Abstract
Introduction
Cross-national comparison suggests that the timing of the obesity epidemic differs across socio-economic groups (SEGs). Similar to the smoking epidemic, these differences might be described by the diffusion of innovations theory, which states that health behaviours diffuse from higher to lower SEGs. However, the applicability of the diffusion of innovations theory to long-term time trends in obesity by SEG is unknown. We studied long-term trends in the obesity prevalence by SEG in England, France, Finland, Italy, Norway, and the USA and examined whether trends are described by the diffusion of innovations theory.
Methods
Obesity prevalence from 1978 to 2019 by educational level, sex, and age group (25+ years) from health surveys was harmonized, age-standardized, Loess-smoothed, and visualized. Prevalence rate differences were calculated, and segmented regression was performed to obtain annual percentage changes, which were compared over time and across SEGs.
Results
Obesity prevalence among lower educated groups has exceeded that of higher educated groups, except among American men, in all countries throughout the study period. A comparable increase across educational levels was observed until approximately 2000. Recently, obesity prevalence stagnated among higher educated groups in Finland, France, Italy, and Norway and lower educated groups in England and the USA.
Discussion
Recent trends in obesity prevalence by SEG are mostly in line with the diffusion of innovations theory; however, no diffusion from higher to lower SEGs at the start of the epidemic was found. The stagnation among higher SEGs but not lower SEGs suggests that the latter will likely experience the greatest future burden.
Keywords: Diffusion of innovations theory, Obesity trends, Socio-economic inequalities
Introduction
The prevalence of obesity (body mass index [BMI] ≥30 kg/m2) in Europe has nearly tripled since the 1980s, commonly referred to as the “obesity epidemic”, and constitutes one of the major threats to public health in high-income countries [1, 2]. Cross-national evidence from countries at different stages of the obesity epidemic suggests that the timing of obesity trends differs across socio-economic groups (SEGs) [3]. Similar to what has been shown for smoking [4], the diffusion of innovations theory [5] might describe the differences in the obesity epidemic across SEGs. However, research on the long-term trends in obesity across SEGs is sparse. Given the high and unequal distribution of obesity, an improved understanding of how the obesity epidemic has and likely will spread across SEGs is warranted.
Previous research on the obesity epidemic focused on national trends and their likely development (e.g., [6]). Based on the empirical evidence, i.e. recent obesity declines among children and lessons from other lifestyle epidemics, it has been proposed that the obesity epidemic will follow a wave-shaped pattern [3, 7] with four consecutive stages [7]. Namely, the obesity prevalence increased slowly (stage 1), followed by a rapid incline in the prevalence (stage 2); currently, the prevalence is stagnating and might decline slowly (stage 3); and eventually, the decline may accelerate and level off (stage 4) [7]. The recent slowing-down of rates of increase in obesity prevalence in 18 European countries and the USA [6] is in line with this wave-shaped pattern of obesity prevalence. To extend the wave-shaped epidemic model with a socio-economic dimension, Jaacks et al. [3] analysed cross-sectional prevalence data from 30 countries at various stages of the epidemic. Their results demonstrate that socio-economic inequalities vary in countries that are at different stages of the epidemic, which suggests that the timing of the wave-shape trends differs across SEGs. More precisely, in countries that are yet to experience the rapid incline, the obesity prevalence in higher SEGs exceeded that of lower SEGs. The prevalence difference between higher and lower SEGs was smaller in countries which were experiencing the rapid incline, while it was reversed in countries where the increase in prevalence started to stagnate among higher but not yet lower SEGs [3].
European studies that examined trends in socio-economic inequalities in the obesity prevalence focused mostly on single countries [8, 9, 10, 11]. Contrary to the global evidence [7], European studies did not document inverse inequalities. Instead, they found that since the 1980s, the obesity prevalence in lower SEGs has exceeded that of the higher SEGs, although socio-economic inequalities did vary over time [8, 9, 10, 11]. Cross-national comparisons on trends in obesity inequalities are scarce. The exception is Hoffmann et al. [12] who compared trends in socio-economic obesity inequalities in 15 European countries and demonstrated that the increase in the obesity prevalence across educational levels was similar from 1990 to 2000. A systematic review conducted by Rokholm et al. [13] on trends after 1999 concluded that obesity might be stagnating among higher SEGs in some European countries. However, it has also been suggested that the reported stagnation among higher SEGs is the result of biases introduced by self-reporting and short study duration [14].
Although many theories aim to explain levels of health inequalities, only the diffusion of innovations theory describes timing differences in the adoption of innovations, such as health behaviours, in relation to socio-economic status, and is therefore relevant for the study of socio-economic differences in trends in obesity prevalence. The diffusion of innovations theory states that higher SEGs initially adopt an innovation which consequently spreads to lower SEGs [5]. Evidence from the smoking epidemic proves that the diffusion of innovations theory describes timing differences across SEGs. Both the uptake and rejection of tobacco smoking first occurred among higher SEGs and only later among lower SEGs [4, 15]. Similarly, the uptake and rejection of obesity-associated behaviours, such as a sedentary lifestyle and high-caloric diet, could follow a diffusion pattern resulting in a diffusion of obesity across SEGs. Thus far, only Krokstad et al. [16] examined the diffusion of obesity across educational groups from 1984 until 2008 in Norway and did neither find compelling evidence for the diffusion of obesity from higher to lower SEGs nor for the earlier stagnation of obesity among higher SEGs. No study so far has investigated the applicability of the diffusion of innovations theory to long-term obesity trends by SEG from multiple countries.
