Purpose of review
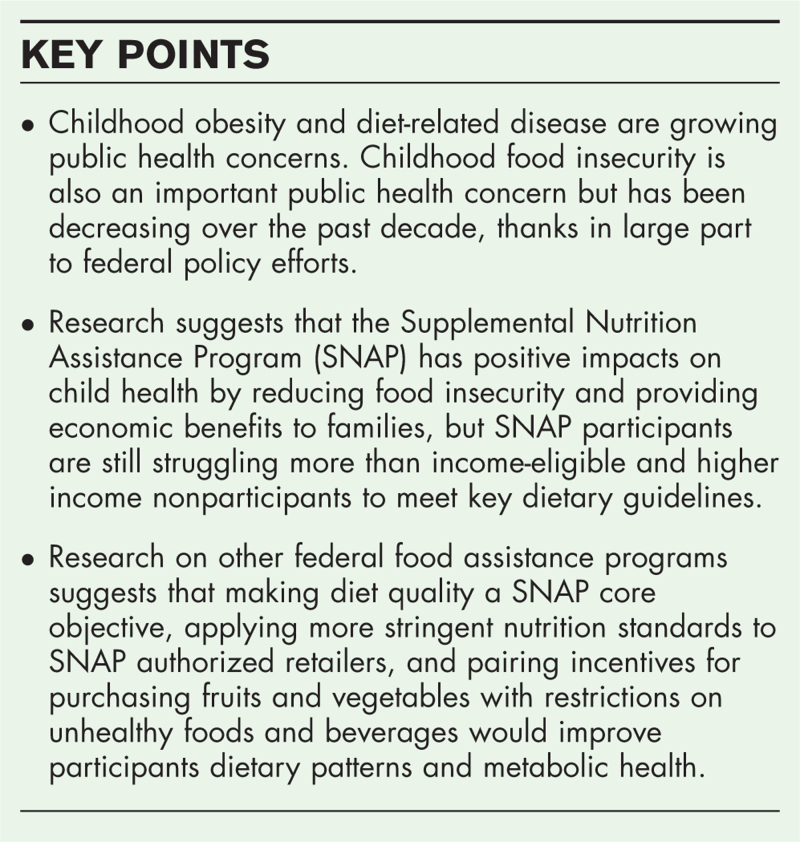
In 2020, obesity prevalence among US children reached 19.7%, impacting about 14.7 million children and adolescents. Food insecurity among children is also a public health concern but has largely decreased or remained stable over the past decade, reaching 6.2% of US households with children in 2021. Given food insecurity and obesity's interconnected nature and their negative consequences on children's health, it is of interest to assess the Supplemental Nutrition Assistance Program's (SNAP's) impact on childhood food security, dietary quality, disease risk, and health outcomes.
Recent findings
Evidence suggests that SNAP participants, including children, struggle to meet key dietary guidelines and perform poorly on key health indicators when compared with income-eligible and higher income nonparticipants. Children participating in SNAP were more likely to have elevated disease risk and consume more sugar-sweetened beverages (SSBs), more high-fat dairy, and more processed meats than income-eligible nonparticipants. However, research suggests that federal food assistance programs with more stringent nutrition standards – the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) and the National School Lunch Program (NSLP) and School Breakfast Program (SBP) – improve dietary quality, increase birth weight and gestation periods, and reduce childhood obesity, infant mortality and healthcare costs.
Summary
After reviewing the evidence on SNAP's impacts on food insecurity, dietary quality, and health as well as research on the health impacts of other more successful federal food assistance programs, we provide three policy recommendations to strengthen SNAP's effectiveness as a health intervention for children and families.
Keywords: diet quality, food insecurity, health intervention, nutrition assistance, Supplemental Nutrition Assistance Program
INTRODUCTION
Obesity and diet-related disease are a growing public health crisis for both adults and children, with significant disparities by race and ethnicity. Childhood food insecurity is also a public health concern and is closely tied to diet-related disease and overall child health. The Supplemental Nutrition Assistance Program (SNAP) is the largest federal food assistance program and is of interest for its potential to further alleviate food insecurity among children while also improving health outcomes.
