Abstract
Human peripheral blood monocytes become apoptotic following phagocytosis of Staphylococcus aureus. In this study, we investigated the mechanisms involved in this phenomenon. Cells exposed to bacteria were examined for the surface expression of Fas and Fas ligand (FasL). The level of soluble form of FasL was also measured in the culture supernatants. As Fas-mediated apoptosis involves the activation of caspases, the activities of caspase-8 and caspase-3 were determined. Finally, the involvement of oxidative stress in apoptosis of infected monocytes was investigated. The data indicated that as a consequence of phagocytosis of S. aureus, FasL is released from the monocyte surface and induces apoptosis of phagocytic monocytes and to some extent the bystander cells. The importance of this mechanism was confirmed by demonstrating that blockage of CD95 prevents S. aureus-induced apoptosis of monocytes. Cell death occurring after phagocytosis of S. aureus involves the activation of caspase-3-like proteases, as the specific caspase-3 inhibitor suppressed apoptosis of infected cells. The generation of reactive oxygen intermediates by phagocytic monocytes by itself is not sufficient as a death signal but rather acts in up-regulating FasL shedding and possibly in modulating caspase activity.
Programmed cell death, resulting from the activation of a cell suicide program known as apoptosis, plays an important role in the development and functioning of the immune system. For example, this phenomenon is essential during the elimination of self-reacting T cells in the thymus, B-cell activation in the germinal center, T-cell-mediated cytotoxicity, and peripheral tolerance (6, 11). Apoptotic cells undergo several morphological and biochemical changes, including cell shrinkage, condensation of nuclear material, and finally the formation of apoptotic bodies (19, 51). These changes can be induced by a number of different stimuli including the ligation of Fas (CD95) and tumor necrosis factor receptors, treatment with glucocorticoids, and the withdrawal of growth factors (7, 8, 31, 43).
Monocytes/macrophages were shown to die by apoptosis after the withdrawal of growth or differentiation factors, after phagocytosis of certain bacteria, and after antigen presentation to CD4+ memory cells (2, 10, 12, 13, 26, 27, 32, 35, 39, 48, 53). Zychlinsky et al. (53) were the first to show that macrophages infected by Shigella flexneri undergo apoptosis. Since then, there have been several reports showing that bacteria may trigger apoptosis of myeloid cells (2, 10, 24, 25, 49). We have previously shown that phagocytosis of Staphylococcus aureus, and other extracellular bacteria, by peripheral blood monocytes results in apoptosis of phagocytic cells (2). Following phagocytosis of viable bacteria, monocytes displayed apoptotic-like changes including typical morphological changes with parallel DNA breaks detected by terminal deoxynucleotidyltransferase-mediated dUTP-biotin nick end labeling assay and finally typical DNA fragmentation as shown by the laddering pattern after DNA electrophoresis. However, the mechanisms responsible for apoptosis of phagocytic monocytes remain unknown. Several studies have documented an important role of reactive oxygen intermediates (ROIs) in apoptosis (reviewed in reference 5). Treatment of cells with hydrogen peroxide, ionizing irradiation, or cytotoxic drugs such as quinones that undergo redox cycling and cause ROI formation induces apoptosis. Intracellular ROI formation has also been implicated in apoptosis induced by tumor necrosis factor alpha or growth factor withdrawal, since antioxidants or the overexpression of antioxidant enzymes prevented cell death in this system (18, 30, 52). However, some reports suggest that ROIs may not be necessary for apoptotic cell death, since in some cases apoptosis was not affected by antioxidants and proceeded in nearly anaerobic conditions where ROIs were not generated (21, 29, 30). Furthermore, under certain conditions oxidants were shown to inhibit apoptosis (15). The growing body of evidence indicates that small amounts of intracellular ROIs, too low to induce cellular damage, may play an important role as second messengers involved in the regulation of gene expression. For example, the activation of transcription factors, such as NF-κB and AP-1, is controlled by ROIs (1, 33, 41).
The respiratory burst which occurs during phagocytosis plays an essential role in the killing of ingested microorganisms; therefore, ROIs are likely to be involved in triggering apoptosis of phagocytic cells. However, as phagocytosis of heat-killed bacteria or latex beads, both inducing a respiratory burst, did not trigger monocyte apoptosis, we initially dismissed this possibility (2). More recent findings, showing that agents which increase the intracellular level of antioxidants also increase the resistance of various cells to apoptosis, prompted us to reevaluate the possible involvement of ROIs in apoptosis of monocytes occurring after phagocytosis of bacteria.
In this study, we examined the effects of various antioxidants on apoptosis induced by S. aureus. We provide evidence which suggests that the overexpression and/or shedding of Fas ligand (FasL) may be controlled by redox processes occurring during or after phagocytosis of S. aureus. Our results suggest that ROIs produced by monocytes during phagocytosis of bacteria are not directly responsible for apoptosis of these cells but rather are involved in the Fas-FasL pathway leading to the activation of downstream caspases such as caspase-3.
MATERIALS AND METHODS
Monocytes.
Peripheral blood mononuclear cells (PBMC) were isolated by standard Ficoll-Paque (Pharmacia, Uppsala, Sweden) gradient centrifugation from EDTA-treated blood from healthy donors. The cells were resuspended in Hanks' balanced salt solution supplemented with 1% autologous plasma and subjected to countercurrent centrifugal elutriation (Beckman JE-6B elutriation system equipped with a 5-ml Sanderson separation chamber) to obtain monocytes. Monocyte enrichment was confirmed by nonspecific esterase staining (85 to 95% positive) and/or the expression of CD14 antigen (80 to 90% positive for Leu-M3 [Becton Dickinson Immunocytometry Systems, San Jose, Calif.]). Monocytes (5 × 106/ml) were then washed once with cold RPMI 1640 and kept on ice in RPMI 1640 supplemented with l-glutamine and 10% fetal calf serum without antibiotics (all reagents from GIBCO, Grand Island, N.Y.) until used.
Bacteria.
S. aureus ATCC 25923 was grown for 18 h on tryptic broth (Tryptone soyabean casein digest medium; Oxoid), washed twice with a large volume of saline, and opsonized (30 min, 37°C) in the presence of 10% human serum (pooled fresh human serum stored in aliquots at −70°C). After further washing, the density of bacteria was measured spectrophotometrically (540 nm), and cell number was calculated using the standard curve based on CFU counts. Finally, the concentration of bacteria was adjusted to 109/ml in phosphate-buffered saline (PBS). To enable the quantitative analysis of phagocytosis by flow cytometry, bacteria were incubated before opsonization for 2 h at 37°C in PBS containing 0.1% fluorescein isothiocyanate (FITC; BHD Chemicals Ltd., Poole, England). After two washings, bacteria were opsonized as described above. In some experiments, bacteria were killed by incubation in a water bath at 72°C for 30 min.
Latex particles.
Latex particles (diameter, 0.8 to 1.0 μm) were obtained from the Institute of Catalysis and Surface Chemistry, Polish Academy of Sciences, Cracow. They were washed twice with 70% ethanol and resuspended in PBS at a concentration of 1.5 × 109/ml.
Phagocytosis.
Monocytes (106/ml) were incubated in Falcon 2054 tubes (Becton Dickinson) with opsonized FITC-labeled S. aureus (ratio of 1:20 unless stated otherwise) in a total volume of 0.5 ml of RPMI 1640 without antibiotics. Cells were incubated with bacteria for 0.5 h and then cultured for up to 24 h in the presence of antibiotics (penicillin, 100 U/ml; streptomycin, 100 μg/ml) (GIBCO). This procedure was chosen to reduce the possibility of some phagocytic cells being lost during the washing procedure. Alternatively, after 30 min of incubation of monocytes with bacteria, 1 ml of ice-cold complete medium (with antibiotics) was added; cells were centrifuged (110 × g, 5 min) to separate phagocytic cells from free bacteria, and the pellet was resuspended in complete medium. In parallel, monocytes without bacteria were also incubated as controls. To increase the intracellular level of antioxidants, in some experiments monocytes were preincubated for 2 h with N-acetyl-l-cysteine (NAC; Sigma, St. Louis, Mo.) or a reduced form of glutathione (GSH; Merck, Darmstadt, Germany), both at a final concentration of 25 mM unless stated otherwise, followed by incubation with bacteria. To block NADPH oxidase activity (9), monocytes were preincubated with 10 μM diphenylene iodonium (DPI; Sigma). Thereafter, bacteria were added and phagocytosis was performed as described above. In some experiments, latex particles (monocyte/particle ratio of 1:50) were used instead of bacteria.
