHARLS survey data.
Figure 5: Prevalence of smoking among the Chinese population from CFPS 2018 data.
3.2.2. Alcohol consumption
Globally, alcohol use was the seventh leading risk factor for both deaths and DALYs in 2016, and studies have linked alcohol consumption to 60 acute and chronic diseases116 while dependent drinking can also lead to injury and potential self-harm or violence. In China, the drinking prevalence among men remains higher than in most other HICs,117 the share of drinkers engaging in harmful drinking behaviours increased over the past decade,118 but the prevalence of alcohol dependence has remained high over the past three decades which is similar to that found in western countries.119 Excessive alcohol consumption is associated with increased mortality from other diseases such as cancer, with liver cancer accounting for more than 60%.120 In China, 4.4% of all cancer deaths were attributable to alcohol consumption, with a male bias (6.7% in men, 0.4% in women).
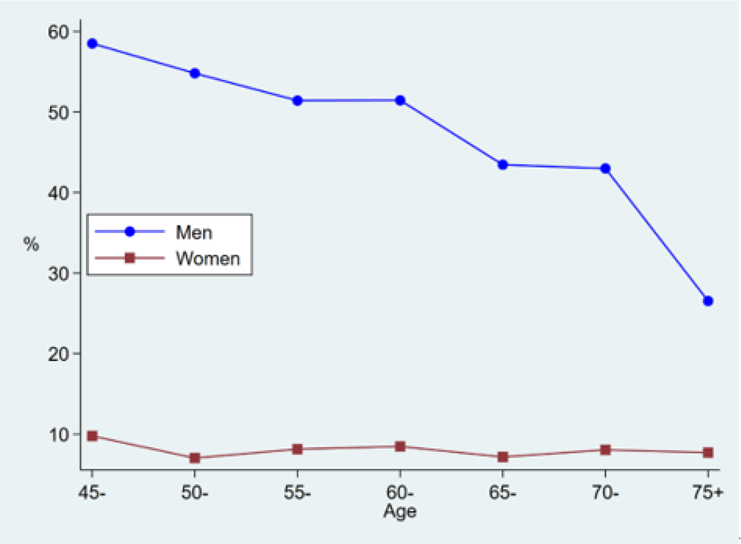
Like smoking, alcohol consumption is primarily a male phenomenon in China, but women catch up quickly. In 1991, among those aged 15 and older, 35.1% of men drank while only 2.6% of women did under the definition of drinking wine, beer, baijiu or yellow rice wine more than 50 grams a month; in 2002, d for the same range of alcohol, the proportion drinking at least once a week rose to 39.6% (growth of 12.8%) and 4.5% (growth of 73%), respectively.120 In 2007, among those age capped at 69, 55.6% of men and 15.0% of women reported consuming any alcoholic beverage over the past 12 months with 62.7% and 51.0%,respectively, drinking excessively.121
CHARLS provides reliable national estimates of drinking among older adults. As men age, their drinking declines sharply, while women drink much less in every cohort (Figure 6). In 2018, 41.3% of men and 7.8% of women aged 60 and older drank. For hukou, drinking prevalences were not significantly different, but education was positively related, with an increase from illiterate (36.2%) to high school and above (45.9%).
Figure 6: Prevalence of drinking among the middle-aged adults from CHARLS 2018 data.
3.2.3. Physical activity
National physical activity has declined with domestic economic development and urbanisation. The CHNS showed that, compared to 1991, average weekly physical activity among adults in China fell by 32% (in 2006).122 According to the CLHLS, Chinese oldest-old persons have become more sedentary and solitary in the past 2 decades. The odds ratio for television viewing among China’s oldest old increased by two to three times since 1998, and both recreational activities, including playing cards and Mah-Jongg, and exercise decreased.123
Over 80.3% of those 60 and older participated in mild physical activity, 42.4% in moderate and 23.0% in vigorous activity, according to the CHARLS survey. Vigorous activities were more popular among men (27.1% vs. 19.1%), and agricultural hukou holders had a higher participation rate than non-agricultural hukou holders (27.8% vs. 12.2%). Rural-urban differences in physical activity are mainly due to their different purposes. Among older Chinese men, participation in the labour force is higher than among women, and rural people work more than urban residents.124 Among those reporting physical activity, 45.0% of men reported activity related to work demands, but only 35.5% of women. In urban areas, 50.4% of people with agricultural hukou reported physical activity associated with their work, compared to 16.2% of people without agricultural hukou. Illiterates were more likely to engage in vigorous activities (24.5% vs. 17.8% in 2018) and to report that physical activities were required for labour work (47.0% vs. 23.4%).
3.2.4. Diet and nutrition
Food scarcity in China was conquered before the 1990s. As a result, it has evolved from a traditional diet high in carbohydrates to one high in fats, sugars, and sodium in packaged processed foods and beverages, and an increase in animal-based foods. Dietary diversity not only brought benefits but also led to an increase in diet-related diseases, such as chronic conditions and cancer. 125
China’s food consumption patterns vary greatly. According to China Kadoorie Biobank (CKB), the main cereal consumed every day was rice in southern China and wheat in northern China.126 Western regions consumed the most livestock meats and dairy products, eastern regions consumed the most poultry and eggs, and eastern and central regions consumed the most aquatic products.125 Regional diet patterns may explain regional health differences. Studies show regional dietary preferences can predict diabetes, hypertension, and body mass index.127
In China, nutritional excess and deficiencies coexist. The CHNS reported both dietary quality problems and dietary imbalances in the older population in 2009.128 Despite excessive intake of cereals, oils, and salt, respondents showed moderate to serious deficits in fish, vegetables, fruits, milk, and soybeans. There was no deficit in meat consumption.
Other studies have found that more than 30% of dietary energy was from fat,129 while inadequate intake of fruits, vegetables and protein was noted after 2010.125,130 A study in Singapore studied sarcopenia in 92 older adults and found that a regimen of physical exercise over six months was able to reduce the severity of respondents’ symptoms.131 Since sarcopenia is related to protein deficiencies, and the Singapore study suggests that protein deficiency is a potential major problem in the diets of Chinese older adults.
Undernutrition has also been documented among older Chinese, especially underweight, defined as BMI less than 18.5. In CHARLS data for respondents 60 and older, 7.7% were underweight, and 12.6% were undernourished. The prevalence of underweight was 47.1% in persons aged older than 80 years, and participants who were underweight suffered from the highest risk of CVD, non-CVD, and all-cause mortality.132
Chinese scholars have conducted intervention studies, which provide evidence for forming public health policies, including reducing salt intake. The results of a large-scale cluster randomised controlled trial conducted in 20,995 Chinese participants aged ≥60 years with hypertension showed that the prevalence of stroke, major cardiovascular events and all-cause mortality in participants who used salt substitutes were lower than participants using ordinary salt.133
3.3. Social Environments
A substantial body of literature suggests that social networks, or the structure of social ties, are important social determinants of health and overall well-being.134 Further, the association between social networks on health in the older generation is particularly noteworthy because of the cumulative nature of exposure. Social networks operate through social support, social engagement, or social integration. While these terms are often used interchangeably, they have different meanings and are often associated with specific health outcomes.134 What’s more, it is important to note the implicit associations of social networks with observed and unobserved dimensions of socioeconomic well-being and vulnerability.
The discussion below emphasizes the positive relationship between social networks, social participation, and health status. Next, “empty nest” households are discussed, and the harm older people may suffer when they lack family in close proximity is highlighted. Finally, in a discussion of square dancing among older Chinese people, the benefits of physical activity are emphasized.
3.3.1. Social Networks and Social Support
People are surrounded by supportive others during their lifetime, and these constitute the social network and support, while the former has structural characteristics135 and the latter has functional characteristics. 136
Social networks and the support and social engagement derived from social relationships contribute to morbidity, mortality, and well-being. Coronary artery disease, all-cause mortality, cancer, and CVD mortality are independently predicted by social networks. In older adults, social relationships are associated with fewer depressive symptoms, better cognitive functioning, less functional disability, and better SWB.137
Over the past four decades, China’s social relationships have reflected both traditional values about family ties and support, as well as massive socioeconomic changes. Rural and urban areas have different social networks and participation. For instance, the massive out-migration and the heavy work associated with urban development have led to less social interaction and this change continues to occur.138
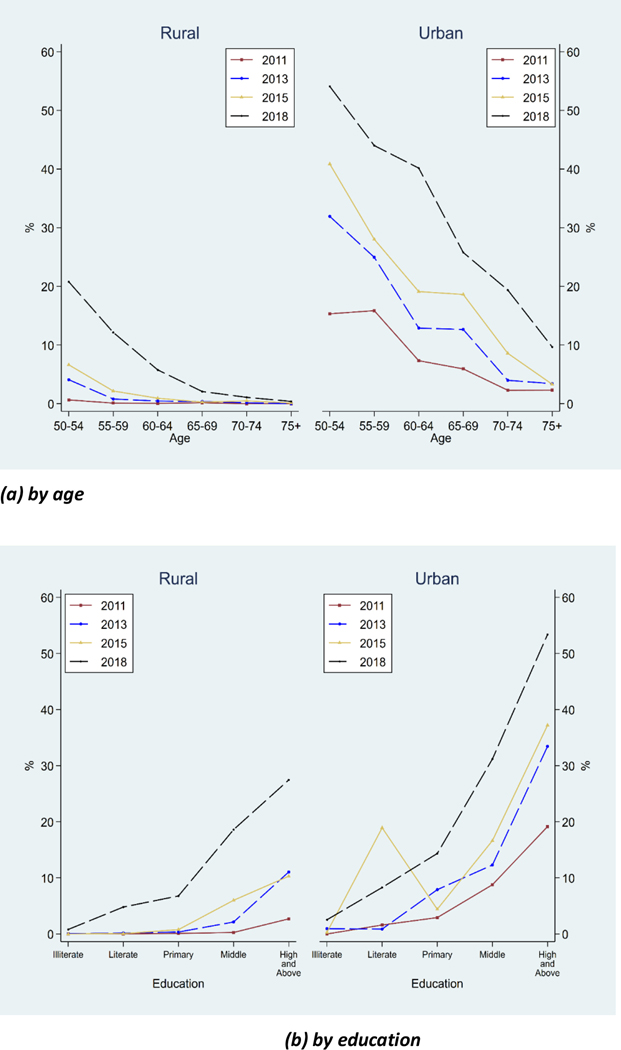
Technological developments, represented by the Internet, can connect people across distances and maintain or expand social ties. CHARLS data show that from 2011 to 2018, the number of people aged 50 and older using the Internet grew from 2.9% to 14.8%, while the distinct gaps in technology adoption between rural and urban areas and across age groups (Figure 7). For instance, the expansion of internet use is greater among urban residents and the more educated (Figure 7). In 2018, 31.9% of urban residents 50 and older used the internet, while the rate was 8.0% among rural residents. Older people are much less likely to adopt the internet. In 2018, only 3.5% of those 75 and older used the internet, while 28.6% of those 50–54 used the internet.
Figure 7: Prevalence of Internet use by education among the adults aged 50+ from CHARLS data.
Of particular interest is the association of certain group activities, such as playing cards and mahjong, with cognitive ability. Organized social activities may be mediated by physical exercise and cognitive ability, with different social activities having different mediating pathways.139 This study demonstrates the specificity of social network structure and function in health outcomes.
However, in other longitudinal studies, we have found that social support is not a strong predictor of maintaining cognitive ability, but rather that social engagement is a stronger predictor. This finding would suggest that participating in games that require older men and women to draw upon cognitive skills by the very nature of the activity and level of social engagement may promote healthy brain ageing in terms of cognition.
3.3.2. Demographic Transitions and Social Network Structure: The Case of Empty-Nest Older People in China
Families and households are integral parts of social networks. As life expectancy has improved significantly in many countries, fertility has decreased, and geographic mobility has increased, the empty nest situation has become more common. Besides economic changes, the one-child policy has also contributed to this situation in China. The number of older Chinese living in “empty nests” is estimated at 59% in 2011.140
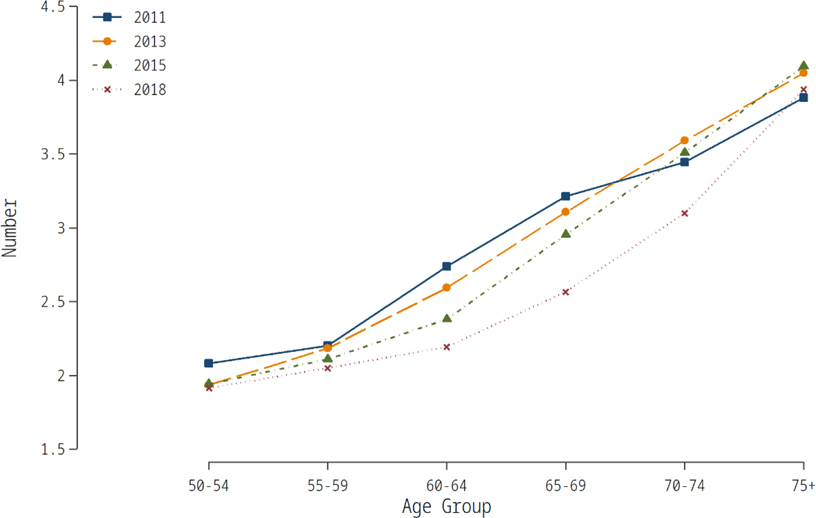
As a result, family support is important in China. Among older Chinese, family support is positively associated with psychological well-being and self-reported health, as reflected by higher life satisfaction and lower depression rates. Also, family support protects older adults from loneliness, whether they are empty nesters or not. Since most empty nesters have children nearby, family support is currently available, but that will change in the future.140 Figure 8 shows a dramatic decline in the number of children by cohorts. In 2018, those 75 years and older had 3.94 living children, but those aged 55–60 only had 2.05. With the out-migration of children, it will be difficult to expect children to live nearby. The stress of living in urban areas in China may make it hard for young migrants to provide support to their rural parents.
Figure 8: Number of living children among the adults aged 50+ from CHARLS data.
3.3.3. When Social Activity and Physical Activity are One: The Case of Square Dancing in China
Disaggregating the social from the physical aspects that lead to health benefits is especially challenging in research, while Tai Chi and square dancing stand out as two typical examples in China of physical-social activities.Square dancing, a type of social activity for older Chinese in which people perform various dances in public areas, has grown in popularity in recent years. A recent study estimated that there are over 100 million people who participate in recreational square dancing in China.141 And square dancing is found to be positively associated with cognition and mental health among older Chinese.142
Social networks and the support and engagement they provide have important health impacts worldwide. Recently, Chinese research has shown that the structural aspects of networks, such as the shared support, the size and composition of the network, and the joint physical and cognitive activities inherent to many social activities, are important predictors of physical and mental health. It is essential to gain a deep understanding of both the upstream social and economic forces influencing China’s society and the multiple pathways leading to healthy longevity. The use of longitudinal data sources and careful identification strategies will be important for future research to verify causality in relationships between social networks and physical health.
3.3.4. Ageism and elder abuse
WHO defines ageism as “the stereotypes (how we think), prejudice (how we feel) and discrimination (how we act) directed towards others or oneself based on age”.143 Ageism could arise in institutions, interpersonal interactions, and even when people are categorised based on their age. As an example, when fatalities occurred on construction sites, many local governments in China reacted by prohibiting people aged 60 and above to work in construction sites. T he prohibition limits older rural migrants’ job opportunities and reduces income security. Ageism in China was further exacerbated by the COVID-19 pandemic. The initial phase of Covid-19 vaccination did not include people over 60. Even after older people were permitted to receive shots, the oldest-old are usually discouraged because they are perceived as having a higher possibility of adverse reactions. Because of these policies, China’s older people have far lower immunisation rates, making them more vulnerable to infection. Recently, the Chinese government reversed its policy and offered financial incentives to inoculate older people.
Elder abuse consists of intentional acts that cause injury or serious injury risk to vulnerable older adults, as well as caregivers’ failure to meet the basic needs and to provide safe living conditions for the older people,144 have been recognized as a globally important public health issue. There are several types of elder abuse, including physical, psychological, emotional, and sexual abuse, as well as neglect.145 Elder abuse is a prevalent problem in China. A meta-analysis of 11 cross-sectional studies involving 23,020 older participants found the overall prevalence of elder abuse in China to be 20.29%.146 The third Chinese Women’s Social Status survey in 2010 indicated that the overall prevalence of elder abuse was 7.0%.147 The COVID-19 pandemic has also further exacerbated elder abuse. During COVID-19, a survey of 10,362 older people aged 65 and over in Hunan Province, China, found that elder abuse was occurring with a prevalence of 15.4%.148 More efforts are needed to prevent elder abuse.
3.4. Physical Environment
Rapid economic growth in China has led to environmental pollution and climate change. Deteriorating environmental quality affects older people’s health. According to the GBD study, 2.76 million deaths and 59.29 million DALYs were caused by environmental risk factors in China in 2019.149
Besides premature mortality, environmental pollution has adverse health effects that persist into old age. Older adults are also susceptible to environmental risk factors, and most deaths and DALYs related to environmental factors occur in them (Figure 9). There are five environmental factors among the top 20 risk factors in China that cause disability in people aged 70 and older.
Figure 9: GBD Study estimated China DALYs (A) and deaths (B) by environmental risk factors and age at death, 2019. DALYs, disability adjusted life years.
Considering China’s unique environmental problems and demographic characteristics, we summarize the effects of environmental issues, climate change, and how age-friendly environments on older people’s health in China.