Box 1.
no caption available
BURDEN OF OBESITY, DIET-RELATED DISEASE, AND FOOD INSECURITY
From 2017 to 2020, for children aged 2 to 19 years, the prevalence of obesity in the United States was 19.7% and impacted about 14.7 million children and adolescents [1▪]. Obesity prevalence was 26.2% among Hispanic children, 24.8% among non-Hispanic black children, 16.6% among non-Hispanic white children, and 9% among non-Hispanic Asian children [2]. Obesity increases a child's risk for adverse diet-related health conditions, including type 2 diabetes, cardiovascular disease, and certain cancers [3]. Among adults, from 2017 to 2020, obesity prevalence was 41.9%, a record high [3]. Obesity prevalence was 49.9% among non-Hispanic black adults, 45.6% among Hispanic adults, 41.4% among non-Hispanic white adults and 16.1% among non-Hispanic Asian adults [3]. In 2017–2018, 93.2% of adults had less-than-optimal metabolic health [4▪]. Diet-related chronic diseases are among the leading causes of death in the United States, and research during the coronavirus 19 (COVID-19) pandemic showed that diet-related chronic diseases were associated with higher risk of COVID-19 infection and two-thirds of COVID-19 hospitalizations [2,5▪].
Food insecurity and very-low food insecurity among households with children decreased from 2020 to 2021. Food insecure households, as defined by USDA, are those that had difficulty at some time during the year providing enough food for all members because of a lack of resources [6]. Very-low food insecurity is a more severe range of food insecurity, wherein the food intake of some household members was reduced, and normal eating patterns was disrupted at times during the year because of limited resources [6]. In 2021, 6.2% of households with children were food-insecure (compared with 7.5% in 2020) and 0.7% had very low food security (compared with 0.8% in 2020) [7▪,8▪]. Food insecurity is associated with a host of short-term and long-term health consequences for children, including infant mortality, fetal epigenetic changes, suboptimal development and function, increased hospitalizations and healthcare use, disrupted or under use of prescribed medications, poorer management of chronic diseases and poor diet quality [9–19].
SUPPLEMENTAL NUTRITION ASSISTANCE PROGRAM BACKGROUND
SNAP is a federal program with the potential to impact childhood food insecurity, obesity, and diet-related disease simultaneously. SNAP provides food-purchasing assistance to low-income Americans. SNAP is the largest federal food assistance program, serving 41.5 million people in fiscal year (FY) 2022 at an expenditure of $140 billion [20]. The most recent data on SNAP household characteristics found that in FY 2019, 41% of participating SNAP households included children [21]. The United States Department of Agriculture (USDA) pays the full cost of SNAP benefits and shares half of the administration costs with states, which operate SNAP. To be eligible to receive SNAP benefits, an individual or household must have a gross income of less than 130% of the federal poverty standard, net income less than 100% of the federal poverty standard, and assets must fall below certain limits [22]. Households deemed eligible for SNAP benefits receive an electronic benefit card (EBT), which is loaded with benefits monthly. Households may use EBT cards at an authorized retailer, of which there are more than 247 000 [23]. SNAP participants may use EBT benefits to purchase food and allowable beverages but may not be used to purchase alcoholic beverages, tobacco, paper goods, and other nonfood items [24]. Heated and hot prepared foods are not considered staple foods and are also not eligible for purchase, except in some areas under certain circumstances [25]. On average, SNAP participants received an estimated $217.88 per month per person in regular SNAP benefits in FY 2021 [26]. Each household's monthly benefit amount is based on the household's net income, so that if a household's net income after deductions is zero, the household receives the maximum SNAP benefit, and the benefit reduction rate is 30% (meaning the monthly benefit is reduced by 30 cents for each dollar of net income) [27]. During the COVID-19 pandemic, Congress provided all SNAP recipients the maximum benefit. The maximum SNAP benefit is tied to the cost of the USDA's Thrifty Food Plan (TFP), a diet plan intended to provide adequate nutrition consistent with the Dietary Guidelines for Americans, and which was updated in 2021 as directed by Congress, increasing SNAP benefits by 21% [28,29].
SUPPLEMENTAL NUTRITION ASSISTANCE PROGRAM'S IMPACT ON CHILD HEALTH
Research suggests that SNAP has positive impacts on health by reducing food insecurity and lifting individuals out of poverty. Research has shown that SNAP meets its goal of reducing hunger and food insecurity among participants, including children [30,31▪▪]. Participation in SNAP has been shown to reduce the incidence of low-birth weight among newborns by 7% for whites and 5–11% for blacks [32]. Research on the relationship between SNAP purchasing power and children's health and health care utilization found that a 10% increase in SNAP purchasing power increases the likelihood a child had a preventive check-in in the past year by 8.1%, increases the likelihood that children had any doctor's visit in the past 12 months by 3.4%, and is associated with a 22% reduction in the number of school days missed because of illness [33]. Research has shown that children receiving SNAP are less likely than low-income nonparticipants to be in fair or poor health or underweight, and their families are less likely to make tradeoffs between paying for health care and paying for other basic health needs, like food, housing, heating, and electricity [34,35]. Reductions and cut offs in SNAP benefits because of increased income have also been associated with poorer child health [36].