We, therefore, aimed to examine long-term trends in the obesity epidemic by SEG and determine how accurately observed trends are described by the diffusion of innovations theory. To do so, we formulated hypotheses for the socio-economic inequalities across the stages of the obesity epidemic [7] based on the diffusion of innovations theory (5) and the European literature on trends in obesity prevalence inequalities [8, 9, 10, 11, 12]:
1. At the start of the first stage of the obesity epidemic, the slow and steady incline, the obesity prevalence in higher SEGs exceeds that of lower SEGs because of the early uptake of obesity-associated behaviours, resulting in negative prevalence rate differences. Later in the first stage, the relationship between obesity and SEG reverses as a consequence of a stronger increase among lower SEGs because of the diffusion of obesity-associated behaviours. Furthermore, if obesity diffused from higher to lower SEGs in Europe, trends should diverge and prevalence rate differences should increase during the first stage.
2. During the second stage of the epidemic, the rapid incline, trends are parallel across SEGs, and thus, the rates of increase are similar across SEGs because behaviours have diffused earlier.
3. The third stage of the epidemic, the stagnation, will first be observable among higher SEGs because of the early uptake of preventive behaviours. Therefore, the rates of increase should first decrease among higher SEGS.
4. The fourth stage of the epidemic, the decline, will first be observable among higher SEGs and consequently among lower SEGs. This would mean that the prevalence should decrease among the higher SEGS followed by lower SEGS.
Data and Methods
See online supplementary Data and Methods file (www.karger.com/doi/10.1159/000527070) for more detailed information on the data and methods.
Data Sources
We obtained long-term time series data on the obesity prevalence among those aged 25 years and over by educational attainment, sex, and 5-year age group from England, Finland, France [17, 18], Italy, Norway, and the USA. To do so, we collected health surveys from the earliest (1978) until the most recent (2019) year available. The included countries were selected because of the availability of early data and their current far progression in the obesity epidemic [6, 7]. We selected surveys in which educational attainment could be converted to the International Standard Classification of Education (ISCED) 1997 and had a similar design over time to ensure a consistent time series. See Table 1 for a short overview of the included data.
Table 1.
Summary of the available survey years and age groups by country
| Country | Survey years | Age range (years) | BMI measure | Weighting |
|---|---|---|---|---|
| England | 1991–2018 (yearly) | 25–80+ | Measured | Unweighted |
| Finland | 1978–2014 (yearly) | 25–64 | Self-reported | Unweighted |
| France | 1980, 1991, 1996, 2000, 2002, 2003, 2005, 2008, 2010, 2014, 2016, 2017 | 25–74 | Self-reported | Weighted |
| Italy | 1990/1, 1994, 1999/2000, 2004/5, 2013, 2001–2018 | 25–75+ | Self-reported | Weighted |
| Norway | 1995, 2002, 2005, 2008, 2012, 2015, 2019 | 25–80+ | Self-reported | Weighted |
| USA | 1999/2000, 2001/2, 2003/4, 2005/6, 2007/8, 2009/10, 2011/12, 2013/14, 2015/16, 2017/18 | 25–80+ | Measured | Weighted |
Variables
Obesity was defined as a BMI of 30 kg/m2 or greater [19]. BMI is based on self-reported height and weight in all countries, except in England and the USA where measured height and weight are used. Respondents with no information on height and weight were excluded.
A lower age limit of 25 years was used to ensure the validity of educational attainment as measure for socio-economic status. Educational attainment was used to operationalize socio-economic status because of its long-term availability across countries, also for women. Furthermore, educational attainment is a robust measure of socio-economic status because it is unlikely to be subjected to reverse causation bias [20]. Trends in educational inequalities in the obesity prevalence are comparable to trends in other socio-economic inequalities, like income quintiles or occupational status [11, 20]. To include an age range as representative as possible, no upper age limit was imposed, except in France and Finland for which we imposed an upper age limit of 64 and 74 years, respectively, because of data restrictions.
Socio-economic status was defined by the highest level of education completed or the highest degree obtained, except in Finland, where educational attainment was based on attended school years. Educational attainment was harmonized according to the ISCED 1997 and reclassified into lower educated (levels 0–2: no, primary or lower secondary education), middle educated (levels 3–4: upper secondary and post-secondary non-tertiary education), and higher educated (levels 5–6: tertiary education) in line with previous research [21]. This categorisation facilitates comparison with other studies on obesity inequalities using the same data (i.e. [12]).