3.4.1. Environmental hazards and climate change
Recently, a number of high-quality longitudinal studies on China’s older population have provided a window into the long-term impact of environmental factors on older people’s health. Chinese studies have linked ambient air pollution to dozens of diseases, mainly CVD, respiratory disease, and lung cancer.150–153 In addition to these well-established associations, longitudinal studies in China have found associations between air pollution and other health outcomes including diabetes, disability, fall-related injury, poor sleep quality, and presbyopia.150,154 Air pollution also affects cognitive and mental health.155 There was a decrease in depressive symptoms score during the Clean Air Policy in China based on results from three waves (2011, 2013 and 2015) of the CHARLS.156 Life expectancy is expected to increase if ambient particulate matter 2.5 (PM2.5) concentrations are reduced, according to a model based on 72 Chinese cities.157 One quasi-experimental study report that improved air quality during 2014 and 2018 is associated with beneficial changes in the cognitive function.158,159 These studies jointly suggest that clean air policies should be implemented as public health measures in countries with ageing societies, especially LMICs with a high air pollution burden.160
Older adults spend more time at home and are more likely to be exposed to indoor environmental toxicants, including air pollutants.161,162 However, fewer studies have focused on associations between health outcomes and household air pollution (HAP) from solid fuel consumption like coal and biomass (e.g., charcoal, wood, crop residues, and animal dung) in Chinese older adults. A recent CHARLS study found significant associations between HAP from solid fuel use and depressive symptoms in older Chinese.163 Other studies reported that solid fuel use was associated with chronic lung diseases, heart diseases, and poor sleep quality in older Chinese.162
Contaminants in water, such as biological agents, chemicals, disinfectants and disinfection by-products, threaten human health.164 The main causes of deaths induced by water pollution were acute and chronic gastrointestinal diseases. Over the past 25 years, partly due to the increased proportion of the population accessing improved water sources, the incidence of water-related infectious diseases in China has declined steadily (Figure 10).149 Meanwhile, NCDs related to water pollutants have begun to raise attention. Studies have found that clusters of cancer cases in China appear to be closely related to locations of major rivers. Consistent with this, many industrial parks are also located in these river basins, which are the likely sources of carcinogenic effects from industrial discharges in water. In recent years, new health risks, including risks to reproductive health and metabolic diseases, were found to be associated with typical chemical contaminants (e.g., polycyclic aromatic hydrocarbons, heavy metals, and disinfection by-products) in water.165
Figure 10: Incidence of cholera, typhoid or paratyphoid and dysentery in China from 1990 to 2019. Chinese Ministry of Health: 2019 health yearbook.
China has acknowledged climate change, but health risks have not received enough attention.
On the one hand, climate change directly threatens human health by causing extreme weather events, like typhoons, floods, heatwaves, cold snaps, and storm events. In spite of the lack of exact data, it is believed that most deaths from extreme weather conditions occur in older people. People over 75 years of age are most at risk of mortality from extreme temperatures, according to a nationwide study in 272 Chinese cities.166 On the other hand, climate change could indirectly affect human health by enhancing the adverse impacts of air pollution, a major public health threat for Chinese people. As an example, the high temperatures in Wuhan, amplified the effects of PM10 on non-accidental, cardiovascular, and cardiopulmonary mortality.167
3.4.2. Age-friendly environments
The commitment to creating more age-friendly, supportive environments for the ageing populations has become a central element of strategies and action plans for active and healthy ageing in China. Age-friendly home modifications can reduce the functional dependency of older adults.168 According to the “China’s implementing age-friendly home modification projects for the older residents”, the goal of age-friendly community promotion is “to develop a model and long-term mechanism for creating age-friendly communities, to better meet the needs of older people in terms of their living environment, everyday travel, health care, social participation, and spiritual and cultural life, and enhance their sense of access, wellbeing, and security.169 The Age-friendly retrofitting contains seven domains: Flooring, doors, bedrooms, toileting and bathing facilities, kitchen equipment, physical environment and equipment for daily living.169
Age-friendly home modifications can improve social and occupational participation and feelings of safety, lower the fear of falling, and reduce the risk of LTC for low-income older adults.170 Older adults can prevent frailty (i.e., need for low/moderate level of care increasing to high level of care) and early mortality with home modifications including handrails or corridors.171 In a randomised controlled trial, home modifications reduced disability and improved quality of life as well as mental health for older community residents.172
According to China’s fourth survey of older people’s living conditions, 58.7% believe their housing needs to be modified, with 63.2% in rural areas. In urban areas, more than half of older residents say their housing lacks emergency call systems, handrails, and adequate lighting. In addition, slippery floors, uneven thresholds, and poorly functioning toilets or bathrooms are common problems.173 A number of positive changes have occurred in China regarding home modifications. According to the CHARLS survey, the percentage of households with running water has increased from 67.9 in 2011 to 91.9% in 2020; the percentage of households with toilets has increased from 74.7 in 2011 to 89.3% in 2020, and the percentage of households that have sitting toilets has increased from 31.2% in 2011 to 49.5% in 2020.68
Section 4. Policy Initiatives to Promote Health and Care for Older People
Access to healthcare is an important channel through which SEP influences health and functional status throughout one’s life. Over the last few decades, the Chinese government has introduced a number of policies that directly or indirectly affect health of older people. In particular, China expanded health insurance to all in 2003 and launched a major health reform in 2009 with the goal of providing all citizens with equal access to basic healthcare of reasonable quality with sufficient protection from financial risk.174 The 2009 reform goals were further expanded by the Healthy China 2030 Strategy, which established the importance of improving population health in advancing the country’s long-term economic and social development goals. This section first reviews and evaluates these policies, which form the necessary foundation for a comprehensive aged-care system.
Due to increases in life expectancy, decreased fertility, and a historic movement of population from rural to urban areas, China’s traditional family support system for older people is under stress.175 Establishing a sustainable LTC system that builds on and supports family-based care is pressing in light of the fact that population ageing will continue over the next 30 years.2 As most older people will continue to receive care from family members in the home, the government of China has focused on expanding the LTC system through a “90-7-3 model,” which aims for 90 percent of all seniors to receive any required care in their homes, 7 percent through community-based hospitals and health centers and 3 percent through nursing homes. Under this arrangement, the wellbeing of older people will depend not only on the availability of informal care from family members, but also on the quality of complementary care provided through community centers and formal institutions. This section reviews evidence on care through family members and current gaps in care,176 discusses efforts to promote community-based solutions capable of easing the burden on family care providers, and evaluates evidence from LTCI pilots in China with a view toward the potential for financing both institutional and community-based care. Finally, this section discusses recent policy initiatives to integrate healthcare and social care.
4.1. Health Insurance
Before the late 1990s, China had only one form of medical coverage, the Free Medical Service (gongfei yiliao) offered to urban employees free of charge since the 1950s. As part of the urban enterprise reforms in the 1990s, urban workers in non-government sectors transitioned to the Urban Workers Basic Medical Insurance (hereafter referred to as the Urban Workers Insurance) funded in part by individual contributions. A New Rural Cooperative Medical Scheme (NRCMS), introduced in 2003, provided health insurance to all rural residents and is the most significant component for extending health insurance coverage to most of the Chinese population. The Urban Resident Basic Medical Insurance (UBMI), introduced in 2009, filled remaining coverage gaps by offering insurance to urban residents who are not covered by the urban workers’ insurance. The two types of resident health insurance schemes are financed by individual contributions and government subsidies. With introduction of the UBMI plan, every Chinese citizen became eligible for medical insurance and over 96% have enrolled. In 2016, the central government called for the merger of the NRCMS and the UBMI into one unified scheme - Rural and Urban Resident Basic Medical Insurance (hereafter referred to as the Resident Insurance scheme). The merger of these two schemes was completed in 2019.
The Urban Workers Insurance has covered both inpatient and outpatient services since its inception in 1998. The Resident Insurance benefit packages are less generous, initially only covering hospitalisation, but has been greatly expanded since 2016. The expansion of outpatient benefits for chronic conditions under the Resident Insurance scheme is of particular significance for the older population. While most cities in China cover outpatient care for diabetes and hypertension, only a small number of cities cover complications deriving from these diseases. The depth of coverage (for example, deductibles, copayments, caps) varies by cities across China’s three regions. In general, Urban Workers Insurance is more generous than Resident Insurance. To the extent that older people are more likely to experience higher health expenditures and/or to suffer from major chronic health conditions, the expanded health insurance coverage and the outpatient reimbursement policy are likely to disproportionately benefit them. A number of studies have shown that expansions in insurance coverage increased healthcare utilisation177 and reduced patients’ out-of-pocket (OOP) expenditure for inpatient services in China178. The evidence on health outcomes is mixed. Some studies found no effect on health outcomes,179,180 while a recent study by Gruber et al. (2021) find that the New Cooperative Medical Scheme (NCMs) program had significant health benefits mostly affecting the older population.181
Despite great achievements made in the past 20 years, China’s health insurance system still faces many challenges, the most significant of which is the segmentation by program types and by localities.
The three major forms of health insurance are segregated by occupations and differ in generosity. The most generous Free Medical Service is offered to public servants, military personnel and certain government-run institutions. The second most generous insurance, Urban Workers Insurance, is offered to workers in urban areas. The least generous type, the Urban and Rural Resident Basic Medical Insurance, is available to rural residents and urban people who do not qualify or want to join the Urban Workers Insurance. To illustrate the difference in generosity between the latter two insurance types, the annual premium is 6586.6 RMB for Urban Workers Insurance and 833 RMB for Resident Insurance In 2020. The national average of reimbursement rates for inpatient service in 2020 was 85.2% for Urban Workers Insurance participants and 70% for Resident Insurance participants and retirees under the Urban Workers Insurance do not pay any premium while those under Resident Insurance must make regular premium payments.182 Additionally, those with Free Medical Service and Urban Workers Insurance require minimum of years of participation to enjoy the same insurance after retirement, which creates barriers to job mobility: those whose shifts in employment require moving between workers’ and residents’ insurance face reduced likelihood of qualifying for higher quality, free health insurance after retirement.
Another dimension of segregation is locality. For the most part, both Urban Workers’ Insurance and Resident Insurance are pooled at the county or city levels. Localized pooling has several ramifications, including differences in generosity, variation in financial pressures migration (migrant-origin regions face deficits while migrant receiving regions have surpluses), and penalties for migration in the form of lower reimbursement rates for expenses incurred outside of home locations. In addition, patients who seek treatment outside their home health insurance jurisdictions have to cover their full medical expenses and then submit all paperwork to their home offices for reimbursement. This onerous, and often unsuccessful, process creates a strong disincentive for older people to move to live with children when they require assistance with daily needs.
Since 2016, the government has initiated efforts to remove the penalty for out-migration by establishing a unified settlement system across regions. As of 2021, the settlement system for inpatient services was successfully implemented for all health insurance programs, but this has been infeasible for out-patient services related to major chronic illnesses, primarily due to variations in local reimbursement rules and the lack of common IT systems supporting the vast heterogenous array of service providers covering outpatient services. Moving all facilities to a common IT system poses complicated coordination problems over both system features and cost-sharing.181
4.2. Public Health Promotion
Since 2006, the prevention and control of NCDs have become part of the Five-Year Plans issued by the State Council. In 2009, China launched the National Essential Public Health Package, providing free public health services. This package has expanded over time and prominently features healthcare for older people. For example, older adults can receive free influenza vaccinations, annual lifestyle evaluations, physical examinations, and health guidance. Patients with hypertension or type 2 diabetes are given priority for health management, including free tests and follow-up visits. In 2017, Health Literacy Promotion Action was added to improve awareness and understanding of risk factors for and health practices related to hypertension, diabetes, and common infectious diseases such as tuberculosis and HIV/AIDS. The practice guidelines under the Program have been updated several times since then (see Table 1 for a list of services over time).
Table 1:
Essential Public Health Services
| Before 2009 | 2009 | 2015 | 2018 | 2020 | |
|---|---|---|---|---|---|
| Cost (Yuan) | 15 | 40 | 55 | 74 | |
| Establishing health records for all citizens | √ | √ | √ | √ | √ |
| Health education | √ | √ | √ | √ | √ |
| Children’s health management | √ | ||||
| 0–36 months | √ | ||||
| 0–6 years | √ | √ | √ | ||
| Maternal health management | √ | √ | √ | √ | √ |
| Vaccination | √ | √ | √ | √ | √ |
| Surveillance of infectious diseases and public health emergencies | |||||
| Infectious diseases | √ | √ | |||
| Health Management for older people, patients with hypertension, type 2 diabetes and psychosis | √ | √ | √ | √ | |
| Health Supervision and Management, Chinese medicine management, and TB health management | √ | √ | √ | ||
| Contraceptives | √ | √ | |||
| Health Literacy Promotion Action | √ | √ | |||
| Others * | √ |
Sources: National basic public health service specification 2009, 2015, 2018.2020.
Others* include: 1) prevention of the endemic diseases, occupational diseases, prevention and control of human avian influenza and SARS, and maintenance of national health emergency team, 2) screening of breast and cervical cancer for women in rural area, 3) nutrition improvement for children and neonatal disease screening in poverty-stricken areas; 4) folic acid supplementation and fortification to prevent neural tube defects, national free pregnancy eugenics health checkup project, prevention and control of thalassaemia, etc.
In 2016, the blueprint of “Healthy China 2030” was formally released by the State Council. The initiatives outlined in the document work towards the national goal of reaching a health standard on par with HICs by 2030. In the blueprint, health service and health insurance for NCDs, as well as healthy lifestyles were listed as important indices for healthy China, which is a momentous endeavor to raise public health for NCDs to the level of a national strategic goal. In 2019, a corresponding action plan was released by the State Council, which encompassed 15 goals to be achieved between 2020 and 2030 with specific targets and benchmarks for moving from the blueprint to action.183 Furthermore, in response to the key principles of Healthy China 2030 and with the focus on NCDs, the State Council issued the “Medium-to-Long Term Plan of China for the Prevention and Treatment of Chronic Diseases (2017–2025)” in 2017. Eight concrete and interconnected strategic measures covering various aspects of prevention and treatment of NCDs were proposed, which also serve as milestones for policy initiatives targeting reduced NCD incidence in China.
4.2.1. Health Literacy Education
Health literacy refers to an individual’s ability to access, process, and comprehend basic health information and services and to use them to make appropriate health decisions.184 Increasing health literacy has been identified by the WHO as an important strategy, measure, and priority for improving public health,185 and inadequate health literacy among older individuals poses significant public health concerns in LMIC countries, including China. Health literacy among older Chinese adults has improved in recent years but remains at a low level, with substantial disparities between urban and rural areas. According to the 2021 CHARLS survey, knowledge of chronic diseases such as CVD and dementia and of how to prevent or to manage these conditions showed considerable scope for improvement. Only 60.2%–74% of respondents understood the 11 areas of health literacy important for the prevention and control of CVD, and only 42.5%–57.5% understood the two health literacy areas important for management of dementia. (Figure 11).
Figure 11: Health literacy towards prevention and control of chronic conditions among Chinese older adults, date derived from the CHARLS 2021 survey.
4.2.2. Health Management for NCDs
Under the national strategy for combating NCDs, there are comprehensive supportive policies (Figure 12). To ensure the quality of primary healthcare by standardizing practices, the government has released national guidelines for primary care providers covering the prevention and control of hypertension (2017) as well as diabetes (2018), and also lists of essential medications for treatment. Implementing both are facilitated through rapid development. Current online healthcare services remain tightly regulated: patients must first see a doctor face-to-face before shifting on-line, and web-based diagnostic services are limited to local doctors. Nevertheless, online healthcare provides a more efficient way to manage chronic diseases for older people by local healthcare providers. If regulations are relaxed in the future, online healthcare services may play a larger role in the health management of NCDs.
Figure 12: Policy initiatives of major non-communicable chronic diseases in China.
4.2.3. Web-Based Health Services
Web-based health services, m-health and a centralized electronic system provide new ideas to promote the health of older adults. Since 2015, the Chinese government has issued more than 50 policy documents to support the development of Internet medicine, involving the construction of Internet hospitals, the development of telemedicine, the inclusion of online healthcare services in medical insurance reimbursement, and online sales of prescription drugs.186 A previous study on China’s telemedicine platform from 2014 to 2020 showed that the development of telemedicine in China experienced rapid growth, especially benefiting older adults in underdeveloped areas.187 However, there is a huge digital divide among Chinese older adults, limiting their access to and use of web-based health services. In China’s largest online medical platforms, few users are over 60 years old.188 In November 2020, the Chinese government issued a policy aiming to bridge the digital divide by urging the development of age-friendly APPs. To date, how to overcome the digital divide remains an important challenge for China’s healthy aging.189
Similarly, online healthcare services have also played an important role in the prevention and control of infectious diseases, and have seen explosive growth since the Covid-19 pandemic. According to the NHC, China added 146 Internet hospitals from January 1 to April 30, 2020,190 and the health services delivery by Internet hospitals increased 17 times over the same period in 2019. These hospitals provide preliminary diagnoses over the internet and deliver prescription drugs to communities and homes through local pharmacies.191
4.2.4. Effects of Public Health Management Programs
From limited research evaluating the effects of health literacy promotion, some common themes emerge. Although health management services are free to older people, participation is low, especially in rural areas. One study found that from 2016 to 2017, only 46.7 percent of eligible older individuals in Beijing received free examinations, compared to a target of 80 percent. While a nationwide survey was more favorable, the interviewees were not randomly selected, .and participation rates were likely overestimates.192
4.3. Primary Health Care and Integrated Delivery System
To strengthen the gatekeeper role of primary healthcare for NCDs, a series of policies and opinions were released by the government, including more investment in primary healthcare,193 building up the referral system, creating a contracting system for family doctors, expanding capacity for educating and training general practitioners, and increasing the incentives for primary healthcare providers.194 Because older patients face greater difficulties in accessing tertiary hospitals and often require company during their hospital visits, these measures are likely to be particularly beneficial for older adults.
Motivated in part by the increasing burden of NCDs associated with population ageing, the State Council issued guidelines for building a “tiered health care delivery” system in 2015. Under the tiered health care delivery system, health facilities at each level deliver services according to their designated functions. The primary function of hospitals is curative care. Primary care providers serve as patients’ first point of contact for care and are responsible for delivering the National Essential Public Health Package services, which include both health promotion and prevention, and health management and maintenance for chronic conditions. Rehabilitation centers and nursing homes are designated to provide rehabilitation and nursing services for non-communicable disease patients in stable condition, patients with rehabilitation needs, older individuals, and patients with terminal cancer. Ultimately, a unified electronic health information system would enable streamlined coordination among providers at different tiers, and a standardised referral system would be put in place to integrate the provision of care across secondary hospitals, tertiary hospitals, and rehabilitation centers.
A family doctor registration system was introduced in 2016 to complement the tiered delivery system. Under the registration system, Chinese residents register with a family doctor team based at a primary health care institution, who is paid on a capitated basis to provide them with basic medical care and preventative medicine, as well as to serve as a gatekeeper to the rest of the health care system. The government set a target of universal registration by 2020.