SUPPLEMENTAL NUTRITION ASSISTANCE AND DIET QUALITY
Although SNAP effectively alleviates food insecurity for children in terms of caloric, macronutrient, and micronutrient intake, SNAP participants are still struggling more than income-eligible and higher income nonparticipants to meet key dietary guidelines.
The average USDA Healthy Eating Index (HEI) score among Americans is 58 (out of a possible 100), suggesting that the majority of Americans have suboptimal diets [37]. However, while other USDA food assistance programs, such as the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) and the National School Lunch Program (NSLP) and School Breakfast Program (SBP), significantly improve diet quality, research suggests that SNAP does not.
The National Health and Nutrition Examination Survey (NHANES) has frequently been used to assess Americans’ dietary quality and health, including by income and SNAP participation status. A study using 2011–2016 NHANES data found that, on average, SNAP participants had lower total HEI scores than income-eligible and higher income nonparticipants (55, 57, and 60 points, respectively) [38▪▪]. SNAP participants scored lower for total fruits, whole fruits, total vegetables, and added sugar components [38▪▪]. Adults participating in SNAP had a higher prevalence of obesity than matched income-eligible nonparticipants (44 versus 38%) [38▪▪]. Children participating in SNAP had a higher prevalence of elevated blood pressure compared with higher income nonparticipant children (9 versus 7%) [38▪▪]. In terms of disease risk, a higher percentage of SNAP participants than either income-eligible or higher income nonparticipants had very high or extremely high-disease risk (31 versus 27%, and 26 and 11% versus 8 and 7%, respectively) [38▪▪].
A study of 1999–2008 NHANES data found that children who received SNAP benefits had substandard diets, consuming 43% more SSBs, 47% more high-fat dairy, and 44% more processed meats than income-eligible nonparticipants [39].
A study of 1999–2014 NHANES data found that between 2003 and 2014, SNAP participants had less improvements in diet quality using American Heart Association (AHA) diet scores than both income-eligible nonparticipants and higher income individuals [40]. Disparities in diet quality persisted for most foods and nutrients and worsened for processed meats, added sugars and nuts and seeds [40].
In addition to NHANES, sales data have also been used to assess foods purchased using SNAP benefits. Sales data obtained from a large supermarket chain in the northeastern United States from April 2012 to April 2014 revealed that customer transactions paid at least partially with SNAP benefits included lower spending on fruits, vegetables, and poultry, and higher spending on SSBs, red meat, and convenience foods than transactions that did not involve SNAP [41]. A USDA study assessed the content of SNAP purchases in 2011 from a leading retailer and found that soft drinks were the number 1 purchase in terms of share of expenditures by SNAP households and the number 2 purchase by non-SNAP households [42].
LESSONS LEARNED FROM OTHER FEDERAL FEEDING PROGRAMS
In contrast to SNAP, other USDA feeding programs targeting children perform better with respect to diet quality. The NSLP, SBP, the Child and Adult Care Food Program, and the WIC Program all apply nutrition standards based on the Dietary Guidelines for Americans.
The Healthy Hunger-Free Kids Act (HHFKA) in 2010 established stronger nutrition standards for the NSLP and SBP, which significantly improved dietary quality. Specifically, the HHFKA regulations required schools to increase the amount of fruits and vegetables served and limit starchy vegetables; serve only low-fat or fat-free milk; and serve more whole grains [43]. The HHFKA also established standards for food and beverage products sold in schools outside of the breakfast and lunch programs, which eliminated most sugary beverages and reduced the sugar and calorie content of food products for sale [44]. Following the changes, the USDA found that the nutritional quality of NSLP lunches increased significantly between school year 2009–2010 and school year 2014–2015 [45▪▪]. Evaluations found that students consumed more fruit, vegetables, whole grains, and fewer starch vegetables than before the HHFKA, without contributing to increases in food waste or reductions in program participation [45▪▪,46]. The mean total HEI-2010 score for NSLP lunches increased 41% – from 57.9 to 81.5 out of a possible 100 [45▪▪].