Methods
For each country and available survey, obesity prevalence was obtained by educational attainment, sex, and 5-year age group. If available, survey-specific sampling weights were applied for the whole time period to ensure consistency over time. For Finland and England, we present trends in unweighted prevalence because survey weights were not available for all years. To address missing within survey years, we linearly interpolated the prevalence in the respective strata from the previous and subsequent survey year. Consequently, prevalence rates were age-standardized using direct age-standardization and the revised European Standard Population [22] to facilitate cross-national and temporal comparison. Loess-smoothing with span 0.6 and degree 1 was applied to the age-standardized prevalence to produce smooth time trends and generate annual estimates for the rate differences.
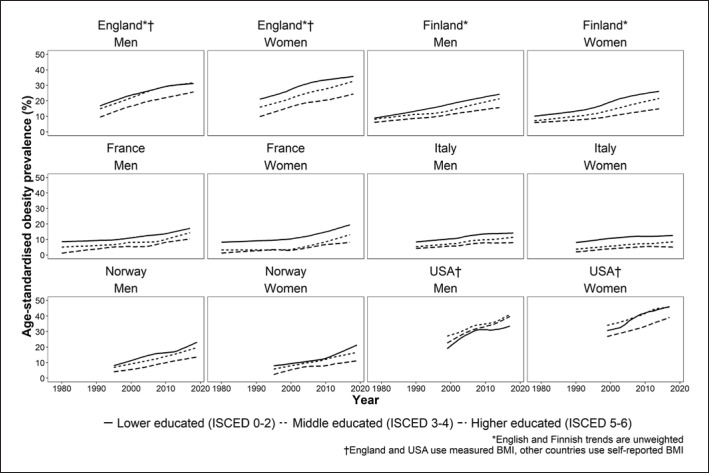
To compare the different trajectories of the obesity epidemic across educational levels, we visualized Loess-smoothed age-standardized obesity prevalence over time by educational level, sex, and country. The smoothed trends capture the individual data points while not being overly sensitive for fluctuations (online suppl. Tables; online suppl. Fig. S1).
To examine whether the obesity prevalence in higher SEGs exceeded that of lower SEGs and thereafter diffused, prevalence rate differences in Loess-smoothed age-standardized obesity prevalence between higher and lower educated groups were calculated by country and sex at a 5-year interval. As a sensitivity check, prevalence rate ratios, a relative measure for socio-economic inequalities, were calculated.
To examine the hypothesized parallel increase and early stagnation among higher SEGs, the annual percentage change (APC) in obesity prevalence by educational level, sex, country, and decade was calculated using segmented regression. Separate linear regression models were fitted by educational level, sex, educational level, decade, and country with interpolated age-specific obesity prevalence as the dependent variable and year and 5-year age group as independent variables.
Results
The obesity prevalence in lower educated groups exceeded that of higher educated groups, except among American men, over the entire examined period in selected countries (Fig. 1). Furthermore, prevalence rate differences have always been positive (Table 2), except among American men throughout. The trends across educational levels were relatively parallel, except in Finland and the USA (Fig. 1). The prevalence rate differences were also not universally increasing in the early years (Table 2). Prevalence rate differences increased in Finland, while those in France and Italy decreased (Table 2). The prevalence rate ratios revealed similar results (online suppl. Tables; online suppl. Fig. S1).
Fig. 1.
Loess-smoothed age-standardized prevalence (%) of obesity (BMI ≥30 kg/m2) in men and women in the six countries under study by educational attainment from 1978 to 2019.
Table 2.
Prevalence rate difference in the Loess-smoothed age-standardized obesity prevalence between lower (ISCED 0–2) and higher (ISCED 5–6) educated groups from 1978 to 2019 by 5-year interval, country, and sex
| Country | 1980 | 1985 | 1990 | 1995 | 2000 | 2005 | 2010 | 2015 | Most recenta |
|---|---|---|---|---|---|---|---|---|---|
| Men | |||||||||
| Englandb, c | − | − | − | 7.18 | 7.13 | 6.61 | 7.26 | 6.31 | 5.29 |
| Finlandb | 3.05 | 3.77 | 4.76 | 5.88 | 6.74 | 7.50 | 8.14 | − | 8.55 |
| France | 7.63 | 6.45 | 4.92 | 4.37 | 5.71 | 6.92 | 5.46 | 6.50 | 6.92 |
| Italy | − | − | 4.25 | 4.51 | 4.73 | 5.45 | 5.74 | 6.17 | 6.17 |
| Norway | − | − | − | 3.80 | 5.85 | 7.32 | 6.49 | 6.58 | 10.23 |
| USAc | − | − | − | − | −3.12 | −1.51 | −1.90 | −5.30 | −6.23 |
| Women | |||||||||
| Englandbc | − | − | − | 10.82 | 11.19 | 12.37 | 13.12 | 12.12 | 11.03 |
| Finlandb | 4.46 | 5.02 | 5.78 | 6.93 | 9.25 | 10.85 | 11.18 | − | 11.03 |
| France | 7.06 | 6.69 | 6.06 | 5.96 | 7.44 | 7.51 | 7.99 | 10.44 | 11.46 |
| Italy | − | − | 6.08 | 6.39 | 6.72 | 7.11 | 6.57 | 7.00 | 7.54 |
| Norway | − | − | − | 5.73 | 3.88 | 3.23 | 4.67 | 7.36 | 10.23 |
| USAc | − | − | − | − | 3.71 | 6.00 | 8.65 | 7.39 | 6.92 |
− indicates that the year was outside the observation period.