However, six years have passed, and China is still far from achieving this goal of establishing a tiered health delivery system. Even though community health centers have been built with government funds near every community, they are much underutilized. On the contrary, tertiary hospitals have siphoned more resources and carried out more medical services proportionally, taking over the services that could have been more conveniently handled at the community health facilities. Family doctors have not played their designated roles even though nominally all patients have been assigned a family doctor. The cause for the heightened monopoly power of tertiary hospitals is a resource allocation system that favors higher level hospitals. Under this system, larger hospitals receive more resources from the government, and their doctors have higher salaries and promotion opportunities. Consequently, community health centers cannot attract good doctors and patients do not trust these facilities and choose to seek medical care in more distant hospitals, even for common chronic diseases. Furthermore, community-level facilities and designated family doctors are deprived of incentives to provide quality care. All revenues are handed over to the government and doctors are paid by the government regardless of the quality or quantity of their medical services. The only incentive is for them to provide health management and maintenance for chronic conditions, as the amount of fees given to the facilities depends on the number of patients with chronic diseases (hypertension and diabetes) under their management.195
4.4. Geriatric Medicine
Because older patients often suffer from multiple diseases, their health needs are best met by geriatricians who can provide comprehensive assessment of their health conditions and prescribe internally consistent medications and treatment. Prior to the late 1980s and early 1990s, geriatric medicine was only available to high-ranking officials, but designated departments resembled modern geriatric wards.
Since 2011, China’s government has actively promoted the development of geriatric medicine., By 2013, nearly all tertiary hospitals had departments of geriatric medicine, and a 2017 policy has promoted departments in secondary hospitals as well..
The proliferation of departments dedicated to geriatric care, does not mean that care is now available. The shortage of trained geriatricians means that most geriatric medicine practices in China have yet to offer comprehensive treatment. As of 2019, only 40 percent of medical schools were authorised to grant master’s degrees in geriatrics, and only 0.34% of the master’s degrees in clinical medicine granted in 2015–2016 were for geriatric medicine. Many physicians who joined geriatric medicine departments were trained as cardiologists, pulmonologists, nephrologists, and other specialists in internal medicine, and career incentives motivate these physicians to focus on their core areas of specialty, and not geriatric medicine.196
4.5. Hospice Care
Hospice care, also called palliative care, aims to relieve the pain and symptoms of terminally ill patients while also caring for their emotional and spiritual needs. The WHO describes palliative care as an approach that improves the quality of life for patients and their families when facing life-threatening illnesses, through the prevention, assessment, and treatment of pain and other physical, psychological, and spiritual problems. Hospice care or palliative care aims to help terminally ill people approach death with dignity and in peace and comfort.
During the past few decades, China has made substantial progress in promoting hospice and palliative care.197 While the concept of hospice care was introduced in the 1980s, efforts to expand have only occurred in recent years, with practice guidelines for hospice care issued in 2017, and pilot areas selected and expanded in 2019,.198 Despite recent progress, palliative care in China continues to face challenges, including insufficient education and training resources, the absence of a legal framework to support patient autonomy, insufficient funding and resources to establish palliative care teams, shortages of pharmaceutical supplies, and a lack of research on attitudes toward death in a rapidly changing society.199 For example, it is taboo for Chinese people to talk about death in traditional Chinese culture, which affects both knowledge of hospice care and willingness to accept it. In addition, medical colleges seldom offer hospice degrees and courses; therefore, Chinese medical students lack knowledge of hospice care.200
4.6. Long-Term Care System
4.6.1. Family Caregivers and Gaps in Care
As in many other LMICs, support for older people in China, whether financial or in the form of instrumental care, is primarily the responsibility of the family, and most studies of care in China note the primary role of sons and their spouses as the main caregivers.201 According to the 2020 special wave of the CHARLS survey, only 1.5% of older respondents requiring care received help exclusively from hired caregivers (including from the nursing homes), while children (including their spouses) remain the dominant care providers (58.5%).202 A slightly lower share (58.1%) receives assistance from a spouse.
The rapid demographic transition over the last four decades has led to a dramatic decline in the number of living children for CHARLS respondents as one moves from older to younger age cohorts: an older person aged 80–84 has an average of four living children, but those aged 70–74 have only 2.8, and many (11%) of the young-old, aged 60–64, have only one child. Future older people will have even fewer children to support them.201 At the same time, with increased migration to cities, the proportion of children living outside the village/county significantly increased from 48% in 2011 to 57% in 2018, implying that the distance of children from their hometowns (and parents) is gradually increasing.203 Consequently, the family, as the traditional dominant care provider, will face growing challenges meeting the needs of older adults and may become a less reliable source of care. Already, there are severe unmet care needs. The 2020 special wave of CHARLS shows that 17.8% of the population over 60 requires assistance with at least one ADL or IADL. Among those who needed help, 11% did not receive care.
Failure to meet care needs may have serious consequences on the wellbeing of older adults. The onset of difficulties with physical mobility, for example, may be better counteracted with the availability of a care provider. In the absence of a care provider, there is a danger that minor mobility problems will more quickly deteriorate. As physical mobility is essential for maintaining social activities, which are associated with better cognitive ability204 and less likelihood of depression, the inability to maintain mobility may lead to deterioration of other dimensions of wellbeing. Relative to older adults who receive appropriate LTC, those who have unmet needs are more likely to have a lower quality of life,205 suffer greater psychological stress,206 have more hospital admissions and readmissions,207 and have a higher rate of mortality.208 These findings suggest that the availability and adequacy of care are especially important for older adults who need LTC.
4.6.2. Impact of Providing Care on Care Providers
Providing care to a family member can be both physically and emotionally demanding. The burden of assisting with bathing, eating and using the toilet for someone with a physical limitation requires that the care provider is sufficiently healthy. A significant body of research points to adverse effects on the health of informal care providers.209 Providing informal care significantly reduces the SWB of caregivers, and earlier research has found this effect to be more pronounced for women.209
In China, informal care providers are unpaid and are most often family members, but could be other acquaintances, community members or volunteers. Informal providers may be contrasted with formal care providers, who typically have formal training and work through some type of facility (either an institution, such as an LTC facility or hospital, or a community-based facility). As noted from studies using CHARLS, adult children are often important providers of care: 43% of adults receiving care had assistance from adult children in the CHARLS 2011 baseline.201 When children are care providers, they may be drawn out of the workforce or have less time available for work. Using the 2011 and 2013 waves from CHARLS data, one finds evidence that caring for an older parent is associated with 5.9 and 4.4 percentage point declines in the probability that rural men and women are working, respectively, and that urban women in households with infirm older work 2.9 fewer hours per week.210
In China, as elsewhere in the world, spouses tend to be the primary providers of care if sufficiently healthy, and they tend to assume greater burdens and provide higher quality care than other providers. Various studies report negative effects on the mental health of spousal caregivers, but these may be driven by factors other than care provision, including the fear of losing a lifelong companion, worse initial health status due to their age, and fewer outlets to relieve pressure due to a smaller community of peers. Further, spousal caregivers may have fewer burdens than children as care providers: adult children have their own families and work responsibilities.211
Given the preponderance of informal support provided by spouses in China, a recent study draws on data from 2011, 2013 and 2015 waves of the China Health and Retirement Survey (CHARLS) to examine the effects of providing care on spouses. When both a husband and wife are still alive, however, the spouse plays a dominant role in care provision. Evidence from three waves of CHARLS (2011, 2013 and 2015) suggest that when both spouses are alive, 67.8% and 59.4%, of men and women, respectively, receive care from a spouse.212 Women providing care for a spouse are 14–15 percent more likely to suffer from depression than women who are not caregivers, whereas this gap is 6–9 percent for men, and women caring for a spouse are 8 percent more likely to have physical pain while this is only true for 5 percent of men. 212 Notable also in this study are the benefits of additional assistance, which allow a reduction in time providing care and/or sharing psychological burdens of providing care. With additional help, depression and physical pain associated with being a spousal care provider are reduced significantly.212
4.6.3. Institutional and Community-Based Care
An important solution to the problems facing families lies with encouraging the development of community-based care services that may relieve the family caregiver burden and reduce the negative consequences of unmet care needs on the health and wellbeing of infirm older people.
Institutional care
Historically, institutional care for older people in China is rare and limited to a small number of publicly supported welfare recipients, who continue to be supported. In urban areas, these are the “Three No’s” (san wu): people without the ability to work, have no source of income, and have no legal guardians to support them or whose guardians do not have the ability to support them, and in rural areas, those who qualify fall under the “five guarantees” (wu bao): older people who are guaranteed food, clothing, medical care and burial expenses by the local government. Most residential care homes for social welfare recipients are run by the state, municipalities, local governments or collectives.
Starting in 2011, the government issued a series of policies to encourage the establishment of LTC facilities by the private sector. With growing consumer demand and government support, residential aged care facilities have expanded significantly in both the public and private sectors, although in urban areas, the private sector has dominated recent growth. While social welfare institutions (which exclusively served social welfare recipients and were financed and run by the state) once dominated the landscape, private sector facilities account for the most recent growth.213,214 The current system has two types of institutional care for older people: one directly owned and managed by the government, and the other market-driven and developed, owned and run by the private sector.175
Quality of Care
The quality of public welfare institutional care facilities, including those with private sector funding or taking paying clients, tends to vary with the level of government under which it is organized. Those under a municipal government tend to have long waitlists, are better equipped and offer more services than those operated by lower-level county governments. In general, observers have found lower occupancy rates in private facilities relative to government-run facilities in large urban settings. Using data from Nanjing and Tianjin in 2009 and 2010, occupancy rates were 69 percent and 76 percent in private facilities, respectively, and 83 and 91 percent in government facilities.215 The lower occupancy rate in privately operated facilities in urban areas may reflect some mix of higher prices and lower quality.
The few case studies examining the quality of institutional care in urban areas suggest considerable heterogeneity both geographically and across public and private sectors. A recent survey-based study of 515 residents in nine long-term care facilities in Shanghai suggests that the quality of life, social support and perceived empowerment of residents are positive, and further notes that these outcomes are significantly better for residents of government owned-privately operated facilities than in those facilities that are both owned and operated by the government.216 In another study, based on interviews with residents in facilities in central and eastern China, residents describe significant unmet care needs related to pain and functional limitations. In the face of service gaps and inadequate direct care, residents adopted a range of self-management coping strategies.217
In China’s rural areas, anecdotal reports describing conditions in rural homes for the aged (jing lao yuan) suggest low occupancy rates with more than half the beds empty.218 A combination of poor conditions, few services and amenities, bad reputations, and persistent stigma associated with living in facilities contributes to underutilization. Even among the target clientele, elders with little income, disability, and no family support, there is a strong reluctance to use these facilities. Older people from families who prefer higher quality care and have more resources are even less likely to use these facilities.219
Community care
Research from the international literature has highlighted likely complementarities between formal care (from institutions or from professional care providers) and informal care (provided by family members). The possibility of complementarities between formal and informal care suggests an important role that expanding community-based health and social services for China’s older adults may play in meeting their care needs. Since the 1990s, the Chinese government has launched several initiatives to promote community-based social service programs. Most of these initiatives have been health-related, such as house calls, emergency aid, adult day care programs, health and wellness clinics, and recreational activities.220 Home- and community-based care for older people programs have also emerged and expanded in recent years, but they are largely concentrated in major metropolitan areas,221 and even there, existing services remain spotty. In recent years, care for older people programs has been promoted in rural areas, but the scope of these service centers or stations is mainly limited to recreation and sometimes meals for older people who are able to attend.
Demand for community-based eldercare services appears to be significant, but the history of these centers suggests that they face difficulty providing services without adequate government subsidies. An early example was the Starlight Program, under which the government-funded construction and operation of 32,000 Starlight Senior Centers nationwide from 2001 to 2004, yet these centers apparently did not serve their intended purpose. After 2005, the Starlight Program lost momentum due to dwindling financial support from the government, raising questions about the viability of similar initiatives.
In urban areas, community-based social services are typically managed and organised by quasi-governmental community organizations and delivered primarily by private small business service providers and volunteers.220 Services at the community level are usually of two types, one of which is the physical community center. Physical community centers can include the provision of cooked meals, organization of social activities, basic diagnostic health checks, rehabilitation equipment and rehabilitation through basic exercise, assistance with personal tasks, companionship, and service referrals. The second type of community services now offered in China is provided through information networks that link community services to seniors. Many local communities host a hotline specifically for seniors, which is either set up and staffed by the local Department of Civil Affairs or outsourced to a private vendor. In addition to community centers, some private companies and non-governmental organizations (NGOs) have trained eldercare workers and coordinated their services for disabled seniors who cannot leave their homes.222
Expanding both types of community-based services are premised, in part, on increasing the role of local government and community responsibility in the provision and delivery of services for older people. Services may also be distinguished by whether they are funded by public welfare assistance funds and therefore targeted at low-income beneficiaries of the dibao (government-provided minimum living guarantee for the needy) system, or other programs and community-oriented initiatives funded from public or private sources.220 As many of these services require some payment, they are affordable only to older populations with some financial ability. Services for poorer older adults are targeted directly by the government and are usually delivered free or at a minimal charge. But the provision of these services depends on local funding, the availability of staff, and the enthusiastic participation of the community.
4.7. Longterm Care Insurance (LTCI)
In countries with universal health insurance coverage, patients requiring LTC often occupy hospital beds for extended periods of time, and their needs can be more efficiently met by LTC arrangements. In a few countries with government-financed and managed health insurance, such concerns gave birth to LTCI as an addition to health insurance.
China’s hospitals, especially tertiary hospitals, have been burdened by patients receiving long-term medical care in their inpatient units. With inpatient hospital beds occupied at capacity, there is often a limited supply for new admissions. The high medical costs associated with long inpatient stays also place significant stress on health insurance programs, prompting the government to impose limits on hospital stays. From 2014 to 2020, China’s central government initiated LTCI pilots in 15 cities to provide an alternative to hospital-based LTC, permitting medical services to be carried out in long-term care facilities or homes, often supplemented with social care support. Local governments have also administered LTCI programs on their own. By the end of 2020, LTCI had expanded to 49 cities. As a result, the number of LTCI participants increased from 44.6 million in 2017 to 108 million in 2020; and 1.93 million people have benefitted from using LTCI. Facing the challenge of a growing demand for LTC.223 A mandatory, public LTCI system operating on social insurance principles, has become a policy alternative under consideration by the Chinese government, and this calls for a timely and effective review of the LTCI experience in China. The following section makes use of evidence from the original 15 LTCI pilots to describe current LTCI schemes and implementation problems.
The LTCI schemes differ considerably across the 15 pilots in the target population, premium level, co-payment, eligibility, benefit scope and financial mechanism.
Participants.
Under current LTCI schemes, all Urban Workers Insurance enrollees are covered in the 15 pilot cities; in 7 cities out of 15, this scheme extends to Resident Insurance enrollees. The total number of LTCI participants (as of June of 2018) was 57.45 million, with 78% enrolled in Urban Workers Insurance (Table 2). As the health status of rural older people is worse than urban counterparts,224 failure to include Resident Insurance enrollees in the LTCI scheme might become a new source of inequality between residents of rural and urban areas. In the pilots where both Urban Workers Insurance and Resident Insurance enrollees are covered, the benefits for Urban Workers Insurance participants are generally more generous than those of Resident Insurance.
Table 2:
The implementation status of social LTCI in 15 pilot cities in China
| N | % | |
|---|---|---|
|
| ||
| Total number of participants (person, million) | 57.45 | 100.0% |
| Urban Employees’ Basic Medical Insurance participants | 44.76 | 77.9% |
| Urban and Rural Residents’ Basic Medical Insurance participants | 12.69 | 22.1% |
| LTCI income (yuan, million) | 4179.67 | 100.0% |
| Employers | 6.40 | 0.15% |
| Individuals | 496.61 | 11.9% |
| Medical insurance | 3317.69 | 79.4% |
| Public Finance | 354.33 | 8.5% |
| Welfare lottery public fund | 4.64 | 0.1% |
| Total number of beneficiaries (person, thousand) | 184.58 | 100.0% |
| Beneficiaries in institutions | 72.90 | 39.5% |
| Beneficiaries at home | 111.68 | 60.5% |
| LTCI payment (yuan, million) | 720.43 | 100.0% |
| Benefits | 556.33 | 77.2% |
| Eligibility assessment | 15.89 | 2.2% |
| Others | 148.22 | 20.6% |
| LTCI balance (yuan, million) | 3454.42 | |
Note: Statistics were estimated in June 2018 and obtained from the National Healthcare Security Administration.
Eligibility.
Qualification for an LTCI benefit is based on the severity of a disability. Four cities extend coverage to people with moderate disabilities and three to those with dementia. Ten out of 15 pilots use the Barthel index to assess functional ability. Other pilots, including Shanghai, Suzhou, Shangrao, Qingdao, and Chengdu, developed local assessment tools.
Benefit scope.
Aiming to promote access to basic daily life care and related nursing care institutional care is covered in all pilots, and in 12, formal home-based care is covered as well. Availability of care, however, is associated with the development of the local LTC market. In areas with under-developed LTC markets, home-care subsidies are provided instead of physical care. In some pilots, like the city of Shangrao, free training on care provision is provided for beneficiaries’ children, spouses and other informal caregivers. As of June 2018, 61% of beneficiaries live in their own home and receive in-kind or cash benefits.
Financing mechanism.
As in many countries implementing social LTCI, the 15 LTCI pilots follow a pay-as-you-go mechanism. What sets China apart from these countries is that in all the 15 pilots, the LTCI premiums mainly come from the healthcare insurance program, whereas in the other countries, LTCI has independent funding. In only three cities of the 15 Chinese pilots, the participants provide additional funds and in one city, the employer provides extra funds. The government contribution comes from local public finance or welfare lottery funds. Based on statistics from the National Health Security Administration (NHSA) (Table 2), the total LTCI premium income was 4.18 billion yuan as of June 2018, with nearly 80% from social medical insurance accounts, 12% from participants, and 9% from public finances.