Unlike SNAP, which does not limit food or nonalcoholic beverage purchases, WIC purchases are limited to different food packages for different groups of participants. Research has shown that WIC lowers Medicaid costs for participating women, and WIC participation is associated with longer gestation periods, higher birth weight, and lower infant mortality [47,48]. The WIC food packages were revised in 2009 to align with the Dietary Guidelines for Americans more closely and to introduce incentives for the purchase of fruits and vegetables, which research showed was associated with a 17.5 and 27.8% increase in fresh and frozen vegetable purchases (respectively) and a 28.6% increase in fresh fruit purchases [49]. The Centers for Disease Control and Prevention (CDC) and the USDA analyzed WIC data from 56 states and territories from 2010 and 2018 and found that 31 WIC agencies reported significant declines in obesity among children aged 2–4 years [50]. Between 2010 and 2018, overall obesity prevalence among WIC participants aged 2–4 years decreased from 15.9 to 14.4% [50].
POLICY INTERVENTIONS TO IMPROVE HEALTH OUTCOMES FOR SUPPLEMENTAL NUTRITION ASSISTANCE PROGRAM PARTICIPANTS
There are three evidence-based policy changes that lawmakers should consider, and that pediatricians could support, to strengthen SNAP's effectiveness as a health intervention for children and families, build on the successes of WIC, CACFP and the NSLP and SBP, and help ensure that every child reaches the age of 18 at a healthy weight. First, policymakers should make diet quality a core SNAP objective and define and report on nutrition security. SNAP's current core objectives (food security and fiscal integrity) should be continued and supplemented with an additional, congressionally mandated focus on diet quality and healthy nutrition. Adding a diet-quality component to SNAP's current core objectives could be accomplished through the next Farm Bill (the omnibus, multiyear law that governs U.S. agricultural and food programs), an executive order, or a voluntary internal policy change at USDA. Once this core objective is in place, the USDA Economic Research Service (ERS) should include nutrition security in its annual reporting of US food security. Nutrition security should be defined using an evidence-based metric such as USDA's HEI (e.g. nutrition security defined as HEI of 80 or higher, nutrition insecurity at HEI between 80 and 60, and very low nutrition security defined as HEI below 60). In addition, the USDA should report on any policy changes that have been made to improve diet quality and nutrition, the impact of USDA policies on diet quality and healthy eating, and any additional authorities that the USDA has identified it needs in order to improve diet quality, nutrition, and healthy eating.
Second, policymakers should strengthen requirements for SNAP-authorized retailers to promote healthier retail food environments, especially for large retailers such as Walmart, Kroger, and Amazon. SNAP-authorized retailers are currently required to either stock three units of three different varieties for each staple food category (vegetables or fruits; dairy products; meat, poultry, or fish; breads or cereals) on a continuous basis or a store must have more than 50% of its total gross retail sales from the sale of staple foods [44]. Despite these requirements, research shows that SNAP authorized retailers offer comparatively fewer fresh fruits and vegetables, whole-grain foods and low-fat dairy products in lower income communities than retailers in higher income communities [51–55]. SNAP retailers should be prohibited from in-store (brick and mortar and on-line) marketing of unhealthy foods such as sugar-sweetened beverages (SSBs) (e.g. endcap displays and favored placement, including for online purchases).
Third, policymakers should support healthy purchases in SNAP by pairing incentives for purchasing fruits, vegetables, and other healthy foods with restrictions on unhealthy foods and sweetened beverages. Today, soft drinks are top commodity typically purchased by SNAP households [42]. Evidence suggests that restricting SSB purchases in SNAP could reduce the calories consumed from SSBs by 15% and reduce negative health consequences including obesity prevalence and diabetes [56]. A separate study of the impact of restricting SSBs on children's health found that if SSBs were substituted with fruit juice and milk, the restriction would be expected to reduce obesity prevalence among SNAP participants by 6.2 percentage points [57▪▪]. A randomized controlled trial found that pairing incentives for purchasing more fruits and vegetables with restrictions on the purchase of less nutritious foods (e.g. SSBs, sweet baked goods, candies) improved diet quality, reduced consumptions of SSBs and sweets, and increased fruit intake compared with individuals who made purchases with no restrictions or incentives [58].
A survey of public attitudes towards policies to improve the nutritional impact of SNAP, including SNAP participants, found that 82% of respondents supported providing additional benefits to SNAP participants that can only be used on healthful foods, 69% of respondents supported removing SNAP benefits for SSBs, and of the 46% of respondents who initially opposed removing SSBs, 45% supported removing SNAP benefits for SSBs if the policy also included additional benefits to purchase healthful foods [59].