Flow cytometry determination of apoptosis and cell viability.
Apoptosis of monocytes was determined by flow cytometry, annexin V binding assay, and/or propidium iodide (PI) staining. At indicated time points cells, were collected, washed with annexin V staining buffer (HEPES buffer containing 150 mM NaCl, 5 mM KCl, 1 mM MgCl2, and 1.8 mM CaCl2 [pH 7.4]), and labeled with phycoerythrin (PE)-conjugated annexin V (Pharmingen) for 15 min on ice to detect phosphatidylserine expression on the outer cell membrane layer. After washing, cells were analyzed on a FACSCalibur flow cytometer (Becton Dickinson). Alternatively, standard PI staining was used to detect monocyte apoptosis and viability after phagocytosis of bacteria. This simple assay was used in the majority of experiments, as we have shown previously that in the case of apoptosis induced by phagocytosis of S. aureus, PI uptake correlates very well with DNA fragmentation assay results (13). PI staining was also very useful in combination with FITC-labeled bacteria.
Isolation of genomic DNA and DNA gel electrophoresis.
To exclude the possibility of leakage of fragmented, low-molecular-weight DNA from cells during washing, DNA was isolated from the whole-cell culture volume (1 ml). Suspensions of monocytes (2 × 106/ml) were supplemented with sodium dodecyl sulfate (Fluka Chemie AG, Buchs, Switzerland) to a final concentration of 0.5%, mixed vigorously, and incubated at 65°C for 1 h to obtain a viscous, clear cell lysate. The lysates were then treated with RNase A (20 μg/ml; 37°C, 1 h) and proteinase K (20 μg/ml; 50°C, 1 h) and extracted twice with an equal volume of phenol-chloroform (1:1). DNA in the aqueous phase was precipitated at −20°C in 0.3 M sodium acetate–75% ethanol. Precipitates were pelleted by centrifugation (13,000 × g, 10 min, 4°C), washed with ice-cold 70% ethanol, and dried. For electrophoresis, DNA samples were dissolved in 50 μl of Tris-EDTA buffer. Gel loading buffer (25% Ficoll 400, 10 mM EDTA, 0.01% bromophenol blue, 0.01% xylene cyanol; 10 μl) was added, and the samples were heated at 65°C for 10 min. Aliquots corresponding to 106 cells were loaded per slot, and samples were subjected to electrophoresis in 2% agarose gel containing ethidium bromide (0.5 μg/ml in Tris—borate—1 mM EDTA buffer [pH 8.2] at 5 V/cm for 90 min). DNA was visualized by UV light detection and then photographed. The analyzed DNA fragments in the samples were compared with standard size fragments of the DNA marker, ΦX174 HincII (Advanced Biotechnologies Ltd., Leatherhead, England). All other chemicals were purchased from Sigma.
Chemiluminescence measurement.
To determine the efficiency of antioxidants, the luminol-dependent chemiluminescence of monocytes triggered by phagocytosis of S. aureus in the presence or absence of ROI scavengers was measured. Krebs-Ringer phosphate buffer containing glucose (11 mM) and bivalent cations (0.54 mM Ca2+ and 1.12 mM Mg2+) plus 2 mM luminol (5-amino-2-3-dihydro-1,4-phatlanedione; Sigma) (CL medium) was used as a medium for chemiluminescence measurement. Monocytes (0.5 × 106) were suspended in 0.5 ml of CL medium, with or without the addition of ROI scavengers, and tubes were placed in a six-channel luminometer (Multi-Biolumat LB9505C; Berthold, Vienna, Austria). Thereafter, a bacterial suspension was added at the ratio 1:50, and chemiluminescence was recorded for 30 min.
CGD patient.
To examine the role of ROIs in apoptosis of monocytes occurring after phagocytosis of bacteria, PBMC were isolated from 5 ml of EDTA-treated peripheral blood of a 5-year-old boy suffering from the X-linked form of chronic granulomatous disease (CGD). The patient was hospitalized at the Paediatric Clinic of the Polish-American Institute of Paediatrics in Cracow, Poland. His blood was taken twice, during routine laboratory tests, after written consent of the parents was obtained. The X-linked form of CGD was confirmed by chemiluminescence measurements of whole blood after stimulation with latex particles and phorbol myristate acetate (Sigma) and by a nitroblue tetrazolium (NBT) reduction test performed using isolated granulocytes. As monocytes comprise up to 20% of the PBMC population, PBMC (106/ml) were incubated (37°C, 0.5 h) alone (control) or with suspensions of opsonized FITC-labeled S. aureus at an estimated monocyte/bacterium ratio of 1:10. Cells were incubated in Falcon 2054 tubes in a total volume of 0.5 ml. PBMC isolated from a healthy donor were similarly treated in parallel. After incubation for 0.5 h, antibiotics were added and cells were cultured for up to 24 h.
Antigen activation of PBMC.
To demonstrate the existence of the Fas-FasL-dependent pathway in monocytes of a CGD patient, 0.5 × 106 PBMC were cultured in 0.5 ml of complete medium in Falcon 2054 tubes with and without the antigen-purified protein derivative of tuberculin (PPD; 25 μg/ml; Statenserum Institut, Copenhagen, Denmark). After 72 h, cultured cells were harvested and labeled with 20 μl of anti-CD14-FITC monoclonal antibody (MAb) Leu-M3 (Becton Dickinson) and analyzed by flow cytometry using a FACSCalibur flow cytometer (Becton Dickinson). PI was added to each sample immediately before analysis.
Detection of Fas expression.
The cell surface expression of CD95 (Fas/Apo-1) antigen was assayed by direct immunofluorescence flow cytometry. After different periods of time, monocytes cultured alone and monocytes cultured in the presence of bacteria were resuspended in ice-cold PBS at a concentration of 106/ml. PE-conjugated anti-CD95 MAb DX2 (20 μl; Pharmingen/Becton Dickinson, San Diego, Calif.) was added to cell suspension aliquots (50 μl), and the cells were incubated for 30 min at 4°C. After a single PBS wash, cells were resuspended in 0.3 ml of PBS containing 0.1% sodium azide and kept at 4°C until flow cytometry analysis. In parallel, staining with irrelevant murine PE-labeled immunoglobulin G1 (Pharmingen) was used as a negative control. In some experiments, to determine the role of Fas-FasL interactions, cells were pretreated (1 h, 4°C) with antagonistic anti-Fas MAb ZB4 (10 μg/ml; Coulter/Immunotech, Westbrook, Maine), followed by flow cytometry analysis as described above, to determine the effectiveness of blocking.
Detection of FasL expression.
As suggested by others (44), the cell surface expression of FasL was verified by flow cytometric analysis using two MAbs, NOK-1 (Pharmingen) and H11 (Alexis Corporation, Laufelfingen, Switzerland). Aliquots (50 μl; 0.5 × 106) of freshly isolated cells or cells cultured for a different period of time were incubated at 4°C for 30 min with biotin-conjugated anti-FasL MAb (NOK-1 or H11). After a wash with ice-cold PBS containing 0.1% sodium azide, cells were incubated at 4°C for 30 min with PE-conjugated streptavidin (1 μg/ml; Pharmingen). Finally, after a single PBS wash, cells were resuspended in 0.3 ml of PBS containing 0.1% sodium azide and kept on ice until analyzed by flow cytometry.
Detection of sFasL.