In pilot cities, the LTCI programs have achieved the intended goals of reducing hospital utilisation and medical expenditures. Not only have the social healthcare insurance accounts in some provinces gone into deficit, but also reduced the financial independence of LTCI. Fiscal deficits are likely to increase with population ageing, and it may be difficult for LTCI to be sustained under a pay-as-you-go framework.225 Further, the experience of Japan highlights a considerable public finance risk as the population ages.226
4.8. Integration of Healthcare and Social Care
With universal health insurance coverage and growing incomes, demand for healthcare services has grown rapidly. The ratio of health expenditure to GDP grew from 3.96% in 1990 to 6.43% in 2018. However, the supply of healthcare services has not kept pace with demand. The pinch is felt disproportionately by older people. Institutional care facilities are often built-in suburbs with no hospitals nearby. Even for older people living in their residential homes, going to the hospital is often a major hassle.
Since 2013, China has made yi-yang-jie-he, or the integration of health care with LTC across care settings, a priority on the aged-care policy agenda. There are essentially four different models: (1) aged-care facilities set up their own internal medical facilities to enable onsite medical practice, (2) medical institutions establish their own post-acute care and/or LTC facilities, (3) health care providers (particularly hospitals) partner with aged-care facilities to provide patients with integrated care through two-way referrals (the hospitals contribute medical services and the aged-care facilities contribute post-acute care and LTC services), and (4) hospitals and health centers dispatch health care practitioners to deliver medical services to older people in their homes or in community-based aged-care settings. Since 2016, China has been piloting these models in 90 localities across the country.
However, the progress on integration has been slow. As of the end of 2020, eldercare institutions that have a medical license accounted for less than 1/3 of the beds in all facilities. Very few hospitals have incentives to set up eldercare facilities or to provide medical services to these facilities or to patients in their homes.
The main obstacle to integration lies with regulations on the provision of medical services and the lack of incentives for hospitals to provide services. Heavy regulations of the healthcare sector in China contributes to high entry barriers. In recent years, the central government has repeatedly called for lowering entry barriers and simplifying the application processes for new medical facilities. In 2018, the responsibility for making policies on healthy ageing was moved from the Ministry of Civil Affairs (MCA) to the Commission of Health, and then on to a new Department of Healthy Ageing. One key objective of this restructuring was to pave the way for a relaxation of regulations in health sector policies governing healthcare and social care for older people. Despite the efforts of this department, local governments still insist on regulating entry. Although it has become relatively easy to establish a clinic within an elder care facility, regulations prevent doctors from seeing patients outside of facilities. With few patients in the in-house clinic, elder care facilities cannot afford to provide full-time medical staff.
As the great majority of older people receive care at home or community-based care centers, in-home medical services are an important part of the integration of health and elder cares. At present, however, doctors in China’s hospitals do not have incentives to visit patients at home. Doctors in community hospitals are paid fixed salaries which will not increase with more patients served and tertiary hospitals have neither sufficient staff nor incentives for staff to visit patients at home. Second tier hospitals may have capacity, but service fees, which are tightly regulated by the government, are too low to sufficiently compensate for the transportation cost and the time spent on route. In addition, laws governing physician practices stipulates that doctor can only practice where they are registered, which is in a hospital, not a home. While the rationale aims to protect doctors and nurses from liability in case of medical emergencies, this law imposes an additional legal risk for doctors even if they are willing to see patients in their homes.
Section 5. Outlook and Policy Recommendations
5.1. Outlook
This report has highlighted both the current circumstances of China’s older population and potential challenges in the future. Specifically, current older adults already confront the challenges of living autonomously as they age, including accessing appropriate health care to cope with NCDs, which are increasing in incidence, and coping with problems associated with finding suitable informal or formal LTC assistance when they require it. With respect to securing the well-being of China’s future older population, economic growth and increases in educational attainment both contribute to improvements in lifetime health status, but as highlighted in Section 2 in the report, these improvements are uneven across urban and rural areas. Over time, there is also a risk that higher incomes and a sedentary lifestyle are contributing to behavioral changes that may heighten the risks of developing NCDs, which may affect well-being at older ages. This outlook section first summarizes the evidence presented earlier in the report before areas for constructive policy intervention are discussed below.
Several factors are likely to improve the health and the functioning of older people in China. Continued economic growth will further improve the population’s nutritional status, education attainment, and health consciousness, especially among China’s less affluent citizens. Over the past four decades, more than 850 million Chinese have been lifted out of poverty, and the government declared the elimination of absolute poverty in 2021. The impacts of economic development on childhood and working-age adult outcomes re well established across social science literatures As cohorts that have benefited from these improvements transition to old age, the health of the older population will likely improve.
The benefits of economic growth on the health of the older population are unevenly distributed, exemplified by the large urban-rural differences in health and physical and instrumental functioning detailed in Section 2. This health gap mirrors an urban-rural income gap -- urban residents have an income of nearly 2.6 times the earnings of rural residents in 2020. Another prominent example is the gender gap in health outcomes – as Section 2 shows, women who typically live longer than men and are more likely to be widowed in their later years tend to fare worse in almost all health dimensions. As a result, some investments in healthy ageing may be directed specifically toward women of advanced ages. There are also some ethnic differences in terms of chronic conditions and functional disabilities. The prevalence of hypertension, diabetes, overweight, and ADL/IADL disabilities among non-Han ethnic groups was higher than that of the Han ethnic group, while the prevalence of CKD disease was higher among Han than in non-Han groups.
Educational levels increased substantially between 2011 and 2020, according to CHARLS data. The increase in educational attainment may contribute both to improved health outcomes and higher standards of living at older ages. In the Ageing Trajectories of Health: Longitudinal Opportunities and Synergies (ATHLOS) study, results from eight harmonised cohorts from USA, UK, Spain, Europe, Australia, Japan, Korea and Mexico also show the substantial benefits of early education for health and functioning in older age.227 Increasing educational attainment thus stands as one long-term investment that also promotes healthy ageing in China.
While increasing educational attainment and economic growth raise the prospect of health improvements, they are also potentially associated with lifestyle changes that may increase the risk of NCDs, with some negative consequences for health at older ages. Most important among these is persistent smoking, particularly among men, and the continued initiation of smoking among younger age cohorts, raising the prospect that cancer risks associated with smoking are unlikely to decline significantly in the future without more focused efforts at tobacco control. Beyond smoking, the shift toward a sedentary lifestyle has led to changes in diet and activity, which may increase the risk of obesity and related CVD.
Apart from tobacco, alcohol consumption is also associated with an increased incidence of cancer (primarily cancer of the liver), CVD and other illnesses. While problem drinking may be less severe than in the past, the share of drinkers engaging in harmful drinking behaviors increased in the past decade,118 and the current estimate of alcohol dependence among Chinese men approaches the level of western countries at 5.7%.119 Unlike patterns observed for cigarette use, alcohol consumption increases with educational attainment, raising the prospect that increases in SEP may not necessarily correspond to a decline in alcohol-related illnesses.
Increases in SEP in recent decades is associated with improved dietary diversity in China, but also a more sedentary lifestyle and a greater incidence of overweight, obesity and diet-related NCDs. Given that roughly 16% of cancers and NCDs diagnosed in China can be associated with diet-related factors affecting mortality risks,125 finding ways to reduce these risks while also focusing on fighting undernutrition in China’s poorer areas will be another serious challenge facing health policy.
Risks associated with lifestyle changes may be lessened with the expanded utilisation of health care services. Both the reforms of China’s health insurance programs since the late 1990s (Section 4.1), and new efforts to strengthen primary healthcare delivery (Section 4.3) may contribute to increased utilisation of health services and improved health status among both current and future cohorts of older adults.
Beyond access to health care, the well-being of older people may be affected by a range of factors related to their living environment and changing family structure. Due to changes in family size, living arrangements and migration, fewer family members will be available to help the aged in the future. As a means of alleviating problems related to physical isolation as older people develop difficulties with mobility, the Chinese government is actively encouraging modifications to buildings to remove physical barriers. This will better enable older people with disabilities to get into and out of buildings and help them to maintain their independence. Under policy recommendations below, we go into greater detail regarding the importance of making buildings more accessible to China’s ageing population.
5.2. Policy Recommendations
While economic growth and improved educational attainment are part of China’s general development story and are likely to continue to benefit the aged and young alike, there are several overlapping policy areas that may influence the well-being of China’s older population in both the near and long-term. Policy efforts can be targeted to improve the health and quality of life of older people, maximize their independence despite illness, and improve the capacity of families, communities and the broader Chinese society to care for them.
Below, the discussion first reviews a range of policies that are of direct importance for healthy ageing and improving the well-being of older people. First and foremost are policies aimed at influencing behaviors that contribute to the onset of NCDs, in particular, smoking, drinking and unhealthy diet. Second, are policies that further promote useful innovations to the healthcare system, health insurance and the policies which influence health and well-being across the age distribution.
The third direction for policy and regulatory innovation addresses care of the current older adults through potential improvements in LTC and LTCI. Delaying the need for care, the physical well-being and independence of older people may also be supported through approaches as diverse as support for adjustments to housing and attention to the training of older people in the use of technology.
5.2.1. Polices to Reduce the Onset of NCDs
As noted in the Health Behaviors section of the report (Section 3.2), despite declines over the last 40 years, smoking incidence remains quite high, and increases in smoking have been observed among adolescents (those aged 15–24).115 Further, while smoking tends to decrease after age 55, the CHARLS 2020 special survey data suggest that older men with agricultural hukou smoke with much higher incidence (50.4%) than those with non-agricultural hukou (39.0%).
Efforts to reduce smoking to date have included a combination of smoking bans in public settings, education campaigns and efforts to raise the price of cigarettes by raising taxes. Bans alone are not effective without some coordination with educational efforts and increases in the cost of cigarettes. By raising the price of smoking, taxes on cigarettes have been shown to discourage smoking, and especially take up among adolescents.228 Unfortunately, with economic growth and rising purchasing power, the real costs of cigarettes have fallen by more than 50% since 1990, making smoking less costly than in Thailand, Malaysia and Singapore.229 One important approach for the policy will involve measures to raise the cost of smoking.
One of the most important barriers to tobacco control can be attributed to effective lobbying by the tobacco industry, the State Tobacco Monopoly Administration (STMA) and the China National Tobacco Corporation (CNTC), which are giant state-owned enterprises. STMA/CNTC controls the production of tobacco leaf and the manufacture and advertising of cigarettes. With a total profit of 1280 billion yuan in 2020, STMA/CNTC profits are a major economic pillar and an important source of revenue for the central government in China.230
When China joined the WHO’s Framework Convention on Tobacco Control (FCTC) in 2005, it accepted the obligation to raise taxes levied on the retail price to 70% by 2014. As of May 2015, it was 56%.231,232 Interestingly, the STMA enjoys a seat at the tobacco control policy table and sits on the central Government’s WHO FCTC implementation committee. This arrangement represents a serious conflict of interest, which undermines the implementation of the WHO FCTC and weakens efforts to support higher taxes on tobacco.233
Other recommendations from the WHO focus on providing health information on tobacco products and ending advertising of tobacco products. In 2015, China banned tobacco advertising and in 2016 banned the promotion of tobacco products through charitable sponsorships. However, China is yet to place large health warning labels on tobacco packaging.
To prevent the chronic disease burden from rising further with population ageing, tobacco control is crucial, and to be effective control activities must be separated from the tobacco industry. Even after the implementation of non-price tobacco control measures, significantly higher tobacco taxes are an important part of efforts to achieve the Healthy China 2030 target for reduced smoking.234 More practical and effective policies and programs, including health literacy education and targeting the most vulnerable social groups, including adolescents, the illiterate and people with agricultural hukou will be indispensable.
Beyond macro level efforts based on affordability and information in efforts to reduce tobacco consumption and to decrease problem drinking, China may benefit from new approaches exploiting ideas from behavioral science (spanning fields from economics to psychology) to “nudge” individuals toward healthier behaviors., and these may be facilitated in wellness visits with primary care providers
Some approaches to promoting exercise, weight loss or smoking cessation might make use of explicit financial awards or punishments and may be individually oriented or alternatively, exploit peer effects within groups to reinforce individual efforts to quit smoking.235 Financial incentives for behavioral change have produced significant short-term results for weight loss and physical activity.236 After some experimentation in the China context, such approaches may be introduced to supplement use of macro-level policy levers (like taxation) to influence behaviors.
One of the more interesting recent efforts to motivate individuals to change health behaviors exploits the use of mobile health (mHealth) lifestyle interventions, which pairs technology with behavioral science. One well-known implementation uses the Noom smartphone application to provide users with tracking features to log food consumption and exercise, and weight along with access to a virtual one-on-one behavior change coach, support groups, and daily curriculum that includes diet-, exercise-, and psychology-based content. Recent studies have highlighted the clinical utility of the application for sustained weight reduction,237 and even noted that mHealth applications have promoted greater weight loss in middle-aged and older populations.238 In China, approximately one out of three cases of dementia are related to vascular disease (vaD). The report discussed a number of determinants, such as early education, health behaviours (smoking, drinking, exercising), social participation, and living environments that could not only contribute to the healthy ageing process but may also enhance cognitive function. In addition, the prevention potential associated with addressing the modifiable risk factors may be greater in China and other LMICs where NCDs are more prevalent, for example, dementia. The prevention potential associated with addressing the modifiable risk factors may be greater in China and other LMICs where NCDs are more prevalent, for example, dementia.239
Experience with mHealth and other behavioral interventions in HICs suggest that some self-selected participants may be recruited through advertising or forms of direct marketing, but one could imagine that recruiting may be more successful if facilitated through a health care provider (either Tier 1 or Tier 2 aides in the discussion below). Further, success with mHealth will require facilities working with mobile technology, suggesting that efforts to educate older adults in use of mobile phones and applications (as discussed below) may be recommended by their potential use for coaching on health behaviors. In order to best adapt these solutions for China, use of mHealth technologies to promote healthy behaviors should be a priority area for research on NCD prevention in China.
5.2.2. Moving from disease-centred to person-centred care
Disease-centered approaches are appropriate when individuals have a single predominant disease; this disease-centered framework is ill-suited, however, for persons with multiple chronic conditions.240 In order to achieve the goal of person-centered care for older adults, geriatricians are one of the key elements. China has strived to expand the number of geriatric departments and train geriatricians as rapidly as possible. However, training geriatricians takes time. During the transitional period, where medical institutions lack geriatric departments, general hospitals should innovate to provide more convenience for older patients. Specifically, they should work to reduce the number of departments a patient has to visit and offer referral services within the institution.
To address this shortage of physicians with expertise in geriatric medicine, the geriatrics branch of the Chinese Medical Association (CMA) has collaborated with other domestic and foreign institutions, including Johns Hopkins University and the American Geriatrics Society, to provide short-term training courses, aiming to train geriatricians on how to train other physicians. Most program participants were department directors from tertiary hospitals who were expected to transform the geriatrics workforce in their respective regions.196 The government has brought new focus to the training of geriatricians in recent years. For the first time, the National Health Care Commission is incorporating geriatricians in the central training program for health-critical personnel, training more than 3,000 people in the first phase. At the same time, staff who do not specialize in the care of older people need to receive training on health and care issues related to older people, as health care is expected to become increasingly concerned with the care of older individuals in China.
China has a growing need for rehabilitative care; however, rehabilitative care has been underdeveloped for decades. Data show that rehabilitative staff have lower education levels and professional titles. To meet the needs of rehabilitation medicine among older people, the government should develop a rehabilitative professional career track as well as increase the capacity to deliver rehabilitative service.
As for hospice care, the most urgent challenge lies with training hospice care providers and educating the public - not just patients, but also healthcare providers (such as doctors, nurses, social workers, and psychologists) - about palliative care. Those who receive palliative care are likely to live in cities. In terms of public health education, mass media may be most effective, since it reaches people of all socioeconomic levels.
As the focus of medical education and clinical training in China is on disease pathophysiology and treatment, healthcare providers may be unaware of palliative care options. and so introducing palliative care into medical training offers promise Through policy, funding increases and education, China is trying to change this situation and making the medical system more patient-centered, which also offers opportunities to emphasize the importance of palliative care.199
5.2.3. Establishing a National Universal Insurance Plan
China has achieved near-universal health insurance coverage thanks to the offering of insurance to all rural residents and urban people who do not qualify for health insurance under Urban Workers Insurance plans. China’s basic medical insurance programs are highly segmented and still leave plan participants at significant financial risk. At one level, health insurance programs differ by occupation/resident identity. At another, for each type of insurance, pooling occurs within small areas, most commonly at the prefecture-level, and many at the county level.
Segmentation imposes costs for geographic mobility. The Resident Insurance requires local household registration to enroll, but most migrant workers cannot receive local registration status in destination areas due to long-standing anti-migration policies in China. Urban Workers Insurance in destination areas is open for migrants to enroll, but it is much more expensive than Resident Health Insurance. Therefore, most migrant workers still hold Resident Health Insurance purchased at their origin places, which imposes a penalty for non-local medical services and requires upfront payment with additional paperwork for reimbursement.
Recently, the government has recognized the value for older parents of living near adult children and requested relevant agencies to enact policies supporting such living arrangements. Since adult children face high opportunity costs if considering a move back home to care for parents, a more efficient arrangement would facilitate moves by older parents into their children’s homes or communities. From our analysis, the most important item on a list of supportive policies would be removal of penalties for parental migration embedded in health insurance system. Instead of piecemeal reforms that merely patch up the embedded and segmented health insurance system, we propose establishing a unified national insurance system that encompasses all citizens, regardless of occupation, resident status, or place of residence. Such a system will help to eliminate inequalities in health benefits, achieve timely reimbursement without the current cumbersome national settlement system, and remove the power of local governments to impose anti-competition measures.
This is a necessary reform, but local governments’ concerns must be addressed to obtain their cooperation. Poor provinces, which are already burdened with more retirees from the Urban Workers Insurance due to net out-migration of young people, will benefit from the nationalisation in this aspect. However, further outflows of older residents may lead to revenue losses in local public hospitals, requiring more subsidies from the government. On the other hand, richer provinces, who have enjoyed surpluses in the Urban Workers Insurance due to a younger and healthier workforce, stand to lose under a national insurance scheme. However, with more population inflows, they will benefit from more demand for medical services in their hospitals and a lower cost workforce. Therefore, as a companion policy, the central government may adjust fiscal transfers across provinces.
As a prerequisite for the national insurance plan, China needs a centralised information system, which has already been an essential component in the push for a national settlement program for medical expense reimbursement and hampered by complicated local rules and regulations in the past. One benefit of a national insurance system is that it will bypass such complications and set up a new set of rules. A national insurance system should offer choices to allow different levels of protection, but all the rules will be clear. This simplification will facilitate the construction of the national information system.