Multiple-expert, nonpartisan bodies have supported one or more of these recommendations, including the National Commission on Hunger; the Bipartisan Policy Center; Healthy Eating Research; and the Report of the 50th Anniversary of the White House Conference on Food, Nutrition, and Health [60–63]. They also build on the recommendations of the Dietary Guidelines for Americans; the CDC; the National Academy of Medicine; and the WHO [64–67].
HOW PEDIATRICIANS CAN LEVERAGE THESE LEARNINGS
Pediatricians can act to improve SNAP's efficacy as a health intervention by urging the American Academy of Pediatrics (AAP) to advocate for the three aforementioned policy recommendations in its legislative priorities. They can also advocate individually and with their local colleagues to their Senator & Representative to make these changes in the 2023 Farm Bill. Pediatricians can become involved with their state SNAP-Education (SNAP-Ed) program (SNAP-Ed is USDA's largest nutrition-education and obesity-prevention program) and seek to have our three recommendations implemented at the state level using SNAP-Ed funds.
CONCLUSION
SNAP has demonstrated its benefit as an economic support for children and families to reduce food insecurity and allow for greater spending on other vital expenditures, such as healthcare. However, research suggests that there is an opportunity to improve its efficacy as a health intervention for children and families, in line with other federal food assistance programs.
Acknowledgements
Nourish Science (https://nourishscience.org/) for funding writing and open access.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1▪. Bryan S, Afful J, Carroll MD, et al. NHSR 158. National Health and Nutrition Examination Survey 2017–March 2020 Pre-pandemic Data Files. Hyattsville, MD, 2021. [Google Scholar]; This report presents prevalence estimates for child and adult obesity from the NHANES from 2017 to March 2020.
- 2.Mokdad AH, Ballestros K, Echko M, et al. The State of US Health, 1990–2016. JAMA 2018; 319:1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention. Adult Obesity Facts | Overweight & Obesity. Available at: https://www.cdc.gov/obesity/data/adult.html. [Accessed 02 September 2022] [Google Scholar]
- 4▪.O’Hearn M, Lauren BN, Wong JB, et al. Trends and disparities in cardiometabolic health among U.S. adults, 1999–2018. J Am Coll Cardiol 2022; 80:138–151. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study investigates US trends in optimal cardiometabolic health from 1999 to 2018.
- 5▪.O’Hearn M, Liu J, Cudhea F, et al. Coronavirus disease 2019 hospitalizations attributable to cardiometabolic conditions in the United States: a comparative risk assessment analysis. J Am Heart Assoc 2021; 10:1–27. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study estimates the absolute and proportional COVID-19 hospitalizations in US adults attributable to four major US cardiometabolic conditions, separately and jointly, and by race/ethnicity, age, and sex.
- 6. USDA ERS - Definitions of Food Security. Available at: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/definitions-of-food-security/. [Accessed 17 September 2022] [Google Scholar]
- 7▪. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States in 2021. 2022. [Google Scholar]; This report provides statistics on food security in US households throughout 2021 based on Current Population Survey Food Security Supplement data collected in December 2021.
- 8▪. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2020. 2021. https://www.ers.usda.gov/publications/pub-details/?pubid=102075. [Accessed 02 September 2022] [Google Scholar]; This report provides statistics on food security in U.S. households throughout 2020 based on Current Population Survey Food Security Supplement data collected in December 2020.