Aliquots of the control monocytes (5.0 × 106/ml), monocytes which phagocytosed opsonized bacteria (monocyte-to-bacterium ratio of 1:20), or opsonized zymosan particles (0.5 mg/ml; Sigma) were cultured in RPMI 1640 for 1 or 6 h. Thereafter, cells were pelleted by centrifugation (280 × g, 10 min), and the supernatants were collected. To exclude the possibility of contamination by zymosan particles or free bacteria, the supernatants were centrifuged at 2,700 × g for 10 min and concentrated ninefold in Centricon-10 centrifugal concentrators (Amicon, Witten, Germany) (5,000 × g, 60 min). The amount of soluble FasL (sFasL) was then determined by sFasL-specific enzyme-linked immunosorbent assay (ELISA) (Medical and Biological Laboratories, Nagoya, Japan) according to the manufacturer's instructions.
Measurement of biological activity of sFasL.
In some experiments, concentrated samples of conditioned medium were added to cultures of fresh monocytes (106/ml in RPMI 1640, ratio of 1:1 [vol/vol]), and after an additional 3 h of culture, apoptosis of monocytes (binding of annexin V) was checked by flow cytometry.
Caspase-3 activity.
Caspase-3 activity was measured by flow cytometry using a caspase-3 fluorogenic substrate kit (PhiPhiLux-G1D2, green fluorescence; Alexis) according to the manufacturer's instructions. Briefly, after 2 to 4 h of incubation with or without bacteria, cells (0.5 × 106 to 1.0 × 106) were centrifuged, and the cell pellets were suspended in 50 μl of 10 μM substrate solution supplemented with 10% fetal calf serum. After incubation at 37°C for 60 min, cells were washed once in ice-cold PBS and resuspended in 500 μl of PBS. In some experiments, caspase-3 activity was blocked by pretreatment of cells (2 h, 37°C) with the specific caspase-3 inhibitor Ac-DEVD-CHO (acetyl-Asp-Glu-Val-Asp-CHO; 300 μM; Pharmingen).
Measurement of GSH content.
The GSH content in monocytes was estimated using monochlorobimane (mCLB; Molecular Probes, Leiden, The Netherlands), which is nonfluorescent and passively diffuses across the plasma membrane into the cytoplasm, where it forms blue fluorescent adducts with intracellular glutathione and thiol-containing proteins (34). Monocytes were stained with 40 μM mCLB (17) for 10 min at 37°C followed by flow cytometry analysis (FACS Vantage, Becton Dickinson). UV light (351 nm) from an Innova Enterprise II laser (Coherent, Santa Clara, Calif.) was used for the excitation of mCLB. Emission light was collected through a 460-nm optical filter (FL5). To determine nonspecific binding, a duplicate sample was depleted of GSH by treatment with 100 μM N-ethylmaleimide (Sigma).
Flow cytometric analysis of ROI production.
The intracellular production of ROI was measured using two oxidation-sensitive fluorescent probes, dihydrorhodamine 123 (DHR 123) and hydroethidine (HE) (both purchased from Sigma), as described elsewhere (36, 37). Briefly, cells exposed to bacteria or other stimuli for the indicated time periods were incubated at 37°C for 15 min in PBS containing 40 μM DHR 123 or 10 μM HE and analyzed by flow cytometry.
Statistics.
Alterations in cells survival or binding of annexin V were compared by Student's t test. Changes were considered significant at P < 0.05. Results are presented as means ± standard deviations (SD).
RESULTS
Augmented intracellular GSH level inhibits monocyte apoptosis triggered by phagocytosis of S. aureus.
It is well known that phagocytosis and the intracellular killing of bacteria by monocytes result in the production of ROIs. The oxidative stress and subsequent decrease in cellular antioxidant levels have been proposed to trigger cell apoptosis (5). To determine the role of intracellular levels of antioxidants in monocyte apoptosis induced by phagocytosis of S. aureus, freshly isolated monocytes were preincubated for 2 h with GSH or NAC (a precursor of GSH) and then incubated with FITC-labeled S. aureus. At indicated time intervals, cells were harvested and their viability was determined by PI staining and binding of annexin V. In addition, the intracellular GSH level was measured using mCLB. As demonstrated in Fig. 1, preincubation with GSH or NAC partially protects monocytes from apoptosis induced by phagocytosis of S. aureus but has no effect on the rate of phagocytosis of bacteria. This effect was dependent on the concentration of thiols used for preincubation and on the bacterium-to-monocyte ratio (Fig. 2). In addition, the better survival of infected monocytes correlated with the higher intracellular content of GSH (Fig. 3). Thus, we concluded that S. aureus-induced apoptosis is closely related to the intracellular level of antioxidants.
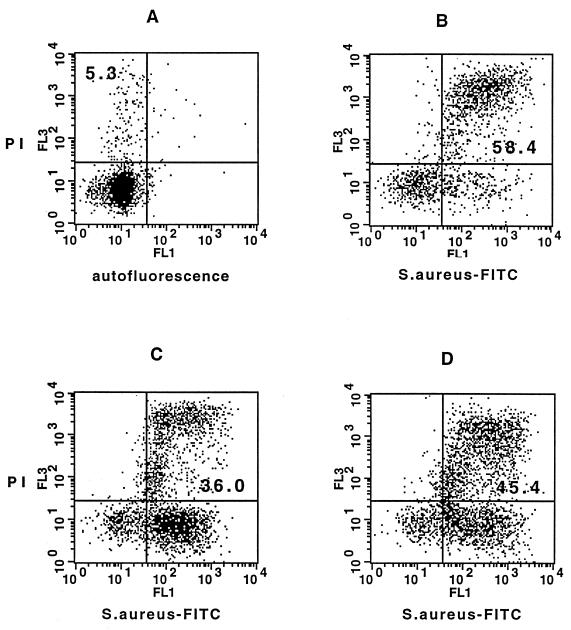
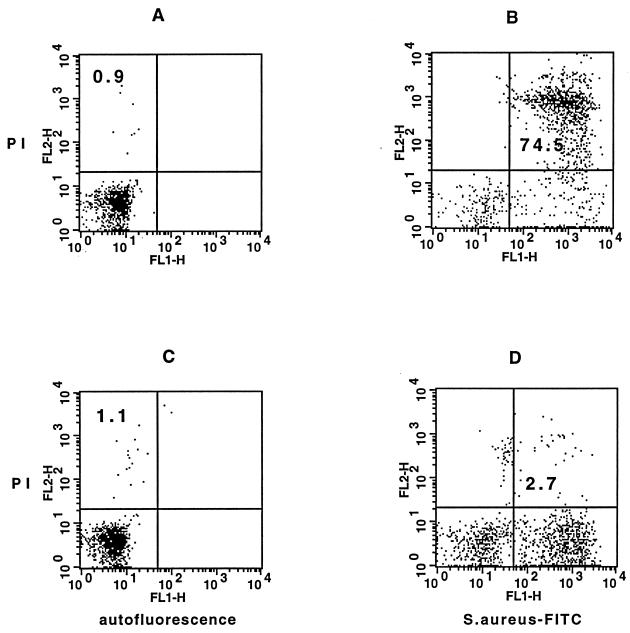
FIG. 1.
Effects of the exogenous antioxidants NAC and GSH on the viability of monocytes after phagocytosis of S. aureus. The cells were cultured in vitro for 6 h with or without bacteria prior to PI staining. Percentages of PI positive cells are shown for control monocytes (A), monocytes exposed to FITC-labeled S. aureus (monocyte-to-bacterium ratio of 1:20) (B), and cells preincubated for 2 h with NAC (25 mM) (C) or GSH (25 mM) (D) and then exposed to FITC-labeled S. aureus. The results of a typical experiment out of five performed are presented. (The mean values ± SD of all experiments performed were 64.5% ± 9.3% PI positive in untreated cells exposed to S. aureus versus 29.8% ± 11.4% or 38.2% ± 15.6% in monocytes exposed to S. aureus after preincubation with NAC [P < 0.001] or GSH [P < 0.01].)