Most recent observations: England 2018, Finland 2014, France 2017, Italy 2018, Norway 2019, USA 2017/2018.
English and Finnish data are unweighted.
England and the USA use measured height and weight, other countries use self-reported height and weight.
The trends (Fig. 1) and APC (Table 3) in age-standardized obesity prevalence show that the increase was comparable across educational levels until approximately 2000. Firstly, in Finland and France, we observed an acceleration in the increase of the obesity prevalence, indicated by a steeper incline in the trends, in line with the first stage of the epidemic (Fig. 1). In Finland, the increase appeared greater among lower educated groups. In the USA, the increase was seemingly similar across educational levels although the prevalence was greatest among middle educated groups. Formal comparison of the APC across educational levels (Table 3) showed that the APC does not differ significantly until 2000 across educational groups in all countries.
Table 3.
APC in age-specific obesity prevalence (%) from 1990 onwards by decade, sex, country, and educational attainment (lower: ISCED 0–2, middle: ISCED 3–4, higher: ISCED 5–6). Obtained through segmented linear regression adjusted for age
| Country | Decade | Men |
Women |
||||
|---|---|---|---|---|---|---|---|
| lower | middle | higher | lower | middle | higher | ||
| Englandab | 1991–1999 | 0.75 (0.31, 1.19) | 0.67 (0.26, 1.07) | 0.76 (0.23, 1.29) | 0.26 (–0.28, 0.80) | 0.56 (0.12, 1.00) | 0.74 (0.16, 1.32) |
| 2000–2009 | 0.48 (0.05, 0.92) | 0.79 (0.40, 1.19) | 0.51 (0.04, 1.19) | 0.45 (0.04, 0.85) | 0.62 (0.24, 1.00) | 0.34 (–0.13, 0.82) | |
| 2010 to recentc | –0.06 (–0.65, 0.53) | 0.13 (–0.34, 0.61) | 0.48 (–0.01, 0.98) | –0.06 (–0.68, 0.55) | 0.54 (0.09, 0.99) | 0.63 (0.03, 1.24) | |
|
| |||||||
| Finlanda | 1990–1999 | 0.38 (0.00, 0.76) | 0.10 (–0.25, 0.45) | 0.17 (–0.14, 0.49) | 0.26 (–0.16, 0.65) | 0.24 (–0.16, 0.65) | 0.37 (0.07, 0.67) |
| 2000–2009 | 0.77 (0.31, 1.24) | 0.93 (0.48, 1.39) | 0.10 (–0.23, 0.43) | 0.67 (–0.10, 1.43) | 0.74 (0.26, 1.22) | 0.50 (0.18, 0.83) | |
| 2010 to recentc | 0.57 (–1.20, 2.35) | –0.65 (–2.32, 1.02) | 0.26 (–0.63, 1.15) | –1.28 (–5.79, 3.24) | –0.66 (–1.94, 0.62) | –0.04 (–0.82, 0.74) | |
|
| |||||||
| France | 1990–1999 | 0.15 (–0.14, 0.44) | 0.32 (–0.90, 1.54) | 0.45 (–0.73, 1.63) | 0.15 (–0.48, 0.78) | –0.21 (–0.81, 0.39) | –0.58 (–2.21, 1.06) |
| 2000–2009 | 0.16 (–0.22, 0.55) | –0.18 (–0.76, 0.40) | 0.32 (–0.05, 0.69) | 0.38 (0.03, 0.74) | 0.47 (0.16, 0.78) | 0.53 (0.13, 0.93) | |
| 2010 to recentc | 0.43 (0.11, 0.75) | 0.52 (0.11, 0.93) | 0.17 (–0.08, 0.42) | 0.61 (0.21, 1.01) | 0.62 (0.35, 0.89) | 0.29 (0.08, 0.50) | |
|
| |||||||
| Italy | 1990–1999 | –0.03 (–0.29, 0.24) | 0.00 (–0.21, 0.22) | 0.01 (–0.26, 0.27) | 0.34 (0.08, 0.60) | 0.18 (–0.01, 0.36) | 0.25 (–0.04, 0.54) |
| 2000–2009 | 0.35 (0.13, 0.56) | 0.38 (0.14, 0.61) | 0.26 (0.01, 0.51) | 0.15 (–0.10, 0.39) | 0.17 (–0.06, 0.40) | 0.05 (–0.18, 0.28) | |
| 2010 to recentc | 0.06 (–0.14, 0.26) | 0.28 (0.08, 0.49) | 0.02 (–0.22, 0.27) | 0.08 (–0.08, 0.24) | 0.19 (0.06, 0.32) | –0.16 (–0.38, 0.07) | |
|
| |||||||
| Norway | 1990–1999 | – | – | – | – | – | – |
| 2000–2009 | 0.91 (0.22, 1.59) | 0.45 (–0.05, 0.94) | 0.68 (0.33, 1.03) | 0.15 (–0.55, 0.86) | 0.23 (–0.16, 0.62) | 0.13 (–0.25, 0.51) | |
| 2010 to recentc | 1.21 (0.39, 2.03) | 0.66 (0.13, 1.19) | 0.35 (–0.17, 0.87) | 0.84 (0.09, 1.59) | 0.41 (–0.04, 0.87) | 0.32 (–0.04, 0.68) | |
|
| |||||||
| USAc | 1990–1999 | – | – | – | – | – | – |
| 2000–2009 | 1.30 (0.24, 2.37) | 1.45 (0.73, 2.17) | 1.04 (0.31, 1.76) | 2.02 (0.83, 3.22) | 0.94 (0.19, 1.68) | 0.75 (–0.06, 1.56) | |
| 2010 to recentc | 0.61 (–0.99, 2.21) | 1.38 (0.06, 2.70) | 1.24 (0.15, 2.33) | 0.87 (–0.88, 2.62) | 0.24 (–0.83, 1.31) | 0.92 (0.01, 1.82) | |
− indicates that only a single survey is conducted in this decade.