- 9.Geraghty AA, Lindsay KL, Alberdi G, et al. Nutrition during pregnancy impacts offspring's epigenetic status-evidence from human and animal studies. Nutr Metab Insights 2015; 8: (Suppl 1): 41–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pascoe JM, Wood DL, Duffee JH, Kuo A. Mediators and adverse effects of child poverty in the United States. Pediatrics 2016; 137:e20160340. [DOI] [PubMed] [Google Scholar]
- 11.Augusto ALP, de Abreu Rodrigues AV, Domingos TB, Salles-Costa R. Household food insecurity associated with gestational and neonatal outcomes: a systematic review. BMC Pregnancy Childbirth 2020; 20:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Drennen CR, Sharon M, Coleman MS, et al. Food insecurity, health, and development in children under age four years. Pediatrics 2019; 144:e20190824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: food insecurity, cost-related medication underuse, and unmet needs. Am J Med 2014; 127:303.e3–310.e3. [DOI] [PubMed] [Google Scholar]
- 14.Berkowitz SA, Basu S, Meigs JB, Seligman HK. Food insecurity and health care expenditures in the United States, 2011–2013. Health Serv Res 2018; 53:1600–1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peltz A, Garg A. Food insecurity and health care use. Pediatrics 2019; 144:e20190347. [DOI] [PubMed] [Google Scholar]
- 16.Herman D, Afulani P, Coleman-Jensen A, Harrison GG. Food insecurity and cost-related medication underuse among nonelderly adults in a nationally representative sample. Am J Public Health 2015; 105 (10):e48–e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff 2015; 34:1830–1839. [DOI] [PubMed] [Google Scholar]
- 18.Laraia BA. Food insecurity and chronic disease. Adv Nutr 2013; 4:203–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hanson KL, Connor LM. Food insecurity and dietary quality in US adults and children: a systematic review. Am J Clin Nutr 2014; 100:684–692. [DOI] [PubMed] [Google Scholar]
- 20. Text - H.R.2471-117th Congress (2021-2022): Consolidated Appropriations Act, 2022 | Congress.gov | Library of Congress. Available at: https://www.congress.gov/bill/117th-congress/house-bill/2471/text. [Accessed 02 September 2022] [Google Scholar]
- 21. United States Department of Agriculture. Percentage of participating SNAP households with children (FY 2018). Available at: https://www.fns.usda.gov/SNAP-State-characteristics. [Accessed 02 September 2022] [Google Scholar]
- 22. Center on Budget and Policy Priorities. A quick guide to SNAP eligibility and benefits. Available at: https://www.cbpp.org/research/food-assistance/a-quick-guide-to-snap-eligibility-and-benefits. [Accessed 02 September 2022] [Google Scholar]
- 23. United States Department of Agriculture. Where can I use SNAP EBT? Available at: https://www.fns.usda.gov/snap/retailer-locator. [accessed 02 September 2022] [Google Scholar]
- 24. United States Department of Agriculture. What can SNAP Buy? Available at: https://www.fns.usda.gov/snap/eligible-food-items. [Accessed 02 September 2022] [Google Scholar]
- 25. United States Department of Agriculture. Retailer eligibility - prepared foods and heated foods. Available at: https://www.fns.usda.gov/snap/retailer-eligibility-prepared-foods-and-heated-foods. [Accessed 02 September 2022] [Google Scholar]
- 26. United States Department of Agriculture. SNAP Data Tables. Available at: https://www.fns.usda.gov/pd/supplemental-nutrition-assistance-program-snap. [Accessed 02 September 2022] [Google Scholar]
- 27. United States Department of Agriculture. SNAP eligibility. Available at: https://www.fns.usda.gov/snap/recipient/eligibility. [Accessed 02 September 2022] [Google Scholar]
- 28. United States Department of Agriculture. USDA modernizes the thrifty food plan, updates SNAP Benefits. Available at: https://www.usda.gov/media/press-releases/2021/08/16/usda-modernizes-thrifty-food-plan-updates-snap-benefits. [Accessed 02 September 2022] [Google Scholar]
- 29. United States Department of Agriculture. SNAP and the Thrifty Food Plan. Available at: https://www.fns.usda.gov/snap/thriftyfoodplan. [Accessed 02 September 2022] [Google Scholar]
- 30. Ratcliffe C, McKernan S-M. How much does SNAP reduce food insecurity? 2010. Available at: https://www.researchgate.net/publication/44206966_How_much_does_SNAP_reduce_food_insecurity. [Accessed 2 September 2022] [Google Scholar]
- 31▪▪. Mabli J, Ohls J, Dragoset L, et al. Measuring the effect of Supplemental Nutrition Assistance Program (SNAP) participation on food security. Mathematica Policy Research Reports. 2022. Available at: https://ideas.repec.org/p/mpr/mprres/69d901432c7a46779666a240a0974a5d.html. [Accessed 2 September 2022] [Google Scholar]; This study uses survey data between October 2011 and September 2012 to assess how household food security and food expenditures vary with SNAP participation and examines how the relationship between SNAP and food security and between SNAP and food expenditures vary by key household characteristics and circumstances.