5.2.4. Deregulate Health Care for Older Patients
As discussed in Section 4.7, despite an urgent need for expanding healthcare to eldercare facilities and those at home, the supply of such services is lacking. One important explanation rest with the combined effects of existing regulations and incentives: existing regulations discourages doctors from performing medical services outside of hospitals, and local governments strive to protect the market power of existing hospitals, and setting low prices further decreases incentives. While patients of all ages are adversely affected by the above issues, older people are the most vulnerable.
We recommend deregulating medical care for older patients. A first priority is amending the Physicians’ Law to allow doctors to visit older patients in their homes. Medical emergency risks at patients’ homes can be mitigated by occupational insurance. Second, clinics in eldercare facilities should be allowed to serve general patients in order for the business to survive. Third, community hospitals should play a larger role in serving older patients and be given financial incentives to do so. Finally, in-home visit fees should increase to reflect time and travel costs for doctors and/or nurses. Recent policy directives call for expanding in-home health services and permitting service providers to charge fees at their cost. Another major policy reform under discussion would transform community health centers into integrated medical and eldercare centers, which makes good sense usually have extra space and insufficient patients. Setting up eldercare beds in these facilities is a win-win solution. Nevertheless, there will still be many older patients living in their own homes. Providing incentives for doctors in community healthcare stations to visit them at home will be essential.
Internet or mHealth has blossomed in China, partly due to the outbreak of Covid-19. Online medical services have a great potential to reach patients in less developed regions and older patients. However, such services are tightly regulated in China, limiting their expansion. For example, medical expenses incurred outside of one’s home area are not reimbursable, and the first visit has to be in a physical hospital. These rules suit situations where a local patient cannot go to the hospital due to quarantine restrictions, or the case of an older patient who needs to refill a prescription but defeats one main purpose of online medical care, which is to provide services to those in distant locations.
There are various reasons why so many regulations exist in the medical sector. One is to protect the monopoly status of local public hospitals. The second is fear of fraudulent charges to the insurance program. The latter concern is reasonable. Most insurance programs are managed locally, many at the city or county level, and local governments often lack manpower or technical expertise to detect fraud. In addition, government-run programs are especially vulnerable to mismanagement. There have been numerous high-profile cases of fraud, many involving local hospitals, even public hospitals and government officials. The process often involves “borrowing” someone’s insurance card, often an older people, sometimes with a bribe, and produce fake treatments or hospitalizations in return for medical reimbursements. A more proactive policy approach is to strengthen the screening for fraud. Moving from local to national management with a uniform information system will allow for more professional management and fraud detection implemented through the IT system will benefit from economies of scale. China is already ahead of many other countries in artificial intelligence and should be able to develop a set of algorithms to detect fraud.
5.2.5. LTCI Should be Independent and Nationally Administered
A review of the implementation and functioning of China’s 15 pilots reveals several problems that must be confronted for successful introduction of LTCI. First, the pilots are funded from the surplus of existing social insurance programs. Most HICs use general taxation or mandatory social insurance to fund LTC and aim to provide universal access to some form of care while protecting older people from major financial risks.241–243 Private insurance and OOP payments play a supplementary role, in the form of co-payments, especially for room and board in institutional settings.244 While China’s pilots have been a useful step forward, there are risks because healthcare expenditures are growing faster than GDP.174 In fact, the insurance pools in many localities are already experiencing a deficit and running down their reserves.245 As the current social health insurance schemes only cover a fraction of costs, OOP medical expenses are significant. Further depleting health insurance funds to support LTCI may make these problems worse.
A second problem evident from the LTCI pilots is that they are all pay-as-you-go schemes. This approach will be difficult to sustain as population ageing progresses. Most beneficiaries of the LTCI pilots are retirees covered under the Urban Workers Insurance, and their number is relatively small because migrant workers have not started to retire through this system. In the future, the number of future beneficiaries relative to payees is likely to be many times larger than the current level. Thus, any successes of current pilot programs can not inform the financial viability of the insurance if it remains as a pay-as-you-go system. LTCI may need to be mandatory to overcome adverse selection and maximize risk pooling. China should also consider introducing an individual saving component to the LTCI financing strategy. The basic idea would be to incentivize saving when young to purchase LTCI as one approach retirement, and this may reduce the need to rely on mandatory LTCI participation.
A third problem arises in that the pilots are all local, and migrants cannot receive benefits, even if they move to another pilot area. The 2020 census of China showed that 8.8% of Chinese live outside one’s province of household registration. If the LTCI stays regionally segmented, members of China’s geographically mobile population may be uninterested in participating in an insurance system. This is a problem faced by health insurance and pensions as well but is less serious in the case of health insurance. For both pensions and LTCI, individuals who do not know where they (or their children) may live in 20 years may be hesitant to participate in the system now.246 Portable LTCI accounts, or savings accounts targeted for future purchase of LTCI, may be more attractive to current working-age adults.
Many local governments offer fiscal subsidies to the eldercare industry aiming to speed up its development. The primary financing mechanism for eldercare facilities is to subsidize construction and operational costs of the provider on a per bed basis. This subsidy method has resulted in a general over-supply of beds in eldercare facilities and a waste of resources. Additionally, most LTC facilities are located in urban areas, but the gap in care needs is more serious in rural areas due to out-migration of the younger generation, enlarging the pre-existing urban-rural inequality in social services. We recommend a fairer subsidy method that gives consumers the power to steer the direction of the industry. Instead of directly subsidizing providers, we recommend issuing vouchers to individuals who have care needs and letting them decide where to use the money. Additionally, people should be allowed to use the voucher anywhere in the country. For example, those in rural areas should be allowed to use their vouchers in cities and towns, or even in the homes of their children. As family-based care has been shown to be less expensive and of better quality than institutional care, this will be Pareto improving for both the society and the family. By letting consumers vote with their feet, this approach has the added advantage of promoting competition in the senior care market, which should improve service quality and lower prices
5.2.6. Improve the Regulatory Framework for Institution-Based Care Delivery
Anecdotal evidence summarised in Chapter 4 of this report suggests that formal, institutional-based care suffers from uneven quality. As consumers of LTC services typically suffer from physical and/or cognitive disabilities, it is difficult for them to change providers when receiving poor services. As private sector provision is viewed as a means of expanding LTC in China, and as the sector has grown rapidly, it will be important for the government to develop an LTC regulatory framework and to strengthen regulatory capacity.
While desirable that regulatory oversight operates as the primary approach to quality assurance for aged care, strict regulations may not be advisable at the early stage in the development of aged care services. In fact, existing regulations about fire safety appear to be overly strict, and anecdotal evidence shows this has caused many, if not most, existing eldercare facilities to fail from registering with the government, which further excludes them from government oversight. We recommend the Chinese government review fire-safety regulations and actively assist or subsidize the existing eldercare facilities to help them meet the standards.
One cost-effective means of reinforcing regulations might be implemented through the government’s procurement of LTC services. Other approaches to improving the quality of LTC service may involve voluntary initiatives through the encouragement of provider and professional associations or the accreditation or quality evaluation by non-governmental rating agencies.219
A voluntary approach requires trust in the provider association or the third-party accreditation process. This trust can only be built over time, but may be facilitated with the development of a standardised information system for the measurement, monitoring and improvement in the quality of care. The information infrastructure will require the periodic collection of high-quality information on LTC providers and service users. Currently, there is little publicly available information about the characteristics of and quality of care provided by senior care service providers to aid quality monitoring or inform consumer choices.213 As in other countries, it would be more feasible to start with collecting such information from institutional care providers and their residents and then to expand the data collection to home and community-based service providers and their customers.
5.2.7. Policies to Support Independence Among Older Adults
Facilitating Financial Security and Social Engagement
Healthy ageing is closely linked to social and economic inequities. Disadvantages in health, education, employment and earnings start early, reinforce each other and accumulate over the life course.2 People born into families in lower SEP are more likely to be in poorer health since early life stages, and those in poorer health often receive less education, earn less and accumulate less wealth. Future policies should adopt a life-course approach to the social determinants and strive to narrow SPS gaps between different groups (e.g., urban/rural) throughout the life-course to ensure financial security at older ages. Such policies include subsidised medical care and education for low-income families and equal treatment for migrants.
Another reform would gradually raise the retirement age of women to equal that of men. Under the Urban Workers Retirement System, blue-collar women retire ten years earlier than men, which causes women to receive substantially lower pensions than men at older ages. While this will reduce inequality in pensions received by men and women, there is still strong resistance to this reform, including from older women. Much of this can be explained by the fact that raising the retirement age conflicts with the dependence on older women for care provision within families. Expanding community-based nurseries (for grandchildren) and care centers (for older parents) may both facilitate raising the retirement age for women.
Support Interventions for Caregivers
In addition to expanding community-based care centers, family members and other informal care providers are important for making sure that older family members can continue to live in their own communities. As noted earlier, care providers themselves are more likely to suffer from depression, social isolation and other health problems as a result of strains associated with their work. To sustain informal caregiving, even in an environment with investments in healthy ageing, appropriate and timely interventions are important to prevent caregivers from suffering negative consequences. Skill building and education, psychosocial support (through the community centers), case management, and leisure and physical fitness programs may all be used to support the needs of informal care providers and to reduce the unmet needs of infirm older people.
Home Environment and Housing Policy
A renewed policy focus on the importance of accessibility to apartments and other buildings will be important for China’s ageing population. Functioning and disability result from an “interaction between the person’s health condition and both personal and environmental factors,” and contextual factors substantially determine whether an impairment is perceived as disabling.247 Accessible dwelling can improve a person’s domain-specific functioning within their home and beyond. Non-accessible home environments expose people with functional impairments to risks of falls and injuries, restricts social participation, negatively affects the quality of life, and increases the burden on caregivers and external social services.
In July of 2020, nine government agencies issued guidance on age-friendly home environments, including installing elevators, installing wheelchair ramps, and making in-house renovations such as non-slip floors, removing thresholds on doors, installing handlebars and modern toilets.402 For older people in poor households, the renovations would be provided for free. However, some renovation projects, especially those that benefit multiple households, have encountered significant difficulties. The nature of the problems reflects a standard public good dilemma: the question of who should pay for the renovation. When village leaders attempt to split the electricity bills from streetlights among households in rural areas, many refused to pay because they seldom live in the village. Indeed, many villages have lost most of their residents due to out-migration, yet most people who stay behind are older residents for whom streetlights are most beneficial. In cities, the contentious negotiations of payment schemes for installing and maintaining elevators have stalled progress. First and second-floor residents see little value of the elevators and a potential loss to their housing value as elevators take up public space. Solving this public-goods issue requires an innovative approach to allocating costs.
Assist Older Adults with the Assistive technology, Internet and Mobile Technologies
Assistive technology (AT) is any service or tool that helps older adults or persons with disabilities perform activities that might otherwise be difficult or impossible. For older adults, such technology may be a walker to improve mobility or an amplification device to make sounds easier to hear. It could also include a magnifying glass for someone who has poor vision or a scooter that makes it possible for someone to travel over distances that are too far to walk. AT allows many people to live independently without long-term nursing or home health care. Considering the low usage of assistive technology (AT) among Chinese older adults, it is encouraging that AT may be able to reduce the dependency rate among them.
In China today, smartphone use has become a prerequisite for daily functioning, but most older people have not adopted them. Supermarkets, even street vendors and taxi drivers, increasingly reject paper money and require electronic payment. During the Covid-19 pandemic and for many months afterwards, one has to scan a QR code to enter a shop, restaurant, post office, any commercial or government building, and when boarding a bus, train or plane, or visiting friends in another community.248 Essentially, those who do not have a smartphone are excluded from society.
The government has installed broadband networks across the country, including many remote rural areas. However, internet use is still low. As revealed by CHARLS, in 2018, 9% of Chinese over 60 use the internet, and almost all use WeChat, a popular platform for communications, information-sharing and payments. Smartphone use is 28% among 50–55, but only 4% for those 70 and older. It is much lower among rural people than their urban counterparts (10% vs. 32%). There is a sharp education gradient in smartphone use: those who can read have an adoption rate of 21%, while those who cannot only have a 1% rate.
The government might enact specific programs that will help disadvantaged older people make use of the internet and mobile technology. Given its importance in daily life, a first priority should be to ensure that every older person has a smartphone. Low-income older people should be given free or subsidised phones. Training in the use of smartphones can also include literacy training sufficient to understand how to use mHealth applications useful for adopting healthy lifestyles and treating NCDs. Financial incentives can be provided to foster learning how to use the devices and relevant health-related applications.
5.3. Plans After This Report
Older people can make important contributions to the family and society. Healthy ageing holds the key - it will not only enable older people to enjoy their later life to the fullest but has the potential to unleash the intellectual and vocational capacities of society as a whole. In China, as the “second baby boomers” are entering retirement age in 2022, it is imperative to take the window of opportunity afforded by the ongoing economic growth to make concerted efforts to achieve the goal of healthy ageing. Individuals must maintain healthy behaviors, families and societies must invest in education and health knowledge, and the government must design a healthcare system that effectively delays the onset of chronic illnesses and controls them afterwards. Recognizing that China’s older population will continue to grow at a rapid pace, families, communities and the government must encourage older people to stay active and prepare well in advance to create an age-friendly environment to maximizes the functional independence of older people and have an eldercare infrastructure ready when care needs arise. It is the intention and ambition of the Lancet and the Commission that this report will serve as a step towards effective and vigorous collective action in order to improve the quality and independence of life for older Chinese and reduce the burden of chronic conditions and age-related diseases.
Key messages.
China has the world’s largest older population. Achieving healthy ageing is necessary for China to reap positive benefits from increased longevity and to reduce potential economic and social burdens that could accompany rapid population ageing.
As NCDs become a greater concern, it is important for policy to promote the adoption of healthy lifestyles and behaviours to improve health status at older ages.
China’s health care delivery system needs to significantly strengthen primary healthcare and move towards integrated delivery to improve access and quality of care for older patients.
China has successfully reduced old-age dependency by pushing for age-friendly communities and home environments. Still, more improvements are necessary to prevent a significant increase in the number of people needing care.
China’s social and demographic changes necessitate finding substitutes to family-based care and helping families take care of their older members. To that end, China needs to train and retain a new cadre of home aid workers, nurses, social workers, and geriatricians.
China’s public health insurance and LTCI should move toward national-level risk pooling to reduce inequality in benefits and facilitate the mobility of older people.
Acknowledgement
We acknowledge the following grants from the National Institute on Ageing. Yaohui Zhao, John Strauss, Huali Wang, Luxia Zhang, John Giles, Haidong Kan, Perry Hu, Xi Chen, Xinxin Chen, Yafeng Wang, Qinqin Meng, Xiaoyan Lei: R01AG037031; James Smith, Yaohui Zhao, Huali Wang: R01AG067625; Yaohui Zhao, John Strauss, John Giles, Xiaoyan Lei, Xinxin Chen: R01AG053228; Xi Chen: R01AG077529. The following grants from the National Natural Science Foundation of China are acknowledged. Yaohui Zhao, Xinxin Chen, Yafeng Wang, Qinqin Meng, Gewei Wang, Jinquan Gong: 72061137005; Xinxin Chen: 71873010; Yao Yao: 81903392; Jin Feng: 71974036; Haidong Kan: 92043301; Xiaoyan Lei: 72061137004; Gewei Wang: 72173008; Yafeng Wang: 71603013; Li Yang: 72174010; Luxia Zhang: 72125009. He Chen was supported by the Fundamental Research Funds for the Central Universities and the Research Funds of Renmin University of China (21XNA004). Huali Wang was supported by the Science and Technology Innovation 2030 - Major Project (2021ZD0201805). John Giles acknowledges the support from the Knowledge for Change Program at the World Bank. Yaohui Zhao also acknowledges the China Medical Board (20-364). These funders supported data collection, analysis, and interpretation. No one is paid to write this article by a pharmaceutical company or other agency. The authors of this report were not precluded from accessing data in the study, and they accept responsibility for submitting it for publication. We thank the National School of Development, Peking University, for arranging and providing meeting spaces and CHARLS staff for logistical support for the commission meetings. We thank the Lancet editors Richard Horton and Helena Wang for their vision in initiating this commission, and they, together with Bill Summerskill, provided directions for this report. We are grateful for Helena Wang, who provided important feedback throughout the process. We also acknowledge the reviewers for their constructive comments regarding our commission report. Finally, we thank the research team members of the working groups who provided assistance with literature searches and synthesis, data extraction, and preparation of figures, namely Ziqi Dong, Yuling Jiang, Lin Kang, Yang Hu, Shaojie Li, Hongmei Li, Xiaolu Nie, Chengxuan Qiu, Longbing Ren, Yan Sun, Huai-Yu Wang, Jingjing Wang, Bojun Wu, Yifei Wu, Anlong Xu, Rui Yang, Hao Zhang, and Qingli Zhang.