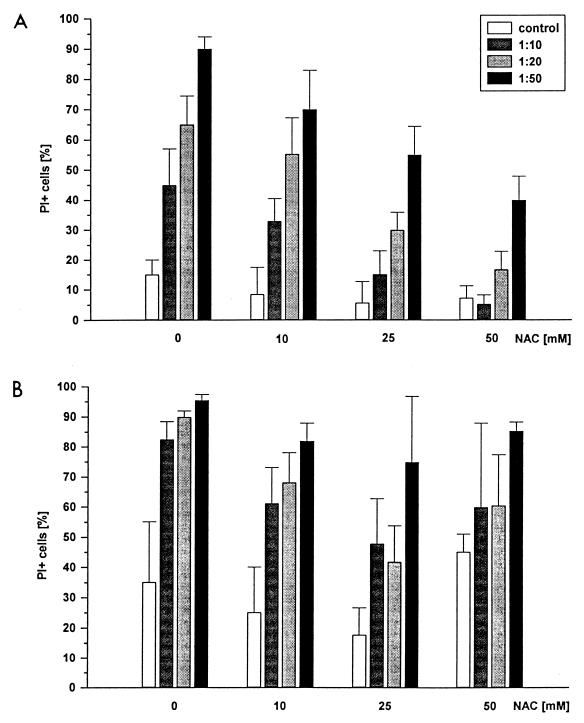
FIG. 2.
Dose-dependent effect of exogenous NAC on the viability of monocytes after phagocytosis of S. aureus. Monocytes were preincubated for 2 h with an increasing concentrations of NAC and cultured in vitro for 6 (A) or 18 (B) h with S. aureus at monocyte-to-bacterium ratios of 1:10, 1:20, and 1:50. Control monocytes were cultured in parallel. Percentages of PI-positive (dead) cells (mean ± SD from three independent experiments) are shown.
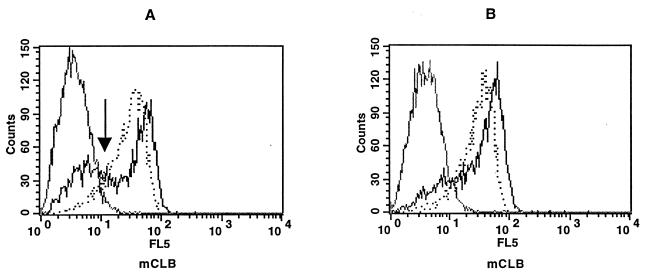
FIG. 3.
Effect of exogenous NAC on monocyte intracellular GSH content after phagocytosis of S. aureus. Monocytes were cultured for 2 h alone (A) or in the presence of NAC (25 mM) (B), exposed to S. aureus (monocyte-to-bacterium ratio of 1:20), and cultured for a further 4 h. Intensities of mCLB fluorescence (x axis) corresponding to monocyte intracellular levels of GSH in control monocytes (black solid lines) and in monocytes after phagocytosis of S. aureus (dotted lines) are shown. A replicate sample was depleted of GSH by treatment with N-ethylmaleimide to give a relative measure of nonspecific binding (grey solid lines). Note the reduced (histogram shift to the left in panel A, indicated by the arrow) level of GSH in phagocytic cells. Results from one of three experiments performed are shown.
Thiol antioxidants effectively reduce the level of ROIs in monocytes stimulated with S. aureus or latex particles.
Since antioxidants had a protective effect on monocytes which ingested bacteria, we determined whether they affect the level of ROIs in phagocytic cells. This was measured inside the cell, using flow cytometry and the oxidation-sensitive fluorogenic probes DHR 123 and HE and by monitoring luminol-dependent chemiluminescence. Results of a representative experiment (Fig. 4) show that preincubation of monocytes with thiol antioxidants reduced the amount of free ROIs detected by both methods. Similarly, antioxidants effectively reduced chemiluminescence triggered by phagocytosis of latex particles (data not shown).
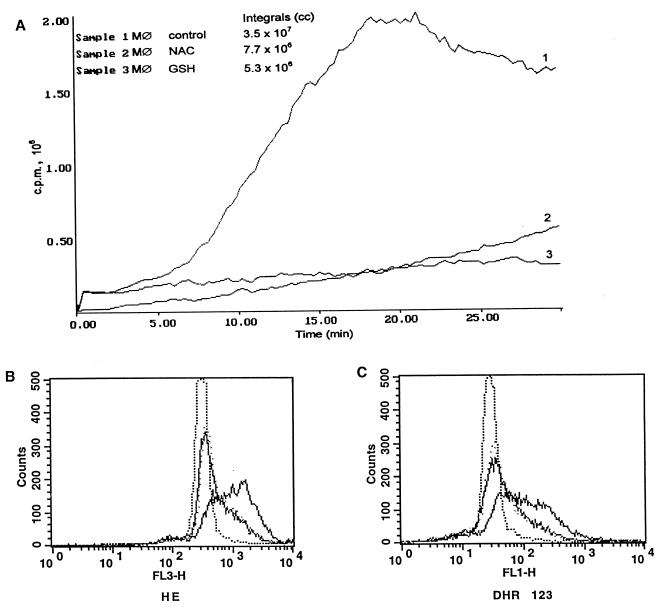
FIG. 4.
Effect of the antioxidants NAC and GSH on monocyte ROI production triggered by phagocytosis of S. aureus (monocyte-to-bacterium ratio of 1:20). ROIs were detected by chemiluminescence and by flow cytometry using the fluorogenic probes HE or DHR 123. Integrals of total ROI produced by 105 monocytes (Mø) during 30-min chemiluminescence measurement (A) and histograms of red (HE; B) and green (DHR 123; C) fluorescence intensity corresponding to O2− and H2O2 production, respectively, are shown. Dotted lines, control monocytes; solid black lines, monocytes stimulated with S. aureus; solid grey lines, monocytes preincubated with 25 mM NAC and stimulated with S. aureus; dotted grey lines, monocytes preincubated with 25 mM GSH and stimulated with S. aureus. Results from one of three experiments performed are shown.
NADPH oxidase deficiency protects monocytes from S. aureus-induced apoptosis.
It has been shown that neutrophils from CGD patients undergo spontaneous as well as Fas/Apo-1-triggered apoptosis, albeit with slower kinetics than cells of healthy individuals (9). Therefore, we examined if monocytes obtained from the CGD patient became apoptotic after phagocytosis of S. aureus. To answer this question, we compared phagocytosis of FITC-labeled S. aureus and the viability of monocytes after phagocytosis of bacteria. Due to the restricted availability of the biological material, in these experiments we used PBMC instead of purified monocytes. In parallel, we examined monocyte apoptosis induced by CD95-FasL interaction to check the intracellular signaling involved in the induction of apoptosis. To simulate the CD95-FasL-dependent pathway, PBMC obtained from the CGD patient were activated with PPD. In such cultures, CD4+ CD45RO+ T cells activated with recall antigens eliminate monocytes via CD95-FasL-induced apoptosis (12, 32, 35). PBMC obtained from the patient (who was known to respond to PPD) and a healthy PPD-responsive donor were cultured for 18 h after exposure to S. aureus or for 72 h in the presence of PPD. Thereafter, cultured cells were labeled with anti-CD14 MAb and their viability was defined by PI exclusion. As shown in Table 1, the viability of monocytes exposed to S. aureus was higher in cells derived from the CGD patient than in control cells from the healthy donor. In contrast, the killing of monocytes by recall antigen-activated T cells was comparable in cultures of cells obtained from the healthy donor and the patient. These data confirm the previous observation that phagocytes from CGD patients are not resistant to Fas-FasL-induced apoptosis (9) and support our observation that the generation of ROIs is essential for apoptosis induced by phagocytosis of S. aureus.
TABLE 1.