In England and Finland, obesity prevalence is unweighted.
England and the USA use measured height and weight, other countries use self-reported height and weight.
Most recent observations: England 2018, Finland 2014, France 2017, Italy 2018, Norway 2019, USA 2017/2018.
The stagnation in the increase of the obesity prevalence occurred earlier among higher than lower educated groups in most countries, except in England and the USA where the opposite is true (Fig. 1; Table 3). In Finland, France, Italy, and Norway, trends show that the prevalence started to stagnate among higher educated groups from approximately mid 2000 onwards. The APC was smaller from 2010 onwards compared to 2000–2009 among higher but not lower and middle-educated groups in aforementioned countries. From 2010 onwards, APC was also smaller among higher than lower educated groups in Finland, France, Italy, and Norway (Table 3). Stagnation in the APC (Table 3) already occurred among higher educated Finnish men and Italian women in 2000–2009, and since 2010, stagnation can also be observed among lower and middle Finnish men and Italian women. In England, the stagnation occurred among all groups but higher educated women. In the USA, stagnation occurred among lower and middle but not among higher educated groups for both sexes.
Discussion
Main Findings
We examined long-term trends, prevalence differences, and APC in obesity prevalence across educational levels and consequently assessed the applicability of the diffusion of innovations theory to the obesity epidemic in five European countries and the USA. The obesity prevalence in lower educated groups has exceeded that of higher educated groups for the available years between 1978 and 2019 in selected countries − except among American men. Increases across educational groups were comparable until about 2000. The stagnation in obesity prevalence was first observed among higher educated in Finland, France, Italy, and Norway, which was followed by stagnation among lower and middle educated among Italian women and Finnish men. In contrast, the obesity prevalence in the USA and England stagnated among lower and not higher educated groups.
Interpretation
The parallel trends (Fig. 1) and the absence of diverging prevalence rate difference (Table 2) in the early years (before 1990) of the obesity epidemic in selected countries do not support a diffusion of obesity from higher to lower educated groups during the first stage of the obesity epidemic in selected European countries. The low obesity prevalence among higher educated groups and steep incline observed, particularly in France and Finland, suggest that we do observe the first stage of the epidemic. Furthermore, the already large inequalities and low prevalence observed during early years in some of the countries suggest that the absence of diffusion is not an artefact of the inability to observe the initial stage of the obesity epidemic. For instance, in 1980, the age-standardized obesity prevalence among higher educated French men and women was 0.7%, and prevalence rate differences were 7.6% for men and 7.1% for women. Hence, it is highly unlikely that obesity diffused during the obesity epidemic that started in these countries (i.e., since the 1980s). Instead, a parallel increase across educational groups was observed until 2000 in contrast to what the global evidence showed [3]. A possible explanation for the absence of the diffusion at the beginning of the obesity epidemic might be provided by the suspected causes of the obesity epidemic in high-income countries. It has been suggested that widespread and sudden changes in environmental factors (i.e., agricultural revolution, urbanization, globalization) resulted in decreased physical activity and a nutritional transition [23, 24, 25], driving the surge of obesity. Such environmental changes are likely to affect all members of society regardless of socio-economic status. Individual behaviours and their diffusion are therefore unlikely to have been a determining factor during the initial stages of the obesity epidemic in high-income countries. In sum, the diffusion of innovations theory does not describe trends by SEG in the early stages of the obesity epidemic in the selected countries because the role of environmental factors likely outweighed that of individual behaviours.
While studies examining European trends [9, 11, 12, 16], including the current study, do not observe a diffusion at the start of the obesity epidemic, the global cross-national comparison by Jaacks et al. [3] does. This discrepancy might be explained by differences in the pace and change in diet, sedentary lifestyle, and interventions by SEGs across nations and over time [23, 24]. Hence, global cross-sectional patterns do not necessarily reflect historic trends in Europe and vice versa [23].