abbreviation
- AD
Alzheimer’s Disease
- ADL
Activities of daily living
- AMI
Acute Myocardial Infarction
- ATHLOS
Longitudinal Opportunities and Synergies
- CES-D
Center for Epidemiologic Studies Depression Scale
- CESD-10
Ten-question Version of the Center for Epidemiological Studies Depression
- CFPS
Chinese Family Panel Studies
- CHARLS
China Health and Retirement Longitudinal Study
- CHD
Coronary Heart Disease
- CHNS
China Health and Nutrition Survey
- CI
Confidence Interval
- CKD
Chronic Kidney Disease
- CKB
China Kadoorie Biobank
- CLHLS
Chinese Longitudinal Healthy Longevity Survey
- CMA
Chinese Medical Association
- CMHS
China Mental Health Survey
- CNFS
China National Fracture Study
- CNTC
China National Tobacco Corporation
- COPD
Chronic Obstructive Pulmonary Diseases
- COVID-19
Corona virus disease 2019
- CVD
Cardiovascular Disease
- DALY
Disability-adjusted life year
- EDM
Erectile Dysfunction Medication
- ELA
Early-life adversity
- EQ-5D
EuroQol five dimensions
- FCTC
Framework Convention on Tobacco Control
- GBD
Global Burden of Disease
- GDS
Geriatric Depression Scale
- HAP
Household Air Pollution
- HAM-D
Hamilton Depression Rating Scale
- HIV/AIDS
Human Immunodeficiency Virus / Acquired Immunodeficiency Syndrome
- HICs
High Income Countries
- IADL
Instrumental activities of daily living
- IHME
Institute for Health Metrics and Evaluation
- IGT
Impaired Glucose Tolerance
- LMICs
Low- and middle-income countries
- LTC
Long-Term Care
- LTCI
Long-Term Care Insurance
- MCA
Ministry of Civil Affairs
- MCI
Mild Cognitive Impairment
- mHealth
Mobile Health
- NCDs
Non-Communicable Diseases
- NCMS
New Cooperative Medical Scheme
- NESS-China
National Epidemiological Survey of Stroke in China
- NHC
National Health Commission
- NHSA
National Health Security Administration
- NGO
Non-governmental organizations
- NRCMS
New Rural Cooperative Medical Scheme
- OOP
Out-of-Pocket
- PHQ-9
Patient Health Questionnaire
- PMP
Per Million Population
- PM2.5
Particulate Matter 2.5
- RMB
Ren Min Bi/Chinese Yuan
- SAGE
Global Ageing and Adult Health
- SEP
Socioeconomic Position
- STMA
State Tobacco Monopoly Administration
- SWB
Subjective well-being
- UBMI
Urban Resident Basic Medical Insurance
- US
United States
- VaD
Vascular Dementia
- WHO
World Health Organization
- YLDs
Years Lived with Disability
- YLLs
Years of Life Lost
Footnotes
Search strategy and selection criteria
Data for this review were identified by searches of Google Scholar, PubMed, China National Knowledge Infrastructure (CNKI), and references from relevant articles; numerous articles were identified through searches of the extensive files of the authors. Articles were included in the study if they provide national based data, give deep insight into healthy aging, or have important policy recommendations. All authors independently searched databases using one or more of the following search terms: “healthy aging”, “health status of elderly”, “DALYs”, “chronic disease”, “non-communicable diseases”, “NCDs”, “CVD”, “hypertension”, “diabetes”, “CKD”, “COPD”, “cancer”, “obesity”, “overweight”, “multimorbidity”, “Infectious disease”, “COVID-19”, “HIV”, “AIDS”, “Viral Hepatitis”, “Tuberculosis”, “Syphilis”, “mental health”, “dementia”, “cognitive impairment”, “depression”, “subjective wellbeing”, “life-satisfaction”, “skin conditions”, “Urinary incontinence”, “ sexual activities”, “physical function”, “disability”, “ADL”, “IADL”, “frailty”, “sarcopenia”, “falls”, “fractures”, “self-reported pain”, “sensory function”, “sensory loss”, “sensory impairment”, “impaired eyesight”, “impaired hearing”, “dental health”, “tooth loss”, “oral health”, “in utero health”, “child health”, “the Great Chinese Famine”, “health behaviour”, “healthy lifestyle”, “smoking”, “ tobacco”, “drinking”, “alcohol”, “ physical activities”, “ dietary”, “nutrition”, “nutritional status”, “ undernutrition”, “ social engagement”, “social relationship”, “social network”, “social activity”, “environmental problem”, “environmental health”, “environmental pollution”, “air pollution”, “water pollution”, “soil pollution”, “climate change”, “age-friendly environment”, “aged-care system”, “health insurance”, “public health service”, “health promotion”, “health education”, “health literacy”, “health management”, “healthcare”, “primary healthcare”, “health delivery system”, “elderly care”, “geriatric medicine”, “rehabilitation medicine”, “hospice care”, “palliative care”, “social care”, “long term care”, “care provider”, “healthcare worker”, “institutional care”, “community care”, “medical service”, “health service”, “epidemiology”, “prevalence”, “impact factors”, “China”. All articles were identified without date restriction. Data and reports were also obtained from government and social organization website. English and Chinese language papers and websites were reviewed.
Conflict of interest statement
The authors declared no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kinsella K, He W. An aging world 2008. International population reports. Washington DC: US Government Printing Office, 2009. [Google Scholar]
- 2.United Nations Department of Economic and Social Affairs Population Division. World Population Prospects; 2022.
- 3.Chatterji S, Byles J, Cutler D, Seeman T, Verdes E. Health, functioning, and disability in older adults--present status and future implications. Lancet (London, England) 2015; 385(9967): 563–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. World Health Organization’s (2015) World report on ageing and health World Health Organization. World report on ageing and health, 2015. [Google Scholar]
- 5.Geriatric Medicine Branch of Chinese Medical Association, Editorial Office of Chinese Journal of Geriatrics. Healthy Standard for Chinese Elderly (2013). Chinese Journal of Geriatrics 2013; (8): 801. [Google Scholar]
- 6.Qiao J, Wang Y, Li X, et al. A Lancet Commission on 70 years of women’s reproductive, maternal, newborn, child, and adolescent health in China. Lancet (London, England) 2021; 397(10293): 2497–536. [DOI] [PubMed] [Google Scholar]
- 7.Weatherall D, Greenwood B, Chee HL, Wasi P. Science and Technology for Disease Control: Past, Present, and Future. 2nd ed: World Bank, Washington (DC); 2006. [PubMed] [Google Scholar]
- 8.Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet (London, England) 2016; 387(10015): 251–72. [DOI] [PubMed] [Google Scholar]
- 9.Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet 2019; 394(10204): 1145–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matchar DB, Chei CL, Yin ZX, et al. Vitamin D Levels and the Risk of Cognitive Decline in Chinese Elderly People: the Chinese Longitudinal Healthy Longevity Survey. J Gerontol A Biol Sci Med Sci 2016; 71(10): 1363–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Center for Cardiovascular Diseases. National Report on Cardiovascular health and diseases in China 2019: Beijing Science Pulishing; Sep, 2020. [In Chinese]. [Google Scholar]
- 12.Wang W, Jiang B, Sun H, et al. Prevalence, Incidence, and Mortality of Stroke in China: Results from a Nationwide Population-Based Survey of 480 687 Adults. Circulation 2017; 135(8): 759–71. [DOI] [PubMed] [Google Scholar]
- 13.Guan T, Ma J, Li M, et al. Rapid transitions in the epidemiology of stroke and its risk factors in China from 2002 to 2013. Neurology 2017; 89(1): 53–61. [DOI] [PubMed] [Google Scholar]
- 14.Wang Z, Chen Z, Zhang L, et al. Status of Hypertension in China: Results From the China Hypertension Survey, 2012–2015. Circulation 2018; 137(22): 2344–56. [DOI] [PubMed] [Google Scholar]
- 15.Lv Y-B, Gao X, Yin Z-X, et al. Revisiting the association of blood pressure with mortality in oldest old people in China: community based, longitudinal prospective study. Bmj 2018; 361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao Y, Crimmins EM, Hu P, et al. Prevalence, diagnosis, and management of diabetes mellitus among older Chinese: results from the China Health and Retirement Longitudinal Study. International Journal of Public Health 2016; 61(3): 347–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang L, Peng W, Zhao Z, et al. Prevalence and Treatment of Diabetes in China, 2013–2018. JAMA 2021; 326(24): 2498–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Y, Teng D, Shi X, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ 2020; 369: m997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang K, Li T, Xiang H. Study on the Epidemiological Characteristics of Diabetes Mellitus and IGT in China Zhonghua Liu Xing Bing Xue Za Zhi 1998. [In Chinese]; 19(5): 282–5. [PubMed] [Google Scholar]
- 20.Wang L, Gao P, Zhang M, et al. Prevalence and Ethnic Pattern of Diabetes and Prediabetes in China in 2013. JAMA 2017; 317(24): 2515–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Asia Pacific Cohort Studies Collaboration. The burden of overweight and obesity in the Asia-Pacific region. Obesity reviews : an official journal of the International Association for the Study of Obesity 2007; 8(3): 191–6. [DOI] [PubMed] [Google Scholar]
- 22.Wang L, Zhou B, Zhao Z, et al. Body-mass index and obesity in urban and rural China: findings from consecutive nationally representative surveys during 2004–18. Lancet (London, England) 2021; 398(10294): 53–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Foreman K, Marquez N, Dolgert A, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016–40 for 195 countries and territories. Lancet (London, England) 2018; 392(10159): 2052–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang L, Wang F, Wang L, et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet (London, England) 2012; 379(9818): 815–22. [DOI] [PubMed] [Google Scholar]
- 25.Huang YM, Xu D, Long J, et al. Spectrum of chronic kidney disease in China: A national study based on hospitalized patients from 2010 to 2015. Nephrology (Carlton) 2019; 24(7): 725–36. [DOI] [PubMed] [Google Scholar]
- 26.Wang H, Yang L, Wang F, Zhang L. Strategies and cost-effectiveness evaluation of persistent albuminuria screening among high-risk population of chronic kidney disease. BMC nephrology 2017; 18(1): 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fang L, Gao P, Bao H, et al. Chronic obstructive pulmonary disease in China: a nationwide prevalence study. The Lancet Respiratory medicine 2018; 6(6): 421–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhong N, Wang C, Yao W, et al. Prevalence of chronic obstructive pulmonary disease in China: a large, population-based survey. American journal of respiratory and critical care medicine 2007; 176(8): 753–60. [DOI] [PubMed] [Google Scholar]
- 29.Wei W, Zeng H, Zheng R, et al. Cancer registration in China and its role in cancer prevention and control. The Lancet Oncology 2020; 21(7): e342–e9. [DOI] [PubMed] [Google Scholar]
- 30.Cao F, Wang Y-B, Xue W-G, et al. Clinical multi-centers report of chronic diseases among elderly inpatients in China. Chinese Journal of Multiple Organ Diseases in the Elderly 2018; 17(11): 801–8. [Google Scholar]
- 31.Cao W, Chen HD, Yu YW, Li N, Chen WQ. Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020. Chin Med J (Engl) 2021; 134(7): 783–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen W, Zheng R, Zhang S, et al. Cancer incidence and mortality in China, 2013. Cancer letters 2017; 401: 63–71. [DOI] [PubMed] [Google Scholar]
- 33.Zeng H, Chen W, Zheng R, et al. Changing cancer survival in China during 2003–15: a pooled analysis of 17 population-based cancer registries. The Lancet Global health 2018; 6(5): e555–e67. [DOI] [PubMed] [Google Scholar]
- 34.The Academy of Medical Sciences (UK). Multimorbidity: a priority for global health research, 2018.
- 35.Lancet The. Making more of multimorbidity: an emerging priority. Lancet (London, England) 2018; 391(10131): 1637. [DOI] [PubMed] [Google Scholar]
- 36.Garin N, Koyanagi A, Chatterji S, et al. Global Multimorbidity Patterns: A Cross-Sectional, Population-Based, Multi-Country Study. J Gerontol A Biol Sci Med Sci 2016; 71(2): 205–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yao SS, Cao GY, Han L, et al. Prevalence and patterns of multimorbidity in a nationally representative sample of older Chinese: results from CHARLS. J Gerontol A Biol Sci Med Sci 2019. [DOI] [PubMed] [Google Scholar]
- 38.Wang X, Wang Y, Zhang Q, Zhao Y. Multimorbidity among Middle-aged and Older Chinese Population: Prevalence, Clustering Patterns, Risk Factors, and Consequences. In: National School of Development, editor. Peking University, China; 2020. [Google Scholar]
- 39.Bureau of Disease Control, National of Health Commission of the People’s Republic of China. 2019 summary report of the national notifiable diseases in China. Apr 20, 2020. [In Chinese]. http://www.nhc.gov.cn/jkj/s3578/202004/b1519e1bc1a944fc8ec176db600f68d1.shtml (accessed Jan 23, 2022.
- 40.Wang L, Wang Y, Jin S, et al. Emergence and control of infectious diseases in China. Lancet (London, England) 2008; 372(9649): 1598–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wu Z, McGoogan JM, Detels R. The enigma of the HIV epidemic in China. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.National Center for AIDS/STD Control and Prevention. 2018 China national HIV/STD/HCV program implementation report. 2019. http://weekly.chinacdc.cn/en/article/doi/10.46234/ccdcw2020.004 (accessed Jan 23, 2022.
- 43.Li AH, Wu ZY, Jiang Z, Mcgoogan JM, Zhao Y, Duan S. Duration of Human Immunodeficiency Virus Infection at Diagnosis among New Human Immunodeficiency Virus Cases in Dehong, Yunnan, China, 2008–2015. Chinese Medical Journal 2018; 131(16): 1936–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tang Z, Wu X, Li G, et al. Aphrodisiac use associated with HIV infection in elderly male clients of low-cost commercial sex venues in Guangxi, China: a matched case-control study. PLoS One 2014; 9(10): e109452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chinese Center for Disease Control and Prevention. 2019 China’s Notifiable Disease Report. 2019. https://www.chinacdc.cn/gsywlswxx_9503/jscbs_1/201811/t20181119_197386.html (accessed Jan 23, 2022.
- 46.Lu Q-B, Jiang W-L, Zhang X, et al. Comorbidities for fatal outcome among the COVID-19 patients: A hospital-based case-control study. Journal of Infection 2021; 82(1): 159–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang Y, Luo W, Li Q, et al. Risk Factors for Death Among the First 80 543 COVID-19 Cases in China: A Closer Look at Age, Underlying Disease, Case Severity, and Region. Manuscript submitted. [DOI] [PMC free article] [PubMed]
- 48.Wang C, Han B, Zhao T, et al. Vaccination willingness, vaccine hesitancy, and estimated coverage at the first round of COVID-19 vaccination in China: A national cross-sectional study. Vaccine 2021; 39(21): 2833–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2017 (GBD 2017) Results. In: Institute for Health Metrics and Evaluation (IHME), editor. Seattle, United States; 2017. [Google Scholar]
- 50.Lu J, Xu X, Huang Y, et al. Prevalence of depressive disorders and treatment in China: a cross-sectional epidemiological study. Lancet Psychiatry 2021; 8(11): 981–90. [DOI] [PubMed] [Google Scholar]
- 51.Huang Y, Wang Y, Wang H, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry 2019; 6(3): 211–24. [DOI] [PubMed] [Google Scholar]
- 52.Zhang L, Xu Y, Nie H, Zhang Y, Wu Y. The prevalence of depressive symptoms among the older in China: a meta-analysis. Int J Geriatr Psychiatry 2012; 27(9): 900–6. [DOI] [PubMed] [Google Scholar]
- 53.Nie X, Wang H, Sun F, Yang Z, Tang S, Tao Q. Detection rate of depression among community-dwelling older adults in China: A systematic review and updated meta-analysis of studies in 2000–2012. J Chin Ment Health J 2013; 11: 805–14. [Google Scholar]
- 54.Lei X, Sun X, Strauss J, Zhang P, Zhao Y. Depressive symptoms and SES among the mid-aged and elderly in China: Evidence from the China Health and Retirement Longitudinal Study national baseline. Social Science & Medicine 2014; 120: 224–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ma Y, Xiang Q, Yan C, Liao H, Wang J. Relationship between chronic diseases and depression: the mediating effect of pain. BMC psychiatry 2021; 21(1): 436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wolitzky-Taylor KB, Castriotta N, Lenze EJ, Stanley MA, Craske MG. Anxiety disorders in older adults: a comprehensive review. Depression and anxiety 2010; 27(2): 190–211. [DOI] [PubMed] [Google Scholar]
- 57.Yan Y, Du X, Lai L, Ren Z, Li H. Prevalence of depressive and anxiety symptoms among Chinese older adults during the COVID-19 pandemic: A systematic review and meta-analysis. Journal of geriatric psychiatry and neurology 2022; 35(2): 182–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li X, Xiao Z, Xiao S. Suicide among the elderly in mainland China. Psychogeriatrics 2009; 9(2): 62–6. [DOI] [PubMed] [Google Scholar]
- 59.Zhong BL, Chiu HF, Conwell Y. Elderly suicide trends in the context of transforming China, 1987–2014. Scientific reports 2016; 6: 37724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Harada CN, Natelson Love MC, Triebel KL. Normal cognitive aging. Clinics in geriatric medicine 2013; 29(4): 737–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jia J, Wang F, Wei C, et al. The prevalence of dementia in urban and rural areas of China. J Alzheimer’s Dementia 2014; 10(1): 1–9. [DOI] [PubMed] [Google Scholar]
- 62.Jia J, Zhou A, Wei C, et al. The prevalence of mild cognitive impairment and its etiological subtypes in elderly Chinese. J Alzheimer’s Dementia 2014; 10(4): 439–47. [DOI] [PubMed] [Google Scholar]
- 63.Jia L, Du Y, Chu L, et al. Prevalence, risk factors, and management of dementia and mild cognitive impairment in adults aged 60 years or older in China: a cross-sectional study. The Lancet Public health 2020; 5(12): e661–e71. [DOI] [PubMed] [Google Scholar]
- 64.Nie H, Xu Y, Liu B, et al. The prevalence of mild cognitive impairment about elderly population in China: a meta - analysis. International journal of geriatric psychiatry 2011; 26(6): 558–63. [DOI] [PubMed] [Google Scholar]
- 65.Nie X, Lyu X, Zhuo L, Chen Y, Wang H, S Z. Prevalence of mild cognitive impairment in China: a meta-analysis of studies in 2001–2015. Chinese Journal of Psychiatry 2016; 49(5): 298–306. [Google Scholar]
- 66.Liang Y, Song A, Du S, Guralnik JM, Qiu C. Trends in disability in activities of daily living among Chinese older adults, 1997–2006: the China Health and Nutrition Survey. J Gerontol A Biol Sci Med Sci 2015; 70(6): 739–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Liang Y, Welmer AK, Moller J, Qiu C. Trends in disability of instrumental activities of daily living among older Chinese adults, 1997–2006: population based study. BMJ open 2017; 7(8): e016996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gong J, Wang G, Wang Y, et al. Nowcasting and forecasting the care needs of the older adults in China: estimates from the China Health and Retirement Longitudinal Study (CHARLS). The Lancet Public health; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2001; 56(3): M146–M57. [DOI] [PubMed] [Google Scholar]
- 70.Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2007; 62(7): 722–7. [DOI] [PubMed] [Google Scholar]
- 71.Fan J, Yu C, Guo Y, et al. Frailty index and all-cause and cause-specific mortality in Chinese adults: a prospective cohort study. The Lancet Public health 2020; 5(12): e650–e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yang F, Gu D. Predictability of frailty index and its components on mortality in older adults in China. BMC Geriatrics 2016; 16(1): 145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.He B, Ma Y, Wang C, et al. Prevalence and risk factors for frailty among community-dwelling older people in China: a systematic review and meta-analysis. The journal of nutrition, health & aging 2019; 23(5): 442–50. [DOI] [PubMed] [Google Scholar]
- 74.Lu Z, Er Y, Zhan Y, et al. Association of frailty status with risk of fall among middle-aged and older adults in China: a nationally representative cohort study. The journal of nutrition, health & aging 2021; 25(8): 985–92. [DOI] [PubMed] [Google Scholar]