Comparison of phagocytic capacity and viability of CD14+ cells from PBMC of a healthy donor and a CGD patient
| Source of cells | Phagocytosis by monocytes (%)a | PI stainability (%)b
|
|||
|---|---|---|---|---|---|
| 18 h
|
72 h
|
||||
| Unstimulated | S. aureus | Unstimulated | PPD | ||
| Healthy donor | 71.3 | 8.3 | 43.3 | 18.0 | 42.7 |
| CGD patient | 73.4 | 8.5 | 18.8 | 34.4 | 52.9 |
PBMC from the healthy donor and CGD patient were incubated with FITC-labeled S. aureus (ratio of 1:10) for 2 h and stained with PE-conjugated anti-CD14 MAb Leu-M3; the level of phagocytosis was determined on the basis of green fluorescence due to phagocytosed bacteria.
Cells were incubated with unlabeled S. aureus (ratio of 1:10) for 18 h or stimulated with recall antigen PPD for 72 h and stained with FITC-conjugated anti-CD14 MAb Leu-M3; viability of CD14+ monocytes was determined by PI staining.
Blocking of NADPH oxidase prevents monocyte apoptosis induced by phagocytosis of S. aureus.
The data obtained from us of the CGD patient's cells prompted us to ask whether the blocking of NADPH oxidase would influence monocyte viability after phagocytosis of bacteria. To answer this question, we compared the survival of control and DPI-treated monocytes after phagocytosis of S. aureus. DPI was shown by others to efficiently block NADPH oxidase (9, 16). As shown in Fig. 5, after phagocytosis of bacteria, which was comparable in DPI-treated and untreated cells, the viability of DPI-treated cells was less compromised than in control monocytes, supporting the results obtained using cells from the CGD patient and indicating a role of ROIs in monocyte apoptosis. Similarly, pretreatment of monocytes with NAC or DPI prevented S. aureus-induced DNA fragmentation of phagocytes (Fig. 6). In contrast, DPI did not prevent killing of monocytes by CD14 MAb and rabbit complement (data not shown).
FIG. 5.
Effect of the NADPH oxidase inhibitor DPI on the viability of monocytes after phagocytosis of S. aureus. Monocytes were cultured in the absence or presence of 10 μM DPI for 1 h, exposed to FITC-labeled S. aureus, and cultured for 6 h. Viability of cells was checked by PI staining. (A and B) Control and S. aureus-exposed monocytes, respectively; (C and D) control and S. aureus-exposed monocytes preincubated with DPI. Percentages of PI-positive cells are shown. Similar results were obtained in three independent experiments and using cells of different donors. (PI-positive cells within control population of monocytes exposed to S. aureus and after preincubation with DPI, 67.1% ± 8.3% versus 3.5% ± 1.1%, P < 0.001.)
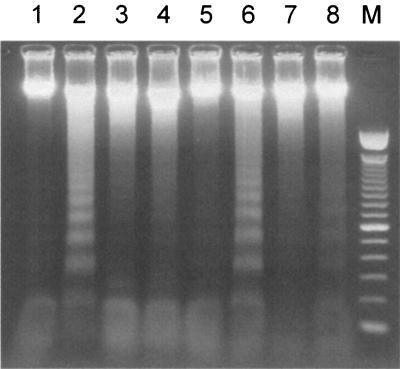
FIG. 6.
DNA fragmentation. Monocytes (2 × 106) were cultured in the presence or absence of NAC (25 mM, 2 h) or DPI (10 μM, 1 h). After 18 h of culture with or without S. aureus (monocyte-to-bacterium ratio of 1:20), DNA was isolated and subjected to electrophoresis. Lanes: 1 and 5, control; 2 and 6, S. aureus; 3, NAC; 4, NAC plus S. aureus; 7, DPI; 8, DPI plus S. aureus; M, DNA marker.
ROIs generated during phagocytosis of bacteria trigger the apoptotic pathway mediated by CD95-CD95L interaction.
The data presented above support the findings that the excessive formation of ROIs may trigger apoptosis (20, 42) and that antioxidant agents or the overexpression of antioxidant enzymes may inhibit the death of various cell types (20, 23, 38). However, it is unclear whether the increased concentration of ROIs is directly involved or sufficient to trigger apoptosis, or whether it represents only a single event which triggers other well-known pathways leading to programmed cell death. In fact, the data presented above (Fig. 2) clearly indicate that treatment with NAC, which protects monocytes from S. aureus-induced cell death, also reduces spontaneous monocyte apoptosis, a phenomenon which is known to result from CD95-CD95L interaction (26). Against this background, we wanted to know whether phagocytosis of S. aureus activates the caspase-3 enzyme family and if it has any impact on CD95 or CD95L expression. Caspase-3 is a crucial downstream enzyme for various pathways triggering cell apoptosis which includes CD95-CD95L interaction. When control monocytes and monocytes exposed to S. aureus were loaded with a caspase-3-specific fluorogenic substrate, a significant increase in enzyme activity was noted in cells which took up bacteria (Fig. 7). Furthermore, both spontaneous apoptosis and apoptosis induced after phagocytosis of bacteria were greatly reduced in monocytes pretreated with the caspase-3 inhibitor Ac-DEVD-CHO (Fig. 8). It is interesting that in contrast to cells incubated with viable bacteria, caspase-3 activity was not significantly increased after the phagocytosis of opsonized heat-killed S. aureus or phagocytosis of latex particles (data not shown).
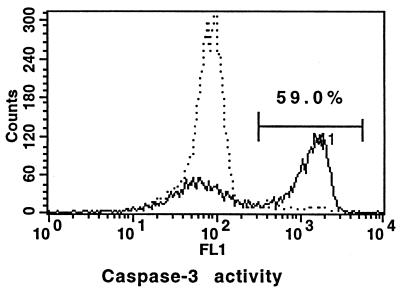
FIG. 7.
Comparison of caspase-3 activities of resting monocytes and monocytes after phagocytosis of S. aureus. The cells were cultured for 2 h with (solid line) or without (dotted line) bacteria, loaded with a caspase-3 fluorogenic substrate, and incubated for another hour. Intensity of green fluorescence (x axis), corresponding to caspase-3 activity, is shown.
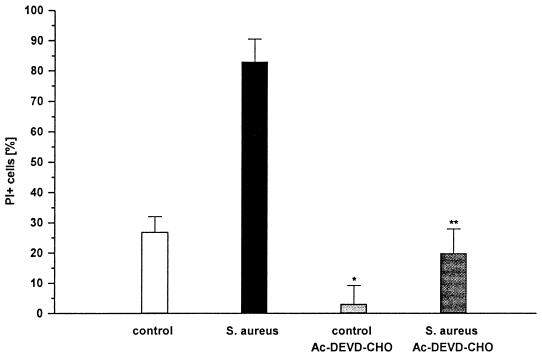
FIG. 8.
Effect of the caspase-3 inhibitor Ac-DEVD-CHO on apoptosis of monocytes triggered by phagocytosis of S. aureus. Monocytes were preincubated in the presence or the absence of 300 μM Ac-DEVD-CHO for 2 h, and then bacteria were added. Cells were further cultured for 18 h, and monocyte death was measured by PI staining. Mean percentages of PI-positive cells ± SD from three independent experiments are shown (∗, P < 0.01; ∗∗, P < 0.001).
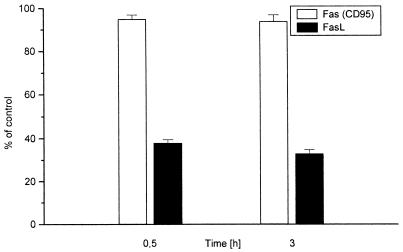
Monocytes constitutively express a high level of CD95 which does not change substantially after phagocytosis of S. aureus (Fig. 9). In contrast, although a fair proportion of freshly isolated monocytes expressed CD95L, the proportion of positive cells was greatly reduced shortly after phagocytosis of bacteria (Fig. 9).
FIG. 9.
Fas and FasL antigen expression on the monocyte surface. Control and S. aureus-exposed (0.5 h of phagocytosis) monocytes were cultured for an additional 3 h. Immediately after phagocytosis and 3 h later, cells were collected and stained with PE-labeled anti-Fas MAb DX2 or by indirect immunofluorescence with the use of biotin-conjugated anti-FasL MAb H11, followed by PE-labeled streptavidin. Data (mean ± SD) from three independent experiments are expressed as a percentage of the control value.