The recent stagnation in obesity prevalence among higher educated groups in most countries is in line with the diffusion of innovations theory and might be explained by the early uptake of preventive behaviours, such as increasing physical activity and reducing ultra-processed food and calorie intake [23, 26]. Furthermore, the stagnation among Italian women and Finnish men with lower socio-economic status following the stagnation among higher SEGs suggests that eventually, the obesity prevalence might also stagnate among lower SEGs, presumably due to the later uptake of preventive behaviours. Our unexpected finding of the early stagnation among lower SEGs observed in England and the USA might be explained by the implementation of policies addressing environmental causes for obesity because of the high obesity prevalence in England and the UK [6]. For example, sugar-sweetened beverage taxation and regulation of food formulations are more likely to reduce the obesity prevalence among lower SEGs than policies that target individuals and their behaviour, such as information campaigns [26, 27]. Widespread introduction of such policies could be more common in countries with high obesity prevalence, such as England and the USA, driving the stagnation among lower SEGs. Additional research is required to test this hypothesis. Despite the deviations observed in England and the USA, recent obesity trends by educational level are relatively well described by the diffusion of innovations theory.
Limitations
Firstly, the predominant issue affecting the reliability of time trends is the lack of consistent annual national health surveys with information on obesity. In France, Italy, and Norway, various national health surveys are conducted at irregular time intervals, and we had to interpolate the available data to obtain yearly data, thereby introducing some bias regarding the trends. In the USA and England, on the other hand, one health survey is conducted biannually or annually, respectively, generating the most reliable time trend series. In countries where the provided information was not consistent over time, we took deliberate choices to enhance the comparability over time. That is, in Finland, although annual survey data were available, we imposed an upper age limit due to changing sampling strategies among older age groups and excluded the data since 2015 because of changes in the survey design. In France, we imposed an upper age limit because of changes of in sampling strategy. In England and Finland, we used unweighted data throughout because weighted data were not consistently available over time. Our sensitivity analysis comparing trends in unweighted and weighted obesity prevalence − when both were available − revealed comparable trends in most countries (online suppl. Data and Methods; online suppl. Fig. S1).
Secondly, trends in educational differences in any outcome are likely affected by changes over time in the composition of education groups. During the time span of our study, and for the countries under study, the proportion of high-educated groups has increased, while that of low-educated groups has decreased with time. This is the so-called educational expansion. It could have resulted in the low-educated groups becoming more select over time and − consequently − more likely to exhibit worse health behaviours and outcomes, which could in itself result in an increase in educational inequalities over time. Our sensitivity analysis using a relative measure for educational status in Finland, namely, tertiles based on years of school attended, revealed largely similar trends, especially for lower and higher educated groups (online suppl. Data and Methods; online suppl. Fig. S2). We, thus, do not expect a large role of educational expansion on our final conclusions. Thirdly, although not the main aim of the study, caution is warranted when comparing obesity prevalences cross-nationally. Firstly, educational attainment was classified by the highest degree completed in all countries, except in Finland where respondents were asked about school years attended, which will likely lead to an overestimation of the number of individuals with higher education compared to other countries. Furthermore, English and Finnish data are unweighted because survey weights were not consistently available, whereas data for the other countries are weighted, which could result in different obesity prevalence levels. Furthermore, the obesity prevalence data for England and the USA were based on measured height and weight instead of self-reported, while self-reporting generally leads to underestimations of BMI and, thus, obesity [28]. As mentioned, the age selections were not consistent throughout.
In line with many previous studies, we focussed solely on obesity prevalence and not overweight. The well-established association between obesity and mortality compared to overweight (BMI between 25 and 30) underlines the importance of examining obesity separately [29, 30]. Additional research is required to analyse long-term trends in overweight and how well the theory of diffusion of innovations describes trends in overweight.
Conclusion
Our study on the applicability of the diffusion of innovations theory to the obesity epidemic in five European countries and the USA for the available years from 1978 until 2019 revealed that while early trends are not indicative of a diffusion of obesity from higher to lower SEGs, recent trends are in line with the diffusion of innovations theory in most selected countries. The absence of the diffusion and parallel increase observed early in the epidemic might be explained by a larger role of structural factors affecting all SEGs equally than socio-economic factors driving group-specific behaviours. The recent stagnation among higher but not lower SEGs in most countries implies that lower SEGs will likely experience the greatest future burden of obesity, and consequently, inequalities may widen even further. Our findings emphasize the importance of comprehensive policies that address structural factors of obesity and thus exert an equitable effect, at minimum [27]. The stagnating obesity prevalence among lower SEGs in England and USA and its drivers could serve as a starting point.
Statement of Ethics
Ethics approval was not required as the research makes use of aggregate secondary data which are publicly available and from which individuals cannot be identified.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
This work is funded by the Netherlands Organisation for Scientific Research (NWO) in relation to the research project “Forecasting future socio-economic inequalities in longevity: the impact of lifestyle ‘epidemics’,” under Grant No. VIC.191.019. See https://www.futurelongevitybyeducation.com/.