- 32.Almond D, Hoynes HW, Schanzenbach DW. Inside the war on poverty: the impact of food stamps on birth outcomes. Rev Econ Stat 2011; 93:387–403. [Google Scholar]
- 33.Bronchetti ET, Christensen G, Hoynes HW. Local food prices, SNAP purchasing power, and child health. J Health Econ 2019; 68:102231. [DOI] [PubMed] [Google Scholar]
- 34.Joyce KM, Breen A, de Cuba SE, et al. household hardships, public programs, and their associations with the health and development of very young children: insights from Children's HealthWatch. J Appl Res Child 2012; 3:2–24. [Google Scholar]
- 35. Children's Health Watch. The SNAP Vaccine: Boosting Children's Health. Available at: https://childrenshealthwatch.org/the-snap-vaccine-boosting-childrens-health/. [Accessed 02 September 2022] [Google Scholar]
- 36.de Cuba SE, Chilton M, Bovell-Ammon A, et al. Loss of SNAP is associated with food insecurity and poor health in working families with young children. Health Aff (Millwood) 2019; 38:765–773. [DOI] [PubMed] [Google Scholar]
- 37. United States Department of Agriculture. HEI Scores for Americans. Available at: https://www.fns.usda.gov/hei-scores-americans. [Accessed 2 September 2022] [Google Scholar]
- 38▪▪. United States Department of Agriculture. Indicators of Diet Quality, Nutrition, and Health for Americans by Program Participation Status, 2011–2016. Available at: https://www.fns.usda.gov/snap/indicators-diet-quality-nutrition-and-health-americans-program-participation-status-2011. [Accessed 30 December 2021] [Google Scholar]; This study uses NHANES data to examine the relationship between SNAP participation and indicators of diet quality, nutrition and health by comparing SNAP participants with income-eligible and higher income nonparticipants, by age and gender.
- 39.Leung CW, Blumenthal SJ, Hoffnagle EE, et al. Associations of food stamp participation with dietary quality and obesity in children. Pediatrics 2013; 131:463–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fang Zhang F, Liu J, Rehm CD, et al. Trends and disparities in diet quality among US adults by supplemental nutrition assistance program participation status. JAMA Netw Open 2018; 1:e180237–e1180237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Franckle RL, Moran A, Hou T, et al. Transactions at a Northeastern supermarket chain: differences by supplemental nutrition assistance program use. Am J Prev Med 2017; 53:e131–e138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. United States Department of Agriculture. Foods Typically Purchased by Supplemental Nutrition Assistance Program (SNAP) Households. 2016. Available at: https://www.fns.usda.gov/snap/foods-typically-purchased-supplemental-nutrition-assistance-program-snap-households. [Accessed 02 September 2022] [Google Scholar]
- 43.United States Department of Agriculture. Nutrition standards in the National School Lunch and School Breakfast Programs. Final rule. Fed Regist 2012; 77:4088–4167. [PubMed] [Google Scholar]
- 44.United States Department of Agriculture. National School Lunch Program and School Breakfast Program: Nutrition Standards for All Foods Sold in School as Required by the Healthy, Hunger-Free Kids Act of 2010. Final rule and interim final rule. Fed Regist 2016; 81:50131–50151. [PubMed] [Google Scholar]
- 45▪▪. United States Department of Agriculture. School Nutrition and Meal Cost Study. Available at: https://www.fns.usda.gov/school-nutrition-and-meal-cost-study. [Accessed April 2019] [Google Scholar]; This report presents findings from the School Nutrition and Meal Cost study, the first comprehensive, nationally representative study of the school meal programs since the Healthy Hunger-Free Kids Act reforms were implemented.