- 75.Xu W, Li Y-X, Wu C. Incidence of frailty among community-dwelling older adults: a nationally representative profile in China. BMC geriatrics 2019; 19(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chen LK, Liu LK, Woo J, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. Journal of the American Medical Directors Association 2014; 15(2): 95–101. [DOI] [PubMed] [Google Scholar]
- 77.Chen LK, Woo J, Assantachai P, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. Journal of the American Medical Directors Association 2020; 21(3): 300–7.e2. [DOI] [PubMed] [Google Scholar]
- 78.Chen Z, Li W-Y, Ho M, Chau P-H. The Prevalence of Sarcopenia in Chinese Older Adults: Meta-Analysis and Meta-Regression. Nutrients 2021; 13(5): 1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wu X, Li X, Xu M, Zhang Z, He L, Li Y. Sarcopenia prevalence and associated factors among older Chinese population: Findings from the China Health and Retirement Longitudinal Study. PLoS One 2021; 16(3): e0247617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ye P, Er Y, Wang H, et al. Burden of falls among people aged 60 years and older in mainland China, 1990–2019: findings from the Global Burden of Disease Study 2019. The Lancet Public health 2021; 6(12): e907–e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Guo YF, Ma WJ, Zhang QJ, et al. Incidence of fall related injury in people aged 50 and above and risk factors in 8 provinces in China: a cross-sectional study. Zhonghua Liu Xing Bing Xue Za Zhi 2018; 39(3): 258–63. [DOI] [PubMed] [Google Scholar]
- 82.Yao Y, Yin P, Liu X. Falls prevention in China: time for action. The Lancet Public health 2021; 6(12): e875–e6. [DOI] [PubMed] [Google Scholar]
- 83.Zhang C, Feng J, Wang S, et al. Incidence of and trends in hip fracture among adults in urban China: A nationwide retrospective cohort study. PLoS Med 2020; 17(8): e1003180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wang L, Yu W, Yin X, et al. Prevalence of Osteoporosis and Fracture in China: The China Osteoporosis Prevalence Study. JAMA Netw Open 2021; 4(8): e2121106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chen W, Lv H, Liu S, et al. National incidence of traumatic fractures in China: a retrospective survey of 512 187 individuals. The Lancet Global health 2017; 5(8): e807–e17. [DOI] [PubMed] [Google Scholar]
- 86.Sherrington C, Michaleff ZA, Fairhall N, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med 2017; 51(24): 1750–8. [DOI] [PubMed] [Google Scholar]
- 87.Burke NN, Finn DP, McGuire BE, Roche M. Psychological stress in early life as a predisposing factor for the development of chronic pain: Clinical and preclinical evidence and neurobiological mechanisms. Journal of neuroscience research 2017; 95(6): 1257–70. [DOI] [PubMed] [Google Scholar]
- 88.Lei P, Xu L, Nwaru BI, Long Q, Wu Z. Social networks and health-related quality of life among Chinese old adults in urban areas: results from 4th National Household Health Survey. Public health 2016; 131: 27–39. [DOI] [PubMed] [Google Scholar]
- 89.Zhu L, Petersen PE, Wang HY, Bian JY, Zhang BX. Oral health knowledge, attitudes and behaviour of adults in China. International dental journal 2005; 55(4): 231–41. [DOI] [PubMed] [Google Scholar]
- 90.Veenhoven R Healthy happiness: effects of happiness on physical health and the consequences for preventive health care. Journal of Happiness Studies 2008; 9(3): 449–69. [Google Scholar]
- 91.Blanchflower DG. Is happiness U-shaped everywhere? Age and subjective well-being in 145 countries. Journal of Population Economics 2021; 34(2): 575–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lei X, Shen Y, Smith JP, Zhou G. Do social networks improve chinese adults’ subjective well-being? J Econ Aging 2015; 6: 57–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Easterlin RA, Morgan R, Switek M, Wang F. China’s life satisfaction, 1990–2010. Proceedings of the National Academy of Sciences of the United States of America 2012; 109(25): 9775–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zhang W, Liu G. Childness, psychological well-being, and life satisfaction amomg the elderly in China. Journal of Cross-Cultural Gerontology 2007; 2007(22): 185–203. [DOI] [PubMed] [Google Scholar]
- 95.Hahnel E, Lichterfeld A, Blume-Peytavi U, Kottner J. The epidemiology of skin conditions in the aged: a systematic review. Journal of tissue viability 2017; 26(1): 20–8. [DOI] [PubMed] [Google Scholar]
- 96.Sinikumpu SP, Jokelainen J, Haarala AK, Keränen MH, Keinänen - Kiukaanniemi S, Huilaja L. The high prevalence of skin diseases in adults aged 70 and older. Journal of the American Geriatrics Society 2020; 68(11): 2565–71. [DOI] [PubMed] [Google Scholar]
- 97.Dong W, An J, Geng P, et al. Years lost due to disability from skin diseases in China 1990–2017: findings from the Global Burden of Disease Study 2017. The British Journal of Dermatology 2020; 182(1): 248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kim EK, Kim HO, Park YM, Park CJ, Yu DS, Lee JY. Prevalence and risk factors of depression in geriatric patients with dermatological diseases. Annals of dermatology 2013; 25(3): 278–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Xue K, Palmer MH, Zhou F. Prevalence and associated factors of urinary incontinence in women living in China: a literature review. BMC urology 2020; 20(1): 1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Luo Y, Zou P, Wang K, Li X, Wang J. Prevalence and Risk Factors of Urinary Incontinence Among Elderly Adults in Rural China: A Cross-Sectional Survey. Journal of Wound Ostomy & Continence Nursing 2022; 49(1). [DOI] [PubMed] [Google Scholar]
- 101.Yuan H, Williams BA. Knowledge of urinary incontinence among Chinese community nurses and community-dwelling older people. Health & social care in the community 2010; 18(1): 82–90. [DOI] [PubMed] [Google Scholar]
- 102.Yang S, Yan E, Bai X. An integrated model to understand sexuality in older adults in urban China: The mediating role of sexual interest. Archives of gerontology and geriatrics 2018; 78: 51–7. [DOI] [PubMed] [Google Scholar]
- 103.Sathyanarayana Rao TS, Ismail S, Darshan MS, Tandon A. Sexual disorders among elderly: An epidemiological study in south Indian rural population. Indian journal of psychiatry 2015; 57(3): 236–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zhou Y, Li C, Jin F, Shao H, Teng Y, Tao M. Prevalence and predictors of sexual function in midlife partnered Chinese women assessed by two simple indicators: Sexual frequency and sexual desire. J Obstet Gynaecol Res 2019; 45(1): 210–6. [DOI] [PubMed] [Google Scholar]
- 105.Shea JL. Older women, marital relationships, and sexuality in China. Ageing International 2011; 36(3): 361–77. [Google Scholar]
- 106.So HW, Cheung FM. Review of Chinese sex attitudes and applicability of sex therapy for chinese couples with sexual dysfunction. J Sex Res 2005; 42(2): 93–101. [DOI] [PubMed] [Google Scholar]
- 107.Guan J Correlates of spouse relationship with sexual attitude, interest, and activity among Chinese elderly. Sexuality and Culture 2004; 8(1): 104–31. [Google Scholar]
- 108.Li C, Miles T, Shen L, et al. Early-life exposure to severe famine and subsequent risk of depressive symptoms in late adulthood: the China Health and Retirement Longitudinal Study. Br J Psychiatry 2018; 213(4): 579–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wang N, Chen Y, Ning Z, et al. Exposure to Famine in Early Life and Nonalcoholic Fatty Liver Disease in Adulthood. J Clin Endocrinol Metab 2016; 101(5): 2218–25. [DOI] [PubMed] [Google Scholar]
- 110.Neel JV. The “thrifty genotype” in 1998. J Nutrition Reviews 1999; 57(5 Pt 2): S2–9. [DOI] [PubMed] [Google Scholar]
- 111.Li Y, Xue QL, Odden MC, Chen X, Wu C. Linking early life risk factors to frailty in old age: evidence from the China Health and Retirement Longitudinal Study. Age and ageing 2020; 49(2): 208–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chen Z, Peto R, Zhou M, et al. Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet (London, England) 2015; 386(10002): 1447–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet (London, England) 2021; 397(10292): 2337–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ng M, Freeman MK, Fleming TD, et al. Smoking Prevalence and Cigarette Consumption in 187 Countries, 1980–2012. JAMA 2014; 311(2): 183–92. [DOI] [PubMed] [Google Scholar]
- 115.Wang M, Luo X, Xu S, et al. Trends in smoking prevalence and implication for chronic diseases in China: serial national cross-sectional surveys from 2003 to 2013. The Lancet Respiratory medicine 2019; 7(1): 35–45. [DOI] [PubMed] [Google Scholar]
- 116.Degenhardt L, Charlson F, Ferrari A, et al. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet Psychiatry 2018; 5(12): 987–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet (London, England) 2018; 392(10152): 1015–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Im PK, Millwood IY, Guo Y, et al. Patterns and trends of alcohol consumption in rural and urban areas of China: findings from the China Kadoorie Biobank. BMC public health 2019; 19(1): 217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Cheng HG, Deng F, Xiong W, Phillips MR. Prevalence of alcohol use disorders in mainland China: a systematic review. Addiction (Abingdon, England) 2015; 110(5): 761–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Liang H, Wang J, Xiao H, et al. Estimation of cancer incidence and mortality attributable to alcohol drinking in China. BMC public health 2010; 10: 730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Li Y, Jiang Y, Zhang M, Yin P, Wu F, Zhao W. Drinking behaviour among men and women in China: the 2007 China Chronic Disease and Risk Factor Surveillance. Addiction (Abingdon, England) 2011; 106(11): 1946–56. [DOI] [PubMed] [Google Scholar]
- 122.Ng SW, Norton EC, Popkin BM. Why have physical activity levels declined among Chinese adults? Findings from the 1991–2006 China Health and Nutrition Surveys. Soc Sci Med 2009; 68(7): 1305–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Feng Q, Fong JH, Zhang W, Liu C, Chen H. Leisure Activity Engagement Among the Oldest Old in China, 1998–2018. Am J Public Health 2020; 110(10): 1535–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Giles J, Lei X, Wang Y, Zhao Y. One country, two systems: Evidence on retirement patterns in china. Journal of Pension Economics & Finance 2021: 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Yin P, Zhang M, Li YC, et al. Survey of dietary intake of Chinese adults in 2010. Zhonghua yu fang yi xue za zhi [Chinese journal of preventive medicine] 2012; 46(8): 692–6. [PubMed] [Google Scholar]
- 126.Qin C, Yu C, Du H, et al. Differences in diet intake frequency of adults: findings from half a million people in 10 areas in China. Zhonghua Liu Xing Bing Xue Za Zhi 2015; 36(9): 911–6. [PubMed] [Google Scholar]
- 127.Zhao Z, Li M, Li C, et al. Dietary preferences and diabetic risk in China: A large - scale nationwide Internet data - based study. Wiley Online Library; 2020. p. 270–8. [DOI] [PubMed] [Google Scholar]
- 128.Xu X, Hall J, Byles J, Shi Z. Assessing dietary quality of older Chinese people using the Chinese Diet Balance Index (DBI). PLoS One 2015; 10(3): e0121618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.National Health and Family Planning Commission. Report on Nutrition and Chronic Diseases of Chinese Residents (2015). Beijing, 2016. [Google Scholar]
- 130.Zhao F, Fang H, Zhao Liyun, et al. Intakes of dietary energy and macronutrients among the elderly aged 65 and above in China in 2015. Journal of Hygiene Research 2021; 50(01): 37–45. [DOI] [PubMed] [Google Scholar]
- 131.Lu Y, Niti M, Yap KB, et al. Assessment of Sarcopenia Among Community-Dwelling At-Risk Frail Adults Aged 65 Years and Older Who Received Multidomain Lifestyle Interventions: A Secondary Analysis of a Randomized Clinical Trial. JAMA Netw Open 2019; 2(10): e1913346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Lv Y, Mao C, Gao X, et al. The obesity paradox is mostly driven by decreased noncardiovascular disease mortality in the oldest old in China: a 20-year prospective cohort study. Nature Aging 2022; 2(5): 389–96. [DOI] [PubMed] [Google Scholar]
- 133.Neal B, Wu Y, Feng X, et al. Effect of salt substitution on cardiovascular events and death. New England Journal of Medicine 2021; 385(12): 1067–77. [DOI] [PubMed] [Google Scholar]
- 134.Berkman LF, Krishna A. Social Network Epidemiology. Social Epidemiology. New York: Oxford University; 2014: 234–89. [Google Scholar]
- 135.Antonucci TC, Akiyama H. Social networks in adult life and a preliminary examination of the convoy model. Journal of gerontology 1987; 42(5): 519–27. [DOI] [PubMed] [Google Scholar]
- 136.Birditt KS, Antonucci TC, Tighe L. Enacted support during stressful life events in middle and older adulthood: An examination of the interpersonal context. Psychology and aging 2012; 27(3): 728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Tough H, Siegrist J, Fekete C. Social relationships, mental health and wellbeing in physical disability: a systematic review. BMC public health 2017; 17(1): 414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Tang D, Xie L. Whose migration matters? The role of migration in social networks and mental health among rural older adults in China. Ageing & Society 2021: 1–20. [Google Scholar]
- 139.Kesavayuth D, Liang Y, Zikos V. An active lifestyle and cognitive function: Evidence from China. The Journal of the Economics of Ageing 2018; (12): 183–91. [Google Scholar]
- 140.Lei X, Strauss J, Tian M, Zhao Y. Living arrangements of the elderly in China: evidence from the CHARLS national baseline. China Economic Journal 2015; 8(3): 191–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Xiao J, Hilton A. An Investigation of Soundscape Factors Influencing Perceptions of Square Dancing in Urban Streets: A Case Study in a County Level City in China. 2019; 16(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Qin J, Rong X, Zhu G, Jiang Y. The effects of square dancing on bone mineral density and bone turnover markers in patients with postmenopausal osteoporosis. Journal of Mechanics in Medicine and Biology 2018; 18(8). [Google Scholar]
- 143.WHO. Global report on ageism. Geneva, Switzerland: World Health Organization, 2021. [Google Scholar]
- 144.Council NR. Elder mistreatment: Abuse, neglect, and exploitation in an aging America. 2003. [PubMed]
- 145.WHO. Abuse of older people. 2022. https://www.who.int/news-room/fact-sheets/detail/abuse-of-older-people (accessed June 23, 2022.
- 146.Hongxia T, jing J, Haihui R, et al. The prevalence of elder abuse in China: a systematic review. Chinese Journal of Evidence-Based Medicine 2020; 20(8): 938–44. [Google Scholar]
- 147.Yun J, Jinwei L, Zhixia W, Zhidi L. Status and countermeasures of elder abuse in China. Chinese Journal of Gerontology 2018; 38(17): 4284–7. [Google Scholar]
- 148.Du P, Chen Y. Prevalence of elder abuse and victim-related risk factors during the COVID-19 pandemic in China. BMC public health 2021; 21(1): 1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (London, England) 2020; 396(10258): 1223–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Guo Y, Lin H, Shi Y, et al. Long-term exposure to ambient PM2.5 associated with fall-related injury in six low- and middle-income countries. Environ Pollut 2018; 237: 961–7. [DOI] [PubMed] [Google Scholar]
- 151.Liang F, Liu F, Huang K, et al. Long-Term Exposure to Fine Particulate Matter and Cardiovascular Disease in China. J Am Coll Cardiol 2020; 75(7): 707–17. [DOI] [PubMed] [Google Scholar]
- 152.Guo C, Zeng Y, Chang LY, et al. Independent and Opposing Associations of Habitual Exercise and Chronic PM(2.5) Exposures on Hypertension Incidence. Circulation 2020; 142(7): 645–56. [DOI] [PubMed] [Google Scholar]
- 153.Ma Q, Li R, Wang L, et al. Temporal trend and attributable risk factors of stroke burden in China, 1990–2019: an analysis for the Global Burden of Disease Study 2019. The Lancet Public health 2021; 6(12): e897–e906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Lin H, Guo Y, Zheng Y, et al. Exposure to ambient PM2.5 associated with overall and domain-specific disability among adults in six low- and middle-income countries. Environ Int 2017; 104: 69–75. [DOI] [PubMed] [Google Scholar]
- 155.Sun R, Gu D. Air pollution, economic development of communities, and health status among the elderly in urban China. Am J Epidemiol 2008; 168(11): 1311–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Xue T, Guan T, Zheng Y, et al. Long-term PM2.5 exposure and depressive symptoms in China: A quasi-experimental study. Lancet Reg Health West Pac 2021; 6: 100079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Qi J, Ruan Z, Qian ZM, et al. Potential gains in life expectancy by attaining daily ambient fine particulate matter pollution standards in mainland China: A modeling study based on nationwide data. PLoS Med 2020; 17(1): e1003027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Yao Y, Lv X, Qiu C, et al. The effect of China’s Clean Air Act on cognitive function in older adults: a population-based, quasi-experimental study. Lancet Healthy Longev 2022; 3(2): e98–e108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Li J, Yao Y, Xie W, et al. Association of long-term exposure to PM2.5 with blood lipids in the Chinese population: Findings from a longitudinal quasi-experiment. Environ Int 2021; 151: 106454. [DOI] [PubMed] [Google Scholar]
- 160.Chen R, Kan H. Preventing cognitive impairment by reducing air pollution. The Lancet Healthy Longevity 2022; 3(2): e81–e2. [DOI] [PubMed] [Google Scholar]
- 161.Zhang J, Smith KR. Household air pollution from coal and biomass fuels in China: measurements, health impacts, and interventions. Environmental health perspectives 2007; 115(6): 848–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Chen C, Liu GG, Sun Y, et al. Association between household fuel use and sleep quality in the oldest-old: Evidence from a propensity-score matched case-control study in Hainan, China. Environmental research 2020; 191: 110229. [DOI] [PubMed] [Google Scholar]
- 163.Liu Y, Chen X, Yan Z. Depression in the house: The effects of household air pollution from solid fuel use among the middle-aged and older population in China. Sci Total Environ 2020; 703: 134706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Etzel RA, Balk SJ. Pediatric Environmental Health. 3rd ed: American Academy of Pediatrics; 2011. [Google Scholar]
- 165.Zhang QL, Zhao Q. Study on the Model of Home-based Community Caring for the Elderly. Journal of Northeastern University 2011. [In Chinese]. [Google Scholar]
- 166.Chen R, Yin P, Wang L, et al. Association between ambient temperature and mortality risk and burden: time series study in 272 main Chinese cities. BMJ 2018; 363: k4306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Qian Z, He Q, Lin H-M, et al. High temperatures enhanced acute mortality effects of ambient particle pollution in the “oven” city of Wuhan, China. Environmental health perspectives 2008; 116(9): 1172–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Xiang L, Shen GQ, Li D, Tan Y, Jin X. A Multi-Agent Platform to Explore Strategies for Age-Friendly Community Projects in Urban China. The Gerontologist 2022; 62(4): 530–42. [DOI] [PubMed] [Google Scholar]
- 169.Implementing age-friendly retrofitting projects for Chinese older residents. In: Ministry of Civil Affairs NDaRC, Ministry of Finance, Ministry of Housing and Urban-Rural Development, National Health Insurance Commission, State Council Poverty Alleviation Office, China Disabled Persons’ Federation, National Office for the Aging, editor.; 2020. [Google Scholar]
- 170.Oaks M The Importance of Home Modification for Occupational Participation and Safety for Low-income Older Adult Homeowners 2017. https://sophia.stkate.edu/ma_osot/9/ (accessed Jan 23, 2022).