Author Contributions
Fanny Janssen conceptualized the study. Eva Kagenaar, Fanny Janssen, Anton E Kunst, and Wanda Monika Johanna Van Hemelrijck contributed to the conception and design of the work. Fanny Janssen and Eva Kagenaar acquired the data. Eva Kagenaar performed the data handling and conducted the analysis. Eva Kagenaar, Fanny Janssen, Anton E Kunst, and Wanda Monika Johanna Van Hemelrijck contributed to the interpretation of the data. Eva Kagenaar wrote the first draft of the paper. Fanny Janssen, Anton E Kunst, and Wanda Monika Johanna Van Hemelrijck revised the work for content. Eva Kagenaar, Fanny Janssen, Anton E Kunst, and Wanda Monika Johanna Van Hemelrijck approved the final submitted version of the work.
Data Availability Statement
The obtained deidentified survey data regarding obesity and the aggregate data on obesity prevalence by educational level, sex, and age cannot be shared with others because of restricted access policy, but access to these data can be requested through the institutes that own the data (see the online suppl. Data and Methods file). The age-standardized obesity prevalence used to create the final tables and figures will be made available through OpenScienceFramework as well as the scripts that we used for the analysis. Further enquires can be made to the corresponding author.
Acknowledgments
The authors thank Jean-Baptiste Richard and Benoît Salanave (both Santé Publique France), Satu Helakorpi and Jonna Ikonen (both Finnish Institute for Health and Welfare THL), and Elin Skretting Lunde and Jacob Osnes (both Statistics Norway) for providing national aggregate obesity prevalence data by educational level; Lidia Gargiulo and Antonella Ciccarese (both Italian National Institute of Statistics [ISTAT]) for providing the deidentified survey data regarding obesity; and Gwenn Menvielle (Institut national de la santé et de la recherche médicale INSERM, France) for help in acquiring the French deidentified survey data through Réseau Quetelet. We also thank Meik Herber (Master Population Studies, University of Groningen) and Mark van der Broek (Research Master Economics, University of Groningen) for their assistance with the data handling.
Funding Statement
This work is funded by the Netherlands Organisation for Scientific Research (NWO) in relation to the research project “Forecasting future socio-economic inequalities in longevity: the impact of lifestyle ‘epidemics’,” under Grant No. VIC.191.019. See https://www.futurelongevitybyeducation.com/.
References
- 1.Catenacci VA, Hill JO, Wyatt HR. The obesity epidemic. Clin Chest Med. 2009;30((3)):415–44. doi: 10.1016/j.ccm.2009.05.001. vii. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization Obesity. 2018 Available from: WHO/Europe | WHO/Europe approaches to obesity. [Google Scholar]
- 3.Jaacks LM, Vandevijvere S, Pan A, McGowan CJ, Wallace C, Imamura F, et al. The obesity transition: stages of the global epidemic. Lancet Diabetes Endocrinol. 2019;7((3)):231–40. doi: 10.1016/S2213-8587(19)30026-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khlat M, Pampel F, Bricard D, Legleye S. Disadvantaged social groups and the cigarette epidemic: limits of the diffusion of innovations vision. Int J Environ Res Public Health. 2016;13((12)):1230. doi: 10.3390/ijerph13121230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rogers EM. Diffusion of innovations. New York: Free Press of Glencoe; 1962. [Google Scholar]
- 6.Janssen F, Bardoutsos A, Vidra N. Obesity prevalence in the long-term future in 18 European countries and in the USA. Obes Facts. 2020;13((5)):514–27. doi: 10.1159/000511023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu L, Lam TH. Stage of obesity epidemic model: learning from tobacco control and advocacy for a framework convention on obesity control. J Diabetes. 2018;10((7)):564–71. doi: 10.1111/1753-0407.12647. [DOI] [PubMed] [Google Scholar]
- 8.Bann D, Johnson W, Li L, Kuh D, Hardy R. Socioeconomic inequalities in body mass index across adulthood: coordinated analyses of individual participant data from three British birth cohort studies initiated in 1946, 1958 and 1970. PLoS Med. 2017;14((1)):e1002214. doi: 10.1371/journal.pmed.1002214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Faeh D, Braun J, Bopp M. Prevalence of obesity in Switzerland 1992–2007: the impact of education, income and occupational class. Obes Rev. 2011;12((3)):151–66. doi: 10.1111/j.1467-789X.2010.00793.x. [DOI] [PubMed] [Google Scholar]
- 10.Gallus S, Colombo P, Scarpino V, Zuccaro P, Negri E, Apolone G, et al. Overweight and obesity in Italian adults 2004, and an overview of trends since 1983. Eur J Clin Nutr. 2006;60((10)):1174–9. doi: 10.1038/sj.ejcn.1602433. [DOI] [PubMed] [Google Scholar]