- 46.Cullen KW, Chen TA, Dave JM. Changes in foods selected and consumed after implementation of the new National School Lunch Program meal patterns in southeast Texas. Prev Med Rep 2015; 2:440–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Avruch S, Cackley AP. Savings achieved by giving WIC benefits to women prenatally. Public Health Rep 1995; 110:27–34. [PMC free article] [PubMed] [Google Scholar]
- 48.Khanani I, Elam J, Hearn R, et al. The impact of prenatal WIC participation on infant mortality and racial disparities. Am J Public Health 2010; 100: (Suppl 1): S204–S209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Andreyeva T, Luedicke J. Incentivizing fruit and vegetable purchases among participants in the Special Supplemental Nutrition Program for Women, Infants, and Children. Public Health Nutr 2015; 18:33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Centers for Disease Control and Prevention. Available at: obesity among young children enrolled in WIC. Available at: https://www.cdc.gov/obesity/data/obesity-among-WIC-enrolled-young-children.html#highweight. [Accessed 02 September 2022] [Google Scholar]
- 51.Shannon J. What does SNAP benefit usage tell us about food access in low-income neighborhoods? Soc Sci Med 2014; 107:89–99. [DOI] [PubMed] [Google Scholar]
- 52.Rigby S, Leone AF, Kim H, et al. Food Deserts in Leon County, FL: Disparate Distribution of Supplemental Nutrition Assistance Program-Accepting Stores by Neighborhood Characteristics. J Nutr Educ Behav 2012; 44:539–547. [DOI] [PubMed] [Google Scholar]
- 53.Laska MN, Caspi CE, Pelletier JE, et al. Lack of healthy food in small-size to mid-size retailers participating in the Supplemental Nutrition Assistance Program, Minneapolis–St. Paul, Minnesota, 2014. Prev Chronic Dis 2019; 12:150171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Caspi CE, Pelletier JE, Harnack L, et al. Differences in healthy food supply and stocking practices between small grocery stores, gas-marts, pharmacies and dollar stores. Public Health Nutr 2016; 19:540–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Racine EF, Batada A, Solomon CA, Story M. Availability of foods and beverages in Supplemental Nutrition Assistance Program−authorized dollar stores in a region of North Carolina. J Acad Nutr Diet 2016; 116:1613–1620. [DOI] [PubMed] [Google Scholar]
- 56.Basu S, Seligman HK, Gardner C, Bhattacharya J. Ending SNAP subsidies for sugar-sweetened beverages could reduce obesity and type 2 diabetes. Health Aff (Millwood) 2017; 33:1032–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57▪▪.Choi SE, Wright DR, Bleich SN. Impact of restricting sugar-sweetened beverages from the Supplemental Nutrition Assistance Program on Children's Health. Am J Prev Med 2021; 60:276–284. [DOI] [PubMed] [Google Scholar]; This study uses National Health and Nutrition Examination Survey data and a microsimulation model to assess expected impact of restricting sugar-sweetened beverage purchases with SNAP benefits on children's daily sugar-sweetened beverage consumption, total calorie intake, BMI, incidence of dental caries and obesity prevalence.
- 58.Harnack L, Oakes JM, Elbel B, et al. Effects of subsidies and prohibitions on nutrition in a food benefit program: a randomized clinical trial. JAMA Intern Med 2016; 176:1610–1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Long MW, Leung CW, Cheung LWY, et al. Public support for policies to improve the nutritional impact of the Supplemental Nutrition Assistance Program (SNAP). Public Health Nutr 2014; 17:219–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. N. Commission on Hunger. Freedom from hunger: an achievable goal for the United States of America. 2015. [Google Scholar]
- 61. Bipartisan Policy Center SNAP Task Force. Leading with nutrition: leveraging federal programs for better health. 2018. Available at: https://bipartisanpolicy.org/report/leading-with-nutrition-leveraging-federal-programs-for-betterhealth/. [Accessed 3 September 2022]. [Google Scholar]
- 62. Healthy Eating Research. Strengthening the Public Health Impacts of SNAP: Key Opportunities for the Next Farm Bill. 2021. Available at: https://healthyeatingresearch.org/research/strengthening-the-public-health-impacts-of-snapkey-opportunities-for-the-next-farm-bill/. [Accessed 3 September 2022] [Google Scholar]
- 63. Final Report on the 50th Anniversary of the White House Conference on Food, Nutrition, and Health: Honoring the Past, Taking Actions for our Future. 2020. Available at: https://sites.tufts.edu/foodnutritionandhealth2019/ [Accessed 3 September 2022] [Google Scholar]
- 64. U.S. Department of Health and Human Services Dietary Guidelines for Americans 2015-2020, “Cut Down on Added Sugars,” 2015. Available at: https://health.gov/sites/default/files/2019-10/DGA_Cut-Down-On-Added-Sugars.pdf. [Accessed 3 September 2022] [Google Scholar]
- 65. Centers for Disease Control and Prevention. Get the facts: sugar-sweetened beverages and consumption. Available at: https://www.cdc.gov/nutrition/data-statistics/sugar-sweetened-beverages-intake.html. [Accessed 03 September 2022] [Google Scholar]
- 66.Glickman D, Parker L, Sim LJ, et al. Committee on Accelerating Progress in Obesity Prevention; Food and Nutrition Board; Institute of Medicine. Accelerating progress in obesity prevention: solving the weight of the nation. Washington (DC): National Academies Press (US); 2012. [PubMed] [Google Scholar]
- 67. World Health Organization. Taxes on sugary drinks: why do it? 2017. Available at: http://apps.who.int/iris/bitstream/handle/10665/260253/WHO-NMH- ND-16.5Rev.1-eng.pdf. [Accessed 3 September 2022] [Google Scholar]