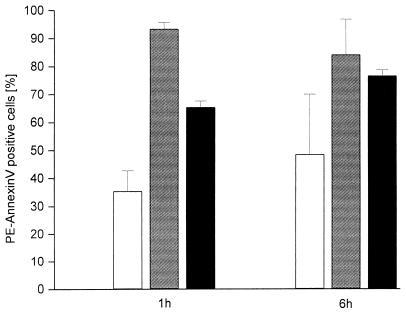
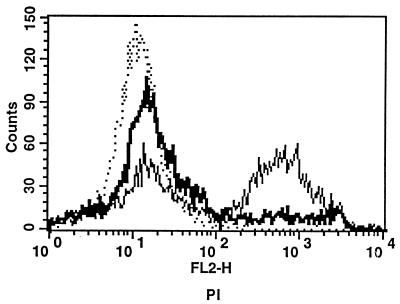
It has been shown recently that phagocytosis of zymosan particles by monocytes results in the shedding of CD95L (4). Therefore, we hypothesized that CD95L is also shed from monocytes following phagocytosis of S. aureus. Therefore, we determined the amount of soluble CD95L in conditioned media from monocytes incubated in the presence or absence of bacteria. As shown in Table 2, the culture supernatants of monocytes exposed to bacteria contained an amount of CD95L exceeding that found in the cultures of monocytes which phagocytosed zymosan particles. Furthermore, the amount of soluble CD95L released to the culture supernatant was lower when heat-killed bacteria were phagocytosed or when cells were treated with DPI to block NADPH oxidase. These data suggested that CD95-CD95L interaction may be in fact responsible for monocyte apoptosis after phagocytosis of bacteria. With this in mind, we examined the ability of conditioned media from monocytes cultured in the presence of S. aureus or zymosan to induce apoptosis of monocytes, as well as the ability of anti-CD95 MAb ZB4 to block apoptosis of monocytes occurring after phagocytosis of bacteria. As shown in Fig. 10, conditioned media were able to induce apoptosis of bystander monocytes. Furthermore, anti-CD95 MAb effectively reduced the proportion of PI-stained cells after phagocytosis of bacteria (Fig. 11). Similarly, pretreatment of cells with anti-CD95 MAb prevented DNA fragmentation in monocytes (data not shown).
TABLE 2.
sFasL in supernatants of monocytes cultured with and without S. aureusa
| Expt | sFasL (pg/ml)
|
||
|---|---|---|---|
| Control | S. aureus | Zymosan | |
| 1 | 102.1 | ND | 259.6 |
| 2 | 0 | 487.0 | 197.0 |
| 3 | 57.3 | 204.2, 117.7b | ND |
| 4 | |||
| −DPI | 0 | 100.0 | ND |
| +DPI | 0 | 0 | ND |
| 5 | |||
| −DPI | 0 | 33.6 | ND |
| +DPI | 0 | 0 | ND |
| 6 | |||
| −DPI | 36.0 | 64.6 | 51.0 |
| +DPI | 0 | 43.1 | 39.2 |
| 7 | |||
| −DPI | 0 | 18.5 | 2.5 |
| +DPI | 0 | 1.4 | ND |
Monocytes (5 × 106/ml) were incubated with either opsonized S. aureus (ratio of 1:20) or zymosan particles (0.5 mg/ml) for 1 h (experiments 6 and 7) or 6 h (experiments 1 to 5). Thereafter, culture supernatants were collected and concentrated, and sFasL was detected by ELISA. ND, not determined.
Heat-killed S. aureus was used.
FIG. 10.
Biological activity of soluble CD95L (FasL) present in conditioned media from monocytes cultured with S. aureus or zymosan. Monocytes were incubated for 3 h in the presence of concentrated conditioned media obtained from primary cultures of untreated monocytes (empty bars) and monocytes exposed to S. aureus (grey bars) or zymosan (black bars), and then proportions of annexin V-positive cells were determined. Primary cultures lasted 1 or 6 h. Bars represent means ± SD of three independent experiments.
FIG. 11.
Effect of anti-Fas blocking MAb on apoptosis of monocytes triggered by phagocytosis of bacteria. Monocytes were preincubated for 2 h with or without anti-Fas blocking MAb ZB4 (10 μg/ml) and cultured for 18 h in the presence of S. aureus. Histogram overlay shows viability determined by PI uptake in untreated cells (dotted line), cells exposed to S. aureus (thin solid line), and anti-Fas-treated cells exposed to bacteria (bold solid line). In all three experiments, anti-Fas blocking MAb protected monocytes from apoptosis triggered by phagocytosis of S. aureus (78.2% ± 4.5% PI-positive cells in cultures exposed to S. aureus versus 19.8% ± 2.8% in cultures of monocytes preincubated with anti-Fas MAb before exposure to bacteria; P < 0.01).
DISCUSSION
The data presented above clearly show that ROIs play an important role in apoptosis in monocytes after phagocytosis of S. aureus. This conclusion is supported by (i) the protective effect of antioxidants (NAC and GSH) on S. aureus-induced apoptosis, (ii) the significant correlation between cell apoptosis and the reduction of the monocyte content of glutathione, and (iii) the inhibition of S. aureus-induced apoptosis in monocytes from the CGD patient and after the blocking of NADPH oxidase. Pretreatment of monocytes with NAC prevented apoptosis after ingestion of S. aureus although, but had no effect on phagocytosis of bacteria. The mechanism of this phenomenon may be related both to altering the redox status of thiol enzymes, such as caspases, and to the direct scavenging of reactive oxygen species, as suggested by the decreased capacity of NAC-treated monocytes to kill ingested S. aureus (J. Baran et al., unpublished data). The direct scavenging of ROIs by NAC was also confirmed by the cytofluorimetric analysis of H2O2 and O2− production using DHR and HE assays, respectively.
Although the above findings indicate the role of ROIs in monocyte apoptosis, the generation of oxygen species by itself cannot explain this phenomenon. A substantial amount of ROIs are generated during phagocytosis of latex particles or opsonized heat-killed bacteria, as determined by chemiluminescence and NBT reduction assay, yet under these conditions apoptosis of monocytes does not occur or is much less pronounced (2). Our data suggest that reactive oxygen species are involved in the modulation of pathways leading to the triggering of apoptosis. It has been shown recently that during phagocytosis of opsonized zymosan, monocytes shed biologically active FasL (4). Similarly, as demonstrated in our studies, phagocytosis of viable bacteria resulted in the rapid shedding of biologically active FasL by monocytes, and the amount of FasL shed by monocytes which phagocytosed bacteria as measured by ELISA was even higher than that triggered by zymosan. No significant change of CD95 expression was noted on monocytes which phagocytosed bacteria; however, it is possible that ROIs contribute to the stable expression of this antigen, since expression of CD95 is reduced in monocytes pretreated with NAC (J. Baran, unpublished observation). Second, it is likely that oxygen species generated in the cell lowered the threshold of antiapoptotic defense by the modulation of caspase activity (9, 14, 47). This may explain the finding that cells which have ingested bacteria preferentially show DNA strand breaks (2) and are stained with PI (this report). Finally, ROIs may contribute to apoptosis by the up-regulation of FasL expression (3, 22) and the modulation of metalloproteinase activity (50). Therefore, we hypothesize that the major mechanism responsible for apoptosis of monocytes after phagocytosis of S. aureus involves CD95-CD95L interactions whereas ROIs positively regulate these interactions. This conclusion was supported by the fact that MAbs which blocked CD95 also protected monocytes from apoptosis although they did not block the production of ROIs triggered following phagocytosis (data not shown). Furthermore, our preliminary data suggest that caspase-8 activity increases in monocytes infected with S. aureus (J. Baran et al., unpublished).