- 11.Prättälä R, Sippola R, Lahti-Koski M, Laaksonen MT, Mäkinen T, Roos E. Twenty-five year trends in body mass index by education and income in Finland. BMC Public Health. 2012;12((1)):936. doi: 10.1186/1471-2458-12-936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoffmann K, De Gelder R, Hu Y, Bopp M, Vitrai J, Lahelma E, et al. Trends in educational inequalities in obesity in 15 European countries between 1990 and 2010. Int J Behav Nutr Phys Act. 2017;14((1)):63. doi: 10.1186/s12966-017-0517-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rokholm B, Baker JL, Sørensen TIA. The levelling off of the obesity epidemic since the year 1999: a review of evidence and perspectives. Obe Rev. 2010;11((12)):835–46. doi: 10.1111/j.1467-789X.2010.00810.x. [DOI] [PubMed] [Google Scholar]
- 14.Visscher TLS, Heitmann BL, Rissanen A, Lahti-Koski M, Lissner L. A break in the obesity epidemic? Explained by biases or misinterpretation of the data? Int J Obes. 2015;39((2)):189–98. doi: 10.1038/ijo.2014.98. [DOI] [PubMed] [Google Scholar]
- 15.Pampel FC. Diffusion, cohort change, and social patterns of smoking. Soc Sci Res. 2005;34((1)):117–39. doi: 10.1016/j.ssresearch.2003.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krokstad S, Ernstsen L, Sund ER, Bjorngaard JH, Langhammer A, Midthjell K, et al. Social and spatial patterns of obesity diffusion over three decades in a Norwegian county population: the HUNT Study. BMC Public Health. 2013;13:973. doi: 10.1186/1471-2458-13-973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Health Barometre, Santé publique France, the French national public health agency, France, YEAR(S) (Health Barometre was funded and carried out by Santé publique France, the French national public health agency)
- 18.Enquête Décennale Santé - Santé Publique France (Gwenn Menvielle & Jean-Baptiste Richard) http://quetelet.progedo.fr/?rubrique75 http://inpes.santepubliquefrance.fr/Barometres/index.asp .
- 19.World Health Organization WHO Global data base on body mass index: BMI classification. 2009. Available from: http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi.
- 20.Daly MC, Duncan GJ, McDonough P, Williams DR. Optimal indicators of socioeconomic status for health research. Am J Public Health. 2002;92((7)):1151–7. doi: 10.2105/ajph.92.7.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.UNESCO International Standard Classification of Education: ISCED 1997. 2006. Available from: https://unesdoc.unesco.org/ark:/48223/pf0000146967.
- 22.EUROSTAT Revision of the European Standard Population. EUROSTAT Methodologies and Working Papers. 2013. Available from: https://ec.europa.eu/eurostat/documents/3859598/5926869/KS-RA-13-028-EN.PDF/e713fa79-1add-44e8-b23d-5e8fa09b3f8f.
- 23.Popkin BM. Nutritional patterns and transitions. Popul Dev Rev. 1993;19((1)):138–57. [Google Scholar]
- 24.Popkin BM. The nutrition transition and obesity in the developing world. J Nutr. 2001;131((3)):871S–3S. doi: 10.1093/jn/131.3.871S. [DOI] [PubMed] [Google Scholar]
- 25.Romieu I, Dossus L, Barquera S, Blottière HM, Franks PW, Gunter M, et al. Energy balance and obesity: what are the main drivers? Cancer Causes Control. 2017;28((3)):247–58. doi: 10.1007/s10552-017-0869-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Swinburn B, Egger G. Preventive strategies against weight gain and obesity. Obes Rev. 2002;3((4)):289–301. doi: 10.1046/j.1467-789x.2002.00082.x. [DOI] [PubMed] [Google Scholar]
- 27.Olstad DL, Teychenne M, Minaker LM, Taber DR, Raine KD, Nykiforuk CIJ, et al. Can policy ameliorate socioeconomic inequities in obesity and obesity-related behaviours? A systematic review of the impact of universal policies on adults and children. Obes Rev. 2016;17((12)):1198–217. doi: 10.1111/obr.12457. [DOI] [PubMed] [Google Scholar]
- 28.Niedhammer I, Bugel I, Bonenfant S, Goldberg M, Leclerc A. Validity of self-reported weight and height in the French GAZEL cohort. Int J Obes Relat Metab Disord. 2000;24((9)):1111–8. doi: 10.1038/sj.ijo.0801375. [DOI] [PubMed] [Google Scholar]
- 29.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309((1)):71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Winter JE, MacInnis RJ, Wattanapenpaiboon N, Nowson CA. BMI and all-cause mortality in older adults: a meta-analysis. Am J Clin Nutr. 2014;99((4)):875–90. doi: 10.3945/ajcn.113.068122. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The obtained deidentified survey data regarding obesity and the aggregate data on obesity prevalence by educational level, sex, and age cannot be shared with others because of restricted access policy, but access to these data can be requested through the institutes that own the data (see the online suppl. Data and Methods file). The age-standardized obesity prevalence used to create the final tables and figures will be made available through OpenScienceFramework as well as the scripts that we used for the analysis. Further enquires can be made to the corresponding author.