- 171.Mitoku K, Shimanouchi S. Home modification and prevention of frailty progression in older adults: a Japanese prospective cohort study. J Gerontol Nurs 2014; 40(8): 40–7. [DOI] [PubMed] [Google Scholar]
- 172.Szanton SL, Thorpe RJ, Boyd C, et al. Community aging in place, advancing better living for elders: a bio-behavioral-environmental intervention to improve function and health-related quality of life in disabled older adults. J Am Geriatr Soc 2011; 59(12): 2314–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.National Office for the Aging. Report of the Fourth Sample Survey on the Living Conditions of the Elderly in Urban and Rural China; 2015.
- 174.Yip W, Fu H, Chen AT, et al. 10 years of health-care reform in China: progress and gaps in Universal Health Coverage. Lancet (London, England) 2019; 394(10204): 1192–204. [DOI] [PubMed] [Google Scholar]
- 175.Feng Z, Liu C, Guan X, Mor V. China’s rapidly aging population creates policy challenges in shaping a viable long-term care system. Health affairs (Project Hope) 2012; 31(12): 2764–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Das J, Hammer J, Leonard K. The Quality of Medical Advice in Low-Income Countries. The Journal of economic perspectives 2008; 22(2): 93–114. [DOI] [PubMed] [Google Scholar]
- 177.Long Q, Klemetti R, Wang Y, Tao F, Yan H, Hemminki E. High Caesarean section rate in rural China: is it related to health insurance (New Co-operative Medical Scheme)? Soc Sci Med 2012; 75(4): 733–7. [DOI] [PubMed] [Google Scholar]
- 178.Sun X, Jackson S, Carmichael G, Sleigh AC. Catastrophic medical payment and financial protection in rural China: evidence from the New Cooperative Medical Scheme in Shandong Province. Health Econ 2009; 18(1): 103–19. [DOI] [PubMed] [Google Scholar]
- 179.Zhou M, Liu S, Kate Bundorf M, Eggleston K, Zhou S. Mortality In Rural China Declined As Health Insurance Coverage Increased, But No Evidence The Two Are Linked. Health affairs (Project Hope) 2017; 36(9): 1672–8. [DOI] [PubMed] [Google Scholar]
- 180.Lei X, Lin W. The New Cooperative Medical Scheme in rural China: does more coverage mean more service and better health? Health Econ 2009; 18 Suppl 2: S25–46. [DOI] [PubMed] [Google Scholar]
- 181.Gruber J, Lin M, Yi J. The Largest Insurance Program in History: Saving One Million Lives Per Year in China. 2021.
- 182.NHSA. Statistical Communiqué of the People’s Republic of China on the 2019 National Health Security Development. Beijing; Jun 24, 2020. [In Chinese]. [Google Scholar]
- 183.Chen P, Li F, Harmer P. Healthy China 2030: moving from blueprint to action with a new focus on public health. The Lancet Public health 2019; 4(9): e447. [DOI] [PubMed] [Google Scholar]
- 184.Berkman ND, Davis TC, McCormack L. Health literacy: what is it? Journal of health communication 2010; 15(S2): 9–19. [DOI] [PubMed] [Google Scholar]
- 185.Kurtz-Rossi S, Schwartz F, Alemayehu G, Chang P, Rubin D. Building Health Literacy Coalitions and NGOs. Studies in health technology and informatics 2020; 269: 258–63. [DOI] [PubMed] [Google Scholar]
- 186.Pengfei B, Zhuo M, Xinyue L, et al. Quantitative analysis of Internet medical policy based on the perspective of text mining in China. Chinese Hospitals 2021; 25(10): 50–3. [Google Scholar]
- 187.Cui F, He X, Zhai Y, et al. Application of Telemedicine Services Based on a Regional Telemedicine Platform in China From 2014 to 2020: Longitudinal Trend Analysis. Journal of medical Internet research 2021; 23(7): e28009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Jiang X, Xie H, Tang R, et al. Characteristics of Online Health Care Services From China’s Largest Online Medical Platform: Cross-sectional Survey Study. Journal of medical Internet research 2021; 23(4): e25817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Liu L, Wu F, Tong H, Hao C, Xie T. The Digital Divide and Active Aging in China. International journal of environmental research and public health 2021; 18(23). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.National Health Commission of the People’s Republic of China. The Internet diagnosis and treatment of the affiliated hospitals has increased 17 times over the same period last year. March 20, 2020. http://health.people.com.cn/n1/2020/0320/c14739-31641811.html (accessed Jan 23, 2022. [Google Scholar]
- 191.Wu J, Xie X, Yang L, et al. Mobile health technology combats COVID-19 in China. The Journal of infection 2021; 82(1): 159–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.He S, Feng D, Feng Z. Investigation on Utilization of Primary Public Health Services and Satisfactory Degree Among Elders in Rural Areas of China Based on the Goal of Equalization. Medicine and society [in Chinese] 2012; 25(5): 49–51. [Google Scholar]
- 193.Zhang X, Xiong Y, Ye J, Deng Z, Zhang X. Analysis of government investment in primary healthcare institutions to promote equity during the three-year health reform program in China. BMC Health Serv Res 2013; 13: 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Li X, Lu J, Hu S, et al. The primary health-care system in China. Lancet (London, England) 2017; 390(10112): 2584–94. [DOI] [PubMed] [Google Scholar]
- 195.Wang Z Policy analysis to promote the integration of health care. China Medical Insurance 2016; (3): 27–30. [Google Scholar]
- 196.Chen HG, Sheng LT, Wan ZZ, et al. The relationship between smoking and hyperuricemia in Chinese residents. Zhonghua yu fang yi xue za zhi [Chinese journal of preventive medicine] 2018; 52(5): 524–9. [DOI] [PubMed] [Google Scholar]
- 197.Lu Y, Gu Y, Yu W. Hospice and Palliative Care in China: Development and Challenges. Asia Pac J Oncol Nurs 2018; 5(1): 26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Yan Y, Zhang H, Gao W, et al. Current awareness of palliative care in China. The Lancet Global health 2020; 8(3): e333–e5. [DOI] [PubMed] [Google Scholar]
- 199.Hu K, Feng D. Barriers in palliative care in China. Lancet (London, England) 2016; 387(10025): 1272. [DOI] [PubMed] [Google Scholar]
- 200.Huang QS. A review on problems of China’s hospice care and analysis of possible solutions. Chin Med J (Engl) 2015; 128(2): 279–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Chen X, Giles J, Wang Y, Zhao Y. Gender Patterns of Eldercare in China. Feminist Economics 2018; 24(2): 54–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Zhao Y, Wang Y, Chen X, et al. China Health and Retirement Longitudinal Study, Survey report of 2020 special wave: China Health and Retirement Longitudinal Study; [working paper]. 2021. [Google Scholar]
- 203.Zhao Y, Wang Y, Chen X, et al. China Health and Retirement Report (in Chinese), 2018.
- 204.Lei X, Hu Y, McArdle JJ, Smith JP, Zhao Y. Gender Differences in Cognition among Older Adults in China. The Journal of human resources 2012; 47(4): 951–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Gibson MJ, Verma SK. Unmet need for personal assistance services among persons 50 or older with disabilities. AARP Public Policy Institute, Working Paper 2006–25 2006. [Google Scholar]
- 206.Quail JM, Wolfson C, Lippman A. Unmet Need for Assistance to Perform Activities of Daily Living and Psychological Distress in Community-Dwelling Elderly Women. Canadian journal on aging 2011; 30(4): 591–602. [DOI] [PubMed] [Google Scholar]
- 207.Xu H, Covinsky KE, Stallard E, Thomas J 3rd, Sands LP. Insufficient help for activity of daily living disabilities and risk of all-cause hospitalization. J Am Geriatr Soc 2012; 60(5): 927–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Zhen Z, Feng Q, Gu D. The Impacts of Unmet Needs for Long-Term Care on Mortality Among Older Adults in China. Journal of Disability Policy Studies 2015; 25(4): 243–51. [Google Scholar]
- 209.Chen L, Fan H, Chu L. The hidden cost of informal care: An empirical study on female caregivers’ subjective well-being. Social science & medicine (1982) 2019; 224: 85–93. [DOI] [PubMed] [Google Scholar]
- 210.Giles J, Glinskaya E, Zhao Y, Chen X, Hu Y. Population Aging and Long-Term Care Needs. In: Glinskaya Elena, Feng Z, eds. Options for Aged Care in China: Building an Efficient and Sustainable Aged Care System. Washington, DC: World Bank; 2018. [Google Scholar]
- 211.Conde-Sala JL, Garre-Olmo J, Turró-Garriga O, Vilalta-Franch J, López-Pousa S. Differential features of burden between spouse and adult-child caregivers of patients with Alzheimer’s disease: An exploratory comparative design. International journal of nursing studies 2010; 47(10): 1262–73. [DOI] [PubMed] [Google Scholar]
- 212.Ai J, Feng J. Gender differences in caring for spouses and their impact on health. School of Economics, Fudan University, mimeo: 2020. [Google Scholar]
- 213.Feng Z, Guan X, Feng X, Liu C, Zhan HJ, Mor V. Long-term care in China: reining in market forces through regulatory oversight. In: Mor V, Leone T, Maresso A, eds. Regulating Long Term Care Quality: An International Comparison. Cambridge, U.K.: Cambridge University Press; 2014: 409–44. [Google Scholar]
- 214.Feng Z, Zhan HJ, Feng X, Liu C, Sun M, Mor V. An Industry in the Making: The Emergence of Institutional Elder Care in Urban China. Journal of the American Geriatrics Society 2011; 59(4): 738–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Liu C, Feng Z, Mor V. Case-mix and quality indicators in Chinese elder care homes: are there differences between government-owned and private-sector facilities? Journal of the American Geriatrics Society 2014; 62(2): 371–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Wang J, Yang Q, Wu B. Effects of Care Arrangement on the Age of Institutionalization among Community-dwelling Chinese Older Adults. Journal of aging & social policy 2020: 1–16. [DOI] [PubMed] [Google Scholar]
- 217.Song Y, Anderson RA, Wu B, et al. Resident Challenges With Pain and Functional Limitations in Chinese Residential Care Facilities. The Gerontologist 2020; 60(1): 89–100. [DOI] [PubMed] [Google Scholar]
- 218.News China. Low Occupancy in Rural Homes for the Aged: Ill Equipped Facilities and Poor Management to Blame, January 21. 2013. https://www.chinanews.com.cn/sh/2013/01-21/4505572.shtml (accessed Jan 23, 2022.
- 219.Feng Z, Li Q, Glinskaya E, Zheng NT, Wiener JM. Building a Long-Term Care Delivery System with a Balanced Mix of Services. In: Glinskaya Elena, Feng Z, eds. Options for Aged Care in China: Building an Efficient and Sustainable Aged Care System. Washington, DC: : World Bank; 2018. [Google Scholar]
- 220.Xu Q, Chow JC. Exploring the community-based service delivery model: Elderly care in China. International social work 2011; 54(3): 374–87. [Google Scholar]
- 221.Wu B, Carter MW, Goins RT, Cheng C. Emerging services for community-based long-term care in urban China: a systematic analysis of Shanghai’s community-based agencies. Journal of Aging & Social Policy 2005; 17(4): 37–60. [DOI] [PubMed] [Google Scholar]
- 222.Wang Y, Jia X, Du W, et al. Intake of liquid beverage among Chinese adults aged 18–59 years old in 15 provinces, 2015. Wei sheng yan jiu = Journal of hygiene research 2018; 47(2): 178–82. [PubMed] [Google Scholar]
- 223.Wang Q, Ding X, Liu H, Shen Y, S. L. Analysis on pilot scheme of long-term care insurance system in China. Health Economics Research 2018. [In Chinese]; 6: 41–5 [Google Scholar]
- 224.Du P, Zaidi A, Chen H, Gu Y. Disparities among Older Persons in China. China Population and Development Studies 2017; 1(1): 19–44. [Google Scholar]
- 225.Zeng Y, Ren CR, Yuan-Yuan LI. Actuarial Evaluation of the Financial Operation Situation of China’s Basic Medical Insurance System. Journal of Finance & Economics [in Chinese] 2012. [Google Scholar]
- 226.Tamiya NP, Noguchi HP, Nishi AMD, et al. Population ageing and wellbeing: lessons from Japan’s long-term care insurance policy. Lancet, The 2011; 378(9797): 1183–92. [DOI] [PubMed] [Google Scholar]
- 227.Wu YT, Daskalopoulou C, Muniz Terrera G, et al. Education and wealth inequalities in healthy ageing in eight harmonised cohorts in the ATHLOS consortium: a population-based study. The Lancet Public health 2020; 5(7): e386–e94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Chaloupka FJ, Warner KE. The economics of smoking. In: Culyer AJ, Newhouse JP, eds. Handbook of Health Economics. Amsterdam: Elsevier; 2000: 1539–627. [Google Scholar]
- 229.Hu TW, Mao Z, Shi J, Chen W. Tobacco Taxation and Its Potential Impact in China. Paris: International Union Against Tuberculosis and Lung Disease; 2008. [Google Scholar]
- 230.Hu T-W, Mao Z, Shi J, Chen W. The role of taxation in tobacco control and its potential economic impact in China. Tob Control 2010; 19(1): 58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Hu T-W, Zhang X, Zheng R. China has raised the tax on cigarettes: what’s next? Tob Control 2016; 25(6): 609–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.WHO FCTC. The WHO Framework Convention on Tobacco Control: an overview 2015. https://www.who.int/fctc/WHO_FCTC_summary.pdf?ua=1 (accessed Jan 23, 2022.
- 233.Yang G, Wang Y, Wu Y, Yang J, Wan X. The road to effective tobacco control in China. Lancet (London, England) 2015; 385(9972): 1019–28. [DOI] [PubMed] [Google Scholar]
- 234.Goodchild M, Zheng R. Tobacco control and Healthy China 2030. Tob Control 2019; 28(4): 409–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Halpern SD, French B, Small DS, et al. Randomized Trial of Four Financial-Incentive Programs for Smoking Cessation. 2015; 372(22): 2108–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Charness G, Gneezy U. Incentives to Exercise. 2009; 77(3): 909–31. [Google Scholar]
- 237.Chin SO, Keum C, Woo J, et al. Successful weight reduction and maintenance by using a smartphone application in those with overweight and obesity. Scientific reports 2016; 6(1): 34563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.DeLuca L, Toro-Ramos T, Michaelides A, Seng E, Swencionis C. Relationship Between Age and Weight Loss in Noom: Quasi-Experimental Study. JMIR diabetes 2020; 5(2): e18363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet (London, England) 2020; 396(10248): 413–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Tinetti ME, Naik AD, Dodson JA. Moving From Disease-Centered to Patient Goals-Directed Care for Patients With Multiple Chronic Conditions: Patient Value-Based Care. JAMA Cardiol 2016; 1(1): 9–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Rhee JC, Done N, Anderson GF. Considering long-term care insurance for middle-income countries: comparing South Korea with Japan and Germany. Health policy (Amsterdam, Netherlands) 2015; 119(10): 1319–29. [DOI] [PubMed] [Google Scholar]
- 242.Mosca I, van der Wees PJ, Mot ES, Wammes JJG, Jeurissen PPT. Sustainability of Long-term Care: Puzzling Tasks Ahead for Policy-Makers. International journal of health policy and management 2017; 6(4): 195–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Ikegami N Financing Long-Term Care: Lessons From Japan % J International Journal of Health Policy and Management. 2019; 8(8): 462–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Colombo F, Llena-Nozal A, Mercier J, Tjadens F. Help Wanted? 2011. https://www.oecd-ilibrary.org/content/publication/9789264097759-en (accessed Jan 23, 2022.
- 245.Li F, Otani J. Financing elderly people’s long-term care needs: Evidence from China. Int J Health Plann Manage 2018; 33(2): 479–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Giles J, Meng X, Xue S, Zhao G. Can Information Influence the Social Insurance Participation Decision of China’s Rural Migrants?: The World Bank, 2018. [Google Scholar]
- 247.WHO. WHO Housing and Health Guidelines. 2018. https://www.who.int/publications/i/item/9789241550376 (accessed Jan 23, 2022.
- 248.Yao Y, Zhang H, Liu X, Liu X, Chu T, Zeng Y. Bridging the digital divide between old and young people in China: challenges and opportunities. The Lancet Healthy Longevity 2021; 2(3): e125–e6. [DOI] [PubMed] [Google Scholar]