Our data, however, do not identify the factor or factors responsible for the triggering of Fas-FasL interaction in response to phagocytosis of S. aureus. Since in contrast to viable S. aureus, phagocytosis of heat-inactivated bacteria does not trigger monocyte apoptosis (2) or increase caspase-3 activity (this report), bacterial toxins seem to be good candidates. S. aureus produces several toxins, some of which, such as α-hemolysin or leukocidin, are cytotoxic (45, 46). Moreover, supernatants of cultured S. aureus are cytotoxic for monocytes (K. Guzik et al., unpublished observation). However, this mechanism is probably not responsible, as leukocidin genes, although present in the strain used in this study, were not expressed under our culture conditions (A. Sabat, unpublished observation). Finally, in contrast to apoptosis induced by phagocytosis of viable bacteria, cytotoxicity induced by bacterial culture supernatants is not blocked by the pretreatment of monocytes with DPI (J. Baran, unpublished).
ACKNOWLEDGMENTS
This work was supported by the Polish Research Committee (grant 4 PO5A 087 14). J.P. is a recipient of a grant from the Foundation for Polish Science, which also supported purchase of the equipment for monocyte elutriation.
The technical assistance of Ewa Isendorf and Erika Kaltenhäuser is greatly appreciated.
REFERENCES
- 1.Baeuerle P A, Henkel T. Function and activation of NF-κB in the immune system. Annu Rev Immunol. 1994;12:141–179. doi: 10.1146/annurev.iy.12.040194.001041. [DOI] [PubMed] [Google Scholar]
- 2.Baran J, Guzik K, Hryniewicz W, Ernst M, Flad H-D, Pryjma J. Apoptosis of monocytes and prolonged survival of granulocytes as a result of phagocytosis of bacteria. Infect Immun. 1996;64:4242–4248. doi: 10.1128/iai.64.10.4242-4248.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bauer M K A, Vogt M, Los M, Siegel J, Wesselborg S, Schulze-Osthoff K. Role of reactive oxygen intermediates in activation-induced CD95 (APO-1/Fas) ligand expression. J Biol Chem. 1998;273:8048–8055. doi: 10.1074/jbc.273.14.8048. [DOI] [PubMed] [Google Scholar]
- 4.Brown S B, Savill J. Phagocytosis triggers macrophage release of Fas ligand and induces apoptosis of bystander leukocytes. J Immunol. 1999;162:480–485. [PubMed] [Google Scholar]
- 5.Buttke T M, Sandstrom P A. Oxidative stress as a mediator of apoptosis. Immunol Today. 1994;15:7–10. doi: 10.1016/0167-5699(94)90018-3. [DOI] [PubMed] [Google Scholar]
- 6.Cohen J J. Programmed cell death in the immune system. Adv Immunol. 1991;50:55–85. doi: 10.1016/s0065-2776(08)60822-6. [DOI] [PubMed] [Google Scholar]
- 7.Collins M K L, Lopez-Rivas A. The control of apoptosis in mammalian cells. Trends Biochem Sci. 1993;18:307–309. doi: 10.1016/0968-0004(93)90042-l. [DOI] [PubMed] [Google Scholar]
- 8.Collins M K L, Perkins G R, Rodriguez-Tarduchy G, Nieto M A, Lopez-Rivas A. Growth factors as survival factors: regulation of apoptosis. Bioessays. 1994;16:133–138. doi: 10.1002/bies.950160210. [DOI] [PubMed] [Google Scholar]
- 9.Fadeel B, Ahlin A, Henter J-I, Orrenius S, Hampton M B. Involvement of caspases in neutrophil apoptosis: regulation by reactive oxygen species. Blood. 1998;92:4808–4818. [PubMed] [Google Scholar]
- 10.Fratazzi C, Arbeit R D, Carini C, Remold H G. Programmed cell death of Mycobacterium avium serovar 4-infected human macrophages prevents the mycobacteria from spreading and induces mycobacterial growth inhibition by freshly added, uninfected macrophages. J Immunol. 1997;158:4320–4327. [PubMed] [Google Scholar]
- 11.Golstein P, Ojcius D M, Young J D-E. Cell death mechanisms and the immune system. Immunol Rev. 1991;121:29–65. doi: 10.1111/j.1600-065x.1991.tb00822.x. [DOI] [PubMed] [Google Scholar]
- 12.Grage-Griebenow E, Baran J, Loppnow H, Los M, Ernst M, Flad H-D, Pryjma J. An Fcγ receptor I (CD64)-negative subpopulation of human peripheral blood monocytes is resistant to killing by antigen-activated CD4-positive cytotoxic T cells. Eur J Immunol. 1997;27:2358–2365. doi: 10.1002/eji.1830270934. [DOI] [PubMed] [Google Scholar]
- 13.Guzik K, Bzowska M, Dobrucki J, Pryjma J. Heat-shocked monocytes are resistant to Staphylococcus aureus-induced apoptotic DNA fragmentation due to expression of HSP72. Infect Immun. 1999;67:4216–4222. doi: 10.1128/iai.67.8.4216-4222.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hampton M B, Fadeel B, Orrenius S. Redox regulation of the caspases during apoptosis. Ann N Y Acad Sci. 1998;854:328–335. doi: 10.1111/j.1749-6632.1998.tb09913.x. [DOI] [PubMed] [Google Scholar]
- 15.Hampton M B, Orrenius S. Dual regulation of caspase activity by hydrogen peroxide: implications for apoptosis. FEBS Lett. 1997;414:552–556. doi: 10.1016/s0014-5793(97)01068-5. [DOI] [PubMed] [Google Scholar]
- 16.Hancock J T, Jones T G. The inhibition by diphenylene iodonium and its analogues of superoxide generation by macrophages. Biochem J. 1987;242:103–107. doi: 10.1042/bj2420103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hedley D W, Chow S. Evaluation of methods for measuring cellular glutathione content using flow cytometry. Cytometry. 1994;15:349–358. doi: 10.1002/cyto.990150411. [DOI] [PubMed] [Google Scholar]
- 18.Hirose K, Longo D L, Oppenheim J J, Matsushima K. Overexpression of mitochondrial manganese superoxide dismutase promotes the survival of tumor cells exposed to interleukin-1, tumor necrosis factor, selected anticancer drugs and ionizing radiation. FASEB J. 1993;7:361–368. doi: 10.1096/fasebj.7.2.8440412. [DOI] [PubMed] [Google Scholar]
- 19.Hockenbery D. Defining apoptosis. Am J Pathol. 1995;146:16–19. [PMC free article] [PubMed] [Google Scholar]
- 20.Hockenbery D M, Oltwai Z N, Yin X M, Milliman C L, Korsmeyer S L. Bcl-2 functions in an antioxidant pathway to prevent apoptosis. Cell. 1993;75:241–251. doi: 10.1016/0092-8674(93)80066-n. [DOI] [PubMed] [Google Scholar]
- 21.Hug H, Enari M, Nagata S. No requirement of reactive oxygen intermediates in Fas-mediated apoptosis. FEBS Lett. 1994;351:311–313. doi: 10.1016/0014-5793(94)00852-3. [DOI] [PubMed] [Google Scholar]
- 22.Hug H, Strand S, Grambihler A, Galle J, Hack V, Stremmel W, Krammer P H, Galle P R. Reactive oxygen intermediates are involved in the induction of CD95 ligand mRNA expression by cytostatic drugs in hepatoma cells. J Biol Chem. 1997;272:28191–28193. doi: 10.1074/jbc.272.45.28191. [DOI] [PubMed] [Google Scholar]
- 23.Kane D J, Sarafian T A, Anton R, Hahn H, Gralla E B, Valentine J S, Ord T, Bredesen D E. Bcl-2 inhibition of neuronal cell death: decreased generation of reactive oxygen species. Science. 1993;262:1274–1277. doi: 10.1126/science.8235659. [DOI] [PubMed] [Google Scholar]
- 24.Keane J, Balcewicz-Sablinska M K, Remold H G, Chupp J, Meek B, Fenton M, Kornfeld H. Infection by Mycobacterium tuberculosis promotes human alveolar macrophage apoptosis. Infect Immun. 1997;65:298–304. doi: 10.1128/iai.65.1.298-304.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khelef N, Zychlinsky A, Guiso N. Bordetella pertussis induces apoptosis in macrophages: role of adenylate cyclase-hemolysin. Infect Immun. 1993;61:4064–4071. doi: 10.1128/iai.61.10.4064-4071.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kiener P A, Davis P M, Starling G C, Mehlin C, Klebanoff S J, Ledbetter J A, Liles W C. Differential induction of apoptosis by Fas-Fas ligand interactions in human monocytes and macrophages. J Exp Med. 1997;185:1511–1516. doi: 10.1084/jem.185.8.1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mangan D, Wahl S M. Differential regulation of human monocyte programmed cell death (apoptosis) by chemotactic factors and pro-inflammatory cytokines. J Immunol. 1991;147:3408–3412. [PubMed] [Google Scholar]
- 28.Manna S K, Aggarwal B B. Lipopolysaccharide inhibits TNF-induced apoptosis: role of nuclear factor κB activation and reactive oxygen intermediates. J Immunol. 1999;162:1510–1518. [PubMed] [Google Scholar]
- 29.Muschel R J, Bernhard E J, Garza L, McKenna W G, Koch C J. Induction of apoptosis at different oxygen tensions: evidence that oxygen radicals do not mediate apoptotic signalling. Cancer Res. 1995;55:995–998. [PubMed] [Google Scholar]
- 30.Packham G, Ashmun R A, Cleveland J L. Cytokine suppress apoptosis independent of increases in reactive oxygen levels. J Immunol. 1996;156:2792–2800. [PubMed] [Google Scholar]
- 31.Packham G, Cleveland J L. c-Myc and apoptosis. Biochim Biophys Acta. 1995;1242:11–28. doi: 10.1016/0304-419x(94)00015-t. [DOI] [PubMed] [Google Scholar]
- 32.Pryjma J, Zembala M, Baran J, Ernst M, Flad H-D. Elimination of monocytes from cultures activated with recall antigens. Immunol Lett. 1995;46:229–235. doi: 10.1016/0165-2478(95)00051-6. [DOI] [PubMed] [Google Scholar]
- 33.Rensing-Ehl A, Hess S, Ziegler-Heitbrock H W, Riethmuller G, Engelmann H. Fas/APO-1 activates nuclear factor kappa B and enhances interleukin-6 production. J Inflamm. 1995;45:161–174. [PubMed] [Google Scholar]
- 34.Rice G C, Bump E A, Shrieve D C, Lee W, Kovacs M. Quantitative analysis of cellular glutathione by flow cytometry utilizing monochlorobimane: some applications to radiation and drug resistance in vitro and in vivo. Cancer Res. 1986;46:6105–6110. [PubMed] [Google Scholar]
- 35.Richardson B C, Buckmaster T, Keren D F, Johnson K J. Evidence that macrophages are programmed to die after activating autologous, cloned, antigen-specific, CD4+ T cells. Eur J Immunol. 1993;23:1450–1455. doi: 10.1002/eji.1830230708. [DOI] [PubMed] [Google Scholar]
- 36.Rothe G, Valet G. Flow cytometry analysis of respiratory burst activity in phagocytes with hydroethidine and 2′,7,-dichlorofluorescein. J Leukoc Biol. 1990;47:440–448. [PubMed] [Google Scholar]
- 37.Royall J A, Ischiropoulos H. Evaluation of 2′,7-dichlorofluorescein and dihydrorhodamine 123 as fluorescent probes for intracellular H2O2 in cultured endothelial cells. Arch Biochem Biophys. 1993;302:348–355. doi: 10.1006/abbi.1993.1222. [DOI] [PubMed] [Google Scholar]
- 38.Sandstrom P A, Mannie M D, Buttke T M. Inhibition of activation-induced death in T cell hybridomas by thiol antioxidants: oxidative stress as a mediator of apoptosis. J Leukoc Biol. 1994;55:221–226. doi: 10.1002/jlb.55.2.221. [DOI] [PubMed] [Google Scholar]
- 39.Scheuerer B, Ernst M, Durrbaum-Landmann I, Fleischer J, Grage-Griebenow E, Brandt E, Flad H-D, Petersen F. The CXC-chemokine platelet factor 4 promotes monocyte survival and induces monocyte differentiation into macrophages. Blood. 2000;95:1158–1166. [PubMed] [Google Scholar]
- 40.Schulze-Osthoff K, Krammer P H, Droge W. Divergent signalling via APO-1/Fas and the TNF receptor, two homologous molecules involved in physiological cell death. EMBO J. 1994;13:4587–4596. doi: 10.1002/j.1460-2075.1994.tb06780.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schulze-Osthoff K, Los M, Baeuerle P A. Redox signalling by transcription factors NF-kappa B and AP-1 in lymphocytes. Biochem Pharmacol. 1995;50:735–741. doi: 10.1016/0006-2952(95)02011-z. [DOI] [PubMed] [Google Scholar]
- 42.Schulze-Osthoff K, Walczak H, Droge W, Krammer P H. Cell nucleus and DNA fragmentation are not required for apoptosis. J Cell Biol. 1994;127:15–20. doi: 10.1083/jcb.127.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schwartz L M, Osborne B A. Programmed cell death, apoptosis and killer genes. Immunol Today. 1993;14:582–590. doi: 10.1016/0167-5699(93)90197-S. [DOI] [PubMed] [Google Scholar]
- 44.Smith D, Sieg S, Kaplan D. Technical note: aberrant detection of cell surface Fas Ligand with anti-peptide antibodies. J Immunol. 1998;160:4159–4160. [PubMed] [Google Scholar]
- 45.Thelestam M. Modes of membrane demaging action of staphylococcal toxins. In: Easmon C S F, Adlam C, editors. Staphylococci and staphylococcal infections. New York, N.Y: Academic Press; 1983. pp. 705–744. [Google Scholar]
- 46.Tomita T, Kamio Y. Molecular biology of the pore-forming cytolysins from Staphylococcus aureus alpha- and gamma-hemolysins and leukocidin. Biosci Biotechnol Biochem. 1997;61:565–572. doi: 10.1271/bbb.61.565. [DOI] [PubMed] [Google Scholar]
- 47.Ueda S, Nakamura H, Masutani H, Sasada T, Yonehara S, Takabayashi A, Yamaoka Y, Yodoi J. Redox regulation of caspase-3(-like) protease activity: regulatory roles of thioredoxin and cytochrome c. J Immunol. 1998;161:6689–6695. [PubMed] [Google Scholar]
- 48.Um H-D, Orenstein J M, Wahl S M. Fas mediates apoptosis in human monocytes by a reactive oxygen intermediate dependent pathway. J Immunol. 1996;156:3469–3477. [PubMed] [Google Scholar]
- 49.Watson R W G, Redmond H P, Wang J H, Condron C, Bouchier-Hayes D. Neutrophils undergo apoptosis following ingestion of Escherichia coli. J Immunol. 1996;156:3986–3992. [PubMed] [Google Scholar]
- 50.Weiss S J, Peppin G, Oritz X, Ragsdalé C, Test S T. Oxidative autoactivation of latent collagenase by human neutrophils. Science. 1986;227:747–749. doi: 10.1126/science.2982211. [DOI] [PubMed] [Google Scholar]
- 51.Wyllie A H, Kerr J F R, Currie A R. Cell death: the significance of apoptosis. Int Rev Cytol. 1980;68:251–306. doi: 10.1016/s0074-7696(08)62312-8. [DOI] [PubMed] [Google Scholar]
- 52.Yamauchi N, Kuriyama M, Watanabe N, Neda H, Maeda M, Niitsu Y. Intracellular hydroxyl radical production induced by recombinant human tumor necrosis factor and its implication in the killing of tumor cells in vitro. Cancer Res. 1989;49:1671–1675. [PubMed] [Google Scholar]
- 53.Zychlinsky A, Prevost M C, Sansonetti P. Shigella flexneri induces apoptosis in infected macrophages. Nature. 1992;358:167–169. doi: 10.1038/358167a0. [DOI] [PubMed] [Google Scholar]